Abstract
Background
In 2023, Kenya recorded approximately 5,845 new cervical cancer cases and 3,591 deaths, primarily affecting women aged 30–49 due to persistent high-risk human papillomavirus (HPV) infections. This study aimed to assess the awareness of cervical cancer, its causes, risk factors, symptoms, and screening rates among women aged 18–46 seeking reproductive health care in eastern Kenya from 2018 to 2020.
Objectives
The aims of this study were to evaluate cervical cancer awareness, its causes, risk factors, and symptoms, and to explore the association between awareness and screening uptake among women in eastern Kenya.
Methods
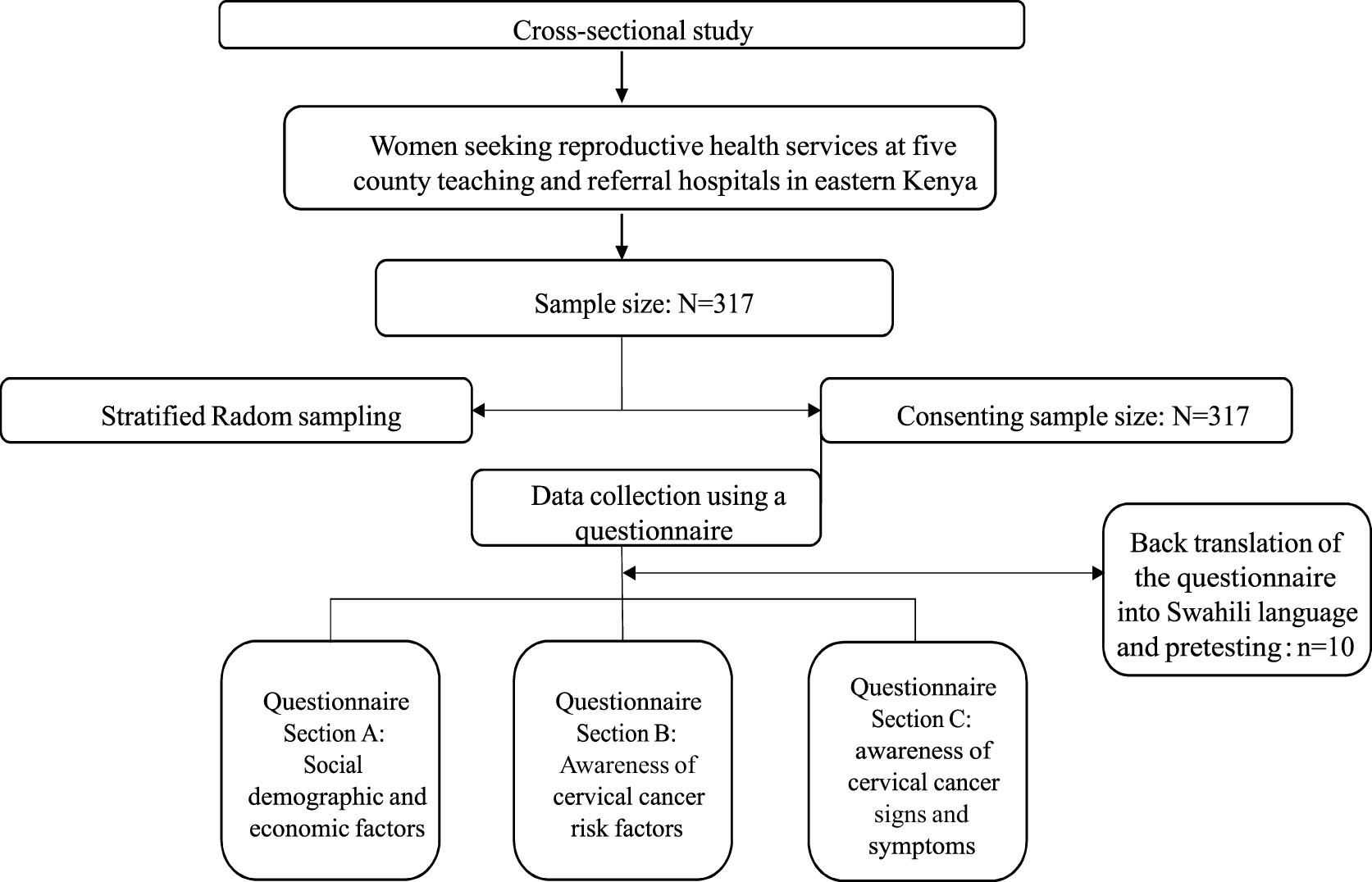
A cross-sectional survey was conducted in Meru, Tharaka-Nithi, Kirinyaga, Embu, and Isiolo counties between 2018 and 2020. Stratified and simple random sampling was used to select participants, resulting in a total of 317 women aged 18–46 years. Data were collected through structured face-to-face interviews and analyzed using SPSS v25. Descriptive statistics summarized key variables, and logistic regression analysis assessed the association between awareness and screening uptake (p < 0.05).
Results
The mean age of participants was 34.2 years (standard deviation ± 10.4). While 93.7% were aware of cervical cancer, only 24.7% identified HPV as its cause, and just 12.5% had undergone screening. Screening uptake was higher in Embu, among women under 30, and those with primary education. Hormonal contraceptive users were less likely to be screened (odd ratio: 0.48, confidence interval: 0.2–0.8).
Conclusion
Despite high awareness, knowledge gaps about cervical cancer’s cause and prevention remain. Targeted educational efforts are necessary to enhance screening uptake in underserved communities.
1 Introduction
Cervical cancer remains a significant global health challenge, ranking as the fourth most common cancer among women, with an estimated 660,000 new cases and 350,000 deaths reported in 2023 – over 85% of these cases occurring in low- and middle-income countries (LMICs) [1,2,3]. In Kenya, cervical cancer is the second most common cancer among women after breast cancer, with an estimated 5,845 new cases and 3,211 deaths annually [1,3]. Despite being largely preventable through early detection and treatment, Kenya continues to experience high mortality rates due to persistent high-risk human papillomavirus (HPV) infections, low awareness, poor screening uptake, and late-stage diagnosis [4,5].
