Effects of dynamic stabilization exercises and muscle energy technique on selected biopsychosocial outcomes for patients with chronic non-specific low back pain: a double-blind randomized controlled trial
Abstract
Objectives
Low back pain is the most prevalent musculoskeletal condition, and causes activity limitations which result in reduced work productivity and high medical expenditure. The management of this condition has been challenging to both clinicians and researchers. While the use of Muscle Energy Technique (MET) as a potentially effective treatment strategy seems promising, studies examining MET combined with exercise therapy are scarce and studies with strong methodology are lacking. Therefore, this study aims to determine the effects of a combination of Dynamic Stabilization Exercises (DSE) and MET on selected biopsychosocial outcomes compared to DSE alone or conventional physiotherapy in the management of chronic non-specific low back pain (NSLBP).
Methods
A total of 125 (80 male and 45 female) patients with chronic NSLBP were involved in this study, they were recruited from Rasheed Shekoni Teaching hospital and Federal Medical centre Birnin-Kudu, Jigawa State, Nigeria. A random number generator method was used to allocate patients to either DSE + MET (n=41), DSE alone (n=39) or conventional physiotherapy (n=45). Interventions were administered twice a week over 12 weeks. Outcome measures included pain intensity, lumbar (flexion and extension) range of motion, functional-disability, self-perceived health status, limitations in activities and participation restrictions. These were assessed at baseline, mid-intervention at six weeks, post-intervention at 12 weeks and long term follow-up at 24 weeks. Data was analyzed using repeated-measures ANOVA to determine significance difference within groups and between groups.
Results
All intervention groups showed within-groups changes of the study outcomes over time (p<0.001). However, between-group comparisons showed greater improvements in pain intensity (F=7.91, p<0.001), lumbar ROM (flexion F=1.51, p<0.001; extension F=3.25, p<0.001), activity limitations/participation restrictions (F=3.7, p<0.001) and health status (F=10.9, p<0.001) for the intervention in which MET and DSE were combined. The MET plus DSE interventions were superior to DSE and convention physiotherapy for all outcome measures, except for functional disability (F=0.53, p=0.590).
Conclusions
The data from this study showed MET combined with DSE had greater therapeutic benefits compared to DSE or conventional physiotherapy on selected biopsychosocial outcomes in patients with chronic NSLBP. The findings from the study show that the combination of MET with DSE is safe and has beneficial effects in the management of patients with chronic NSLBP.
Clinical trial registration
The study protocol has been registered with www.ClinicalTrial.gov with the registration number NCT3449810.
Introduction
Low Back Pain (LBP) has a high global prevalence, with estimations ranging between 30 and 80% among the general population [1]. It is the most prevalent musculoskeletal condition in both developed and developing nations. The condition is associated with a high disease burden and has been listed by the Global Burden of Disease (GBD) on the 6th place out of 291 conditions [2]. This results in significant activity limitations, reductions in work productivity and a high medical expenditure incurring billions of dollars annually [2], [3]. The prevalence of the condition has been associated with lower socioeconomic status and lower education levels [4], [5], [6], and therefore it has been postulated that the burden of LBP is greater in lower and middle-income countries like Africa [7], [8]. The prognosis after an acute episode of LBP is not favourable, as 60–80% of the patients will experience recurrence or persistence of their LBP complaints [6], [9].
Currently, the management of LBP is challenging because of its complexity, high cost and unpredictable outcomes [10], [11]. Single model interventions for LBP have demonstrated little or no effect [12], [13]. Little is known about the precise causes of LBP, and a clear patho-anatomic diagnosis cannot be identified in 85% of the patients labelling them with non-specific LBP (NSLBP) [14]. There is evidence that biopsychosocial factors play a role in the development of chronic NSLBP, and the biopsychosocial model of chronic pain is gaining widespread acceptance as the appropriate framework for understanding and managing chronic NSLBP [5], [13].
From a biophysical perspective, structural and functional alterations of the back muscles have been demonstrated in NSLBP [14], [15], [16], [17]. Muscle functional alterations seem to play a crucial contributing factor to the persistence of NSLBP, as an optimal function of the back muscles is a prerequisite for static and dynamic control of spinal flexibility and movement. From a psychological perspective, NSLBP patients are known to suffer from higher levers of fear-avoidance, depression, and anxiety, and reduced self-efficacy [12], [18]. Psychological factors have been shown to play an important role in the chronification process of NSLBP [18], [19], [20] and the treatment prognosis of chronic NSLBP [21], [22]. As previously mentioned, factors like economic and social status contribute to the societal component of NSLBP, but other factors such as cultural traditions, social support, and availability of medical care can also contribute to the pain disability [23]. The use of therapeutic interventions that address musculoskeletal dysfunctions within a combined treatment approach can be justified within the biopsychosocial model of chronic pain. Psychosocial factors like stress can increase muscle tension, which exacerbates pain [5], [13], [24]. Other psychosocial factors like anxiety and fear have been linked to dysfunctional back muscle contractions and decreased lumbar flexion in patients with chronic NSLBP [5], [24]. Based on these interactions Geisser et al. [24], [25], suggested a successful management programs of chronic NSLBP should address both psychosocial factors and musculoskeletal dysfunction that contribute to pain.
Dynamic stabilization exercises (DSE) are used as a treatment approach to improve neuromuscular functions of muscles that are central in maintaining dynamic spinal and trunk stability [26], [27], [28]. While anecdotal reports in the literature suggest that DSE may also lead to improvement of biopsychosocial outcomes in patients with NSLBP, no studies have documented this assumption [26]. While there is evidence for the presence of musculofascial deficits in chronic NSLBP, which can arise from injuries or repetitive negative motor patterns reflected by compensatory mechanisms, accumulation of muscular tension, motor limitations, stress and functional disorders [29], [30], [31], the treatment of the musculofascial system is not addressed during DSE. A way to approach this is to combine DSE with muscle energy techniques (MET) as the latter can be used to address musculofascial drivers of pain. While MET is often used for the treatment of NSLBP, there is a lack of empirical evidence on its effectiveness in this population due to the lack of studies with a robust methodology [32], [33]. MET might potentiate the therapeutic effects of DSE, by relaxing and stretching contracted musculature, strengthening weak muscles, reducing muscular tension, improving joint mobility and normalizing motor function [31], [32], [34], [35].
This study aimed to determine the effectiveness of the combination of DSE intervention with MET and to compare the therapeutic outcomes of the intervention with DSE as a standalone treatment or with conventional physiotherapy in patients with chronic NSLBP. The study evaluates the treatment effects on biopsychosocial outcomes of pain intensity, lumbar range of motion, functional disability, health status, limitations in activities and participation restrictions by evaluating changes in time (i.e. baseline, mid intervention at the 6th week, post-intervention at the 12th week and long term follow up at the 24th week) and between intervention groups (i.e. DSE + MET, DSE alone and conventional physiotherapy), and finally the interaction between the time and groups effects. Therefore, we hypothesized that the combined therapeutic effects of DSE and MET would result in concomitant positive effects for the biopsychosocial outcomes associated with chronic NSLBP as compared to the effects of a single model regime which could be expressed by greater changes in magnitudes of the outcome measures and longer retention of the treatment effects following interventions.
