Clinical implications of fear extinction in anxiety disorders
-
Armin Zlomuzica
, Silvia Schneider
, Carolin Konrad
, Oliver T. Wolf
, Friederike Raeder
Abstract
Anxiety disorders (ADs) are characterized by increased chronicity and comorbidity with other ADs. Although exposure is the most effective therapy option for ADs, some patients show poor treatment response and a heightened vulnerability for relapse after treatment completion. Hence, significant research effort needs to be devoted to improve the long-term effectiveness of exposure effects. Recent attempts to increase exposure therapy efficacy use strategies aimed at promoting the acquisition and retrieval of extinction memories. The present review illustrates the value and limitations of such extinction-based therapy approaches. We present and discuss recent findings from translational studies using cortisol and self-efficacy enhancement as an add-on to exposure therapy. We illustrate how the integration of findings from experimental research on fear extinction learning and self-efficacy could advance the development of more optimized treatments for ADs.
Zusammenfassung
Angststörungen zeichnen sich durch eine erhöhte Chronizität und Komorbidität mit anderen Angststörungen aus. Obwohl die Exposition eine effektive Therapieoption für Angststörungen darstellt, profitieren einige Patienten nicht von dieser Intervention und/oder zeigen eine erhöhte Anfälligkeit für Rückfälle nach The-rapieabschluss. Es gibt daher zunehmend Forschungsbedarf zur Verbesserung der Langzeiteffektivität von Exposition. Kürzliche Ansätze zur Erhöhung der Expositionsthe-rapieeffektivität beinhalten Strategien zur Verbesserung des Extinktionslernens. In dieser Übersichtsarbeit werden die Vorteile und Limitationen dieser extinktions-basierten Strategien näher beleuchtet. Wir präsentieren und diskutieren die neusten Befunde aus translationalen Studien zu Effekten von Cortisol und Erhöhung der Selbstwirksamkeits-erwartung als potenzielle Strategien zur Verbesserung der Expositionstherapieeffekte. Wir illustrieren wie die Integration der experimentellen Befunde zum Extinktionslernen und Selbstwirksamkeitserwartung die Entwicklung optimierter Therapien für Angststörungen vorantreiben kann.
Anxiety disorders (ADs) belong to the most prevalent mental disorders (Bandelow and Michaelis, 2015). Chronicity and comorbidities with other ADs affect the disease course of ADs (Bandelow and Michaelis, 2015). Cognitive behavioral therapy (CBT) is both highly efficient and effective in the treatment of ADs (Otte, 2011). CBT involves a set of cognitive and behavioral interventions such as exposure. Although exposure is the most effective therapeutic tool for ADs, some patients fail to exhibit significant symptom improvement or show recovery of fear and avoidance after completion of exposure (Hoffmann and Smits, 2008; Norton and Price, 2007). Current knowledge on the mechanisms governing the beneficial effects of exposure has been largely influenced by the general propositions of the inhibitory learning and inhibitory regulation models (Craske et al., 2006, 2008). Here, fear extinction is considered a central candidate to explain the beneficial effects of exposure as well as relapse phenomena after successful treatment (Craske and Mystkowski, 2006).
The association between fear extinction and exposure therapy
From an inhibitory learning perspective (Craske and Mystkowski, 2006, 2008), interindividual variability in exposure treatment outcome (Norton and Price, 2007) may be explained by the level of interindividual differences in fear extinction learning. In line with this idea, initial studies demonstrated that differences in extinction learning performance during a differential fear conditioning task were associated with variability in CBT outcomes in phobic children (Waters and Pine, 2016) and with the level of treatment gains during an exposure therapy analog in spider phobia (Forcadell et al., 2017). Likewise, anxiety reductions after exposure in patients with social anxiety could be predicted on the basis of extinction learning performance (Ball et al., 2017). Work from our group indicates that interindividual differences in fear extinction learning might also influence the patient’s general ability to complete an exposure task within one or two sessions (Raeder et al., 2020). We showed that spider-phobic participants who were able to complete exposure within two 60-min sessions (i.e., completers) exhibited more pronounced short- and long-term therapy benefit than non-completers. Most importantly, fear extinction performance is linked to the ability to complete the exposure. Completers showed more pronounced fear extinction (retrieval) relative to noncompleters. This finding indicates that one subgroup of patients with specific phobia (non-completers) failed to accomplish exposure in a predetermined time possibly owing to deficient fear extinction.
These results bear important implications for the implementation of exposure in routine care. The inability of some patients to accomplish exposure in a predetermined time might be at odds with the specific regularities of routine care (Gunther and Whittal, 2010). To conclude, research on fear extinction might not only explain the variability in exposure treatment efficacy across patients but also bear specific implications for the implementation of exposure to routine care (Richter et al., 2017).