Cancer is defined as the uncontrolled growth of abnormal cells that may invade nearby tissues or spread to distant organs. This uncontrolled growth can be influenced by genetic mutations, environmental exposures, and lifestyle factors [2,3,4,5]. Cervical cancer typically develops through a gradual progression of cervical intraepithelial neoplasia (CIN), leading to stages such as CIN 1 (mild dysplasia), CIN 2 (moderate dysplasia), CIN 3 (severe dysplasia), carcinoma in situ (full-thickness abnormal cells without invasion), and finally invasive cervical cancer (ICC) [4,5,6].
The burden of cervical cancer in LMICs is exacerbated by societal and structural risk factors such as limited healthcare access, poverty, low awareness, gender inequality, and cultural stigma surrounding reproductive health [3,4]. In rural and marginalized communities, women face financial, logistical, and psychosocial barriers to screening and vaccination. Misinformation and fatalistic beliefs about cancer further delay diagnosis and care [4,5]. Sub-Saharan Africa, including Kenya, bears a disproportionately high cervical cancer burden, with human immunodeficiency virus (HIV) infection increasing susceptibility to HPV and contributing to high incidence and mortality [7,8].
HPV genotyping advancements have identified high-risk strains, notably HPV16 and HPV18, as key contributors to cervical dysplasia and CIN. Persistent infection with these strains can progress to ICC, if untreated [4,6,8,9,10]. In response, the World Health Organization (WHO) launched the 90:70:90 strategy – aiming for 90% HPV vaccination coverage among girls by age 15, 70% cervical screening coverage by ages 35 and 45, and 90% access to treatment for precancer and cancer cases [1,4,9,11]. Kenya’s National Cancer Control Strategy (2023–2027) supports these targets, but major gaps persist in rural and underserved areas where awareness, screening, and vaccination remain critically low [4,8].
Physiological and behavioral risk factors such as early sexual debut, prolonged hormonal contraceptive use, pregnancy-related cervical changes, and immunocompromised conditions like HIV increase susceptibility to persistent HPV infection [12]. Early-stage cervical cancer symptoms are often vague, including irregular bleeding and abnormal discharge, making early detection reliant on routine screening services that many women in eastern Kenya cannot access [11,13].
Although studies on cervical cancer and HPV exist, few explore awareness of risk factors and symptoms in high HIV-prevalent rural areas. This study uses the Health Belief Model (HBM) to examine how awareness and perceptions influence screening uptake [14].
1.1 Rationale
Cervical cancer remains a major health burden in Kenya due to persistent HPV infections, low awareness, poor screening uptake, and late diagnosis. Rural areas face greater barriers to screening and vaccination, highlighting the need to assess awareness and its influence on screening behavior to inform effective prevention strategies.
Research questions
What is the level of awareness of cervical cancer risk factors, symptoms, and prevention among women in eastern Kenya’s resource-limited communities?
Is there an association between cervical cancer awareness and the utilization of screening services?
Study objectives
To determine awareness of cervical cancer, its causes, risk factors, and symptoms among women aged 18–46 years in eastern Kenya.
To determine the association between cervical cancer awareness and screening uptake among women aged 18–46 years in eastern Kenya.
2 Materials and methods
This cross-sectional study was conducted among women seeking reproductive health services at five county teaching and referral hospitals in eastern Kenya. The facilities included Isiolo Referral Hospital (Isiolo County), Kerugoya County Hospital (Kirinyaga County), Meru Teaching and Referral Hospital (Meru County), Chuka Teaching and Referral Hospital (Tharaka-Nithi County), and Embu Teaching and Referral Hospital (Embu County). These counties were purposively selected to represent a broad range of geographic, cultural, and socio-economic contexts within eastern Kenya.
2.1 Sample size determination and sampling procedures
The sample size (N = 317) was calculated using the formula [15]: n = Z 2 P(1–P)/d 2, where Z is the Z-score for a 95% confidence interval (CI) (1.96), P is the estimated infection rate (2.8%), and d is the margin of error (0.02) [14]. The infection rate was based on the annual proportion of patients presenting with reproductive health infections, as reported in hospital records.
Stratified sampling was employed across the five counties, and simple random sampling was used within each hospital to select participants. Sample distribution was guided by the cervical abnormality reports from January 2018 (n = 27), resulting in the following participant allocation: Embu (85), Meru (81), Isiolo (64), Kirinyaga (56), and Tharaka-Nithi (31).
2.2 Inclusion and exclusion criteria
The study targeted women aged 18–46 years who were residents of eastern Kenya and attended clinics for voluntary HIV counselling and testing, family planning, or routine cervical cancer screening between January 2018 and December 2020. Although cervical screening is generally recommended from the age of 25 [7], this study included younger women under 25 who presented with reproductive health concerns or known cervical abnormalities. The age range of 18–46 years was selected to capture sexually active women within the reproductive age group who are most at risk of HPV infection and cervical cancer and who commonly present with reproductive health concerns in the Kenyan clinical context [1]. No exclusion criteria were applied.
2.3 Data collection and measures
Data were collected using a structured, pre-tested questionnaire translated into Swahili and back-translated to ensure accuracy and cultural relevance. The questionnaire was pilot-tested among ten women from Embu and Meru counties, who were not included in the main study. Feedback from the pre-test informed revisions for clarity and contextual appropriateness.
The questionnaire consisted of three sections: Section A: Socio-demographic and economic characteristics; Section B: Awareness of cervical cancer risk factors, including parity, number of sexual partners, age at sexual debut, history of urinary tract infections, and prior screening. Responses were classified as “aware” or “not aware,” and Section C: Awareness of cervical cancer symptoms, sources of information (e.g., media, healthcare providers), belief in cancer treatability (yes/no), and screening frequency (reported in days, months, or years). The questionnaire also included a specific item on whether the participant had ever been screened for cervical cancer to assess the relationship between awareness and screening uptake.