Methods
Participants
This is a two-centred parallel-group randomized control trial recruited 137 (male=85 and female=52) patients who were diagnosed with chronic NSLBP by a physician and referred for physiotherapy treatment. Patients were recruited from the Rasheed Shekoni Specialist Hospital and Birnin–Kudu Federal Medical Centre, both located in the Jigawa State of Nigeria. An advert calling for volunteers to participate in the study was posted on all the notice boards of the two hospitals. All interested volunteers were requested to notify examiner (the study physician) via email, text message or self-reporting. The examiner screened them using the inclusion criteria to determine whether participants were eligible for study participation.
Eligibility criteria for participants were: age range of 20–55 years; NSLBP with a duration of minimum 24 weeks or longer and with associated pain in the lower extremity and lumbopelvic area; lumbar hypomobility and mobility deficits of the thorax and hip regions [36] as confirmed by a physiotherapist with expertise in manual therapy; decreased muscle power of the trunk and pelvis; movement restrictions during recreational and/or occupational activities. Participants were excluded if they had: LBP of a specific nature (e.g. due to fractures, malignant tumours, ankyloses, infections, or pregnancy); LBP with radiating pain due to nerve root involvement; been on immunosuppression or steroid medication; spinal deformities; a history of severe rheumatic, orthopaedic, cardiovascular or neurologic disorders in the last three months before study participation. Furthermore, eligible patients were also re-evaluated (prescreening) using the central sensitization inventory (CSI) [37] to screen for central sensitization pain and using the Tampa scale for kinesiophobia (TSK) [38] to screening for fear of (re)injury due to movement or activities. Scores of 29 for CSI and less than 37 for TSK respectively were used as a cut-off and patients obtaining higher scores were not eligible for study inclusion. This was done to make the sample more homogenous.
Patients were requested to notify the researchers if they had alternate therapies or changed their medication during participation to the study, but none reported receiving alternate therapy or changed medications.
The flow of the participants throughout the study is depicted in Figure 1. The study protocol was approved by the University of KwaZulu-Natal Biomedical Research Ethics Committee (Ethics Number: BFC198/18). Data was collected from January 2018 to December 2019. Confidentiality of patient-related personal and clinical information was strictly protected.
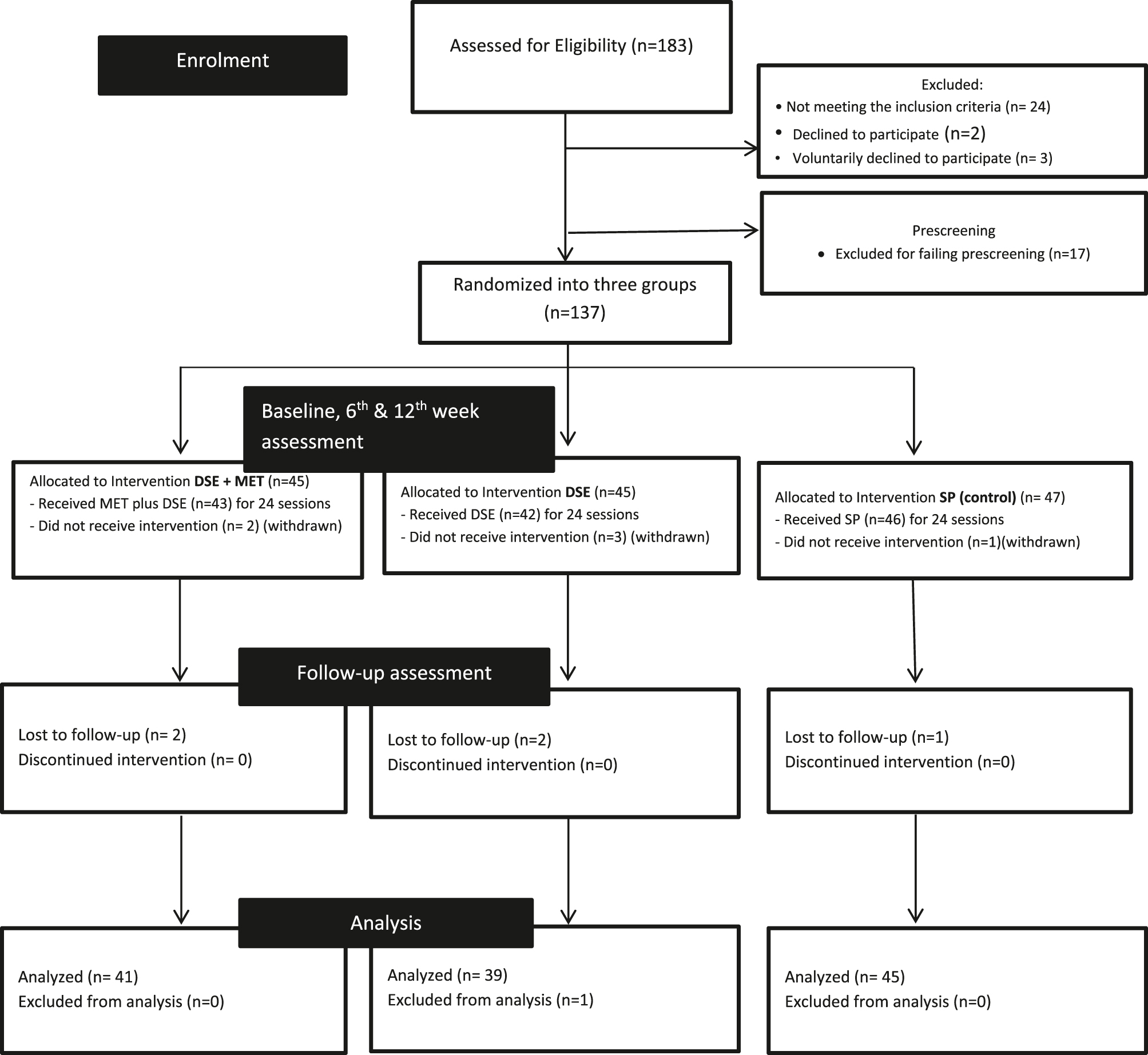
Outline of the study CONSORT flow diagram from enrolment to analysis. After baseline assessments, six participants were withdrawn from the study because they could not avail themselves after baseline assessments in the groups and thus withdrawn. Additionally, five participants were lost to follow-up assessment due to challenges with transportation and/or work-related responsibilities and one participant in the DSE group had incomplete data, therefore they were excluded from the analysis.
Sample size
The sample size was estimated using G*Power 3.1.9.2. The following parameters were used: the power of the study=85%, level of significance=0.05, number of groups=3 (DSE, DSE + MET), and conventional physiotherapy), number of repeated measurements=4, expected medium effect size=0.25 [39], anticipated dropout rate=30%. The initial calculated sample size 147 (i.e. 49 participants for each intervention group).
Measurements
Three physiotherapists were trained to perform the study assessments. All outcome measures were assessed at baseline, week 6 (mid-treatment), week 12 (post-treatment), and week 24 (post-treatment).
Outcome measures
Pain: The 11-point Numeric Pain Rating Scale (NPRS) was used for assessing pain intensity. This scale is commonly used in the scientific literature and clinical practice, as it is reliable and responsive in LBP (r=0.61) and has a minimal clinically important difference of 1.99 points [40]. Participants rated their present, lowest and worst level of pain during the preceding 24 h [40]. The average of these three ratings was used to represent the participants’ overall pain intensity.
