Abstract
Objectives
Subcutaneous fat necrosis of the newborn (SCFN) is a rare panniculitis that can affect newborn patients who have experienced perinatal stress, hypoxia, or hypothermia. Risk factors include gestational diabetes and pre-eclampsia. This condition is usually self-limiting; however, it can lead to severe complications, including hypercalcemia. After diagnosis, it is important to monitor calcium levels. There is no current standard for how frequently these levels should be monitored.
Case presentation
We present a full-term African American male with multiple risk factors, who was diagnosed with SCFN. The patient’s hypercalcemia secondary to SCFN led to renal complications.
Conclusions
This case highlights the importance of early and frequent monitoring of calcium levels in patients with SCFN.
Introduction
Subcutaneous fat necrosis of the newborn (SCFN) is a rare panniculitis that occurs within the first few weeks of life, often in full-term neonates who experience perinatal stress, hypoxia, or hypothermia [1]. This condition presents as erythematous nodules or plaques on the cheeks, back, buttocks, or proximal extremities [2]. SCFN is self-limiting; however, patients can develop complications including hypercalcemia and thrombocytopenia [1]. Although the etiology of this condition is unclear, it is thought to be due to perinatal stress interfering with the blood supply of the fat tissue, which leads to inflammation and necrosis [2]. Granulomatous infiltrates within these lesions increase the expression of 1-alpha-hydroxylase, which activates vitamin D3 and leads to the increased release of calcium [3]. When calcium levels exceed the kidneys’ excretion capacity, renal complications such as nephrolithiasis can occur [4]. Maternal risk factors include gestational diabetes, pre-eclampsia, cocaine and cigarette exposure, calcium blocker use, and familial dyslipidemia disorders [2].
SCFN can be diagnosed clinically or via biopsy, with radially arranged crystals in fat cells and lymphocytes on histopathology [3]. Treatments for cutaneous symptoms consist of supportive care and pain management as the lesions resolve within weeks [5]. Calcium monitoring is recommended for six months due to potential complications of hypercalcemia including renal failure, cardiac arrest, and metastatic calcifications [2, 6]. Recommended managements for hypercalcemia consist of calcium-wasting loop diuretics, steroids, bisphosphonates, and calcitonin depending on the severity of lab abnormalities [5]. Despite the potential complications of hypercalcemia, there are no current standards for the frequency of calcium monitoring. This case presents an infant with hypercalcemia and renal complications secondary to SCFN, which highlights the importance of early and frequent monitoring of calcium levels in patients with this diagnosis.
Case presentation
A 2.905 kg African American male was delivered by a 42-year-old G2P1 female at 37 weeks with a history of chronic hypertension with superimposed severe pre-eclampsia, gestational diabetes, tobacco use during pregnancy, and a BMI greater than 40 kg/m2. The patient was delivered via primary cesarian section due to non-reassuring fetal heart tones and lack of cervical dilation. The patient was initially hypotonic and apneic with APGAR scores of 2, 6, and 9 at 1, 5, and 10 min, respectively. Resuscitation efforts included deep suction, positive pressure ventilation for 2 min, and continuous positive airway pressure for 5 min, before transitioning to room air. He was transferred to the ICU for treatment of hypoglycemia despite feedings, hypothermia, respiratory distress, and concern for sepsis. His lowest serum glucose measurement was <5 mg/dL at 2 h of life, which was treated with two boluses of 6 mL of Dextrose 10% in water. The patient’s hypoglycemia management required a peripherally inserted central catheter with a maximum glucose infusion rate of 11.3 mg/kg/min for 12 h on his second day of life, his blood glucose stabilized six days later. On day 4, dermatology was consulted for new tender, flat, violaceous, plaque-like lesions on the bilateral cheeks, shoulders, and buttocks (Figure 1). The facial and shoulder lesions were firm and well demarcated (Figure 2). They determined that the diagnosis was likely SCFN and recommended supportive care with serial calcium monitoring. His serum calcium was within normal limits on day 4 and 5, but he had thrombocytopenia with a platelet count of 23 × 109/L, which was attributed to SCFN.
