Abstract
Objectives
Orofacial pain in patients taking part in a multimodal rehabilitation programme (MMRP) due to chronic bodily pain is common but it is not known whether such a rehabilitation programme can also have an effect on the presence of orofacial pain. The first aim of this study was to evaluate the effect of an MMRP on orofacial pain frequency. The second aim was to evaluate differences in the effect on quality of life and on psychosocial factors related to chronic pain.
Methods
MMRP was evaluated through validated questionnaires from the Swedish Quality Registry for Pain Rehabilitation (SQRP). Fifty-nine patients participating in MMRP filled out the two screening questions for orofacial pain in addition to the SQRP questionnaires before and after participation in MMRP during the period August 2016 to March 2018.
Results
Pain intensity decreased significantly after the MMRP (p=0.005). Fifty patients (69.4 %) reported orofacial pain before MMRP and no significant decrease after the programme (p=0.228). Among individuals with orofacial pain, the self-reported level of depression decreased after participation in the programme (p=0.004).
Conclusions
Even though orofacial pain is common among patients with chronic bodily pain, participation in a multimodal pain programme was not enough to reduce frequent orofacial pain. This finding implies that specific orofacial pain management including information about jaw physiology could be a justified component of patient assessment prior to a multimodal rehabilitation programme for chronic bodily pain.
Introduction
Chronic pain that persists for more than three months and beyond normal tissue healing is a common condition [1, 2]. In Europe and in Sweden, approximately 20 % of the adult population report moderate to severe chronic pain complaints [3]. Chronic, musculoskeletal pain is often located in several anatomical regions and about ten percent of adults report widespread pain including fibromyalgia [4]. Pain in the orofacial region is the third most common pain location after back pain and knee pain [3, 5]. In addition to overlap between widespread pain and orofacial pain [6, 7], the coexistence of other overlapping chronic pain conditions, such as chronic fatigue and tension type headache, is common [8]. Furthermore, comorbidities such as increased level of stress, depression and anxiety are common in individuals with chronic pain [9], and are largely related to treatment outcome and prognosis [10]. All in all, and considering the magnitude of the individual consequences of chronic pain, these symptoms are related to a negative impact on daily living and quality of life [11].
Due to its prevalent nature, pain is a common reason for seeking treatment, both in healthcare and dental care [12, 13]. Patients examined by one physician may be offered single, conservative, and relatively inexpensive treatments but invasive, irreversible, and costly treatments by another physician – for the same set of symptoms [14]. Patients with orofacial pain are commonly examined by a general practice dentist. For orofacial pain complaints, reversible and conservative treatment strategies are standard procedure including physical therapy modalities, occlusal appliances, and relaxation techniques [15, 16]. However, among patients with a combination of widespread pain and orofacial pain, such standard treatments are not considered effective and instead multimodal and multidisciplinary strategies are recommended [17]. Participation in a multimodal rehabilitation programme (MMRP) can be effective treatment to improve the long-term prognosis of patients with chronic pain [18]. MMRP is an evidence-based rehabilitation method for patients with chronic pain which also addresses patient-reported outcomes on quality of life and comorbid symptoms. A recent study has shown that orofacial pain is common among patients being treated at a pain rehabilitation clinic [19]. However, it is not known whether an MMRP can also have an effect on the presence of orofacial pain even though that is not the main objective of the programme. Since MMRP is an evidence-based rehabilitation method for patients with chronic pain [20], it is of interest to investigate whether participation in MMRP has an effect on pain in the orofacial region.
The first aim of this study was to evaluate the effect of an MMRP on orofacial pain frequency among participants with orofacial pain. The second aim was to evaluate the effect on quality of life and on psychosocial factors related to chronic pain.
Methods
Study population
Patients aged 18–65 years with chronic pain who participated in an MMRP at the Pain Rehabilitation Clinic, Umeå University Hospital, Sweden, from August 2016 to March 2018 were eligible for inclusion. Patients who completed the MMRP and filled in questionnaires before and after the MMRP were included in the study.
The multimodal pain rehabilitation programme
The MMRP is a team-based goal-oriented programme run by a multidisciplinary team over the course of four consecutive weeks. The timetabled activities include both group sessions and individual sessions based on a biopsychosocial perspective. The multidisciplinary team consists of a physiotherapist, occupational therapist, physician, social worker and a psychologist. The teamwork is integrated using an interdisciplinary approach and the patient is encouraged to take an active part in their rehabilitation process. The MMR programme included physical and occupational therapy, information and training in coping strategies, information about bodily and psychological reactions to chronic pain, relaxation and body-awareness training. All patients also had an individual schedule. No specific treatment targeting the orofacial area in specific was given. At the end of the programme, contacts were established with external collaborating partners such as the workplace, and the patient’s general practitioner.