2.4 Data analysis procedures
Data were analyzed using SPSS version 20. Descriptive statistics (frequencies and percentages) were used to summarize socio-demographic factors and awareness levels. Pearson’s chi-square test examined the associations between categorical variables, such as awareness and screening behavior. Multivariate logistic regression analysis was used to evaluate the association between screening uptake and awareness of risk factors and symptoms.
2.5 Ethical considerations
Ethical approval was obtained from the Kenya Medical Research Institute (KEMRI) Scientific and Ethical Review Unit (Approval Number: KEMRI/-SERU/CVR/004/3342). Written informed consent was obtained from all participants prior to enrolment, and confidentiality was maintained throughout the study.
3 Results
3.1 Baseline social demographic factors and the recognizable risks associated with cervical cancer
A total of 317 women (mean age: 34 years and 3 months, standard deviation 10.395) were recruited from Meru (81/317 [25.6%]), Tharaka-Nithi (31/317 [9.8%]), Kirinyaga (56/317 [17.6%]), Embu (85/317 [26.8%]), and Isiolo (64/317 [20.2%]). Logistic regression analysis shows that participants with parity up to three had a higher cervical screening rate (7.9%) and an increased likelihood of undergoing cervical screening (odd ratio: 2.9 [CI: 1.02–8.6]) than participants with a higher parity (2.8%). Those with primary school (16.7%) and college or university education (15.0%) had higher cervical cancer screening rates than women with secondary education (9.6%) (Table 1).
Association between socio-demographic factors, cervical cancer screening rates, and awareness of recognizable risk factors in eastern Kenya (2018–2020)
| Characteristics Category | Total participants [N/(%)] | Cervical screening rate | Screening rate by risk factors associated with cervical cancer (odd ratio [95% CI]) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Multiple sex partners | Smoking habit | Prolonged hormonal contraceptives use | Multiparity (>3) | Early sex debut | Recurrent UTIs | HIV infection | |||
| Residence | |||||||||
| Meru | 81 (25.6) | 7 (8.6) | 1.1 (0.4–2.6) | 0.98 (0.2–3.9) | 1.22 (0.4–3.9) | 0.86 (0.1–8.6) | 1.16 (0.2–6.0) | 0.522 (0.2–1.2) | 1.12 (0.5–2.7) |
| Kirinyaga | 56 (17.6) | 4 (7.1) | 3.85 (1.3–11.3) | 1.39 (0.3–6.6) | 0.63 (0.2–1.9) | 1.8 (0.1–30.4) | 1.7 (0.3–9.1) | 0.37 (0.1–0.9) | 0.93 (0.4–2.3) |
| Embu | 85 (26.8) | 13 (15.3) | 6.13 (2.1–17.8) | 1.03 (0.2–4.1) | 0.89 (0.2–2.7) | 0.67 (0.7–6.2) | 2.6 (0.5–12.3) | 0.34 (0.1–0.8) | 0.71 (0.3–1.71 |
| Isiolo | 64 (20.2) | 7 (10.9) | 2.6 (0.9–7.1) | 1.26 (0.3–5.6) | 1.17 (0.3–3.8) | 2.2 (0.1–34.7) | 1.2 (0.2–6.7) | 0.46 (0.2–1.2) | 1.81 (0.7–4.4) |
| T. Nithi | 31 (9.8) | 3 (9.3) | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Age | |||||||||
| ≤30 | 219 (69.1) | 24 (11.0) | 0.87 (0.5–1.6) | 0.98 (0.4–2.2) | 1.5 (0.8–2.8) | 0.14 (0.1–0.2) | 1.45 (0.6–3.3) | 1.06 (0.6–1.7) | 0.57 (0.3–0.9) |
| >30 | 98 (30.8) | 10 (10.2) | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Education | |||||||||
| Primary | 96 (30.3) | 16 (16.7) | 0.7 (0.2–2.6) | 0.81 (0.1–4.2) | 4.1 (1.2–13.7) | 1.19 (0.1–11.9) | 7.1 (2.5–2.0) | 2.4 (0.7–8.2) | 3.0 (0.7–11.4) |
| Secondary | 135 (42.6) | 13 (9.6) | 1.07 (0.3–3.5) | 1.7 (0.3–9.7) | 1.87 (0.6–5.5) | 1.66 (0.2–17.1) | 7.3 (2.8–9.3) | 2.7 (0.8–8.9) | 4.0 (1.1–14.7) |
| College/university | 86 (27.1) | 5 (15.0) | Ref | ||||||
| Marital status | |||||||||
| Married | 228 (71.9) | 23 (10.2) | 0.9 (0.2–4.3) | 2.15 (0.4–11.3) | 1.66 (0.4–6.9) | 1.2 (0.32–4.7) | 2.84 (0.8–9.0) | 0.45 (0.1–1.5) | 3.1 (0.7–15.3) |
| Separated | 89 (28.1) | 11 (33.0) | 0.51 (0.9–2.8) | 3.27 (0.4–28.2) | 14.12 (1.2–2) | 10.3 (0.9–11.8) | 2.2 (0.4–11.4) | 0.29 (0.1–1.2) | 3.3 (0.6–18.6) |
| Widowed | Ref | Ref | Ref | Ref | Ref | Ref | Ref | ||
| Religion | |||||||||
| Christian | 255 (80.4) | 30 (11.8) | 1.2 (0.6–2.4) | 1.48 (0.5–3.7) | 0.43 (0.2–1.1) | 0.46 (0.1–3.7) | 0.99 (0.4–2.5) | 1.38 (0.7–2.5) | 0.52 (0.2–0.9) |
| Muslim | 62 (19.6) | 4 (6.5) | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| FP method | |||||||||
| Hormonal | 94 (29.4) | 11 (3.5) | 0.68 (0.3–1.5) | 0.84 (0.3–2.1) | 2.08 (1.1–3.9) | 4.2 (1.1–15.9) | 1.65 (0.7–4.1) | 1.33 (0.8–2.2) | 0.54 (0.3–0.9) |
| Non-hormonal | 223 (70.3) | 23 (7.3) | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Parity | |||||||||
| >3 | 68 (21.5) | 9 (2.8) | 0.94 (0.5–1.8) | 0.79 (0.29–1.9) | 1.28 (0.5–2.7) | 0.37 (0.1–1.3) | 0.65 (0.2–1.7) | 0.56 (0.3–1.1) | 1.68 (0.9–2.9) |
| ≤3 | 249 (78.5) | 25 (7.9) | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
Notes: Categorized socio-demographic characteristics and their frequencies among study participants (N = 317). The cervical cancer screening rate was calculated based on the total number of participants. Binary logistic regression was used to assess the association between socio-demographic factors and cervical cancer screening rates, stratified by awareness of risk factors. UTI = urinary tract infection; HIV = human immunodeficiency virus; FP method = family planning method; CI = confidence interval.
