Abstract
Background and objectives
Falls are a leading cause of death and disability for adults aged 65 and older, despite the availability of evidence-based interventions to decrease fall risk. We sought to assess public awareness of falls in the United States (US), including when falls are most likely to occur.
Methods
An online survey was distributed to US adults aged 18 or older.
Results
A total of 1,069 individuals agreed to be contacted for the study, and 966 (90.4%) of them participated in the study. The largest proportion of participants believed that falls are most likely to occur at night (41.2%). Most of the participants correctly identified falls as preventable (97.9%) and recognized homes as the primary location (94.8%). Participants understood the increased risk of subsequent falls after a single fall (97.4%) and the low rate of informing doctors after a fall (82.9%). However, many were unaware that falls are not a normal part of aging (58.8%), one in four older adults fall annually (58.0%), most falls do not cause injury (60.8%), or that $50 billion is the annual cost of falls (96.3%).
Conclusions
This study reveals gaps in public awareness of fall epidemiology and severity among older adults. Contrary to common belief, falls occur predominantly during morning and afternoon hours, not in the evening or at night. While most respondents correctly identified falls as preventable, many erroneously considered them an inevitable consequence of aging. Additionally, the actual medical costs of falls far exceed public estimates. These findings underscore the need for targeted public health interventions to address misconceptions and enhance the awareness of fall risks and prevention strategies.
1 Introduction
Falls are a leading cause of injury and mortality in the United States (US), resulting in $50 billion in medical costs annually [1,2]. Despite extensive research, community programs, and government-funded initiatives to focus on fall prevention, falls have risen from 24th to the 15th leading cause of US disability-adjusted life years (DALYs) between 1990 and 2010, with fall death rates among older adults increasing by 30% between 2007 and 2016 [3,4,5]. While evidence-based fall prevention strategies exist, ranging from exercise-based programs to home modifications, and often accessible at no cost to the recipient, their adoption rates remain low [6,7,8]. Education effectively reduces fall risk, yet the gap between available prevention resources and their utilization suggests a potential disconnect in public awareness [1,9]. Currently, no studies have assessed the American public’s baseline awareness of fall epidemiology, limiting the ability to develop targeted educational interventions. This study addresses this critical knowledge gap by evaluating US adults’ awareness of falls, which could inform more effective public health messaging and ultimately improve prevention strategy adoption.
2 Methods
This cross-sectional study utilized a convenience sample recruited through ResearchMatch, a secure NIH-sponsored volunteer registry that includes individuals of all ages and backgrounds from across the US. A sample size was calculated using the formula for cross-sectional studies with categorical outcomes, assuming a 50% response distribution, 95% confidence level, and 5% margin of error, which indicated a minimum required sample of 385 participants. Adults aged 18 and older, residing in the US, and able to comprehend English were eligible to participate. Individuals on the registry who met inclusion criteria were routed a message with a brief description of the study and an option to participate. Those who opted in were sent a link to an online survey. The survey instrument developed for this pilot study consisted of three components: sociodemographic characteristics (sex, age, race, education, employment, household income, marital status, and state of residence), personal connections to fall-related injuries (family member, extended family member, friend, co-worker, acquaintance, or none), and knowledge of fall epidemiology. The knowledge assessment included multiple choice and true/false questions adapted from the CDC’s publicly available fact sheet on older adult fall prevention, supplemented with questions about fall timing based on recent literature [1,10]. Face validation was conducted with three subject matter experts in fall epidemiology who reviewed the survey for clarity, relevance, and alignment with the CDC content. The survey was refined based on expert feedback to improve comprehensibility before final administration via REDCap, with an approximate completion time of five minutes.
2.1 Analytic strategy
Participants with incomplete surveys were removed from the data set, and the epidemiology answers were coded into dichotomous variables (1 = correct, 0 = incorrect) and summarized as percentages. Participant-reported states of residence were grouped according to US Census Regions and Divisions of the United States [11]. Descriptive statistics were used to summarize the study outcomes. SPSS version 28 released in 2021 (IBM, Chicago, IL) was used to perform analysis.
-
Informed consent: All participants in this study provided informed consent prior to participation.
-
Ethics approval: This study was determined exempt from review by the Institutional Review Board at The Ohio State University in accordance with qualifying exempt category 2A.