Procedure
Before(baseline) and after participating in MMRP (follow-up), the patients filled in the questionnaires commonly used for the Swedish Quality Registry for Pain Rehabilitation (SQRP). Orofacial pain was assessed by two screening questions on frequent orofacial pain from the 3Q/TMD [21, 22]:
Do you have pain in your temple, face, jaw or jaw joint once a week or more?
Do you have pain once a week or more when you open your mouth or chew?
Each question is answered with a “yes” and a “no”. Orofacial pain was categorized as positive in the case of an affirmative answer to any of the two questions.
The number of pain sites was registered using 36 pre-defined anatomical areas. The patient reported the number of sites with pain on the left side of the body (n=18) and on the right side of the body (n=18), a total of 36 locations. These pain sites were: (1) head/face, (2) neck, (3) shoulder, (4) upper arm, (5) elbow, (6) forearm, (7) hand, (8) anterior aspect of chest, (9) lateral aspect of chest, (10) belly, (11) sexual organs, (12) upper back, (13) lower back, (14) hip/gluteal area, (15) thigh, (16) knee, (17) shank, and (18) foot. The total score ranges between 1–36.
Patient-reported outcome measures (PROM)
Orofacial pain was regarded as being present when a participant answered affirmatively for at least one of the two screening questions. Pain intensity was assessed using the West Haven-Yale Multidimensional Pain Inventory (WHYMPI), the Swedish version (MPI-S) of on a 7-point numerical rating scale (range 0–6) [23]. Higher scores indicate higher pain intensity.
To evaluate the impact on quality of life, the Short Form Health Survey (SF-36) [24] and the EuroQol 5 Dimensions (EQ-5D) [25] were used. SF-36 intends to represent conditions and limitations in daily life including well-being and personal evaluations of health. The instrument consists of 36 questions comprising eight dimensions reported in a scale 0–100. Higher scores reflect better self-reported health status. This study used the dimensions: physical functioning, role physical, general health, vitality, social functioning, role emotional and mental health. The EQ-5D consists of 2 parts: the EQ-5D (3-L) and the EQ-VAS. This study used the EQ-5D (3-L) that contains 5 dimensions: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. Each dimension has 3 levels: no problems, some problems, and extreme problems. The answers on the 5 dimensions are converted into a single EQ-5D index ranging from −0.594 to 1, where 1 indicates optimal health.
Level of anxiety and depression
The Hospital Anxiety and Depression Scale (HADS) was used for assessment of symptoms indicating anxiety (HADS-A) and depression (HADS-D) [26]. The scale consists of 14 items on a 4-point Likert scale (range 0–3) divided into two subscales- anxiety and depression. The total score range in both scales 0–21. A higher score in each subscale indicates a higher risk of depression and anxiety. The total score is summarized and categorized as normal (0–7), possible, (8–10) or likely (11–21) for indicating anxiety and depression, respectively [27].
Fear of movement
The Swedish version of the Tampa Scale for Kinesiophobia (TSK-SV) was used for assessment of fear of movement [28]. Each of the 17 items are scored by using a 4-point Likert-type scale ranging from disagree to strongly agree. The total score ranges 17–68 points, and a cut-off at 37 points with an error margin of +/−3 points is suggested.
Statistical analysis
Descriptive statistics were used to present patient characteristics before and after the MMRP, using median scores with interquartile range (IQR) and means with standard deviations (SD). For categorical variables, numbers and percentages were presented. Wilcoxon signed-ranked test was used for the study of paired observations and Mann Whitney U test for comparison between groups. Questionnaires with separate missed items in SQRP questionnaires were accepted, and no imputations were made for missing values. An exact McNemar’s test was used to evaluate difference in proportion of participants with orofacial pain before and after intervention. A p-value <0.05 was considered statistically significant.
Results
Lost at follow up
Out of 72 individuals with information on orofacial pain status at baseline, there were 13 (of which 11 women, 84.6 %) who were lost at follow-up (Figure 1). Of those, five individuals (38.5 %) reported orofacial pain at baseline, compared with 50/72 (69.4 %) for the whole group. The mean age was 42.5 (SD 11.6) and 43.8 (SD 9.5) for participants with and without orofacial pain, respectively. There were no significant differences in self-reported level of depression, anxiety nor impact on quality of life among the individuals lost at follow up when compared with the study sample (p=0.3, p=0.4 and p=0.9, respectively).

