Regaining the intention to live after relief of intractable phantom limb pain: A case study
-
Maria Munoz-Novoa
, Joanna EWF van Veldhoven
Abstract
Objectives
Phantom limb pain (PLP) is common after limb amputation and can lead to chronic pain and psychosocial risks, potentially leading to suicide or euthanasia. This study aimed to explore the consequences of intractable PLP on a person’s life before, during, and after receiving phantom motor imagery (PMI) treatment, focusing on the person’s experiences with PMI and how it influenced his life and decision regarding euthanasia.
Methods
This case study focused on a single participant from the PMI treatment group of a PLP randomized clinical trial (RCT). The participant, who joined the RCT as a last resort before euthanasia, experienced decreased PLP during the trial, but the pain returned 1 month post-treatment. Subsequently, the participant initiated self-administered PMI training at home. A mixed quantitative–qualitative method approach was used to analyze this case study.
Results
Understanding and living with PLP was challenging for the participant, making him lose interest in life. Despite starting with low expectations, the participant enjoyed PMI, particularly home training. PLP disappeared during the RCT, returned after therapy cessation, and vanished again during PMI home training. PMI returned his motivation to live, leading him to discontinue his plans for euthanasia.
Conclusions
This case illustrates the severity of chronic PLP, highlighting also the complex interaction of biopsychosocial factors in pain, which can lead a person to consider euthanasia. Representing the first use of PMI in a home setting, this study, along with previous studies in clinical setting, indicates PMI to be a promising and feasible innovative intervention for decreasing PLP, encouraging further research. This study also emphasizes the need to enhance PLP education among clinicians and people with amputations.
1 Introduction
Phantom limb pain (PLP), affecting about 64% of the individuals post-amputation [1], is a neuropathic pain perceived as arising from a missing limb. Chronic PLP, lasting over 3 months [2], often diminishes participation and quality of life in individuals with an amputation [3,4,5] and has been associated with increased anxiety, stress, sleep deficiency, and depression [6,7]. Further, chronic pain more than doubles the odds of suicidal intentions, behaviors, or suicide attempts [8,9,10]. Recent research involving over 44,000 individuals who had undergone leg amputations found that those diagnosed with PLP were significantly more likely to experience psychiatric comorbidities, including suicidal thoughts, depression, and anxiety, compared to those without PLP [11].
In countries like the Netherlands, euthanasia, where a third party administers drugs to end a person’s life at their voluntary and competent request [12,13], is legal for alleviating physical or mental suffering, including chronic pain from conditions like cancer and neuropathic pain [13,14,15,16,17]. Requests for euthanasia in the Netherlands must undergo a comprehensive assessment by an independent End-of-Life (EOL) clinic to evaluate decision-making capacity, rule out treatable psychiatric conditions, confirm that all reasonable treatment options have been exhausted, and include an independent medical consultation from a trained psychiatrist [18,19].
Several treatments for PLP have been explored, but none have definitively and successfully alleviated the various PLP cases [20,21]. Phantom motor execution (PME) is a novel treatment utilizing myoelectric pattern recognition from residual limb muscle signals to control virtual reality (VR) and augmented reality (AR) environments in which serious gaming is employed to promote the movement of the phantom limb [22,23,24]. A multicenter, double-blind, randomized clinical trial (RCT) evaluated PME’s effectiveness in alleviating PLP across eight countries and ten institutions, including The University Medical Center Groningen in the Netherlands (UMCG) [23,25]. The control group was treated with phantom motor imagery (PMI), where participants only imagined the phantom movements while observing them in a VR environment [23,25].
At UMCG, an exceptional case emerged in the PMI group. A participant referred to as “MB” (pseudonym) had experienced intractable chronic PLP for several years following a transfemoral amputation and was already engaged in the formal euthanasia process through an EOL clinic due to the unbearable and untreatable nature of his pain when he chose to join the RCT as a last resort to relieve his suffering. Positive results were observed during the RCT after the training protocol [23]; however, his PLP returned at the 1-month follow-up, and so did his intention to continue the euthanasia process. Considering the seriousness of the case, MB was removed from the RCT, discontinued the follow-up assessment [23], and was given a customized PMI software for independent home training.
In this study, we aimed to explore the severity and daily life consequences of PLP before, during, and after PMI treatment at the clinic and home in a person with chronic PLP. Furthermore, we explored how the PMI treatment influenced this individual’s life and his decision regarding euthanasia.
2 Methods
This mixed-method design included quantitative and qualitative data [26,27]. Quantitative data on PLP and quality of life were collected during the RCT until the 1-month follow-up [23,25] and 6 months and 1 year after the beginning of the PMI home training. Additionally, a semi-structured interview was conducted 6 months after the PMI home training began (Figure 1). The ethical committee of the UMCG approved and provided a waiver prior to the start of the study, as it was not considered clinical research involving human subjects as defined by the Dutch Medical Research Involving Human Subjects Act (file number METc 2021/437). Informed consent was obtained from the participant prior to participation in the PLP RCT study and this case study. This study follows the Consolidated Criteria for Reporting Qualitative Research (COREQ) checklist [28] and Case Report guidelines (CARE) [29].
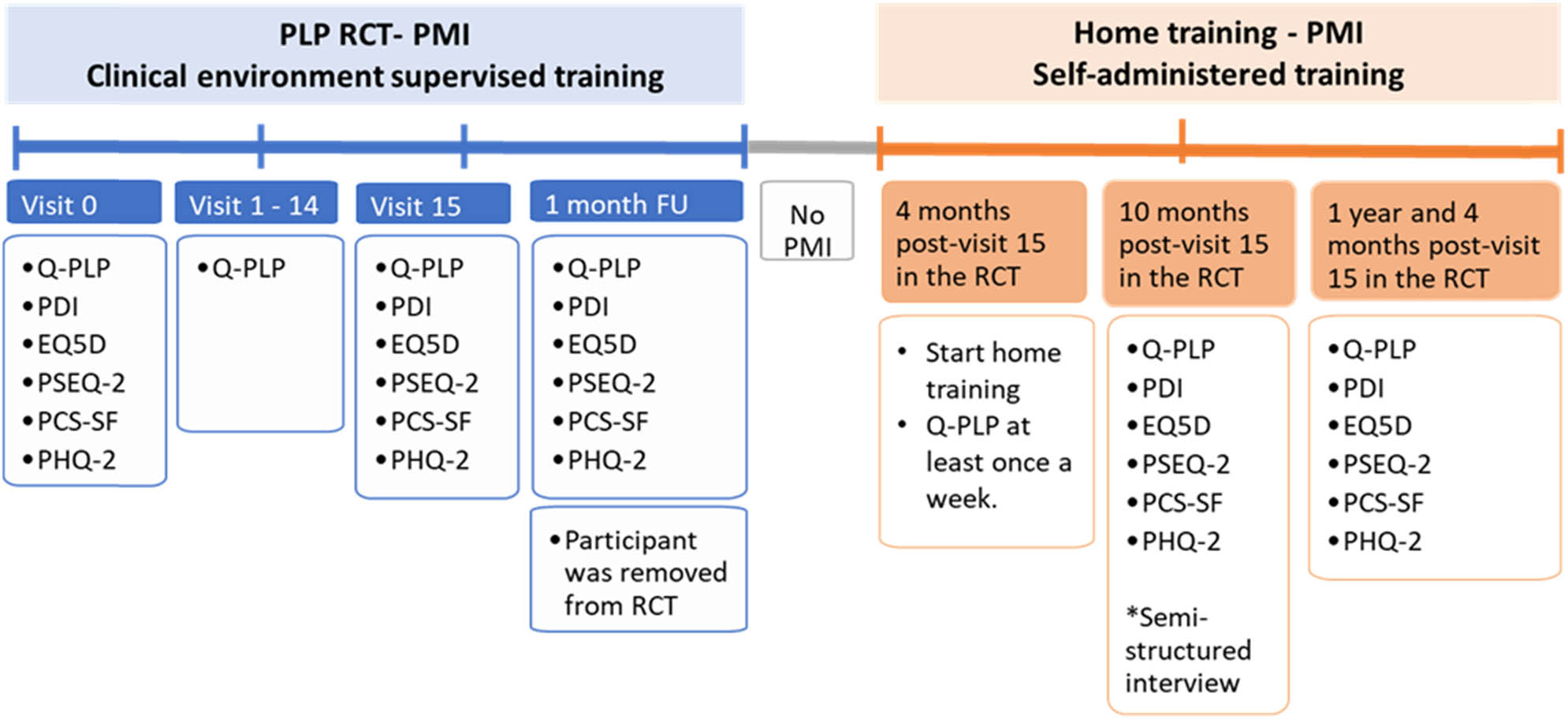
Timeline assessments. Abbreviations: PLP, phantom limb pain; RCT, Randomized Clinical Trial; PMI, phantom motor imagery; Q-PLP, Questionnaire about Phantom Limb Pain; PDI, Pain Disability Index; EQ-5D, European Quality of Life 5 Dimensions; PSEQ-2, Pain Self-Efficacy Questionnaire; PCS-6, Pain Catastrophizing Scale; PHQ-2, Patient Health Questionnaire-2 (PHQ-2); FU; follow-up; m, month.