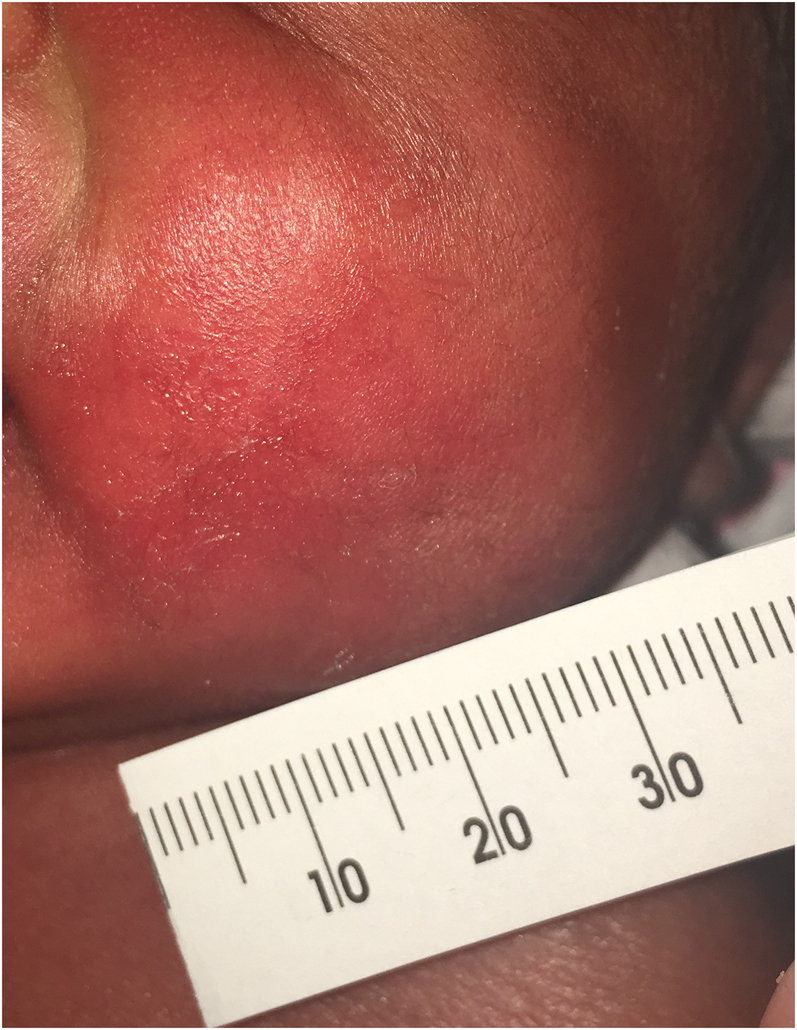
A tender, flat, violaceous, plaque-like lesion on the left cheek that appeared on day 4.

A firm, well demarcated plaque-like lesion on the right shoulder.
On day 12, dermatology was consulted again to examine a scaly eruption of unknown etiology over the affected areas which was managed with hydrocortisone 2.5% cream and hydrophilic topicals (Figure 3). A punch biopsy was obtained, which confirmed subcutaneous fat necrosis with crystals and focal lymphohistiocytic inflammation (Figure 4). Dermatology again recommended daily calcium monitoring with pediatric endocrinology follow up. His serum calcium was next checked on day 14 and 17, both levels were elevated at 11.9 and 13.2 mg/dL, respectively (normal 8.8–11.3 mg/dL) [7]. His ionized calcium was also elevated to 1.64 mmol/L at this time, but serum magnesium, phosphorous, alkaline phosphatase, and albumin were within normal limits. Throughout this time, the patient did have symptoms of hypercalcemia, as he was exhibiting feeding intolerance due to signs of gastrointestinal reflux and immature oromotor skills requiring partial gavage. On day 17, pediatric endocrinology was consulted for hypercalcemia; he was treated with furosemide and switched to a low calcium formula. His platelet count normalized on day 18. His serum calcium levels were monitored every 12 h and peaked at 13.9 mg/dL on day 20. A 2 mg/kg per day dose of oral prednisolone was added to his treatment regimen for two months, then decreased to 0.4 mg/kg for two weeks before discontinuing.

A scaly eruption on the previously affected areas of the left cheek.
