Abstract
Objectives
Pressure algometry is a validated method for objectively quantifying pain sensitivity in musculoskeletal disorders, particularly useful for diagnosis and monitoring of treatment responses. However, its application to abdominal pain sensitivity remains insufficiently standardized, especially regarding the influence of physiological factors such as respiration. This study investigated the impact of respiratory phase (inhalation vs exhalation) on abdominal pressure pain thresholds (PT) to support the development of standardized assessment protocols.
Methods
Thirty-one healthy medical students were recruited for the study. Each participant underwent three assessments of the abdominal PT with varying respiration phases. Furthermore, intraclass correlation coefficients (ICCs) were estimated to quantify the reliability of PT measurements.
Results
The respiration phase has a significant impact on the PT, which was found to be significantly lower during exhalation than during inhalation (431 ± 177 vs 492 ± 186 kPa, p = 0.0003). The pressure application rate (PAR) for the expiratory measurements was significantly lower compared to the inspiratory PAR (112 ± 56 vs 130 ± 63 kPa/s, p = 0.0007). Both ICCs had similar magnitudes (close to 0.9). No significant difference in PT was found between sexes.
Conclusions
Our study underscores the impact of respiration on pain perception, revealing increased abdominal PT during inhalation. A standardized approach is needed for abdominal PT assessment to guarantee its success in diagnostic and therapeutic evaluations.
1 Introduction
The quantification of pain is an essential part of a physician’s daily practice and is crucial for both diagnostic and monitoring purposes [1]. Although unidimensional self-report scales such as the numeric rating scale (NRS) and the visual analogue scale are widely used, they have limitations. For example, these scales are influenced by patients’ mood and previous pain experiences, which can introduce bias into evaluations [2,3,4]. In contrast, pressure algometry (PA) provides an objective quantitative evaluation of pain sensitivity, complementing self-reported assessments. Algometry refers to methods that quantify pain thresholds (PT) by applying controlled pressure to tissues until pain is elicited [5]. It has proven valuable for diagnosing and evaluating the treatment of various conditions: lower back pain [6], neck pain [7,8], chronic pelvic pain [9], patellar tendinopathy [10], knee osteoarthritis [11], and Achilles tendinitis [12], as well as non-orthopedic disorders, such as fibromyalgia [13,14,15], dysmenorrhea [16], and endometriosis [17]. In addition to assessments of superficial tissues, studies focused on the pain sensitivity of deep somatic [18] and visceral afferents [9]. In a retrospective study involving over 400 children with suspected appendicitis, PA demonstrated diagnostic accuracy that exceeded many published clinical algorithms and was comparable to the precision of ultrasound findings [19]. However, the reliability of abdominal PT determination has not been extensively studied, with few investigations to date [2,9]. One aspect that might contribute to the variability of abdominal PT is the activation of the sympathetic nervous system by different phases of respiration (further referred to as the respiration phase), which is particularly strong at low respiratory frequencies (0.1 Hz). It has been shown that pain and pain-related brain activity may be reduced during inhalation [20], which may be at least in part linked to activity of the autonomic nervous system. We therefore explored the impact of varying respiratory positions on the assessment of abdominal PT, aiming to identify sources of variability and thereby increase intrarater reliability of abdominal PT measurements, and to investigate a possible respiration-driven modulation of pain sensitivity.
2 Methods
This study was approved by the local Research Ethics Committee (EK 2021-604). The observational study was registered in the German Clinical Trials Register (DRKS00032288). Prior to enrolment in the study, all participants gave their informed consent both verbally and in writing. Data collection for the study took place entirely on a single day at the medical university’s facilities, with no follow-up conducted thereafter. A total of 31 participants were enrolled, with sampling conducted sequentially over the course of that day. The study design and reporting adhered to the STROBE guidelines, ensuring comprehensive and transparent presentation of observational data [21].
2.1 Eligibility criteria
Students without abdominal disorders or any kind of pain, such as migraine, lower back pain, or inflammatory diseases, were eligible. Previous abdominal surgery, polyneuropathy, intake of daily medications, and poor German language communication skills were excluded. Participants were required to be at least 18 years old, with no upper age limit.
2.2 Procedure
Participants were instructed to lie down in a slightly supine position. Participants were instructed to breathe normally (self-paced) during the assessments, with no external respiratory pacing or monitoring. Six specific abdominal acupuncture points (Figure 1) were manually palpated to identify the most sensitive point for further examination. These points are according to Traditional Chinese Theories situated in areas relevant to gastrointestinal movement and digestion [22,23].
