Abstract
Objectives
The purpose of the study was to assess the prevalence of both non-chronic and chronic pain among women of childbearing age and describe the impact that pain has on their health-related quality of life (HRQoL).
Methods
This is a cross-sectional cohort study, and the data were collected as part of the ICEPAIN nationwide study. Participants were recruited from a randomised sample, stratified by age and residence to secure a proportional sample, by email invitation. Women between 18 and 45 years of age participated, and data were collected through a web-based platform with questionnaires that measured sociodemographic characteristics, lifestyle factors, sleep quality, pain severity, characteristics of pain, pain interference (Brief Pain Inventory), and HRQoL (SF-12-v2). Spearman correlation was used when assessing relationships between demographic and lifestyle factors, and HRQoL and pain. Chi-square, Mann–Whitney U, ANOVA, and multivariate general linear model were used to assess group differences.
Results
In total, 969 women of childbearing age (18–45 years) participated in the study, and the response rate was 34.8%. The average age was 36.1 ± 6.3 years, and the majority (82.5%) were married, cohabiting, or in a steady relationship. Altogether, 45.9% of the sample reported having pain during the past week (n = 445); the vast majority, 80.4% (n = 366), had chronic pain. The majority of the participants, 57.3%, had moderate or severe pain. Chronic pain was significantly correlated with higher age, higher BMI, experiencing pain during the period, and poorer sleep quality. In contrast, no significant correlation was found between chronic pain and parity, residence, education, physical exercise, smoking, or alcohol drinking. Both non-chronic and chronic pain interfered with mood, sleep, general activities, and other aspects of daily life, and the effect of pain was significantly greater among women with chronic pain. Among these, pain severity was strongly correlated with the level of pain interference (0.79). A negative correlation between pain interference and HRQoL (physical component score, −0.64, and mental component score, −0.34) was observed among women with chronic pain.
Conclusions
Both non-chronic and chronic pain are common among women of childbearing age in Iceland. It interferes with daily life and affects their HRQoL.
1 Introduction
Pain is considered one of the most burdensome health problems that affects people’s general activities. Studies have been conducted on the general prevalence of non-chronic and chronic pain in the population; however, many have focused on elderly individuals rather than examining how pain affects the health-related quality of life (HRQoL) of young women. Understanding the frequency of non-chronic and chronic pain among young women and its impact on their lives is important because they often engage in multiple activities, such as studying, working, and caring for children and their families. Women are more likely to experience pain than men, which can partly be related to pain during menstruation, endometriosis, miscarriage, pregnancy or childbirth [1,2,3].
It is essential not only to focus on the prevalence of chronic pain but also to examine the overall prevalence of non-chronic pain among women of childbearing age and its potential impact on their lives [3]. Chronic pain can negatively impact quality of life and affect both physical and mental health [4,5,6]. According to Westergården et al. [7], women living with chronic pain experience various consequences that chronic pain has on daily life, such as feeling lonely and neglected, as well as struggling between a sense of ability and inability. Hence, women found it difficult to cope with the increased stress and reliance on others caused by chronic pain, which made them feel uncertain about their abilities in daily life. Planning their daily activities was also challenging, as they could never predict how the pain would impact them each day. The prevalence of chronic pain varies significantly across population-based studies worldwide, with reported rates ranging from 0 to 24%, depending on various definitions of chronic pain on inclusion criteria, and the variables measured, culture, age, and more. Additionally, approximately one in ten adults in the general population has reported chronic pain, with potential variations influenced by sociocultural factors [8].
The prevalence of chronic pain has been measured worldwide, and in a review study, the prevalence was 11–31% among individuals of different ages. According to Abate et al. [9], women have greater overall years lived with disability (YLD) rates from the age of 10–14 years than men. The YLD rate from 1990 to 2017 decreased by 3–9%, and the leading causes of YLDs were low-back pain and headache disorders. Chronic pain as a primary symptom, such as migraine, headache, neck pain, and low-back pain, accounted for 22.9% of the total YLD worldwide compared to mental disorders (accounting for 14.4%) and cardiovascular disease (accounting for 8.5%) [9]. Pain also had both a personal and an economic burden for women and their families [10].
Studies indicate that chronic pain is more common among women and individuals over the age of 40. Other studies have also shown that women tend to experience pain more frequently than men, pain and pain prevalence tend to rise with age, and those who live in rural areas typically exhibit higher pain prevalence compared to those in urban areas [2,3,11].
In a population-based study conducted in Iceland among people aged 20–70 years, the prevalence of pain during the past week was 55%. Women were more likely to have experienced pain during the previous week (57.3%) than men (53.2%), and among women of childbearing age between 20 and 40 years, the prevalence was approximately 50–52% [12].
Focusing on non-chronic pain, lasting less than 3 months, and pain persisting for more than 3 months is important to define different types of pain. The International Association for the Study of Pain has defined pain as an unpleasant sensory and emotional experience associated with or resembling that associated with actual or potential tissue damage; the definition is expanded by the addition of six key notes, and the etymology of the word “pain” is included for further valuable context. For example, pain is said to be always a personal experience influenced, to varying degrees, by biological, psychological, and social factors [13]. Chronic pain has been defined as pain that has persisted past the normal time of healing and lasted longer than 3 months [14].
Women of childbearing age often experience non-chronic pain related to menstruation, pregnancy, childbirth, and the postpartum period. This pain can affect their lives in many ways [15,16]. Menstruation can cause severe pain both before and during menstruation, especially among women who have not had children [17]. Furthermore, in a recent study conducted in Spain, findings showed that during menstruation, up to 45% of women experience menstrual migraine [15]. According to Allais et al. [18], among approximately 50% of women with migraine, migraine attacks are strongly related to the perimenstrual period.
Endometriosis, a condition in which the tissues that line the uterus grow outside the uterus, is associated with severe abdominal pain, as well as pain during sex and menstrual periods [15]. Hence, women living with endometriosis often experience chronic pain, which limits their daily life activities and negatively affects mood, sleep, walking ability, and enjoyment of life. Studies have shown that women tend to avoid activities in which they cannot participate due to pain, which limits their social interactions. Additionally, pain also has negative effects on their overall health [19]. According to Jonsdottir et al. [12], myalgia was the cause of chronic pain among 41% of women in Iceland, and in 26% of the cases, the cause was earlier trauma. Wear and tear was the cause of pain for 25%, osteoarthritis for 23.9%, and fibromyalgia for 12.8% among participants.
Significant physical and emotional changes occur during pregnancy that can affect women’s health. The physical changes often cause both non-chronic and chronic pain during early and late pregnancy, such as back pain caused by increased weight [20,21]. Pelvic girdle pain (PGP) is often a problem, according to Gashaw et al. [22], who conducted a study with a sample consisting of 424 pregnant women at 6–39 weeks’ gestation. The results showed that the prevalence of PGP was 24.3%. According to Persson et al. [23], pain during and after birth can be caused by PGP, which can cause difficulties in women’s lives during their childbearing age. Women describe increasing restrictions on daily activities during pregnancy, leading to exhaustion and a dysfunctional sexual life characterised by guilt and sexual frustration. Chronic pain affects sleep quality and increases their feeling of being dependent on others, leading to major internal conflict that negatively impacts their self-image [24].
Some of the main factors contributing to the reduction in HRQoL during pregnancy are non-chronic back pain, complications before and after pregnancy, smoking, history of alcohol dependence, and sleeping difficulties. Other critical key factors associated with poor HRQoL are, for example, nausea and vomiting, a history of alcohol abuse, stress, and sexual or domestic violence [6,24].
Chronic pain can significantly impact a woman’s HRQoL, both physically and emotionally, and her social well-being. It can lead to sleep disturbances, reduced mobility, anxiety, and depression, and can affect her ability to work and care for her family [25,26]. In a study conducted in Brazil among women, where the average age was 37 years, chronic pelvic pain significantly decreased women’s HRQoL compared with women who did not have chronic pelvic pain [4].
The aim of this study was to evaluate the prevalence of both non-chronic and chronic pain among women of childbearing age and to describe its impact on their HRQoL. The hypothesis was that the prevalence of both non-chronic and chronic pain among women of childbearing age is relatively high and significantly affects their HRQoL.
