Abstract
Adequate nutrition during pregnancy supports maternal and fetal health; however, a comprehensive or sophisticated understanding of nutrition literacy among pregnant women remains limited. This systematic review aimed to evaluate the current literature on nutrition literacy in pregnant women, with a focus on socioeconomic factors and nutrition education interventions. Databases including PubMed (MEDLINE), Web of Science, SCOPUS, CINAHL, and the Cochrane Database of Systematic Reviews were searched for publications that described nutrition literacy, and related concepts, in pregnant women. The search included studies published in English between January 2000 and May 23, 2025. While 1757 studies were identified, only 5 met the inclusion criteria. These studies explored nutrition literacy levels, the influence of socioeconomic factors, and/or the effectiveness of education interventions on nutrition literacy during pregnancy. Socioeconomic factors, such as income, education, and health insurance were strongly associated with nutrition literacy levels. Nutrition education interventions improved dietary quality and nutrition literacy. However, challenges remain in measuring nutrition literacy as there are various assessment tools which limited the ability to perform cross-study comparisons. Improving socioeconomic conditions and providing nutrition education programs during pregnancy are essential for improving nutrition literacy among pregnant women. Future research should focus on creating standardized, culturally adaptable assessment tools, as well as evaluate the long-term impacts of nutrition education programs during the prenatal period.
Introduction
Nutrition literacy can be defined as possessing the skills and knowledge to make informed decisions about food choices that can impact one’s health [1]. Not only does this include the ability to pick nutrient-rich food over nutrient scarce options, nutrition literacy also includes an understanding of how food choices impact an individual’s health [2]. Furthermore, nutrition literacy incorporates the abilities to both seek out and sort through reliable nutrition resources [3]. Nutrition literacy is an inherently important concept, but also a broadly global issue, as people of all ages, socioeconomic, and cultural backgrounds are affected [1]. But this breadth may create additional challenges, where either people are bombarded with too much information and may not know how to synthesize it, or individuals lack access to understandable resources to make knowledgeable decisions [1]. Further, with increasing obesity and chronic disease rates in today’s society, emphasizing nutrition literacy is of utmost importance [2].
Many studies have shown that nutrition literacy plays an important role in establishing healthy diet patterns that impact an individual’s overall health [3]. Evidence has shown that even a basic level of nutrition literacy is positively associated with food selection, eating habits, and diet quality [3], 4]. Expanding on this, poor nutrition literacy translates to poor diet patterns that can negatively impact one’s health [4]. Several studies have linked poor nutrient intake and diet patterns to increased risk of diabetes mellitus, cardiovascular disease [5], 6], and the development and pathogenesis of autoimmune conditions such as rheumatoid arthritis and thyroid disease [7], 8]. Nutrition impacts a broad spectrum of disease conditions; therefore, improving nutrition literacy has the potential to positively impact many disease outcomes. Nutrition literacy is a foundational skill that not only impacts personal health outcomes, but also influences future generations, particularly among vulnerable populations such as pregnant women.
When it comes to nutrition, pregnant women have additional unique dietary requirements essential for their own health as well as their children’s development (which can extend well into adulthood) [9], 10]. To support the cellular and metabolic activities that occur during pregnancy, it is recommended that pregnant women eat a balanced diet with adequate intakes of micronutrients, such as calcium, iron, magnesium, folate, iodine, zinc, vitamin D, vitamin A, and omega-3 fatty acids [9]. Many pregnant women suffer nutritional deficiencies such as iron and vitamin D during pregnancy, and these deficiencies can be exacerbated even more during adolescent pregnancies when the mother must support both the fetus and their own growth [9], 11]. Folic acid is an especially important nutrient during pregnancy as it helps prevent neural tube defects; however, deficiency of this nutrient is also common in pregnancy, and supplementation in the periconceptional period (eight weeks before and eight weeks after conception) is recommended by the World Health Organization [9]. Additionally, following the recommended weight gain guidelines during pregnancy, which are based on an individual’s pre-pregnancy body mass index (BMI), is important for supporting optimal health outcomes for both mother and child [9]. Navigating these nutritional requirements can be difficult for pregnant women without a foundational understanding of nutrition literacy. Therefore, understanding nutrition literacy levels in pregnant females could help improve health outcomes for women and their unborn children during this important period of time.
The aim of this systematic review is to evaluate how socioeconomic factors and nutrition education interventions impact nutrition literacy among pregnant women. This review will synthesize the existing literature to identify gaps in knowledge and recommend targeted strategies to improve nutrition literacy. While many studies explore the broad topics of nutrition knowledge, attitudes, and practices, this review focuses specifically on research that evaluates nutrition literacy levels as a critical determinant of health outcomes during pregnancy.
Methods
Research question
This review was guided by the following research question: “How do socioeconomic factors and nutrition education interventions impact nutrition literacy among pregnant women?”
Data search strategy
PubMed (MEDLINE), Web of Science, SCOPUS, CINAHL, and Cochrane Database of Systematic Reviews were searched for publications describing nutrition literacy levels among pregnant women. The search strategy used a combination of relevant keywords and Medical Subject Heading (MeSH) terms to identify potential studies. The following search string was used (“nutrition literacy” or “nutrition knowledge”) AND (“pregnant” or “pregnancy” or “prenatal”). Peer-reviewed studies written in English that specifically evaluated nutrition literacy in pregnant women using either quantitative, qualitative, or mixed-methods designs in all countries published between January 2000 and May 2025 were included. We excluded studies that focused only on health literacy.
Results
The initial search yielded a total of 3,715 articles. After the removal of 1,958 duplicates, a total of 1,757 articles remained for screening. These records were imported into Covidence, a systematic review management platform, to facilitate initial screening and collaboration. During title and abstract screening, 1,703 articles were excluded as they did not meet the predefined inclusion criteria. Following the initial screening, the full-text of 54 articles was reviewed for eligibility by both authors and disagreements were resolved through discussion. After this was completed, 5 of the identified articles met the inclusion criteria of nutrition literacy among pregnant women. (See Figure 1). Reasons for exclusion were documented, and a Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) flowchart was used to illustrate the selection process (see Table 1).