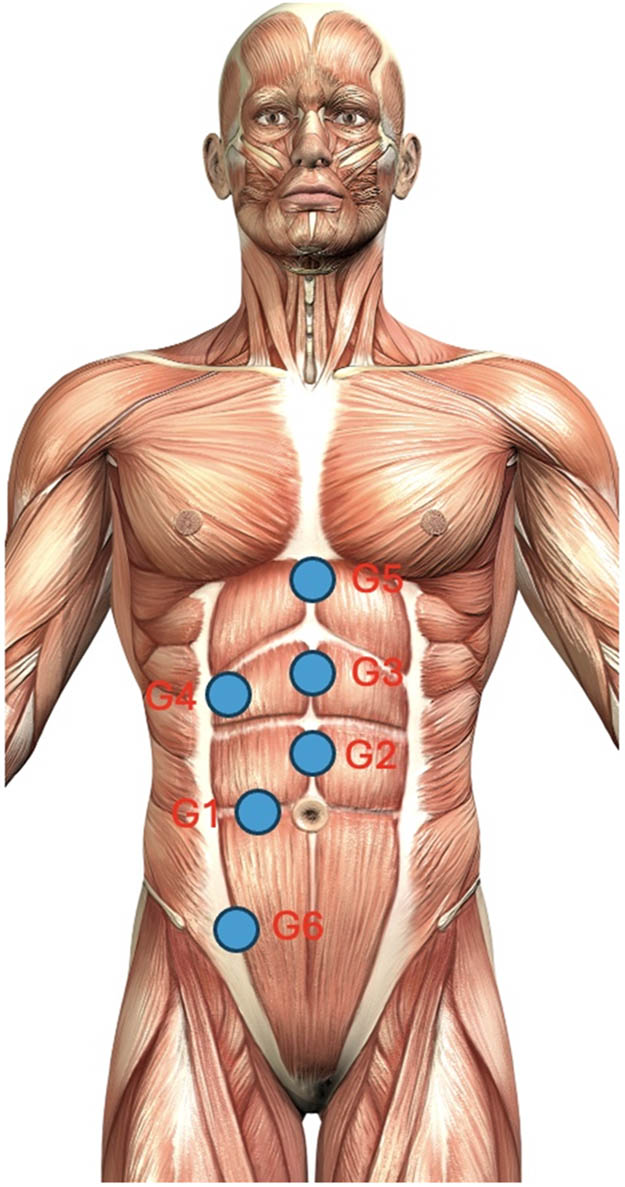
Location of abdominal pressure points and their location on acupuncture points: G1: stomach 25; G2: conception vessel 12; G3: conception vessel 14; G4: gallbladder 24; G5: conception vessel 16; G6: spleen 21. Figure created by the authors using © Freepik (Premium License) resources, modified for the purposes of this study.
To ensure exact forces applied in the measurement of the PT, a force gauge (PCE-instruments FM-200) with a 1 cm2 tip was used. The force at the designated point was gradually increased until participants experienced pain rather than just a sensation of pressure. This turning point was defined as the PT, ensuring an objective pain measurement [1].
This process was repeated three times for each participant and respiration phase (inhalation and exhalation). The average of three values was obtained. Each set of three PT trials for a given respiratory phase required only a few minutes to complete, so that, with the 15-min break between phases, the overall testing session for each participant lasted approximately 30 min.
A real-time force–time diagram was displayed on the screen to visually guide the examiner in maintaining this pressure application rate (PAR), thus reducing variability in the pressure application.
The assessment of the PT was conducted in an alternating manner between the two respiration phases (inhalation and exhalation). After the initial measurement, a 15-min resting period was provided before proceeding with the PT evaluation in the remaining respiration phase. Respiratory phase assessments alternated to prevent order effects.
During the inspiratory PT assessment, pressure application ceased when participants needed to exhale. Each PT measurement lasted only a few seconds and was thus completed within a few breathing cycles. Similarly, for expiratory PT measurements, pressure application ceased when participants needed to inhale. This approach ensured that the assessments aligned with the respective respiratory phases for accuracy and reproducibility. Participants naturally pause briefly at the end of each inspiratory and expiratory phase; in this study, these transition pauses were treated as part of the preceding respiratory phase and did not affect the measurement protocol. All measurements were performed by a single examiner to eliminate inter-rater bias. To minimize expectation bias, participants were instructed only to report when they first experienced pain during the pressure application under different respiration conditions. They were not informed about the specific hypothesis regarding the effects of the respiration phase on pain perception. For example, participants were not told that inhalation was expected to produce higher PT; this blinding of the hypothesis aimed to reduce expectation bias in their pain reports.
2.3 Statistical analysis
The methods of data collection and analysis were carried out in accordance with the guidelines for Good Clinical Practice. Pseudonymized data were entered into an internal Research Electronic Data Capture database by trained research team members. Statistical analysis was performed using the SAS software (version 9.4; SAS Institute, Cary, North Carolina, USA). For qualitative variables, absolute and relative frequencies were reported. To compare two groups with respect to a qualitative variable, Fisher’s exact test was applied. Quantitative variables are presented as mean ± standard deviation. Since the mean is more sensitive to variations in the data than the median, we opted to use the mean for our analysis. To compare the mean values of the two groups, a two-sample t-test was used. A paired t-test was used for paired samples. To assess reliability, repeated-measures analyses of variance (ANOVAs) were conducted to compare the three measurements, separately for inhalation and exhalation. Post hoc tests, according to Scheffé, were conducted for pairwise comparisons. These analyses were performed using the SAS procedure PROC MIXED with time as a fixed factor and participants’ ID as a random factor. A post hoc power analysis was performed using the SAS procedure PROC POWER to ensure that a medium effect size (Cohen’s d ≈ 0.5) could be verified with a paired t-test. Furthermore, intraclass correlation coefficients (ICCs) were estimated as measures of reliability. In accordance with the classification proposed by Shrout and Fleiss, the ICC (2,1) model was applied to assess the consistency among three independently and randomly obtained measurements per subject [24]. The result of a statistical test was considered statistically significant if the p-value was less than 0.05.
3 Results
A total number of 31 medical students were included in this study. Basic characteristics are shown in Table 1. The Fisher’s exact test revealed no significant difference in the distribution of the most sensitive abdominal pressure points between sexes (p = 1.0, Table 2).