Flow chart of participants process through the multimodal rehabilitation programme.
Study sample
The final study sample consisted of 59 participants (of which 48 women, 81.9 %) (Table 1). The mean age was 42.9 years (SD 10.9). The median number of pain sites was 16 of 36 (IQR 12). The median pain intensity before MMRP was 4.0 (IQR 1) and after the MMRP 3.5 (IQR 1.5) with a significant decrease over time (Wilcoxon signed ranks test, p=0.005).
Characteristics of the study sample. Orofacial pain (OFP) was assessed from self-reported symptoms of pain once a week or more.
| No OFP | OFP | Total | No OFP | OFP | Total | |
|---|---|---|---|---|---|---|
| Before MMRP | After MMRP | |||||
| Age (mean, SD) | 43.8(9.5) | 42.5(11.6) | 42.88(10.93) | |||
| Gender, women % | 27.1(46.2) | 72.9(53.8) | 81.9(18.1) | 29.2(45.5) | 70.8(54.5) | 81.4(18.6) |
| Anxiety (median, IQR)a | 6(5.5) | 9(5.8) | 8(6) | 8(6) | 9(4) | 8.5(6) |
| Depression (median, IQR)a | 8(5) | 9(5) | 8(5) | 7(5) | 7(5) | 7(5.8) |
| Physical functioningb | 50(33.8) | 55(30) | 55(35) | 50(26.7) | 57.5(28.8) | 55(30) |
| Role physicalb | 0(0) | 0(0) | 0(0) | 0(50) | 0(25) | 0(25) |
| Role emotionalb | 41.7(91.7) | 33.3(100) | 33.3(100) | 66.7(100) | 50(100) | 66.7(100) |
| Vitalityb | 30(28.8) | 25(20) | 25(20) | 35(30) | 30(23.8) | 30(25) |
| Social functioningb | 50(37.5) | 37.5(25) | 50(25) | 50(37.5) | 50(25) | 50(31.2) |
| Mental healthb | 68(27) | 58(24) | 60(28) | 60(20) | 68(23) | 64(22) |
| General healthb | 40(20) | 40(20) | 40(20) | 40(23.8) | 45(25) | 45(25) |
| Kinesiophobiac | 38(6) | 33.5(9.2) | 34(9) | 35(5.5) | 32(10.2) | 34(10.5) |
| Quality of lifed | 0.6(0.6) | 0.2(0.5) | 0.2(0.6) | 0.6(0.6) | 0.3(0.6) | 0.5(0.6) |
-
aAssessed by the hospital anxiety and depression scale (HADS). bAssessed by the 36-Item short form survey instrument (SF-36). Higher scores imply better outcomes. cAssessed by the tampa scale for kinesiophobia (TSK). dAssessed by the EQ-5D.
The frequency of orofacial pain before and after MMRP was n=50 (69.4 %) and n=40 (67.8 %), respectively. There was no significant difference in frequency of orofacial pain from before to after MMRP (McNemar’s test p=0.228).
Among individuals with orofacial pain, there was a significant decrease in the level of indicated self-reported possible depression from before (baseline) to after MMRP (follow-up) (p=0.004) (Figure 2). Apart from this decrease, there was no difference in self-reported level of possible anxiety nor quality of life between individuals with or without orofacial pain, nor between before and after MMRP.
