Abstract
Background and aims
Several methods for pain management following total hip arthroplasty (THA) have been described but the best postoperative pain management technique remains uncertain. We compared surgeon applied local infiltration analgesia (LIA) with anaesthesiologist performed femoral nerve block (FNB) using ultrasound. The primary aim was to assess pain intensity 24 h after THA.
Methods
In this randomized, double-blind study, 56 patients (ASA I-III) undergoing THA consented to participate. In Group FNB, patients received an ultrasound-guided femoral nerve block using 30 ml of ropivacaine 7.5 mg/ml (225 mg) while Group LIA received a similar volume of saline. Spinal anaesthesia was then performed and bupivacaine heavy, 3–3.5 ml injected depending on patient characteristics. During surgery, patients in Group LIA received a mixture of 300 mg (150 ml) ropivacaine, ketorolac 30 mg (1 ml) and adrenaline 0.5 mg (0.5 ml) (total volume 151.5 ml) peri-articularly and subcutaneously while Group FNB received 151.5 ml of saline peri-articularly in a systematic way by the surgeon. A multi-hole catheter was placed with the tip placed intra-articularly at the end of surgery in both groups. After 23 h, the LIA mixture consisting of 20 ml ropivacaine (7.5 mg/ml), ketorolac 30 mg (1 ml), adrenaline 0.1 mg (1 ml) (total volume 22 ml) was injected in Group LIA and the same volume of saline in Group FNB. Postoperative pain, analgesic consumption (postoperative and post-discharge), side effects, home discharge, quality of life and hip function were recorded, the latter up to 6 months after surgery.
Results
Postoperative pain intensity was significantly lower in Group LIA compared to Group FNB during mobilization at 24 h (primary endpoint), mean difference 1.8 NRS units (95% CI 0.7–2.9) (P = 0.006), at rest after 4 h (P = 0.029) and on standing after 24 (P = 0.0003) and 48 h (P = 0.043). Rescue morphine consumption was also significantly lower in Group LIA during 0–24, mean difference 13.5 mg (95% CI, 6.1–20.9) (P = 0.002) postoperatively. Motor block was greater at 6 h (P = 0.029) postoperatively in Group FNB. Two patients (one in each group) had persistent post-surgical pain (NRS > 3) at 3 months (3.6%) but none at 6 month. No other differences were found between the groups.
Conclusion
Local infiltration analgesia significantly reduces pain intensity on standing and mobilization, and rescue analgesic consumption compared to femoral nerve block without causing significant side effects. The superior analgesia in the LIA group may result from the secondary injection at 23 h postoperatively and needs to be furtherevaluated in future studies. No differences were found in home discharge, quality of life and hip dysfunction between the groups.
Implication
Local infiltration analgesia is the preferred method for postoperative pain management following THA compared to single-shot femoral nerve block.
© 2017 Scandinavian Association for the Study of Pain. Published by Elsevier B.V. All rights reserved.
1 Introduction
Total hip arthroplasty (THA) is a common procedure often performed under spinal anaesthesia in Sweden. Postoperative pain is moderate and pain relief can be achieved using spinal morphine, local infiltration analgesia (LIA) [1], patient controlled analgesia or peripheral nerve blocks (PNB). The PROSPECT group recommends a multimodal pain management strategy using oral and intravenous drugs following THA [2]. Recently, and with the easy availability of ultrasound technique, PNBs have become popular for postoperative pain management. In a comprehensive review of the literature and meta-analysis, however, no difference was found between LIA and PNB [3]. In this meta-analysis, PNBs included femoral nerve block or 3-in-1 block, lumbar plexus block, psoas compartment block, and fascia iliaca compartment block. We have previously shown better patient-related outcomes following LIA compared to intrathecal morphine in patients undergoing THA [4].
The nerve supply to the hip joint is complex but it is primarily innervated by the femoral, obturator and lateral femoral cutaneous nerves anteriorly and the sciatic nerve posteriorly. Multiple blocks encompassing the whole hip joint to achieve complete pain relief can be time-consuming and a challenge, even when using ultrasound techniques. The ideal PNB for THA is probably the lumbar plexus block but this requires long operator experience, takes time to perform and has a greater risk for complications [5]. The femoral nerve block (FNB) has recently been shown to be as effective as lumbar plexus block for THA [6]. Alternatively, the FNB may be used together with distal pressure on the nerve and a larger volume of local anaesthetic (also called 3-in-1 block), resulting in better lateral and medial spread of local anaesthetic, and improved outcomes [7]. The FNB has been shown to be efficacious for THA in several studies [8,9].
Our hypothesis was that local infiltration analgesia is superior to ultrasound-guided FNB for postoperative pain management following THA. The primary aim of this study was to determine pain intensity on mobilization at 24 h after total hip arthroplasty. Secondary aims were: cumulative morphine consumption at 24 h, incidence of persistent post-surgical pain, time to home discharge, side effects and complications, analgesic consumption at home during two weeks postoperatively, and health-related quality of life and hip disability at three and six months after home discharge using standardized questionnaires.
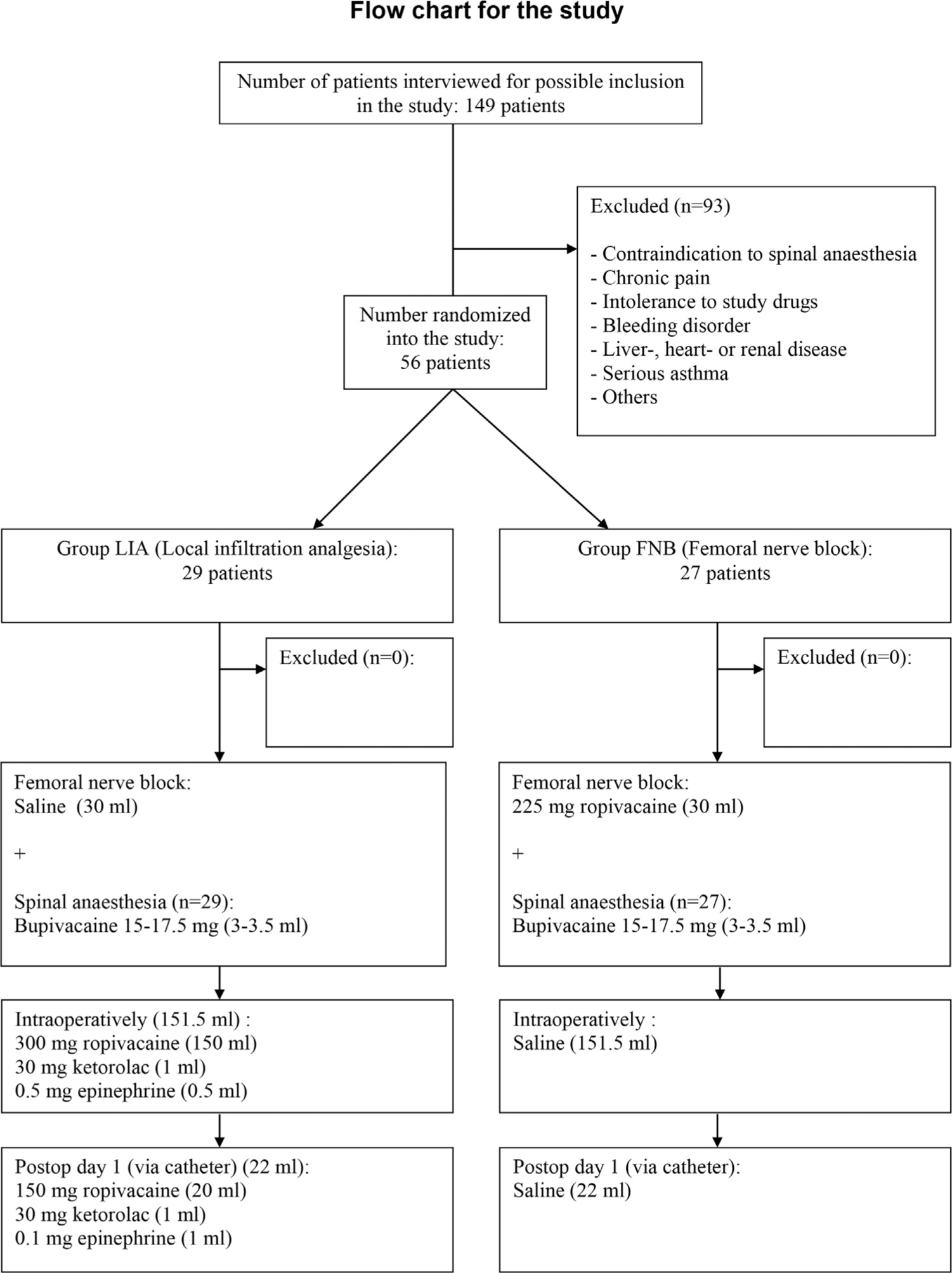
CONSORT diagram on patient recruitment, inclusion and exclusion is shown. FNB = Femoral nerve block, LIA = Local infiltration analgesia.