Basic characteristics
| Female | Male | p-value | |
|---|---|---|---|
| Sex distribution (n, %) | 16 (48%) | 15 (52%) | — |
| Age (years) | 22.9 ± 2.1 | 24.3 ± 2.5 | 0.1351 |
| BMI (kg/m2) | 20.8 ± 2.1 | 23.8 ± 2.4 | 0.0008 |
BMI, body mass index.
Sex-based distribution of the most sensitive abdominal pressure points
| G1 | G2 | G3 | G4 | G5 | G6 | Total | |
|---|---|---|---|---|---|---|---|
| Female | 3 (19%) | 4 (25%) | 3 (19%) | 0 (0%) | 3 (19%) | 3 (19%) | 16 (52%) |
| Male | 3 (20%) | 4 (27%) | 3 (20%) | 0 (0%) | 2 (13%) | 3 (20%) | 15 (48%) |
| Total | 6 | 8 | 6 | 0 | 5 | 6 | 31 |
Three measurements were performed during inhalation and exhalation. The findings revealed a consistent and significant difference in the PT between the two phases. PT was higher during inhalation than during exhalation (492 ± 186 vs 492 ± 186 kPa, p = 0.0003; Table 3, Figure 2).
Pain thresholds during inhalation and exhalation
| Inhalation (kPa) | Exhalation (kPa) | Differences (inhalation- exhalation) | p-value | |
|---|---|---|---|---|
| Measurement of PT | ||||
| 1. | 510 ± 190 | 438 ± 194 | 72 ± 141 | 0.0083 |
| 2. | 496 ± 215 | 424 ± 178 | 72 ± 104 | 0.0006 |
| 3. | 468 ± 176 | 432 ± 177 | 37 ± 94 | 0.0420 |
| Average | 492 ± 186 | 431 ± 177 | 61 ± 83 | 0.0003 |

PT during inhalation and exhalation for each measurement. Significant differences were observed for each value (red: Inhalation; blue: Exhalation).
Interestingly, the first measurement, regardless of whether it was during inhalation or exhalation, yielded the highest PT values. The ANOVA for repeated measurements slightly failed to reach statistical significance (p = 0.0853) for measurements taken during inhalation. The largest difference was found between measurements 1 and 3 (p = 0.0896 after Scheffé’s adjustment). This suggests that PT values tended to decrease over the course of repeated measurements during inhalation. In contrast, the ANOVA for expiratory measurements showed no significant differences (p = 0.6553), indicating that PT values remained stable. Based on the ICC assessments, the reliability of the three measurements obtained during exhalation and inhalation was rather high (ICC = 0.8927 and ICC = 0.8718, respectively). According to Altman and Bland, these values indicate a high level of reliability [25].
Moreover, our findings revealed that sex exerted no impact on PT, with no noteworthy variations observed in any of the measurements. The p-values range from 0.4993 to 0.7438 (Figure 3).
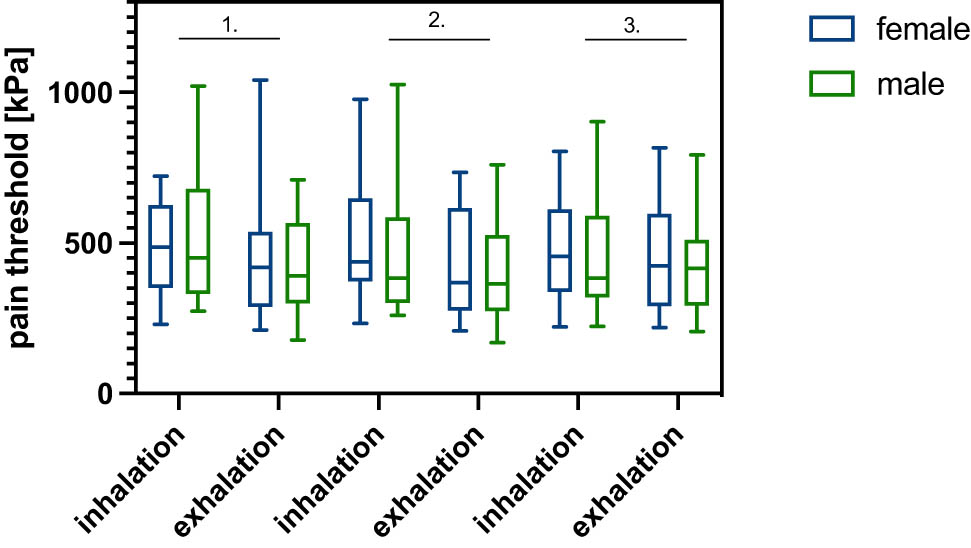
Sex-specific PT: Female (blue) and male (green). No difference in PT was observed between the sexes.
3.1 Power size
We recruited a maximum of 31 volunteers, which provided sufficient power (0.809) to detect a statistically significant difference between inhalation and exhalation using a paired t-test, assuming a medium effect size (Cohen’s d ≈ 0.53) with a significance level of α = 0.05.
The PAR was also assessed. The results in Table 4 show that the PAR for expiratory measurements was significantly lower than that for inspiratory measurements (average p = 0.0007).
The PAR during inhalation and exhalation
| Inhalation (kPa/s) | Exhalation (kPa/s) | Differences inhalation- exhalation) | p-value | |
|---|---|---|---|---|
| PAR | ||||
| 1. | 122 ± 63 | 108 ± 48 | 14 ± 83 | 0.0800 |
| 2. | 133 ± 75 | 114 ± 67 | 19 ± 83 | 0.0127 |
| 3. | 130 ± 72 | 114 ± 58 | 19 ± 42 | 0.0206 |
| Average | 130 ± 63 | 112 ± 56 | 18 ± 27 | 0.0007 |
Interestingly, within one group of measurements (either inhalation or exhalation), no relevant differences in PAR were observed (p = 0.3169 and p = 0.4231, respectively), suggesting that the individual measurements taken during the same respiratory phase showed consistent application rates, indicating a stable pattern for each participant during that specific respiration phase.