3 Results
The survey had 1,069 respondents, and 966 (90.4%) completed the survey. Participant demographics are presented in Table 1.
Demographics of survey participants
| Variable | Number (%) |
|---|---|
| Age | |
| 18–25 | 83 (8.6) |
| 26–34 | 189 (19.6) |
| 35–44 | 157 (16.3) |
| 45–54 | 145 (15.0) |
| 55–64 | 164 (17.0) |
| 65–74 | 155 (16.0) |
| 75–91 | 73 (7.6) |
| Sex | |
| Female | 728 (75.4) |
| Male | 238 (24.6) |
| Race | |
| American Indian/Alaska Native | 4 (0.4) |
| Asian | 31 (3.2) |
| Black or African American | 55 (5.7) |
| White | 830 (85.9) |
| More than one race | 46 (4.8) |
| Household income | |
| <$25,000 | 111 (11.5) |
| $25,000–$49,999 | 184 (19.0) |
| $50,000–$74,999 | 179 (18.5) |
| $75,000–$100,000 | 165 (17.1) |
| $100,000–$250,000 | 282 (29.2) |
| >$250,000 | 45 (4.7) |
| Level of education | |
| High school graduate or equivalent | 47 (4.9) |
| Some college or associate degree | 214 (22.2) |
| Bachelor’s degree | 322 (33.3) |
| Graduate or professional degree | 383 (39.6) |
| Region of residence | |
| Northeast | 153 (15.8) |
| Midwest | 273 (28.6) |
| South | 342 (35.4) |
| West | 195 (20.2) |
| Number of individuals who did not know someone who has fallen | N = 966 (% within age range) |
| 18–25 | 8 (9.6) |
| 26–34 | 34 (18.0) |
| 35–44 | 25 (15.9) |
| 45–54 | 17 (11.7) |
| 55–64 | 16 (9.8) |
| 65–74 | 23 (14.8) |
| 75–91 | 5 (6.9) |
3.1 Personal experience with falls
The majority of participants (86.8%) knew someone who had been injured by a fall. The 26–34 age group had the largest proportion of individuals (18.0%) who did not personally know someone who had experienced a fall-related injury.
3.2 Fall epidemiology awareness
Participant responses to fall epidemiology questions varied considerably (Table 2). High awareness was demonstrated for falls being preventable (97.9% correct), falls most likely occurring at home (94.8% correct), and the rate of reporting falls to doctors (82.9% correct). However, significant knowledge gaps were identified in fall frequency, economic impact, fall outcomes, and fall normalcy. Most participants (53.9%) severely underestimated fall rates, believing falls occurred in only 1 in 100 or fewer older adults (1 in 100: 30.7%, 1 in 1,000: 18.2%, and 1 in 10,000: 5.0%), compared to the actual rate of 1 in 4. Additionally, 54.8% of the respondents estimated the annual medical costs of falls at $100–$500 million, representing just 0.2–1% of the actual $50 billion cost. A majority (60.8%) also incorrectly believed that most falls result in an injury and 58.8% incorrectly believed that falls are a normal part of aging.
Responses to fall fact questions
| Fall fact statement | Question format | Correct answer | Correct response (%) |
|---|---|---|---|
| Falls are a normal part of aging | True/False | False | 41.2 |
| Falls can be prevented | True/False | True | 97.9 |
| _____ older adults fall each year in the United States | Multiple choice | 1 in 4 | 42.0 |
| When an older adult falls, _____ older adults tell their doctor | Multiple choice | Less than half | 82.9 |
| Medical costs for falls in the United States are _____ each year | Multiple choice | $50 billion | 3.7 |
| Falls are most likely to happen at home | True/False | True | 94.8 |
| Most falls do not result in injury | True/False | True | 39.2 |
| Having a single fall increases your risk for another fall | True/False | True | 97.4 |
3.3 Timing of falls
Most participants believed falls and fall-related injuries were most likely to occur at night and least likely to occur during the afternoon (Figures 1 and 2).