2 Patients and methods
The Regional Ethics committee in Uppsala and the Swedish Medical Products Agency approved the study prior to patient recruitment. It was registered in an International database (EudraCT number 2012-003875-20) and the study was conducted according to Good Clinical Practice. All patients gave verbal and written informed consent prior to enrolment. The study was prospective, randomized, double-blind, parallel group and conducted at the University Hospital, Örebro during the period 25th September 2013 to 1st December 2015 (last patient follow-up).No changes were made to study protocol after study start. Inclusion criteria were: ASA I-III patients, 18–80 years age who had no difficulty in understanding the Swedish language or following the protocol. Exclusion criteria were: patients taking opiates preoperatively for pain management, allergy to local anaesthetics or known contraindications to non-steroidal anti-inflammatory drugs (NSAIDs), re-operation THA, serious liver, heart or kidney diseases, known bleeding disorders, contraindications to spinal anaesthesia and participation in another clinical trial. All patients stopped taking NSAIDs or acetylsalicylic acid prior to surgery. Patients were given instructions about the numeric rating score (NRS) 0–10 (0 = no pain, 10 = worst imaginable pain) as well as on the use of the patient-controlled analgesia (PCA) morphine device prior to anaesthesia.
2.1 Preoperative preparation
All surgeons saw a pre-recorded film demonstrating the volume and site where the drugs/saline were to be injected during LIA. Health-related quality of life was measured using the EQ5D (European Quality of life, 5 Dimensions) and the degree of preoperative disability using the HOOS (Hip and Osteoarthritis Outcome Score) (described below). All patients received midazolam 0.03 mg/kg orally as premedication, paracetamol 1 g 1 h before planned surgery, and cloxacillin 1 g as prophylactic antibiotic just before incision.
2.2 Randomization and blinding
Randomization was performed with concealed allocation using computer generated random numbers inserted into opaque, sealed envelopes. A total of 60 envelopes (30/group) numbered 1–60 were thus created. Personnel not involved in the study performed the blinding. The randomization list was kept in a locked cupboard, not accessible to the researchers or personnel involved in the study. Full blinding was thus maintained until the study was terminated.
2.3 Anaesthesia and analgesia
An ultrasound-guided probe was used in order to identify the femoral nerve, and correct needle placement was confirmed by using a nerve stimulator and observing the “patellar dance”. Thereafter, and according to group randomization, one of the following solution was injected while applying distal pressure at the injection site.
Group LIA (Local Infiltration Analgesia): 30 ml of 0.9% saline;Group FNB (Femoral nerve block): 30 ml of ropivacaine 7.5 mg/ml.
Spinal anaesthesia with bupivacaine plain 3–3.5 ml, depending on patient characteristics, was used as the anaesthetic. During surgery, a total of 151.5 ml of the study drug was injected in a standardized and systematic way (described below) by the surgeon according to group randomization.
Group LIA: Ropivacaine 0.2% (150 ml), ketorolac 30 mg (1 ml) and adrenaline 5 mg (0.5 ml);Group FNB: An equal volume (151.5 ml) of 0.9% saline.
2.3.1 Surgical technique
Surgery was performed in a standardized way using the posterior or lateral approach, depending on the surgeon’s preference. The posterior approach uses a curved incision centred on the posterior side of the greater trochanter. The fascia lata is incised and the gluteus maximus split by blunt dissection. Subsequently, the external rotators can be divided and the posterior aspect of the capsule exposed and incised. The direct lateral approach uses a longitudinal incision also centred on the greater trochanter. The gluteal fascia and the iliotibial band are divided and the insertion of the gluteus medius is divided down to the bone. The capsule is then exposed and incised and thereafter the surgical procedure is similar.
2.3.2 LIA technique
The first injection is made around the cup of the acetabulum after it is in place, avoiding injection into the sciatic nerve. After fixing the femur component, the analgesic mixture is injected into the rotators, on the medial side of their attachment to the femur. The last injection is made subcutaneously and around the catheter. At each of these three sites,∼50 ml of the mixture is injected. At the end of surgery, a multi-hole catheter (Infiltralong 600,19G, 600 mm long, Pajunk) was inserted lateral to the incision by the surgeon under aseptic conditions and the tip placed intra-articularly and a bacterial filter connected.
2.4 Postoperative pain management
All patients received paracetamol 1 g, four times a day. Additionally, a patient controlled analgesia (PCA) device was connected as rescue medication to administer 1 mg morphine i.v. when needed with a 6 min lock-out time. After approximately 23 h, one of the following study solutions was injected via the intraarticular catheter, according to group randomization.
Group LIA: 20 ml ropivacaine (7.5 mg/ml), ketorolac 30 mg (1 ml), adrenaline 0.1 mg (1 ml);Group FNB: An equal volume (22 ml) of 0.9% saline.
After 48 h, the PCA pump was disconnected and all patients then received tramadol 50 mg, maximum four times a day as rescue medication.
2.5 Recordings and measurements
Pain
Pain intensity was recorded on an NRS scale (0–10) at rest preoperatively and postoperatively (after 4, 23, 24, 48 and 72 h), and on standing and walking (preoperatively, 24, 48 and 72 h postoperatively). Thereafter, pain intensity was measured at 3 and 6 months as a component of the HOOS questionnaire.
Analgesic consumption
Total analgesic consumption was recorded during 0–4 h, 4–24 h and 24–48 h. Following discharge, patients recorded analgesic consumption at home during 2 weeks (3–7 days and 8–14 days) postoperatively.
Side effects
Postoperative nausea and vomiting (PONV), pruritus, respiratory depression (respiratory rate < 8/min), sedation and urinary retention were recorded.
Motor block
The Bromage scale (0–3) was used to record motor function in the lower extremity during 4–8 h, 23 h, 24 h and 48 h.
Patient satisfaction
This was assessed using the following scale: 1 = poor, 2 = satisfactory, 3 = good, and 4 = excellent.
Postoperative complications
These were registered each day while in hospital and thereafter via a telephone call after 3 and 6 months.
Home discharge
Criteria for home discharge were: Mild pain (<3 on NRS), ability to walk with the help of crutches, eating and drinking without nausea or vomiting, and no surgical complications.
2.6 Patient-assessed outcomes
2.6.1 European Quality of life, 5 Dimensions (EQ5D)
Patients were asked to complete the Swedish validated questionnaire EQ5D pre-operatively and after 3 months and 6 months to assess health-related quality of life. A weighted average is constructed that varies from 1.0 (completely healthy) to 0 (dead) [10].
2.6.2 Hip dysfunction and Osteoarthritis Outcome Score (HOOS)
Hip function was assessed preoperatively and after 3 and 6 months postoperatively using a standardized and validated questionnaire (HOOS). HOOS evaluates symptoms and functional limitation related to the hip and assesses five separate patientrelevant dimensions: Pain (P), symptoms (S) including stiffness and range of motion, activity limitations-daily living (A), sport and recreation function (SP), and hip related quality of life (Q). All items are scored from zero to four, and each of the five subscales is calculated as the sum of the items included. To enhance the interpretation, HOOS is transformed into a 0–100, best to worst scale [11].
The primary outcome measure was pain intensity on mobilization at 24 h after total hip arthroplasty. Secondary outcome measures were: total morphine consumption 0–24 h, time to home discharge (days), side effects, and health-related quality of life and hip disability at three and six months using EQ-5-D and HOOS respectively. For efficacy of trial, both pain intensity and morphine consumption were to be significantly lower at 24 h.