4 Discussion
Algometry is considered an objective stimulation method for assessing PT and is a valuable tool for diagnosing and evaluating the effectiveness of treatments for various disorders [5]. By utilizing PA, researchers and clinicians can obtain more standardized and reproducible measurements of pain sensitivity, thereby reducing the impact of subjective bias. In this study, we found that respiration modulates the abdominal PT and thus needs to be considered in the standardized measurement.
The reliability of PA has been shown in various studies, as described above. The correlation between self-reported instruments for pain assessment (e.g., NRS or VRS) and PT evaluation was described as moderate [26,27] to high [5].
Our findings revealed a significant decrease in PT during exhalation compared to inhalation, indicating a notable reduction in pain perception during the inspiratory phase. This phase is associated with a higher sympathetic tone, while the expiratory phase is characterized by predominant vagal tone [28]. Arsenault et al. highlighted two potential mechanisms for the decreased pain perception during inhalation: one involves central mechanisms during inhalation rather than exhalation. Another explanation worth considering is the distraction effect (i.e., reduced pain perception due to attentional shift away from the pain stimulus) attributed to cued respiration [20]. Additionally, the increased resistance of the abdominal muscles during exhalation [29] may contribute to a shift in the perception of pain. Reyes del Paso et. al. postulated that breath-holding after deep inhalation might reduce pain perception due to the activation of baroreceptors [30]. They only compared pain perception under two conditions: breath-holding after deep and slow inhalation. Nevertheless, this mechanism could also be relevant for this study.
One might argue that intra-abdominal pressure rises with diaphragmatic contraction during inhalation [31]. An external pressure increase during inhalation could further elevate intra-abdominal pressure within the abdominal cavity, potentially leading to a lower PT. However, contrary to this expectation, we observed a higher PT during inhalation, suggesting that increased intra-abdominal pressure alone does not explain this finding.
A possible explanation for the observed differences in PT values between respiratory phases may lie in the variation of PAR, as differences in PAR can influence pain perception and threshold assessments. The PAR used in previous studies varies from 0.05 to 20 N/s [32]. It has been noted that faster rates may lead to false-low threshold evaluations [33,34]. Although the PAR was slightly higher during inhalation, the absolute difference remained below 20 kPa/s and is unlikely to account for the observed difference in pressure PT. In areas like the abdomen, where PT can be higher, a very low rate of 0.63 kPa/s (equivalent to 0.05 N/s when using a 1 cm2 algometer tip) may be clinically impractical, as each measurement could become very time-consuming; for instance, assessing a PT of 450 kPa would require approximately 13 min. One way to mitigate potential inaccuracies is to repeat measurements.
Nevertheless, the PT assessment for both respiration phases revealed a high ICC value, indicating high reliability of the data.
In the research conducted by Chesterton and colleagues [35], they observed a sex-based disparity in the assessment of PT at the first interosseous muscle. The present study did not exhibit this sex-specific distinction.
All measurements were performed by the same examiner to ensure consistency in the evaluation process. Additionally, each participant underwent both inhalation and exhalation measurements, providing a direct comparison of pain sensitivity under different respiratory conditions. Given the slightly higher reliability observed during expiration, we suggest that future studies standardize abdominal pressure threshold assessments to a single respiratory phase, preferably expiration. It is important to consistently consider the breathing position during testing and avoid conducting measurements across different respiratory phases within the same protocol. However, our study employed a small sample size and concentrated solely on healthy young individuals. Additionally, the respiratory phase was assessed solely through observation. To achieve more precise control over the respiratory state, the use of a respiratory monitor may be necessary. Further research is needed to confirm this phenomenon in a more diverse and generalized population. Interrater reliability needs to be explored in subsequent studies, with due consideration given to the participant’s respiration phase.
5 Conclusion
Our findings indicate that standardizing respiration phase is crucial for obtaining reliable measurements of abdominal PT, as it may significantly influence pain sensitivity. This modulation may stem from the activation patterns of the autonomic nervous system or variations in muscle tone. These insights are important for developing clinical and research protocols that improve the reliability of abdominal pain assessments.
Acknowledgments
This research received no specific funding. EG was supported by a scholarship from the Karl and Veronica Carstens-Foundation, grant number KVC 0/124/2022.
-
Research ethics: Research involving human subjects complied with all relevant national regulations, institutional policies and is in accordance with the tenets of the Helsinki Declaration (as amended in 2013), and has been approved by local ethical committee (EK 2021-604).
-
Informed consent: Informed consent has been obtained from all individuals included in this study.
-
Author contributions: The authors have accepted responsibility for the entire content of this manuscript and approved its submission. JK and AA conducted the study. CW performed the statistical analysis and revised the manuscript. CR co-designed the study, the interpreted findings, and revised the manuscript. CY co-designed the study, interpreted the findings, revised the manuscript. MS interpreted the findings and revised the manuscript. EG co-designed the study, supervised the data collection, interpreted findings, and produced the first and final draft of the manuscript.
-
Competing interests: Authors state no conflict of interest.
-
Research funding: None declared.
-
Data availability: The raw data can be obtained on request from the corresponding author.
