Abstract
Objectives
X-linked ichthyosis (XLI) is a genetic disorder caused by a deficiency in steroid sulfatase, an enzyme which catalyzes a reaction in estrone synthesis. The disorder primarily manifests as dry, scaly skin which may be difficult to diagnose in extremely preterm infants, as the dermatological features may be falsely attributed to a normal variant of skin for this population.
Case presentation
In this case report, we describe a male with XLI, born at 24 weeks gestation, who had persistent dry, flaky and hyperpigmented skin. This case is notable for the age of diagnosis in an extremely premature infant; day of life 105. In addition, this infant experienced out of proportion bronchopulmonary symptoms that we postulate may be linked to the steroid sulfatase deficiency, as estrogen is a mediator of surfactant production.
Conclusions
This report underscores the need to potentially evaluate persistent dry, flaky skin in the preterm infant, as XLI may also impact long term neurodevelopmental outcomes.
Introduction
X-linked ichthyosis (XLI) is a disorder of keratinization characterized by generalized scaling of the skin with extracutaneous manifestations, inherited in an X-linked recessive manner [1]. The prevalence of XLI is about 1 in 4,000 male births, and almost exclusively affects males [2]. In 90% of cases, a deletion in the steroid sulfatase (STS) gene is implicated [2]. Adjacent genes may be affected depending on the size and location of the deletion, leading to associations with Kallmann Syndrome (hypogonadotropic hypogonadism, hearing loss, color blindness, and impaired sense of smell due to a gonadotropin releasing hormone deficiency), cryptorchidism, attention deficit hyperactivity disorder (ADHD), and autism spectrum disorder [3]. XLI is one of the most common forms of ichthyosis, along with ichthyosis vulgaris [1].
The typical clinical presentation is characterized by dry, scaly skin which becomes more pigmented over time [1]. Since dry and flaky skin in extremely preterm infants is common, identification of XLI creates a diagnostic challenge in this population [4]. The diagnosis can be made through a skin biopsy which tests STS activity levels, or through mutation analysis of the STS gene on the X chromosome [1]. Skin biopsies are often nonspecific and challenging in extremely preterm infants, and therefore genetic testing is increasingly relied on for diagnosis [4]. This case report describes a 24 week gestation male who presented with dry peeling skin and was subsequently diagnosed with XLI via genetic testing on day of life 105 (39 weeks postmenstrual age). To our knowledge, this case report documents both the most preterm infant and earliest postnatal age of XLI diagnosis, while highlighting a potential novel association with pulmonary findings.
Case presentation
A 25-year-old mother gravida 3 para 0020 presented at 24 weeks gestation with preterm premature rupture of membranes. The mother's past medical history was notable for obesity and pre-eclampsia. One course of antenatal steroids and magnesium sulfate were administered 22 h prior to delivery. On the day of delivery, labor was induced due to signs of chorioamnionitis. The labor period was prolonged for two days in this case, which is common during the delivery of infants with XLI [5]. Mothers of babies with XLI often have a delayed delivery or failed induction of labor leading to cesarean delivery due to low levels of estrogen secondary to low STS activity [5]. The infant was delivered vaginally at 24 and 2/7 weeks gestation and required chest compressions, intubation, and positive pressure ventilation prior to transfer to the neonatal intensive care unit. Apgar scores were 1, 1, 2, and 7 at 1, 5, 10, and 20 min, respectively.
The physical exam revealed cryptorchidism, which is common in preterm infants, but also attributable to XLI and adjacent gene deletion. The initial skin exam noted pink, thin, translucent and sticky skin, with scattered petechiae on extremities, consistent with extreme prematurity. Dry and flaky skin was visible on the chest as early as day of life 9, with hyperpigmentation on the lower extremities on day of life 81 (Figure 1). On day of life 105, chromosomal microarray revealed a 1.7 megabase deletion at Xp22.31, which included the STS gene and confirmed the diagnosis of XLI. The patient's mother was subsequently found to be a carrier of the deletion via fluorescence in situ hybridization, excluding a novel mutation in the infant. In addition, the family history was notable for dry and scaly skin in the patient's maternal uncle.