2.7 Statistical analysis
Power calculation was performed using a superiority study design. Our hypothesis was that patients receiving LIA experience lower pain on standing and mobilization at 24 h after surgery compared to those receiving a FNB block. A previous study has shown that mean NRS pain on movement at 24 h is 5 (SD 3) (4). Using β = 80% and α = 0.05, we calculated that we needed 25 patients/group for a reduction in pain intensity by 50%. We planned to recruit a total of 60 patients to compensate for dropouts. Continuous variables normally distributed were summarized with mean and standard deviation (SD) and categorical variables with percentages. In view of the study setting with repeated measurements on patients, we applied linear mixed model with unstructured correlation structure to evaluate the outcome variable analgesic consumption and with study group, time and statistical interaction (group × time) as independent variables. The same model was used to evaluate outcomes: pain intensity, EQ5D and HOOS scores, but adjustment was made for the pre-operative measurements of the outcomes. Due to some possible violation of normality assumptions the Mann–Whitney test was also used for sensitivity analysis for the significant findings but, as no different conclusions were made, these results are not reported. Mann–Whitney test, Chi-2 test or Fischer exact test when appropriate were used to compare study groups for categorical data such as side effects and complications. All reported p-values are corrected for multiple testing of outcomes overtime between the study groups with Bonferroni-Holm method [12]. P-values <0.05 were considered to be statistically significant. All statistical analyses were done using SPSS version 22 or STATA release 14.
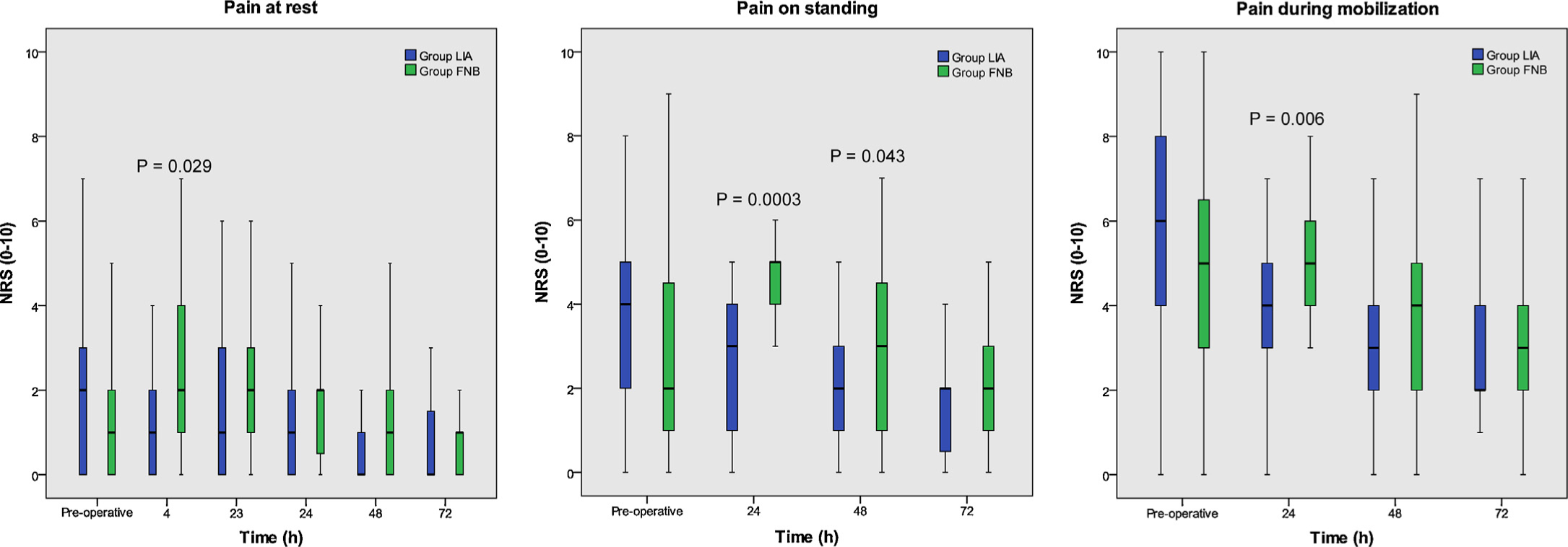
(a–c) Pain at rest (a), on standing (b) and on mobilization (c) are shown as box and whisker plot during 0–72h (median, IQR). NRS = Numeric rating scale, Group FNB = Femoral nerve block, Group LIA = Local infiltration analgesia. Corrected p-values for multiple testing with Bonferroni-Holm method are presented and refer to differences between the groups.
3 Results
Our intention was to recruit 60 patients although power calculations suggested that 50 patients would adequately answer the primary outcome measure. A total of 56 patients were interviewed and agreed to participate in the study. The study was terminated on 1st June 2015 when we found that there was no missing data for the primary endpoint. CONSORT diagram for patient recruitment is shown in Fig. 1. No patient was excluded after randomization and all patients completed the study, including the six months follow-up when the trial ended. Demographic data and operation characteristics were similar in the two groups (Table 1). Pain intensity during rest, standing and walking are shown in Fig. 2a–c. For the primary outcome, patients in group LIA had significant lower pain during mobilization at 24 h compared to Group FNB, mean difference 1.8 NRS units (95% CI 0.7–2.9) (P = 0.006) (Fig. 2c). Patients in group LIA had lower pain scores at rest at 4 h (P = 0.029) (Fig. 2a) and during standing after 24 h (P = 0.0003) and 48 h (P = 0.043) compared to Group FNB (Fig. 2b). No significant differences were found between the groups in pain intensity at rest, standing or walking at 72 h. Rescue analgesic consumption is shown in Table 2. Patients in the LIA group had significant lower mean (SD) morphine consumption between 0 and 24 h, 16.4 (10.7) mg compared to group FNB, 30 (16.6) mg, mean difference 13.5 mg (95% CI 6.1–20.9) (P = 0.002). No significant differences in paracetamol or tramadol consumption were found postoperatively between the groups.
Demographic data and duration of surgery.
| Group LIA (n = 29) | Group FNB (n = 27) | |
|---|---|---|
| No of females, n (%) | 15(52) | 15(56) |
| Age, years | 64 ± 7 | 63 ± 8 |
| Weight, kg | 84 ± 18 | 82 ± 19 |
| Height, cm | 174 ± 7 | 173 ± 7 |
| ASA, I/II/III (n) | 13/15/1 | 12/15/0 |
| Operation time, minutes | 97 ± 20 | 92 ± 17 |
-
Values are shown as mean ± SD, unless otherwise stated; Group LIA = local infiltration analgesia; Group FNB = femoral nerve block; ASA physical status: I = A normal healthy patient, II = A patient with mild systemic disease, III = A patient with severe systemic disease, n = number of patients.
Postoperative analgesic consumption.
| Group LIA mean (SD) | N | Group FNB mean (SD) | N | Mean difference FNB – LIA (95%CI) | Corrected P-value | |
|---|---|---|---|---|---|---|
| Morphine iv (mg) | ||||||
| 0–4 h after surgery | 0.9 (2.5) | 29 | 1.9 (3.1) | 27 | 0.9 (−0.6 to 2.4) | NS |
| 4–24 h | 15.5 (9.6) | 29 | 28.1 (16.1) | 27 | 12.5 (5.5–19.6) | 0.002 |
| 0–24 h | 16.4 (10.7) | 29 | 30.0 (16.6) | 27 | 13.5 (6.1–20.9) | 0.002 |
| 24–48 h | 8.1 (14.0) | 29 | 14.1 (13.5) | 27 | 6.0 (−1.4 to 13.4) | NS |
| Paracetamol orally (g) | ||||||
| 3–7 days after surgery | 14.6 (5.5) | 29 | 16.2 (4.5) | 26 | 1.6 (−1.1 to 4.4) | NS |
| 8–14 days | 14.9 (8.7) | 29 | 18.0 (9.8) | 26 | 3.1 (−1.9 to 8.1) | NS |
| Tramadol orally (mg) | ||||||
| 3–7 days after surgery | 222 (321) | 29 | 336 (373) | 26 | 114 (−74 to 302) | NS |
| 8–14 days | 209 (397) | 29 | 312 (402) | 26 | 102 (−113 to 319) | NS |
-
Analgesic consumption of morphine, paracetamol and tramadol is shown. N = number of patients; Group LIA = local infiltration analgesia; Group FNB = femoral nerve block. Statistically evaluated using mixed model. Corrected p-values for multiple testing with Bonferroni-Holm method are presented.
No significant differences were seen between the groups in the frequency of side effects (Table 3). Patient satisfaction was similar between Groups LIA and FNB median (range), 3 (2–4) and 3 (1–4) respectively. Median time to first mobilization was identical in both groups and time to home readiness was similar between the groups, median (range) Group LIA, 3 (2–4) days and Group FNB, 3 (2–6) days. Significantly greater motor block was seen in Group FNB compared to Group LIA at 6 h postoperatively (Table 3) and at 24 and 48 h postoperatively.