Pharmacological enhancement of exposure therapy efficacy: lessons from studies using cortisol as an add-on to exposure therapy
Studying exposure treatment processes from the perspective of the fear extinction model might provide valuable information on how to optimize exposure treatment efficacy (Craske et al., 2018). A great number of studies showed alterations in fear acquisition (Mosig et al., 2014) and/or deficits in fear extinction in ADs (Lissek et al., 2005). Fortunately, research on cognitive and neurobiological mechanisms of extinction produced a great wealth of meaningful results on how fear extinction can be selectively enhanced (Craske et al., 2018). For instance, data from animal and human work suggest that stress and cortisol can modulate the acquisition, consolidation, and retrieval of extinction memories (de Quervain et al., 2017; Stockhorst and Antov, 2016). Accordingly, the translation of these findings to the context of exposure therapy has received great interest. Systemic administration of glucocorticoids (i.e., cortisol) before exposure has been shown to enhance the efficacy of exposure-based treatments (for a review, see de Quervain et al., 2017). However, possible timing-dependent effects of cortisol on exposure outcome have been neglected in clinical studies. This is surprising given that the effects of stress and cortisol on (extinction) memory processes are not ubiquitous but might depend on the exact timing of administration (Stockhorst and Antov, 2016). Likewise, existing clinical studies rarely considered the possible impact of cortisol on the generalization of therapy effects across contexts. Given the existence of context-specific effects of cortisol on fear extinction (Meir Drexler et al., 2019), cortisol might affect the generalization of exposure treatment effects from the treatment context to other unfamiliar contexts. In other words, owing to the impact of cortisol on context specificity of fear extinction, the pharmacological enhancement of exposure with cortisol can possibly aggravate or dampen the return of fear after successful treatment. In the therapy setting, return of fear can be observed when patients encounter their feared object in an unfamiliar context, for example, seeing a spider in the basement instead of the room in which the exposure therapy took place – termed as fear renewal (Craske and Mystkowski, 2006, 2008).
Raeder et al. (2019a) conducted the first study that examined the effect of cortisol on both exposure efficacy and fear renewal after exposure. We showed that the administration of cortisol after exposure did not enhance the efficacy of exposure therapy in spider phobia. We further observed a detrimental effect on context-dependent return of fear (fear renewal) in the long term in participants who received cortisol relative to placebo-treated participants. In light of previous clinical studies in this field (de Quervain et al., 2017), our findings indicate that cortisol may boost exposure therapy efficacy only when given before (rather than after) exposure. Furthermore, the exact timing of cortisol administration seems to be critical when attempting to increase the generalization of therapeutic effects across contexts (Meir Drexler et al., 2019). Accordingly, post-exposure administration of cortisol might be a less well-suited augmentation strategy because it may lead to an increase in fear renewal in the long term.
Exposure treatment efficacy: mediators and moderators
Some important mediators/moderators need to be taken into consideration when conducting clinical studies assessing the putative role of cognitive enhancers in exposure therapy. ADs are more frequent in women (Kessler et al., 2005). There is a gender-dependent effect in fear extinction (Merz et al., 2018). The sex hormone estrogen may affect the short- and long-term processing of extinction memories (Maeng and Milad, 2015). The use of oral contraceptives (OCs) affects endogenous estrogen secretion in women. Women using OCs show impaired fear extinction learning (Merz et al., 2012, 2018). Considering the influence of OC use and the variations in estrogen levels during the menstrual cycle in the context of exposure treatment in women might therefore be highly valuable. In support of this proposition, work from our laboratory (Raeder et al., 2019c) and that from others (Graham et al., 2018) indicate that hormonal contraceptive use in women has an impact on the immediate and long-term effects of exposure. Precisely, free-cycling women and women using hormonal contraceptives showed different response profiles to exposure therapy (Raeder et al., 2019c). Spider-phobic women using hormonal contraceptives exhibited less fear reduction and symptom improvement from pre-treatment to post-treatment and at six-week follow-up than their free-cycling counterparts.
The aforementioned findings suggest that the implementation of hormonal measurements and the systematic assessment of contraceptive use, which itself affects variability in exposure outcome, is important to derive a complete picture on the possible effects of cognitive enhancers in exposure therapy. This is especially true with regard to the effects of cortisol because OC use alters the effects of cortisol on fear learning (Merz et al., 2012, 2018). Interestingly, the Stress Timing affects Relapse (STAR) model has been proposed as a valuable framework to stimulate future clinical studies on the interaction between cortisol and sex hormones on extinction memories (Meir Drexler et al., 2019).
Exposure: is it more than fear extinction?