Lumbar range of motion: An inclinometer was used for measuring lumbar range of flexion and extension. The body landmarks were the thoracolumbar junction (lower edge of the T12 vertebral bone) and the upper edge of the sacrum [41]. The inclinometer was placed at the junction of the thoracolumbar and sacrum with the patient in a neutral position. The patient was instructed to flex maximally and the difference in motion represented the lumbar flexion range after which the patient extended maximally and the difference in motion was recorded and reflected the lumbar extension range [41]. Petra et al. [41] reported high reliability and validity for inclinometer by comparing this assessment procedure with the radiological determination of the range of motion (ROM) (r=0.93). The estimated lumbar flexion and extension under clinical conditions being 40.9° and 11.8° respectively.
Functional disability: The Oswestry Disability Index (ODI) is a commonly used questionnaire to determine the level of functional disability in patients with LBP, as it has been recognized as an acceptable standard with established reliability, validity and responsiveness [42]. The ODI consist of 10 items, of which eight relate to activities of daily living and two relate to pain. Each item is scored from 0‒5 and the total score is expressed as a percentage with high scores corresponding to greater disability [43]. The minimum clinically important difference on the ODI, which interventions should reach to have an effective impact on LBP related functional disability, is estimated to be 11% [42]. Adamu et al. [44] reported that the Hausa version of the ODI, which was used in this study, has adequate psychometric properties equivalent to the English version (r=0.937, 0.75).
Activity limitations and participation restrictions: The Orebro Musculoskeletal Pain Screening Questionnaire (OMPSQ) consists of 25 items, with items 1–4 are used to collect sociodemographic information, and the remaining 21 being scored. 21 items are scored, covering pain experience (five items), physical functioning (five items), coping (one item), job satisfaction (one item), anxiety/stress (one item), depression (one item), fear-avoidance beliefs (three items), recovery expectations (two items), heavy or monotonous work (one item), and sick leave (one item). Miscellaneous items relating to age, sex, and nationality [45], [46]. Each item is scored from 0 to 10 [45]. The scored items were summed to obtain a total score ranging from 0 to 210; a higher score indicates a higher disability. A score of <105 points indicates low disability, as a score between 105 and 130 points moderate disability, and a score of >130 points high disability [45], [47]. The ÖMPSQ can also be used to identify LBP patients at risk for chronicity and prolonged disability, therefore a score of <90 indicates low risk, a score of 90–105 moderate risk, and a score of >105 high risks [48]. Gabel et al. [49] reported that the ÖMPSQ has high reliability (0.975) and was strongly correlated with recovery time (Spearman’s r=0.71). Also, Ahmed et al. [50] reported that the Hausa version of the ÖMPSQ, which was used in this study, has adequate psychometric properties which are equivalent to these of the English version (reliability r=0.80, internal consistency α=0.72).
Measurement of self-perceived changes in health status: The Global Rating of Change (GROC) scale was used to determine the participants’ overall perceived treatment effect. Scores ranged from −7 (being a great deal worse) to 0 (was about the same) to +7 (being a great deal better). Jaeschke et al. [51] reported that scores of ±1 to ±3 represent small changes, scores of ±4 to ±5 represent moderate changes, and scores of ±6 to ±7 represent large changes perceived due to the treatment. The GROC has adequate test–retest reliability (ICC 0.90) and is sensitive to change (standardized response mean 0.5–2.714, 7-point), with a minimal detectable change of 0.45 points on seven points and a minimal clinically important change of two points on seven points) [52].
Study interventions
Before each intervention, patients were given a 10-min lecture providing information and advice on NSLBP, describing self-help strategies and the benefits of spinal and abdominal exercises. Patients were encouraged to stay active because inactivity could worse their pain. All the study interventions were administered and/or supervised by physiotherapists with a postgraduate qualification in musculoskeletal physiotherapy, who received additional training in regards to execution and standardization of the study interventions. Each session of the interventions were performed twice a week in the hospital and supplemented with home strengthening exercises for the spinal and abdominal muscles (i.e. prone trunk extensions and planks for 5 min, bridging exercises for 5 min and sides bridging exercises for 5 min) [31] which were performed on days when not attending the hospital. The total intervention period was 12 weeks.
Dynamic Stabilization Exercise (DSE) intervention: Patients in this group received DSE as a standalone intervention, which comprised seven exercises at each session as prescribed by Moon et al. [26]. The exercises are (1) Bridging, (2) Supine twist stretch, (3) Double leg knee to chest, (4) Plank heel raised, (5) Ball squat, (6) Leg press on the Swiss ball, (7) Hip lifts, most of the exercises had 12 repetitions performed with 5 s rest interval, except for two (Ball squat and Leg press on Swiss ball) which had 25 repetitions with 5 s rest interval as indicated below.
The primary aim of these exercises was to improve neuromuscular control, strength and endurance of the lumbar core stabilizers, i.e. TrA, multifidus, rectus abdominus, erector spinae, quadratus lumborum, and the internal and external oblique muscles. The duration of a DSE session was 35 min, which included 3 min of warm-up stretching exercises (front and side lunges) and 2 min of cool-down exercise which consisted of cycling on an ergometer [26]. See Figure 2 for the picture demonstration of the DSE exercises.
Dynamic Stabilization Exercise combined with Muscle Energy Technique (DSE + MET) intervention: The MET procedure was adopted from the work of Szulc et al. [31]. MET is a post-isometric relaxation technique dependent on the direction of movement limitation in the thoracolumbar region. The procedure is based on the following specific parameters: (1) the duration of the isometric voluntary contractions in 30 s with 5 s of rest in-between consecutive contractions; (2) the intensity of the contractions corresponds to 20–35% of maximum isometric voluntary contraction (MIVC); (3) begins in the intermediate extent of movement restriction for a given patient; (4) loss on movement restrictions pushed to next restrictive barriers, segments when the participant was completely relaxed; (5) this was followed by contraction of the antagonist muscle at the end phase of the contractions; (6) passive return to the rest position. The protocol of these exercises requires the relaxation of erector spinae muscle group and is performed with the patient seated on a stool or the edge of a treatment bed. The therapist stands to the left and posterior to the patient who has the right hand placed on the left shoulder with the therapist’s left hand grasping the patient’s right shoulder. The therapist identifies the area and extent of movement restrictions and performs left rotation, right side bending, trunk flexion and extension until the movement restriction is slowly released. This is repeated for the opposite side to balance the muscular tension of the erector spinae and to resolve the disorder of the musculofascial system in the thoracolumbar region [25], [31].