Side effects and motor block.
| Group LIA | N | Group FNB | N | Corrected P-value | |
|---|---|---|---|---|---|
| Nausea, n (%) | |||||
| 0–4 h postoperative | 6 (21) | 29 | 8 (30) | 27 | NS |
| 4–24 h | 12 (41) | 29 | 15 (56) | 27 | NS |
| 24–48 h | 4 (14) | 29 | 10 (37) | 27 | NS |
| Vomiting, n (%) | |||||
| 0–4 h postoperative | 0 (0) | 29 | 1 (4) | 27 | NS |
| 4–24 h | 3 (10) | 29 | 4 (15) | 27 | NS |
| 24–48 h | 1 (3) | 29 | 0 (0) | 27 | NS |
| Pruritus, n (%) | |||||
| 0–4 h postoperative | 0 (0) | 29 | 1 (4) | 27 | NS |
| 4–24 h | 2 (7) | 29 | 3 (11) | 27 | NS |
| 24–48 h | 1 (3) | 29 | 5 (19) | 27 | NS |
| Bromage scale (0/1/2/3), n | |||||
| Preoperative | 29/0/0/0 | 29 | 26/0/1/0 | 27 | |
| 6 h postoperative | 19/8/2/0 | 29 | 10/9/7/1 | 27 | 0.029 |
| 23 h | 24/5/0/0 | 29 | 16/11/0/0 | 27 | NS |
| 24 h[a] | 28/1/0/0 | 29 | 16/11/0/0 | 27 | <0.001 |
| 48 h[b] | 29/0/0/0 | 29 | 17/10/0/0 | 27 | 0.001 |
-
N = number of patients; Group LIA= local infiltration analgesia; Group FNB = femoral nerve block; Bromage scale (0–3): 0 = The patient is able to move hip knee and ankle, 1 = patient is unable to move the hip but is able to move knee and ankle, 2 = patient is unable to move the hip and knee but is able to move the ankle, 3 = patient is unable to move the hip, knee and ankle.
No significant differences were found in EQ5D between the groups but an improvement was seen between pre-operative and postoperative scores (Table 4). The hip disability score (HOOS) showed no significant differences between the groups but a significant improvement in hip function from preoperative to 3 and 6 months postoperatively. Two patients (one in each group) had persistent post-surgical pain (NRS > 3) at 3 months but none at 6 months. Additionally, one patient in Group FNB had deep vein thrombosis that required treatment with warfarin.
Hip dysfunction and Osteoarthritis Outcome Score (HOOS) and European Quality of life (EQ5D).
| Pre-operative | 3 months | 6 months | Overall post-operative | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
||||||||
| LIA (N: 29) | FNB (N: 27) | LIA (N: 29) | FNB (N: 27) | Corrected P-value | LIA (N: 29) | FNB (N: 27) | Corrected P-value | Group | Time | Group × Time | |
|
|
|||||||||||
| P-value | P-value | P-value | |||||||||
| HOOS Pain | 61.49 ± 13.21 | 60.49 ± 15.70 | 13.59 ± 14.41 (N: 28) | 12.55 ± 13.48 | NS | 8.62 ± 10.00 | 10.49 ± 13.00 | NS | 0.833 | 0.021 | 0.355 |
| HOOS Symptoms | 63.10 ± 16.50 | 63.15 ± 15.26 | 22.07 ± 17.04 | 19.07 ± 15.07 | NS | 15.86 ± 12.33 | 16.48 ± 13.14 | NS | 0.737 | 0.012 | 0.288 |
| HOOS ADL | 54.31 ± 15.23 | 56.10 ± 15.91 | 19.57 ± 13.91 | 17.97 ± 12.76 | NS | 11.46 ± 10.23 | 13.78 ± 14.05 | NS | 0.982 | <0.001 | 0.154 |
| HOOS SR | 81.25 ± 17.28 | 80.09 ± 19.69 | 31.68 ± 27.60 | 40.97 ± 26.76 | NS | 23.49 ± 22.64 | 37.03 ± 27.02 | NS | 0.77 | 0.035 | 0.452 |
| HOOS QOL | 74.57 ± 11.20 | 75.00 ± 15.50 | 34.27 ± 20.64 | 34.03 ±17.71 | NS | 28.44 ±19.81 | 24.77 ± 19.26 | NS | 0.678 | 0.001 | 0.424 |
| Pre-operative | 3 months | 6 months | Overall postoperative | ||||||||
|
|
|
|
|
||||||||
| LIA (N: 29) | FNB (N: 27) | LIA (N: 29) | FNB (N: 26) | P-value | LIA (N: 29) | FNB (N: 27) | P-value | Group | Time | Group × Time | |
| P-value | P-value | P-value | |||||||||
|
|
|||||||||||
| EQ5D | 0.45 ± 0.26 | 0.54 ± 0.27 | 0.85 ± 0.17 | 0.85 ± 0.21 | NS | 0.82 ± 0.23 | 0.88 ± 0.20 | NS | 0.785 | 0.879 | 0.352 |
-
Results of Hip dysfunction and Osteoarthritis Outcome Score (HOOS) questionnaire and European Quality of life in five dimensions (EQ5D) are shown as mean ± SD, p re-operatively and 3 and 6 months post-operatively. Statistically evaluated with mixed model adjusted for preoperative measurements (see statistics section for details). N= number of patients, Group FNB = femoral nerve block, Group LIA= local infiltration analgesia, HOOS-Pain = Pain, HOOS-Symptoms = Symptoms including stiffness and range of motion, HOOS-ADL=Activity limitations-daily living, HOOS-SR = Sport and Recreation Function, HOOS-QOL=Hip Related Quality of Life. HOOS is transformed into a 0–100 scale, where 0 = best and 100 = worst outcome score. EQ5D: 1.0 = completely healthy and 0 = dead. The higher the score, the better the quality of life. Corrected p-values for multiple testing with Bonferroni-Holm method are presented.
4 Discussion
We found that patients having LIA for postoperative pain management during THA have lower pain intensity on mobilization at 24 h compared to femoral nerve block, which was our primary outcome measure. The analgesic effect in the LIA group lasted up to 48 h postoperatively. Additionally, patients in the LIA group needed less rescue analgesics compared to those receiving a FNB block, and fewer had motor block in the LIA group at 6 h. It remains uncertain if the analgesic effect was from the primary LIA technique during surgery or the secondary injection administered after 23 h postoperatively.No other significant differences were found between the groups.
There are several components in the successful management of patients undergoing THA including good pain management, early recovery and mobilization, absence of complications, early discharge, full rehabilitation and complete patient satisfaction. Effective pain management is central to many of these outcomes, and several methods have been used for management of postoperative pain following THA [13] but no “gold standard” exists. Direct comparison between methods as well as several meta-analysis have not been able to point to the single best method for pain management. In a previous study, we compared LIA to spinal morphine and showed that the former was superior and associated with lower incidence of side effects [4]. Therefore, we were now interested in investigating if femoral nerve block is superior to LIA for postoperative pain management. We chose FNB since it is easy to apply, has a low incidence of complications and a high success rate. We used the ultrasound technique to visually identify the nerve, and a nerve stimulator to confirm correct positioning (“patellar dance”) before injecting the drugs. We used a larger volume of local anaesthetic and applied compression distal to the injection site to ensure adequate spread of the LA resulting in an extended femoral nerve block (femoral and lateral cutaneous nerve and possibly obturator, 3-in-1 block). Additionally, both anaesthetists involved in performing the ultrasound-guided block were experienced in the use of the technique. Importantly, the study was double-blinded for all involved in patient management. Our results show that despite an optimal FNB, not only was pain intensity on mobilization at 24 h lower in the LIA group (primary endpoint) but even rescue morphine consumption, a surrogate measure of pain management, was also lower during 0–24 h. Additionally, we were able to prolong the effect of LIA for up to 48 h when we injected the LIA mixture after approximately 23 h via an intraarticular catheter inserted during surgery. The use of catheter during THA has been questioned by some surgeons in view of the risk of infection. Therefore, it was important for us to understand whether the intraarticular catheter does prolong analgesia after 24 h. Whether the secondary injection of the LIA mixture at 23 h resulted in improved analgesia measured at 24 h or from the primary injection remain unclear, and is a limitation of the present study. However, rescue morphine consumption was also significantly lower during 0–24 h in the LIA group, which would support our findings that injection of the LIA mixture via the catheter has the advantage of prolonging analgesia. We acknowledge that the two groups were not equally balanced in that the FNB group did not receive a supplementary dose of local anaesthetic at 23 h via a catheter placed along the femoral nerve. Although the use of continuous FNB has been examined in previous studies, the results are equivocal [6,14,15]. Better analgesic effect can be achieved with an FNB catheter in situ but catheter dislocation can be a problem, placing the catheter is a challenge and there is a risk of motor block. The latter may be a problem during mobilization since it increases the risk of falls after hip and knee arthroplasties [16]. Although short-lasting, our patients in group FNB had greater motor block measured using Bromage scale at 6 h. Additionally, patients in the FNB group could not flex the hip joint adequately at 24 and 48 h after surgery, which may be due to pain in the hip joint after THA, but residual motor block after FNB cannot be completely excluded. The lumbar plexus block is possibly more efficacious than FNB but technically more challenging [5] and may also lead to residual motor block.