The rationale behind exposure therapy is to assist patients in overcoming their anxiety by creating a safe environment in which they encounter feared or avoided scenarios. Thus, a central goal of exposure is to induce positive mastery experiences that are ideally accompanied by substantial decrements of fear and avoidance in treated patients. According to Bandura (1988), positive mastery experiences lead to an increase in self-efficacy beliefs, which might constitute a prerequisite for a successful CBT. Several studies showed a positive association between increased self-efficacy and therapy outcome in patients with ADs (Bouchard et al., 2007; Gallagher et al., 2013). Given the mutual relationship between exposure and self-efficacy, the selective modulation of perceived self-efficacy might be effective to promote key processes (i.e., fear extinction learning) of exposure. In line with this, we showed that an increase in perceived self-efficacy (induced by false-positive verbal feedback) affects the acquisition and retrieval of extinction memories. Healthy participants with an increased self-efficacy showed better fear extinction learning and retrieval in a differential fear conditioning task (Zlomuzica et al., 2015).
Promoting self-efficacy might also represent an effective strategy to increase exposure efficacy. Raeder et al. (2019b) recently showed that increasing self-efficacy via the active rehearsal of personal mastery experiences is suitable to promote exposure outcome in patients with height phobia. In particular, self-efficacy enhancement led to more pronounced reductions in fear and avoidance after one session of standardized exposure in virtual reality (Raeder et al., 2019b). The mechanisms underlying the beneficial effect of an increased self-efficacy on fear extinction remain to be explored. Increased self-efficacy might lead to changes in the processing of extinguished memories (Zlomuzica et al., 2015). Alternatively, the utilization of positive personal experiences might affect the way how subjects perceive and cope with future challenges (Margraf and Zlomuzica, 2015; Zlomuzica et al., 2018). Since an adaptive processing of mastery experiences is fundamental to self-efficacy (Bandura, 1988), a better understanding of mechanisms underlying the storage and retrieval of personally relevant memories in patients with ADs would be highly valuable (Zlomuzica et al., 2014, 2016).
Generalization of exposure therapy effects
The comorbidity of ADs with other ADs is common (Bandelow and Michaelis, 2015). For instance, phobic individuals tend to suffer from multiple fears at the same time (Davey, 1991; Matchett and Davey, 1991). Individuals with fear of spiders tend to fear other similar insects (e.g., cockroaches) and/ or small animals (e.g., rats). Such multiple fears might even be functionally related and lead to an increase in psychopathological symptoms (Rachman and Lopatka, 1986a, b). Surprisingly, recommendations on how to systematically treat multiple fears and/or comorbid anxieties do not exist. Likewise, there is no therapeutic tool that can induce a generalization of therapeutic effects for different functionally related fears. Notwithstanding, we have recently shown that exposure might lead to a generalization of therapeutic effects to untreated fear stimuli.