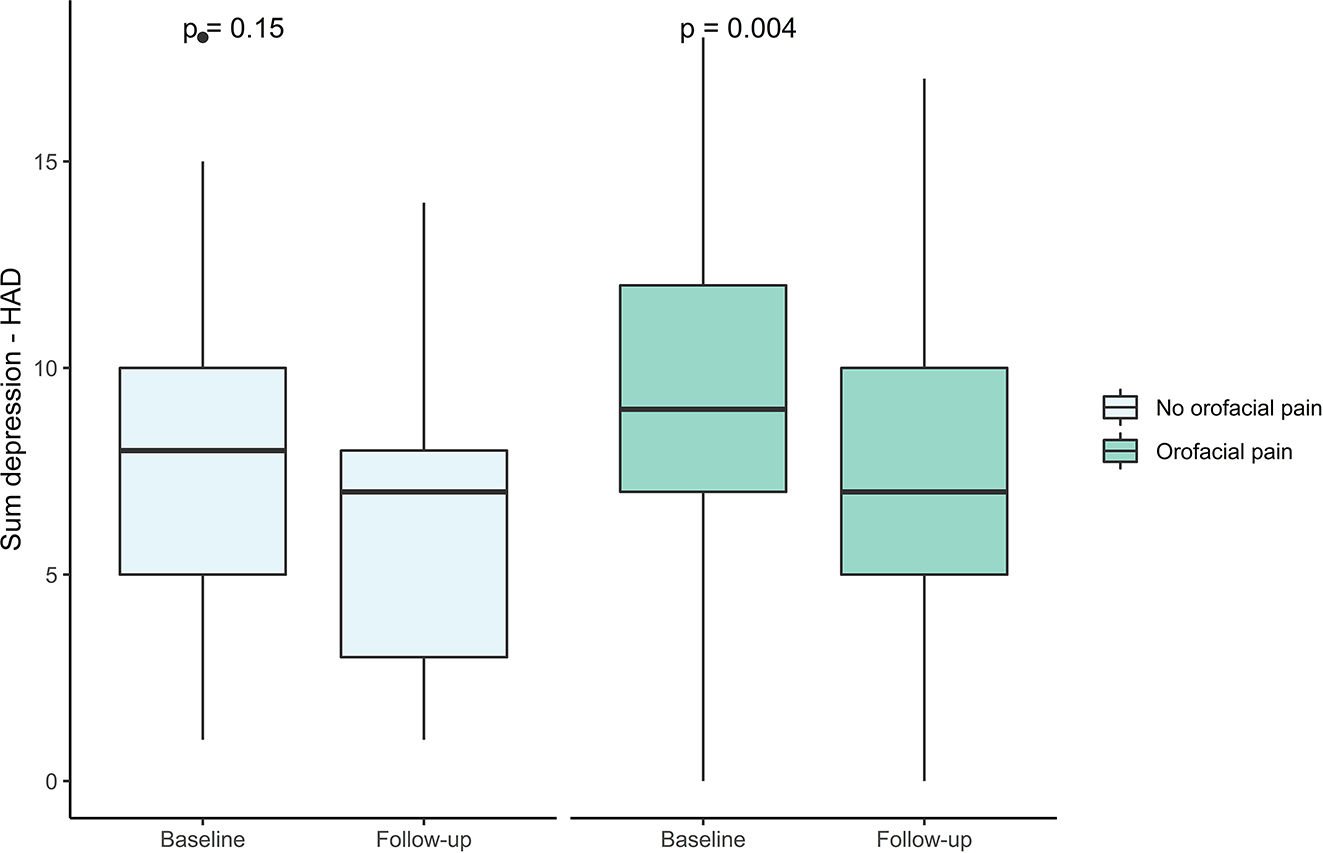
Level of possible depression among individuals with and without orofacial pain respectively, and level of possible depression before and after the multimodal rehabilitation programme.
Discussion
The main finding of this study was that pain intensity decreased significantly after the MMRP in comparison with before while the frequency of orofacial pain was not significantly reduced after completing the rehabilitation programme. Apart from a decrease in level of symptoms indicating depression among individuals with orofacial pain, no differences in quality of life or level of anxiety between the groups were found.
Frequency of orofacial pain before and after MMRP
With an overlap between widespread pain and orofacial pain of about 70 %, our findings are well in line with previous reports on overlap pain [29, 30].
At pain rehabilitation clinics, the professionals working in MMRP have experience of meeting patients suffering from different types of chronic pain conditions. The majority of the interventions in the MMRP are conducted in group sessions based on cognitive-behavioural principles. The programme consists of physical exercises including relaxation and body awareness training, adopting coping strategies according to cognitive-behavioural therapy approaches, and pain education together with education in pain management [31]. When needed, the patients were given individually tailored sessions with different members of the team, for example, individually designed meetings with an occupational therapist, physiotherapist, or psychologist. However, the team members are probably not used to paying attention to functional jaw disorders including orofacial pain, since the two conditions are commonly treated separately today. In clinical practice, it is essential to use methods that are efficient when identifying patients in need of treatment. The present study shows that the 3Q/TMD questionnaire could easily be introduced at pain specialist healthcare clinics, together with an initial clinical assessment by the physician to identify individuals with comorbidity that may need further examination or dental care treatment.
The non-significant decrease in frequency of orofacial pain after completing the programme suggests that the multimodal interventions included in the MMRP may have significant impact on pain intensity but not on frequent orofacial pain alone. When local orofacial pain complaints are related to oral behaviours such as teeth clenching and grinding, a majority of these individuals benefit from information targeting jaw relaxation or the provision of occlusal appliances [32]. The results from this pilot study suggest that in settings like ours, additional screening procedures may be needed to specifically target orofacial pain complaints. In addition, the inclusion of specific information on the jaw system in the MMRP could be both cost-effective and useful for these individuals with orofacial pain.