-
Artificial intelligence/Machine learning tools: During the preparation of this work, the authors used Paperpal to improve grammar and language aspects of this manuscript. Paperpal is an AI-assisted language refinement tool designed to help authors improve grammar, clarity, and readability in scientific writing. After using this service, the authors reviewed and edited the content as needed and took full responsibility for the content of the publication.
References
[1] Pelfort X, Torres-Claramunt R, Sanchez-Soler JF, Hinarejos P, Leal-Blanquet J, Valverde D, et al. Pressure algometry is a useful tool to quantify pain in the medial part of the knee: an intra- and inter-reliability study in healthy subjects. Orthop Traumatol Surg Res. 2015;101(5):559–63.Search in Google Scholar
[2] Montenegro ML, Braz CA, Mateus-Vasconcelos EL, Rosa-e-Silva JC, Candido-dos-Reis FJ, Nogueira AA, et al. Pain pressure threshold algometry of the abdominal wall in healthy women. Braz J Med Biol Res. 2012;45(7):578–82.10.1590/S0100-879X2012007500064Search in Google Scholar PubMed PubMed Central
[3] Schiavenato M, Craig KD. Pain assessment as a social transaction: beyond the “gold standard”. Clin J Pain. 2010;26(8):667–76.10.1097/AJP.0b013e3181e72507Search in Google Scholar PubMed
[4] Rollman GB, Abdel-Shaheed J, Gillespie JM, Jones KS. Does past pain influence current pain: biological and psychosocial models of sex differences. Eur J Pain. 2004;8(5):427–33.10.1016/j.ejpain.2004.03.002Search in Google Scholar PubMed
[5] Pelfort X, Torres-Claramunt R, Sánchez-Soler JF, Hinarejos P, Leal-Blanquet J, Valverde D, et al. Pressure algometry is a useful tool to quantify pain in the medial part of the knee: an intra- and inter-reliability study in healthy subjects. Orthop Traumatol Surg Res. 2015;101(5):559–63.10.1016/j.otsr.2015.03.016Search in Google Scholar PubMed
[6] Farasyn AD, Meeusen R, Nijs J. Validity of cross-friction algometry procedure in referred muscle pain syndromes: preliminary results of a new referred pain provocation technique with the aid of a Fischer pressure algometer in patients with nonspecific low back pain. Clin J Pain. 2008;24(5):456–62.10.1097/AJP.0b013e3181643403Search in Google Scholar PubMed
[7] Walton DM, Macdermid JC, Nielson W, Teasell RW, Chiasson M, Brown L. Reliability, standard error, and minimum detectable change of clinical pressure pain threshold testing in people with and without acute neck pain. J Orthop Sports Phys Ther. 2011;41(9):644–50.10.2519/jospt.2011.3666Search in Google Scholar PubMed
[8] Walton DM, Macdermid JC, Nielson W, Teasell RW, Nailer T, Maheu P. A descriptive study of pressure pain threshold at 2 standardized sites in people with acute or subacute neck pain. J Orthop Sports Phys Ther. 2011;41(9):651–7.10.2519/jospt.2011.3667Search in Google Scholar PubMed
[9] Fenton BW, Palmieri PA, Durner C, Fanning J. Quantification of abdominal wall pain using pain pressure threshold algometry in patients with chronic pelvic pain. Clin J Pain. 2009;25(6):500–5.10.1097/AJP.0b013e31819a3cf9Search in Google Scholar PubMed
[10] van Wilgen P, van der Noord R, Zwerver J. Feasibility and reliability of pain pressure threshold measurements in patellar tendinopathy. J Sci Med Sport. 2011;14(6):477–81.10.1016/j.jsams.2011.05.004Search in Google Scholar PubMed
[11] Stausholm MB, Bjordal JM, Moe-Nilssen R, Naterstad IF. Pain pressure threshold algometry in knee osteoarthritis: intra- and inter-rater reliability. Physiother Theory Pract. 2023;39(3):615–22.10.1080/09593985.2021.2023929Search in Google Scholar PubMed
[12] Fredberg U, Bolvig L, Pfeiffer-Jensen M, Clemmensen D, Jakobsen BW, Stengaard-Pedersen K. Ultrasonography as a tool for diagnosis, guidance of local steroid injection and, together with pressure algometry, monitoring of the treatment of athletes with chronic jumper’s knee and Achilles tendinitis: a randomized, double-blind, placebo-controlled study. Scand J Rheumatol. 2004;33(2):94–101.10.1080/03009740310004126Search in Google Scholar PubMed
[13] Jespersen A, Dreyer L, Kendall S, Graven-Nielsen T, Arendt-Nielsen L, Bliddal H, et al. Computerized cuff pressure algometry: A new method to assess deep-tissue hypersensitivity in fibromyalgia. Pain. 2007;131(1–2):57–62.10.1016/j.pain.2006.12.012Search in Google Scholar PubMed
[14] de la Coba P, Montoro CI, Reyes Del Paso GA, Galvez-Sanchez CM. Algometry for the assessment of central sensitisation to pain in fibromyalgia patients: a systematic review. Ann Med. 2022;54(1):1403–22.10.1080/07853890.2022.2075560Search in Google Scholar PubMed PubMed Central
[15] King CD, Jastrowski Mano KE, Barnett KA, Pfeiffer M, Ting TV, Kashikar-Zuck S. Pressure pain threshold and anxiety in adolescent females with and without juvenile fibromyalgia: a pilot study. Clin J Pain. 2017;33(7):620–6.10.1097/AJP.0000000000000444Search in Google Scholar PubMed PubMed Central