In particular, Preusser et al. (2017) demonstrated that exposure-induced reduction in fear and avoidance can also be observed for untreated stimuli, that is, those that bear feature overlap with treated stimuli but do not belong to the same category of fear stimuli (Figure 1).
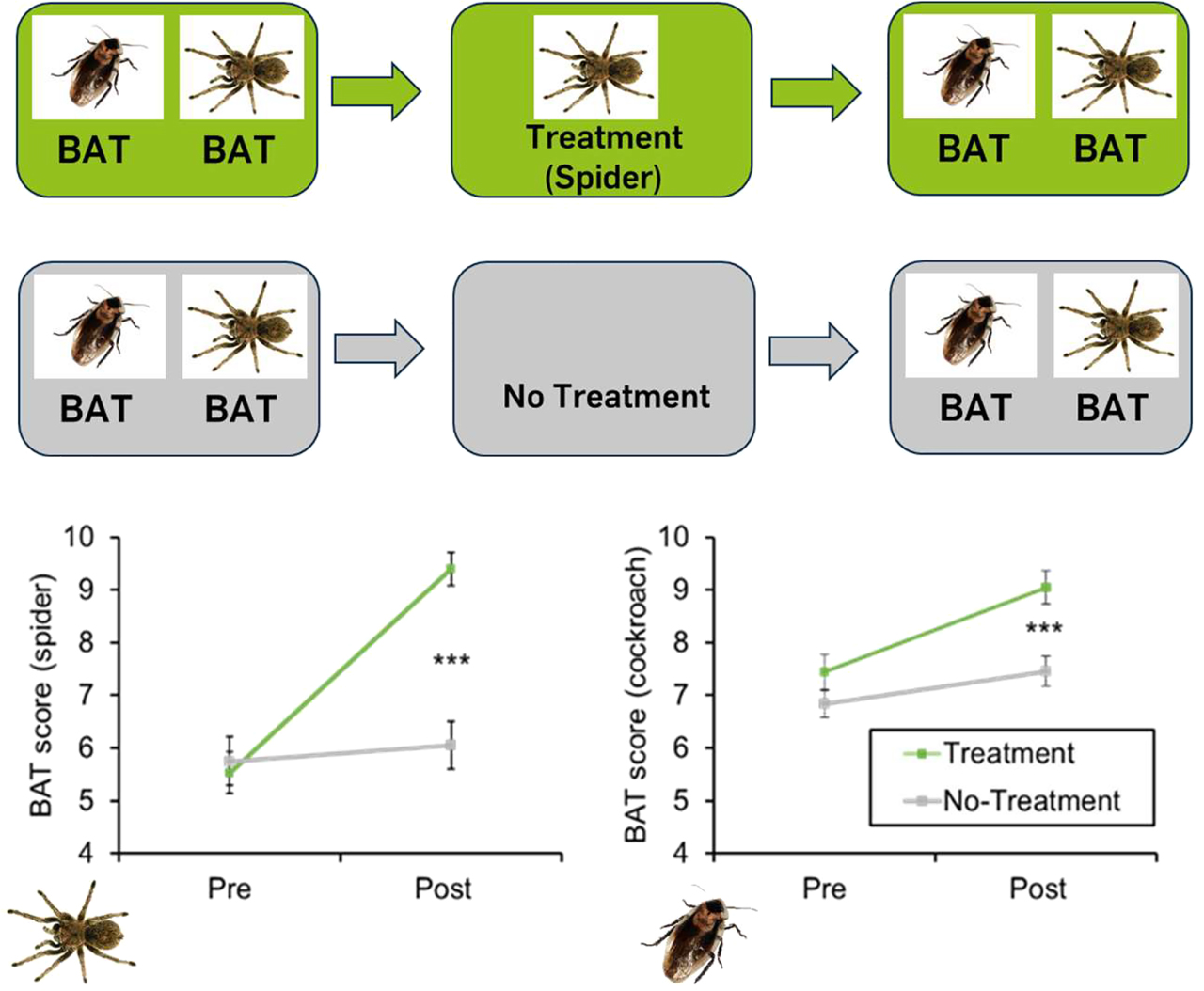
Participants with spider and cockroach phobia were subjected to exposure (Treatment) or a waiting control condition (No-Treatment). In addition to a Behavioral Approach Test (BAT) for spiders, the participants from both groups were subjected to a BAT for cockroaches before and after the assessment. Participants in the Treatment condition were subjected to a standardized in vivo exposure treatment for spider phobia. Cockroaches were not presented during the Treatment or No-Treatment condition. In contrast to the participants in the No-Treatment condition, those in the Treatment condition showed significantly less avoidance and fear during the BAT for spiders (left panel) and cockroaches (right panel).
These findings, which present to our knowledge the first study on this research gap, indicate that exposure effects are not restricted to the specific fear stimulus used during exposure (Preusser et al., 2017). Interestingly, such a generalization of clinical exposure treatment was recently also demonstrated in other fears (Hollander et al., 2020). How can we explain such generalization of exposure therapy effects? Findings from basic research on fear generalization (in particular, extinction generalization) (Dymond et al. 2015; Pittig et al., 2018) cannot fully account for the generalization of exposure effects to untreated fear stimuli. Alternatively, the self-efficacy concept of Bandura offers a more parsimonious account for the generalization of mastery experiences across different related (fear) domains (Bandura, 1988). Nevertheless, studying the generalization of therapeutic effects in ADs represents an important but neglected research field (Pittig et al., 2018).
Conclusions
Fear extinction might be a central candidate to explain exposure therapy benefit. The formation of personal mastery experiences during exposure leads to an increased self-efficacy, which might constitute another important element of a successful therapy for ADs. Attempts to promote fear extinction learning (e.g., via pharmacological modulation with cognitive enhancers) and to increase self-efficacy represent promising strategies to enhance exposure treatment efficacy and increase generalization of therapeutic effects.
Funding source: Deutsche Forschungsgemeinschaft
Award Identifier / Grant number: FOR 1581, SFB 1280
About the authors

Armin Zlomuzica is junior professor of “Behavioral and Clinical Neuroscience” at the Mental Health Research and Treatment Center (MHRTC) at the Ruhr University Bochum (RUB). He obtained his diploma in psychology and his PhD from the Heinrich-Heine University Düsseldorf. He further completed a postgradual training in cognitive behavioural therapy (CBT) at the Rheinish Academy of Behavioral Medicine and Psychotherapy. His research in the field of behavioural and clinical neuroscience includes studies on the behavioural and neurobiological basis of learning and memory, emotion and motivation. Another research focus is on the implementation of interventions grounded in basic research on memory, attention and cognitive bias to treat anxiety and addictive behaviors.

