Abstract
Objectives
Lymphatic malformations are benign vascular anomalies comprised of lymphatic elements and most commonly occur in the neck. They may be diagnosed prenatally on ultrasound, and, in addition to confirming the diagnosis, fetal MRI can delineate the presence and extent of airway involvement. A variety of therapies are available for the treatment of lymphatic malformations including medical management, sclerotherapy, and surgery.
Case presentation
We report a case of a 28 year-old pregnant female diagnosed with a fetal neck mass by ultrasound at 21 weeks gestation. A fetal MRI was performed which demonstrated a multiseptated cystic neck mass most suggestive of a lymphatic malformation. The mass was noted to be intimately associated with the fetal airway. Follow up ultrasounds showed continued growth of the lesion throughout pregnancy. The baby was born by EXIT procedure and the lymphatic malformation was ultimately treated by a combination of medical treatment, sclerotherapy, and surgery.
Conclusions
Cervical lymphatic malformations have a classic imaging appearance and can enlarge throughout gestation as well as after delivery. The treatment plan typically involves a multidisciplinary approach.
Introduction
Lymphatic malformations (LM) are benign vascular malformations of the lymphatic system. They consist of dilated lymphatic channels or cystic lymphatic spaces filled with chylous material and lined by endothelial cells. They are characterized according to the International Society for the Study of Vascular Anomalies as “Slow-flow” type “simple vascular malformations” with the subcategory of “common (cystic) lymphatic malformations.” These common cystic lymphatic malformations can occur alone or can also occur as combined vascular malformations with venous, arteriovenous and capillary malformations [1]. They can be localized in the common form or diffusely distributed as in the case of generalized lymphatic anomaly (aka “lymphangiomatosis”). Some LM lesions present with overgrowth and belong to the PIK3CA overgrowth spectrum (e.g. Klippel-Trenaunay Syndrome and CLOVES syndrome Congenital Lipomatous Overgrowth, Vascular malformations, Epidermal nevi, and Skeletal abnormalities). Interestingly, recent genetic research suggests sporadic PIK3CA mutations may be found in up to 94% of LMs. The mTOR/PIK3 signaling pathway plays a key role in lymphangiogenesis and the use of the mTOR inhibitor sirolimus has become crucial in medical therapy [2].
The reported incidence of LM is about one in 6,000 live births. The majority (75%) occur in the head and neck but they also commonly occur in the torso and axilla. On imaging, lymphatic malformations can be categorized into three different types based on the size of the cysts: macrocystic (cysts ≥1 cm), microcystic (cysts <1 cm), and mixed (containing both sizes of cysts). MRI and ultrasound are two commonly used imaging modalities for characterization and can be used prenatally for diagnosis [3].
Although benign lesions, LMs may become inflamed or suddenly larger due to internal bleeding. Cervical LMs surrounding the airway may pose a significant risk in the perinatal period, and can result in feeding difficulties, respiratory compromise, and significant disfigurement [3].
Case presentation
A pregnant 28-year-old G4P2 female was referred to maternal fetal medicine at 21 weeks gestation with concern for a fetal neck mass. The mother reported a history of preeclampsia resulting in preterm delivery with a past pregnancy but was otherwise healthy. Fetal ultrasound performed at 21 weeks revealed a complex cystic mass with internal septations originating off of the right side of the fetal neck. There was no definite internal doppler flow. In addition to follow up ultrasounds, the patient also underwent fetal MRI at 32 weeks. The MRI confirmed the presence of a complex cystic neck mass, which increased in size. The mass extended in close proximity to the fetal airway; however, at the time of the MRI, the airway was visualized and patent. There were no internal calcifications in the mass, and the fetal thyroid appeared normal. A diagnosis of lymphatic malformation was made on the basis of the prenatal imaging (Figure 1). Follow up ultrasounds throughout gestation showed continued growth of the neck lesion.