2.1 Participant
MB, 58 years old at the time of the RCT, suffered from severe PLP after losing his leg above the knee in a traumatic incident in 2011. Over the years, MB tried several treatments such as mirror therapy, transcutaneous electrical stimulation, surgery for neuroma, and high doses of opioids (Fentanyl and Oxycodone). However, none of these treatments successfully relieved his PLP, highlighting its intractability. PLP interfered in all aspects of MB’s life, leading him to seek euthanasia in the Netherlands (his homeland) due to the unbearable suffering. At the time of enrolment in the RCT, MB had already been evaluated and accepted into the euthanasia process through an EOL clinic, and he chose to participate in the trial as a final attempt to alleviate his pain. The clinical and research teams from UMCG, including an experienced physiatrist, confirmed that MP could provide informed consent and to adhere to the study protocol. His medication regimen was stable and met the inclusion criteria for the RCT.
2.2 Intervention
MB underwent two PMI training phases: PMI treatment according to the RCT study protocol until the 1-month follow-up and self-administrated PMI home training, 4 months after the last session of the RCT (Figure 1).
2.2.1 RCT trial, PMI-guided treatment
MB joined the RCT in October 2020. Severe depression or suicidal ideation were not exclusion criteria for joining the RCT, but a thorough pre-study clinical evaluation took place regarding MB’s capability of giving informed consent and being able to comply with the study protocol. Subsequently, MB completed a 15-session protocol twice a week with guidance from a clinician trained in PMI treatment.
PMI consisted of participants imagining moving their phantom limb in synchrony with a virtual limb moving on a computer screen (Figure 2) [23,25]. For those in the control group of the RCT, surface electrodes were applied to monitor EMG activity. If the electrodes detected muscle contractions, the VR program would pause and display a warning message instructing the user to relax and focus solely on imagining the movements. The user must acknowledge this warning to allow the software to resume execution, ensuring adherence to the RCT training protocol [23,25].

PMI training setup during RCT. Upper panel: The patient imagines the movements of his phantom limb based on the movements shown on the screen. Surface electrodes were positioned to ensure that the participant did not engage in actual muscle contractions. If muscular activity was detected, the VR program automatically paused and displayed a warning message, instructing the participant to relax and focus exclusively on motor imagery. Lower panels: The software includes four training steps guiding different degrees of freedom of several phantom movements: VR, target achievement control (TAC), AR, and several serious games. Source: Illustration by Mirka Buist.
2.2.2 Home training, PMI self-administered treatment
Customized PMI software was installed on MB’s computer, where no electrodes or devices were required for its operation. He was instructed to use the software at home and encouraged to train twice weekly for at least 30 min per session, with the freedom to choose the training frequency and movements. As MB was familiar with the PMI software, the researchers only sporadically contacted him to confirm everything was working.
2.3 Data collection
The main outcome was the PLP questionnaire (Q-PLP), built upon the Short-Form McGill Pain Questionnaire, including 16 questions investigating different aspects of PLP [23,25]. MB answered all the questions; however, only three questions from the Q-PLP are presented here, focusing on PLP intensity and PLP interference in sleep and daily life activities, addressing MB’s main complaints (Supplementary 1) [23,30]. Secondary assessments included the Pain Disability Index (PDI) to investigate the self-reported disability associated with pain (0–70 scale, 70 indicating full disability) [31]; Pain Self-Efficacy Questionnaire (PSEQ-2) is a two-item questionnaire assessing pain self-efficacy in people with chronic pain (0–6 score per question, 6 indicating complete confidence) [32]; Pain Catastrophizing Scale – 6 (PCS-6) is a six-item questionnaire measuring catastrophizing thinking in relation to pain experience (0–24 scale, 24 indicating the highest level of catastrophizing) [33,34]; Patient Health Questionnaire-2 (PHQ-2) is a two-item questionnaire investigating the frequency of depressed mood over a time of the past two weeks (0–3 scale, 3 indicating highest probability of depression) [35]; and the EuroQol-5D-5L specifically question 6 (EuroQoL Visual Analogue Scale, 100 indicating the best imaginable health), was chosen to assess the impact of PLP on the participant’s overall health perception [36]. Assessments were performed before, during, and after the RCT and during the home training phase (Figure 1).
A semi-structured interview was conducted at UMCG with MB, with his wife present for additional insights, half a year after starting the home training (Figure 1). The interview was led by a professor (CVDS), who was experienced in qualitative research and observed by a resident of Rehabilitation Medicine (JVV) for whom the qualitative approach was unfamiliar. Neither interacted with the participant during or before the trial. The interview guide was developed in English based on a previous qualitative study conducted during the RCT [37] and translated into Dutch. The interview included questions concerning the participant’s perception of his PLP journey, PLP characteristics and changes over time, the impact of PLP on his life, and PMI experience (Supplementary 2). The interview was conducted in Dutch and was audio-recorded and transcribed verbatim by one of the authors (JVV). The transcription was translated to English (JVV) and reviewed for accuracy (CVDS and SP), anonymized, and securely stored for author access only.
2.4 Data analysis
The semi-structured interview was analyzed using an inductive thematic analysis, following Braun and Clarke's steps [38], with data organized and coded utilizing NVivo 12 software. The steps followed were data familiarization, generating initial codes, searching themes, reviewing themes, and defining and naming themes to finally produce a report [36]. The analysis process involved four authors (MMN, JVV, CVDS, and SP). Two authors (MMN and JVV) independently developed preliminary codes and themes and then reached a consensus to discuss with the rest of the team. Reflexivity was maintained throughout the analysis to minimize bias, and investigator triangulation was used to strengthen the credibility of the findings [39]. To enhance transparency and confirmability [39], quotes from both the participant and his wife were included to illustrate themes and detailed notes were kept throughout the coding process to document how the themes were developed.