Silvia Schneider, Ph.D., is Professor of Clinical Child and Adolescent Psychology and Head of the Research and Treatment Centre for Mental Health at the Ruhr University Bochum (kkjp.rub.de/schneider). She studied psychology at the Universities of Mannheim and Marburg, and has been Professor of Clinical Child and Adolescent Psychology since 2004 (2004-2010 University of Basel). Her research focuses on anxiety disorders in childhood, regulatory disorders in infancy, familial transmission of emotional disorders, clinical-psychological diagnostics with children, adolescents and adults. Her research is supported by individual DFG projects as well as by collaborative and large-scale projects (BMBF collaborative projects, innovation fund project, DFG Graduate School Situated Cognition, SFB 1280 - Extinction Learning). She is spokesperson of the Division of Clinical Psychology and Psychotherapy of the German Society of Psychology (DGPs), member of the Research Council of the University Alliance Ruhr and the DGPs Commission Psychology and Psychotherapy as well as a member of various national and international boards of journals and research projects/institutions.

Carolin Konrad is a Post-Doctoral Researcher in the Department of Clinical Child and Adolescent Psychology at the Ruhr University Bochum. She received her diploma in psychology from the Westfälische-Wilhelms Universität Münster and her PhD from the Ruhr University Bochum. She worked as a research fellow at TU Dortmund University in the Department of Developmental Psychology. Her special interest is in factors influencing learning and memory in infancy and childhood and its clinical implications. Her latest focus is on extinction learning from infancy to adulthood.

Christian J. Merz is Principal Investigator and Assistant Professor in the Department of Cognitive Psychology at the Ruhr University Bochum. He received his diploma in psychology from the Justus Liebig University Giessen and his PhD and habilitation from the Ruhr University Bochum. He conducted his postdoctoral work in Giessen, Bochum and Trier, where he also was interim Professor for Biological and Clinical Psychology. His special interests concern the modulation of declarative and fear memories by stress and sex hormones and its clinical implications. In addition, he is involved in several meta-research projects in the field of fear conditioning.
Oliver T. Wolf is full Professor and head of the Department of Cognitive Psychology at the Ruhr University Bochum. He received his diploma in psychology from Trier University where he also conducted his PhD thesis. After a postdoc at Rockefeller University and New York University he moved to Heinrich-Heine University Düsseldorf where he obtained his habilitation. In 2005 he became full Professor at Bielefeld University before moving to Ruhr University Bochum in 2007. For more than 20 years he has investigated the impact of acute and chronic stress on cognitive processes taking a psychoneuroendocrine perspective. While his focus has been on learning and memory, additional processes of interest like decision making, social cognition and emotion regulation have emerged over the years.

Friederike Raeder is a postdoctoral researcher in the Department of Clinical Psychology and Psychotherapy at the Ruhr University Bochum. She obtained her master's degree in psychology from the Heinrich-Heine University Düsseldorf and her PhD from the Ruhr University Bochum. Her research revolves around learning and memory processes in both psychopathological conditions and their treatment, with a special focus on anxiety disorders. During her PhD, she addressed the clinical implications of extinction learning in specific phobia.

Jürgen Margraf studied psychology, sociology and physiology in Germany and Belgium. After a research scholarship in Psychiatry and Behavioral Sciences at Stanford University he completed his PhD at the University of Tübingen in 1986 and subsequently held professorships in Berlin, Dresden, Basel and Bochum. In 2009 he was the first psychologist to be awarded an Alexander von Humboldt-Professorship, Germany's most highly endowed scientific award. His work focuses on the interplay between psychological, biological and social factors in mental health, using a combination of etiological, epidemiological and intervention research strategies and leading to some 500 publications. He is member of the Leopoldina - German National Academy of Science, member of the Academia Europaea and Fellow of the Association for Psychological Science as well as past president of the European Association for Behavioural and Cognitive Therapies (EABCT), the German National Scientific Council on Psychotherapy and the German Society of Psychology.
-
Author contribution: All the authors have accepted responsibility for the entire content of this submitted manuscript and approved submission.
-
Funding: Our work was supported by the Deutsche Forschungsgemeinschaft (DFG) through the research unit FOR 1581 (subprojects P5 and P9 to AZ, SS, CJM, OTW and JM) and the subprojects A09, A13 and A16 of the collaborative research center SFB 1280 (project number 316803389, awarded to AZ, SS, CJM, OTW and, JM).
-
Conflict of interest statement: The authors declare no conflicts of interest regarding this article.