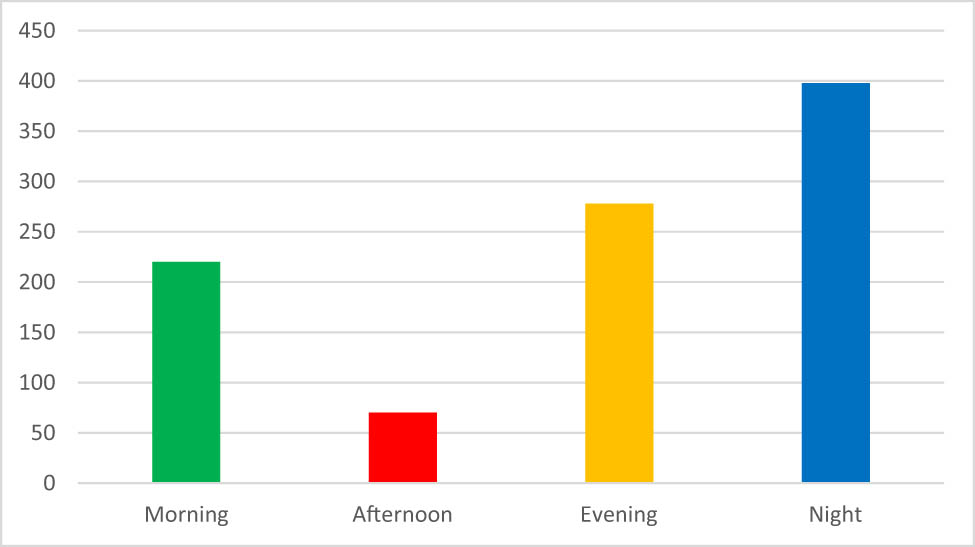
Time of day participants thought falls most likely to occur.
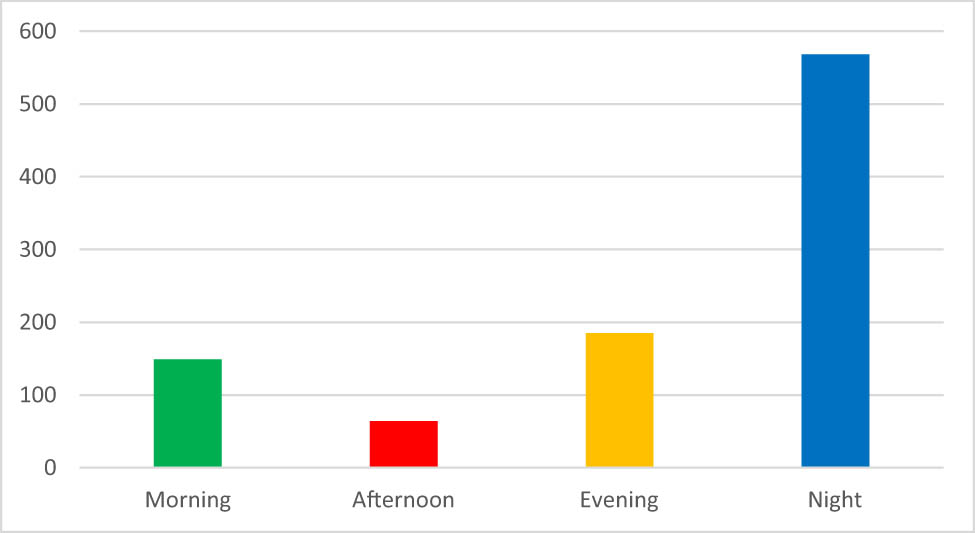
Time of day participants thought an injury from a fall was most likely to occur.
4 Discussion
Our survey captured perspectives from a demographically diverse sample across the US, with respondents spanning ages 18–91, though notably skewed toward higher education and income levels. Most respondents (86.8%) knew someone who had been injured by a fall, emphasizing the broad impact of falls [12]. Interestingly, younger adults aged 26–34 were least likely to have personal connections to fall-related injuries, suggesting potential gaps in fall awareness among this demographic.