Psychosocial comorbidities are a well-established clinical challenge among patients with chronic pain, not least since such factors have a negative effect on prognosis. In a previous study of 320 patients with orofacial pain, significant associations between more severe depression and higher pain intensity as well as higher pain-related disability were found [33]. Even though the MMRP did not affect the frequency of orofacial pain, there was a decrease in level of symptoms indicating depression after participation in the programme. This finding reinforces the importance of holistic management of all patients with chronic pain, including orofacial pain. Since this is often not the case in clinical practice today, improvements in collaboration between healthcare and public dental care services are warranted to offer patients who require a proper examination and treatment with the vision of a life with less pain interference in daily life and consequently with increased quality of life. Further studies, using larger samples, are needed to verify the findings of this pilot study.
Strengths and weaknesses
In this study, we used valid questionnaires for the definition of orofacial pain and patient-reported outcome evaluation. Thus, the results mirror the patients ‘self-reported measures’. The study was carried out in a context that can be regarded as optimal, with staff who have considerable experience of pain conditions and rehabilitation. However, selection bias may have occurred where patients with more severe symptoms were possibly more eager and willing to participate in the study. Nevertheless, this would then be the case both among participants with and without orofacial pain. As is the case with most frequent chronic pain conditions, women more commonly suffer from chronic pain conditions than men. The uneven sex distribution with more women than men participating is therefore in line with distributions commonly found in similar settings to ours. We therefore regard our findings as being representative for comparable settings. Given the small sample, potentially significant effects may be undetected and our results should be interpreted with caution. In addition, since patients filled in the questionnaires directly after participating in MMRP, some of the results might be different with a longer follow-up period. Given the importance of optimizing the healthcare organization for patients with complex and overlapping pain complaints, we regard our results as being encouraging for further studies in larger samples including the implementation and evaluation of treatment methods that specifically target orofacial pain.
Conclusions
Even though orofacial pain is common among patients with chronic bodily pain, participation in a multimodal pain programme decreased pain intensity but was not enough to reduce frequent orofacial pain. Among individuals with orofacial pain there was a decrease in level of symptoms indicating depression. These findings suggest that orofacial pain assessment and management could be a reasonable additional part of the evaluation of patients prior to participation in multimodal rehabilitation programs for bodily pain.
-
Research funding: Authors state no funding involved.
-
Author contributions: All authors have accepted responsibility for the entire content of this manuscript and approved its submission
-
Competing interests: Authors state no conflict of interest.
-
Informed consent: Informed consent has been obtained from all individuals included in this study.
-
Ethical approval: Research involving human subjects complied with all relevant national regulations, institutional policies and is in accordance with the tenets of the Helsinki Declaration (as amended in 2013), and has been approved by the Regional Ethical Review Board in Umeå, Sweden 2016/227-31.
References
1. Treede, RD, Rief, W, Barke, A, Aziz, Q, Bennett, MI, Benoliel, R, et al.. Chronic pain as a symptom or a disease: the IASP classification of chronic pain for the international classification of diseases (ICD-11). Pain 2019;160:19–27. https://doi.org/10.1097/j.pain.0000000000001384.Suche in Google Scholar PubMed