One unanswered question remains: Is the effect of LIA via local analgesia or through the systemic absorption of component drugs? It is known that ketorolac has a very high degree of protein and tissue binding [17]. The plasma concentration of ketorolac following intraarticular injection is much lower (0.51–1.13 mg/L, 95% CI) [18] compared to that after intramuscular injection (1.45–3.82 mg/L, 95% CI) [19] and reaches a peak within <1 h [18]. A previous clinical study showed that 5 mg IA ketorolac provided similar analgesia to 10 mg IV [20]. These findings would support hyothesis that the effect of ketorolac is predominantly local, and not via systemic absorption and central mechanisms.
We found no significant difference in the incidence of nausea, vomiting and pruritus between the groups. We also found that the time to home discharge was similar, which was disappointing since we had hoped that better pain management and mobilization would lead to earlier home discharge. However, multiple factors play a role in hospital stay, not just good pain management. No difference was seen between the groups in analgesic consumption at home, after discharge. Pain intensity following discharge was low and consequently oral analgesics at home are adequate for pain management.
The incidence of complications at 3 and 6 months after surgery were also similar between the groups. Persistent post-surgical pain was seen in 3.6% patients at 3 months, similar to previous studies in patients undergoing THA [21,22]. There was considerable improvement in the health-related quality of life from preoperative to postoperative scores, but no significant difference between the groups. Finally, we also found a clear improvement over time on HOOS after THA in all variables but no significant differences between the groups.
4.1 Study limitations
One limitation of this study is that we did not evaluate the effect of the FNB before application of the spinal anaesthetic. Although this would have confirmed adequate block, blinding would be a problem. Since the anaesthetists who performed the FNB were experienced in ultrasound technique, they confirmed the position of the needle using the nerve stimulator and thus preserved blinding. Another, and a major limitation of this study, is that we injected the LIA mixture at 23 h after surgery in the LIA group and measured pain intensity on mobilization and rescue morphine consumption at 24 h. This may be a source of bias since better pain relief may have been achieved in Group LIA at 24 h, which was our primary endpoint. In hindsight, we should have evaluated pain on mobilization also at 24 h and subsequently injected the study drugs. This may have confirmed the adequacy of the primary injection during surgery. Nevertheless, the composite efficacy endpoint of lower pain and lesser rescue analgesic consumption at 24 h in LIA group would mean that the LIA technique is as good, if not better than FNB. The major advantage of the intraarticular catheter technique is that a secondary injection can be given after the primary (intraoperative) injection, which prolongs pain relief. This may not be possible when using perineural catheter during FNB because of the attendant problems discussed earlier.
5 Conclusion
We found that local infiltration analgesia using a combination of local anaesthetic, ketorolac and adrenaline, performed in a systematic way by orthopaedic surgeons, offers better postoperative analgesia at 24 h and 48 h, lower rescue analgesic consumption (0–24 h) and lower incidence of residual motor block (0–6 h) compared to an ultrasound-guided femoral nerve block using ropivacaine, and is a simple and good alternative for patients undergoing total hip arthroplasty. The analgesic effect recorded at 24 h may result from the secondary injection of the LIA drugs via the catheter at 23 h, and is a problem with the study design. Future studies should therefore be done to confirm our present findings. In the limited number of patients studied, no side effects or complications of this technique were observed.
Highlights
LIA results in good postoperative analgesia and lower rescue morphine requirements.
Lower risk of motor block during 0–6 h after surgery.
A secondary injection via the intraarticular catheter at 23 h prolongs analgesia further.
DOI of refers to article: http://dx.doi.org/10.1016/j.sjpain.2017.05.003.
-
Author contribution: J Kuchálik: Design, patient recruitment, data control and writing the manuscript; A Magnuson: Design and statistical analysis, and writing the manuscript; A Lundin: Design and writing the manuscript; A Gupta: Design, data assessment, writing the manuscript.
-
Ethical issues: Informed written and verbal consent was required and obtained from each patient prior to inclusion. The study was approved by the Regional Ethic Board and the study protocol was registered in an international database prior to study start.
-
Conflict of interest: None declared.
Acknowledgements
We would like to thank Anna Calais for meticulous data collection and entry, and the staff in the Postoperative and orthopaedic wards for their attention to details. Dr Henrik Öhrström helped us in patient recruitment and performed some blocks and we are grateful for his involvement in the study.
References
[1] Kerr DR, Kohan L. Local infiltration analgesia: a technique for the control of acute postoperative pain following knee and hip surgery. A case study of 325 patients. Acta Orthop 2008;79:174–83.Suche in Google Scholar
[2] http://www.postoppain.org/sections/?rootid=8641§ion=3 [accessed 4.10.16].Suche in Google Scholar
[3] Jiménez-Almonte JH, Wyles CC, Wyles SP, Norambuena-Morales GA, Báez PJ, Murad MH, Sierra RJ. Is local infiltration analgesia superior to peripheral nerve blockade for pain management after THA: a network meta-analysis. Clin Orthop Relat Res 2016;474:495–516.Suche in Google Scholar
[4] Kuchálik J, Granath B, Ljunggren A, Magnuson A, Lundin A, Gupta A. Post-operative pain relief after total hip arthroplasty: a randomized, double-blind comparison between intrathecal morphine and local infiltration analgesia. Br J Anaesth 2013;111:793–9.Suche in Google Scholar
[5] Capdevila X, Coimbra C, Choquet O. Approaches to the lumbar plexus: success, risks and outcome. Reg Anesth Pain Med 2005;30:150–62.Suche in Google Scholar
[6] Ilfeld BM, Mariano ER, Madison SJ, Loland VJ, Sandhu NS, Suresh PJ, Bishop ML, Kim TE, Donohue MC, Kulidjian AA, Ball ST. Continuous femoral versus posterior lumbar plexus nerve blocks for analgesia after hiparthroplasty: a randomized, controlled study. Anesth Analg 2011;113:897–903.Suche in Google Scholar
[7] Köroglu S, Takmaz AS, Kaymak C, Narli A, Karalezli K, Dikmen B. The preoperative analgesic effect of 3-in-1 block on postoperative pain and tramadol consumption in total hip arthroplasty. AGRI 2008;20:19–25.Suche in Google Scholar
[8] Singelyn FJ, Ferrant T, Malisse MF, Joris D. Effects of intravenous patientcontrolled analgesia with morphine, continuous epidural analgesia, and continuous femoral nerve sheath block on rehabilitation after unilateral total-hip arthroplasty. Reg Anesth Pain Med 2005;30:452–7.Suche in Google Scholar
[9] Wiesmann T, Steinfeldt T, Wagner G, Wulf H, Schmitt J, Zoremba M. Supplemental single shot femoral nerve block for total hip arthroplasty: impact on early postoperative care, pain management and lung function. Minerva Anestesiol 2014;80:48–57.Suche in Google Scholar
[10] Jansson KÅ, Granath F. Health-related quality of life (EQ-5D) before and after orthopedic surgery. Acta Orthop 2011;82:82–9.Suche in Google Scholar
[11] Klässbo M, Larsson E, Mannevik E. Hip disability and osteoarthritis out-come score. An extension of the Western Ontario and McMaster Universities Osteoarthritis Index. Scand J Rheumatol 2003;32:46–51.Suche in Google Scholar
[12] Holm S. A simple sequentially multiple test procedure. Scand J Stat 1979;6:65–70.Suche in Google Scholar
[13] Rostlund T, Kehlet H. High-dose local infiltration analgesia after hip and knee replacement – what is it, why does it work, and what are the future challenges? Acta Orthop 2007;78:159–61.Suche in Google Scholar
[14] Fournier R, Van Gessel E, Gaggero G, Boccovi S, Forster A, Gamulin Z. Postoperative analgesia with “3-in-1” femoral nerve block after prosthetic hip surgery. Can J Anaesth 1998;45:34–8.Suche in Google Scholar
[15] Biboulet P, Morau D, Aubas P, Bringuier-Branchereau S, Capdevila X. Postoperative analgesia after total-hip arthroplasty: comparison of intravenous patient-controlled analgesia with morphine and single injection of femoral nerve or psoas compartment block. A prospective, randomized, double-blind study. Reg Anaesth Pain Med 2004;29:102–9.Suche in Google Scholar