3.2 Awareness of cervical cancer and screening rate
Multivariate analysis revealed an overall low cervical screening rate (10.7%), increased awareness of cervical cancer (93.7%), decreased awareness of its causes (24.7%), and recommended screening cycle (12.5%). However, the screening rate (10.2%) increased in participants who were more aware of having cervical cancer than in other categories. The most recognizable symptoms of cervical cancer were the presence of blood in the urine (89.9%), pelvic pain (89.0%), and vaginal discharge (88.7%) (Figure 1).
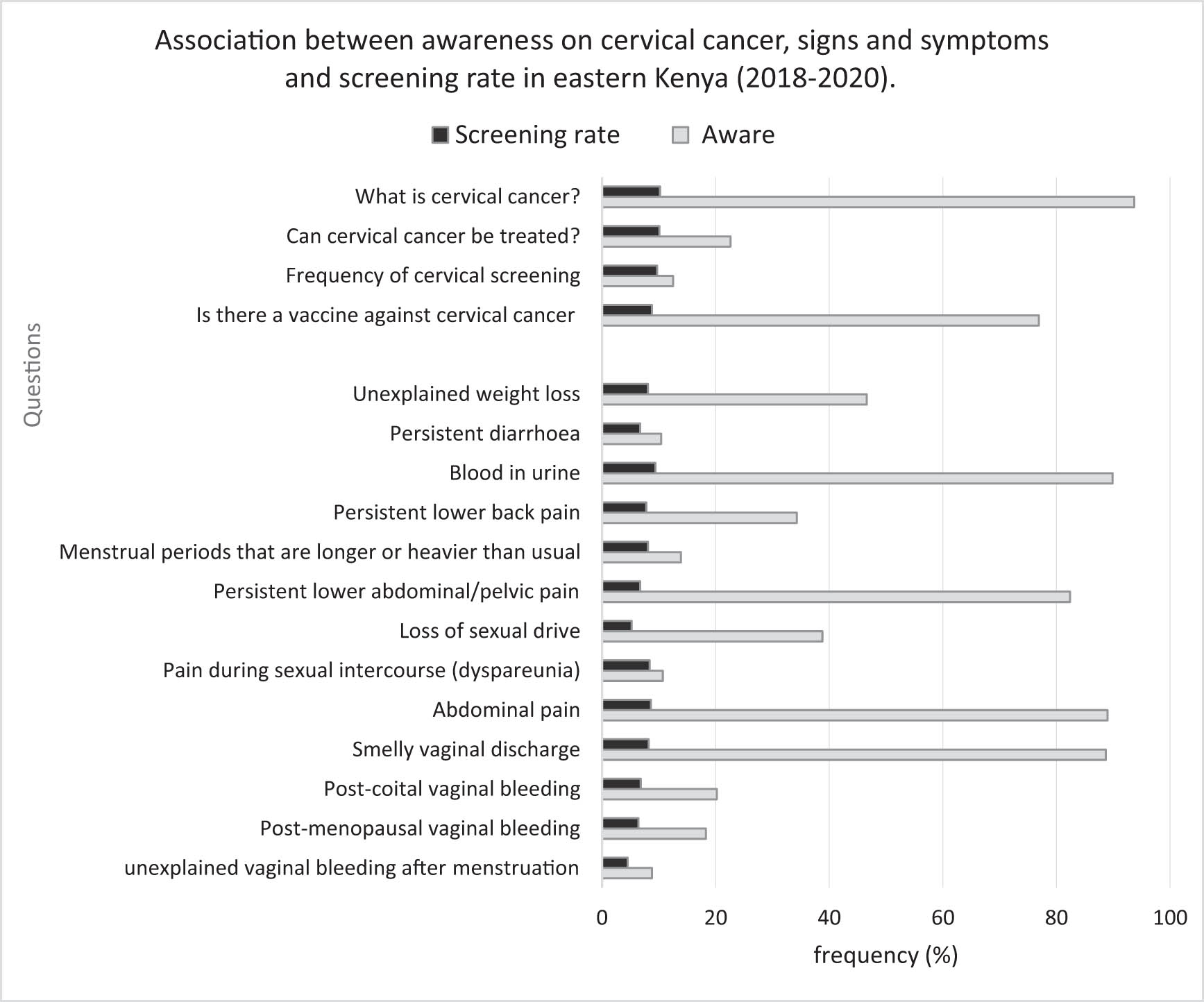
Awareness of cervical cancer disease and screening uptake. The figure shows responses given by participants on cervical cancer and 13 symptoms against screening uptake.
3.3 Cervical screening rate by the source of information
Women whose main source of information about cervical cancer was television (72/317 [22.7%]; screening rate: 17/317 [5.4%]) reported the increased utilization of cervical screening compared to other sources (Figure 2).