References
Ball, T.M., Knapp, S.E., Paulus, M.P., and Stein, M.B. (2017). Brain activation during fear extinction predicts exposure success. Depress. Anxiety 34, 257–266, https://doi.org/10.1002/da.22583.Suche in Google Scholar PubMed
Bandelow, B. and Michaelis, S. (2015). Epidemiology of anxiety disorders in the 21st century. Dialogues Clin. Neurosci. 17, 327–335.10.31887/DCNS.2015.17.3/bbandelowSuche in Google Scholar PubMed PubMed Central
Bandura, A. (1988). Self-efficacy conception of anxiety. Anxiety. Res. 1, 77–98, https://doi.org/10.1080/10615808808248222.Suche in Google Scholar
Bouchard, S., Gauthier, J., Nouwen, A., Ivers, H., Vallieres, A., Simard, S., and Fournier, T. (2007). Temporal relationship between dysfunctional beliefs, self-efficacy and panic apprehension in the treatment of panic disorder with agoraphobia. J. Behav. Ther. Exp. Psy. 38, 275–292, https://doi.org/10.1016/j.jbtep.2006.08.002.Suche in Google Scholar PubMed
Craske, M.G. and Mystkowski, J. (2006). Exposure therapy and extinction: Clinical studies. Fear and Learning: From Basic Processes to Clinical Implications. M.G. Craske, D. Hermans, and D. Vansteenwegen, eds. (Washington, DC: American Psychological Association), pp. 217–233.10.1037/11474-011Suche in Google Scholar
Craske, M.G., Kircanski, K., Zelikowsky, M., Mystkowski, J., Chowdhury, N., and Baker, A. (2008). Optimizing inhibitory learning during exposure therapy. Behav Res Ther. 46, 5–27, https://doi.org/10.1016/j.brat.2007.10.003.Suche in Google Scholar PubMed
Craske, M.G., Hermans, D., and Vervliet, B. (2018). State-of-the-art and future directions for extinction as a translational model for fear and anxiety. Philos. Trans. R. Soc. Lond. B Biol. Sci. 373, 20170, https://doi.org/10.1098/rstb.2018.0432.Suche in Google Scholar PubMed PubMed Central
Davey, G.C. (1991). Characteristics of individuals with fear of spiders. Anxiety Res. 4, 299–314, https://doi.org/10.1080/08917779208248798.Suche in Google Scholar
de Quervain, D.J.-F., Schwabe, L., and Roozendaal, B. (2017). Stress, glucocorticoids and memory: implications for treating fear-related disorders. Nat. Rev. Neurosci. 18, 7–19, https://doi.org/10.1038/nrn.2016.155.Suche in Google Scholar PubMed
Dymond, S., Dunsmoor, J. E., Vervliet, B., Roche, B., and Hermans, D. (2015). Fear generalization in humans: systematic review and implications for anxiety disorder research. Behav. Ther. 46, 561–582, https://doi.org/10.1016/j.beth.2014.10.001.Suche in Google Scholar PubMed
Forcadell, E., Torrents-Rodas, D., Vervliet, B., Leiva, D., Tortella-Feliu, M., Fullana, M.A. (2017). Does fear extinction in the laboratory predict outcomes of exposure therapy? A treatment analog study. Int J Psychophysiol. 121, 63–71, https://doi.org/10.1016/j.ijpsycho.2017.09.001.Suche in Google Scholar PubMed
Gallagher, M.W., Payne, L.A., White, K.S., Shear, K.M., Woods, S.W., Gorman, J.M., and Barlow, D.H. (2013). Mechanisms of change in cognitive behavioral therapy for panic disorder: The unique effects of self-efficacy and anxiety sensitivity. Behav. Res. Ther. 51, 767–777, https://doi.org/10.1016/j.brat.2013.09.001.Suche in Google Scholar PubMed PubMed Central
Graham, B.M., Li, S.H., Black, M.J., and Öst, L.-G. (2018). The association between estradiol levels, hormonal contraceptive use, and responsiveness to one-session-treatment for spider phobia in women. Psychoneuroendocrinology 90, 134–140, https://doi.org/10.1016/j.psyneuen.2018.02.019.Suche in Google Scholar PubMed
Gunter, R.W. and Whittal, M.L. (2010). Dissemination of cognitive-behavioral treatments for anxiety disorders: Overcoming barriers and improving patient access. Clin. Psychol. Rev. 30, 194–202, https://doi.org/10.1016/j.cpr.2009.11.001.Suche in Google Scholar PubMed
Hofmann, S.G. and Smits, J.A.J. (2008). Cognitive-behavioral therapy for adult anxiety disorders: A meta-analysis of randomized placebo-controlled trials. J. Clin. Psychiatr. 69, 621–632. https://doi.org/10.4088/jcp.v69n0415.Suche in Google Scholar PubMed PubMed Central
Hollander, M.D., de Jong, J., Onghena, P., and Vlaeyen, J.W.S. (2020). Generalization of exposure in vivo in complex regional pain syndrome type I. Behav. Res. Ther. 124, 103511, https://doi.org/10.1016/j.brat.2019.103511.Suche in Google Scholar PubMed