2 Methods
2.1 Setting, sample, and data collection
Iceland has a population of approximately 390,000 inhabitants, with about 75,000 women aged between 18 and 45 years, and each year, about 4,400 women give birth. The total number of live-born babies per woman in 2022 was 1.59, the lowest since the measurement began in 1853. About 14% of women in Iceland are single and live with their children at home [27]. In 2022, 53.9% of women aged 25–64 years in Iceland had a university education, compared to 32.9% of men, and the level of education among individuals residing in rural areas was lower compared to those living in the capital region. In 2021, 75.1% of women worked outside their home, with an average of 32.4 h of work per week [28].
Data were collected through a web-based platform provided by a service contractor, Maskina, using a national panel representing a randomised population sample from the National Population Register of Iceland.
This study is part of the ICEPAIN study, where a sample of 12,400 individuals aged 18–80 years was randomly selected and invited by email to participate in the study, and to secure proportionality, the sample was stratified in relation to age and residence. The overall response rate was 44.8% (N = 5.557), where 57.3% were women, and the response rate among childbearing women was 34.8%. A sample from the study was drawn from that database. The inclusion criteria specified that participants had to be women between the ages of 18 and 45, who could understand and complete the questionnaires in Icelandic. There were no exclusion criteria for participation.
The questionnaire measured sociodemographic characteristics, lifestyle factors, sleep quality, pain severity, characteristics of pain, pain interference, and HRQoL.
2.2 Sociodemographic characteristics
The sociodemographic data collected were age (years), marital status (married/cohabiting, single, divorced, widow), education (years of education, primary, tertiary, higher), residency (rural/capital area), and fertility history such as if they had children (yes/no, and if yes, how many), if they had a child under one year of age, if they were pregnant (yes/no, if yes, number of pregnancies, 1–10), miscarriage (yes/no, if yes, number, 1–10), pregnancy (yes/no, if yes, number, 1–10), and experience of last birth (very positive/rather positive/mixed feelings/rather negative/very negative). Participants were asked about their height (cm) and weight (kg), which were used to calculate their BMI. Only two (0.2%) of the participants could be categorised as underweight. Correspondingly, BMI values were placed into three categories: normal weight (BMI < 25), overweight (BMI 25–30), or obesity (BMI > 30).
2.3 Lifestyle variables
Questions on lifestyle were specially designed to collect data for this study. Questions from the Health and Well-being of Icelanders questionnaire were used to evaluate the physical activity [29]. Participants were asked how often and for how long they engaged in physical exercise for the conscious purpose of strengthening the body, for example, swimming, walking, cycling, or other physical exercises. The response options for frequency were never, less than once per month, 1–3 times per month, 1–2 times per week, 3 times per week, or more. The response options for duration were less than 15 min, 15–29 min, 30–60 min, or more than 60 min. Based on information on frequency and duration, physical exercise was recorded into four categories: no exercise, little exercise (<15 min per week), moderate exercise (15–45 min per week), or exercise more than 45 min per week.
Information about smoking was collected by asking participants if they smoked or had ever smoked (cigarettes, cigars, pipes), and current smokers were asked about smoking habits (daily, at least once a week, less than once a week). Questions on the frequency and type of alcoholic beverage (light wine, beer, strong alcohol drinks) were asked to assess participants’ alcoholic consumption, and responses were categorised into two groups: those who drank once a month or less and those who drank twice a month or more.
Questions from the Health and Well-being of Icelanders questionnaire were used to evaluate the quality of sleep, sleep hours, and sleeping problems [29]. Participants were asked how many hours (less than 5 h up to more than 10 h) they usually sleep each night. Answers were collapsed into three categories: ≤6 h, 7–8 h, or ≥9 h. Sleep quality was assessed by the question: How often or rarely have the following occurred in the last 4 weeks in relation to sleeping at night? The statements were (1) I slept continuously all night, (2) I woke up rested after a good night’s sleep, (3) I had a hard time falling asleep, and (4) I woke up after falling asleep and had a hard time getting back to sleep. The response options for each statement were never, seldom, sometimes, often, or every night. Responses were grouped into three categories: no sleeping problems, moderate sleeping problems, and serious sleeping problems. Those who responded to statements 1 and 2 with never or seldom and statement 3 with often or always were considered as having severe sleeping problems. Those responding sometimes to all statements, or seldom or sometimes to one or two statements, and sometimes to others were considered as having moderate sleeping problems. Those who responded often or always to statements 1 and 2 and never or seldom to statements 3 and 4 were considered to have no sleeping problems.
2.4 Pain prevalence, characteristics of pain, and pain interference with life
The Icelandic version of the Brief Pain Inventory (BPI) was used to evaluate pain severity, pain location, and pain interference [30,31]. Participants were asked if they had experienced pain (other than minor headaches, sprains, or toothache) the previous week (yes/no), and those who responded with yes were asked how long the pain had lasted (years, months, weeks) and to indicate locations where they felt pain on a body map.
The BPI contains four questions regarding pain severity during the past 24 h (pain now, average pain, worst, and least pain) on a scale from 0 to 10, where 0 indicates no pain, and 10 is the worst pain imaginable. Questions on pain interference evaluate pain interference in seven aspects of daily life: daily activities, mood, mobility, work, social relations, sleep, and life satisfaction. On a 0–10 scale, anchored with does not interfere (0) and completely interferes (10) [30]. By using the mean of the four severity items and the seven interference items separately, two composite scores, the Pain Severity Index (PSI) and the Pain Interference Index (PII), are calculated [32]. The BPI has been translated into Icelandic and validated in a general population sample of Icelandic adults experiencing pain of various origins and found to be both reliable and valid [12,31].
2.5 HRQoL
The Short Form 12 Health Survey Version 2 (SF-12v2) is a self-rated questionnaire developed to assess some primary aspects of HRQoL and perceived health status in various health conditions [33]. The instrument comprises 12 multiple-choice questions, measuring 8 domains (physical functioning, physical role limitations, bodily pain, general health, vitality, social functioning, emotional role limitations, and mental health). From these eight domains, the physical component (PCS) and mental component (MCS) summary scores are calculated. Each component is scored on a 0–100 scale, with a mean of 50, where higher scores indicate better health [33,34]. The instrument has shown good reliability and validity when assessing HRQoL in population surveys. The reliability and validity of the instrument have been tested and confirmed in relation to public health [33,35,36].
2.6 Statistical analyses
Data were analysed using SPSS for Windows (version 28.0). Descriptive statistics are presented as numbers and percentages for categorical variables, while continuous variables are presented with mean, standard deviation, and the number of observations. The chi-square test for independence was used to analyse the relationship between categorical variables. Differences in mean age and BMI among pain groups were analysed using ANOVA with a Bonferroni post-hoc test to determine which group means are significantly different. Group differences in pain interference scale scores were analysed using the Mann–Whitney U test due to the ordinal nature of the data. Spearman’s rank-order correlation coefficient (rho) was used to assess the strength and direction of the relationship between chronic pain, pain interference, and participant characteristics. A bootstrapped multivariate general linear model was used to assess the impact of PCS, MCS, age, and chronic pain on seven health-related outcome variables: daily activities, mood, mobility, work, social relations, sleep, and life satisfaction. Bootstrapping helps ensure robust inference in case of unequal error variances. Pairwise deletion was used in the analyses to handle missing data, as the analyses focused mainly on pairwise relationships. This allows for maximum use of available data, which can lead to more robust statistical analyses. Also, in most cases, the proportion of missing data was less than 5%. This methodological approach corroborates the study’s aim to evaluate the prevalence of pain and chronic pain among women of childbearing age and to elucidate its impact on HRQoL. The underlying hypothesis suggests that both non-chronic and chronic pain significantly affect multiple aspects of women’s lives.