[16] Ilfeld BM, Duke KB, Donohue MC. The association between lower extremity continuous peripheral nerve blocks and patient falls after knee and hip arthroplasty. Anesth Analg 2010;111:1552–4.Suche in Google Scholar
[17] Owen SG, Francis HW, Roberts MS. Disappearance kinetics of solutes from synovial fluid after intra-articular injection. Br J Clin Pharmacol 1994;38:349–55.Suche in Google Scholar
[18] Affas F, Eksborg S, Wretenberg P, Olofsson C, Stephanson N, Stiller CO. Plasma concentration of ketorolac after local infiltration analgesia in hip arthroplasty. Acta Anaesthesiol Scand 2014;58:1140–5.Suche in Google Scholar
[19] Jallad NS, Garg DC, Martinez JJ, Mroszczak EJ, Weidler DJ. Pharmacokinetics of single-dose oral and intramuscular ketorolac tromethamine in the young and elderly. J Clin Pharmacol 1990;30:76–81.Suche in Google Scholar
[20] Convery PN, Milligan KR, Quinn P, Scott K, Clarke RC. Low-dose intra-articular ketorolac for pain relief following arthroscopy of the knee joint. Anaesthesia 1998;53:1125–9.Suche in Google Scholar
[21] Nikolajsen L, Brandsborg B, Lucht U, Jensen TS, Kehlet H. Chronic pain following total hip arthroplasty: a nationwide questionnaire study. Acta Anaesthesiol Scand 2006;50:495–500.Suche in Google Scholar
[22] Liu SS, Buvanendran A, Rathmell JP, Sawhney M, Bae JJ, Moric M, Perros S, Pope AJ, Poultsides L, Della Valle CJ, Shin NS, McCartney CJL, Ma Y, Shah M, Wood MJ, Manion SC, Sculco TP. A cross-sectional survey on prevalence and risk factors for persistent postsurgical pain 1 year after total hip and knee replacement. Reg Anaesth Pain Med 2012;37:415–22.Suche in Google Scholar
© 2017 Scandinavian Association for the Study of Pain
Artikel in diesem Heft
- Scandinavian Journal of Pain
- Editorial comment
- Glucocorticoids – Efficient analgesics against postherpetic neuralgia?
- Original experimental
- Effect of intrathecal glucocorticoids on the central glucocorticoid receptor in a rat nerve ligation model
- Editorial comment
- Important new insight in pain and pain treatment induced changes in functional connectivity between the Pain Matrix and the Salience, Central Executive, and Sensorimotor networks
- Original experimental
- Salience, central executive, and sensorimotor network functional connectivity alterations in failed back surgery syndrome
- Editorial comment
- Education and support strategies improve assessment and management of pain by nurses
- Clinical pain research
- Using education and support strategies to improve the way nurses assess regular and transient pain – A quality improvement study of three hospitals
- Editorial comment
- The interference of pain with task performance: Increasing ecological validity in research
- Original experimental
- The disruptive effects of pain on multitasking in a virtual errands task
- Editorial comment
- Analyzing transition from acute back pain to chronic pain with linear mixed models reveals a continuous chronification of acute back pain
- Observational study
- From acute to chronic back pain: Using linear mixed models to explore changes in pain intensity, disability, and depression
- Editorial comment
- NSAIDs relieve osteoarthritis (OA) pain, but cardiovascular safety in question even for diclofenac, ibuprofen, naproxen, and celecoxib: what are the alternatives?
- Clinical pain research
- Efficacy and safety of diclofenac in osteoarthritis: Results of a network meta-analysis of unpublished legacy studies
- Editorial comment
- Editorial comment on Nina Kreddig’s and Monika Hasenbring’s study on pain anxiety and fear of (re) injury in patients with chronic back pain: Sex as a moderator
- Clinical pain research
- Pain anxiety and fear of (re) injury in patients with chronic back pain: Sex as a moderator
- Editorial comment
- Intraoral QST – Mission impossible or not?
- Clinical pain research
- Multifactorial assessment of measurement errors affecting intraoral quantitative sensory testing reliability
- Editorial comment
- Objective measurement of subjective pain-experience: Real nociceptive stimuli versus pain expectation
- Clinical pain research
- Cerebral oxygenation for pain monitoring in adults is ineffective: A sequence-randomized, sham controlled study in volunteers
- Editorial comment
- Association between adolescent and parental use of analgesics
- Observational study
- The association between adolescent and parental use of non-prescription analgesics for headache and other somatic pain – A cross-sectional study
- Editorial comment
- Cancer-pain intractable to high-doses systemic opioids can be relieved by intraspinal local anaesthetic plus an opioid and an alfa2-adrenoceptor agonist
- Clinical pain research
- Spinal analgesia for severe cancer pain: A retrospective analysis of 60 patients
- Editorial comment
- Specific symptoms and signs of unstable back segments and curative surgery?
- Clinical pain research
- Symptoms and signs possibly indicating segmental, discogenic pain. A fusion study with 18 years of follow-up
- Editorial comment
- Local anaesthesia methods for analgesia after total hip replacement: Problems of anatomy, methodology and interpretation?
- Clinical pain research
- Local infiltration analgesia or femoral nerve block for postoperative pain management in patients undergoing total hip arthroplasty. A randomized, double-blind study
- Editorial
- Scientific presentations at the 2017 annual meeting of the Scandinavian Association for the Study of Pain (SASP)
- Abstracts
- Correlation between quality of pain and depression: A post-operative assessment of pain after caesarian section among women in Ghana
- Abstracts
- Dynamic and static mechanical pain sensitivity is associated in women with migraine
- Abstracts
- The number of active trigger points is associated with sensory and emotional aspects of health-related quality of life in tension type headache
- Abstracts
- Chronic neuropathic pain following oxaliplatin and docetaxel: A 5-year follow-up questionnaire study
- Abstracts
- Expression of α1 adrenergic receptor subtypes by afferent fibers that innervate rat masseter muscle
- Abstracts
- Buprenorphine alleviation of pain does not compromise the rat monoarthritic pain model
- Abstracts
- Association between pain, disability, widespread pressure pain hypersensitivity and trigger points in subjects with neck pain
- Abstracts
- Association between widespread pressure pain hypersensitivity, health history, and trigger points in subjects with neck pain
- Abstracts
- Neuromas in patients with peripheral nerve injury and amputation - An ongoing study
- Abstracts
- The link between chronic musculoskeletal pain and sperm quality in overweight orthopedic patients
- Abstracts
- Several days of muscle hyperalgesia facilitates cortical somatosensory excitability
- Abstracts
- Social stress, epigenetic changes and pain
- Abstracts
- Characterization of released exosomes from satellite glial cells under normal and inflammatory conditions
- Abstracts
- Cell-based platform for studying trigeminal satellite glial cells under normal and inflammatory conditions
- Abstracts
- Tramadol in postoperative pain – 1 mg/ml IV gave no pain reduction but more side effects in third molar surgery
- Abstracts
- Tempo-spatial discrimination to non-noxious stimuli is better than for noxious stimuli
- Abstracts
- The encoding of the thermal grill illusion in the human spinal cord
- Abstracts
- Effect of cocoa on endorphin levels and craniofacial muscle sensitivity in healthy individuals
- Abstracts
- The impact of naloxegol treatment on gastrointestinal transit and colonic volume
- Abstracts
- Preoperative downregulation of long-noncoding RNA Meg3 in serum of patients with chronic postoperative pain after total knee replacement
- Abstracts
- Painful diabetic polyneuropathy and quality of life in Danish type 2 diabetic patients
- Abstracts
- “What about me?”: A qualitative explorative study on perspectives of spouses living with complex chronic pain patients
- Abstracts
- Increased postural stiffness in patients with knee osteoarthritis who are highly sensitized
- Abstracts
- Efficacy of dry needling on latent myofascial trigger points in male subjects with neck/shoulders musculoskeletal pain. A case series
- Abstracts
- Identification of pre-operative of risk factors associated with persistent post-operative pain by self-reporting tools in lower limb amputee patients – A feasibility study
- Abstracts
- Renal function estimations and dose recommendations for Gabapentin, Ibuprofen and Morphine in acute hip fracture patients
- Abstracts
- Evaluating the ability of non-rectangular electrical pulse forms to preferentially activate nociceptive fibers by comparing perception thresholds