Kessler, R.C., Berglund, P., Demler, O., Jin, R., Merikangas, K.R., and Walters, E.E. (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch. Gen. Psychiatry 62, 593–602, https://doi.org/10.1001/archpsyc.62.6.593.Suche in Google Scholar PubMed
Lissek, S., Powers, A.S., McClure, E.B., Phelps, E.A., Woldehawariat, G., Grillon, C., and Pine, D.S. (2005). Classical fear conditioning in the anxiety disorders: a meta-analysis. Behav. Res. Ther. 43, 1391–1424, https://doi.org/10.1016/j.brat.2004.10.007.Suche in Google Scholar PubMed
Maeng, L.Y. and Milad, M.R. (2015). Sex differences in anxiety disorders: Interactions between fear, stress, and gonadal hormones. Horm. Behav. 76, 106–117, https://doi.org/10.1016/j.yhbeh.2015.04.002.Suche in Google Scholar PubMed PubMed Central
Margraf, J. and Zlomuzica, A. (2015). Changing the future, not the past: a translational paradigm shift in treating anxiety. EMBO Rep. 16, 259–260, https://doi.org/10.15252/embr.201540076.Suche in Google Scholar PubMed PubMed Central
Matchett, G. and Davey, G.C. (1991). A test of a disease-avoidance model of animal phobias. Behav. Res. Ther. 29, 91–94, https://doi.org/10.1016/s0005-7967(09)80011-9.Suche in Google Scholar PubMed
Meir Drexler, S., Merz, C.J., Jentsch, V.L., and Wolf, O.T. (2019). How stress and glucocorticoids timing-dependently affect extinction and relapse. Neurosci. Biobehav. Rev. 98, 145–153, https://doi.org/10.1016/j.neubiorev.2018.12.029.Suche in Google Scholar PubMed
Merz, C.J., Tabbert, K., Schweckendiek, J., Klucken, T., Vaitl, D., Stark, R., and Wolf, O.T. (2012). Oral contraceptive usage alters the effects of cortisol on implicit fear learning. Horm. Behav. 62, 531–538, https://doi.org/10.1016/j.yhbeh.2012.09.001.Suche in Google Scholar PubMed
Merz, C.J., Kinner, V.L., and Wolf, O.T. (2018). Let’s talk about sex… differences in human fear conditioning. Curr. Opin. Behav. Sci. 23, 7–12, https://doi.org/10.1016/j.cobeha.2018.01.021.Suche in Google Scholar
Mosig, C., Merz, C.J., Mohr, C., Adolph, D., Wolf, O.T., Schneider, S., Margraf, J., and Zlomuzica, A. (2014). Enhanced discriminative fear learning of phobia-irrelevant stimuli in spider-fearful individuals. Front. Behav. Neurosci. 8, 328, https://doi.org/10.3389/fnbeh.2014.00328.Suche in Google Scholar PubMed PubMed Central
Norton, P.J. and Price, E.C. (2007). A meta-analytic review of adult cognitive-behavioral treatment outcome across the anxiety disorders. J. Nerv. Ment. Dis. 195, 521–531, https://doi.org/10.1097/01.nmd.0000253843.70149.9a.Suche in Google Scholar PubMed
Otte, C. (2011). Cognitive behavioral therapy in anxiety disorders: current state of the evidence. Dialogues Clin. Neurosci. 13, 413–421.10.31887/DCNS.2011.13.4/cotteSuche in Google Scholar PubMed PubMed Central
Pittig, A., Treanor, M., LeBeau, R.T., and Craske, M.G. (2018). The role of associative fear and avoidance learning in anxiety disorders: Gaps and directions for future research. Neurosci. Biobehav. Rev. 88, 117–140, https://doi.org/10.1016/j.neubiorev.2018.03.015.Suche in Google Scholar PubMed
Preusser, F., Margraf, J., and Zlomuzica, A. (2017). Generalization of extinguished fear to untreated fear stimuli after exposure. Neuropsychopharmacology, 42, 2545, https://doi.org/10.1038/npp.2017.119.Suche in Google Scholar PubMed PubMed Central
Rachman, S., and Lopatka, C. (1986a). Do fears summate?—III. Behav. Res. Ther. 24, 653–660, https://doi.org/10.1016/0005-7967(86)90060-4.Suche in Google Scholar PubMed
Rachman, S., and Lopatka, C. (1986b). A simple method for determining the functional independence of two or more fears—IV. Behav. Res. Ther. 24 661–664, https://doi.org/10.1016/0005-7967(86)90061-6.Suche in Google Scholar PubMed
Raeder, F., Merz, C.J., Tegenthoff, M., Wolf, O.T., Margraf, J., and Zlomuzica, A. (2019a). Post-exposure cortisol administration does not augment the success of exposure therapy: A randomized placebo-controlled study. Psychoneuroendocrinology 99, 174–182, https://doi.org/10.1016/j.psyneuen.2018.09.015.Suche in Google Scholar PubMed