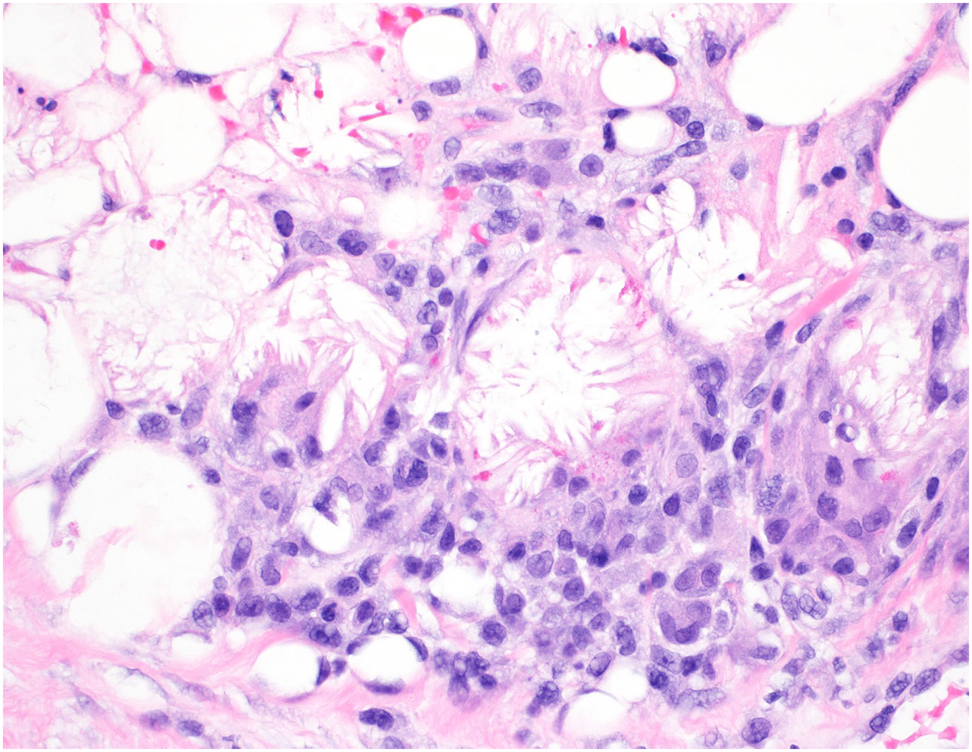
Histology of the left hip revealed subcutaneous fat necrosis with crystals and focal lymphohistiocytic inflammation.
On day 22, nephrology was consulted, and the patient received a renal ultrasound which showed 3 mm non-obstructive renal calculi without nephrocalcinosis, likely secondary to SCFN related hypercalcemia. The patient was also hyponatremic and hypokalemic due to the low calcium formula. They recommended a three-month ultrasound follow-up, as the calculi would likely pass on their own. By day 26, his serum calcium levels had decreased to 10.6 mg/dL and he was able to discontinue furosemide on the next day.
Conclusions
The patient had multiple risk factors for SCFN including perinatal stress, hypoxia, hypothermia, maternal diabetes, pre-eclampsia, and cigarette use during pregnancy, and was diagnosed on initial presentation. However, he was not closely monitored for hypercalcemia and was 0.1 mg/dL below the threshold for a hypercalcemic crisis at his peak [6]. Although his serum calcium was within normal limits at the time of his diagnosis, it was likely trending upward for several days until it was checked again nine days later. A systematic review showed that more than half of infants who are diagnosed with SCFN develop hypercalcemia [6]. In 95% of these cases, hypercalcemia developed within 60 days after the onset of the skin lesions [6]. This indicates the importance of monitoring calcium, even in asymptomatic SCFN patients, given the high rate of elevated levels. Several studies have recommended six months of calcium screening after diagnosis of SCFN, however there is no standard of care for the frequency of these screenings in an inpatient setting.
In this case, late identification of increased calcium levels may have led to renal complications. Although the resulting calculi were small and did not require extensive treatment, if they progressed to 5 mm, they would require surgical intervention [8]. Untreated hypercalcemia can also lead to seizures, electrolyte imbalances, arrythmias, hypotonia, and failure to thrive [4]. This case indicates that daily screening and early identification of hypercalcemia after a diagnosis of SCFN can lead to earlier treatment and prevention of sequelae.
This case highlights the importance of early identification and management of SCFN, which can help prevent potentially severe complications, including hypercalcemia. Due to the high rates of hypercalcemia associated with this condition, it is important to closely monitor patient’s calcium levels after their initial diagnosis. Parents of patients with many risk factors for SCFN should also be educated on signs of these lesions after discharge to assist with early identification and monitoring.
-
Research funding: None declared.
-
Author contributions: All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Competing interests: Authors state no conflict of interest.
-
Informed consent: Informed consent was obtained from all individuals included in this study.
-
Ethical approval: The local Institutional Review Board deemed the study exempt from review.