Given the mixed methods study design, the quantitative and qualitative results were collectively analyzed.
3 Results
3.1 RCT and home training assessments
3.1.1 Primary outcome
Similar patterns were observed for the Q-PLP questions related to PLP intensity, sleep, and daily life activities (Figure 3). Initially, high PLP interference was seen, gradually decreasing until session 15. At the 1-month follow-up, scores increased, but home training reduced PLP and its impact on daily life to zero, maintaining long-term improvement.
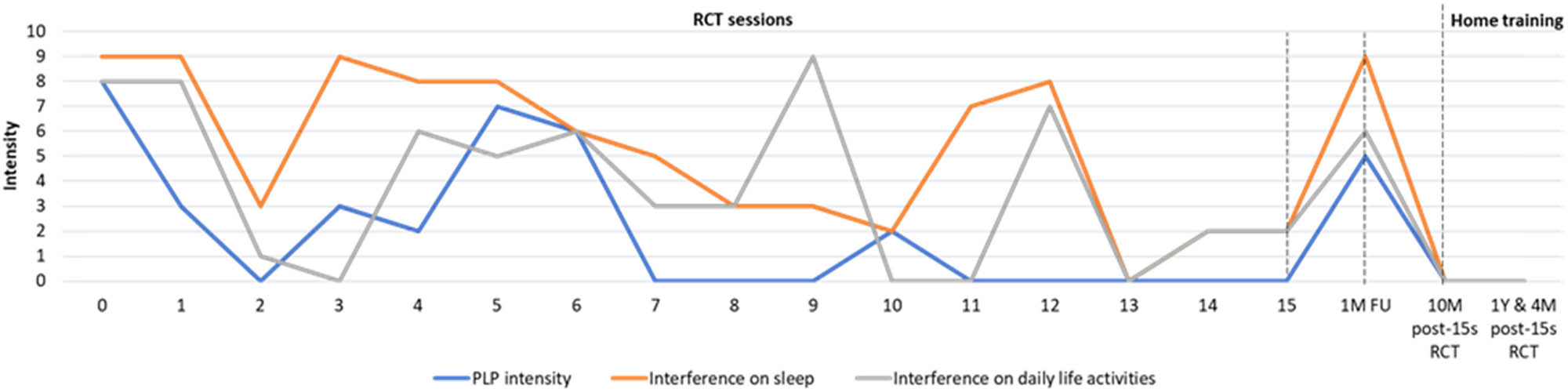
Phantom limb pain questionnaire (Q-PLP). The intensity of PLP, interference with sleep, and daily activities (blue, orange, and gray lines, respectively) are depicted for all treatment sessions during the RCT, the 1-month follow-up assessment, and the home training. Abbreviations: PLP, phantom limb pain; M, months; Y, year, FU, follow-up; s, session; RCT, randomized clinical trial; PMI, phantom motor imagery.
3.1.2 Secondary outcomes
PDI, PCS-6, and PHQ-2 showed similar tendencies across visits (Figure 4a). Fluctuations in scores were observed across phases; however, an overall decreasing trend suggested a reduced impact of PLP following PMI.
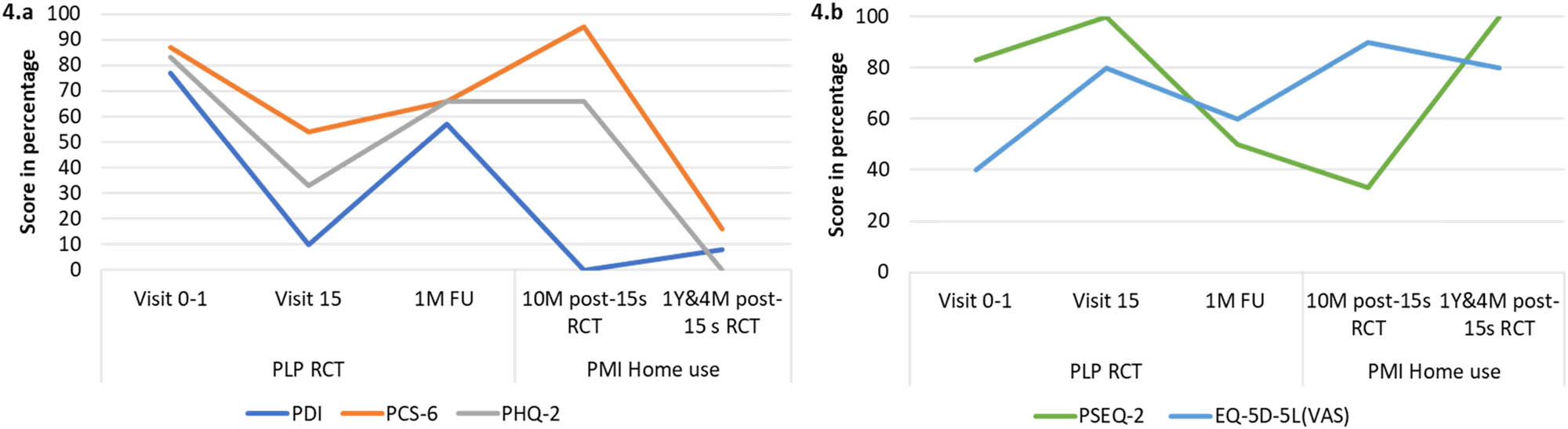
Assessments – secondary outcomes. (a) PDI (blue line), PCS-6 (orange line), and PHQ-2 (gray line) scores as assessed during the RCT, at 1-month follow-up, and during home use: lower scores are better scores. (b) PSEQ-2 (green line) and EQ-5D-5L (blue line) scores as assessed during the RCT, at 1-month follow up and during home use: higher scores are better scores. Abbreviations: Pain Disability Index; PSEQ-2, Pain Self-Efficacy Questionnaire; PCS-6, Pain Catastrophizing Scale – 6; PHQ-2, Patient Health Questionnaire-2; EQ-5D-5L, European Quality of Life 5 Dimensions; q6: question 6; PMI, phantom motor imagery; FU, follow-up; m, months; PLP, phantom limb pain; RCT, randomized clinical trial; VAS, visual analog scale.
PSEQ-2 and EQ-5D-5L (Figure 4b), initially low, increased by over 20 points after session 15. Despite a decline at the 1-month follow-up, scores increased during PMI home training, indicating an overall positive trend and better outcomes.
3.2 Semi-structured interview: 6 months of PMI home training
The interview was conducted in September 2022 and lasted around 90 min. Four main themes were identified.
3.2.1 PLP understanding
Before amputation, MB did not know about PLP and could not have imagined such pain existed. After the amputation, he received unclear explanations about PLP and was told it might disappear. It was hard for MB and the people around him to understand PLP. The first time he perceived to fully comprehend PLP was during the RCT.
At a certain moment you think that you yourself are not completely normal. How can you get pain in something that is no longer there. And if you undergo such a treatment here, you will look at it differently. Especially because then the pain disappears in between [treatments] and you can handle it better.
3.2.2 Experiences of PLP and PMI over time
3.2.2.1 PLP before PMI
The participant’s PLP was constant and got worse over the years. The most unbearable pain episodes occurred at night, limiting his sleep to 2–3 h, and the highest pain was in the phantom foot and toes. MB and his wife described PLP had transformed him into a different person, one with a bad temper, tiredness, depression, desperation, and low tolerance to everyday circumstances. The PLP also robbed him of enjoyment in hobbies and social contact.