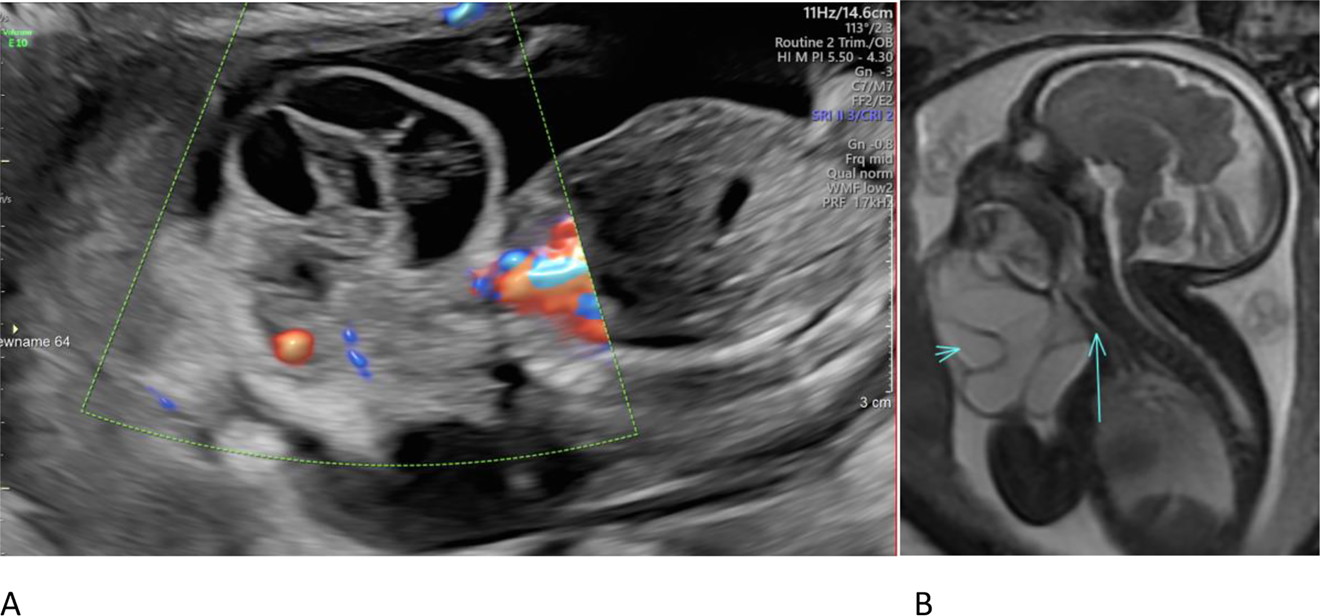
Figure Images at different weeks of pregnancy.
(A) Fetal ultrasound sagittal image at 21 weeks demonstrated a septated cystic neck mass with absent internal blood flow. (B) Fetal MRI T2 FIESTA sagittal image at 32 weeks demonstrates a cystic neck mass (short arrow) with oral cavity involvement and abutment of the trachea (long arrow).
The baby was delivered at 33 weeks gestation via emergency Cesarean section secondary to signs of severe maternal pre-eclampsia with features of HELLP syndrome (Hemolysis, Elevated Liver Enzymes, Low Platelet count). The fetus was also in breech presentation. Due to concern for airway involvement by the mass, an EXIT-to-airway delivery was performed. The baby was delivered with an intact placenta and cord. A large, predominantly right-sided fluctuant soft tissue mass with a bluish hue was noted extending from the right neck and face to the midline. The otolaryngologist visualized the airway with a scope and demonstrated slight protrusion of the mass on the right into the supraglottic region. The patient was intubated, a peripheral IV was placed, and the infant was transferred to the NICU.
The neonate was stable early in his NICU course. Consultation with the vascular anomalies team, including members from hematology/oncology, interventional radiology, otolaryngology, and plastic surgery was obtained to develop a plan for the timing of treatment.
At 18 days of age, sirolimus was initiated to decrease lymphatic production. At 32 days of life, initial sclerotherapy was performed by instilling Doxycycline through percutaneous drains inserted into the dominant macrocysts under ultrasound guidance. This was performed over a multi-day regimen without exceeding a 150 mg dose per treatment [4, 5].
Microlaryngoscopy and bronchoscopy were performed by otolaryngology which demonstrated increasing involvement of the airway since the EXIT procedure. The lymphatic malformation was noted at the base of the tongue, vallecula, and obscuring the glottis. Due to the significant size and distribution of the lesion, the patient underwent modified radical neck dissection/debulking of the lesion along with tracheostomy. The baby did well postoperatively and was ultimately discharged from the hospital. The response to treatment is illustrated on the patient’s three MRIs (Figure 2).

Sagittal T2 fat saturated MRI performed shows decreasing size of the neck lymphatic malformation after one round of sclerotherapy (A), two rounds of sclerotherapy and sirolimus (B) and 1 year after sclerotherapy, neck dissection and sirolimus (C).