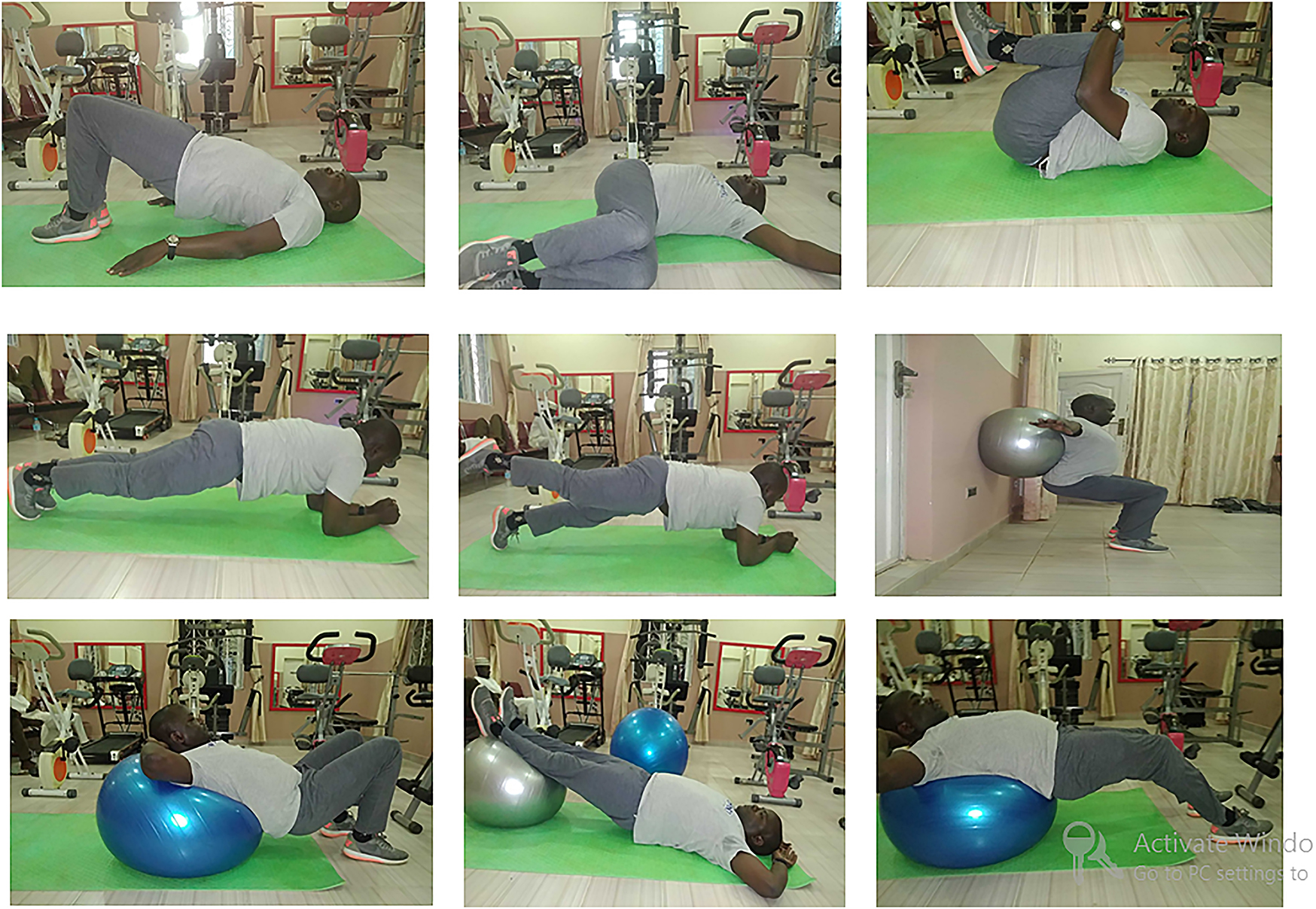
Dynamic stabilization exercises (illustrated by the first author).
This MET procedure was combined with the previous described DSE. MET was performed by a physiotherapist with MET certification and exercises were performed under supervision. The total treatment duration of this group was 45 min per session (MET 10 min and DES 35 min), the MET procedure was demonstrated in Figure 3.
Conventional physiotherapy intervention: Patients in this group received conventional physiotherapy treatment for chronic NSLBP in Nigeria [53], [54], [55]. This involves the use of therapeutic massage (comprising of effleurages, petrissages, stripping, frictions and tapping) using methyl salicylate as a coupling medium, and a combination (COMBO) of interferential electrotherapy (treatment dose frequency: 4,000 Hz, base frequency: 90 Hz, sweep frequency: 40 Hz, polarity: bipolar (two electrodes), duration: 6 min) and therapeutic ultrasound (treatment dose frequency: 1 MHz, intensity: 0.8 W/cm2, mode: continuous mode, duration: 4 min) using the Sonicator Plus 920® apparatus (Mettler Electronics Corp., Anaheim, CA, USA), which were applied bilaterally on the lumbosacral region. Additionally, patients performed general exercises from the prone, supine and lateral position in order to improve muscle endurance and strength of the spinal and abdominal muscles, relaxation capacity of the lumbopelvic muscles and flexibility of the lumbopelvic joint.

Muscles energy techniques (permission has been obtained from the subject).
Massage and interferential therapy combined with ultrasound were applied for 10 min each by a physiotherapist, and general exercises were performed for 15 min under supervision. The total treatment duration of this group was 45 min per session.
Randomization and blinding
After the participants were selected an independent researcher used a random number generator method to allocate the participants to one of the three intervention groups. Two study assessors took measurements of all outcomes at baseline and were blinded to group allocation and the participants were instructed not to disclose their study allocation to the assessors. The group allocation per participant was preserved in a sealed opaque envelope, which was opened after the baseline assessments were performed. The study assessors repeat the assessments at 6th week, 12th week and 24th-week post-intervention (follow-up). Additionally, participants were expected to be unaware of their group procedure/intervention including those in Conventional physiotherapy group. Therefore, the physiotherapists who administered the interventions were instructed not to disclose the name of the group procedures to the participants. To ensure the internal validity of the findings, the blinding procedure was designed to achieve double-blinding of both study participants and the assessors. Besides, to guarantee a treatment allocation balance within the groups, stratified permuted blocks were used to randomly allocate different treatments within the groups at every intervention session of the study. The double-blinding is the gold standard for evidence-based medicine [56], [57].
Statistical analyses
Statistical analyses were performed in SPSS statistics version 24.0. The p-value was set at <0.05. Sociodemographic data, i.e. age, gender, current medication use, marital status, educational level, occupation/employment status, and place of residence (urban/rural), and anthropometric data, i.e. height and weight (to calculate the body mass index [BMI]) and supra iliac skinfold thickness, were divided into continue and categorical variables for ease of analysis as depicted in Table 1. Baseline differences regarding these data were examined using one-way ANOVA testing in case of a continuous variable and chi-square tests in the case of categorical variables.
Socio-demographic and anthropometric characteristics.