I’m not a guy who easily cries, but at some point, I was done with it. I say um, I want, I won’t go on like this. It’s for me, it’s enough. Then I entered that euthanasia process, yes then this came on my way.
3.2.2.2 PMI hospital treatment – RCT
MB had initially low expectations about PMI, but his attitude shifted positively as his pain decreased. PMI was the first intervention to positively impact his PLP. As facilitators, MB highlighted the therapist’s good disposition and understanding, well-organized training, and the non-invasive nature of the intervention. Factors he considered contributing to the treatment’s success were also presenting a positive attitude towards the training and good training adherence. The barriers he described were difficulty concentrating due to noise and distractions, long travel time to the hospital, exhausting sessions, and discomfort with the uncertainty of the treatment results.
Well, the first two times, I thought, why should I do this. But um, the third or fourth time it went a lot better. I didn’t have any problems at night either. And, yes, I have to say that I loved doing it. A lot of pain was gone after the treatment.
3.2.2.3 PMI software at home
During the home training, MB described his PLP progressively disappearing, allowing him to sleep 6–7 h at night, feel more energetic, have positive thoughts, and reconnect to his hobbies and loved ones. Another benefit was that he completely stopped taking pain-relieving medication, regaining control over his life.
MB preferred to train at home than at the hospital because he could concentrate better, felt less pressure, and appreciated the flexibility in his training schedule. Moreover, he enjoyed using the software and found it easy to use. His goal was to gradually decrease the training frequency while maintaining consistency to prevent relapse, emphasizing the importance of discipline for success. He considered home training an effective approach that could be implemented for other PLP cases. MB and his wife were happy and satisfied with the home training outcomes.
[Achieving the treatment goal:] 99 percent achieved. I thought when I continue with that [PMI training] at home, my goal would be to become free of pain and, yes, I succeeded.
3.2.3 Phantom limb movements and PMI
Before PMI, MB was unable to move his phantom. During the training, imagining the different movements felt intuitive, but it still required mental effort and concentration. MB described visual feedback on the computer screen made it easier to recall and imagine the phantom's movements and imagining the phantom as part of himself created a stronger connection with his phantom. During the treatment, he vividly felt his leg with the same shape, size, and height as his non-affected limb, which was a new experience for him. Gaining control of his phantom took some time, but once achieved, he felt a decrease in his PLP. MB believed controlling his phantom, especially the toes, was crucial for the treatment's success.
When I started the treatment, I did get more control. For a long time, I couldn’t move my toes. I’ve been practicing on that. It took about 6 weeks before I could do something with my toes. Now I can do it at home, that’s not much of a problem. And when the phantom is there, I can twist my ankle, and I can do anything with it.
3.2.4 Euthanasia
Although his PLP decreased considerably during the PMI hospital treatment, MB did not cancel the euthanasia process, wanting to ensure the effect was lasting. During the home training, his PLP vanished, and he felt “reborn” and a “new man,” eager to embrace life and create future plans. His wife also reported that PMI brought hope and happiness to their home. At the 1-year follow-up, after several months of treatment and PLP gone, MB mentioned having no more thoughts about euthanasia.
Became a different person, yes. Otherwise, I wouldn’t be here anymore. If this [PMI treatment] hadn’t crossed my path, I wouldn’t be here anymore.
3.3 Mixed data
Quantitative and qualitative data closely aligned, showing that pain intensity fluctuated with and without PMI, impacting the participant’s behavior. MB’s description of a “pain-free life” after PMI home training matched Q-PLP results. Yet, the semi-structured interview revealed the intensity of his PLP experience, including thoughts of euthanasia, which Q-PLP scores did not fully capture. Secondary outcomes showed the participant’s initial depression, disability, and reduced quality of life due to PLP, though they did not reflect MB's full desperation. Together, quantitative and qualitative analyses demonstrated that PMI reduced pain and improved quality of life, providing a comprehensive view of the case.
4 Discussion
This mixed-method study exemplifies how complex, severe, and chronic PLP can be, leading a person to even consider ending their life to conclude their suffering. In this case study, PMI was the first intervention to alleviate the participant’s chronic PLP, first in a clinical setting and then in a home setting, after several years of unsuccessful treatments. This reduction in PLP had a positive impact on all aspects of the participant’s life, especially on sleep and daily activities, which are common aspects disrupted due to PLP. While this is an extraordinary case, further and more extensive research is needed to investigate the effectiveness of PMI and explore solutions for the unresolved PLP cases.
PLP is a complex and poorly understood condition [22,40], making PLP difficult for people with amputation and clinicians to comprehend, manage, and treat [41,42]. A study investigating healthcare professionals’ views on PLP indicated that only a few professionals felt they fully understood PLP, leading to inconsistent and insufficient patient information [42]. Similarly, people with amputation consider that PLP is not always accurately explained by clinicians, stressing the need for early education after amputation [41]. The present study is an example of this fact, in which the participant struggled to understand his PLP for more than 9 years (until the RCT). Understanding and contextualizing chronic pain through psychoeducation has been shown to reduce pain-related distress, enhance coping with pain, and decrease pain catastrophizing [43,44,45]. In the context of PLP, where the affected limb is not visible, education that includes an explanation of the neurophysiological mechanisms of pain may help individuals make sense of their experience and feel less isolated. Furthermore, the therapeutic relationship and empathetic understanding from clinicians have been shown to positively influence treatment outcomes in chronic pain by promoting trust, validation, and adherence to self-management strategies [46,47]. This was evident in the present study, where the participant reported a positive experience with the therapist’s supportive and understanding approach during the PMI training conducted at the hospital. These findings emphasize the need to enhance PLP-related education for both clinicians and individuals with amputations.
This case study demonstrates the profound and multidimensional impact PLP could have on an individual’s life, affecting biological, psychological, and social factors [48]. As seen in this case, PLP can create a persistent, negative cycle of chronic pain, emotional distress, and social isolation so severe that it can lead a person to consider euthanasia as a means of escaping the suffering. In this unique case, PMI helps disrupt this negative loop, leading to significant improvements across all aspects of the individual’s life and restoring their will to live. However, it is important to emphasize that this is an exceptional case. While the outcome was undoubtedly positive, the findings must be interpreted with caution and within the ethical and contextual boundaries of a single-case design. Such an individual experience may not be generalizable to all persons suffering from PLP or experiencing suicidal ideation due to chronic pain. The participant’s decision to discontinue the euthanasia process was personal and shaped by his biopsychosocial context. Still, while this case cannot serve as a broadly applicable clinical precedent, it offers valuable insights into the multidimensional factors that must be considered when treating PLP.
This case study is the first to incorporate PMI at home, showing it is a feasible self-administered intervention and may lead to a long-lasting reduction in PLP. The participant described enjoying the training at home more than in the clinic, appreciating the flexibility in the training schedule, the absence of commuting, improved concentration, and reduced pressure, indicating the potential benefits PMI could offer in a home environment. A previous study on PME home use also indicated to be a feasible intervention, however, with variable adherence due to challenges like electrode placement and system complexity [49]. In contrast, PMI for home use does not require electrodes or hardware, simplifying the process, reducing complications, eliminating the need for clinical assistance, and lowering costs. Hence, this case study shows that PMI appears as an enjoyable, practical, and cost-effective home solution. Its potential for high adherence and long-term use makes it a promising intervention for reducing PLP. However, further research is necessary to investigate these outcomes and better understand their long-term effects.