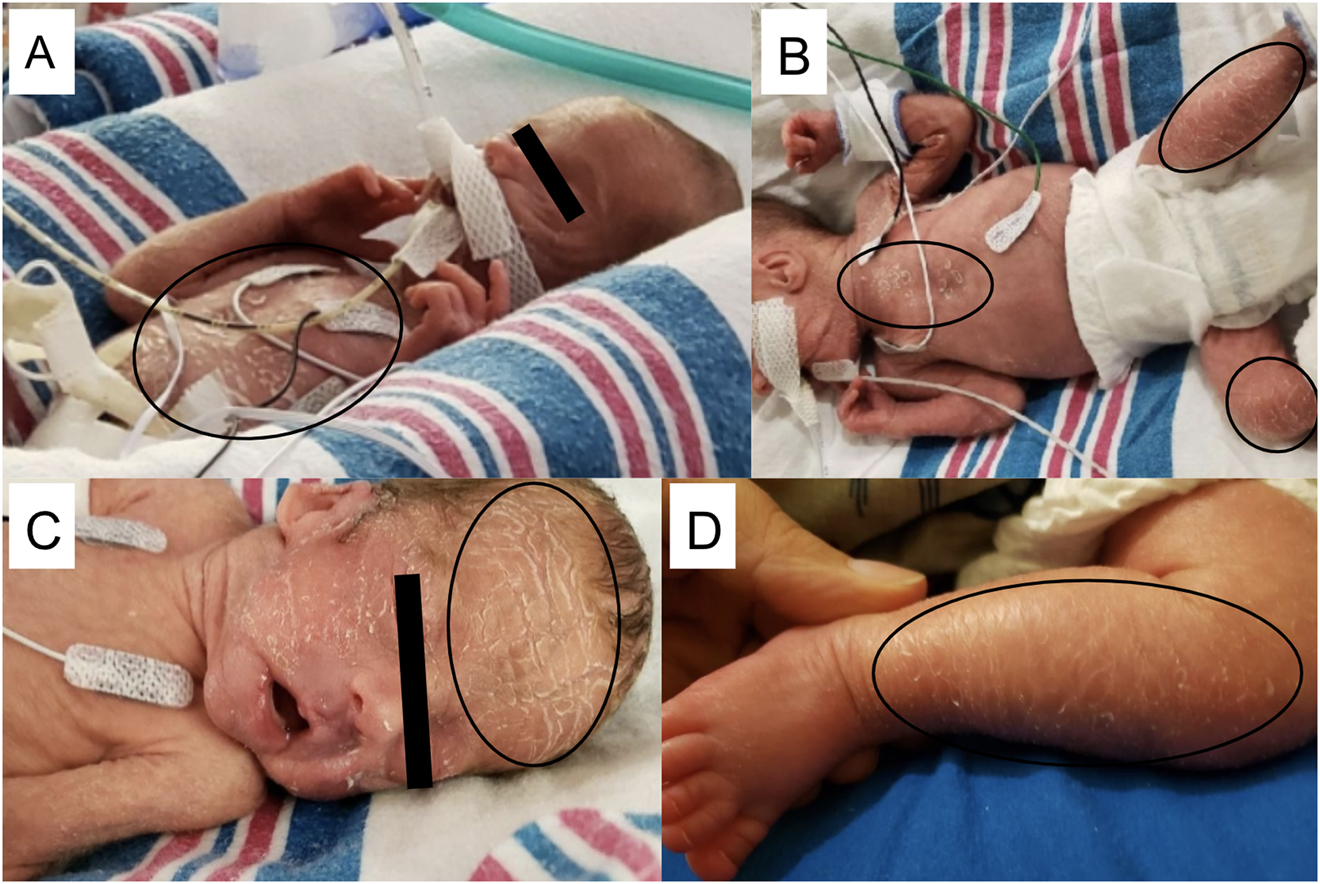
X-Linked ichthyosis imitates prematurity: time lapse of physical exam during NICU hospitalization.Dry, peeling skin on day of life 9 (A), day of life 17 (B), day of life 29 (C). Hyperpigmentation and scales seen on lower extremities on day of life 81 (D).