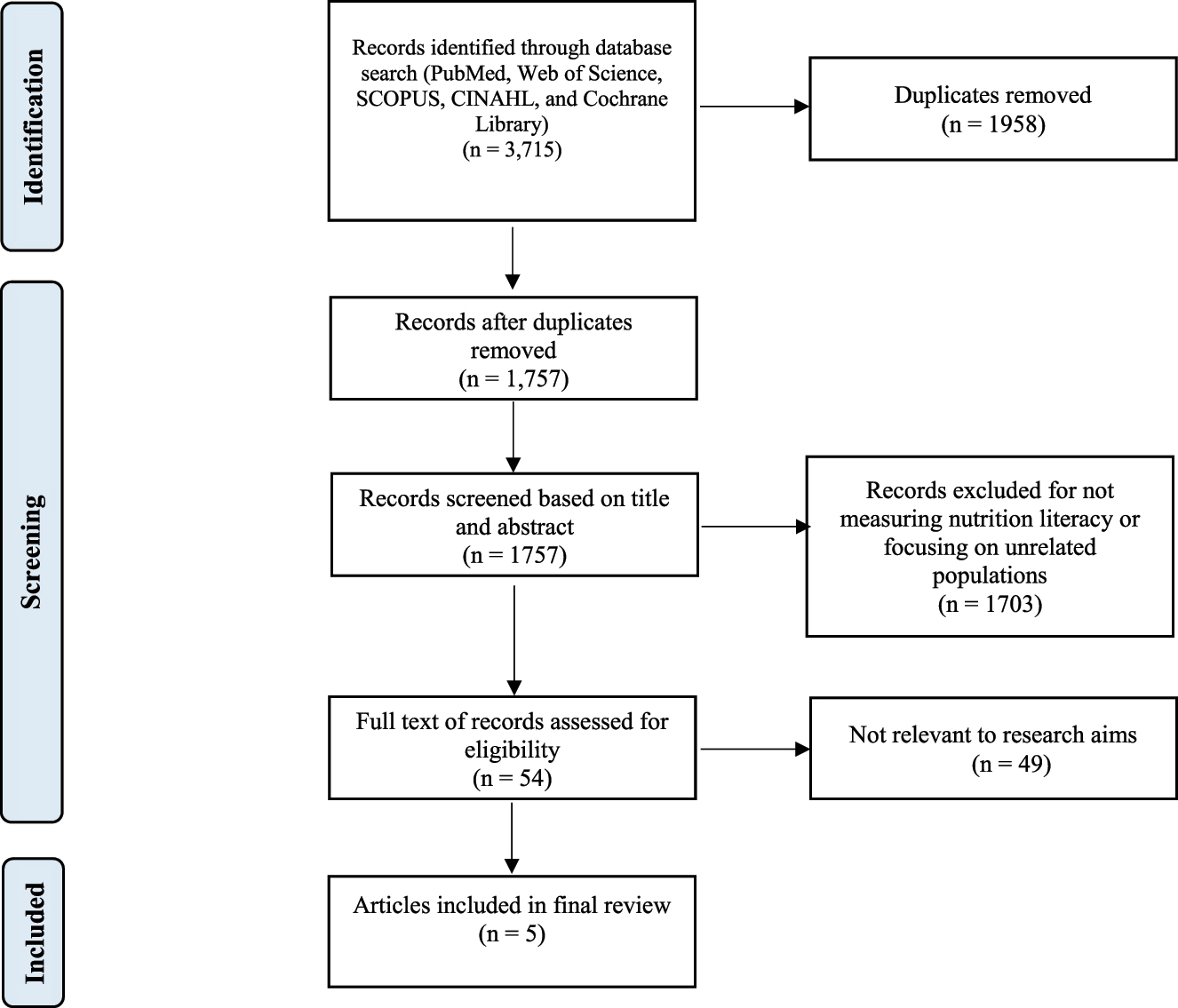
PRISMA diagram.
Summary of study findings by author.
| Reference | Study title | Study design | Aim of study | Sample size and population | Literacy instrument used | Primary study findings |
|---|---|---|---|---|---|---|
| Camargo et al., [12] | Nutrition literacy among Latina/x people during pregnancy is associated with socioeconomic position | Cross-sectional study | Assess the level of nutrition literacy among Latina/x pregnant women and its association with socioeconomic position. | n=112 Latina pregnant women between 12 and 20 weeks’ gestation, Kansas city, USA | Nutrition literacy assessment instrument (NLit) | Most participants demonstrated low nutrition literacy; significant associations were found between low nutrition literacy and socioeconomic variables. |
| Camargo et al., [12] | Higher diet quality in Latina women during pregnancy may be associated with sociodemographic factors | Cross-sectional study | Investigate diet quality among pregnant Latina women in relation to acculturation and nutrition literacy. | n=99 Latina pregnant women, between 12 and 20 weeks’ gestation | Nutrition literacy assessment instrument (NLit) | 76.8 % of participants had scores indicating low nutrition literacy. Women who were bicultural and were born in Latin American countries other than Mexico had lower diet quality scores than women who had lower acculturation and were born in Mexico. |
| Li et al., [13] | Effects of a comprehensive dietary intervention program, Promoting nutrition literacy, eating behavior, dietary quality, and gestational weight gain in Chinese urban women with normal body Mass index during pregnancy |
Cross-sectional study | Measure the impact of a dietary intervention program administered during pregnancy on pre and postintervention nutrition literacy scores | n=88 Chinese pregnant women, between 6 and 12 weeks of gestation and primiparous | Nutrition literacy assessment instrument for pregnant women in China (NLAI-P) | The intervention group (n=44; 100 % complete data) showed significant differences (mean (SD)) compared to the control group (n=42; 95.5 % complete data) in nutrition literacy (53.39 ± 6.60 vs. 43.55 ± 9.58, p<0.001). |
| Nguyen et al., [14] | Nutrition literacy in Vietnamese pregnant women: a cross-sectional study | Cross-sectional study | Determine the association between nutrition literacy and income level, education level, and pre-pregnancy BMI | n=360 Vietnamese pregnant women at any stage of pregnancy | Nutrition literacy assessment instrument for pregnant women in China (NLAI-P) | The findings revealed that 70.3 % of participants had inadequate NL. High household monthly income, age, normal pre-pregnancy weight and indoor work were statistically associated with higher NL scores. |
| Papežová et al., [10] | Nutritional health knowledge and literacy among pregnant women in the Czech republic: Analytical cross-sectional study | Analytical cross-sectional study | Evaluate nutritional knowledge and literacy among Czech pregnant women. | n=401 Czech pregnant women between 36 and 38 weeks’ gestation | Nutrition knowledge test (NKT) | Only 5 % of participants achieved an overall nutritional score of 80 % or more; there were specific demographic factors that were associated with higher nutritional knowledge scores. |
Five studies focused on nutrition literacy in pregnancy [10], [12], [13], [14], [15]. Papežová and colleagues explored nutrition literacy among 401 pregnant women in the Czech Republic using a newly created instrument called the Nutrition Knowledge Test (NKT) to conduct their cross-sectional study [10]. The authors reported that only 5 % of the participants achieved an overall nutrition literacy score of 80 % or more (which indicated a satisfactory level of nutrition knowledge). Their findings suggested that several factors impacted the scores positively, including university education, residence in the capital city, first pregnancy, having a normal or overweight status, and having a chronic noncommunicable disease. They found participants had the lowest knowledge areas in regards to optimal energy intake during pregnancy, optimal weight gain during pregnancy, and the role of micronutrients in the diet during pregnancy.
Camargo et al. assessed the level of nutrition literacy among 112 pregnant Latina/x individuals in the United States [12]. Their cross-sectional study utilized the Nutrition Literacy Assessment Instrument (NLit) and they reported that most participants demonstrated low nutrition literacy during pregnancy, with significant associations reported between low nutrition literacy and Spanish-speaking individuals with low household incomes and those who lack health insurance. Their study was nested within the phase III randomized clinical trial known as the Assessment of Docosahexaenoic Acid on reducing Early Preterm Birth (ADORE) study.