After amputation, people often feel their phantom limbs are immovable [19,36]. PMI seemed to have enabled the participant to move his phantom limb. The participant perceived a direct relation between control of the phantom movements and pain reduction, especially when mastering distal joint movements. This is consistent with preliminary evidence showing an inversed correlation between phantom limb movement and PLP [22,50,51]. These findings suggest that people with an amputation might benefit from trying to keep their phantom limbs mobile to prevent or reduce PLP [50,51].
Further research is needed to investigate PMI’s effectiveness and its relation to PLP reduction [22]. However, as noted by the participant in this case study, visual feedback seems to play a crucial role in imagining phantom movements. Previous evidence suggests that combining action observation (watching a movement) with imagination enhances motor-related brain activity more effectively than either activity alone [52,53,54,55]. Another element described by the participant was the relationship between an increased sense of ownership of the phantom and a reduction in PLP, which is consistent with previous studies showing that greater prosthesis ownership is related to lower PLP [56]. Although this single case provides valuable experiential insights, it does not allow for definitive conclusions about the underlying neurophysiological mechanisms of PMI, nor on the role of non-specific effects (education, bonding with therapists, etc.), and so discussion of potential processes should be considered exploratory and should be investigated further in future research.
This study’s strength lies in its combination of quantitative and qualitative data, providing a comprehensive overview of the case. Qualitative data collection and analysis were performed by independent researchers not involved in the intervention, ensuring the trustworthiness of the findings through triangulation and consensus among researchers [57]. A limitation of this study is that data represent only one case, which may not represent all people suffering from PLP. Additionally, the absence of long-term follow-up limits the extent to which the durability of the restored will to live can be evaluated.
5 Conclusion
This study shows that PLP can be chronic and severe enough to lead someone to pursue euthanasia. PMI appeared to be a promising intervention to decrease PLP, and in this particular case, it motivated the discontinuation of the euthanasia process and restored the will to live in a person with chronic PLP. The findings suggest PMI is also a feasible and enjoyable intervention for home and self-administered training, leading to long-term PLP reduction. This study encourages further investigation of PMI in home and clinical settings, and its effect on chronic PLP. Furthermore, the study highlights the importance of qualitative research to deepen the understanding of PLP and emphasizes the need for enhanced PLP education among clinicians and people with amputation.
Acknowledgments
We sincerely thank the participant and his wife for actively participating in the study and generously sharing their personal and challenging experiences with PLP. Additionally, we thank Mirka Buist for her valuable collaboration in creating the figures.
-
Research ethics: The UMCG ethical committee approved the study and granted a waiver (file METc 2021/437).
-
Informed consent: Informed consent was obtained from the participant prior to participation in the PLP RCT study, and this case study.
-
Author contributions: All authors have contributed substantially, reviewed, and approved the manuscript.
-
Competing interests: MBK, MMN, and MOC consulted for Integrum AB during the execution of this study.
-
Research funding: This work was supported by the Promobilia Foundation (19500).
-
Data availability: Not applicable.
-
Artificial intelligence/machine learning tools: Not applicable.
-
Supplementary material: This article contains supplementary material (followed by the link to the article online).
References
[1] Limakatso K, Bedwell GJ, Madden VJ, Parker R. The prevalence and risk factors for phantom limb pain in people with amputations: A systematic review and meta-analysis. PLoS One. 2020;15(10):e0240431.10.1371/journal.pone.0240431Search in Google Scholar PubMed PubMed Central
[2] Treede RD, Rief W, Barke A, Aziz Q, Bennett MI, Benoliel R, et al. A classification of chronic pain for ICD-11. Pain. 2015;156(6):1003–7.10.1097/j.pain.0000000000000160Search in Google Scholar PubMed PubMed Central
[3] Schug SA, Lavand’homme P, Barke A, Korwisi B, Rief W, Treede RD, et al. The IASP classification of chronic pain for ICD-11: Chronic postsurgical or posttraumatic pain. Pain. 2019;160(1):45–52.10.1097/j.pain.0000000000001413Search in Google Scholar PubMed
[4] van der Schans CP, Geertzen JH, Schoppen T, Dijkstra PU. Phantom pain and health-related quality of life in lower limb amputees. Pain Symptom Manage. 2002;24(4):429–36.10.1016/S0885-3924(02)00511-0Search in Google Scholar PubMed
[5] Bosmans JC, Suurmeijer TP, Hulsink M, van der Schans CP, Geertzen JH, Dijkstra PU. Amputation, phantom pain and subjective well-being: A qualitative study. Int J Rehabil Res. 2007;30(1):1–8.10.1097/MRR.0b013e328012c953Search in Google Scholar PubMed
[6] Polat CS, Konak HE, Altas EU, Akinci MG, S. Onat S. Factors related to phantom limb pain and its effect on quality of life. Somatosens Mot Res. 2021;38(4):322–6.10.1080/08990220.2021.1973405Search in Google Scholar PubMed
[7] Padovani MT, Martins MR, Venancio A, Forni JE. Anxiety, depression and quality of life in individuals with phantom limb pain. Acta Ortop Bras. 2015;23(2):107–10.10.1590/1413-78522015230200990Search in Google Scholar PubMed PubMed Central
[8] Racine M. Chronic pain and suicide risk: A comprehensive review. Prog Neuropsychopharmacol Biol Psychiatry. 2018;87(Pt B):269–80.10.1016/j.pnpbp.2017.08.020Search in Google Scholar PubMed
[9] Fine P. Long-term consequences of chronic pain: Mounting evidence for pain as a neurological disease and parallels with other chronic disease states. Pain Med. 2011;12(7):996–1004.10.1111/j.1526-4637.2011.01187.xSearch in Google Scholar PubMed
[10] Fishbain DA, Cutler R, Rosomoff HL, Rosomoff RS. Chronic pain-associated depression: Antecedent or consequence of chronic pain? A review. Clin J Pain. 1997;13(2):116–37.10.1097/00002508-199706000-00006Search in Google Scholar PubMed
[11] Hogan WB, Anderson G, Kovoor M, Alsoof D, McDonald CL, Zhang AS, et al. Phantom limb syndrome: Assessment of psychiatric and medical comorbidities associated with Phantom pain in 44,028 below knee amputees. Injury. 2022;53(11):3697–701.10.1016/j.injury.2022.09.018Search in Google Scholar PubMed
[12] Pereira J. Legalizing euthanasia or assisted suicide: the illusion of safeguards and controls. Curr Oncol. 2011;18(2):e38–45.10.3747/co.v18i2.883Search in Google Scholar PubMed PubMed Central
[13] Foley KM. Pain, physician-assisted suicide, and euthanasia. Pain Forum. 1995;4(3):163–78.10.1016/S1082-3174(11)80050-4Search in Google Scholar
[14] Mroz S, Dierickx S, Deliens L, Cohen J, Chambaere K. Assisted dying around the world: A status quaestionis. Ann Palliat Med. 2021;10(3):3540–53.10.21037/apm-20-637Search in Google Scholar PubMed
[15] Steck N, Egger M, Maessen M, Reisch T, Zwahlen M. Euthanasia and assisted suicide in selected European countries and US states: Systematic literature review. Med Care. 2013;51(10):938–44.10.1097/MLR.0b013e3182a0f427Search in Google Scholar PubMed
[16] Groenewoud AS, Atsma F, Arvin M, Westert GP, Boer TA. Euthanasia in the Netherlands: A claims data cross-sectional study of geographical variation. BMJ Support Palliat Care. 2021;11(1):e1.10.1136/bmjspcare-2020-002573Search in Google Scholar PubMed