3 Results
3.1 Characteristics of participants
In total, 5.557 people participated in the ICEPAIN study, with a response rate of 44.8%. Of these, 3,173 were women, and 996 were women of childbearing age (18–45 years), which constituted the sample in our study. The average age of the sample was 36.1 ± 6.3 years, and 3.4% of the women were pregnant at the time they answered the questionnaire, which does not allow further analysis for that group. The majority, 82.5%, were married, cohabiting, or in a steady relationship, and 17.5% were divorced or single. More than half lived in the capital area (54.2%), and most of the women (75.8%) had children, where 10.4% having a child under the age of one year. Mean BMI was 28.4 ± 6.1. Most of the women reported having menstrual pain during their periods (75.2%), and for 47.9%, the pain had negative effects on their daily lives. Further information is presented in Table 1.
Characteristics of participants (N = 969)
| n | % | |
|---|---|---|
| Age group (years) | ||
| 21–25 | 50 | 5.2 |
| 26–30 | 168 | 17.3 |
| 31–35 | 207 | 21.4 |
| 36–40 | 231 | 23.8 |
| 41–45 | 313 | 32.3 |
| Marital status | ||
| Married/cohabiting/steady relationship | 799 | 82.5 |
| Single/divorced/widowed | 170 | 17.5 |
| Residence | ||
| Capital area | 524 | 54.2 |
| Outside the capital area | 442 | 45.8 |
| Education | ||
| Primary | 56 | 6.5 |
| Secondary | 227 | 26.4 |
| Tertiary | 577 | 67.1 |
| BMI (kg/m²) | ||
| <25 | 285 | 34.1 |
| 25–30 | 253 | 30.2 |
| >30 | 299 | 35.7 |
| Smoking | ||
| Never | 528 | 62.3 |
| Previous | 233 | 27.5 |
| Current | 87 | 10.3 |
| Alcohol drinking | ||
| Once a month or less | 505 | 56.4 |
| Twice a month or more | 391 | 43.6 |
| Sleep quality | ||
| No sleeping problems | 361 | 39.7 |
| Moderate sleeping problems | 244 | 26.8 |
| Severe sleeping problems | 305 | 33.5 |
| Physical exercise | ||
| No exercise/less than 15 min per week | 170 | 18.9 |
| Little exercise 15–45 min per week | 179 | 19.9 |
| Moderate exercise 45–90 min per week | 236 | 26.2 |
| Exercise more than 90 min per week | 316 | 35.1 |
| Pain associated with period | ||
| Yes | 652 | 75.2 |
| No | 215 | 24.8 |
| Impact of menstrual pain on daily life during the period a | ||
| Yes | 312 | 47.9 |
| No | 340 | 52.1 |
| Children | ||
| Yes | 658 | 75.8 |
| No | 210 | 24.2 |
| Have you given birth in the last 12 months? | ||
| Yes | 69 | 10.4 |
| No | 594 | 89.6 |
| Are you pregnant now? | ||
| Yes | 33 | 5.0 |
| No | 630 | 95.0 |
| Experience of the last birth | ||
| Very positive | 267 | 40.9 |
| Rather positive | 174 | 26.6 |
| Mixed feelings | 83 | 12.7 |
| Rather negative | 87 | 13.3 |
| Very negative | 42 | 6.4 |
| Miscarried | ||
| Yes | 261 | 31.1 |
| No | 605 | 69.9 |
aOnly those who feel pain during periods.
3.2 Prevalence, severity, and location of non-chronic and chronic pain among women during the past week
Of the total sample of respondents (n = 969), 45.9% reported having experienced pain during the past week. Among those with pain, the frequency of reported locations of the pain were in the head and shoulder region (74%), lower extremities (53%), the hip region (48%), lower back (47%), upper extremities (38%), upper back (24%), chest region (21%), and pelvis and genitals (20%). A large proportion of women identified multiple pain locations during the past week (n = 452), with 79% marking more than one area. Moreover, 21% of the women reported pain in only one region. Those with pain in two regions were 21%; in three regions, 18%; in four regions, 13%; and 27% between five and eight regions. Figure 1 shows the results from BPI assessing pain severity during the past 24 h (pain now, average pain, worst, and least pain). The mean for worst pain was 4.6 ± 2.3, while the mean for least pain was 1.7 ± 1.7. The average mean pain during the last 24 h was 3.9 ± 2.0.
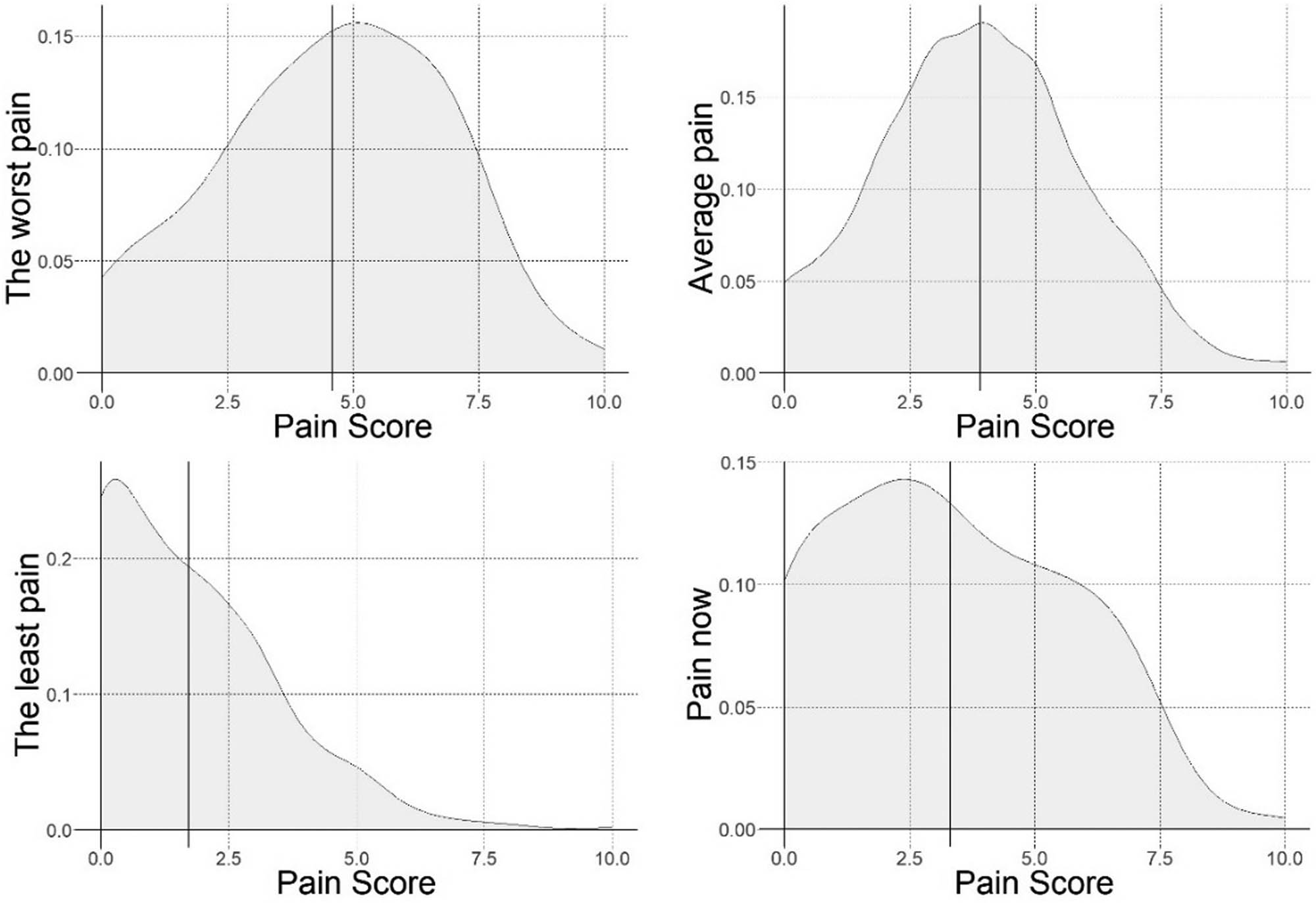
Density plots of pain severity during the last 24 h for worst, average, least, and pain now, with the mean value indicated.
Among women reporting pain during the past week (n = 445), the vast majority, 80.4% (n = 366), had chronic pain, with an average duration of 9.6 ± 9.7 years. Table 2 presents a comparison between the three groups: no pain during the past week, non-chronic pain during the past week, and chronic pain.