A similar study conducted by Camargo et al. (that was also part of the ADORE study) investigated nutrition literacy and how it relates to diet quality and acculturation among 99 pregnant Latina(x) individuals in the United States [15]. The authors also used the NLit tool and reported that 76.8 % of participants had low nutrition literacy and none of the participants in their study had high nutrition literacy. They found an association between improved diet quality and women who were 35 years or older. They also reported lower diet quality scores among women who were bicultural and were born in Latin American countries other than Mexico.
Nguyen et al. analyzed nutrition literacy levels in 360 Vietnamese pregnant women and the factors that can influence nutrition literacy levels [14]. Researchers in this study employed the Nutrition Literacy Assessment Instrument for Pregnant Women (NLAI-P) to evaluate metrics including knowledge regarding food sources, balanced nutrition, weight management, and nutrition label reading. Overall, the team found that 70.3 % of the women had inadequate nutrition literacy. Demographics like high age, normal pre-pregnancy weight, household monthly income were statistically associated with higher nutrition literacy scores. This study highlighted important financial considerations when it comes to addressing nutritional education in pregnant women.
The last study included in our review, Li et al., is unique in that it includes results from nutrition literacy evaluations in pregnant women both before and after an education intervention was introduced [13]. 88 Chinese women were randomized into 2 groups, the control group and the Comprehensive Dietary Intervention Program (CDIP) group. Total nutritional literacy score was calculated for each group before any intervention and calculated again for the CDIP group after intervention. The NLAI-P was used to measure participants’ nutritional literacy score. Ultimately, study results showed that the CDIP intervention compared to the control group was associated with a statistically significant increase in nutritional literacy (23.4 %) in pregnant women who were tested pre-to post-intervention (from 43.28 ± 7.25 to 53.39 ± 6.60, p<0.001).
The studies included in our review had many strengths. Each research study included a well-defined set of inclusion and exclusion criteria that helped define their populations of interest. These articles also utilized standardized tools to measure subject nutrition literacy levels. By using validated nutrition literacy instruments, researchers were able to quantify subject knowledge level and generate data needed for statistical analysis. Furthermore, each study employed appropriate statistical tests to analyze the data generated. Using the same standardized statistical methods and a p-value of 0.05, all these studies allow other researchers to draw comparisons between different study findings. An important nuance to consider is that each study included in this review looked at very different study populations across the world. While this can be beneficial when compiling research on a specific topic, it can make it more difficult to apply the findings to a specific population.
After summarizing these studies, we conducted a quality assessment using the Joanna Briggs Institute (JBI) Checklist for Analytical Cross-Sectional Studies [16]. This assessment helped evaluate the methodological rigor of the studies, focusing on aspects such as inclusion criteria, study design, and statistical analysis. The findings from this assessment indicate that all five studies clearly identified their inclusion criteria, used validated tools for measurement, and used appropriate statistical analysis. (See Table 2).
Summary of study focus and strengths.
| Study | Focus | Key strengths |
|---|---|---|
| Nutrition literacy among Latina/x people during pregnancy | Association between nutrition literacy and socioeconomic position | Well-defined criteria, part of a clinical trial called the ADORE study, reliable measurement instruments, appropriate statistical analysis |
| Higher diet quality in Latina women during pregnancy | Influence of acculturation and demographic factors on diet quality | Well-defined criteria, part of a clinical trial called the ADORE study, reliable measurement instrument, appropriate statistical analysis |
| Effects of a comprehensive dietary intervention Program, Promoting nutrition literacy, eating behavior, dietary quality, and gestational weight gain in Chinese urban women with normal body Mass index during pregnancy | Effects of a comprehensive dietary intervention program during pregnancy on pre and postintervention nutrition literacy scores | Comprehensive inclusion criteria, reliable measurement instrument, appropriate statistical analysis |
| Nutrition literacy in Vietnamese pregnant women: a cross-sectional study | Association between nutrition literacy and income level, education level, and pre-pregnancy BMI | Comprehensive inclusion criteria, reliable measurement instrument, appropriate statistical analysis |
| Nutritional health knowledge and literacy among pregnant women in the Czech Republic | Assessment of nutritional knowledge and literacy | Comprehensive inclusion criteria, standardized data collection, appropriate statistical analysis |
Due to the lack of studies that met our inclusion criteria, a meta-analysis was not feasible. Therefore, we conducted a narrative synthesis to summarize the findings thematically. We reviewed research on nutrition knowledge, attitudes, and practices (KAP) among pregnant women, along with studies involving nutrition education interventions during pregnancy. This approach helped to provide insights into the factors that impact nutrition behaviors and to identify possible interventions to support maternal and fetal health outcomes through improved nutrition literacy. We also felt it was important to focus on exploring the definitions and measures of nutrition literacy. Because there are different instruments used to evaluate nutrition literacy, clarifying how nutrition literacy is conceptualized and assessed may also highlight areas for future research in this area.
Definitions and measures of nutrition literacy
Camargo et al. refer to an already published definition of nutrition literacy as the “degree to which individuals can obtain, process, and understand basic nutrition information and services needed to make appropriate decisions.” [12], 17] They further indicate that nutrition literacy includes 2 key components of nutrition knowledge: declarative (an awareness of facts and information) and procedural (an ability to apply the knowledge to accomplish a task) [12]. This idea is also expressed by Papežová et al. who agree that nutritional knowledge is a component of nutrition literacy, representing the ability to “obtain, understand, and use information” to positively impact one’s health behaviors [10].
In the studies we evaluated, different tools to assess nutrition literacy were used. Camargo et al. and Camargo et al. utilized the NLit to evaluate nutrition literacy levels among pregnant women in both of their studies [12], 15]. The NLit was originally developed to assess nutrition literacy within a nutrition education setting in the United States [18], 19]. The original tool was reviewed by registered dietitians for content validity and pilot tested [18]. It has since been used to measure nutrition literacy in different populations and utilizes different versions in English and Spanish [20], [21], [22], [23], [24]. Camargo et al. used the short NLit version with 42 questions that measure 6 subscales of nutrition literacy. The score interpretation is divided into 3 categories: low nutrition literacy, moderate nutrition literacy, and high nutrition literacy.
Papežová et al. developed a new tool, the NKT [10]. Papežová et al. explained development of the tool was necessary as this was the first study of its kind in the Czech Republic and there was no tool available for their population. In creating their tool, they referred to previous research for guidance, involved dietitians in the process to confirm accuracy, and pilot-tested it before using it for their investigation. The final version of the NKT included 40 questions related to nutrition knowledge with 5 subscales and 5 Likert scale questions related specifically to nutrition literacy. For the NKT, a satisfactory level of nutritional knowledge was a score of >80 %.