[17] Kouwenhoven PS, van Thiel GJ, Raijmakers NJ, Rietjens JA, van der Heide A, van Delden JJ. Euthanasia or physician-assisted suicide? A survey from the Netherlands. Eur J Gen Pract. 2014;20(1):25–31.10.3109/13814788.2013.813014Search in Google Scholar PubMed
[18] Rietjens JA, van der Maas PJ, Onwuteaka-Philipsen BD, van Delden JJ, van der Heide A. Two decades of research on euthanasia from the Netherlands. What have we learnt and what questions remain? J Bioeth Inq. 2009;6(3):271–83.10.1007/s11673-009-9172-3Search in Google Scholar PubMed PubMed Central
[19] Kimsma GK. Death by request in The Netherlands: Facts, the legal context and effects on physicians, patients and families. Med Health Care Philos. 2010;13(4):355–61.10.1007/s11019-010-9265-0Search in Google Scholar PubMed PubMed Central
[20] Subedi B, Grossberg GT. Phantom limb pain: Mechanisms and treatment approaches. Pain Res Treat. 2011;2011:864605.10.1155/2011/864605Search in Google Scholar PubMed PubMed Central
[21] Collins KL, Russell HG, Schumacher PJ, Robinson-Freeman KE, O’Conor EC, Gibney KD, et al. A review of current theories and treatments for phantom limb pain. J Clin Invest. 2018;128(6):2168–76.10.1172/JCI94003Search in Google Scholar PubMed PubMed Central
[22] Ortiz-Catalan M. The stochastic entanglement and phantom motor execution hypotheses: A theoretical framework for the origin and treatment of Phantom limb pain. Front Neural. 2018;9:748.10.3389/fneur.2018.00748Search in Google Scholar PubMed PubMed Central
[23] Lendaro E, Hermansson L, Burger H, Van der Sluis CK, McGuire BE, Pilch M, et al. Phantom motor execution as a treatment for phantom limb pain: protocol of an international, double-blind, randomised controlled clinical trial. BMJ Open. 2018;8(7):e021039. 10.1136/bmjopen-2017-021039Search in Google Scholar PubMed PubMed Central
[24] Ortiz-Catalan M, Guethmundsdottir RA, Kristoffersen MB, Zepeda-Echavarria A, Caine-Winterberger K, Kulbacka-Ortiz K, et al. Phantom motor execution facilitated by machine learning and augmented reality as treatment for phantom limb pain: a single group, clinical trial in patients with chronic intractable phantom limb pain. Lancet. 2016;388(10062):2885–94.10.1016/S0140-6736(16)31598-7Search in Google Scholar PubMed
[25] Lendaro E, Van der Sluis CK, Hermansson L, Bunketorp-Kall L, Burger H, Keesom E, et al. Extended reality used in the treatment of phantom limb pain: a multicenter, double-blind, randomized controlled trial. Pain. 2024;166(3):571–86.10.1097/j.pain.0000000000003384Search in Google Scholar PubMed PubMed Central
[26] Lee S, Smith CA. Criteria for quantitative and qualitative data integration: mixed-methods research methodology. Comput Inf Nurs. 2012;30(5):251–6.10.1097/NXN.0b013e31824b1f96Search in Google Scholar PubMed
[27] Schoonenboom J, Johnson RB. How to construct a mixed methods research design. Kolner Z Soz Sozpsychol. 2017;69(Suppl 2):107–31.10.1007/s11577-017-0454-1Search in Google Scholar PubMed PubMed Central
[28] Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57.10.1093/intqhc/mzm042Search in Google Scholar PubMed
[29] Gagnier JJ, Kienle G, Altman DG, Moher D, Sox H, Riley D, et al. The CARE guidelines: Consensus-based clinical case reporting guideline development. Glob Adv Health Med. 2013;2(5):38–43.10.7453/gahmj.2013.008Search in Google Scholar PubMed PubMed Central
[30] Melzack R. The short-form McGill pain questionnaire. Pain. 1987;30(2):191–7.10.1016/0304-3959(87)91074-8Search in Google Scholar PubMed
[31] Pollard CA. Preliminary validity study of the pain disability index. Percept Mot Skills. 984;59(3):974.10.2466/pms.1984.59.3.974Search in Google Scholar PubMed
[32] Nicholas MK, McGuire BE, Asghari A. A 2-item short form of the pain self-efficacy questionnaire: Development and psychometric evaluation of PSEQ-2. J Pain. 2015;16(2):153–63.10.1016/j.jpain.2014.11.002Search in Google Scholar PubMed
[33] McWilliams LA, Kowal J, Wilson KG. Development and evaluation of short forms of the pain catastrophizing scale and the pain self-efficacy questionnaire. Eur J Pain. 2015;19(9):1342–9.10.1002/ejp.665Search in Google Scholar PubMed
[34] Darnall BD, Sturgeon JA, Cook KF, Taub CJ, Roy A, Burns JW, et al. Development and validation of a daily pain catastrophizing scale. J Pain. 2017;18(9):1139–49.10.1016/j.jpain.2017.05.003Search in Google Scholar PubMed PubMed Central
[35] Kroenke KSR, Williams JB. The patient health questionnaire-2: Validity of a two-item depression screener. Med Care. 2003;41(11):1284–92.10.1097/01.MLR.0000093487.78664.3CSearch in Google Scholar PubMed
[36] Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res. 2011;20(10):1727–36.10.1007/s11136-011-9903-xSearch in Google Scholar PubMed PubMed Central
[37] Pilch M, van Rietschoten T, Ortiz-Catalan M, Lendaro E, van der Sluis CK, Hermansson L. Interplay between innovation and intersubjectivity: Therapists perceptions of phantom motor execution therapy and its effect on phantom limb pain. J Pain Res. 2023;16:2747–61.10.2147/JPR.S412895Search in Google Scholar PubMed PubMed Central
[38] Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.10.1191/1478088706qp063oaSearch in Google Scholar
[39] Malterud K. Qualitative research: Standards, challenges, and guidelines. Lancet. 2001;358(9280):483–8.10.1016/S0140-6736(01)05627-6Search in Google Scholar PubMed
[40] Schone HR, Baker CI, Katz J, Nikolajsen L, Limakatso K, Flor H, et al. Making sense of phantom limb pain. J Neurol Neurosurg Psychiatry. 2022;93(8):833–43.10.1136/jnnp-2021-328428Search in Google Scholar PubMed PubMed Central
[41] Mortimer CM, Steedman WM, McMillan IR, Martin DJ, Ravey J. Patient information on phantom limb pain: A focus group study of patient experiences, perceptions and opinions. Health Educ Res. 2002;17(3):291–304.10.1093/her/17.3.291Search in Google Scholar PubMed
[42] Mortimer CM, MacDonald RJ, Martin DJ, McMillan IR, Ravey J, Steedman WM. A focus group study of health professionals’ views on phantom sensation, phantom pain and the need for patient information. Patient Educ Couns. 2004;54(2):221–6.10.1016/S0738-3991(03)00237-4Search in Google Scholar PubMed
[43] Moseley GL, Butler DS. Fifteen years of explaining pain: The past, present, and future. J Pain. 2015;16(9):807–13.10.1016/j.jpain.2015.05.005Search in Google Scholar PubMed
[44] Zahari ZIA, Justine M. The effectiveness of patient education in improving pain, disability and quality of life among older people with low back pain: A systematic review. J Back Musculoskelet Rehabil. 2020;33(4):625–37.10.3233/BMR-181305Search in Google Scholar PubMed
[45] Watson JA, Ryan CG, Cooper L, Ellington D, Whittle R, Lavender M, et al. Pain neuroscience education for adults with chronic musculoskeletal pain: A mixed-methods systematic review and meta-analysis. J Pain. 2019;20(10):1140 e1–e22.10.1016/j.jpain.2019.02.011Search in Google Scholar PubMed
[46] Fuentes J, Armijo-Olivo S, Funabashi M, Miciak M, Dick B, Warren S, et al. Enhanced therapeutic alliance modulates pain intensity and muscle pain sensitivity in patients with chronic low back pain: an experimental controlled study. Phys Ther. 2014;94(4):477–89.10.2522/ptj.20130118Search in Google Scholar PubMed
[47] Hall AM, Ferreira PH, Maher CG, Latimer J, Ferreira ML. The influence of the therapist-patient relationship on treatment outcome in physical rehabilitation: A systematic review. Phys Ther. 2010;90(8):1099–110.10.2522/ptj.20090245Search in Google Scholar PubMed
[48] Hanley MA, Jensen MP, Ehde DM, Hoffman AJ, Patterson DR, Robinson LR. Psychosocial predictors of long-term adjustment to lower-limb amputation and phantom limb pain. Disabil Rehabil. 2004;26(14–15):882–93.10.1080/09638280410001708896Search in Google Scholar PubMed
[49] Lendaro E, Middleton A, Brown S, Ortiz-Catalan M. Out of the clinic, into the home: The in-home use of phantom motor execution aided by machine learning and augmented reality for the treatment of phantom limb pain. J Pain Res. 2020;13:195–209.10.2147/JPR.S220160Search in Google Scholar PubMed PubMed Central