References
1. Del Pozzo-Magaña, BR, Ho, N. Subcutaneous fat necrosis of the newborn: a 20-year retrospective study. Pediatr Dermatol 2016;33:e353–e355. https://doi.org/10.1111/pde.12973.Search in Google Scholar PubMed
2. Lara, LG, Villa, AV, Rivas, MM, Capella, MS, Prada, F, Enseñat, MA. Subcutaneous fat necrosis of the newborn: report of five cases. Pediatr Neonatol 2017;58:85–8. https://doi.org/10.1016/j.pedneo.2014.06.010.Search in Google Scholar PubMed
3. Chikaodinaka, AA, Jude, AC. Subcutaneous fat necrosis of the newborn: a case report of a term infant presenting with malaise and fever at age of 9 weeks. Case Rep Pediatr 2015;2015:638962. https://doi.org/10.1155/2015/638962.Search in Google Scholar PubMed PubMed Central
4. Lee, DB, Zawada, ET, Kleeman, CR. The pathophysiology and clinical aspects of hypercalcemic disorders. West J Med 1978;129:278–320.Search in Google Scholar
5. Alsofyani, KA. Neonatal subcutaneous fat necrosis with hypercalcemia treatment using calcitonin. Saudi Med J 2018;39:622–6. https://doi.org/10.15537/smj.2018.6.22025.Search in Google Scholar PubMed PubMed Central
6. Stefanko, NS, Drolet, BA. Subcutaneous fat necrosis of the newborn and associated hypercalcemia: a systematic review of the literature. Pediatr Dermatol 2019;36:24–30. https://doi.org/10.1111/pde.13640.Search in Google Scholar PubMed
7. Lietman, SA, Germain-Lee, EL, Levine, MA. Hypercalcemia in children and adolescents. Curr Opin Pediatr 2010;22:508–15. https://doi.org/10.1097/MOP.0b013e32833b7c23.Search in Google Scholar PubMed PubMed Central
8. Erturhan, S, Bayrak, O, Sarica, K, Seckiner, I, Baturu, M, Sen, H. Efficacy of medical expulsive treatment with doxazosin in pediatric patients. Urology 2013;81:640–3. https://doi.org/10.1016/j.urology.2012.11.031.Search in Google Scholar PubMed
© 2021 Nicole A. Karikari and FNU Nutan, published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Editorial
- The journal Case Reports in Perinatal Medicine starts with open access
- Case Reports – Obstetrics
- Myomectomy scar pregnancy ‒ a serious, but scarcely reported entity: literature review and an instructive case
- Postpartum ovarian vein thrombosis
- Management of a patient in the state of total occlusion of aorta due to Takayasu arteritis in preconceptional and pregnancy period
- Stress degree demonstrated in mothers with phenylketonuria or hyperphenylalaninemia infant when requested for total or partial breastfeeding replacement
- Successful pregnancy outcome in patient with cardiac transplantation
- Further insights into unusual acrania-exencephaly-anencephaly sequence caused by amniotic band – first trimester fetoscopic correlation with two- and three-dimensional ultrasound
- Elevated fetal middle cerebral artery peak systolic velocity in diabetes type 1 patient: a case report
- Postpartum fibroid degeneration associated with elevated procalcitonin levels
- Case report: The first COVID-19 case among pregnant women at 21-week in Vietnam
- Posterior urethral valves (PUVs): prenatal ultrasound diagnosis and management difficulties: a review of three cases
- Premature fetal closure of the ductus arteriosus of unknown cause – could it be influenced by maternal consumption of large quantities of herbal chamomile tea – a case report?
- Spontaneous resolution of fetal ascites secondary to gastrointestinal abnormality
- A case of severe SARS-CoV-2 infection with negative nasopharyngeal PCR in pregnancy
- Respiratory decompensation due to COVID-19 requiring postpartum extracorporeal membrane oxygenation
- Obstetrical history of a family with combined oxidative phosphorylation deficiency 3 and methylenetetrahydrofolate reductase polymorphisms
- A case of newly diagnosed autoimmune diabetes in pregnancy presenting after acute onset of diabetic ketoacidosis
- Mother and child with osteogenesis imperfecta type III. Pregnancy management, delivery, and outcome
- Early detection of Emanuel syndrome: a case report
- Case Reports – Newborn
- Neonatal cervical lymphatic malformation involving the fetal airway the setting of emergency caesarean section
- Rothia dentocariosa bacteremia in the newborn: causative pathogen or contaminant?