Li et al. and Nguyen et al. used a different tool called the NLAI-P, which was developed by Yalin Zhou [13], 14], 25]. Nguyen et al. indicated they chose the NLAI-P because it comprehensively evaluates nutrition knowledge, dietary behaviors, and practical nutrition skills specific to pregnancy [14]. Nguyen et al. indicated they translated and adapted the NLAI-P to ensure cultural and linguistic appropriateness for use with Vietnamese pregnant women following the WHO translation protocol. This included forward and back translation by bilingual health professionals, expert panel review, and a pilot study with 50 pregnant women. The final instrument Nguyen et al. used demonstrated strong face and content validity (CVI=0.98) and acceptable internal consistency (Cronbach’s alpha=0.71).
The NLit and the NLAI-P were each used in 2 studies, while the NKT was used in 1 study. Differences in the instruments and lack of standardization across cultural settings limited cross-study comparability. It is important to note that while these instruments are different, they are all effective at assessing aspects of nutrition literacy because they focus on reading comprehension, numeracy, and the ability to apply nutrition information in daily life.
Nutrition knowledge, attitudes, and practices (KAP)
In our literature review we found several studies that did not assess nutrition literacy in pregnant women, but rather explored nutrition knowledge levels in pregnant women, or a combination of nutrition KAP in pregnant women. Studies show that awareness of the importance of nutrition increases during pregnancy, but that many women lack reliable sources of nutrition information [26], [27], [28], [29]. One theme that emerged was that nutrition knowledge levels among pregnant women were consistently low [26], 28], 30], 31]. Blondin and LoGiudice reported that 60 % of multiparous and 83.3 % of primiparous women in the United States failed a nutritional knowledge exam [26]. Similarly, Bookari indicated that 65 % of pregnant women in Australia were not familiar with the national nutritional guidelines during pregnancy [28]. Zelalem and colleagues found that 73 % of pregnant women in Ethiopia had poor nutrition knowledge levels [31]. There has also been research related to nutrition knowledge levels of the intake of specific nutrients, for example, folic acid [32], 33], iodine [34], and fruit and vegetable intake [35]. These studies suggest there are opportunities and arguable needs for improved nutrition education in pregnancy.
When it comes to attitudes and practices about nutrition in pregnancy, there is data indicating many pregnant women are aware of the importance of nutrition during pregnancy, but they face barriers that impact their nutritional behaviors during pregnancy [26]. Despite understanding the importance of nutrition, many women feel nutrition education is not adequately addressed during pregnancy. In a study conducted among pregnant women in the USA, many participants reported they felt nutrition was addressed in a “reactive manner” instead of the desired “proactive approach” which led participants to seek out nutrition information on their own instead of from their healthcare provider [36]. Duthie, Drew, and Flynn reported discrepancies between obstetricians’ and patients’ perceptions of discussions related to healthy eating and weight gain during prenatal visits [37]. Blondin et al. reported that many pregnant women use the internet (specifically Google) as their primary source for obtaining information about pregnancy nutrition [26]. Additionally, many women experienced difficulties during their pregnancies such as morning sickness, cravings, and limited access to healthy food options that they believe impacted their nutrition behaviors [26].
Nutrition education interventions
There is evidence that supports the use of nutrition education interventions as a method of improving nutrition knowledge, nutrition literacy, and nutrition behaviors in pregnant women. In addition to assessing nutrition literacy, Li et al. also studied nutrition education interventions in pregnant women [13]. They reported significant improvements in nutrition literacy scores following a nutrition education intervention in urban Chinese pregnant women with normal body weight [13]. Their study evaluated the effectiveness of a health education program with online and offline components that included health education on prenatal nutrition, weekly weight monitoring, and real-time dietary guidance, and their findings suggest that interactive and tailored nutrition interventions can be an effective approach to improving nutrition during pregnancy [13]. Other studies have also shown that individualized nutritional counseling during pregnancy has positive effects on nutritional status [26], [38], [39], [40]. Group nutrition education interventions during pregnancy have also reported improvements in nutrition knowledge, literacy, and health outcomes [41], 42]. Researchers in Malawi also noted improvements in the quality of dietary intake when a nutrition education intervention that promoted the use of locally available nutrient-dense foods was implemented [43]. Nutrition education interventions focused on improving culinary skills during pregnancy have also shown improvements in dietary quality and health-related outcomes [44]. Razzazi et al. developed a Health Action Process Approach (HAPA)-based nutrition education program for pregnant women that enhanced nutrition-related behavioral intentions among participants [45]. Collectively, these efforts highlight the potential benefits of nutrition education interventions during pregnancy.
Discussion
Nutrition literacy during pregnancy is significant for all women, regardless of background or location. This was especially evident when viewing the articles included in this study as a whole, as they included women in the United States Czech Republic, China, and Vietnam. Looking at research that focused on nutrition KAP and nutrition education interventions during pregnancy, this trend continued, as there were studies published on this topic from countries all over the world. This underscores the important role that nutrition literacy plays in the health and well-being of pregnant women worldwide. And while cultural differences exist, it is possible and perhaps very likely that findings from a study in 1 country would potentially be applicable to other countries.
The studies included in this review were all cross-sectional studies; however, their assessment methods varied. As mentioned previously, 2 studies utilized the previously developed and validated NLit instrument, 2 studies used the NLAI-P, and study utilized the newly-created NKT instrument. Camargo et al. nested their studies within a clinical trial, Li et al. included their assessment in an intervention, Papežová et al. and Nguyen et al. used questionnaires for direct assessment [10], [12], [13], [14], [15]. These different strategies suggest there are multiple ways to evaluate nutrition literacy among pregnant women. At this point in time, a standardized nutrition literacy tool for use among different populations does not exist. Comparability among different populations could be enhanced if such a tool were created; however, given the diverse nature of participants that span the globe it may be impossible to develop something that could be uniformly applicable to all cultures.
Socioeconomic disparities and nutrition literacy
Similar to many domains across medicine, nutrition literacy is heavily influenced by social factors that include socioeconomic status and education level, and several studies have confirmed this relationship [10], 12], 41], [46], [47], [48]. Low-income levels have consistently been associated with lower levels of diet quality and nutrition literacy [12], [46], [47], [48]. Camargo et al. found that pregnant women in their study who had lower annual incomes also had lower rates of nutrition literacy [12]. They additionally pointed out that those women who did not have medical insurance also had lower nutrition literacy levels. Further, education level has been associated with nutrition literacy in pregnancy [10], 12], 41], 47], 48]. Camargo et al. and Papežová et al. reported lower levels of nutrition literacy in pregnant women with lower levels of education [10], 12]. These lower levels of nutrition literacy may be due to the reduced ability to interpret food labels or critically evaluate nutrition sources.
Camargo et al. found an association between age and diet quality during pregnancy [15]. They reported that pregnant women age 35-years or older had higher diet quality than their younger counterparts. The authors hypothesize this may be because younger generations typically have lower fruit and vegetable intake as well as higher intakes of ultra-processed foods.
Papežová et al. also reported a correlation between pregnancy order and nutrition literacy levels [10]. They reported that primigravida women had significantly higher levels of nutritional knowledge compared to women with were already mothers. The authors suggest there might be a significant relationship between pregnancy order and level of nutrition knowledge because women during their first pregnancy may be more motivated to learn and may have more time to dedicate to educating themselves than those who have children. A nutrition education intervention study in Istanbul also reported higher nutrition knowledge levels in first time pregnant women [41], and another study reported pregnant African American women identified time constraints were a barrier to making healthy dietary choices [48], but it was difficult to find other studies to confirm this finding.