| Variables | All participants (n=125) M ± SD |
MET + DSE group (n=41) M ± SD |
DSE group (n=39) M ± SD |
Control group (n=45) M ± SD |
p-Value* | |
|---|---|---|---|---|---|---|
| Continuous | ||||||
| Age, years | 39.78 ± 8.97 | 38.76 ± 9.87 | 39.21 ± 8.62 | 41.22 ± 8.4 | 0.398 | |
| Height, m | 1.71 ± 0.21 | 1.67 ± 0.21 | 1.73 ± 0.20 | 1.74 ± 0.22 | 0.299 | |
| Weight, kg | 82.79 ± 15.32 | 80.49 ± 16.20 | 82.15 ± 15.56 | 85.44 ± 14.17 | 0.312 | |
| BMI, kg/m2 | 29.89 ± 9.56 | 31.15 ± 9.70 | 28.79 ± 9.33 | 29.70 ± 9.73 | 0.541 | |
| Skin fold thickness, mm | 23.93 ± 7.90 | 25.09 ± 7.97 | 23.30 ± 8.34 | 23.43 ± 7.50 | 0.517 | |
| Pain duration, months |
7.62 ± 4.93 |
7.83 ± 4.83 |
8.00 ± 5.07 |
7.11 ± 4.96 |
0.679 |
|
| Categorical | p-value** | |||||
| Gender | Female | 45 (36.0%) | 18 (43.9%) | 14 (35.9%) | 13 (28.9%) | 0.350 |
| Male | 80 (64.0%) | 23 (56.1%) | 25 (64.1%) | 32 (71.1%) | ||
| Medication | Nil | 67 (53.6%) | 24 (58.5%) | 22 (56.4%) | 21 (46.7%) | 0.498 |
| Yes | 58 (46.4%) | 17 (41.5%) | 17 (43.6%) | 24 (53.3%) | ||
| Marital status | Single | 33 (26.4%) | 15 (36.6%) | 11 (28.2%) | 7 (15.6%) | 0.080 |
| Married | 92 (73.6%) | 26 (63.4%) | 28 (71.8%) | 38 (84.4%) | ||
| Educational level | Primary | 11 (8.8%) | 6 (14.6%) | 1 (2.6%) | 4 (8.9%) | 0.580 |
| Secondary | 31 (24.8%) | 11 (26.8%) | 10 (25.6%) | 10 (22.2%) | ||
| Post-secondary | 52 (41.6%) | 16 (39.1%) | 18 (46.2%) | 18 (40.0%) | ||
| Masters | 25 (20.0%) | 7 (17.1) | 9 (23.1) | 9 (20.0%) | ||
| PhD | 6 (4.8%) | 1 (2.4%) | 1 (2.6%) | 4 (8.9%) | ||
| Employment status | Part-time | 14 (11.2%) | 7 (17.1%) | 4 (10.3%) | 3 (6.7%) | 0.303 |
| Full-time | 111 (88.8%) | 34 (82.9%) | 35 (89.7%) | 42 (93.3%) | ||
| Place of residence | Rural | 20 (16.0%) | 10 (24.4%) | 7 (17.9%) | 3 (6.7%) | 0.075 |
| Urban | 105 (84%) | 31 (75.6%) | 32 (82.1%) | 42 (93.3%) | ||
-
M, mean; SD, standard deviation; p-value*, p value of between groups from ANOVA test; p-value**, p-value from chi-square between groups test; n (%), number and percentage.
Repeated-measures ANOVA was used to compare mean scores for each outcome measure variables between assessment points in time and between groups. Multiple pairwise comparisons were conducted to identify the significant pairs between groups and when necessary two-way ANCOVA was used to remove the effect of baseline differences post-intervention. Post-hoc analyses were conducted using multiple pairwise comparisons after Bonferroni adjustment to reveal significant mean difference at a 95% confidence interval.
Results
A total of 137 chronic NSLBP patients underwent the baseline assessments (DSE + MET=47, DSE=45, conventional physiotherapy=45), of which 125 completed the full study protocol including the 24-weeks (follow-up) (DS + MET=41 [32.8%], DSE=39 [31.2%], Conventional physiotherapy=45 [36.0%]). This implies that there was a dropout rate of 8.76% (n=12). Analyses were performed on data of participants who completed the full study protocol. The sociodemographic characteristics of the included study sample are depicted in Table 1. In summary, the sample consisted of 80 (64.0%) males and 45 (36.0%) females, with a mean age 39.8 years (SD=8.97), a mean BMI of 29.9 (SD=9.56) (kg/m2) and a mean pain duration of 7.62 (SD=4.93) months. Patients were employed either in the public or private sector, with 111 (88.80%) of them being employed full-time and 14 (11.20%) being employed part-time. The patients were mainly farmers, nurses, traders, administrative professionals, artisans and teachers with 105 (84.0%) of them living in urban areas.
No significant mean difference was found between the groups on any of the outcomes (p-value>0.05) at baseline, except for lumbar flexion ROM (p=0.002) (Table 2). More specifically, the lumbar flexion ROM was significantly lower (p=0.002) in the DSE + MET compared to the DSE or conventional physiotherapy group. Therefore, based on the analysis of the baseline data patients from all groups were homogenous and comparable, except for lumbar flexion ROM, before commencing the interventions.
Participants’ baseline mean scores of study outcomes.
| Variables | All participants (n=125) M ± SD |
MET + DSE group (n=41) M ± SD | DSE group (n=39) M ± SD |
Control group (n=45) M ± SD |
F-value | p-Value |
|---|---|---|---|---|---|---|
| PNRS | 5.50 ± 1.20 | 5.59 ± 1.09 | 5.31 ± 1.2 | 5.60 ± 1.25 | 0.763 | 0.469 |
| LfxROM | 29.58 ± 9.65 | 25.61 ± 10.07 | 30.13 ± 8.92 | 32.71 ± 8.74 | 6.419 | 0.002 |
| LexROM | 15.36 ± 6.26 | 13.90 ± 5.42 | 15.13 ± 6.01 | 16.89 ± 6.89 | 2.542 | 0.083 |
| ODI | 30.41 ± 8.57 | 30.59 ± 8.94 | 31.00 ± 9.71 | 29.73 ± 7.21 | 0.239 | 0.788 |
| OMPSQ | 113.70 ± 13.80 | 115.12 ± 12.61 | 112.21 ± 17.08 | 113.69 ± 11.69 | 0.442 | 0.644 |
| GROCS | 1.90 ± 1.07 | 1.84 ± 1.26 | 1.94 ± 0.79 | 1.93 ± 1.11 | 0.106 | 0.899 |
-
M, mean; SD, standard deviation; PNRS, pain numeric rating scale; LfxROM, lumbar flexion range of motion; LexROM, lumbar extension range of motion; ODI, Oswestry Disability Scale; ÖMPSQ, Örebro Musculoskeletal Pain Screening Questionnaire; GROCS, Global Rating of Change Scale.
The results showed significant time × intervention interaction effects, suggesting the implemented therapeutic interventions exerted variable time-dependent effects on NPRS scores, lumbar ROM (flexion and extension) scores, ODI scores, OMPSQ scores and GROCS scores (Table 3).
Estimate of the effects of the study interventions on the biophysical outcomes.