[16] Machado AFP, Perracini MR, Rampazo EP, Driusso P, Liebano RE. Effects of thermotherapy and transcutaneous electrical nerve stimulation on patients with primary dysmenorrhea: A randomized, placebo-controlled, double-blind clinical trial. Complement Ther Med. 2019;47:102188.10.1016/j.ctim.2019.08.022Search in Google Scholar PubMed
[17] Nunes FR, Ferreira JM, Bahamondes L. Pain threshold and sleep quality in women with endometriosis. Eur J Pain. 2015;19(1):15–20.10.1002/ejp.514Search in Google Scholar PubMed
[18] Shraim MA, Sluka KA, Sterling M, Arendt-Nielsen L, Argoff C, Bagraith KS, et al. Features and methods to discriminate between mechanism-based categories of pain experienced in the musculoskeletal system: a Delphi expert consensus study. Pain. 2022;163(9):1812–28.10.1097/j.pain.0000000000002577Search in Google Scholar PubMed PubMed Central
[19] Postuma R, Vajcner G, Postuma RB, Keijzer R. Bedside pressure-pain threshold algometry to measure abdominal tenderness in childhood appendicitis: A retrospective cohort study. Int J Surg Open. 2021;32:100338.10.1016/j.ijso.2021.100338Search in Google Scholar
[20] Arsenault M, Ladouceur A, Lehmann A, Rainville P, Piche M. Pain modulation induced by respiration: phase and frequency effects. Neuroscience. 2013;252:501–11.10.1016/j.neuroscience.2013.07.048Search in Google Scholar PubMed
[21] von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453–7.10.1016/S0140-6736(07)61602-XSearch in Google Scholar PubMed
[22] Ghanad E, Staff S, Weiss C, Goncalves M, Santos MJ, Correia N, et al. Reduction of pain after laparoscopic bariatric surgery by personalized checkpoint acupuncture-data of a STRICTA conform pilot study. Obes Surg. 2023;33(7):2176–85.10.1007/s11695-023-06654-8Search in Google Scholar PubMed PubMed Central
[23] Ghanad E, Yang C, Weiss C, Goncalves M, Santos MJ, Correia N, et al. Personalized checkpoint acupuncture can reduce postoperative pain after abdominal surgery-a STRICTA-conform pilot study. Langenbecks Arch Surg. 2023;408(1):391.10.1007/s00423-023-03051-8Search in Google Scholar PubMed PubMed Central
[24] Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86(2):420–8.10.1037//0033-2909.86.2.420Search in Google Scholar PubMed
[25] Altman DG, Bland JM. Measurement in medicine: the analysis of method comparison studies. J R Stat Soc Ser D: Statistician. 1983;32(3):307–17.10.2307/2987937Search in Google Scholar
[26] Sand T, Zwart JA, Helde G, Bovim G. The reproducibility of cephalic pain pressure thresholds in control subjects and headache patients. Cephalalgia. 1997;17(7):748–55.10.1046/j.1468-2982.1997.1707748.xSearch in Google Scholar PubMed
[27] Alfonsin MM, Chapon R, de Souza CAB, Genro VK, Mattia MMC, Cunha-Filho JS. Correlations among algometry, the visual analogue scale, and the numeric rating scale to assess chronic pelvic pain in women. Eur J Obstet Gynecol Reprod Biol X. 2019;3:100037.10.1016/j.eurox.2019.100037Search in Google Scholar PubMed PubMed Central
[28] Berntson GG, Cacioppo JT, Quigley KS. Respiratory sinus arrhythmia: autonomic origins, physiological mechanisms, and psychophysiological implications. Psychophysiology. 1993;30(2):183–96.10.1111/j.1469-8986.1993.tb01731.xSearch in Google Scholar PubMed
[29] Goldman JM, Lehr RP, Millar AB, Silver JR. An electromyographic study of the abdominal muscles during postural and respiratory manoeuvres. J Neurol Neurosurg Psychiatry. 1987;50(7):866–9.10.1136/jnnp.50.7.866Search in Google Scholar PubMed PubMed Central
[30] Reyes del Paso GA, Munoz Ladron de Guevara C, Montoro CI. Breath-holding during exhalation as a simple manipulation to reduce pain perception. Pain Med. 2015;16(9):1835–41.10.1111/pme.12764Search in Google Scholar PubMed
[31] Gertler R. Respiratory mechanics. Anesthesiol Clin. 2021;39(3):415–40.10.1016/j.anclin.2021.04.003Search in Google Scholar PubMed PubMed Central
[32] Melia M, Schmidt M, Geissler B, Konig J, Krahn U, Ottersbach HJ, et al. Measuring mechanical pain: the refinement and standardization of pressure pain threshold measurements. Behav Res Methods. 2015;47(1):216–27.10.3758/s13428-014-0453-3Search in Google Scholar PubMed
[33] Jensen K, Andersen HO, Olesen J, Lindblom U. Pressure-pain threshold in human temporal region. Evaluation of a new pressure algometer. Pain. 1986;25(3):313–23.10.1016/0304-3959(86)90235-6Search in Google Scholar PubMed
[34] Kinser AM, Sands WA, Stone MH. Reliability and validity of a pressure algometer. J Strength Cond Res. 2009;23(1):312–4.10.1519/JSC.0b013e31818f051cSearch in Google Scholar
[35] Chesterton LS, Barlas P, Foster NE, Baxter DG, Wright CC. Gender differences in pressure pain threshold in healthy humans. Pain. 2003;101(3):259–66.10.1016/S0304-3959(02)00330-5Search in Google Scholar PubMed
© 2025 the author(s), published by De Gruyter
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Editorial Comment
- Abstracts presented at SASP 2025, Reykjavik, Iceland. From the Test Tube to the Clinic – Applying the Science
- Quantitative sensory testing – Quo Vadis?