[50] Raffin E, Richard N, Giraux P, Reilly KT. Primary motor cortex changes after amputation correlate with phantom limb pain and the ability to move the phantom limb. Neuroimage. 2016;130:134–44.10.1016/j.neuroimage.2016.01.063Search in Google Scholar PubMed
[51] Ramachandran VS, Rogers-Ramachandran D. Synaesthesia in phantom limbs induced with mirrors. Brain and Perception Laboratory 0109, University of California, San Diego, La Jolla, California 92093, USA; 1997.Search in Google Scholar
[52] Mulder T. Motor imagery and action observation: Cognitive tools for rehabilitation. J Neural Transm (Vienna). 2007;114(10):1265–78.10.1007/s00702-007-0763-zSearch in Google Scholar PubMed PubMed Central
[53] Eaves DL, Riach M, Holmes PS, Wright DJ. Motor imagery during action observation: A brief review of evidence, theory and future research opportunities. Front Neurosci. 2016;10:514.10.3389/fnins.2016.00514Search in Google Scholar PubMed PubMed Central
[54] Bolognini N, Olgiati E, Maravita A, Ferraro F, Fregni F. Motor and parietal cortex stimulation for phantom limb pain and sensations. Pain. 2013;154(8):1274–80.10.1016/j.pain.2013.03.040Search in Google Scholar PubMed
[55] Ziegler K, Folkard R, Gonzalez AJ, Burghardt J, Antharvedi-Goda S, Martin-Cortecero J, et al. Primary somatosensory cortex bidirectionally modulates sensory gain and nociceptive behavior in a layer-specific manner. Nat Commun. 2023;14(1):2999.10.1038/s41467-023-38798-7Search in Google Scholar PubMed PubMed Central
[56] Bekrater-Bodmann R, Reinhard I, Diers M, Fuchs X, Flor H. Relationship of prosthesis ownership and phantom limb pain: Results of a survey in 2383 limb amputees. Pain. 2021;162(2):630–40.10.1097/j.pain.0000000000002063Search in Google Scholar PubMed
[57] Nowell LS, Norris JM, White DE, Moules NJ. Thematic analysis: Striving to meet the trustworthiness criteria. Int J Qual Methods. 2017;16(1):1–13.10.1177/1609406917733847Search in Google Scholar
© 2025 the author(s), published by De Gruyter
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Editorial Comment
- Abstracts presented at SASP 2025, Reykjavik, Iceland. From the Test Tube to the Clinic – Applying the Science
- Quantitative sensory testing – Quo Vadis?
- Stellate ganglion block for mental disorders – too good to be true?
- When pain meets hope: Case report of a suspended assisted suicide trajectory in phantom limb pain and its broader biopsychosocial implications
- Transcutaneous electrical nerve stimulation – an important tool in person-centered multimodal analgesia
- Clinical Pain Researches
- Exploring the complexities of chronic pain: The ICEPAIN study on prevalence, lifestyle factors, and quality of life in a general population
- The effect of peer group management intervention on chronic pain intensity, number of areas of pain, and pain self-efficacy
- Effects of symbolic function on pain experience and vocational outcome in patients with chronic neck pain referred to the evaluation of surgical intervention: 6-year follow-up
- Experiences of cross-sectoral collaboration between social security service and healthcare service for patients with chronic pain – a qualitative study
- Completion of the PainData questionnaire – A qualitative study of patients’ experiences
- Pain trajectories and exercise-induced pain during 16 weeks of high-load or low-load shoulder exercise in patients with hypermobile shoulders: A secondary analysis of a randomized controlled trial
- Pain intensity in anatomical regions in relation to psychological factors in hypermobile Ehlers–Danlos syndrome
- Opioid use at admittance increases need for intrahospital specialized pain service: Evidence from a registry-based study in four Norwegian university hospitals
- Topically applied novel TRPV1 receptor antagonist, ACD440 Gel, reduces temperature-evoked pain in patients with peripheral neuropathic pain with sensory hypersensitivity, a randomized, double-blind, placebo-controlled, crossover study
- Pain and health-related quality of life among women of childbearing age in Iceland: ICEPAIN, a nationwide survey
- A feasibility study of a co-developed, multidisciplinary, tailored intervention for chronic pain management in municipal healthcare services
- Healthcare utilization and resource distribution before and after interdisciplinary pain rehabilitation in primary care
- Measurement properties of the Swedish Brief Pain Coping Inventory-2 in patients seeking primary care physiotherapy for musculoskeletal pain
- Understanding the experiences of Canadian military veterans participating in aquatic exercise for musculoskeletal pain
- “There is generally no focus on my pain from the healthcare staff”: A qualitative study exploring the perspective of patients with Parkinson’s disease
- Observational Studies
- Association between clinical laboratory indicators and WOMAC scores in Qatar Biobank participants: The impact of testosterone and fibrinogen on pain, stiffness, and functional limitation
- Well-being in pain questionnaire: A novel, reliable, and valid tool for assessment of the personal well-being in individuals with chronic low back pain
- Properties of pain catastrophizing scale amongst patients with carpal tunnel syndrome – Item response theory analysis
- Adding information on multisite and widespread pain to the STarT back screening tool when identifying low back pain patients at risk of worse prognosis
- The neuromodulation registry survey: A web-based survey to identify and describe characteristics of European medical patient registries for neuromodulation therapies in chronic pain treatment
- A biopsychosocial content analysis of Dutch rehabilitation and anaesthesiology websites for patients with non-specific neck, back, and chronic pain
- Topical Reviews
- An action plan: The Swedish healthcare pathway for adults with chronic pain
- Team-based rehabilitation in primary care for patients with musculoskeletal disorders: Experiences, effect, and process evaluation. A PhD synopsis
- Persistent severe pain following groin hernia repair: Somatosensory profiles, pain trajectories, and clinical outcomes – Synopsis of a PhD thesis
- Systematic Reviews
- Effectiveness of non-invasive vagus nerve stimulation vs heart rate variability biofeedback interventions for chronic pain conditions: A systematic review
- A scoping review of the effectiveness of underwater treadmill exercise in clinical trials of chronic pain
- Neural networks involved in painful diabetic neuropathy: A systematic review
- Original Experimental
- Knowledge, attitudes, and practices of transcutaneous electrical nerve stimulation in perioperative care: A Swedish web-based survey
- Impact of respiration on abdominal pain thresholds in healthy subjects – A pilot study
- Measuring pain intensity in categories through a novel electronic device during experimental cold-induced pain
- Robustness of the cold pressor test: Study across geographic locations on pain perception and tolerance
- Experimental partial-night sleep restriction increases pain sensitivity, but does not alter inflammatory plasma biomarkers
- Is it personality or genes? – A secondary analysis on a randomized controlled trial investigating responsiveness to placebo analgesia
- Investigation of endocannabinoids in plasma and their correlation with physical fitness and resting state functional connectivity of the periaqueductal grey in women with fibromyalgia: An exploratory secondary study
- Educational Case Reports
- Stellate ganglion block in disparate treatment-resistant mental health disorders: A case series
- Regaining the intention to live after relief of intractable phantom limb pain: A case study
- Trigeminal neuralgia caused by dolichoectatic vertebral artery: Reports of two cases
- Short Communications
- Neuroinflammation in chronic pain: Myth or reality?