Despite the high degree of prematurity, the patient's respiratory course was out of proportion for the infant's gestational age and receipt of antenatal steroids. After receiving two doses of surfactant therapy, the infant failed conventional mechanical ventilation, and was quickly escalated to high frequency ventilation and developed pulmonary interstitial emphysema. Postnatal steroids were started on day of life 14, which resulted in the infant transitioning to a conventional ventilator. A second course of postnatal betamethasone one month later resulted in successful extubation to noninvasive ventilation. At 36 weeks post menstrual age (PMA), the patient was diagnosed with bronchopulmonary dysplasia, requiring nasal intermittent positive pressure ventilation with an FiO2 of 23%. He was discharged on day of life 135 (43 weeks PMA) on ¼ liter FiO2 100% as well as inhaled budesonide, with no evidence of pulmonary hypertension. To our knowledge, there are no other reported cases of a child with XLI and severe respiratory problems.
On day of life 56, the ophthalmic exam revealed stage one retinopathy of prematurity (ROP) in zone two. In a subsequent eye exam, there was stage two ROP in zone one bilaterally, for which the patient underwent corrective laser surgery. Interestingly, corneal opacity, a hallmark symptom, was not present in this patient.
Upon follow-up examination at adjusted age 8 months, the patient was weaned off oxygen and prescribed albuterol sulfate 2.5 mg/3 mL solution for three times daily usage. His ROP which was initially treated with laser surgery was found to have regressed. The patient's ichthyosis rash was controlled with petrolatum ointment daily as well as a steroid cream when necessary. He is receiving occupational therapy to ensure that he continues to meet his adjusted milestones, and his behavior was appropriate for his age.
Discussion
X-linked ichthyosis is a rare genetic condition caused by a deletion in the steroid sulfatase gene [2]. This STS deficiency manifests cutaneously as dry, scaly, pigmented skin in neonates [1]. Since it is common for desquamation and large scales to appear on the skin of very premature infants up to several weeks postnatally, XLI is challenging to diagnose in very preterm infants [4]. The differential diagnosis of preterm infants with dry, scaly skin includes cutaneous candidiasis, congenital ichthyosis including ichthyosis prematurity syndrome and congenital ichthyosiform erythroderma, or a bacterial infection such as Staphylococcal scalded skin syndrome [1, 4]. Management of cutaneous symptoms in neonates and infants is limited to maintaining skin hydration and use of emollients to decrease scale formation [2].
To date, the most premature infant reported in the literature with XLI was a 28 week gestation male diagnosed at 11 years of age [6]. His clinical findings included dry skin with peeling scales in addition to neurodevelopmental issues, including psychosis, intellectual disability, autism spectrum disorder, inattentive ADHD, and epilepsy [6]. The neurodevelopmental findings are consistent with other case reports, which note XLI associated with ADHD, autism, epilepsy, and other psychiatric disorders. For example, our patient had the same 1.7 megabase deletion at Xp22.31 as a patient in another case report, encompassing six genes; STS, PUDP, MIR4767, VCX, PNPLA4, and MIR651. This patient later presented with ADHD and mild autism in addition to the classic cutaneous features of XLI [7]. At an adjusted age 8 months, our patient has development appropriate for his age, yet this deletion necessitates the need for long term neurodevelopmental surveillance.