Regarding fall epidemiology awareness, our findings reveal concerning knowledge gaps despite high recognition of falls being preventable (97.9%) and primarily occurring at home (94.8%). Only half of the CDC-sourced facts were answered correctly by the majority of participants. The questions that most participants missed were related to the severity of falls, including the rate, costs, and likelihood of injury. Worryingly, most participants believed that falls are a normal part of aging. This misconception not only poses a significant barrier to effective prevention strategies but may also reflect underlying ageist attitudes in society. Ageism refers to cognitive biases (e.g., stereotypes and prejudice) and the resulting behavior toward oneself or others on the basis of age [13]. Falls are frequently the focus of prevention for older adults, yet a recent study found that of the annual 9.9 million fall-related injuries in the US, incidence was fairly evenly distributed among older adults (32.3%), middle-aged adults (35.3%), and younger adults (32.3%) [12]. Furthermore, this perspective fails to take into account the fact that falls are preventable, which a notable majority of the survey respondents understood. It is imperative to correct inaccurate views of aging not only for the sake of older adults but also to improve the quality of life for young and middle-aged adults in the present and future [13,14].
The economic impact of ineffective fall prevention strategies in the US was also severely underestimated by participants. Over half of the respondents (54.8%) estimated annual medical costs at $100–500 million, representing only 1% or less of the actual cost of nonfatal falls in the US, which is about $50 billion. Medicare and Medicaid are responsible for over 75% of these costs ($28.9 billion and $8.7 billion, respectively), highlighting a financial impact that extends beyond individuals to their greater community [2]. Targeting falls prevention activities may, therefore, also result in alleviation of a significant financial burden on healthcare resources.
Regarding fall timing, participants demonstrated a striking misalignment between perception and reality. Participants had consensus on the timing of falls, with night being considered the time of day that people are both most likely to fall and most likely to be injured from a fall, and the afternoon being the time of day that people are least likely to fall or be injured from a fall. It feels intuitive that nights would have the highest risk of accidental falls and injuries, since in many contexts, nighttime activity results in increased risk of injury [15,16]. However, most falls happen during the daytime [10]. One study found only 13.1% of falls happen between 6pm and 6am, and most falls occurred during the morning (33.5%) and afternoon (50.5%) hours [17]. This is likely due to people being less active in the evening and nighttime hours.
Healthcare providers play a pivotal role in bridging these knowledge gaps, yet less than half of older adults tell their doctor about falls, suggesting a critical missed opportunity for intervention [9,18]. This communication barrier, combined with the public’s misconceptions about fall timing and preventability, indicates a need for proactive screening and education by healthcare providers. Additionally, the widespread underestimation of fall frequency and costs suggests an opportunity to leverage social media and targeted public health messaging to reach younger demographics before they or their loved ones experience falls.
Increased awareness is an important initial step to preventing falls and may yield sustained behavior change [19]. By improving the public understanding of fall epidemiology, dispelling myths about aging, and highlighting the economic impact of falls, a more receptive environment for implementing prevention measures may be developed. This increased awareness can encourage individuals to seek out and engage with available resources and interventions.
While our study is the first to examine fall awareness in a US population, similar investigations have been conducted internationally, revealing both common themes and notable variations. Uniquely, our study recruited adults of all ages regardless of fall history, while previous studies focused exclusively on older adults. Across studies, recognition of fall preventability was consistently high – 97.9% in our US sample, 81.4% in a Saudi Arabian study by Almesned and Jahan and 89% (combined agreed/somewhat agreed) in a Canadian study by Russell et al. [20,21]. Malaysian research by Goh et al., also focused on older adults, found that non-fallers demonstrated higher fall prevention knowledge compared to those with a history of falls, suggesting that knowledge acquisition may occur too late for some older adults [22]. The variation in findings across studies suggests that population and region-specific awareness campaigns may be necessary for maximum effectiveness. Further research is needed across all regions to identify these specific knowledge gaps and determine the most effective methods for disseminating fall prevention information to diverse populations.
5 Limitations
This study is subject to several limitations. First, the times of day were defined generally, so there may have been variations in interpretation of the terms (i.e., morning, afternoon, and evening). Second, the sample featured a large representation of individuals with graduate or professional degrees and high annual household incomes. These adults are in higher proportion on the research volunteer registry than in the general population.