Raeder, F., Woud, M. L., Schneider, S., Totzeck, C., Adolph, D., Margraf, J., et al. (2019b). Reactivation and evaluation of mastery experiences promotes exposure benefit in height phobia. Cognit. Ther. Res. 43, 948–958. https://doi.org/10.1007/s10608-019-10018-x. In press.Suche in Google Scholar
Raeder, F., Heidemann, F., Schedlowski, M., Margraf, J., Zlomuzica, A. (2019c). No pills, more skills: The adverse effect of hormonal contraceptive use on exposure therapy benefit. J Psychiatr Res. 119, 95–101, https://doi.org/10.1016/j.jpsychires.2019.09.016.Suche in Google Scholar PubMed
Raeder, F., Merz, C.J., Margraf, J., Zlomuzica, A. (2020). The association between fear extinction, the ability to accomplish exposure and exposure therapy outcome in specific phobia. Sci. Rep. 10, 4288. https://doi.org/10.1038/s41598-020-61004-3. In press.Suche in Google Scholar PubMed PubMed Central
Richter, J., Pittig, A., Hollandt, M., and Lueken, U. (2017). Bridging the gaps between basic science and cognitive-behavioral treatments for anxiety disorders in routine Care. Z. für Psychol. 225, 252–267, https://doi.org/10.1027/2151-2604/a000309.Suche in Google Scholar
Stockhorst, U. and Antov, M.I. (2016). Modulation of fear extinction by stress, stress hormones and estradiol: A review. Front Behav. Neurosci. 9, 359, https://doi.org/10.3389/fnbeh.2015.00359.Suche in Google Scholar PubMed PubMed Central
Waters, A.M. and Pine, D.S. (2016). Evaluating differences in Pavlovian fear acquisition and extinction as predictors of outcome from cognitive behavioural therapy for anxious children. J. Child Psychol. Psychiatry 57, 869–876, https://doi.org/10.1111/jcpp.12522.Suche in Google Scholar PubMed
Zlomuzica, A., Dere, D., Machulska, A., Adolph, D., Dere, E., Margraf, J. (2014). Episodic memories in anxiety disorders: Clinical implications. Front. Behav. Neurosci. 8, 131, https://doi.org/10.3389/fnbeh.2014.00131.Suche in Google Scholar PubMed PubMed Central
Zlomuzica, A., Preusser, F., Schneider, S., and Margraf, J. (2015). Increased perceived self-efficacy facilitates the extinction of fear in healthy participants. Front. Behav. Neurosci. 9, 270, https://doi.org/10.3389/fnbeh.2015.00270.Suche in Google Scholar PubMed PubMed Central
Zlomuzica, A., Preusser, F., Totzeck, C., Dere, E., and Margraf, J. (2016). The impact of different emotional states on the memory for what, where and when features of specific events. Behav. Brain Res. 298, 181–187, https://doi.org/10.1016/j.bbr.2015.09.037.Suche in Google Scholar PubMed
Zlomuzica, A., Woud, M.L., Machulska, A., Kleimt, K., Dietrich, L., Wolf, O.T., Assion, H.J., Huston, J.P., Silva, M.A.D.S., and Dere, E. (2018). Deficits in episodic memory and mental time travel in patients with post-traumatic stress disorder. Prog. Neuro Psychopharmacol. Biol. Psychiatr. 83, 42–54, https://doi.org/10.1016/j.pnpbp.2017.12.014.Suche in Google Scholar PubMed
© 2020 Armin Zlomuzica et al., published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.
Artikel in diesem Heft
- Frontmatter
- Editorial
- Editorial
- Review articles
- Stress modulation of fear and extinction in psychopathology and treatment
- Clinical implications of fear extinction in anxiety disorders
- From gut feelings to memories of visceral pain
- Principles of extinction learning of nonaversive experience
- Beyond the classic extinction network: a wider, comparative view
- How learning shapes immunity
- Presentation of scientific institutions
- Forschungskolleg “NeurodegX”
- Nachrichten aus der Gesellschaft
- Nachrichten aus der Gesellschaft
Artikel in diesem Heft
- Frontmatter
- Editorial
- Editorial
- Review articles
- Stress modulation of fear and extinction in psychopathology and treatment
- Clinical implications of fear extinction in anxiety disorders
- From gut feelings to memories of visceral pain
- Principles of extinction learning of nonaversive experience
- Beyond the classic extinction network: a wider, comparative view
- How learning shapes immunity
- Presentation of scientific institutions
- Forschungskolleg “NeurodegX”
- Nachrichten aus der Gesellschaft
- Nachrichten aus der Gesellschaft