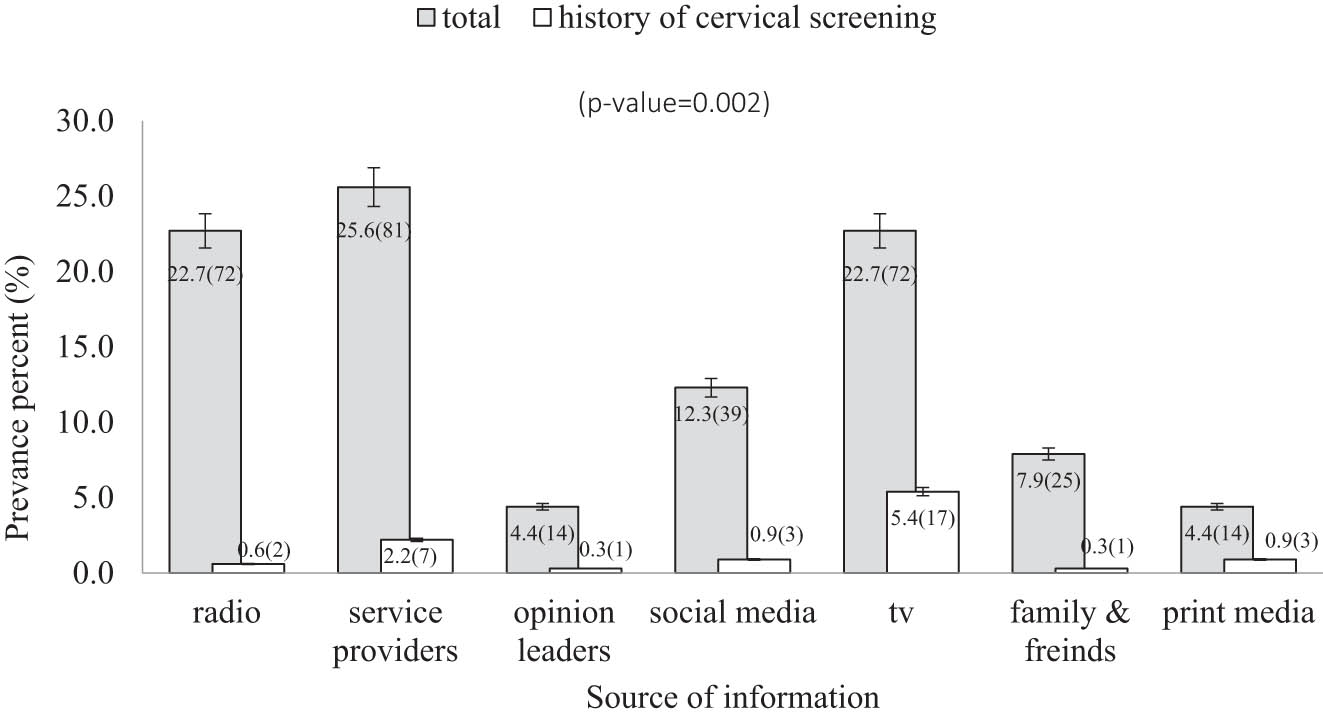
Cervical screening rate by the source of information in eastern Kenya (2018–2020). The figure shows participants’ source of information and impact on cervical screening uptake. Participants were highly likely to undergo cervical screening if their main source of information was television than other sources.
4 Discussion
This study reveals a high level of cervical cancer awareness (93.7%) among women, which is consistent with findings from western Kenya (81%) [16], Uasin Gishu (91.4%) [17], eastern Kenya (80%) [18], Kisii Town (84.1%) [19], and in Uganda [20]. This widespread awareness is likely a result of ongoing public health awareness campaigns detailed in Kenya’s National Cancer Control Strategy, 2017–2022 [4]. However, despite high awareness, screening uptake remains critically low, a concern also highlighted by previous studies [19,21]. This finding underscores the disconnection between knowledge and behavior change, emphasizing the need for systemic approaches to translate awareness into action.
National cervical cancer screening coverage in Kenya remains alarmingly low, with an estimated 14% coverage as of 2020 [21], similar to findings in western Kenya (22%) [19] and Kisii (16.6%) [19]. As previously noted, regional disparities in screening uptake remain, with urban areas like Nairobi reporting higher rates (20–30%) than rural areas, where access to services remains a significant barrier [3]. These regional variations highlight the critical need for equitable access to cervical cancer screening across Kenya and the importance of addressing the infrastructural challenges of system-level interventions for cancer care in Kenya [22].
The study also found that younger women (<30 years), single women, and those with primary education or higher incomes were more likely to participate in screening. This finding aligns with studies in Kisii Town [16] and Uganda [23], which emphasize that socio-economic factors play a major role in determining health-seeking behavior [21]. Furthermore, younger women tend to have a higher perceived susceptibility to HPV and are more likely to undergo screening due to increased public health awareness and the availability of HPV vaccination programs [21,24,25]. This suggests that public health efforts should prioritize younger women as a target group for screening campaigns to improve uptake, especially in rural and underserved areas.
Despite high awareness, misconceptions about cervical cancer treatment options persist. Only 22.6% of participants believed the disease was treatable, a finding consistent with earlier research in Kisii Town (17.4%) [16], and but significantly lower than figures reported in Uganda (92%) [20]. These discrepancies underscore the need for targeted public health education to correct misconceptions and emphasize the importance of early detection and treatment [3]. This is supported by a study [19] which highlighted that a lack of awareness about the treatability of cervical cancer can negatively influence health-seeking behavior and early detection efforts in African settings [19].
Another key finding of this study was the substantial knowledge gap regarding the etiology of cervical cancer, as 79.3% of the participants were unaware that HPV is the primary cause. This trend mirrors findings of 75.6% in Uashin Gishu, Kenya [16], Uganda [19], Ethiopia [24], and India [26], where low awareness of HPV as the cause of cervical cancer contributes to missed opportunities for prevention and early detection. This gap in knowledge highlights the need for targeted educational campaigns that emphasize the HPV–cervical cancer link, particularly given that the burden of cervical cancer remains high in many African countries [3].
Awareness of key cervical cancer symptoms such as dyspareunia and postmenstrual bleeding was alarmingly low in this study, which is consistent other studies [16,26,27]. Although symptoms such as persistent vaginal discharge and pelvic pain were more frequently recognized, they are non-specific and may delay timely diagnosis. This underscores the need for public health education to emphasize early, less ambiguous symptoms [28,29]. Additionally, the source of information significantly influenced screening behavior. Women whose main source of information was television (22.7%) demonstrated a higher screening uptake than those informed through other means. This supports findings from the 2022 Kenya DHS [30], which showed a 31% increase in screening among women exposed to mass media [25,28,30]. Moreover, interpersonal communication from healthcare providers, particularly when reinforced by media messages, has been shown to further enhance screening uptake [31]. Effective interventions should integrate symptom education with accessible, trusted, and culturally appropriate communication strategies [21,22,28].