Pre-pregnancy body weight was also found to be a factor that impacted levels of nutrition literacy [10]. Both an abnormal BMI at the time of conception and irregular weight gain during pregnancy can have long-term health implications for the mother and fetus [49], 50]. Papežová et al. found that women who had a normal body weight or who were overweight before becoming pregnant had higher levels of nutrition literacy than participants who were underweight or obese. They attributed this to limited knowledge related to the optimal energy intake for appropriate weight gain during pregnancy [10]. Other researchers have also found that obese pregnant women have low levels of nutrition knowledge and health literacy [51], 52]. This reinforces the importance of nutrition education about proper energy intakes and recommended weight gain during the pregnancy.
Camargo et al. also explored the relationship between diet quality and acculturation [15]. They found that women who were born in Mexico or who were classified as having low acculturation had higher diet quality than those born in other Latin American countries and who were classified as bicultural. They define acculturation as “the process of learning and incorporating the attitudes, values, customs, beliefs, and behaviors of the mainstream culture of the new country immigrants and their families are living in,” and further explain that acculturation is complex and impacted by many individual, interpersonal, and systemic factors [15].
Taken together, the research highlights the fact that improving nutrition literacy among pregnant women involves a deeper understanding of the specific socioeconomic, educational, time constraints, and cultural issues faced by this population. With such a large potential impact on health, nutrition literacy must be prioritized in pregnant patients. Researchers should focus on the impact of nutrition-related self-care practices during pregnancy, emphasizing how pregnant women are incorporating nutrition information into their lives, and if doing so leads to better diet quality and/or health outcomes. While there is already research indicating individual educational initiatives and group programs can improve nutrition-knowledge levels during pregnancy, additional research that explores how these programs impact health outcomes in populations with low nutrition literacy levels and low socioeconomic status would be beneficial. Because pre-pregnancy BMI and gestational weight gain impact long-term maternal and fetal outcomes, it is crucial for nutrition education during pregnancy to provide women with an understanding of the appropriate energy requirements and weight gain recommendations. However, many pregnant women report the nutrition guidance they receive during their prenatal visits is insufficient, indicating there is room for improvement in communication between the patient and provider. In support of this acknowledged gap, programs like the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) serve as important resources [53], 54]. By providing nutritional support and education, WIC directly addresses these barriers and participation in the program may provide an opportunity to enhance nutrition literacy.
Limitations
The studies included in our review had several limitations that impact the strength and generalizability of the findings. Several studies had smaller sample sizes, reducing statistical power. There was variability in the instruments used to assess nutrition literacy which limits comparability. Additionally, most of the studies were limited to specific geographic regions, which may impact broader generalizability of the findings. These limitations suggest a need for more rigorous research in this area.
Because nutrition literacy is complex, discussions continue about how to best to measure it [55]. In reaction multiple tools have been developed throughout the world for evaluating nutrition literacy, and in this review, the prior use of different instruments made it more difficult to compare the researchers’ findings. The development of a standardized instrument to measure nutrition literacy in different populations across the globe could add value to the current body of knowledge on this topic.
The fact that only 5 studies met the inclusion criteria indicates there is a severe gap in research on nutrition literacy in pregnancy. While these studies certainly enhance the general understanding of this topic, they also highlight the fact that many factors impact nutrition literacy. The overall concept of nutrition literacy is not just limited to an individual’s knowledge levels, it also involves making informed decisions every day to navigate one’s food environment. In order to fully evaluate the impact of nutrition literacy on maternal and fetal outcomes, more research is needed. Future studies targeting specific populations and socioeconomic disparities may help improve our knowledge of this topic.
Conclusions
This systematic review highlights the complexities associated with nutrition literacy among pregnant women. While the literature search revealed a limited number of relevant studies on this specific topic, the examination of related KAP and intervention studies did provide valuable insights.
As nutrition literacy encompasses more than just knowledge, there are many obstacles that pregnant women face when trying to eat healthfully. Our review highlighted challenges pregnant women face related to understanding and applying reliable nutrition information. All of the identified studies (n=5) addressed nutrition literacy through questions related to nutrition knowledge and consumer skills. But the revelation that there are only a handful of quality, relevant studies in this area also clarified that data about and insights into nutrition literacy during pregnancy is limited, and more high-quality research is needed.
Our research indicates that improvements in the social determinants of health are necessary to improve nutrition literacy in pregnant women. In addition to policy changes that may help improve social determinants of health, it may also be worthwhile to focus efforts on improving access to nutrition education during pregnancy.
Acknowledgements
The authors thank the entire faculty, staff, and fellow trainees at the Weill Cornell Medicine Career Advancement for Research in Health Equity (CARE T37) program for inspiring this research. The authors thank Dr. Ahmad Hakemi for his continued interest and support of advancing the medical field through research and collaboration. The authors are grateful for the reviewer’s valuable comments that improved the manuscript.
-
Funding information: Authors state no funding involved.
-
Author contribution: All authors have accepted responsibility for the entire content of this manuscript and consented to its submission to the journal, reviewed all the results and approved the final version of the manuscript. ES and MM wrote the main manuscript text. ES prepared Figure 1. ES and MM prepared Tables 1 and 2.
-
Conflicts of interest: Authors state no conflict of interest.
-
Data availability statement: All data included in this systematic review were extracted from previously published studies. No new data were generated or analyzed by the authors. The full list of sources is included in the reference section.