- Stellate ganglion block for mental disorders – too good to be true?
- When pain meets hope: Case report of a suspended assisted suicide trajectory in phantom limb pain and its broader biopsychosocial implications
- Transcutaneous electrical nerve stimulation – an important tool in person-centered multimodal analgesia
- Clinical Pain Researches
- Exploring the complexities of chronic pain: The ICEPAIN study on prevalence, lifestyle factors, and quality of life in a general population
- The effect of peer group management intervention on chronic pain intensity, number of areas of pain, and pain self-efficacy
- Effects of symbolic function on pain experience and vocational outcome in patients with chronic neck pain referred to the evaluation of surgical intervention: 6-year follow-up
- Experiences of cross-sectoral collaboration between social security service and healthcare service for patients with chronic pain – a qualitative study
- Completion of the PainData questionnaire – A qualitative study of patients’ experiences
- Pain trajectories and exercise-induced pain during 16 weeks of high-load or low-load shoulder exercise in patients with hypermobile shoulders: A secondary analysis of a randomized controlled trial
- Pain intensity in anatomical regions in relation to psychological factors in hypermobile Ehlers–Danlos syndrome
- Opioid use at admittance increases need for intrahospital specialized pain service: Evidence from a registry-based study in four Norwegian university hospitals
- Topically applied novel TRPV1 receptor antagonist, ACD440 Gel, reduces temperature-evoked pain in patients with peripheral neuropathic pain with sensory hypersensitivity, a randomized, double-blind, placebo-controlled, crossover study
- Pain and health-related quality of life among women of childbearing age in Iceland: ICEPAIN, a nationwide survey
- A feasibility study of a co-developed, multidisciplinary, tailored intervention for chronic pain management in municipal healthcare services
- Healthcare utilization and resource distribution before and after interdisciplinary pain rehabilitation in primary care
- Measurement properties of the Swedish Brief Pain Coping Inventory-2 in patients seeking primary care physiotherapy for musculoskeletal pain
- Understanding the experiences of Canadian military veterans participating in aquatic exercise for musculoskeletal pain
- “There is generally no focus on my pain from the healthcare staff”: A qualitative study exploring the perspective of patients with Parkinson’s disease
- Observational Studies
- Association between clinical laboratory indicators and WOMAC scores in Qatar Biobank participants: The impact of testosterone and fibrinogen on pain, stiffness, and functional limitation
- Well-being in pain questionnaire: A novel, reliable, and valid tool for assessment of the personal well-being in individuals with chronic low back pain
- Properties of pain catastrophizing scale amongst patients with carpal tunnel syndrome – Item response theory analysis
- Adding information on multisite and widespread pain to the STarT back screening tool when identifying low back pain patients at risk of worse prognosis
- The neuromodulation registry survey: A web-based survey to identify and describe characteristics of European medical patient registries for neuromodulation therapies in chronic pain treatment
- A biopsychosocial content analysis of Dutch rehabilitation and anaesthesiology websites for patients with non-specific neck, back, and chronic pain
- Topical Reviews
- An action plan: The Swedish healthcare pathway for adults with chronic pain
- Team-based rehabilitation in primary care for patients with musculoskeletal disorders: Experiences, effect, and process evaluation. A PhD synopsis
- Persistent severe pain following groin hernia repair: Somatosensory profiles, pain trajectories, and clinical outcomes – Synopsis of a PhD thesis
- Systematic Reviews
- Effectiveness of non-invasive vagus nerve stimulation vs heart rate variability biofeedback interventions for chronic pain conditions: A systematic review
- A scoping review of the effectiveness of underwater treadmill exercise in clinical trials of chronic pain
- Neural networks involved in painful diabetic neuropathy: A systematic review
- Original Experimental
- Knowledge, attitudes, and practices of transcutaneous electrical nerve stimulation in perioperative care: A Swedish web-based survey
- Impact of respiration on abdominal pain thresholds in healthy subjects – A pilot study
- Measuring pain intensity in categories through a novel electronic device during experimental cold-induced pain
- Robustness of the cold pressor test: Study across geographic locations on pain perception and tolerance
- Experimental partial-night sleep restriction increases pain sensitivity, but does not alter inflammatory plasma biomarkers
- Is it personality or genes? – A secondary analysis on a randomized controlled trial investigating responsiveness to placebo analgesia
- Investigation of endocannabinoids in plasma and their correlation with physical fitness and resting state functional connectivity of the periaqueductal grey in women with fibromyalgia: An exploratory secondary study
- Educational Case Reports
- Stellate ganglion block in disparate treatment-resistant mental health disorders: A case series
- Regaining the intention to live after relief of intractable phantom limb pain: A case study
- Trigeminal neuralgia caused by dolichoectatic vertebral artery: Reports of two cases
- Short Communications
- Neuroinflammation in chronic pain: Myth or reality?