5 Conclusion, limitations, and recommendations
This study demonstrates that although awareness of cervical cancer among women has increased, the uptake of preventive measures – such as regular screening and HPV vaccination – remains substantially low. While many participants were familiar with cervical cancer, their understanding of its causes, symptoms, risk factors, and recommended screening intervals was often limited or inaccurate. These findings highlight that awareness, although necessary, is not sufficient to catalyze preventive health behaviors, underscoring a persistent gap between knowledge and action.
Theoretically, the study contributes to the literature by illustrating the need to expand health behavior models to incorporate contextual realities such as economic hardship, cultural norms, and systemic healthcare limitations. It also emphasizes the potential of incentive systems theory within health organizations to drive provider and community engagement in promoting prevention, including HPV vaccination and regular screening. A systems-thinking approach is essential to address the interlinked structural and behavioral determinants of cervical cancer control.
From a policy and practice perspective, systematized public health interventions are crucial. Strategies must go beyond awareness to include culturally appropriate, economically accessible, and incentive-based initiatives such as subsidized screening, school-based HPV vaccination programs, community mobilization, and engagement through mass media and trusted local figures. Building public trust and tailoring communication to specific community contexts are also essential.
Several limitations must be acknowledged. The self-developed questionnaire was not validated for the African context, limiting reliability and comparability. The cross-sectional design precludes causal conclusions. Translation challenges may have diluted key terms, while categorical responses potentially oversimplified complex perceptions. The small sample size and geographic scope constrain generalizability. Recall, interviewer, and social desirability biases may have affected responses. The study also did not assess internal consistency of the questionnaire and excluded women not seeking care, further limiting representativeness. Additionally, the lack of triangulation with qualitative methods reduced the depth of behavioral insights.
To improve preventive uptake, national and county governments should strengthen culturally grounded health education and expand HPV vaccination via school and community-based programs. Sustainable interventions should be supported by monitoring frameworks and economic incentives, with active involvement from civil society and private-sector partners. Future research should develop validated tools and explore structural and sociocultural barriers to behavior change.
Acknowledgments
Special thanks to the National Council for Science Technology and Innovation (NACOSTI) and Kenya National Research Fund (NRF) for funding this project and Kenyatta University for accepting this project as an academic proposal. Thank you to all the staff at Level Five, Referral and Teaching Hospitals in Meru, Embu, Kirinyaga, Isiolo, and Tharaka-Nithi counties in eastern Kenya for allowing us to interview their clients.
-
Funding information: Research approval and funding was obtained from the Kenya National Commission for Science, Technology and Innovation and Kenya National Research Fund. Ref: NACOSTI/P/17/85191/15335.
-
Author contributions: All authors have accepted responsibility for the entire content of this manuscript and consented to its submission to the journal. All authors reviewed the final manuscript. NJK, MM, LK, and RL designed the study and designed the questionnaire. NJK conducted the survey, interpreted the data, and wrote the main manuscript text.
-
Conflict of interest: Authors state no conflict of interest.
-
Ethical approval: This study was approved by the KEMRI Scientific and Ethical Review Unit (Approval Number: KEMRI/-SERU/CVR/004/3342). Participants were required to sign an informed consent form before inclusion into the study.
-
Informed consent: Informed consent was obtained from all individuals included in this study, or their legal guardians or wards.
-
Data availability statement: The datasets and questionnaires analyzed during the current study are available from the corresponding author upon reasonable request.
References
[1] World Health Organization (WHO). Global strategy to accelerate the elimination of cervical cancer as a public health problem. 2024. Retrieved from https://www.who.int/news-room/fact-sheets/detail/cervical-cancer.Suche in Google Scholar
[2] TogetHER for Health. Global burden of cervical cancer. 2024. Retrieved from https://togetherforhealth.org/global-burden-cervical-cancer/.Suche in Google Scholar
[3] Ministry of Health, Kenya. Cervical cancer-related deaths and new cases in Kenya. 2025. Retrieved from https://www.health.go.ke/kenya-intensifies-efforts-combat-cervical-cancer-amid-rising-burden.Suche in Google Scholar
[4] BMC Public Health. Cervical cancer screening and its associated factors among women of reproductive age in Kenya. 2024. Retrieved from https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-024-18148-y.Suche in Google Scholar
[5] Elmi AA, Bansal D, Acharya A, Skariah S, Dargham SR, Abu-Raddad LJ, et al. Human papillomavirus (HPV) infection: Molecular epidemiology, genotyping, seroprevalence and associated risk factors among Arab women in Qatar. PLoS One. 2017;12(1):e0169197.10.1371/journal.pone.0169197Suche in Google Scholar PubMed PubMed Central
[6] Nayar R, Wilbur DC, editors. The Bethesda system for reporting cervical cytology: definitions, criteria, and explanatory notes. 3rd edn. Cham, Switzerland: Springer International Publishing; 2015. 10.1007/978-3-319-11074-5.Suche in Google Scholar
[7] Ministry of Health, Kenya. National cancer control strategy 2023–2027 [Internet]. Nairobi: Government of Kenya; 2023 [cited 2025 Mar 12]. https://www.iccp-portal.org/system/files/plans/NATIONAL%20CANCER%20CONTROL%20STRATEGY%202023-2027_compressed.pdf.Suche in Google Scholar
[8] Pratiwi N, Ulfah AJ, Rachmadina R, Irham LM, Afief AR, Adikusuma W, et al. Promising candidate drug target genes for repurposing in cervical cancer: A bioinformatics-based approach. Narra J. 2024;4(3):e938.10.52225/narra.v4i3.938Suche in Google Scholar PubMed PubMed Central