6 Conclusions
This study unveils a disparity between public perception and the reality of fall epidemiology among US adults. Alarmingly, the majority incorrectly believe that falls are a normal part of aging – a misconception that poses significant barrier to effective prevention strategies. This belief, coupled with limited awareness of fall timing and impact, underscores a pressing public health concern. There is also a widespread lack of awareness of the substantial financial burden falls impose on both individuals and taxpayers. Despite this, there is a promising recognition that falls are preventable. Overall, the study findings highlight a pressing need for targeted educational initiatives to bridge the gap between existing fall prevention evidence and public awareness.
Acknowledgements
Recruitment for the study was done via ResearchMatch, a national health volunteer registry that was created by several academic institutions and supported by the US National Institutes of Health as part of the Clinical Translational Science Award (CTSA) program. ResearchMatch has a large population of volunteers who have consented to be contacted by researchers about health studies for which they may be eligible. Review and exemption determination for this study and all procedures was obtained from The Ohio State University Biomedical Review Board.
-
Funding information: This article was funded by National Institute on Aging, award number K76AG068435.
-
Author contributions: All authors accept responsibility for the content of the manuscript and consented to its submission. All authors reviewed the results and approved the final version of the manuscript. ES and JMW developed the research project. ES conducted data analysis and JMW created the manuscript draft. CEQ contributed to the research idea, and all authors participated in editing the manuscript in preparation for publication.
-
Conflict of interest: The authors state no conflicts of interest.
-
Data availability statement: Data from this study are not publicly available.
References
[1] Centers for Disease Control and Prevention. Facts about Falls. 2024; https://www.cdc.gov/falls/data-research/facts-stats/index.html. Accessed 08/12/2024.Suche in Google Scholar
[2] Florence CS, Bergen G, Atherly A, Burns E, Stevens J, Drake C. Medical costs of fatal and nonfatal falls in older adults. J Am Geriatr Soc. 2018;66(4):693–8.10.1111/jgs.15304Suche in Google Scholar PubMed PubMed Central
[3] Grossman DC, Curry SJ, Owens DK, Barry MJ, Caughey AB, Davidson KW, et al. Interventions to prevent falls in community-dwelling older adults: US preventive services task force recommendation statement. JAMA. 2018;319(16):1696–704.10.1001/jama.2018.3097Suche in Google Scholar PubMed
[4] World Health Organization. Health promotion and disease prevention through population-based interventions, including action to address social determinants and health inequity. 2017. https://www.emro.who.int/about-who/public-health-functions/health-promotion-disease-prevention.html. Accessed 08/12/2024.Suche in Google Scholar
[5] Murray CJ, Atkinson C, Bhalla K, Birbeck G, Burstein R, Chou D, et al. The state of US health, 1990-2010: burden of diseases, injuries, and risk factors. JAMA. 2013;310(6):591–608.10.1001/jama.2013.13805Suche in Google Scholar PubMed PubMed Central
[6] Burns E, Kakara R, Moreland BA. CDC compendium of effective fall interventions: what works for community-dwelling older adults. Atlanta, GA: Centers for Disease Control and Prevention; 2023.Suche in Google Scholar
[7] Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012;2012(9):Cd007146.10.1002/14651858.CD007146.pub3Suche in Google Scholar PubMed PubMed Central