Characteristics of those who experienced no pain, non-chronic pain during the past week, and chronic pain (N = 969)
| No pain during the past week | Pain during the past week | Pain during the past week | p-valuea | |
|---|---|---|---|---|
| Non-chronic pain | Chronic pain | |||
| m (sd/n) | m (sd/n) | m (sd/n) | ||
| Age (years) | 35.8 (6.1/524) | 35.7 (6.7/79) | 36.8 (6.5/366) | 0.044 |
| BMI | 27.6 (5.7/417) | 28.2 (5.7/76) | 29.5 (6.4/344) | <0.001 |
| Age group (years) | n (%) | n (%) | n (%) | p-valueb |
| 21–25 | 21 (4.0) | 11 (13.9) | 18 (4.9) | <0.001 |
| 26–30 | 101 (19.3) | 8 (10.1) | 59 (16.1) | |
| 31–35 | 119 (22.7) | 14 (17.7) | 74 (20.2) | |
| 36–40 | 138 (26.3) | 23 (29.1) | 70 (19.1) | |
| 41–45 | 145 (27.7) | 23 (29.1) | 145 (39.6) | |
| Marital status | ||||
| Married/cohabit/steady relationship | 438 (83.6) | 60 (75.9) | 301 (82.2) | 0.248 |
| Single/divorced/widowed | 86 (16.4) | 19 (24.1) | 65 (17.8) | |
| Residence | ||||
| Capital area | 295 (56.6) | 44 (55.7) | 185 (50.5) | 0.195 |
| Outside the capital area | 226 (43.4) | 35 (44.3) | 181 (49.5) | |
| Education | ||||
| Primary | 16 (3.6) | 7 (10.4) | 33 (9.4) | 0.002 |
| Secondary | 111 (25.2) | 13 (19.4) | 103 (29.3) | |
| Tertiary | 314 (71.2) | 47 (70.1) | 216 (61.4) | |
| BMI (kg/m 2 ) | ||||
| <25 | 167 (40.0) | 29 (38.2) | 89 (25.9) | 0.002 |
| 25–30 | 121 (29.0) | 21 (27.6) | 111 (32.3) | |
| >30 | 129 (30.9) | 26 (34.2) | 144 (41.9) | |
| Smoking | ||||
| Never | 296 (68.7) | 43 (58.1) | 189 (55.1) | 0.002 |
| Previous | 102 (23.7) | 21 (28.4) | 110 (32.1) | |
| Current | 33 (7.7) | 10 (13.5) | 44 (12.8) | |
| Alcohol drinking | ||||
| Once a month or less | 237 (52.5) | 40 (50.6) | 228 (62.3) | 0.011 |
| Twice a month or more | 214 (47.5) | 39 (49.4) | 138 (37.7) | |
| Sleep quality | ||||
| No sleeping problems | 229 (49.0) | 29 (37.7) | 103 (28.1) | <0.001 |
| Moderate sleeping problems | 123 (26.3) | 23 (29.9) | 98 (26.8) | |
| Severe sleeping problems | 115 (24.6) | 25 (32.5) | 165 (45.1) | |
| Physical exercises | ||||
| No exercise/less than 15 min per week | 74 (16.2) | 14 (17.7) | 82 (22.4) | 0.236 |
| Little exercise 15–45 min per week | 85 (18.6) | 15 (19.0) | 79 (21.6) | |
| Moderate exercise 45–90 min per week | 125 (27.4) | 22 (27.8) | 89 (24.3) | |
| Exercise more than 90 min per week | 172 (37.7) | 28 (35.4) | 116 (31.7) | |
| Pain associated with the period | ||||
| Yes | 315 (60.1) | 60 (75.9) | 277 (75.7) | <0.001 |
| No/not applicable/missing | 209 (39.9) | 19 (24.1) | 89 (24.3) | |
| Effect of menstrual pain on daily life during the period | ||||
| Yes | 124 (39.4) | 27 (45.0) | 161 (58.1) | <0.001 |
| No | 191 (60.6) | 33 (55.0) | 116 (41.9) | |
| Children | ||||
| Yes | 339 (64.7) | 49 (62.0) | 270 (73.8) | 0.009 |
| No | 185 (35.3) | 30 (38.0) | 96 (26.2) | |
| Experience of the last birth | ||||
| Very positive | 160 (47.8) | 20 (40.8) | 87 (32.3) | 0.004 |
| Rather positive | 77 (23.0) | 17 (34.7) | 80 (29.7) | |
| Mixed feelings | 36 (10.7) | 6 (12.2) | 41 (15.2) | |
| Rather negative | 45 (13.4) | 6 (12.2) | 36 (13.4) | |
| Very negative | 17 (5.1) | 0 (0.0) | 25 (9.3) | |
| Miscarried | ||||
| Yes | 127 (24.2) | 20 (25.3) | 114 (31.1) | 0.069 |
| No | 397 (75.8) | 59 (74.7) | 252 (68.9) |
aANOVA with Bonferroni post-hoc test revealing no significant differences in the mean between pain groups and a significantly lower BMI in those with no pain compared to those with pain. bChi-square tests.
3.3 Pain interference
To clarify the relationship between chronic pain and the participants’ characteristics, Table 3 presents an analysis of the correlations observed in the study. It highlights how chronic pain significantly correlates with poorer HRQoL and other lifestyle factors. Specifically, the data indicate that chronic pain was correlated with a higher BMI, current smoking, poorer sleep quality, and menstrual pain. In contrast, no significant correlation between chronic pain and parity, residence, education, physical exercise, smoking, or alcohol drinking was observed. Furthermore, pain interference was significantly correlated (p < 0.001) with chronic pain and HRQoL (both physical and mental component scores), alongside other participant characteristics such as pain severity and education level. More information is presented in Table 3.
Correlation between chronic pain, pain interference, and characteristics of participants
| Chronic pain | Pain interference | |||
|---|---|---|---|---|
| Spearman’s rho | p-value | Spearman’s rho | p-value | |
| Chronic pain | 1 | 0.233 | <0.001 | |
| Pain interference | 0.233 | <0.001 | 1 | |
| Physical component score | −0.424 | <0.001 | −0.641 | <0.001 |
| Mental component score | −0.182 | <0.001 | −0.339 | <0.001 |
| Pain severity | 0.232 | <0.001 | 0.795 | <0.001 |
| Age | 0.091 | 0.005 | 0.144 | 0.003 |
| Marital status | 0.004 | 0.891 | 0.025 | 0.614 |
| Residence | 0.058 | 0.072 | 0.072 | 0.147 |
| Education | −0.110 | 0.001 | −0.194 | <0.001 |
| BMI (kg/m2) | 0.143 | <0.001 | 0.214 | <0.001 |
| Smoking | 0.123 | <0.001 | 0.124 | 0.015 |
| Alcohol drinking | 0.099 | 0.003 | 0.082 | 0.096 |
| Sleep quality | 0.222 | <0.001 | 0.400 | <0.001 |
| Physical exercises | −0.087 | 0.009 | −0.135 | 0.006 |
| Pain associated with the period | 0.139 | <0.001 | 0.049 | 0.316 |
| Effect of menstrual pain on daily life during the period | 0.177 | <0.001 | 0.278 | <0.001 |
| Children | 0.098 | 0.002 | 0.119 | 0.015 |
| Miscarried | 0.074 | 0.021 | 0.127 | 0.010 |
The SF-12 questionnaire includes a question regarding how pain has interfered with daily activities over the past 4 weeks. Among the participants, 59.7% reported that pain negatively impacted their normal work outside the home and their housework. Specifically, 4.7% of women indicated that pain affected them extremely, 9.0% noted it affected them quite a bit, 10.4% stated it moderately affected their work, and 35.5% a little.
Table 4 presents the mean levels of pain interference across seven aspects of daily life among participants with non-chronic and chronic pain. The results indicate that individuals with chronic pain reported significantly higher interference in all assessed domains compared to those with non-chronic pain. Specifically, interference was greatest among the chronic pain group in areas such as sleep (m = 3.80, sd = 3.07), mood (m = 3.72, sd = 2.87), and daily activities (m = 3.66, sd = 2.94). All between-group differences were statistically significant (p < 0.001), as determined by the Mann–Whitney U test.