| Variable | Intervention | 1 | 2 | 3 | 4 | Arm | Two-way ANOVA | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | SE | M | SE | M | SE | M | SE | |||||
| Pain intensity | ||||||||||||
| A | 5.60 | 0.19 | 4.80 | 0.14 | 2.76 | 0.12 | 2.95 | 0.12 | 1–2 p<0.001 1–3 p<0.001 1–4 p<0.001 2–3 p<0.001 2–4 p<0.001 3–4 p=0.100 |
Main effect “within group”: F(1.7, 213)=204; p<0.001; η2=0.626 Main effect “between group”: F(2, 122)=7.91; p<0.001; η2=0.12 Interaction effect (time × interventions): F(3.5, 213)=11.63; p<0.001; η2=0.626 |
||
| B | 5.31 | 0.19 | 4.64 | 0.14 | 3.80 | 0.12 | 3.97 | 0.13 | 1–2 p<0.001 1–3 p<0.001 1–4 p<0.001 2–3 p<0.001 2–4 p<0.001 3–4 p=0.139 |
|||
| C | 5.60 | 0.18 | 4.82 | 0.13 | 3.64 | 0.12 | 4.22 | 0.12 | 1–2 p<0.001 1–3 p<0.001 1–4 p<0.001 2–3 p<0.001 2–4 p<0.001 3–4 p<0.001 |
|||
| R | A–B p=0.302 A–C p=0.955 B–C p=0.267 |
A–B p=0.406 A–C p=0.927 B–C p=0.347 |
A–B p<0.001 A–C p<0.001 B–C p=0.373 |
A–B p<0.001 A–C p<0.001 B–C p=0.155 |
Post-hoc Bonferroni adjustment |
|||||||
| LfxROM | ||||||||||||
| A | 25.61 | 1.45 | 31.00 | 1.36 | 46.34 | 1.26 | 43.17 | 1.14 | 1–2 p<0.001 1–3 p<0.001 1–4 p<0.001 2–3 p<0.001 2–4 p<0.001 3–4 p<0.001 |
Main effect “within group”: F(2.2, 264)=199; p<0.001; η2=0.620 Main effect “between group”: F(2, 122)=1.51; p<0.001; η2=0.24 Interaction effect (time × interventions): F(4.3, 264)=199; p<0.001; η2= |
||
| B | 30.13 | 1.48 | 35.39 | 1.39 | 40.51 | 1.29 | 39.74 | 1.17 | 1–2 p<0.001 1–3 p<0.001 1–4 p<0.001 2–3 p<0.001 2–4 p<0.001 3–4 p=0.362 |
|||
| C | 32.71 | 1.38 | 35.60 | 1.30 | 45.00 | 1.20 | 41.67 | 1.09 | 1–2 p=0.005 1–3 p<0.001 1–4 p<0.001 2–3 p<0.001 2–4 p=0.001 3–4 p<0.001 |
|||
| R | A–B p=0.377 A–C p=0.270 B–C p=0.196 |
A–B p=0.545 A–C p=0.237 B–C p=0.582 |
A–B p<0.001 A–C p<0.001 B–C p=0.017 |
A–B p<0.001 A–C p<0.001 B–C p=0.301 |
Post-hoc Bonferroni adjustment |
|||||||
| LfxROM (after baseline adjustment) | ||||||||||||
| A | 33.67 | 0.98 | 47.99 | 1.14 | 44.51 | 1.06 | 2–3 p<0.001 2–4 p<0.001 3–4 p=0.240 |
Main effect “within group”: F(1.7, 205)=58; p<0.001; η2=0.324 Main effect “between group”: F(2, 121)=4.7; p<0.001; η2=0.390 Interaction effect (time × interventions): F(3.39, 205)=16.68; p<0.001; η2=0.141 |
||||
| B | 35.01 | 0.97 | 40.28 | 1.14 | 39.56 | 1.06 | 2–3 p<0.001 2–4 p<0.001 3–4 p=0.388 |
|||||
| C | 33.49 | 0.93 | 43.69 | 1.08 | 40.60 | 1.01 | 2–3 p<0.001 2–4 p<0.001 3–4 p<0.001 |
|||||
| R | A–B p=0.026 A–C p=0.016 B–C p=0.910 |
A–B p=0.002 A–C p=0.040 B–C p=0.012 |
A–B p=0.038 A–C p=0.024 B–C p=0.230 |
Post-hoc Bonferroni adjustment |
||||||||
| LexROM | ||||||||||||
| A | 13.90 | 0.97 | 18.05 | 0.92 | 29.63 | 0.74 | 28.17 | 0.75 | 1–2 p<0.001 1–3 p<0.001 1–4 p<0.001 2–3 p<0.001 2–4 p<0.001 3–4 p<0.305 |
Main effect “within group”: F(2, 247)=253; p<0.001; η2=0.675 Main effect “between group”: F(2, 122)=3.25; p<0.001; η2=0.510 Interaction effect (time × interventions): F(4, 247)=17.50; p<0.001; η2=0.223 |
||
| B | 15.13 | 0.99 | 18.85 | 0.94 | 22.95 | 0.75 | 22.69 | 0.77 | 1–2 p<0.001 1–3 p<0.001 1–4 p<0.001 2–3 p<0.001 2–4 p<0.001 3–4 p<0.604 |
|||
| C | 16.89 | 0.92 | 19.56 | 0.88 | 25.44 | 0.70 | 23.78 | 0.71 | 1–2 p=0.005 1–3 p<0.001 1–4 p<0.001 2–3 p<0.001 2–4 p=0.001 3–4 p<0.001 |
|||
| R | A–B p=0.377 A–C p=0.270 B–C p=0.196 |
A–B p=0.545 A–C p=0.237 B–C p=0.582 |
A–B p<0.001 A–C p<0.001 B–C p=0.017 |
A–B p<0.001 A–C p<0.001 B–C p=0.301 |
Post-hoc Bonferroni adjustment |
|||||||
-
1=Baseline assessment, 2=6th-week assessment, 3=12th-week assessment, 4=24th-week assessment, A=DSE plus MET intervention group, B=DSE alone intervention group, C=control group, Arm=intragroup difference between stages of the study, R=between-group difference, M, mean; SE, standard error; LexROM, Lumbar extension range of motion; LfxROM, Lumbar flexion range of motion.
Data on NPRS show the significant within-group difference (i.e. at baseline, 6, 12, and 24 weeks) (p<0.001), and between-group (i.e. conventional physiotherapy, DSE, and DSE + MET) (p<0.001). The post-hoc analysis following Bonferroni adjustment revealed that the DSE + MET intervention resulted in a significant (p<0.001) better outcome expressed as a larger NPRS reduction compared to the other interventions (DSE or conventional physiotherapy). The effects on NPRS in the DSE + MET group and the DSE group showed no significant differences when compared at 12 weeks (post-treatment) and 24 weeks (follow-up) (Table 3), indicating that the achieved treatment effects of these interventions were retained at 24 weeks follow-up which was not the case for the conventional physiotherapy group.
ROM for lumbar flexion scores showed significant within-group changes (i.e. baseline, 6-weeks, 12-weeks, and 24 weeks) (p<0.001), and between-groups differences (DSE + MET, DSE, and conventional physiotherapy) (p=0.001). The post-hoc analysis following Bonferroni adjustment revealed a better outcome for the DSE + MET intervention compared to the other interventions (DSE and conventional physiotherapy) (p<0.001) (Table 3). Because there was a between-group difference in lumbar flexion ROM at baseline, ANCOVA analysis was conducted to remove this baseline effect when analyzing and comparing between-group effects. The results show significant within-group changes (i.e. baseline, 6, 12, and 24 weeks) (p<0.001) and between-groups differences (DSE + MET, DSE, and conventional physiotherapy) (p<0.001). The post-hoc analysis revealed a significant interaction effect (time × group) (p<0.001) (Table 3). ROM for lumbar extension scores showed similar effects and the ROM for lumbar flexion scores, with significant difference within-group changes (i.e. at baseline, 6, 12, and 24 weeks) (p<0.001), and between-group differences (DSE + MET, DSE, and conventional physiotherapy) (p<0.001). The post-hoc analysis following Bonferroni adjustment revealed a significantly better outcome in lumbar extension ROM for the DSE + MET intervention compared to the DSE and conventional physiotherapy intervention p=0.001 Table 3. In conclusion, the results show that DSE + MET demonstrated better treatment effect than DSE or the conventional physiotherapy intervention on measures of lumbar ROM. The highest improvement in lumbar mobility was observed in the DSE + MET group with a mean value of 46.34°, or 47.99° after baseline adjustment, for lumbar flexion and 29.63° for extension (Table 3).
ODI scores showed significant within-group changes (i.e. at baseline, 6, 12, and 24 weeks) (p<0.001), with ODI scores decreasing in time in all groups irrelevant of the type of intervention which was received (Table 4). Hence, between-group comparisons did not reveal any significant differences (DSE + MET, DSE, and conventional physiotherapy) (partial eta squared = 0.009). The post-hoc analysis following Bonferroni adjustment revealed no significant interaction effects (time × group).