The severity of our patient's lung disease may also be attributable to the STS gene defect reported in XLI. While there are no reported studies specifically linking XLI to lung disease, STS is constitutively expressed in the lungs [8]. The role of STS is to hydrolyze estrone sulfate and dehydroepiandrosterone sulfate to estrone and dehydroepiandrosterone, which is a crucial step in the synthesis of estrogen from its inactive precursor in human tissues [5]. Estrogen plays an important role in formation of lamellar bodies and release of surfactant [9]. In fetal rabbit lung tissue, estrogen stimulates the synthesis and release of surface active phospholipids and development of lamellar bodies [9]. In addition, glucocorticoids have been shown to decrease STS activity and expression in certain cells, which may partially explain our patient's poor response to both antenatal and postnatal steroid treatment [10]. Given that XLI has behavioral and developmental manifestations that have been attributed to decreased expression of STS in brain tissue, we cannot exclude the possibility that there may be a link to lung disease as well. Moving forward, this patient will continue to be monitored for neurodevelopmental delays as well as respiratory issues.
Conclusions
X-linked ichthyosis is a rare genetic condition that can have varying presentations at birth and can be exceptionally difficult to diagnose in a premature infant. In this case report, we outline the presentation and early diagnosis of a premature baby with XLI and bronchopulmonary disease. Clinicians should be aware of the expression of STS in other tissues, including the brain and lung, in order to understand that there can be an association between XLI and further clinical problems.
-
Research funding: None declared.
-
Author contributions: All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Competing interests: Authors state no conflict of interest.
-
Informed consent: Not applicable.
-
Ethical approval: Not applicable.
References
1. Fernandes, NF, Janniger, CK, Schwartz, RA. X-linked ichthyosis: an oculocutaneous genodermatosis. J Am Acad Dermatol 2010;62:480. https://doi.org/10.1016/j.jaad.2009.04.028.Search in Google Scholar PubMed
2. Traupe, H, Fischer, J, Oji, V. Nonsyndromic types of ichthyoses - an update. J Dtsch Dermatol Ges 2014;12:109–21. https://doi.org/10.1111/ddg.12229.Search in Google Scholar PubMed
3. Kent, L, Emerton, J, Bhadravathi, V, Weisblatt, E, Pasco, G, Willatt, LR, et al.. X-linked ichthyosis (steroid sulfatase deficiency) is associated with increased risk of attention deficit hyperactivity disorder, autism and social communication deficits. J Med Genet 2008;45:519–24. https://doi.org/10.1136/jmg.2008.057729.Search in Google Scholar PubMed
4. Craiglow, BG. Ichthyosis in the newborn. Semin Perinatol 2013;37:26–31. https://doi.org/10.1053/j.semperi.2012.11.001.Search in Google Scholar PubMed PubMed Central
5. Dreyer, F, Abdulrahman, GO, Waring, G, Hinshaw, K. Placental steroid sulphatase deficiency: an approach to antenatal care and delivery. Ann Saudi Med 2018;38:445–9. https://doi.org/10.5144/0256-4947.2018.445.Search in Google Scholar PubMed PubMed Central
6. Malik, A, Amer, AB, Salama, M, Haddad, B, Alrifai, MT, Balwi, MA, et al.. X-linked ichthyosis associated with psychosis and behavioral abnormalities: a case report. J Med Case Rep 2017;11:267–2. https://doi.org/10.1186/s13256-017-1420-2.Search in Google Scholar PubMed PubMed Central
7. Baek, WS, Aypar, U. Neurological manifestations of X-linked ichthyosis: case report and review of the literature. Case Rep Genet 2017;2017:9086408. https://doi.org/10.1155/2017/9086408.Search in Google Scholar PubMed PubMed Central
8. Fagerberg, L, Hallström, BM, Oksvold, P, Kampf, C, Djureinovic, D, Odeberg, J, et al.. Analysis of the human tissue-specific expression by genome-wide integration of transcriptomics and antibody-based proteomics. Mol Cell Proteomics 2014;13:397–406. https://doi.org/10.1074/mcp.m113.035600.Search in Google Scholar PubMed PubMed Central