Level of pain interference in seven aspects of daily life among participants with non-chronic and chronic pain
| Non-chronic pain | Chronic pain | p-valuea | |
|---|---|---|---|
| m (sd/n) | m (sd/n) | ||
| Daily activities | 2.01 (2.31/70) | 3.66 (2.94/364) | <0.001 |
| Mood | 2.44 (2.41/71) | 3.72 (2.87/361) | <0.001 |
| Mobility | 1.47 (2.29/70) | 2.70 (2.93/361) | <0.001 |
| Work | 1.49 (2.50/70) | 2.96 (3.38/351) | <0.001 |
| Social relations | 0.84 (1.78/68) | 1.76 (2.37/357) | <0.001 |
| Sleep | 1.96 (2.56/69) | 3.80 (3.07/360) | <0.001 |
| Life satisfaction | 1.86 (2.29/69) | 3.47 (2.96/359) | <0.001 |
aMann–Whitney U test.
Table 5 summarises results from a multivariate general linear model examining the effects of PCS, MCS, age, and chronic pain status on the seven functional and psychosocial health outcomes. PCS, MCS, and age all showed significant multivariate effects (Pillai’s Trace, all p < 0.001), while chronic pain did not contribute significantly at the multivariate level (p = 0.330). Other background variables did not show significant multivariate effects when included in the model and were therefore excluded. PCS and MCS were the most consistent and robust predictors, significantly associated with lower impairment across all outcomes. For example, higher PCS predicted fewer difficulties with daily activities (β = −0.15, 95% CI [−0.17, −0.13]) and life satisfaction (β = −0.12, 95% CI [−0.14, −0.10]), while higher MCS was similarly protective, particularly for mood and social relations. Age had weaker effects overall but was positively associated with sleep problems (β = 0.07, 95% CI [0.03, 0.11]) and life satisfaction (β = 0.04, 95% CI [0.01, 0.08]). Chronic pain status predicted daily activities and sleep, but no other outcomes, with broader confidence intervals indicating less precision.
Multivariate general linear model results: unstandardised regression coefficients (β) predicting seven health outcomes
| Predictor | Age | PCS | MCS | Chronic pain |
|---|---|---|---|---|
| Outcome | β [95% CI] | β [95% CI] | β [95% CI] | β [95% CI] |
| Daily activities | 0.02 [−0.02, 0.06] | −0.15*** [−0.17, −0.13] | −0.07*** [−0.09, −0.05] | −0.65* [−1.15, −0.12] |
| Mood | −0.01 [−0.05, 0.02] | −0.11*** [−0.13, −0.09] | −0.11*** [−0.13, −0.09] | −0.43 [−1.00, 0.14] |
| Mobility | 0.02 [−0.02, 0.05] | −0.15*** [−0.17, −0.13] | −0.03*** [−0.06, −0.01] | −0.34 [−0.81, 0.22] |
| Work | 0.01 [−0.03, 0.05] | −0.17*** [−0.19, −0.14] | −0.06*** [−0.09, −0.03] | −0.42 [−0.94, 0.12] |
| Social relations | 0.03† [−0.01 ,0.05] | −0.10*** [−0.11, −0.08] | −0.09*** [−0.11, −0.07] | −0.19 [−0.62, 0.25] |
| Sleep | 0.07*** [0.03, 0.11] | −0.12*** [−0.14, −0.10] | −0.09*** [−0.12, −0.07] | −0.90** [−1.59, −0.21] |
| Life satisfaction | 0.04* [0.01, 0.08] | −0.12*** [−0.14, −0.10] | −0.12*** [−0.14, −0.10] | −0.55† [−1.06, 0.01] |
***p < 0.001, **p < 0.01, *p < 0.05, † p < 0.10, and n.s. = not significant. Values in brackets are 95% bootstrap confidence intervals based on 1,000 bootstrap resamples.
4 Discussion
Overall, there is a general lack of literature addressing the prevalence of non-chronic and chronic pain among women of childbearing age in Iceland and HRQoL. Indeed, no published studies on pain among women of childbearing age were found. Approximately 20% of people living in Iceland are women of childbearing age [27]. The results of this study indicate that both non-chronic and chronic pain affect HRQoL among women of childbearing age. Therefore, it is crucial to consider the overall impact of both non-chronic and chronic pain, even though chronic pain has a greater effect on their lives than non-chronic pain. Quantitative comparisons of levels of pain interference further supported this. As shown in Table 4, women with chronic pain reported significantly higher interference across all life domains compared to those with non-chronic pain, with the largest differences observed in sleep, mood, and daily activities (all p < 0.001).
In the present study, 45.9% of the women reported pain during the past week, 38% of whom had chronic pain (pain lasting longer than 3 months). The prevalence of chronic pain among women of childbearing age in Iceland is higher than that has been reported for different age groups in other recent studies [3,37]. Our findings demonstrate that chronic pain among women of childbearing age in Iceland is high compared to findings in other studies, which show that the global prevalence of chronic pain varies widely. For example, a systematic review and meta-analysis of 43 articles from 22 countries, involving a total of 97,437 participants aged 15–34 years, found that the prevalence of chronic pain ranged from 4.1% to 34.4%, with an overall pooled random-effect prevalence of 11.6% for the entire group [37]. In a meta-analysis encompassing the prevalence of pain based on the definition of pain lasting 1 month or longer, the prevalence was 28%. Pain was more common among women and increased with age, and tended to be greater in rural areas as opposed to urban ones [3]. The present study focused on pain among women of childbearing aged 18–45 years, while the aforementioned studies presented data on pain prevalences among both men and women and from different age groups.
Some studies have reported chronic pain among childbearing women. For example, a study among women between the ages of 15 and 49 years in Australia reported a 9.7% chronic or recurrent pain rate among non-pregnant women. The prevalence of chronic pain in that study was lower than in the present study; however, it is notable that the definition of chronic pain was not the same in our study as in Miller et al.’s study. The definition of chronic pain used by Miller et al. [38] was stricter (requiring pain to have lasted for at least 6 months) than the definition used in the present study. Hence, several differences that might affect prevalence in disparate studies, such as age range, assessment, and definition of chronic pain, might explain the prevalences measured by the two studies. Murray et al. [37] also conducted a systematic review of the prevalence of chronic pain among women of childbearing age. In their study, the prevalence was reported to be 11.6%. However, the age range in their research was 15–34 years, which diverges from the 18 to 45 age range in our study. This distinction in age groups might explain some variations in the prevalence rates observed between the two studies.
Due to varying definitions of chronic pain, it is difficult to directly compare findings between different studies. It is interesting that in the present study, chronic pain was significantly correlated with higher age, higher BMI, menstrual pain, and poorer sleep quality. Increased BMI is linked to increased pain, both mild/moderate and severe, and/or limiting pain [39,40]. Furthermore, Stokes et al. [40] found that between 1992 and 2016, the proportion of US adults aged 55–61 experiencing severe or limiting chronic pain increased substantially, increasing from 17 to 23% among females. Simultaneously, the proportion of women with obesity or overweight also increased from 61.4 to 74.9%. Even though the age range in their study diverges from ours, our findings linked to higher BMI and chronic pain are noteworthy and should be considered. Steingrimsdottir et al. [11] also highlighted that it is often difficult to compare findings from distinct studies because the definition of chronic pain varies significantly across studies. A systematic review and meta-analysis of 86 studies found that no two studies from independent research groups used the same criteria. The prevalence of chronic pain varied from 8.7 to 64% across groups, with different inclusion and exclusion criteria. Although it is unclear what the clinical significance of the high prevalence of both chronic and non-chronic pain among women of childbearing age in Iceland, the findings of this study highlight the importance of healthcare providers paying attention to women’s experiences of pain and its impact on their lives.