[8] Szanton SL, Thorpe RJ, Boyd C, Tanner EK, Leff B, Agree E, et al. Community aging in place, advancing better living for elders: a bio-behavioral-environmental intervention to improve function and health-related quality of life in disabled older adults. J Am Geriatr Soc. 2011;59(12):2314–20.10.1111/j.1532-5415.2011.03698.xSuche in Google Scholar PubMed PubMed Central
[9] Ong MF, Soh KL, Saimon R, Wai MW, Mortell M, Soh KG. Fall prevention education to reduce fall risk among community-dwelling older persons: A systematic review. J Nurs Manag. 2021;29(8):2674–88.10.1111/jonm.13434Suche in Google Scholar PubMed PubMed Central
[10] Sheridan E, Wiseman JM, Quatman CE. Timing of emergency medical services activations for falls. Archives of Gerontology and Geriatrics Plus. Vol. 1, 2024. https://www.sciencedirect.com/science/article/pii/S2950307824000171.10.1016/j.aggp.2024.100020Suche in Google Scholar PubMed PubMed Central
[11] U.S. Census Bureau. Census regions and divisions of the United States. https://www2.census.gov/geo/pdfs/maps-data/maps/reference/us_regdiv.pdf. Accessed 08/12/2024.Suche in Google Scholar
[12] Verma SK, Willetts JL, Corns HL, Marucci-Wellman HR, Lombardi DA, Courtney TK. Falls and fall-related injuries among community-dwelling adults in the United States. PLoS One. 2016;11(3):e0150939.10.1371/journal.pone.0150939Suche in Google Scholar PubMed PubMed Central
[13] World Health Organization. Ageing: Ageism. 2021; https://www.who.int/news-room/questions-and-answers/item/ageing-ageism. Accessed 08/12/2024.Suche in Google Scholar
[14] Allen JO, Solway E, Kirch M, Singer D, Kullgren JT, Moïse V, et al. Experiences of everyday ageism and the health of older US adults. JAMA Netw Open. 2022;5(6):e2217240.10.1001/jamanetworkopen.2022.17240Suche in Google Scholar PubMed PubMed Central
[15] Calabrese C, Mejia B, McInnis CA, France M, Nadler E, Raslear TG. Time of day effects on railroad roadway worker injury risk. J Saf Res. 2017;61:53–64.10.1016/j.jsr.2017.02.007Suche in Google Scholar PubMed
[16] Mustard CA, Chambers A, McLeod C, Bielecky A, Smith PM. Work injury risk by time of day in two population-based data sources. Occup Environ Med. 2013;70(1):49–56.10.1136/oemed-2012-100920Suche in Google Scholar PubMed PubMed Central
[17] Kim M, Chang M, Nam E, Kim SG, Cho SI, Ryu DH, et al. Fall characteristics among elderly populations in urban and rural areas in Korea. Medicine (Baltimore). 2020;99(46):e23106.10.1097/MD.0000000000023106Suche in Google Scholar PubMed PubMed Central
[18] Goodwin V, Jones-Hughes T, Thompson-Coon J, Boddy K, Stein K. Implementing the evidence for preventing falls among community-dwelling older people: A systematic review. J Saf Res. 2011;42(6):443–51.10.1016/j.jsr.2011.07.008Suche in Google Scholar PubMed
[19] Ludwig VU, Brown KW, Brewer JA. Self-regulation without force: Can awareness leverage reward to drive behavior change? Perspect Psychol Sci. 2020;15(6):1382–99.10.1177/1745691620931460Suche in Google Scholar PubMed
[20] Almesned RA, Jahan S. Awareness about fall risk and measures of fall prevention among older adults in Buraidah, Saudi Arabia. Cureus. 2024;16(6):e63328.10.7759/cureus.63328Suche in Google Scholar PubMed PubMed Central
[21] Russell K, Taing D, Roy J. Measurement of fall prevention awareness and behaviours among older adults at home. Can J Aging = La Rev Canadienne du Vieillissement. 2017;36(4):522–35.10.1017/S0714980817000332Suche in Google Scholar PubMed PubMed Central
[22] Goh JW, Singh DKA, Mesbah N, Hanafi AAM, Azwan AF. Fall awareness behaviour and its associated factors among community dwelling older adults. BMC Geriatr. 2021;21(1):226.10.1186/s12877-021-02122-zSuche in Google Scholar PubMed PubMed Central
© 2025 the author(s), published by De Gruyter
This work is licensed under the Creative Commons Attribution 4.0 International License.