9. Thuresson-Klein, A, Moawad, AH, Hedqvist, P. Estrogen stimulates formation of lamellar bodies and release of surfactant in the rat fetal lung. Obstet Gynecol 1985;151:506–14. https://doi.org/10.1016/0002-9378(85)90279-0.Search in Google Scholar PubMed
10. Dias, NJ, Selcer, KW. Steroid sulfatase in the human MG-63 preosteoblastic cell line: antagonistic regulation by glucocorticoids and NFκB. Mol Cell Endocrinol 2016;420:85–96. https://doi.org/10.1016/j.mce.2015.11.029.Search in Google Scholar PubMed
© 2021 Walter de Gruyter GmbH, Berlin/Boston
Articles in the same Issue
- Editorial
- The journal Case Reports in Perinatal Medicine starts with open access
- Case Reports – Obstetrics
- Myomectomy scar pregnancy ‒ a serious, but scarcely reported entity: literature review and an instructive case
- Postpartum ovarian vein thrombosis
- Management of a patient in the state of total occlusion of aorta due to Takayasu arteritis in preconceptional and pregnancy period
- Stress degree demonstrated in mothers with phenylketonuria or hyperphenylalaninemia infant when requested for total or partial breastfeeding replacement
- Successful pregnancy outcome in patient with cardiac transplantation
- Further insights into unusual acrania-exencephaly-anencephaly sequence caused by amniotic band – first trimester fetoscopic correlation with two- and three-dimensional ultrasound
- Elevated fetal middle cerebral artery peak systolic velocity in diabetes type 1 patient: a case report
- Postpartum fibroid degeneration associated with elevated procalcitonin levels
- Case report: The first COVID-19 case among pregnant women at 21-week in Vietnam
- Posterior urethral valves (PUVs): prenatal ultrasound diagnosis and management difficulties: a review of three cases
- Premature fetal closure of the ductus arteriosus of unknown cause – could it be influenced by maternal consumption of large quantities of herbal chamomile tea – a case report?
- Spontaneous resolution of fetal ascites secondary to gastrointestinal abnormality
- A case of severe SARS-CoV-2 infection with negative nasopharyngeal PCR in pregnancy
- Respiratory decompensation due to COVID-19 requiring postpartum extracorporeal membrane oxygenation
- Obstetrical history of a family with combined oxidative phosphorylation deficiency 3 and methylenetetrahydrofolate reductase polymorphisms
- A case of newly diagnosed autoimmune diabetes in pregnancy presenting after acute onset of diabetic ketoacidosis
- Mother and child with osteogenesis imperfecta type III. Pregnancy management, delivery, and outcome
- Early detection of Emanuel syndrome: a case report
- Case Reports – Newborn
- Neonatal cervical lymphatic malformation involving the fetal airway the setting of emergency caesarean section
- Rothia dentocariosa bacteremia in the newborn: causative pathogen or contaminant?
- Severe hypocalcemia and seizures after normalization of pCO2 in a patient with severe bronchopulmonary dysplasia and permissive hypercapnia
- Infrequent association of two rare diseases: amniotic band syndrome and osteogenesis imperfecta
- Transient congenital Horner syndrome and multiple peripheral nerve injury: a scarcely reported combination in birth trauma
- No footprint too small: case of intrauterine herpes simplex virus infection
- Liver laceration presented as intraabdominal bleeding in a newborn with hypoxic-ischemic encephalopathy
- Extremely preterm infant with persistent peeling skin: X-linked ichthyosis imitates prematurity
- Thrombospondin domain1-related congenital chylothorax in an infant with maple syrup urine disease: a challenging case
- Parenteral nutrition extravasation into the abdominal wall mimicking an abscess
- Subcutaneous fat necrosis of the newborn and nephrolithiasis
- Fetal MRI assessment of head & neck vascular malformation in predicting outcome of EXIT-to-airway procedure
- Scimitar syndrome – a case report
- Asymptomatic severe laryngotracheoesophageal cleft (LTEC) in a preterm newborn
- Transient generalized proximal tubular dysfunction in an infant with a urinary tract infection: the effect of maternal infliximab therapy?