2. Treede, RD, Rief, W, Barke, A, Aziz, Q, Bennett, MI, Benoliel, R, et al.. A classification of chronic pain for ICD-11. Pain 2015;156:1003–7. https://doi.org/10.1097/j.pain.0000000000000160.Suche in Google Scholar PubMed PubMed Central
3. Breivik, H, Collett, B, Ventafridda, V, Cohen, R, Gallacher, D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain 2006;10:287–333. https://doi.org/10.1016/j.ejpain.2005.06.009.Suche in Google Scholar PubMed
4. Bergman, S, Herrström, P, Högström, K, Petersson, IF, Svensson, B, Jacobsson, LT. Chronic musculoskeletal pain, prevalence rates, and sociodemographic associations in a Swedish population study. J Rheumatol 2001;28:1369–77.Suche in Google Scholar
5. Häggman-Henrikson, B, Liv, P, Ilgunas, A, Visscher, CM, Lobbezoo, F, Durham, J, et al.. Increasing gender differences in the prevalence and chronification of orofacial pain in the population. Pain 2020;161:1768–75.10.1097/j.pain.0000000000001872Suche in Google Scholar PubMed PubMed Central
6. Kleykamp, BA, Ferguson, MC, McNicol, E, Bixho, I, Arnold, LM, Edwards, RR, et al.. The prevalence of comorbid chronic pain conditions among patients with temporomandibular disorders: a systematic review. J Am Dent Assoc 2022;153:241–50. https://doi.org/10.1016/j.adaj.2021.08.008.Suche in Google Scholar PubMed
7. John, MT, Miglioretti, DL, LeResche, L, Von Korff, M, Critchlow, CW. Widespread pain as a risk factor for dysfunctional temporomandibular disorder pain. Pain 2003;102:257–63. https://doi.org/10.1016/s0304-3959(02)00404-9.Suche in Google Scholar
8. Slade, GD, Greenspan, JD, Fillingim, FB, Maixner, W, Sharma, S, Ohrbach, R, et al.. Overlap of five chronic pain conditions: temporomandibular disorders, headache, back pain, irritable bowel syndrome, and fibromyalgia. J Oral Facial Pain Headache 2020;34:s15-28. https://doi.org/10.11607/ofph.2581.Suche in Google Scholar PubMed PubMed Central
9. Fillingim, RB, Ohrbach, R, Greenspan, JD, Knott, C, Diatchenko, L, Dubner, R, et al.. Psychological factors associated with development of TMD: the OPPERA prospective cohort study. J Pain 2013;14:T75–90. https://doi.org/10.1016/j.jpain.2013.06.009.Suche in Google Scholar PubMed PubMed Central
10. Rogers, AH, Farris, SG. A meta-analysis of the associations of elements of the fear-avoidance model of chronic pain with negative affect, depression, anxiety, pain-related disability and pain intensity. Eur J Pain 2022;26:1611–35. https://doi.org/10.1002/ejp.1994.Suche in Google Scholar PubMed PubMed Central
11. Shueb, SS, Nixdorf, D, John, M, Alonso, BF, Durham, J. What is the impact of acute and chronic orofacial pain on quality of life? J Dent 2015;43:1203–10. https://doi.org/10.1016/j.jdent.2015.06.001.Suche in Google Scholar PubMed
12. Macfarlane, TV, Blinkhorn, AS, Davies, RM, Kincey, J, Worthington, HV. Factors associated with health care seeking behaviour for orofacial pain in the general population. Community Dent Health 2003;20:20–6.Suche in Google Scholar
13. Blyth, FM, March, LM, Brnabic, AJ, Cousins, MJ. Chronic pain and frequent use of health care. Pain 2004;111:51–8. https://doi.org/10.1016/j.pain.2004.05.020.Suche in Google Scholar PubMed
14. Becker, A, Held, H, Redaelli, M, Strauch, K, Chenot, JF, Leonhardt, C, et al.. Low back pain in primary care: costs of care and prediction of future health care utilization. Spine 2010;35:1714–20. https://doi.org/10.1097/brs.0b013e3181cd656f.Suche in Google Scholar PubMed
15. Argueta-Figueroa, L, Flores-Mejía, LA, Ávila-Curiel, BX, Flores-Ferreyra, BI, Torres-Rosas, R. Nonpharmacological interventions for pain in patients with temporomandibular joint disorders: a systematic review. Eur J Dermatol 2022;16:500–13. https://doi.org/10.1055/s-0041-1740220.Suche in Google Scholar PubMed PubMed Central
16. Eliassen, M, Hjortsjö, C, Olsen‐Bergem, H, Bjørnland, T. Self-exercise programmes and occlusal splints in the treatment of TMD-related myalgia-evidence-based medicine? J Oral Rehabil 2019;46:1088–94. https://doi.org/10.1111/joor.12856.Suche in Google Scholar PubMed
17. Raphael, KG, Marbach, JJ. Widespread pain and the effectiveness of oral splints in myofascial face pain. J Am Dent Assoc 2001;132:305–16. https://doi.org/10.14219/jada.archive.2001.0173.Suche in Google Scholar PubMed