References
1. Silva, P, Araújo, R, Lopes, F, Ray, S. Nutrition and food literacy: framing the challenges to health communication. Nutrients 2023;15:4708. https://doi.org/10.3390/nu15224708.Suche in Google Scholar PubMed PubMed Central
2. Haldeman, L. Separating fact from fiction: enhancing nutrition literacy to navigate healthy eating decisions. J Nutr Educ Behav 2023;55:698. https://doi.org/10.1016/j.jneb.2023.08.008.Suche in Google Scholar PubMed
3. Mohsen, H, Sacre, Y, Hanna-Wakim, L, Hoteit, M. Nutrition and food literacy in the MENA region: a review to inform nutrition research and policy makers. Int J Environ Res Publ Health 2022;19:10190. https://doi.org/10.3390/ijerph191610190.Suche in Google Scholar PubMed PubMed Central
4. Palumbo, R. Sustainability of well-being through literacy. The effects of food literacy on sustainability of well-being. Agric Agric Sci Procedia 2016;8:99–106.10.1016/j.aaspro.2016.02.013Suche in Google Scholar
5. Casas, R, Castro-Barquero, S, Estruch, R, Sacanella, E. Nutrition and cardiovascular health. Int J Mol Sci 2018;19:3988. https://doi.org/10.3390/ijms19123988.Suche in Google Scholar PubMed PubMed Central
6. Yuan, S, He, J, Wu, S, Zhang, R, Qiao, Z, Bian, X, et al.. Trends in dietary patterns over the last decade and their association with long-term mortality in general US populations with undiagnosed and diagnosed diabetes. Nutr Diabetes 2023;13:5. https://doi.org/10.1038/s41387-023-00232-8.Suche in Google Scholar PubMed PubMed Central
7. Nikiphorou, E, Philippou, E. Nutrition and its role in prevention and management of rheumatoid arthritis. Autoimmun Rev 2023;22:103333. https://doi.org/10.1016/j.autrev.2023.103333.Suche in Google Scholar PubMed
8. Rayman, MP. Multiple nutritional factors and thyroid disease, with particular reference to autoimmune thyroid disease. Proc Nutr Soc 2019;78:34–44. https://doi.org/10.1017/S0029665118001192.Suche in Google Scholar PubMed
9. Jouanne, M, Oddoux, S, Noël, A, Voisin-Chiret, AS. Nutrient requirements during pregnancy and lactation. Nutrients 2021;13:692. https://doi.org/10.3390/nu13020692.Suche in Google Scholar PubMed PubMed Central
10. Papežová, K, Kapounová, Z, Zelenková, V, Riad, A. Nutritional health knowledge and literacy among pregnant women in the Czech Republic: analytical cross-sectional study. Int J Environ Res Publ Health 2023;20:3931. https://doi.org/10.3390/ijerph20053931.Suche in Google Scholar PubMed PubMed Central
11. Sherer, EL, Bello Trujillo, AM. Barriers to adequate nutrition in pregnant adolescent Colombian females. Int J Adolesc Med Health 2023;35:291–7. https://doi.org/10.1515/ijamh-2023-0060.Suche in Google Scholar PubMed
12. Camargo, JT, Ramirez, M, Gajewski, BJ, Sullivan, DK, Carlson, SE, Gibbs, HD. Nutrition literacy among latina/x people during pregnancy is associated with socioeconomic position. J Acad Nutr Diet 2022;122:2097–105. https://doi.org/10.1016/j.jand.2022.05.011.Suche in Google Scholar PubMed
13. Li, Q, Piaseu, N, Phumonsakul, S, Thadakant, S. Effects of a comprehensive dietary intervention program, promoting nutrition literacy, eating behavior, dietary quality, and gestational weight gain in Chinese urban women with normal body mass index during pregnancy. Nutrients 2024;16:217. https://doi.org/10.3390/nu16020217.Suche in Google Scholar PubMed PubMed Central
14. Nguyen, HT, Tran, HTT, Dao-Tran, TH, Huang, LC. Nutrition literacy in Vietnamese pregnant women: a cross-sectional study. Health Promot Int 2025;40:daae187. https://doi.org/10.1093/heapro/daae187.Suche in Google Scholar PubMed
15. Teruel, CJ, Taylor, MK, Gajewski, BJ, Carlson, SE, Sullivan, DK, Gibbs, HD. Higher diet quality in Latina women during pregnancy may be associated with sociodemographic factors. Int J Environ Res Publ Health 2022;19:13895. https://doi.org/10.3390/ijerph192113895.Suche in Google Scholar PubMed PubMed Central
16. Aromataris, E, Lockwood, C, Porritt, K, Pilla, B, Jordan, Z, editors. JBI manual for evidence synthesis. Adelaide, South Australia: JBI; 2024.10.46658/JBIMES-24-01Suche in Google Scholar
17. Silk, KJ, Sherry, J, Winn, B, Keesecker, N, Horodynski, MA, Sayir, A. Increasing nutrition literacy: testing the effectiveness of print, web site, and game modalities. J Nutr Educ Behav 2008;40:3–10. https://doi.org/10.1016/j.jneb.2007.08.012.Suche in Google Scholar PubMed
18. Gibbs, H, Chapman-Novakofski, K. Establishing content validity for the nutrition literacy assessment instrument. Prev Chronic Dis 2013;10:E109. https://doi.org/10.5888/pcd10.120267.Suche in Google Scholar PubMed PubMed Central
19. Gibbs, HD. Nutrition literacy: foundations and development of an instrument for assessment [Internet]: Illinois.edu; 2012 [cited 2025 Sept 11]. Available from: https://www.ideals.illinois.edu/items/31475.Suche in Google Scholar
20. Gibbs, HD, Camargo, JMTB, Owens, S, Gajewski, B, Cupertino, AP. Measuring nutrition literacy in spanish-speaking latinos: an exploratory validation study. J Immigr Minority Health 2018;20:1508–15. https://doi.org/10.1007/s10903-017-0678-1.Suche in Google Scholar PubMed PubMed Central
21. Gibbs, HD, Ellerbeck, EF, Gajewski, B, Zhang, C, Sullivan, DK. The nutrition literacy assessment instrument is a valid and reliable measure of nutrition literacy in adults with chronic disease. J Nutr Educ Behav 2018;50:247–57.e1. https://doi.org/10.1016/j.jneb.2017.10.008.Suche in Google Scholar PubMed PubMed Central
22. Gibbs, HD, Ellerbeck, EF, Befort, C, Gajewski, B, Kennett, AR, Yu, Q, et al.. Measuring nutrition literacy in breast cancer patients: development of a novel instrument. J Cancer Educ 2016;31:493–9. https://doi.org/10.1007/s13187-015-0851-y.Suche in Google Scholar PubMed PubMed Central
23. Gibbs, HD, Kennett, AR, Kerling, EH, Yu, Q, Gajewski, B, Ptomey, LT, et al.. Assessing the nutrition literacy of parents and its relationship with child diet quality. J Nutr Educ Behav 2016;48:505–9.e1. https://doi.org/10.1016/j.jneb.2016.04.006.Suche in Google Scholar PubMed PubMed Central
24. Chaves, CDS, Camargo, JT, Zandonadi, RP, Nakano, EY, Ginani, VC. Nutrition literacy level in bank employees: the case of a large Brazilian company. Nutrients 2023;15:2360. https://doi.org/10.3390/nu15102360.Suche in Google Scholar PubMed PubMed Central
25. Zhou, Y, Lyu, Y, Zhao, R, Shi, H, Ye, W, Wen, Z, et al.. Development and validation of nutrition literacy assessment instrument for Chinese pregnant women. Nutrients 2022;14:2863. https://doi.org/10.3390/nu14142863.Suche in Google Scholar PubMed PubMed Central
26. Blondin, JH, LoGiudice, JA. Pregnant women’s knowledge and awareness of nutrition. Appl Nurs Res 2018;39:167–74. https://doi.org/10.1016/j.apnr.2017.11.020.Suche in Google Scholar PubMed
27. Bianchi, CM, Huneau, JF, Le Goff, G, Verger, EO, Mariotti, F, Gurviez, P. Concerns, attitudes, beliefs and information seeking practices with respect to nutrition-related issues: a qualitative study in French pregnant women. BMC Pregnancy Childbirth 2016;16:306. https://doi.org/10.1186/s12884-016-1078-6.Suche in Google Scholar PubMed PubMed Central
28. Bookari, K, Yeatman, H, Williamson, M. Exploring Australian women’s level of nutrition knowledge during pregnancy: a cross-sectional study. Int J Womens Health 2016;8:405–19. https://doi.org/10.2147/IJWH.S110072.Suche in Google Scholar PubMed PubMed Central
29. Downs, DS, Savage, JS, Rauff, EL. Falling short of guidelines? Nutrition and weight gain knowledge in pregnancy. J Women’s Health Care 2014;3:1000184. https://doi.org/10.4172/2167-0420.1000184.Suche in Google Scholar PubMed PubMed Central