[9] Anakwenze C, Kalra A, Lumley C, Geng Y, Grover S. Cervical cancer stage distribution and survival outcomes in Africa: A systematic review and meta-analysis. Int J Gynecol Cancer. 2025;35(1):100008.10.1016/j.ijgc.2024.100008Suche in Google Scholar PubMed
[10] Bruni L, Albero G, Serrano B, Mena M, Collado JJ, Gómez D, et al. ICO/IARC Information Centre on HPV and Cancer (HPV Information Centre). Human papillomavirus and related diseases report-World. HPV Information Centre; 2023.Suche in Google Scholar
[11] World Health Organization. Cervical cancer elimination initiative: Global strategy for the elimination of cervical cancer as a public health problem. Geneva: WHO; 2020. [cited 2025 Mar 12] https://www.who.int/publications/i/item/9789240014107.Suche in Google Scholar
[12] George Onyango C, Ogonda L, Guyah B. The role of co-infections and hormonal contraceptives in cervical intraepithelial neoplasia prevalence among women referred to a tertiary hospital in Western Kenya. Infect Agents Cancer. 2025;20(1):11.10.1186/s13027-024-00620-4Suche in Google Scholar PubMed PubMed Central
[13] World Health Organization. WHO guideline for screening and treatment of cervical pre-cancerous lesions for cervical cancer prevention. Geneva: WHO; 2021 Jul. [cited 2025 Mar 12] https://www.who.int/publications/i/item/9789240066489.Suche in Google Scholar
[14] Yirsaw AN, Tefera M, Bogale EK, Abebe E, Alemayehu A, Abebe D, et al. Applying the Health Belief Model to cervical cancer screening uptake among women in Ethiopia: A systematic review and meta-analysis. BMC Cancer. 2024;24:Article 1055. 10.1186/s12885-024-13055-2.Suche in Google Scholar PubMed PubMed Central
[15] Harvard Medical School. N in statistics: How to determine the right sample size for your study. RITS Cloud; 2025 Feb. https://ritscloud.hms.harvard.edu/n-in-statistics-how-to-determine-the-right-sample-size-for-your-study.Suche in Google Scholar
[16] Sakwa G, Bukhala P, Kipmerewo M, Kwena Z. Knowledge, attitude and practices in cervical cancer screening in Kakamega County, Kenya. J Health Med Nurs. 2021;7(3):51–66. 10.47604/jhmn.1427.Suche in Google Scholar
[17] Kemboi G, Obiri J, Mutai C. Awareness of cervical cancer among women in Uasin Gishu County, Kenya. Int J Sci Basic Appl Res. 2018;41(1):167–80.Suche in Google Scholar
[18] Gatumo M, Gacheri S, Sayed AR, Scheibe A. Women’s knowledge and attitudes related to cervical cancer and cervical cancer screening in Isiolo and Tharaka Nithi counties, Kenya: A cross-sectional study. BMC Cancer. , 2018 Jul;18(1):745. 10.1186/s12885-018-4642-9.Suche in Google Scholar PubMed PubMed Central
[19] Kei RM, M’Ndegwa JK, Ndwiga T, Masika F. Challenges of cervical cancer screening among women of reproductive age in Kisii Town, Kisii County, Kenya. Sci J Public Health. 2016;4:289.10.11648/j.sjph.20160404.14Suche in Google Scholar
[20] Adoch W, Garimoi CO, Scott SE, Okeny GG, Moodley J, Komakech H, et al. Knowledge of cervical cancer risk factors and symptoms among women in a refugee settlement: A cross-sectional study in northern Uganda. Confl Health. 2020;14(1):1–9.10.1186/s13031-020-00328-3Suche in Google Scholar PubMed PubMed Central
[21] Gatune JW, Nyamongo IK. Predictors of cervical cancer screening among Kenyan women: Results of a nested case-control study in a nationally representative survey. BMC Public Health. 2021;21:1234. 10.1186/s12889-021-11234-5. Taflinger S, Sattler S. A situational test of the health belief model: How perceived susceptibility mediates the effects of the environment on behavioral intentions. Soc Sci Med. 2024;346:116715. 10.1016/j.socscimed.2024.116715.Suche in Google Scholar PubMed PubMed Central
[22] Maloba M, Wamai R, Mwaura-Tenambergen W. Systems-based interventions for cervical cancer prevention in Kenya: An integrative review. Afr J Reprod Health. 2022;26(1):47–55.Suche in Google Scholar
[23] Mwaka AD, Orach CG, Were EM, Lyratzopoulos G, Wabinga H, Roland M. Awareness of cervical cancer risk factors and symptoms: A cross-sectional community survey in post-conflict northern Uganda. Health Expect. 2016;19(4):854–67. 10.1111/hex.12382.Suche in Google Scholar PubMed PubMed Central
[24] Okyere J. Multiple sexual partnership as an independent predictor of cervical cancer screening among women of reproductive age: An analysis of the 2022 Kenya demographic and health survey. BMC Cancer. 2025;25(1):259.10.1186/s12885-025-13704-0Suche in Google Scholar PubMed PubMed Central
[25] Agimas MC, Adugna DG, Derseh NM, Kassaw A, Kassie YT, Abate HK, et al. Uptake of human papillomavirus vaccine and its determinants among females in East Africa: A systematic review and meta-analysis. BMC Public Health. 2024;24:Article 842. 10.1186/s12889-024-18141-5.Suche in Google Scholar PubMed PubMed Central
[26] Priya N, Sharma S. Awareness of cervical cancer and its screening among women in rural and urban areas of Haryana, India: A cross-sectional study [Internet]. PubMed; 2020 [cited 2025 Mar 12]. https://pubmed.ncbi.nlm.nih.gov/32112367/.Suche in Google Scholar
[27] Gebisa T, Bala ET, Deriba BS. Knowledge, attitude, and practice toward cervical cancer screening among women attending health facilities in central Ethiopia. Cancer Control. 2022;29:10732748221076680.10.1177/10732748221076680Suche in Google Scholar PubMed PubMed Central
[28] Adams T, Denny L. Abnormal vaginal bleeding in women with gynaecological malignancies. Best Pract Res Clin Obstet Gynaecol. 2017;40:134–47.10.1016/j.bpobgyn.2016.09.014Suche in Google Scholar PubMed
[29] Nkonge NG, Ng’ang’a A, Nyangasi G, Gathitu E, Kibachio J, Gichangi P, et al. Predictors of cervical cancer screening among Kenyan women: Results of a nested case-control study in a nationally representative survey. BMC Public Health. 2018 Nov;18(Suppl 3):1221.10.1186/s12889-018-6054-9Suche in Google Scholar PubMed PubMed Central
[30] Kenya National Bureau of Statistics (KNBS). Kenya demographic and health survey 2022: Key indicators report. Nairobi, Kenya: KNBS; 2023.Suche in Google Scholar
[31] Mutisya R, Wambua BK. Influence of interpersonal communication on cervical cancer screening among women attending Moi Teaching and Referral Hospital, Kenya. Afr J Empir Res. 2023;4(2):71–84. https://www.ajol.info/index.php/ajempr/article/view/259885.10.51867/ajernet.4.2.126Suche in Google Scholar
© 2025 the author(s), published by De Gruyter
This work is licensed under the Creative Commons Attribution 4.0 International License.