- Severe hypocalcemia and seizures after normalization of pCO2 in a patient with severe bronchopulmonary dysplasia and permissive hypercapnia
- Infrequent association of two rare diseases: amniotic band syndrome and osteogenesis imperfecta
- Transient congenital Horner syndrome and multiple peripheral nerve injury: a scarcely reported combination in birth trauma
- No footprint too small: case of intrauterine herpes simplex virus infection
- Liver laceration presented as intraabdominal bleeding in a newborn with hypoxic-ischemic encephalopathy
- Extremely preterm infant with persistent peeling skin: X-linked ichthyosis imitates prematurity
- Thrombospondin domain1-related congenital chylothorax in an infant with maple syrup urine disease: a challenging case
- Parenteral nutrition extravasation into the abdominal wall mimicking an abscess
- Subcutaneous fat necrosis of the newborn and nephrolithiasis
- Fetal MRI assessment of head & neck vascular malformation in predicting outcome of EXIT-to-airway procedure
- Scimitar syndrome – a case report
- Asymptomatic severe laryngotracheoesophageal cleft (LTEC) in a preterm newborn
- Transient generalized proximal tubular dysfunction in an infant with a urinary tract infection: the effect of maternal infliximab therapy?
- Congenital Lobular Capillary Hemangioma in a 48 hours old neonate: a case report and a literature review
- Neonate born with ischemic limb to a COVID-19 positive mother: management and review of literature
Articles in the same Issue
- Editorial
- The journal Case Reports in Perinatal Medicine starts with open access
- Case Reports – Obstetrics
- Myomectomy scar pregnancy ‒ a serious, but scarcely reported entity: literature review and an instructive case
- Postpartum ovarian vein thrombosis
- Management of a patient in the state of total occlusion of aorta due to Takayasu arteritis in preconceptional and pregnancy period
- Stress degree demonstrated in mothers with phenylketonuria or hyperphenylalaninemia infant when requested for total or partial breastfeeding replacement
- Successful pregnancy outcome in patient with cardiac transplantation
- Further insights into unusual acrania-exencephaly-anencephaly sequence caused by amniotic band – first trimester fetoscopic correlation with two- and three-dimensional ultrasound
- Elevated fetal middle cerebral artery peak systolic velocity in diabetes type 1 patient: a case report
- Postpartum fibroid degeneration associated with elevated procalcitonin levels
- Case report: The first COVID-19 case among pregnant women at 21-week in Vietnam
- Posterior urethral valves (PUVs): prenatal ultrasound diagnosis and management difficulties: a review of three cases
- Premature fetal closure of the ductus arteriosus of unknown cause – could it be influenced by maternal consumption of large quantities of herbal chamomile tea – a case report?
- Spontaneous resolution of fetal ascites secondary to gastrointestinal abnormality
- A case of severe SARS-CoV-2 infection with negative nasopharyngeal PCR in pregnancy
- Respiratory decompensation due to COVID-19 requiring postpartum extracorporeal membrane oxygenation
- Obstetrical history of a family with combined oxidative phosphorylation deficiency 3 and methylenetetrahydrofolate reductase polymorphisms
- A case of newly diagnosed autoimmune diabetes in pregnancy presenting after acute onset of diabetic ketoacidosis
- Mother and child with osteogenesis imperfecta type III. Pregnancy management, delivery, and outcome
- Early detection of Emanuel syndrome: a case report
- Case Reports – Newborn
- Neonatal cervical lymphatic malformation involving the fetal airway the setting of emergency caesarean section
- Rothia dentocariosa bacteremia in the newborn: causative pathogen or contaminant?
- Severe hypocalcemia and seizures after normalization of pCO2 in a patient with severe bronchopulmonary dysplasia and permissive hypercapnia
- Infrequent association of two rare diseases: amniotic band syndrome and osteogenesis imperfecta
- Transient congenital Horner syndrome and multiple peripheral nerve injury: a scarcely reported combination in birth trauma
- No footprint too small: case of intrauterine herpes simplex virus infection
- Liver laceration presented as intraabdominal bleeding in a newborn with hypoxic-ischemic encephalopathy
- Extremely preterm infant with persistent peeling skin: X-linked ichthyosis imitates prematurity
- Thrombospondin domain1-related congenital chylothorax in an infant with maple syrup urine disease: a challenging case
- Parenteral nutrition extravasation into the abdominal wall mimicking an abscess
- Subcutaneous fat necrosis of the newborn and nephrolithiasis
- Fetal MRI assessment of head & neck vascular malformation in predicting outcome of EXIT-to-airway procedure
- Scimitar syndrome – a case report
- Asymptomatic severe laryngotracheoesophageal cleft (LTEC) in a preterm newborn
- Transient generalized proximal tubular dysfunction in an infant with a urinary tract infection: the effect of maternal infliximab therapy?
- Congenital Lobular Capillary Hemangioma in a 48 hours old neonate: a case report and a literature review
- Neonate born with ischemic limb to a COVID-19 positive mother: management and review of literature