- The use of registry data to assess clinical hunches: An example from the Swedish quality registry for pain rehabilitation
- Letter to the Editor
- Letter to the Editor For: “Stellate ganglion block in disparate treatment-resistant mental health disorders: A case series”
- Corrigendum
- Corrigendum to “Patient characteristics in relation to opioid exposure in a chronic non-cancer pain population”
Articles in the same Issue
- Editorial Comment
- Abstracts presented at SASP 2025, Reykjavik, Iceland. From the Test Tube to the Clinic – Applying the Science
- Quantitative sensory testing – Quo Vadis?
- Stellate ganglion block for mental disorders – too good to be true?
- When pain meets hope: Case report of a suspended assisted suicide trajectory in phantom limb pain and its broader biopsychosocial implications
- Transcutaneous electrical nerve stimulation – an important tool in person-centered multimodal analgesia
- Clinical Pain Researches
- Exploring the complexities of chronic pain: The ICEPAIN study on prevalence, lifestyle factors, and quality of life in a general population
- The effect of peer group management intervention on chronic pain intensity, number of areas of pain, and pain self-efficacy
- Effects of symbolic function on pain experience and vocational outcome in patients with chronic neck pain referred to the evaluation of surgical intervention: 6-year follow-up
- Experiences of cross-sectoral collaboration between social security service and healthcare service for patients with chronic pain – a qualitative study
- Completion of the PainData questionnaire – A qualitative study of patients’ experiences
- Pain trajectories and exercise-induced pain during 16 weeks of high-load or low-load shoulder exercise in patients with hypermobile shoulders: A secondary analysis of a randomized controlled trial
- Pain intensity in anatomical regions in relation to psychological factors in hypermobile Ehlers–Danlos syndrome
- Opioid use at admittance increases need for intrahospital specialized pain service: Evidence from a registry-based study in four Norwegian university hospitals
- Topically applied novel TRPV1 receptor antagonist, ACD440 Gel, reduces temperature-evoked pain in patients with peripheral neuropathic pain with sensory hypersensitivity, a randomized, double-blind, placebo-controlled, crossover study
- Pain and health-related quality of life among women of childbearing age in Iceland: ICEPAIN, a nationwide survey
- A feasibility study of a co-developed, multidisciplinary, tailored intervention for chronic pain management in municipal healthcare services
- Healthcare utilization and resource distribution before and after interdisciplinary pain rehabilitation in primary care
- Measurement properties of the Swedish Brief Pain Coping Inventory-2 in patients seeking primary care physiotherapy for musculoskeletal pain
- Understanding the experiences of Canadian military veterans participating in aquatic exercise for musculoskeletal pain
- “There is generally no focus on my pain from the healthcare staff”: A qualitative study exploring the perspective of patients with Parkinson’s disease
- Observational Studies
- Association between clinical laboratory indicators and WOMAC scores in Qatar Biobank participants: The impact of testosterone and fibrinogen on pain, stiffness, and functional limitation
- Well-being in pain questionnaire: A novel, reliable, and valid tool for assessment of the personal well-being in individuals with chronic low back pain
- Properties of pain catastrophizing scale amongst patients with carpal tunnel syndrome – Item response theory analysis
- Adding information on multisite and widespread pain to the STarT back screening tool when identifying low back pain patients at risk of worse prognosis
- The neuromodulation registry survey: A web-based survey to identify and describe characteristics of European medical patient registries for neuromodulation therapies in chronic pain treatment
- A biopsychosocial content analysis of Dutch rehabilitation and anaesthesiology websites for patients with non-specific neck, back, and chronic pain
- Topical Reviews
- An action plan: The Swedish healthcare pathway for adults with chronic pain
- Team-based rehabilitation in primary care for patients with musculoskeletal disorders: Experiences, effect, and process evaluation. A PhD synopsis
- Persistent severe pain following groin hernia repair: Somatosensory profiles, pain trajectories, and clinical outcomes – Synopsis of a PhD thesis
- Systematic Reviews
- Effectiveness of non-invasive vagus nerve stimulation vs heart rate variability biofeedback interventions for chronic pain conditions: A systematic review
- A scoping review of the effectiveness of underwater treadmill exercise in clinical trials of chronic pain
- Neural networks involved in painful diabetic neuropathy: A systematic review
- Original Experimental
- Knowledge, attitudes, and practices of transcutaneous electrical nerve stimulation in perioperative care: A Swedish web-based survey
- Impact of respiration on abdominal pain thresholds in healthy subjects – A pilot study
- Measuring pain intensity in categories through a novel electronic device during experimental cold-induced pain
- Robustness of the cold pressor test: Study across geographic locations on pain perception and tolerance
- Experimental partial-night sleep restriction increases pain sensitivity, but does not alter inflammatory plasma biomarkers
- Is it personality or genes? – A secondary analysis on a randomized controlled trial investigating responsiveness to placebo analgesia
- Investigation of endocannabinoids in plasma and their correlation with physical fitness and resting state functional connectivity of the periaqueductal grey in women with fibromyalgia: An exploratory secondary study
- Educational Case Reports
- Stellate ganglion block in disparate treatment-resistant mental health disorders: A case series
- Regaining the intention to live after relief of intractable phantom limb pain: A case study
- Trigeminal neuralgia caused by dolichoectatic vertebral artery: Reports of two cases
- Short Communications
- Neuroinflammation in chronic pain: Myth or reality?
- The use of registry data to assess clinical hunches: An example from the Swedish quality registry for pain rehabilitation
- Letter to the Editor
- Letter to the Editor For: “Stellate ganglion block in disparate treatment-resistant mental health disorders: A case series”
- Corrigendum
- Corrigendum to “Patient characteristics in relation to opioid exposure in a chronic non-cancer pain population”