Artikel in diesem Heft
- Research Articles
- Relationship between body mass index and quality of life, use of dietary and physical activity self-management strategies, and mental health in individuals with polycystic ovary syndrome
- Evaluating the challenges and opportunities for diabetes care policy in Nigeria
- Body mass index is associated with subjective workload and REM sleep timing in young healthy adults
- Prediction of hypoglycaemia in subjects with type 1 diabetes during physical activity
- Investigation by the Epworth Sleepiness Scale of daytime sleepiness in professional drivers during work hours
- Understanding public awareness of fall epidemiology in the United States: A national cross-sectional study
- Impact of Covid-19 stress on urban poor in Sylhet Division, Bangladesh: A perception-based assessment
- Impact of the COVID-19 pandemic on mental health, relationship satisfaction, and socioeconomic status: United States
- Psychological factors influencing oocyte donation: A study of Indian donors
- Cervical cancer in eastern Kenya (2018–2020): Impact of awareness and risk perception on screening practices
- Older LGBTQ+ and blockchain in healthcare: A value sensitive design perspective
- Trends and disparities in HPV vaccination among U.S. adolescents, 2018–2023
- Do cell towers help increase vaccine uptake? Evidence from Côte d’Ivoire
- In search of the world’s most popular painkiller: An infodemiological analysis of Google Trend statistics from 2004 to 2023
- Brain fog in chronic pain: A concept analysis of social media postings
- Association between multidimensional poverty intensity and maternal mortality ratio in Madagascar: Analysis of regional disparities
- A “disorder that exacerbates all other crises” or “a word we use to shut you up”? A critical policy analysis of NGOs’ discourses on COVID-19 misinformation
- Smartphone use and stroop performance in a university workforce: A survey-experiment
- Review Articles
- The management of body dysmorphic disorder in adolescents: A systematic literature review
- Navigating challenges and maximizing potential: Handling complications and constraints in minimally invasive surgery
- Examining the scarcity of oncology healthcare providers in cancer management: A case study of the Eastern Cape Province, South Africa
- Dietary strategies for irritable bowel syndrome: A narrative review of effectiveness, emerging dietary trends, and global variability
- The impact of intimate partner violence on victims’ work, health, and wellbeing in OECD countries (2014–2025): A descriptive systematic review
- Nutrition literacy in pregnant women: a systematic review
- Short Communications
- Experience of patients in Germany with the post-COVID-19 vaccination syndrome
- Five linguistic misrepresentations of Huntington’s disease
- Letter to the Editor
- PCOS self-management challenges transcend BMI: A call for equitable support strategies
Artikel in diesem Heft
- Research Articles
- Relationship between body mass index and quality of life, use of dietary and physical activity self-management strategies, and mental health in individuals with polycystic ovary syndrome
- Evaluating the challenges and opportunities for diabetes care policy in Nigeria
- Body mass index is associated with subjective workload and REM sleep timing in young healthy adults
- Prediction of hypoglycaemia in subjects with type 1 diabetes during physical activity
- Investigation by the Epworth Sleepiness Scale of daytime sleepiness in professional drivers during work hours
- Understanding public awareness of fall epidemiology in the United States: A national cross-sectional study
- Impact of Covid-19 stress on urban poor in Sylhet Division, Bangladesh: A perception-based assessment
- Impact of the COVID-19 pandemic on mental health, relationship satisfaction, and socioeconomic status: United States
- Psychological factors influencing oocyte donation: A study of Indian donors
- Cervical cancer in eastern Kenya (2018–2020): Impact of awareness and risk perception on screening practices
- Older LGBTQ+ and blockchain in healthcare: A value sensitive design perspective
- Trends and disparities in HPV vaccination among U.S. adolescents, 2018–2023
- Do cell towers help increase vaccine uptake? Evidence from Côte d’Ivoire
- In search of the world’s most popular painkiller: An infodemiological analysis of Google Trend statistics from 2004 to 2023
- Brain fog in chronic pain: A concept analysis of social media postings
- Association between multidimensional poverty intensity and maternal mortality ratio in Madagascar: Analysis of regional disparities
- A “disorder that exacerbates all other crises” or “a word we use to shut you up”? A critical policy analysis of NGOs’ discourses on COVID-19 misinformation
- Smartphone use and stroop performance in a university workforce: A survey-experiment
- Review Articles
- The management of body dysmorphic disorder in adolescents: A systematic literature review
- Navigating challenges and maximizing potential: Handling complications and constraints in minimally invasive surgery
- Examining the scarcity of oncology healthcare providers in cancer management: A case study of the Eastern Cape Province, South Africa
- Dietary strategies for irritable bowel syndrome: A narrative review of effectiveness, emerging dietary trends, and global variability
- The impact of intimate partner violence on victims’ work, health, and wellbeing in OECD countries (2014–2025): A descriptive systematic review
- Nutrition literacy in pregnant women: a systematic review
- Short Communications
- Experience of patients in Germany with the post-COVID-19 vaccination syndrome
- Five linguistic misrepresentations of Huntington’s disease
- Letter to the Editor
- PCOS self-management challenges transcend BMI: A call for equitable support strategies