- The use of registry data to assess clinical hunches: An example from the Swedish quality registry for pain rehabilitation
- Letter to the Editor
- Letter to the Editor For: “Stellate ganglion block in disparate treatment-resistant mental health disorders: A case series”
- Corrigendum
- Corrigendum to “Patient characteristics in relation to opioid exposure in a chronic non-cancer pain population”
Articles in the same Issue
- Editorial Comment
- Abstracts presented at SASP 2025, Reykjavik, Iceland. From the Test Tube to the Clinic – Applying the Science
- Quantitative sensory testing – Quo Vadis?
- Stellate ganglion block for mental disorders – too good to be true?
- When pain meets hope: Case report of a suspended assisted suicide trajectory in phantom limb pain and its broader biopsychosocial implications
- Transcutaneous electrical nerve stimulation – an important tool in person-centered multimodal analgesia
- Clinical Pain Researches
- Exploring the complexities of chronic pain: The ICEPAIN study on prevalence, lifestyle factors, and quality of life in a general population
- The effect of peer group management intervention on chronic pain intensity, number of areas of pain, and pain self-efficacy
- Effects of symbolic function on pain experience and vocational outcome in patients with chronic neck pain referred to the evaluation of surgical intervention: 6-year follow-up
- Experiences of cross-sectoral collaboration between social security service and healthcare service for patients with chronic pain – a qualitative study
- Completion of the PainData questionnaire – A qualitative study of patients’ experiences
- Pain trajectories and exercise-induced pain during 16 weeks of high-load or low-load shoulder exercise in patients with hypermobile shoulders: A secondary analysis of a randomized controlled trial
- Pain intensity in anatomical regions in relation to psychological factors in hypermobile Ehlers–Danlos syndrome
- Opioid use at admittance increases need for intrahospital specialized pain service: Evidence from a registry-based study in four Norwegian university hospitals
- Topically applied novel TRPV1 receptor antagonist, ACD440 Gel, reduces temperature-evoked pain in patients with peripheral neuropathic pain with sensory hypersensitivity, a randomized, double-blind, placebo-controlled, crossover study
- Pain and health-related quality of life among women of childbearing age in Iceland: ICEPAIN, a nationwide survey
- A feasibility study of a co-developed, multidisciplinary, tailored intervention for chronic pain management in municipal healthcare services
- Healthcare utilization and resource distribution before and after interdisciplinary pain rehabilitation in primary care
- Measurement properties of the Swedish Brief Pain Coping Inventory-2 in patients seeking primary care physiotherapy for musculoskeletal pain
- Understanding the experiences of Canadian military veterans participating in aquatic exercise for musculoskeletal pain
- “There is generally no focus on my pain from the healthcare staff”: A qualitative study exploring the perspective of patients with Parkinson’s disease
- Observational Studies
- Association between clinical laboratory indicators and WOMAC scores in Qatar Biobank participants: The impact of testosterone and fibrinogen on pain, stiffness, and functional limitation
- Well-being in pain questionnaire: A novel, reliable, and valid tool for assessment of the personal well-being in individuals with chronic low back pain
- Properties of pain catastrophizing scale amongst patients with carpal tunnel syndrome – Item response theory analysis
- Adding information on multisite and widespread pain to the STarT back screening tool when identifying low back pain patients at risk of worse prognosis
- The neuromodulation registry survey: A web-based survey to identify and describe characteristics of European medical patient registries for neuromodulation therapies in chronic pain treatment
- A biopsychosocial content analysis of Dutch rehabilitation and anaesthesiology websites for patients with non-specific neck, back, and chronic pain
- Topical Reviews
- An action plan: The Swedish healthcare pathway for adults with chronic pain
- Team-based rehabilitation in primary care for patients with musculoskeletal disorders: Experiences, effect, and process evaluation. A PhD synopsis
- Persistent severe pain following groin hernia repair: Somatosensory profiles, pain trajectories, and clinical outcomes – Synopsis of a PhD thesis
- Systematic Reviews
- Effectiveness of non-invasive vagus nerve stimulation vs heart rate variability biofeedback interventions for chronic pain conditions: A systematic review
- A scoping review of the effectiveness of underwater treadmill exercise in clinical trials of chronic pain
- Neural networks involved in painful diabetic neuropathy: A systematic review
- Original Experimental
- Knowledge, attitudes, and practices of transcutaneous electrical nerve stimulation in perioperative care: A Swedish web-based survey
- Impact of respiration on abdominal pain thresholds in healthy subjects – A pilot study
- Measuring pain intensity in categories through a novel electronic device during experimental cold-induced pain
- Robustness of the cold pressor test: Study across geographic locations on pain perception and tolerance
- Experimental partial-night sleep restriction increases pain sensitivity, but does not alter inflammatory plasma biomarkers
- Is it personality or genes? – A secondary analysis on a randomized controlled trial investigating responsiveness to placebo analgesia
- Investigation of endocannabinoids in plasma and their correlation with physical fitness and resting state functional connectivity of the periaqueductal grey in women with fibromyalgia: An exploratory secondary study
- Educational Case Reports
- Stellate ganglion block in disparate treatment-resistant mental health disorders: A case series
- Regaining the intention to live after relief of intractable phantom limb pain: A case study
- Trigeminal neuralgia caused by dolichoectatic vertebral artery: Reports of two cases
- Short Communications
- Neuroinflammation in chronic pain: Myth or reality?
- The use of registry data to assess clinical hunches: An example from the Swedish quality registry for pain rehabilitation
- Letter to the Editor
- Letter to the Editor For: “Stellate ganglion block in disparate treatment-resistant mental health disorders: A case series”
- Corrigendum
- Corrigendum to “Patient characteristics in relation to opioid exposure in a chronic non-cancer pain population”