Pain affects daily life, including daily functioning and sleep quality. Based on findings from a population-based study, including 225,541 participants, poor sleep quality is significantly associated with lower HRQoL. In comparison with individuals with good sleep quality, people with poor sleep quality are almost twice as likely to have pain and to experience limited ability regarding physical exercise and daily activities [41]. This aligns with the results of our study, where women with chronic pain were more likely to report poor sleep quality compared to those who did not experience non-chronic or chronic pain during the previous week. As shown in Table 5, multivariate regression analysis revealed that PCS, MCS, and age had significant multivariate effects on all outcomes (p < 0.001), while chronic pain status did not (p = 0.330). Nonetheless, chronic pain significantly predicted interference with daily activities and sleep. PCS and MCS were the strongest and most consistent predictors, with higher scores associated with fewer limitations across all domains. Age showed weaker effects but was significantly linked to sleep problems and life satisfaction. The findings suggest that overall physical and mental health significantly impact functioning more than pain status alone.
Supported by the regression analysis, this study found that chronic pain interferes with mood. The effect of chronic pain on mood has been assessed in other studies, for example, in a study by Garnaes et al. [42]. Using a cross-sectional design with data on patients with chronic musculoskeletal pain in primary health care in Norway, demographic factors and pain characteristics associated with HRQoL were analysed. Variables that are associated with poorer HRQoL include female sex and factors such as mood, sleep, life enjoyment, and relations with other people. Having chronic pain for more than 6 months was also correlated with poorer HRQoL [5,41]. A strong inverse relationship was found between chronic pain and HRQoL in the present study. These results align with those of similar studies [5,41], which have shown that pain affects HRQoL. Furthermore, our findings show that the relationship between pain and HRQoL depended on severity, duration of the pain, as well as individual social demographic and lifestyle variables. Most participants reported that pain, whether they had non-chronic or chronic pain, influenced their HRQoL, which is notable considering that our sample comprised young women, often mothers who are usually very active and typically in the prime of their lives. It is therefore important to acknowledge that both chronic and non-chronic pain affect women’s HRQoL, and it is essential to study both. While this study offers valuable insights into the impact of especially chronic pain on HRQoL among women of childbearing age, it is essential to recognise that confounding factors may influence the observed relationships. For instance, demographic variables such as marital status, residence, education, and lifestyle factors were initially included in the multivariate model and tested for potential confounding effects. However, as they did not show significant associations, they were excluded from the final model. Thus, while these factors were considered, residual confounding cannot be entirely ruled out. Thus, the comparisons of SF-12 results between pain groups should be interpreted with this in mind.
This study had several limitations. Pain and HRQoL were measured using a retrospective self-reported tool. Therefore, recall bias may have affected our findings, as it could have led to underreporting or overreporting of pain’s severity and interference, ultimately skewing the results. In addition, the response rate was low at 34.8%, which could have affected the study’s reliability. The major strength of this study is that it provides valuable data on the relationships between chronic pain and diverse demographic, lifestyle, and adverse life experiences among women in a total population sample.
5 Conclusion
Both non-chronic and chronic pain among women of childbearing age is common and should be recognised as a significant public health issue, as this group is usually highly active, working outside their home, taking care of children, and many are also studying. The present study brings new information to the literature. It highlights the importance of recognising the high prevalence of non-chronic and chronic pain among women of childbearing age in Iceland, as well as its impact on their HRQoL.
Acknowledgments
We would like to thank the participants who took part in this study for their involvement and time.
-
Research ethics: This study was approved by the Icelandic National Bioethics Committee (VSN-19-096).
-
Informed consent: Participants received information about the study by email and an invitation to participate by logging into a website containing the questionnaire. Participants gave their informed consent by answering and submitting the web-based questionnaire.
-
Author contributions: All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Competing interests: The authors state no conflict of interest.
-
Research funding: The study was funded by the University of Akureyri Research Fund and the Icelandic Public Health Fund (Lýðheilsusjóður).
-
Data availability: Complete datasets, generated or analysed during this study, are not shared due to confidentiality.
-
Artificial intelligence/Machine learning tools: Not applicable.
References
[1] Bala M, Jahan E, Hashami U, Khan M, Tabassum S, Imtiaz R. Endometriosis: Overview and management options: A review article. JRMDS. 2022;10:300–4.10.18535/ijsrm/v10i12.mp04Suche in Google Scholar
[2] Komatsu R, Ando K, Flood PD. Factors associated with persistent pain after childbirth: A narrative review. BJA. 2020;124:e117–30.10.1016/j.bja.2019.12.037Suche in Google Scholar PubMed PubMed Central
[3] Zimmer Z, Fraser K, Grol-Prokapcyk H, Zajacova A. A global study of pain prevalence across 52 countries: Examining the role of country-level contextual factors. Pain. 2022;163:1740–50.10.1097/j.pain.0000000000002557Suche in Google Scholar PubMed PubMed Central
[4] Da Luz RA, de Deus JM, Conde DM. Quality of life and associated factors in Brazilian women with chronic pelvic pain. J Pain Res. 2018;11:1367–74.10.2147/JPR.S168402Suche in Google Scholar PubMed PubMed Central
[5] Cohen SP, Vase L, Hooten WM. Chronic pain: An update on burden, best practices, and new advances. The Lancet (British edition). 2021;397:2082–97.10.1016/S0140-6736(21)00393-7Suche in Google Scholar PubMed
[6] Lagadec N, Steinecker M, Kapassi A, Magnier AM, Chastang J, Robert S, et al. Factors influencing the quality of life of pregnant women: A systematic review. BMC Pregnancy Childbirth. 2018;18:1–14.10.1186/s12884-018-2087-4Suche in Google Scholar PubMed PubMed Central
[7] Westergården M, Aili K, Larsson I. “Moving between living in the shadow of pain and living a life with the pain in the shadows” – women’s experiences of daily life with chronic widespread pain: A qualitative study. Int J Qual Stud Health Well-being. 2021;16:1–8.10.1080/17482631.2021.1926057Suche in Google Scholar PubMed PubMed Central
[8] Mansfield KE, Sim J, Jordan JL, Jordan KP. A systematic review and meta-analysis of the prevalence of chronic widespread pain in the general population. Pain. 2016;157:55–64.10.1097/j.pain.0000000000000314Suche in Google Scholar PubMed PubMed Central
[9] Abate KH, Abebe Z, Abil OZ, Afshin A, Ahmed MB, Alahdab F, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet (Br Ed). 2018;392:1789–858.Suche in Google Scholar
[10] Nielsen CS. Assessing the societal cost of chronic pain. Scand J Pain. 2022;22:684–5.10.1515/sjpain-2022-0101Suche in Google Scholar PubMed
[11] Steingrímsdóttir ÓA, Landmark T, Macfarlane GJ, Nielsen CS. Defining chronic pain in epidemiological studies: A systematic review and meta-analysis. Pain. 2017;158:2092–107.10.1097/j.pain.0000000000001009Suche in Google Scholar PubMed