- Congenital Lobular Capillary Hemangioma in a 48 hours old neonate: a case report and a literature review
- Neonate born with ischemic limb to a COVID-19 positive mother: management and review of literature
Articles in the same Issue
- Editorial
- The journal Case Reports in Perinatal Medicine starts with open access
- Case Reports – Obstetrics
- Myomectomy scar pregnancy ‒ a serious, but scarcely reported entity: literature review and an instructive case
- Postpartum ovarian vein thrombosis
- Management of a patient in the state of total occlusion of aorta due to Takayasu arteritis in preconceptional and pregnancy period
- Stress degree demonstrated in mothers with phenylketonuria or hyperphenylalaninemia infant when requested for total or partial breastfeeding replacement
- Successful pregnancy outcome in patient with cardiac transplantation
- Further insights into unusual acrania-exencephaly-anencephaly sequence caused by amniotic band – first trimester fetoscopic correlation with two- and three-dimensional ultrasound
- Elevated fetal middle cerebral artery peak systolic velocity in diabetes type 1 patient: a case report
- Postpartum fibroid degeneration associated with elevated procalcitonin levels
- Case report: The first COVID-19 case among pregnant women at 21-week in Vietnam
- Posterior urethral valves (PUVs): prenatal ultrasound diagnosis and management difficulties: a review of three cases
- Premature fetal closure of the ductus arteriosus of unknown cause – could it be influenced by maternal consumption of large quantities of herbal chamomile tea – a case report?
- Spontaneous resolution of fetal ascites secondary to gastrointestinal abnormality
- A case of severe SARS-CoV-2 infection with negative nasopharyngeal PCR in pregnancy
- Respiratory decompensation due to COVID-19 requiring postpartum extracorporeal membrane oxygenation
- Obstetrical history of a family with combined oxidative phosphorylation deficiency 3 and methylenetetrahydrofolate reductase polymorphisms
- A case of newly diagnosed autoimmune diabetes in pregnancy presenting after acute onset of diabetic ketoacidosis
- Mother and child with osteogenesis imperfecta type III. Pregnancy management, delivery, and outcome
- Early detection of Emanuel syndrome: a case report
- Case Reports – Newborn
- Neonatal cervical lymphatic malformation involving the fetal airway the setting of emergency caesarean section
- Rothia dentocariosa bacteremia in the newborn: causative pathogen or contaminant?
- Severe hypocalcemia and seizures after normalization of pCO2 in a patient with severe bronchopulmonary dysplasia and permissive hypercapnia
- Infrequent association of two rare diseases: amniotic band syndrome and osteogenesis imperfecta
- Transient congenital Horner syndrome and multiple peripheral nerve injury: a scarcely reported combination in birth trauma
- No footprint too small: case of intrauterine herpes simplex virus infection
- Liver laceration presented as intraabdominal bleeding in a newborn with hypoxic-ischemic encephalopathy
- Extremely preterm infant with persistent peeling skin: X-linked ichthyosis imitates prematurity
- Thrombospondin domain1-related congenital chylothorax in an infant with maple syrup urine disease: a challenging case
- Parenteral nutrition extravasation into the abdominal wall mimicking an abscess
- Subcutaneous fat necrosis of the newborn and nephrolithiasis
- Fetal MRI assessment of head & neck vascular malformation in predicting outcome of EXIT-to-airway procedure
- Scimitar syndrome – a case report
- Asymptomatic severe laryngotracheoesophageal cleft (LTEC) in a preterm newborn
- Transient generalized proximal tubular dysfunction in an infant with a urinary tract infection: the effect of maternal infliximab therapy?
- Congenital Lobular Capillary Hemangioma in a 48 hours old neonate: a case report and a literature review
- Neonate born with ischemic limb to a COVID-19 positive mother: management and review of literature