Estimate of the effects of the study interventions on the psychosocial and health status outcomes.
| Variable | Intervention | 1 | 2 | 3 | 4 | Two-way ANOVA | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| M | SE | M | SE | M | SE | M | SE | Arm | |||
| ODI | |||||||||||
| A | 30.59 | 1.34 | 26.88 | 1.09 | 19.76 | 0.47 | 19.39 | 0.38 | 1–2 p<0.001 1–3 p<0.001 1–4 p<0.001 2–3 p<0.001 2–4 p<0.001 3–4 p=0.910 |
Main effect “within group”: F(1.34, 164)=192; p<0.001; η2=0.612 Main effect “between group”: F(2, 122)=0.531; p<0.590;η2=0.009 Interaction effect (time × interventions): F(2.7, 164)=0.77; p<0.596; η2=0.612 |
|
| B | 31.00 | 1.38 | 27.39 | 1.12 | 20.74 | 0.48 | 21.21 | 0.39 | 1–2 p<0.001 1–3 p<0.001 1–4 p<0.001 2–3 p<0.001 2–4 p<0.001 3–4 p=0.038 |
||
| C | 29.73 | 1.29 | 25.96 | 1.04 | 20.60 | 0.45 | 20.27 | 0.36 | 1–2 p<0.001 1–3 p<0.001 1–4 p<0.001 2–3 p<0.001 2–4 p=0.001 3–4 p=0.107 |
||
| R | A–B p=0.830 A–C p=0.648 B–C p=0.503 |
A–B p=0.746 A–C p=0.541 B–C p=0.350 |
A–B p=0.142 A–C p=0.193 B–C p=0.826 |
A–B p<0.001 A–C p=0.097 B–C p=0.080 |
Post-hoc Bonferroni adjustment |
||||||
| OMPSQ | |||||||||||
| A | 115.12 | 2.17 | 111.32 | 1.81 | 82.17 | 1.56 | 83.42 | 1.40 | 1–2 p=0.001 1–3 p<0.001 1–4 p<0.001 2–3 p<0.001 2–4 p<0.001 3–4 p=0.800 |
Main effect “within group”: F(1.42, 173)=384; p<0.001; η2=0.759 Main effect “between group”: F(2, 122)=3.7; p<0.0.001; η2=0.058 Interaction effect (time × interventions): F(2.8, 173)=31.57; p<0.001; η2=0.759 |
|
| B | 112.21 | 2.22 | 106.59 | 1.86 | 97.72 | 1.59 | 97.69 | 1.44 | 1–2 p<0.001 1–3 p<0.001 1–4 p<0.001 2–3 p<0.001 2–4 p<0.001 3–4 p=957 |
||
| C | 113.69 | 2.07 | 107.29 | 1.73 | 94.91 | 1.48 | 94.18 | 1.34 | 1–2 p=0.005 1–3 p<0.001 1–4 p<0.001 2–3 p<0.001 2–4 p=0.001 3–4 p=0.100 |
||
| R | A–B p=0.349 A–C p=0.633 B–C p=0.626 |
A–B p=0.071 A–C p=0.110 B–C p=0.783 |
A–B p<0.001 A–C p<0.001 B–C p=0.200 |
A–B p<0.001 A–C p<0.001 B–C p=0.076 |
Post-hoc Bonferroni adjustment |
||||||
| GROCS | |||||||||||
| A | 1.84 | 0.18 | 2.49 | 0.14 | 5.19 | 0.13 | 5.27 | 0.12 | 1–2 p<0.001 1–3 p<0.001 1–4 p<0.001 2–3 p<0.001 2–4 p<0.001 3–4 p=0.328 |
Main effect “within group”: F(2.3, 135)=412; p<0.001; η2=0.786 Main effect “between group”: F(2, 112)=10.9; p<0.001; η2=0.162 Interaction effect (time × interventions): F(4.8, 262):27.63; p<0.001; η2=0.786 |
|
| B | 1.94 | 0.18 | 2.78 | 0.14 | 3.58 | 0.13 | 3.64 | 0.12 | 1–2 p<0.001 1–3 p<0.001 1–4 p<0.001 2–3 p<0.001 2–4 p<0.001 3–4 p=0.508 |
||
| C | 1.93 | 0.166 | 2.74 | 0.13 | 3.93 | 0.12 | 4.17 | 0.12 | 1–2 p=0.005 1–3 p<0.001 1–4 p<0.001 2–3 p<0.001 2–4 p=0.001 3–4 p=0.003 |
||
| R | A–B p=0.637 A–C p=0.709 B–C p=0.948 |
A–B p=0.153 A–C p=0.199 B–C p=0.840 |
A–B p<0.001 A–C p<0.001 B–C p=0.056 |
A–B p<0.001 A–C p<0.001 B–C p=0.001 |
Post-hoc Bonferroni adjustment |
||||||
-
1=Baseline assessment, 2=6th-week assessment, 3=12th-week assessment, 4=24th-week assessment, A=DSE plus MET intervention group, B=DSE alone intervention group, C=control group, Arm=Intragroup difference between stages of the study, R=between-group difference, M, mean; SE, standard error; ODI, Oswestry Disability Index; OMPSQ, Orebro Musculoskeletal Pain Screen Questionnaire; GROCS, Global Rating of Change Scale.
ÖMPSQ scores showed significant within-group changes (i.e. baseline, 6, 12, and 24 weeks) (p<0.001) decreasing over time. Furthermore, there was a significant difference in between-group change (DSE + MET, DSE & conventional physiotherapy) (p<0.001). The post-hoc analysis following Bonferroni adjustment revealed that DSE + MET had a significantly lower score than the DSE or conventional group (p<0.001) (Table 4). Furthermore, significant interaction effects between the groups (time × group) were revealed. Pairwise comparisons showed that ÖMPSQ scores at 12 weeks (post-treatment) and 24 weeks (follow-up) did not significantly differ, evidencing that the effects were retained at 24 weeks follow-up, which was observed in all groups. In contrast, DSE + MET intervention had the highest pronounced effect on the ÖMPSQ score p<0.001.
GROCS scores showed significant within-group changes (i.e. baseline, 6, 12, and 24 weeks) p<0.001 increase over time. Between-group comparisons show significant difference p<0.001 with DSE + MET demonstrating better outcome compared to DSE or conventional group. Significant interaction effects (time × group) showed that the DSE + MET group reported the greatest change of GROCS score over time compared to the other groups, with a change of 5.19 at 12th week and 5.27 at 24th week as against 1.84 baseline score, this indicates a score of quite a bit better on the questionnaire grading (p<0.001) (Table 4).
Discussion
Studies reporting on the effectiveness of MET as a standalone treatment intervention or MET in combination with other therapeutic exercises (particularly trunk stabilization exercises) for NSLBP are limited [32], [33]. A Cochrane review showed that MET in combination with other therapeutic modalities shows potential and can be regarded as safe for treating chronic NSLBP [32]. However, it was suggested that further research using a robust methodology is needed to enhance treatment effects for the management of chronic NSLBP and to examine whether these effects can be maintained on the long-term [32]. Also, a recent scoping review we performed indicated that most existing studies which have examined the effects of MET in chronic NSLBP lack methodological rigour which resulted in the inability to establish the effectiveness of MET in combination with other therapeutic modalities for the treatment of chronic NSLBP [33]. Therefore, based on the identified shortcomings and previously made recommendations the methodological quality of the present study was significantly improved compared to the previously reviewed studies [33]. Specific improvements included the use of appropriate sample size, a double-blind design, explanation of sampling and randomization procedures, increasing the number and the duration of the intervention sessions, and reassessment of the outcome measures at 24-week follow-up to examine whether treatment effects were retained in the long term.