[12] Jonsdottir T, Aspelund T, Jonsdottir H, Gunnarsdottir S. The relationship between chronic pain pattern, interference with life and health-related quality of life in a nationwide community sample. Pain Manag Nurs. 2014;15:641–51.10.1016/j.pmn.2013.07.005Suche in Google Scholar PubMed
[13] International Association for the Study of Pain. ISAP announces revised definition of pain. https://www.iasp-pain.org/publications/iasp-news/iasp-announces-revised-definition-of-pain/. Assessed 8 February 2024.Suche in Google Scholar
[14] International Association for the Study of Pain. Definitions of chronic pain syndromes. https://www.iasp-pain.org/advocacy/definitions-of-chronic-pain-syndromes/. Assessed 8 February 2024.Suche in Google Scholar
[15] Fernández-Martínez E, Dolores M, Abreu-Sánchez A, González-Sanz JD, Iglesias-López MT, Fernández-Muñoz JJ, et al. Menstrual migraine among Spanish university students. J Pediatr Nurs. 2021;56:e1–6.10.1016/j.pedn.2020.06.013Suche in Google Scholar PubMed
[16] Del Prado R, García-Arrabé M, González-de-la-Flor Á, De La Plaza San Frutos M, Almazán Polo J, Guérineau F, et al. Exploration of the relationship between primary dysmenorrhea, pain perception, and menstruation-related quality of life in young women: a cross-sectional observational study. Front Glob Womens Health. 2025;6:1521276.10.3389/fgwh.2025.1521276Suche in Google Scholar PubMed PubMed Central
[17] Ayca Ş, Dolgun G. The effect of acupressure on menstrual pain. IJTCM. 2022;3:71–81.10.53811/ijtcmr.1052531Suche in Google Scholar
[18] Allais G, Chiarle G, Sinigaglia S, Benedetto C. Menstrual migraine: A review of current and developing pharmacotherapies for women. Expert Opin Pharmacother. 2018;19:123–36.10.1080/14656566.2017.1414182Suche in Google Scholar PubMed
[19] Leuenberger J, Kohl Schwartz AS, Geraedts K, Haeberlin F, Eberhard M, von Orellie S, et al. Living with endometriosis: Comorbid pain disorders, characteristics of pain and relevance for daily life. Eur J Pain. 2022;26:1021–38.10.1002/ejp.1926Suche in Google Scholar PubMed PubMed Central
[20] Shanshan H, Liying C, Huihong Z, Yanting W, Tiantian L, Tong J, et al. Prevalence of lumbopelvic pain during pregnancy: A systematic review and meta‐analysis of cross‐sectional studies. AOGS. 2024;103:225–40.10.1111/aogs.14714Suche in Google Scholar PubMed PubMed Central
[21] Ozdilek R, Yıldırım M, Aksoy SD, Gul DK. The frequency of back pain, lumbar pain, and pelvic girdle pain during pregnancy. Pain Manag Nurs. 2025;26(4):470–7.10.1016/j.pmn.2025.01.005Suche in Google Scholar PubMed
[22] Gashaw M, Gedlu S, Janakiraman B. Burden of pelvic girdle pain during pregnancy among women attending ante-natal clinic, Ethiopia: A cross-sectional study. https://www.proquest.com/docview/2539308717. Assessed 8 February 2024.Suche in Google Scholar
[23] Persson M, Winkvist A, Dahlgren L, Mogren I. “Struggling with daily life and enduring pain”: A qualitative study of the experiences of pregnant women living with pelvic girdle pain. BMC Pregnancy Childbirth. 2013;13:111.10.1186/1471-2393-13-111Suche in Google Scholar PubMed PubMed Central
[24] Manyozo SD, Nesto T, Bonongwe P, Muula AS. Low back pain during pregnancy: Prevalence, risk factors and association with daily activities among pregnant women in urban Blantyre, Malawi. Malawi Med J. 2019;31:71–6.10.4314/mmj.v31i1.12Suche in Google Scholar PubMed PubMed Central
[25] Andrews P, Steultjens M, Riskowski J. Chronic widespread pain prevalence in the general population: a systematic review. EJP. 2018;22:5–18.10.1002/ejp.1090Suche in Google Scholar PubMed
[26] Othman AJ. The effects of pregnancy and childbirth on women’s health-related quality of life: A scoping review. EBM. 2024;6:39–52.10.47104/ebnrojs3.v6i1.321Suche in Google Scholar
[27] Statistics Iceland. Population - Key figures. https://px.hagstofa.is/pxen/pxweb/en/Ibuar/Ibuar__mannfjoldi__1_yfirlit__yfirlit_mannfjolda/MAN00000.px. Accessed 24 October 2024.10.18356/9789213587744c002Suche in Google Scholar
[28] Statistics Iceland. More than half of women aged 25-64 have university education. https://hagstofa.is/utgafur/frettasafn/menntun/menntunarstada-2022/. Accessed 24 October 2024.Suche in Google Scholar
[29] Directorate of Health. Health and well-being in Iceland: Questionnaire from the electronic survey 2022. https://island.is/en/news/implementation-report-of-the-study-health-and-well-being-in-iceland-2022. Accessed 24 October 2024.Suche in Google Scholar
[30] Cleeland CS, Ryan K. Pain assessment: Global use of the brief pain inventory. Ann Acad Med Singap. 1994;23:129–38.Suche in Google Scholar
[31] Gunnarsdottir S, Ward S, Serlin RC. Attitudinal barriers to cancer pain management in the icelandic population. Cancer Nurs. 2008;31:95–102.10.1097/01.NCC.0000305706.91787.8eSuche in Google Scholar PubMed
[32] Zelman DC, Gore M, Dukes E, Tai K, Brandenburg N. Validation of a modified version of the brief pain inventory for painful diabetic peripheral neuropathy. JPSM. 2005;29:401–10.10.1016/j.jpainsymman.2004.06.018Suche in Google Scholar PubMed
[33] Ware JE, Kosinski M, Keller SD. A 12-item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–33.10.1097/00005650-199603000-00003Suche in Google Scholar PubMed
[34] Hayes CJ, Bhandari NR, Kathe N, Payakachat N. Reliability and validity of the medical outcomes study short form-12 version 2 (SF-12v2) in adults with non-cancer pain. Healthcare. 2017;5:22.10.3390/healthcare5020022Suche in Google Scholar PubMed PubMed Central
[35] Cheak-Zamora NC, Wyrwich KW, McBride TD. Reliability and validity of the SF-12v2 in the medical expenditure panel survey. Qual Life Res. 2009;18:727–35.10.1007/s11136-009-9483-1Suche in Google Scholar PubMed
[36] Montazeri A, Vahdaninia M, Mousavi SJ, Asadi-Lari M, Omidvari S, Tavousi M. The 12-item medical outcomes study short form health survey version 2.0 (SF-12v2): A population-based validation study from Tehran, Iran. HRQOL. 2011;9:12.10.1186/1477-7525-9-12Suche in Google Scholar PubMed PubMed Central
[37] Murray CB, de la Vega R, Murphy LK, Kashikar-Zuck S, Palermo TM. The prevalence of chronic pain in young adults: A systematic review and meta-analysis. Pain. 2022;163:e972–84.10.1097/j.pain.0000000000002541Suche in Google Scholar PubMed
[38] Miller AM, Sanderson K, Bruno RB, Breslin M, Neil AL. Chronic pain, pain severity and analgesia use in Australian women of reproductive age. Women Birth. 2019;32:e272–8.10.1016/j.wombi.2018.06.013Suche in Google Scholar PubMed
[39] Garcia MM, Corrales P, Huerta MÁ, Czachorowski MJ, López-Miranda V, Medina-Gómez G, et al. Adults with excess weight or obesity, but not with overweight, report greater pain intensities than individuals with normal weight: A systematic review and meta-analysis. Front Endocrinol. 2024;15:1340465.10.3389/fendo.2024.1340465Suche in Google Scholar PubMed PubMed Central
[40] Stokes AC, Xie W, Lundberg DJ, Hempstead K, Zajacova A, Zimmer Z, et al. Increases in BMI and chronic pain for US adults in midlife, 1992 to 2016. SSM Popul Health. 2020;12:100644.10.1016/j.ssmph.2020.100644Suche in Google Scholar PubMed PubMed Central
[41] Lee S, Kim JH, Chung JH. The association between sleep quality and quality of life: A population-based study. Sleep Med. 2021;84:121–6.10.1016/j.sleep.2021.05.022Suche in Google Scholar PubMed
[42] Garnaes KK, Mørkved S, Salvesen Ø, Tønne T, Furan L, Grønhaug G, et al. What factors are associated with health‐related quality of life among patients with chronic musculoskeletal pain? A cross‐sectional study in primary health care. BMC Musculoskelet Disord. 2021;22:102–12.10.1186/s12891-020-03914-xSuche in Google Scholar PubMed PubMed Central
© 2025 the author(s), published by De Gruyter
This work is licensed under the Creative Commons Attribution 4.0 International License.
Artikel in diesem Heft
- Editorial Comment
- Abstracts presented at SASP 2025, Reykjavik, Iceland. From the Test Tube to the Clinic – Applying the Science
- Quantitative sensory testing – Quo Vadis?
- Stellate ganglion block for mental disorders – too good to be true?