18. Kamper, SJ, Apeldoorn, AT, Chiarotto, A, Smeets, RJEM, Ostelo, RWJG, Guzman, J, et al.. Multidisciplinary biopsychosocial rehabilitation for chronic low back pain: cochrane systematic review and meta-analysis. Brit Med J 2015;350:h444. https://doi.org/10.1136/bmj.h444.Suche in Google Scholar PubMed PubMed Central
19. Stalnacke, C, Ganzer, N, Liv, P, Wänman, A, Lövgren, A. Prevalence of temporomandibular disorder in adult patients with chronic pain. Scand J Pain 2021;21:41–7. https://doi.org/10.1515/sjpain-2020-0077.Suche in Google Scholar PubMed
20. Gerdle, B, Fischer, MR, Ringqvist, Å. Interdisciplinary pain rehabilitation programs: evidence and clinical real-world results. In: Alice, W, editor. Pain management – from pain mechanisms to patient care. Rijeka: IntechOpen; 2022.Suche in Google Scholar
21. Lövgren, A, Visscher, CM, Häggman-Henrikson, B, Lobbezoo, F, Marklund, S, Wänman, A. Validity of three screening questions (3Q/TMD) in relation to the DC/TMD. J Oral Rehabil 2016;43:729–36. https://doi.org/10.1111/joor.12428.Suche in Google Scholar PubMed
22. Lovgren, A, Parvaneh, H, Lobbezoo, F, Häggman-Henrikson, B, Wänman, A, Visscher, CM. Diagnostic accuracy of three screening questions (3Q/TMD) in relation to the DC/TMD in a specialized orofacial pain clinic. Acta Odontol Scand 2018:1–7. https://doi.org/10.1080/00016357.2018.1439528.Suche in Google Scholar PubMed
23. Kerns, RD, Turk, DC, Rudy, TE. The West Haven-Yale multidimensional pain inventory (WHYMPI). Pain 1985;23:345–56. https://doi.org/10.1016/0304-3959(85)90004-1.Suche in Google Scholar PubMed
24. Ware, JEJr, Sherbourne, CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 1992;30:473–83. https://doi.org/10.1097/00005650-199206000-00002.Suche in Google Scholar
25. Rabin, R, de Charro, F. EQ-5D: a measure of health status from the EuroQol Group. Ann Med 2001;33:337–43. https://doi.org/10.3109/07853890109002087.Suche in Google Scholar PubMed
26. Zigmond, AS, Snaith, RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361–70. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x.Suche in Google Scholar PubMed
27. Bjelland, I, Dahl, AA, Haug, TT, Neckelmann, D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res 2002;52:69–77. https://doi.org/10.1016/s0022-3999(01)00296-3.Suche in Google Scholar PubMed
28. Bunketorp, L, Carlsson, J, Kowalski, J, Stener-victorin, E. Evaluating the reliability of multi-item scales: a non-parametric approach to the ordered categorical structure of data collected with the Swedish version of the Tampa Scale for Kinesiophobia and the Self-Efficacy Scale. J Rehabil Med 2005;37:330–4. https://doi.org/10.1080/16501970510036411.Suche in Google Scholar PubMed
29. Aaron, LA, Burke, MM, Buchwald, D. Overlapping conditions among patients with chronic fatigue syndrome, fibromyalgia, and temporomandibular disorder. Arch Intern Med 2000;160:221–7. https://doi.org/10.1001/archinte.160.2.221.Suche in Google Scholar PubMed
30. Ohrbach, R, Sharma, S, Fillingim, R, Greenspan, J, Rosen, J, Slade, G. Clinical characteristics of pain among five chronic overlapping pain conditions. J Oral Facial Pain Headache 2020;34:s29–s42. https://doi.org/10.11607/ofph.2573.Suche in Google Scholar PubMed PubMed Central
31. Ringqvist, A, Dragioti, E, Björk, M, Larsson, B, Gerdle, B. Moderate and stable pain reductions as a result of interdisciplinary pain rehabilitation-a cohort study from the Swedish quality Registry for pain rehabilitation (SQRP). J Clin Med 2019;8. https://doi.org/10.3390/jcm8060905.Suche in Google Scholar PubMed PubMed Central
32. Kostrzewa-Janicka, J, Mierzwinska-Nastalska, E, Rolski, D, Szczyrek, P. Occlusal stabilization splint therapy in orofacial pain and tension-type headache. Adv Exp Med Biol 2013;788:181–8. https://doi.org/10.1007/978-94-007-6627-3_27.Suche in Google Scholar PubMed
33. Su, N, Lobbezoo, F, van Wijk, A, van der Heijden, GJMG, Visscher, CM. Associations of pain intensity and pain-related disability with psychological and socio-demographic factors in patients with temporomandibular disorders: a cross-sectional study at a specialised dental clinic. J Oral Rehabil 2017;44:187–96. https://doi.org/10.1111/joor.12479.Suche in Google Scholar PubMed
© 2023 Walter de Gruyter GmbH, Berlin/Boston
Artikel in diesem Heft
- Frontmatter
- Editorial Comment
- What do we mean by “biopsychosocial” in pain medicine?