Artikel in diesem Heft
- Research Articles
- Relationship between body mass index and quality of life, use of dietary and physical activity self-management strategies, and mental health in individuals with polycystic ovary syndrome
- Evaluating the challenges and opportunities for diabetes care policy in Nigeria
- Body mass index is associated with subjective workload and REM sleep timing in young healthy adults
- Prediction of hypoglycaemia in subjects with type 1 diabetes during physical activity
- Investigation by the Epworth Sleepiness Scale of daytime sleepiness in professional drivers during work hours
- Understanding public awareness of fall epidemiology in the United States: A national cross-sectional study
- Impact of Covid-19 stress on urban poor in Sylhet Division, Bangladesh: A perception-based assessment
- Impact of the COVID-19 pandemic on mental health, relationship satisfaction, and socioeconomic status: United States
- Psychological factors influencing oocyte donation: A study of Indian donors
- Cervical cancer in eastern Kenya (2018–2020): Impact of awareness and risk perception on screening practices
- Older LGBTQ+ and blockchain in healthcare: A value sensitive design perspective
- Trends and disparities in HPV vaccination among U.S. adolescents, 2018–2023
- Do cell towers help increase vaccine uptake? Evidence from Côte d’Ivoire
- In search of the world’s most popular painkiller: An infodemiological analysis of Google Trend statistics from 2004 to 2023
- Brain fog in chronic pain: A concept analysis of social media postings
- Association between multidimensional poverty intensity and maternal mortality ratio in Madagascar: Analysis of regional disparities
- A “disorder that exacerbates all other crises” or “a word we use to shut you up”? A critical policy analysis of NGOs’ discourses on COVID-19 misinformation
- Smartphone use and stroop performance in a university workforce: A survey-experiment
- Review Articles
- The management of body dysmorphic disorder in adolescents: A systematic literature review
- Navigating challenges and maximizing potential: Handling complications and constraints in minimally invasive surgery
- Examining the scarcity of oncology healthcare providers in cancer management: A case study of the Eastern Cape Province, South Africa
- Dietary strategies for irritable bowel syndrome: A narrative review of effectiveness, emerging dietary trends, and global variability
- The impact of intimate partner violence on victims’ work, health, and wellbeing in OECD countries (2014–2025): A descriptive systematic review
- Nutrition literacy in pregnant women: a systematic review
- Short Communications
- Experience of patients in Germany with the post-COVID-19 vaccination syndrome
- Five linguistic misrepresentations of Huntington’s disease
- Letter to the Editor
- PCOS self-management challenges transcend BMI: A call for equitable support strategies
Artikel in diesem Heft
- Research Articles
- Relationship between body mass index and quality of life, use of dietary and physical activity self-management strategies, and mental health in individuals with polycystic ovary syndrome
- Evaluating the challenges and opportunities for diabetes care policy in Nigeria
- Body mass index is associated with subjective workload and REM sleep timing in young healthy adults
- Prediction of hypoglycaemia in subjects with type 1 diabetes during physical activity
- Investigation by the Epworth Sleepiness Scale of daytime sleepiness in professional drivers during work hours
- Understanding public awareness of fall epidemiology in the United States: A national cross-sectional study
- Impact of Covid-19 stress on urban poor in Sylhet Division, Bangladesh: A perception-based assessment
- Impact of the COVID-19 pandemic on mental health, relationship satisfaction, and socioeconomic status: United States
- Psychological factors influencing oocyte donation: A study of Indian donors
- Cervical cancer in eastern Kenya (2018–2020): Impact of awareness and risk perception on screening practices
- Older LGBTQ+ and blockchain in healthcare: A value sensitive design perspective
- Trends and disparities in HPV vaccination among U.S. adolescents, 2018–2023
- Do cell towers help increase vaccine uptake? Evidence from Côte d’Ivoire
- In search of the world’s most popular painkiller: An infodemiological analysis of Google Trend statistics from 2004 to 2023
- Brain fog in chronic pain: A concept analysis of social media postings
- Association between multidimensional poverty intensity and maternal mortality ratio in Madagascar: Analysis of regional disparities
- A “disorder that exacerbates all other crises” or “a word we use to shut you up”? A critical policy analysis of NGOs’ discourses on COVID-19 misinformation
- Smartphone use and stroop performance in a university workforce: A survey-experiment
- Review Articles
- The management of body dysmorphic disorder in adolescents: A systematic literature review
- Navigating challenges and maximizing potential: Handling complications and constraints in minimally invasive surgery
- Examining the scarcity of oncology healthcare providers in cancer management: A case study of the Eastern Cape Province, South Africa
- Dietary strategies for irritable bowel syndrome: A narrative review of effectiveness, emerging dietary trends, and global variability
- The impact of intimate partner violence on victims’ work, health, and wellbeing in OECD countries (2014–2025): A descriptive systematic review
- Nutrition literacy in pregnant women: a systematic review
- Short Communications
- Experience of patients in Germany with the post-COVID-19 vaccination syndrome
- Five linguistic misrepresentations of Huntington’s disease
- Letter to the Editor
- PCOS self-management challenges transcend BMI: A call for equitable support strategies