Discussion
Lymphatic malformations are commonly encountered in the pediatric practice, and cases with airway involvement can be a source of anxiety for both providers and families during the perinatal period. A multidisciplinary approach to management is crucial to discuss the most appropriate plan and timing of care. Treatment options commonly include a combination of sclerotherapy for macrocystic disease, mTOR inhibitors, and surgical debulking with tracheostomy. In this case, the birth of a patient with a threatened airway due to cervical lymphatic malformation occurred in an emergency circumstance, and proper multidisciplinary planning enabled a good patient outcome.
-
Research funding: None declared.
-
Author contributions: All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Competing interests: Authors state no conflict of interest.
-
Informed consent: Informed consent was obtained from all individuals included in this study.
-
Ethical approval: The local Institutional Review Board deemed the study exempt from review.
References
1. International Society of the Study of Vascular Anomalies (ISSVA). 2018 update ISSVA. Available from: https://issva.org/classification.Search in Google Scholar
2. Borst, A, Nakano, T, Blei, F, Adams, DM, Duis, J. A primer on a comprehensive genetic approach to vascular anomalies. Front Pediatr 2020;8:1–19. https://doi.org/10.3389/fped.2020.579591.Search in Google Scholar PubMed PubMed Central
3. Greene, A. Vascular anomalies: classification, diagnosis and management. Quality Medical Publishing, Inc. 100–18 pp.Search in Google Scholar
4. Cahill, AM, Nijs, E, Ballah, D, Rabinowitz, D, Thompson, L, Rintoul, N, et al.. Percutaneous sclerotherapy in neonatal and infant head and neck lymphatic malformations: a single center experience. J Pediatr Surg 2011;46:2083–95. https://doi.org/10.1016/j.jpedsurg.2011.07.004.Search in Google Scholar PubMed
5. Molitch, HI, Unger, EC, Witte, CL, van Sonnenberg, E. Percutaneous sclerotherapy of lymphangiomas. Radiology 1995;194:343–7. https://doi.org/10.1148/radiology.194.2.7529933.Search in Google Scholar PubMed
© 2021 Walter de Gruyter GmbH, Berlin/Boston
Articles in the same Issue
- Editorial
- The journal Case Reports in Perinatal Medicine starts with open access
- Case Reports – Obstetrics
- Myomectomy scar pregnancy ‒ a serious, but scarcely reported entity: literature review and an instructive case
- Postpartum ovarian vein thrombosis
- Management of a patient in the state of total occlusion of aorta due to Takayasu arteritis in preconceptional and pregnancy period
- Stress degree demonstrated in mothers with phenylketonuria or hyperphenylalaninemia infant when requested for total or partial breastfeeding replacement
- Successful pregnancy outcome in patient with cardiac transplantation
- Further insights into unusual acrania-exencephaly-anencephaly sequence caused by amniotic band – first trimester fetoscopic correlation with two- and three-dimensional ultrasound
- Elevated fetal middle cerebral artery peak systolic velocity in diabetes type 1 patient: a case report
- Postpartum fibroid degeneration associated with elevated procalcitonin levels
- Case report: The first COVID-19 case among pregnant women at 21-week in Vietnam
- Posterior urethral valves (PUVs): prenatal ultrasound diagnosis and management difficulties: a review of three cases
- Premature fetal closure of the ductus arteriosus of unknown cause – could it be influenced by maternal consumption of large quantities of herbal chamomile tea – a case report?
- Spontaneous resolution of fetal ascites secondary to gastrointestinal abnormality
- A case of severe SARS-CoV-2 infection with negative nasopharyngeal PCR in pregnancy
- Respiratory decompensation due to COVID-19 requiring postpartum extracorporeal membrane oxygenation
- Obstetrical history of a family with combined oxidative phosphorylation deficiency 3 and methylenetetrahydrofolate reductase polymorphisms
- A case of newly diagnosed autoimmune diabetes in pregnancy presenting after acute onset of diabetic ketoacidosis
- Mother and child with osteogenesis imperfecta type III. Pregnancy management, delivery, and outcome
- Early detection of Emanuel syndrome: a case report
- Case Reports – Newborn
- Neonatal cervical lymphatic malformation involving the fetal airway the setting of emergency caesarean section
- Rothia dentocariosa bacteremia in the newborn: causative pathogen or contaminant?