- Systematic Review
- The efficacy of manual therapy on HRV in those with long-standing neck pain: a systematic review
- Clinical Pain Research
- Development of a binary classifier model from extended facial codes toward video-based pain recognition in cancer patients
- Experience and usability of a website containing research-based knowledge and tools for pain self-management: a mixed-method study in people with high-impact chronic pain
- Effect on orofacial pain in patients with chronic pain participating in a multimodal rehabilitation programme – a pilot study
- Analysis of Japanese nationwide health datasets: association between lifestyle habits and prevalence of neuropathic pain and fibromyalgia with reference to dementia-related diseases and Parkinson’s disease
- Impact of antidepressant medication on the analgetic effect of repetitive transcranial magnetic stimulation treatment of neuropathic pain. Preliminary findings from a registry study
- Does lumbar spinal decompression or fusion surgery influence outcome parameters in patients with intrathecal morphine treatment for persistent spinal pain syndrome type 2 (PSPS-T2)
- Original Experimentals
- Low back-pain among school-teachers in Southern Tunisia: prevalence and predictors
- Economic burden of osteoarthritis – multi-country estimates of direct and indirect costs from the BISCUITS study
- Demographic and clinical factors associated with psychological wellbeing in people with chronic, non-specific musculoskeletal pain engaged in multimodal rehabilitation: –a cross-sectional study with a correlational design
- Interventional pathway in the management of refractory post cholecystectomy pain (PCP) syndrome: a 6-year prospective audit in 60 patients
- Original Articles
- Preoperatively assessed offset analgesia predicts acute postoperative pain following orthognathic surgery
- Oxaliplatin causes increased offset analgesia during chemotherapy – a feasibility study
- Effects of conditioned pain modulation on Capsaicin-induced spreading muscle hyperalgesia in humans
- Effects of oral morphine on experimentally evoked itch and pain: a randomized, double-blind, placebo-controlled trial
- The potential effect of walking on quantitative sensory testing, pain catastrophizing, and perceived stress: an exploratory study
- What matters to people with chronic musculoskeletal pain consulting general practice? Comparing research priorities across different sectors
- Is there a geographic and gender divide in Europe regarding the biopsychosocial approach to pain research? An evaluation of the 12th EFIC congress
Artikel in diesem Heft
- Frontmatter
- Editorial Comment
- What do we mean by “biopsychosocial” in pain medicine?
- Systematic Review
- The efficacy of manual therapy on HRV in those with long-standing neck pain: a systematic review
- Clinical Pain Research
- Development of a binary classifier model from extended facial codes toward video-based pain recognition in cancer patients
- Experience and usability of a website containing research-based knowledge and tools for pain self-management: a mixed-method study in people with high-impact chronic pain
- Effect on orofacial pain in patients with chronic pain participating in a multimodal rehabilitation programme – a pilot study
- Analysis of Japanese nationwide health datasets: association between lifestyle habits and prevalence of neuropathic pain and fibromyalgia with reference to dementia-related diseases and Parkinson’s disease
- Impact of antidepressant medication on the analgetic effect of repetitive transcranial magnetic stimulation treatment of neuropathic pain. Preliminary findings from a registry study
- Does lumbar spinal decompression or fusion surgery influence outcome parameters in patients with intrathecal morphine treatment for persistent spinal pain syndrome type 2 (PSPS-T2)
- Original Experimentals
- Low back-pain among school-teachers in Southern Tunisia: prevalence and predictors
- Economic burden of osteoarthritis – multi-country estimates of direct and indirect costs from the BISCUITS study
- Demographic and clinical factors associated with psychological wellbeing in people with chronic, non-specific musculoskeletal pain engaged in multimodal rehabilitation: –a cross-sectional study with a correlational design
- Interventional pathway in the management of refractory post cholecystectomy pain (PCP) syndrome: a 6-year prospective audit in 60 patients
- Original Articles
- Preoperatively assessed offset analgesia predicts acute postoperative pain following orthognathic surgery
- Oxaliplatin causes increased offset analgesia during chemotherapy – a feasibility study
- Effects of conditioned pain modulation on Capsaicin-induced spreading muscle hyperalgesia in humans
- Effects of oral morphine on experimentally evoked itch and pain: a randomized, double-blind, placebo-controlled trial
- The potential effect of walking on quantitative sensory testing, pain catastrophizing, and perceived stress: an exploratory study
- What matters to people with chronic musculoskeletal pain consulting general practice? Comparing research priorities across different sectors
- Is there a geographic and gender divide in Europe regarding the biopsychosocial approach to pain research? An evaluation of the 12th EFIC congress