- When pain meets hope: Case report of a suspended assisted suicide trajectory in phantom limb pain and its broader biopsychosocial implications
- Transcutaneous electrical nerve stimulation – an important tool in person-centered multimodal analgesia
- Clinical Pain Researches
- Exploring the complexities of chronic pain: The ICEPAIN study on prevalence, lifestyle factors, and quality of life in a general population
- The effect of peer group management intervention on chronic pain intensity, number of areas of pain, and pain self-efficacy
- Effects of symbolic function on pain experience and vocational outcome in patients with chronic neck pain referred to the evaluation of surgical intervention: 6-year follow-up
- Experiences of cross-sectoral collaboration between social security service and healthcare service for patients with chronic pain – a qualitative study
- Completion of the PainData questionnaire – A qualitative study of patients’ experiences
- Pain trajectories and exercise-induced pain during 16 weeks of high-load or low-load shoulder exercise in patients with hypermobile shoulders: A secondary analysis of a randomized controlled trial
- Pain intensity in anatomical regions in relation to psychological factors in hypermobile Ehlers–Danlos syndrome
- Opioid use at admittance increases need for intrahospital specialized pain service: Evidence from a registry-based study in four Norwegian university hospitals
- Topically applied novel TRPV1 receptor antagonist, ACD440 Gel, reduces temperature-evoked pain in patients with peripheral neuropathic pain with sensory hypersensitivity, a randomized, double-blind, placebo-controlled, crossover study
- Pain and health-related quality of life among women of childbearing age in Iceland: ICEPAIN, a nationwide survey
- A feasibility study of a co-developed, multidisciplinary, tailored intervention for chronic pain management in municipal healthcare services
- Healthcare utilization and resource distribution before and after interdisciplinary pain rehabilitation in primary care
- Measurement properties of the Swedish Brief Pain Coping Inventory-2 in patients seeking primary care physiotherapy for musculoskeletal pain
- Observational Studies
- Association between clinical laboratory indicators and WOMAC scores in Qatar Biobank participants: The impact of testosterone and fibrinogen on pain, stiffness, and functional limitation
- Well-being in pain questionnaire: A novel, reliable, and valid tool for assessment of the personal well-being in individuals with chronic low back pain
- Properties of pain catastrophizing scale amongst patients with carpal tunnel syndrome – Item response theory analysis
- Adding information on multisite and widespread pain to the STarT back screening tool when identifying low back pain patients at risk of worse prognosis
- The neuromodulation registry survey: A web-based survey to identify and describe characteristics of European medical patient registries for neuromodulation therapies in chronic pain treatment
- Topical Review
- An action plan: The Swedish healthcare pathway for adults with chronic pain
- Systematic Reviews
- Effectiveness of non-invasive vagus nerve stimulation vs heart rate variability biofeedback interventions for chronic pain conditions: A systematic review
- A scoping review of the effectiveness of underwater treadmill exercise in clinical trials of chronic pain
- Neural networks involved in painful diabetic neuropathy: A systematic review
- Original Experimental
- Knowledge, attitudes, and practices of transcutaneous electrical nerve stimulation in perioperative care: A Swedish web-based survey
- Impact of respiration on abdominal pain thresholds in healthy subjects – A pilot study
- Measuring pain intensity in categories through a novel electronic device during experimental cold-induced pain
- Robustness of the cold pressor test: Study across geographic locations on pain perception and tolerance
- Experimental partial-night sleep restriction increases pain sensitivity, but does not alter inflammatory plasma biomarkers
- Educational Case Reports
- Stellate ganglion block in disparate treatment-resistant mental health disorders: A case series
- Regaining the intention to live after relief of intractable phantom limb pain: A case study
- Trigeminal neuralgia caused by dolichoectatic vertebral artery: Reports of two cases
- Short Communications
- Neuroinflammation in chronic pain: Myth or reality?
- The use of registry data to assess clinical hunches: An example from the Swedish quality registry for pain rehabilitation
- Letter to the Editor
- Letter to the Editor For: “Stellate ganglion block in disparate treatment-resistant mental health disorders: A case series”
- Corrigendum
- Corrigendum to “Patient characteristics in relation to opioid exposure in a chronic non-cancer pain population”
Artikel in diesem Heft
- Editorial Comment
- Abstracts presented at SASP 2025, Reykjavik, Iceland. From the Test Tube to the Clinic – Applying the Science
- Quantitative sensory testing – Quo Vadis?
- Stellate ganglion block for mental disorders – too good to be true?
- When pain meets hope: Case report of a suspended assisted suicide trajectory in phantom limb pain and its broader biopsychosocial implications
- Transcutaneous electrical nerve stimulation – an important tool in person-centered multimodal analgesia
- Clinical Pain Researches
- Exploring the complexities of chronic pain: The ICEPAIN study on prevalence, lifestyle factors, and quality of life in a general population
- The effect of peer group management intervention on chronic pain intensity, number of areas of pain, and pain self-efficacy
- Effects of symbolic function on pain experience and vocational outcome in patients with chronic neck pain referred to the evaluation of surgical intervention: 6-year follow-up
- Experiences of cross-sectoral collaboration between social security service and healthcare service for patients with chronic pain – a qualitative study
- Completion of the PainData questionnaire – A qualitative study of patients’ experiences
- Pain trajectories and exercise-induced pain during 16 weeks of high-load or low-load shoulder exercise in patients with hypermobile shoulders: A secondary analysis of a randomized controlled trial
- Pain intensity in anatomical regions in relation to psychological factors in hypermobile Ehlers–Danlos syndrome
- Opioid use at admittance increases need for intrahospital specialized pain service: Evidence from a registry-based study in four Norwegian university hospitals
- Topically applied novel TRPV1 receptor antagonist, ACD440 Gel, reduces temperature-evoked pain in patients with peripheral neuropathic pain with sensory hypersensitivity, a randomized, double-blind, placebo-controlled, crossover study
- Pain and health-related quality of life among women of childbearing age in Iceland: ICEPAIN, a nationwide survey
- A feasibility study of a co-developed, multidisciplinary, tailored intervention for chronic pain management in municipal healthcare services
- Healthcare utilization and resource distribution before and after interdisciplinary pain rehabilitation in primary care
- Measurement properties of the Swedish Brief Pain Coping Inventory-2 in patients seeking primary care physiotherapy for musculoskeletal pain
- Observational Studies
- Association between clinical laboratory indicators and WOMAC scores in Qatar Biobank participants: The impact of testosterone and fibrinogen on pain, stiffness, and functional limitation
- Well-being in pain questionnaire: A novel, reliable, and valid tool for assessment of the personal well-being in individuals with chronic low back pain
- Properties of pain catastrophizing scale amongst patients with carpal tunnel syndrome – Item response theory analysis
- Adding information on multisite and widespread pain to the STarT back screening tool when identifying low back pain patients at risk of worse prognosis
- The neuromodulation registry survey: A web-based survey to identify and describe characteristics of European medical patient registries for neuromodulation therapies in chronic pain treatment
- Topical Review
- An action plan: The Swedish healthcare pathway for adults with chronic pain
- Systematic Reviews
- Effectiveness of non-invasive vagus nerve stimulation vs heart rate variability biofeedback interventions for chronic pain conditions: A systematic review
- A scoping review of the effectiveness of underwater treadmill exercise in clinical trials of chronic pain
- Neural networks involved in painful diabetic neuropathy: A systematic review
- Original Experimental
- Knowledge, attitudes, and practices of transcutaneous electrical nerve stimulation in perioperative care: A Swedish web-based survey
- Impact of respiration on abdominal pain thresholds in healthy subjects – A pilot study
- Measuring pain intensity in categories through a novel electronic device during experimental cold-induced pain
- Robustness of the cold pressor test: Study across geographic locations on pain perception and tolerance
- Experimental partial-night sleep restriction increases pain sensitivity, but does not alter inflammatory plasma biomarkers
- Educational Case Reports
- Stellate ganglion block in disparate treatment-resistant mental health disorders: A case series
- Regaining the intention to live after relief of intractable phantom limb pain: A case study
- Trigeminal neuralgia caused by dolichoectatic vertebral artery: Reports of two cases
- Short Communications
- Neuroinflammation in chronic pain: Myth or reality?
- The use of registry data to assess clinical hunches: An example from the Swedish quality registry for pain rehabilitation
- Letter to the Editor
- Letter to the Editor For: “Stellate ganglion block in disparate treatment-resistant mental health disorders: A case series”
- Corrigendum
- Corrigendum to “Patient characteristics in relation to opioid exposure in a chronic non-cancer pain population”