- Abstracts
- Detection of systemic inflammation in severely impaired chronic pain patients, and effects of a CBT-ACT-based multi-modal pain rehabilitation program
- Abstracts
- Fixed or adapted conditioning intensity for repeated conditioned pain modulation
- Abstracts
- Combined treatment (Norspan, Gabapentin and Oxynorm) was found superior in pain management after total knee arthroplasty
- Abstracts
- Effects of conditioned pain modulation on the withdrawal pattern to nociceptive stimulation in humans – Preliminary results
- Abstracts
- Application of miR-223 onto the dorsal nerve roots in rats induces hypoexcitability in the pain pathways
- Abstracts
- Acute muscle pain alters corticomotor output of the affected muscle stronger than a synergistic, ipsilateral muscle
- Abstracts
- The subjective sensation induced by various thermal pulse stimulation in healthy volunteers
- Abstracts
- Assessing Offset Analgesia through electrical stimulations in healthy volunteers
- Abstracts
- Metastatic lung cancer in patient with non-malignant neck pain: A case report
- Abstracts
- The size of pain referral patterns from a tonic painful mechanical stimulus is increased in women
- Abstracts
- Oxycodone and macrogol 3350 treatment reduces anal sphincter relaxation compared to combined oxycodone and naloxone tablets
- Abstracts
- The effect of UVB-induced skin inflammation on histaminergic and non-histaminergic evoked itch and pain
- Abstracts
- Topical allyl-isothiocyanate (mustard oil) as a TRPA1-dependent human surrogate model of pain, hyperalgesia, and neurogenic inflammation – A dose response study
- Abstracts
- Dissatisfaction and persistent post-operative pain following total knee replacement – A 5 year follow-up of all patients from a whole region
- Abstracts
- Paradoxical differences in pain ratings of the same stimulus intensity
- Abstracts
- Pain assessment and post-operative pain management in orthopedic patients
- Abstracts
- Combined electric and pressure cuff pain stimuli for assessing conditioning pain modulation (CPM)
- Abstracts
- The effect of facilitated temporal summation of pain, widespread pressure hyperalgesia and pain intensity in patients with knee osteoarthritis on the responds to Non-Steroidal Anti-Inflammatory Drugs – A preliminary analysis
- Abstracts
- How to obtain the biopsychosocial record in multidisciplinary pain clinic? An action research study
- Abstracts
- Experimental neck muscle pain increase pressure pain threshold over cervical facet joints
- Abstracts
- Are we using Placebo effects in specialized Palliative Care?
- Abstracts
- Prevalence and pattern of helmet-induced headache among Danish military personnel
- Abstracts
- Aquaporin 4 expression on trigeminal satellite glial cells under normal and inflammatory conditions
- Abstracts
- Preoperative synovitis in knee osteoarthritis is predictive for pain 1 year after total knee arthroplasty
- Abstracts
- Biomarkers alterations in trapezius muscle after an acute tissue trauma: A human microdialysis study
- Abstracts
- PainData: A clinical pain registry in Denmark
- Abstracts
- A novel method for investigating the importance of visual feedback on somatosensation and bodily-self perception
- Abstracts
- Drugs that can cause respiratory depression with concomitant use of opioids
- Abstracts
- The potential use of a serious game to help patients learn about post-operative pain management – An evaluation study
- Abstracts
- Modelling activity-dependent changes of velocity in C-fibers
- Abstracts
- Choice of rat strain in pre-clinical pain-research – Does it make a difference for translation from animal model to human condition?
- Abstracts
- Omics as a potential tool to identify biomarkers and to clarify the mechanism of chronic pain development
- Abstracts
- Evaluation of the benefits from the introduction meeting for patients with chronic non-malignant pain and their relatives in interdisciplinary pain center
- Observational study
- The changing face of acute pain services
- Observational study
- Chronic pain in multiple sclerosis: A10-year longitudinal study
- Clinical pain research
- Functional disability and depression symptoms in a paediatric persistent pain sample
- Observational study
- Pain provocation following sagittal plane repeated movements in people with chronic low back pain: Associations with pain sensitivity and psychological profiles
- Observational study
- A longitudinal exploration of pain tolerance and participation in contact sports
- Original experimental
- Taking a break in response to pain. An experimental investigation of the effects of interruptions by pain on subsequent activity resumption
- Clinical pain research
- Sex moderates the effects of positive and negative affect on clinical pain in patients with knee osteoarthritis
- Original experimental
- The effects of a brief educational intervention on medical students’ knowledge, attitudes and beliefs towards low back pain
- Observational study
- The association between pain characteristics, pain catastrophizing and health care use – Baseline results from the SWEPAIN cohort
- Topical review
- Couples coping with chronic pain: How do intercouple interactions relate to pain coping?
- Narrative review
- The wit and wisdom of Wilbert (Bill) Fordyce (1923 - 2009)
- Letter to the Editor
- Unjustified extrapolation
- Letter to the Editor
- Response to: “Letter to the Editor entitled: Unjustified extrapolation” [by authors: Supp G., Rosedale R., Werneke M.]
Artikel in diesem Heft
- Scandinavian Journal of Pain
- Editorial comment
- Glucocorticoids – Efficient analgesics against postherpetic neuralgia?
- Original experimental
- Effect of intrathecal glucocorticoids on the central glucocorticoid receptor in a rat nerve ligation model
- Editorial comment
- Important new insight in pain and pain treatment induced changes in functional connectivity between the Pain Matrix and the Salience, Central Executive, and Sensorimotor networks
- Original experimental
- Salience, central executive, and sensorimotor network functional connectivity alterations in failed back surgery syndrome
- Editorial comment
- Education and support strategies improve assessment and management of pain by nurses
- Clinical pain research
- Using education and support strategies to improve the way nurses assess regular and transient pain – A quality improvement study of three hospitals
- Editorial comment
- The interference of pain with task performance: Increasing ecological validity in research
- Original experimental
- The disruptive effects of pain on multitasking in a virtual errands task
- Editorial comment
- Analyzing transition from acute back pain to chronic pain with linear mixed models reveals a continuous chronification of acute back pain
- Observational study
- From acute to chronic back pain: Using linear mixed models to explore changes in pain intensity, disability, and depression
- Editorial comment
- NSAIDs relieve osteoarthritis (OA) pain, but cardiovascular safety in question even for diclofenac, ibuprofen, naproxen, and celecoxib: what are the alternatives?
- Clinical pain research
- Efficacy and safety of diclofenac in osteoarthritis: Results of a network meta-analysis of unpublished legacy studies
- Editorial comment
- Editorial comment on Nina Kreddig’s and Monika Hasenbring’s study on pain anxiety and fear of (re) injury in patients with chronic back pain: Sex as a moderator
- Clinical pain research
- Pain anxiety and fear of (re) injury in patients with chronic back pain: Sex as a moderator
- Editorial comment
- Intraoral QST – Mission impossible or not?
- Clinical pain research
- Multifactorial assessment of measurement errors affecting intraoral quantitative sensory testing reliability
- Editorial comment
- Objective measurement of subjective pain-experience: Real nociceptive stimuli versus pain expectation
- Clinical pain research
- Cerebral oxygenation for pain monitoring in adults is ineffective: A sequence-randomized, sham controlled study in volunteers
- Editorial comment
- Association between adolescent and parental use of analgesics
- Observational study
- The association between adolescent and parental use of non-prescription analgesics for headache and other somatic pain – A cross-sectional study
- Editorial comment
- Cancer-pain intractable to high-doses systemic opioids can be relieved by intraspinal local anaesthetic plus an opioid and an alfa2-adrenoceptor agonist
- Clinical pain research
- Spinal analgesia for severe cancer pain: A retrospective analysis of 60 patients
- Editorial comment
- Specific symptoms and signs of unstable back segments and curative surgery?