30. Lee, A, Belski, R, Radcliffe, J, Newton, M. What do pregnant women know about the healthy eating guidelines for pregnancy? A web-based questionnaire. Matern Child Health J 2016;20:2179–88. https://doi.org/10.1007/s10995-016-2071-4.Suche in Google Scholar PubMed
31. Zelalem, T, Mikyas, A, Erdaw, T. Nutritional knowledge, attitude and practices among pregnant women who attend antenatal care at public hospitals of addis Ababa, Ethiopia. Int J Nurs Midwifery 2018;10:81–9.10.5897/IJNM2017.0289Suche in Google Scholar
32. Tavares, BB, Sabino, AMNF, Lima, JC, Garcia, CT. Knowledge of folic acid supplementation during pregnancy. Invest Educ Enfermería 2015;33:456–64.10.17533/udea.iee.v33n3a09Suche in Google Scholar PubMed
33. Sadiq, Z, Hussein, H. Assessment of knowledge and attitudes among pregnant women’s towards folic acid intake during pregnancy in a sample of women attending primary health care centers in babylon province. Med J Babylon 2022;19:142.10.4103/MJBL.MJBL_72_21Suche in Google Scholar
34. Martin, JC, Savige, GS, Mitchell, EKL. Health knowledge and iodine intake in pregnancy. Aust N Z J Obstet Gynaecol 2014;54:312–6. https://doi.org/10.1111/ajo.12201.Suche in Google Scholar PubMed
35. de Jersey, SJ, Nicholson, JM, Callaway, LK, Daniels, LA. An observational study of nutrition and physical activity behaviours, knowledge, and advice in pregnancy. BMC Pregnancy Childbirth 2013;13:115. https://doi.org/10.1186/1471-2393-13-115.Suche in Google Scholar PubMed PubMed Central
36. Daigle Millan, K, Poccia, S, Fung, TT. Information seeking behaviors, attitudes, and beliefs about pregnancy-related nutrition and supplementation: a qualitative study among US women. Nutr Health 2022;28:563–9. https://doi.org/10.1177/02601060211038842.Suche in Google Scholar PubMed
37. Duthie, EA, Drew, EM, Flynn, KE. Patient-provider communication about gestational weight gain among nulliparous women: a qualitative study of the views of obstetricians and first-time pregnant women. BMC Pregnancy Childbirth 2013;13:231. https://doi.org/10.1186/1471-2393-13-231.Suche in Google Scholar PubMed PubMed Central
38. Kaleem, R, Adnan, M, Nasir, M, Rahat, T. Effects of antenatal nutrition counselling on dietary practices and nutritional status of pregnant women: a quasi-experimental hospital based study. Pakistan J Med Sci Q 2020;36:632–6. https://doi.org/10.12669/pjms.36.4.1919.Suche in Google Scholar PubMed PubMed Central
39. Garnweidner, LM, Sverre Pettersen, K, Mosdøl, A. Experiences with nutrition-related information during antenatal care of pregnant women of different ethnic backgrounds residing in the area of Oslo, Norway. Midwifery 2013;29:e130–7. https://doi.org/10.1016/j.midw.2012.12.006.Suche in Google Scholar PubMed
40. Lucas, C, Charlton, KE, Yeatman, H. Nutrition advice during pregnancy: do women receive it and can health professionals provide it? Matern Child Health J 2014;18:2465–78. https://doi.org/10.1007/s10995-014-1485-0.Suche in Google Scholar PubMed
41. Aktaç, S, Sabuncular, G, Kargin, D, Gunes, FE. Evaluation of nutrition knowledge of pregnant women before and after nutrition education according to sociodemographic characteristics. Ecol Food Nutr 2018;57:441–55. https://doi.org/10.1080/03670244.2018.1544561.Suche in Google Scholar PubMed
42. Sudaryati, E, Zuska, F, Masthalina, H. Strengthening food security reduces the anemic status of pregnant women in the coastal area of central tapanuli. Curr Res Nutr Food Sci J 2023;11:445–55.10.12944/CRNFSJ.11.1.34Suche in Google Scholar
43. Ziyenda Katenga-Kaunda, L, Iversen, PO, Holmboe-Ottesen, G, Fjeld, H, Mdala, I, Kamudoni, PR. Dietary intake and processes of behaviour change in a nutrition education intervention for pregnant women in rural Malawi: a cluster-randomised controlled trial. Public Health Nutr 2020;23:2345–54. https://doi.org/10.1017/S1368980020000294.Suche in Google Scholar PubMed PubMed Central
44. Taylor, RM, Wolfson, JA, Lavelle, F, Dean, M, Frawley, J, Hutchesson, MJ, et al.. Impact of preconception, pregnancy, and postpartum culinary nutrition education interventions: a systematic review. Nutr Rev 2021;79:1186–203. https://doi.org/10.1093/nutrit/nuaa124.Suche in Google Scholar PubMed PubMed Central
45. Razzazi, A, Griffiths, MD, Alimoradi, Z. The effect of nutritional education based on the health action process approach (HAPA) on the pregnancy outcomes among malnourished pregnant mothers. BMC Pregnancy Childbirth 2024;24:83. https://doi.org/10.1186/s12884-024-06276-7.Suche in Google Scholar PubMed PubMed Central
46. Michou, M, Panagiotakos, DB, Lionis, C, Costarelli, V. Socioeconomic inequalities in relation to health and nutrition literacy in Greece. Int J Food Sci Nutr 2019;70:1007–13. https://doi.org/10.1080/09637486.2019.1593951.Suche in Google Scholar PubMed
47. Wesołowska, E, Jankowska, A, Trafalska, E, Kałużny, P, Grzesiak, M, Dominowska, J, et al.. Sociodemographic, lifestyle, environmental and pregnancy-related determinants of dietary patterns during pregnancy. Int J Environ Res Publ Health 2019;16:754. https://doi.org/10.3390/ijerph16050754.Suche in Google Scholar PubMed PubMed Central
48. Groth, SW, Simpson, AH, Fernandez, ID. The dietary choices of women who are low-income, pregnant, and African American. J Midwifery Womens Health 2016;61:606–12. https://doi.org/10.1111/jmwh.12463.Suche in Google Scholar PubMed
49. Koletzko, B, Godfrey, KM, Poston, L, Szajewska, H, van Goudoever, JB, de Waard, M, et al.. Nutrition during pregnancy, lactation and early childhood and its implications for maternal and long-term child health: the early nutrition project recommendations. Ann Nutr Metab 2019;74:93–106. https://doi.org/10.1159/000496471.Suche in Google Scholar PubMed PubMed Central
50. Goldstein, RF, Abell, SK, Ranasinha, S, Misso, M, Boyle, JA, Black, MH, et al.. Association of gestational weight gain with maternal and infant outcomes: a systematic review and meta-analysis. JAMA 2017;317:2207–25. https://doi.org/10.1001/jama.2017.3635.Suche in Google Scholar PubMed PubMed Central
51. Mohd-Shukri, NA, Forbes, S, Denison, FC, Norman, JE, Walker, BR, Reynolds, RM. Food intake and nutrition knowledge in severely Obese pregnant women in Scotland. Proc Nutr Soc 2011;70.10.1017/S0029665111000279Suche in Google Scholar
52. Meldgaard, M, Jensen, AL, Johansen, AD, Maimburg, RD, Maindal, HT. Health literacy and related behaviour among pregnant women with obesity: a qualitative interpretive description study. BMC Pregnancy Childbirth 2022;22:712. https://doi.org/10.1186/s12884-022-05023-0.Suche in Google Scholar PubMed PubMed Central
53. Venkataramani, M, Ogunwole, SM, Caulfield, LE, Sharma, R, Zhang, A, Gross, SM, et al.. Maternal, infant, and child health outcomes associated with the special supplemental nutrition program for women, infants, and children : a systematic review. Ann Intern Med. 2022;175:1411–22, https://doi.org/10.7326/M22-0604.Suche in Google Scholar PubMed
54. Caulfield, LE, Bennett, WL, Gross, SM, Hurley, KM, Ogunwole, SM, Venkataramani, M, et al.. Maternal and child outcomes associated with the special supplemental nutrition program for women, infants, and children (WIC). Rockville (MD): Agency for Healthcare Research and Quality (US); 2022.10.23970/AHRQEPCCER253Suche in Google Scholar PubMed
55. Carbone, ET, Zoellner, JM. Nutrition and health literacy: a systematic review to inform nutrition research and practice. J Acad Nutr Diet 2012;112:254–65. https://doi.org/10.1016/j.jada.2011.08.042.Suche in Google Scholar PubMed
© 2025 the author(s), published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.
