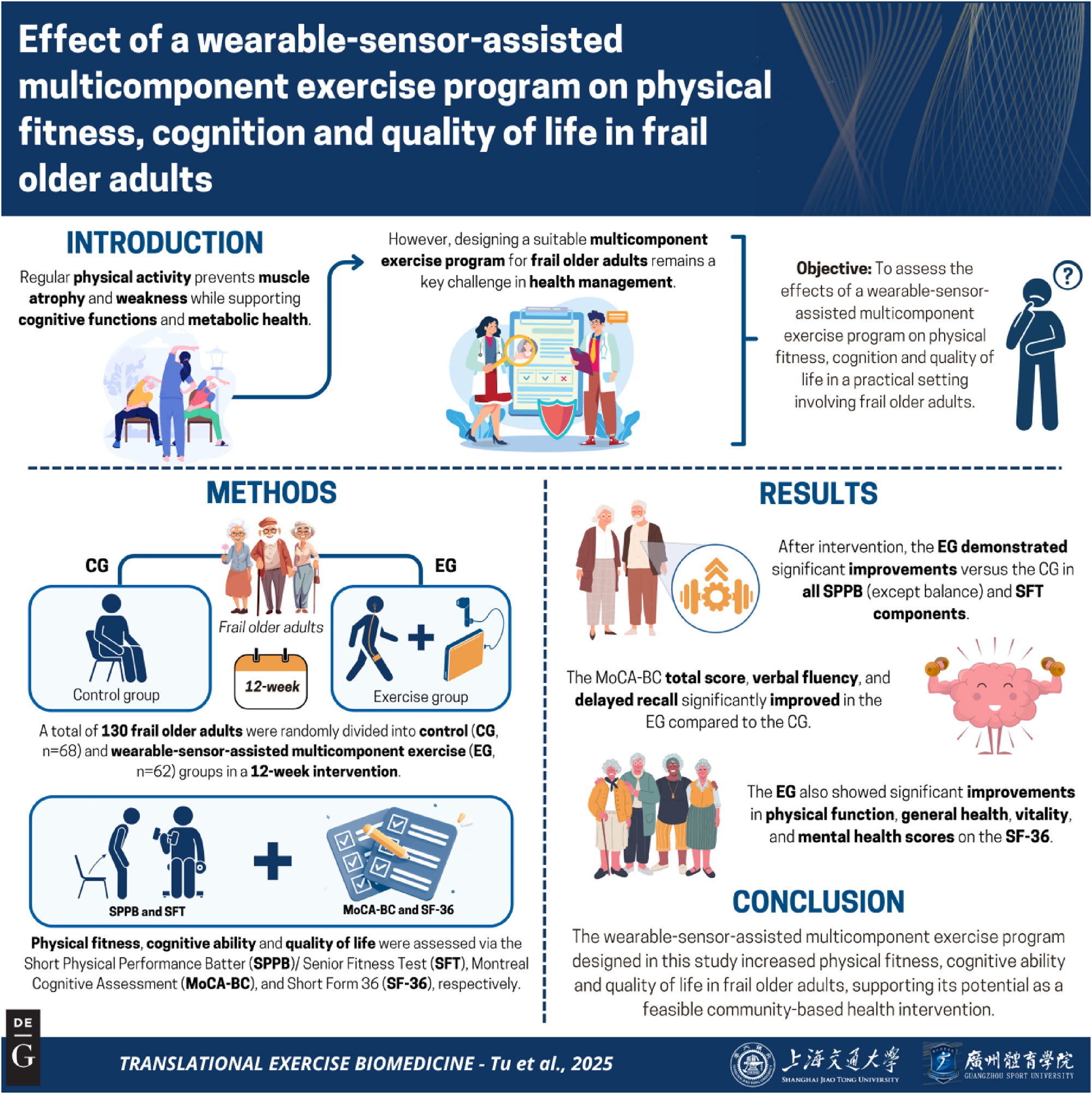
Objectives To assess the effects of a wearable-sensor-assisted multicomponent exercise program on physical fitness, cognition and quality of life in a practical setting involving frail older adults. Methods Frail older adults (n=130) were randomly divided into a control (CG, n=68) group and an exercise group (EG, n=62) in a 12-week intervention, which included stride gait training with wearable sensors; aerobic exercise; and resistance, flexibility, balance, and cognitive training. Primary outcomes (physical fitness) were evaluated via the SPPB and SFT. Secondary outcomes (cognitive ability, quality of life and frailty) were evaluated via the MoCA-BC, SF-36 and Fried frailty criteria, respectively. Results After the 12-week intervention, the EG demonstrated significant improvements (p<0.05) vs. the CG in gait speed (β 3 =0.424, coefficient of interaction effect between group and time from the generalized linear mixed model), chair stand (β 3 =0.501) and total score (β 3 =65.466) of SPPB and all SFT components including 6MWT (walked distance, β 3 =1.098; walking speed, β 3 =0.105; stride length, β 3 =0.041), back scratch (β 3 =4.926), chair sit and reach (β 3 =3.762), 30s arm curl (β 3 =6.124), 30s sit-to-stand (β 3 =3.04), and TUG (β 3 =−6.712). The MoCA-BC total, verbal fluency and delayed recall scores; the physical function, general health, vitality, and mental health scores of the SF-36; and the frailty phenotype in the EG were significantly improved compared with those of the CG. Conclusions The progressive wearable-sensor-assisted multicomponent exercise program designed in this study enhanced physical fitness, cognitive ability and quality of life and slowed down the progression of frailty in frail older adults, supporting its potential as a feasible community-based health intervention.