- Clinical pain research
- Symptoms and signs possibly indicating segmental, discogenic pain. A fusion study with 18 years of follow-up
- Editorial comment
- Local anaesthesia methods for analgesia after total hip replacement: Problems of anatomy, methodology and interpretation?
- Clinical pain research
- Local infiltration analgesia or femoral nerve block for postoperative pain management in patients undergoing total hip arthroplasty. A randomized, double-blind study
- Editorial
- Scientific presentations at the 2017 annual meeting of the Scandinavian Association for the Study of Pain (SASP)
- Abstracts
- Correlation between quality of pain and depression: A post-operative assessment of pain after caesarian section among women in Ghana
- Abstracts
- Dynamic and static mechanical pain sensitivity is associated in women with migraine
- Abstracts
- The number of active trigger points is associated with sensory and emotional aspects of health-related quality of life in tension type headache
- Abstracts
- Chronic neuropathic pain following oxaliplatin and docetaxel: A 5-year follow-up questionnaire study
- Abstracts
- Expression of α1 adrenergic receptor subtypes by afferent fibers that innervate rat masseter muscle
- Abstracts
- Buprenorphine alleviation of pain does not compromise the rat monoarthritic pain model
- Abstracts
- Association between pain, disability, widespread pressure pain hypersensitivity and trigger points in subjects with neck pain
- Abstracts
- Association between widespread pressure pain hypersensitivity, health history, and trigger points in subjects with neck pain
- Abstracts
- Neuromas in patients with peripheral nerve injury and amputation - An ongoing study
- Abstracts
- The link between chronic musculoskeletal pain and sperm quality in overweight orthopedic patients
- Abstracts
- Several days of muscle hyperalgesia facilitates cortical somatosensory excitability
- Abstracts
- Social stress, epigenetic changes and pain
- Abstracts
- Characterization of released exosomes from satellite glial cells under normal and inflammatory conditions
- Abstracts
- Cell-based platform for studying trigeminal satellite glial cells under normal and inflammatory conditions
- Abstracts
- Tramadol in postoperative pain – 1 mg/ml IV gave no pain reduction but more side effects in third molar surgery
- Abstracts
- Tempo-spatial discrimination to non-noxious stimuli is better than for noxious stimuli
- Abstracts
- The encoding of the thermal grill illusion in the human spinal cord
- Abstracts
- Effect of cocoa on endorphin levels and craniofacial muscle sensitivity in healthy individuals
- Abstracts
- The impact of naloxegol treatment on gastrointestinal transit and colonic volume
- Abstracts
- Preoperative downregulation of long-noncoding RNA Meg3 in serum of patients with chronic postoperative pain after total knee replacement
- Abstracts
- Painful diabetic polyneuropathy and quality of life in Danish type 2 diabetic patients
- Abstracts
- “What about me?”: A qualitative explorative study on perspectives of spouses living with complex chronic pain patients
- Abstracts
- Increased postural stiffness in patients with knee osteoarthritis who are highly sensitized
- Abstracts
- Efficacy of dry needling on latent myofascial trigger points in male subjects with neck/shoulders musculoskeletal pain. A case series
- Abstracts
- Identification of pre-operative of risk factors associated with persistent post-operative pain by self-reporting tools in lower limb amputee patients – A feasibility study
- Abstracts
- Renal function estimations and dose recommendations for Gabapentin, Ibuprofen and Morphine in acute hip fracture patients
- Abstracts
- Evaluating the ability of non-rectangular electrical pulse forms to preferentially activate nociceptive fibers by comparing perception thresholds
- Abstracts
- Detection of systemic inflammation in severely impaired chronic pain patients, and effects of a CBT-ACT-based multi-modal pain rehabilitation program
- Abstracts
- Fixed or adapted conditioning intensity for repeated conditioned pain modulation
- Abstracts
- Combined treatment (Norspan, Gabapentin and Oxynorm) was found superior in pain management after total knee arthroplasty
- Abstracts
- Effects of conditioned pain modulation on the withdrawal pattern to nociceptive stimulation in humans – Preliminary results
- Abstracts
- Application of miR-223 onto the dorsal nerve roots in rats induces hypoexcitability in the pain pathways
- Abstracts
- Acute muscle pain alters corticomotor output of the affected muscle stronger than a synergistic, ipsilateral muscle
- Abstracts
- The subjective sensation induced by various thermal pulse stimulation in healthy volunteers
- Abstracts
- Assessing Offset Analgesia through electrical stimulations in healthy volunteers
- Abstracts
- Metastatic lung cancer in patient with non-malignant neck pain: A case report
- Abstracts
- The size of pain referral patterns from a tonic painful mechanical stimulus is increased in women
- Abstracts
- Oxycodone and macrogol 3350 treatment reduces anal sphincter relaxation compared to combined oxycodone and naloxone tablets
- Abstracts
- The effect of UVB-induced skin inflammation on histaminergic and non-histaminergic evoked itch and pain
- Abstracts
- Topical allyl-isothiocyanate (mustard oil) as a TRPA1-dependent human surrogate model of pain, hyperalgesia, and neurogenic inflammation – A dose response study
- Abstracts
- Dissatisfaction and persistent post-operative pain following total knee replacement – A 5 year follow-up of all patients from a whole region
- Abstracts
- Paradoxical differences in pain ratings of the same stimulus intensity
- Abstracts
- Pain assessment and post-operative pain management in orthopedic patients
- Abstracts
- Combined electric and pressure cuff pain stimuli for assessing conditioning pain modulation (CPM)
- Abstracts
- The effect of facilitated temporal summation of pain, widespread pressure hyperalgesia and pain intensity in patients with knee osteoarthritis on the responds to Non-Steroidal Anti-Inflammatory Drugs – A preliminary analysis
- Abstracts
- How to obtain the biopsychosocial record in multidisciplinary pain clinic? An action research study
- Abstracts
- Experimental neck muscle pain increase pressure pain threshold over cervical facet joints
- Abstracts
- Are we using Placebo effects in specialized Palliative Care?
- Abstracts
- Prevalence and pattern of helmet-induced headache among Danish military personnel
- Abstracts
- Aquaporin 4 expression on trigeminal satellite glial cells under normal and inflammatory conditions
- Abstracts
- Preoperative synovitis in knee osteoarthritis is predictive for pain 1 year after total knee arthroplasty
- Abstracts
- Biomarkers alterations in trapezius muscle after an acute tissue trauma: A human microdialysis study
- Abstracts
- PainData: A clinical pain registry in Denmark
- Abstracts
- A novel method for investigating the importance of visual feedback on somatosensation and bodily-self perception
- Abstracts
- Drugs that can cause respiratory depression with concomitant use of opioids
- Abstracts
- The potential use of a serious game to help patients learn about post-operative pain management – An evaluation study
- Abstracts
- Modelling activity-dependent changes of velocity in C-fibers
- Abstracts
- Choice of rat strain in pre-clinical pain-research – Does it make a difference for translation from animal model to human condition?
- Abstracts
- Omics as a potential tool to identify biomarkers and to clarify the mechanism of chronic pain development
- Abstracts
- Evaluation of the benefits from the introduction meeting for patients with chronic non-malignant pain and their relatives in interdisciplinary pain center
- Observational study
- The changing face of acute pain services
- Observational study
- Chronic pain in multiple sclerosis: A10-year longitudinal study
- Clinical pain research
- Functional disability and depression symptoms in a paediatric persistent pain sample
- Observational study
- Pain provocation following sagittal plane repeated movements in people with chronic low back pain: Associations with pain sensitivity and psychological profiles
- Observational study
- A longitudinal exploration of pain tolerance and participation in contact sports
- Original experimental
- Taking a break in response to pain. An experimental investigation of the effects of interruptions by pain on subsequent activity resumption
- Clinical pain research
- Sex moderates the effects of positive and negative affect on clinical pain in patients with knee osteoarthritis
- Original experimental
- The effects of a brief educational intervention on medical students’ knowledge, attitudes and beliefs towards low back pain
- Observational study
- The association between pain characteristics, pain catastrophizing and health care use – Baseline results from the SWEPAIN cohort
- Topical review
- Couples coping with chronic pain: How do intercouple interactions relate to pain coping?
- Narrative review
- The wit and wisdom of Wilbert (Bill) Fordyce (1923 - 2009)
- Letter to the Editor
- Unjustified extrapolation
- Letter to the Editor
- Response to: “Letter to the Editor entitled: Unjustified extrapolation” [by authors: Supp G., Rosedale R., Werneke M.]