- Severe hypocalcemia and seizures after normalization of pCO2 in a patient with severe bronchopulmonary dysplasia and permissive hypercapnia
- Infrequent association of two rare diseases: amniotic band syndrome and osteogenesis imperfecta
- Transient congenital Horner syndrome and multiple peripheral nerve injury: a scarcely reported combination in birth trauma
- No footprint too small: case of intrauterine herpes simplex virus infection
- Liver laceration presented as intraabdominal bleeding in a newborn with hypoxic-ischemic encephalopathy
- Extremely preterm infant with persistent peeling skin: X-linked ichthyosis imitates prematurity
- Thrombospondin domain1-related congenital chylothorax in an infant with maple syrup urine disease: a challenging case
- Parenteral nutrition extravasation into the abdominal wall mimicking an abscess
- Subcutaneous fat necrosis of the newborn and nephrolithiasis
- Fetal MRI assessment of head & neck vascular malformation in predicting outcome of EXIT-to-airway procedure
- Scimitar syndrome – a case report
- Asymptomatic severe laryngotracheoesophageal cleft (LTEC) in a preterm newborn
- Transient generalized proximal tubular dysfunction in an infant with a urinary tract infection: the effect of maternal infliximab therapy?
- Congenital Lobular Capillary Hemangioma in a 48 hours old neonate: a case report and a literature review
- Neonate born with ischemic limb to a COVID-19 positive mother: management and review of literature
Articles in the same Issue
- Editorial
- The journal Case Reports in Perinatal Medicine starts with open access
- Case Reports – Obstetrics
- Myomectomy scar pregnancy ‒ a serious, but scarcely reported entity: literature review and an instructive case
- Postpartum ovarian vein thrombosis
- Management of a patient in the state of total occlusion of aorta due to Takayasu arteritis in preconceptional and pregnancy period
- Stress degree demonstrated in mothers with phenylketonuria or hyperphenylalaninemia infant when requested for total or partial breastfeeding replacement
- Successful pregnancy outcome in patient with cardiac transplantation
- Further insights into unusual acrania-exencephaly-anencephaly sequence caused by amniotic band – first trimester fetoscopic correlation with two- and three-dimensional ultrasound
- Elevated fetal middle cerebral artery peak systolic velocity in diabetes type 1 patient: a case report
- Postpartum fibroid degeneration associated with elevated procalcitonin levels
- Case report: The first COVID-19 case among pregnant women at 21-week in Vietnam
- Posterior urethral valves (PUVs): prenatal ultrasound diagnosis and management difficulties: a review of three cases
- Premature fetal closure of the ductus arteriosus of unknown cause – could it be influenced by maternal consumption of large quantities of herbal chamomile tea – a case report?
- Spontaneous resolution of fetal ascites secondary to gastrointestinal abnormality
- A case of severe SARS-CoV-2 infection with negative nasopharyngeal PCR in pregnancy
- Respiratory decompensation due to COVID-19 requiring postpartum extracorporeal membrane oxygenation
- Obstetrical history of a family with combined oxidative phosphorylation deficiency 3 and methylenetetrahydrofolate reductase polymorphisms
- A case of newly diagnosed autoimmune diabetes in pregnancy presenting after acute onset of diabetic ketoacidosis
- Mother and child with osteogenesis imperfecta type III. Pregnancy management, delivery, and outcome
- Early detection of Emanuel syndrome: a case report
- Case Reports – Newborn
- Neonatal cervical lymphatic malformation involving the fetal airway the setting of emergency caesarean section
- Rothia dentocariosa bacteremia in the newborn: causative pathogen or contaminant?
- Severe hypocalcemia and seizures after normalization of pCO2 in a patient with severe bronchopulmonary dysplasia and permissive hypercapnia
- Infrequent association of two rare diseases: amniotic band syndrome and osteogenesis imperfecta
- Transient congenital Horner syndrome and multiple peripheral nerve injury: a scarcely reported combination in birth trauma
- No footprint too small: case of intrauterine herpes simplex virus infection
- Liver laceration presented as intraabdominal bleeding in a newborn with hypoxic-ischemic encephalopathy
- Extremely preterm infant with persistent peeling skin: X-linked ichthyosis imitates prematurity
- Thrombospondin domain1-related congenital chylothorax in an infant with maple syrup urine disease: a challenging case
- Parenteral nutrition extravasation into the abdominal wall mimicking an abscess
- Subcutaneous fat necrosis of the newborn and nephrolithiasis
- Fetal MRI assessment of head & neck vascular malformation in predicting outcome of EXIT-to-airway procedure
- Scimitar syndrome – a case report
- Asymptomatic severe laryngotracheoesophageal cleft (LTEC) in a preterm newborn
- Transient generalized proximal tubular dysfunction in an infant with a urinary tract infection: the effect of maternal infliximab therapy?
- Congenital Lobular Capillary Hemangioma in a 48 hours old neonate: a case report and a literature review
- Neonate born with ischemic limb to a COVID-19 positive mother: management and review of literature