Artikel in diesem Heft
- Research Articles
- Relationship between body mass index and quality of life, use of dietary and physical activity self-management strategies, and mental health in individuals with polycystic ovary syndrome
- Evaluating the challenges and opportunities for diabetes care policy in Nigeria
- Body mass index is associated with subjective workload and REM sleep timing in young healthy adults
- Prediction of hypoglycaemia in subjects with type 1 diabetes during physical activity
- Investigation by the Epworth Sleepiness Scale of daytime sleepiness in professional drivers during work hours
- Understanding public awareness of fall epidemiology in the United States: A national cross-sectional study
- Impact of Covid-19 stress on urban poor in Sylhet Division, Bangladesh: A perception-based assessment
- Impact of the COVID-19 pandemic on mental health, relationship satisfaction, and socioeconomic status: United States
- Psychological factors influencing oocyte donation: A study of Indian donors
- Cervical cancer in eastern Kenya (2018–2020): Impact of awareness and risk perception on screening practices
- Older LGBTQ+ and blockchain in healthcare: A value sensitive design perspective
- Trends and disparities in HPV vaccination among U.S. adolescents, 2018–2023
- Do cell towers help increase vaccine uptake? Evidence from Côte d’Ivoire
- In search of the world’s most popular painkiller: An infodemiological analysis of Google Trend statistics from 2004 to 2023
- Brain fog in chronic pain: A concept analysis of social media postings
- Association between multidimensional poverty intensity and maternal mortality ratio in Madagascar: Analysis of regional disparities
- A “disorder that exacerbates all other crises” or “a word we use to shut you up”? A critical policy analysis of NGOs’ discourses on COVID-19 misinformation
- Smartphone use and stroop performance in a university workforce: A survey-experiment
- Review Articles
- The management of body dysmorphic disorder in adolescents: A systematic literature review
- Navigating challenges and maximizing potential: Handling complications and constraints in minimally invasive surgery
- Examining the scarcity of oncology healthcare providers in cancer management: A case study of the Eastern Cape Province, South Africa
- Dietary strategies for irritable bowel syndrome: A narrative review of effectiveness, emerging dietary trends, and global variability
- The impact of intimate partner violence on victims’ work, health, and wellbeing in OECD countries (2014–2025): A descriptive systematic review
- Nutrition literacy in pregnant women: a systematic review
- Short Communications
- Experience of patients in Germany with the post-COVID-19 vaccination syndrome
- Five linguistic misrepresentations of Huntington’s disease
- Letter to the Editor
- PCOS self-management challenges transcend BMI: A call for equitable support strategies
Artikel in diesem Heft
- Research Articles
- Relationship between body mass index and quality of life, use of dietary and physical activity self-management strategies, and mental health in individuals with polycystic ovary syndrome
- Evaluating the challenges and opportunities for diabetes care policy in Nigeria
- Body mass index is associated with subjective workload and REM sleep timing in young healthy adults
- Prediction of hypoglycaemia in subjects with type 1 diabetes during physical activity
- Investigation by the Epworth Sleepiness Scale of daytime sleepiness in professional drivers during work hours
- Understanding public awareness of fall epidemiology in the United States: A national cross-sectional study
- Impact of Covid-19 stress on urban poor in Sylhet Division, Bangladesh: A perception-based assessment
- Impact of the COVID-19 pandemic on mental health, relationship satisfaction, and socioeconomic status: United States
- Psychological factors influencing oocyte donation: A study of Indian donors
- Cervical cancer in eastern Kenya (2018–2020): Impact of awareness and risk perception on screening practices
- Older LGBTQ+ and blockchain in healthcare: A value sensitive design perspective
- Trends and disparities in HPV vaccination among U.S. adolescents, 2018–2023
- Do cell towers help increase vaccine uptake? Evidence from Côte d’Ivoire
- In search of the world’s most popular painkiller: An infodemiological analysis of Google Trend statistics from 2004 to 2023
- Brain fog in chronic pain: A concept analysis of social media postings
- Association between multidimensional poverty intensity and maternal mortality ratio in Madagascar: Analysis of regional disparities
- A “disorder that exacerbates all other crises” or “a word we use to shut you up”? A critical policy analysis of NGOs’ discourses on COVID-19 misinformation
- Smartphone use and stroop performance in a university workforce: A survey-experiment
- Review Articles
- The management of body dysmorphic disorder in adolescents: A systematic literature review
- Navigating challenges and maximizing potential: Handling complications and constraints in minimally invasive surgery
- Examining the scarcity of oncology healthcare providers in cancer management: A case study of the Eastern Cape Province, South Africa
- Dietary strategies for irritable bowel syndrome: A narrative review of effectiveness, emerging dietary trends, and global variability
- The impact of intimate partner violence on victims’ work, health, and wellbeing in OECD countries (2014–2025): A descriptive systematic review
- Nutrition literacy in pregnant women: a systematic review
- Short Communications
- Experience of patients in Germany with the post-COVID-19 vaccination syndrome
- Five linguistic misrepresentations of Huntington’s disease
- Letter to the Editor
- PCOS self-management challenges transcend BMI: A call for equitable support strategies