Based on the available literature, this study is the first to use the ÖMPSQ in an RCT design examining the combined effect of manual therapy and stabilization exercises on limitation in daily activities and participation restrictions or on the risk to develop disabling chronic NSLBP. The advantage of this tool is that it provides important information that it contains constructs which provide insight on psychosocial factors explaining the patient’s experience of the condition which can be used to identify the risk of chronicity, which might be difficult to assess using other standard medical examination tools. The finding of this study reveals better post-intervention ÖMPSQ scores in DSE combined with MET compared to DSE as a standalone intervention or to conventional physiotherapy.
The overwhelming majority of studies on chronic NSLBP use heterogeneous samples to test the effectiveness of therapeutic interventions [58], this might be the reason why some interventions have not yielded satisfactory results as many of these studies could not establish whether a specific subgroup of patients may be more responsive to a particular intervention. Thus, the sample of this present study was homogeneous as only chronic NSLBP with hip/thoracic stiffness and lumbar hypomobility were included and patients with central sensitization and fear of movement were excluded.
The approach of a combination of stabilization exercises (DSE) and manual therapy (MET) proved more beneficial in relieving pain and improving lumbar mobility deficits and demonstrated the greatest satisfaction based on improved health status than DSE alone or conventional therapy. This finding is supported by studies which reported that multimodal treatments involving manual therapy and therapeutic exercises have the greatest impact on pain levels, lumbar mobility and general health status in patients with chronic NSLBP [10], [59], [60], [61], [62], [63]. Niemistö et al. [64] further noted that the increase in mobility could be due to the effect of MET, as it is used to correct any biomechanical dysfunctions in the lumbar or pelvic segments. Any muscular tension producing pain was treated by passively stretching the muscles and teaching auto stretching techniques, thus resulting in better changes on health status and treatment satisfaction. Additionally, Balthazard and Goumoens [63] demonstrated that MET, when combined with therapeutic exercises, provide immediate and long-term analgesic effects for patients with chronic NSLBP.
As far as we are aware, this is the first RCT aimed at examining the effectiveness of the combination of MET as a manual therapy technique with DSE as motor control exercises for the treatment of chronic NSLBP, which was based on the idea that the treatment objectives of each treatment strategy would complement each other and results in concomitant positive effects for biopsychosocial outcomes (pain, trunk range of motion, functional disability, health status, activity limitations and participation restrictions) of greater magnitude than the effects of a single model regime. This study shows that the therapeutic effects were obtained within the 12 weeks of the study and were retained at the 24 weeks follow-up period, this was more often retained for DSE + MET group.
In regards of functional disability, this study showed a reduction of the ODI score across all groups, and although DSE in combination with MET led to the greatest reductions in disability which were of clinical importance [42] no significant between-group differences could be established. This finding was corroborated by other studies which have reported that MET combined with therapeutic exercises is not superior to a standalone MET intervention or to conventional physiotherapy for improving chronic NSLBP related disability [25], [31], [35], [60], [61], [62], [64]. Additionally, Franca et al. [59] even reported that MET alone, in the form of selected lumbar muscle stretching, was less effective than segmental stabilization exercises in reducing functional disability in chronic NSLBP. In contrast, some studies reported manual therapy and therapeutic exercise interventions in chronic NSLBP to significantly reduce functional disability and the combination of both resulting in better outcomes than standalone interventions or conventional physiotherapy [62], [63], [66]. Hence, there was no consistent finding in the literature on the effectiveness of the combination of motor control exercises like DSE and manual therapy in the form of MET compared to standalone interventions or conventional physiotherapy for the management of patients with chronic NSLBP. The current study findings also could not establish the better therapeutic effect of the combination of MET with DSE as compared to DSE alone or conventional physiotherapy in improving functional disability. But there was a significant increase of clinical importance in the DSE + MET group and that the therapeutic effects were retained at least 24 weeks post-intervention in patients with chronic NSLBP.
In summary, based on the findings of this study, it was concluded that DSE combined with MET can be administered to patients with chronic NSLBP with lumbar hypomobility to reduce pain intensity, functional disability, limitations in activities and restrictions in participation, and to improve lumbar ROM and self-perceived health status in patients with chronic NSLBP. This procedure can, therefore, serve as a valid additional alternative therapeutic intervention to clinicians for the management of chronic NSLBP as it shows greater effects on pain intensity, trunk ROM, activity limitations/participation restrictions and changes in health status than DSE alone or conventional physiotherapy and the treatment effects were better retained on the long term. An additional benefit is that the use of medication which has many side effects and surgical intervention costs could potentially be reduced or avoided.
The researchers concede limitations to this study. First, the study location was urban and in Nigeria, there is a large difference in sociodemographic characteristics between urban and rural dwellers so the research findings need caution as they may not be representative for the general population of patients with chronic NSLBP. Second, moderate-intensity DSE was used in both treatment interventions because cardiorespiratory parameters were not of interest in this study and this intensity was sufficient to provide the desired effects on the outcome variables in patients with chronic NSLBP. Third, the results of this study should only be generalized to patients with chronic NSLBP tested and classified into a movement coordination impairment subgroup and displaying signs of hip/thoracic stiffness and lumbar hypomobility. To allow generalizability of the study findings, further research is recommended to provide evidence on the clinical importance of the combination of DSE and MET in chronic NSLBP patients with other clinical presentations.
Harms
The research did not potentially involve any serious risk or harms. The MET procedure was generally described as safe [32], [62]. However, patients in the DSE + MET and the other groups may experience mild discomfort due to the exercises. This may include temporary muscle soreness and dizziness and increases in heart rate, blood pressure, and sweating. However, every precaution was taken to prevent injuries.
Conclusion
Based on the findings of this study, it was concluded that DSE in combination with MET leads to greater therapeutic benefits than DSE alone or conventional physiotherapy on selected biopsychosocial outcomes, including pain intensity, lumbar ROM, functional disability, limitation in activities, restrictions in participation and self-perceived health status, in patients with chronic NSLBP. This conclusion was based on the methodological strengths of this study which include adequate sample size, elimination of selection bias (through randomization) and interpretation bias (through double blinding). Additionally, the therapeutic intervention is safe and can elicit beneficial effects which can serve as a valid additional alternative therapy to physiotherapists in the management of patients with chronic NSLBP.
Acknowledgements
Dr Abdulwali Sabo Abdulrahaman (PT) provided support for data cleaning and statistical analysis. We would like to thank all the physiotherapists and medical doctors who contributed to the success of the study and, most importantly, the patients for their voluntary participation.
-
Research funding: The study is funded by the College of Health Science of the University of KwaZulu-Natal post-graduate student bursary (internal funding). No external funding was received from any source for the study. Jessica Van Oosterwijck holds a post-doctoral research fellowship funded by the Research Foundation – Flanders (FWO) [12L5619N and 12L5616N].
-
Author contributions: UAA and SSM conceptualized and designed the study protocol, UAA collected and analyzed the data, SSM and JVO provided grammatical and critical review of the manuscript. Also, SSM obtained funding for the study. All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Competing interests: The authors declare that they have no competing interests.
-
Informed consent: A written and signed informed consent was obtained from all recruited participants for the study by a third party who is independent and not part of the core study team; the consent form was designed by the Biomedical Research Ethics Committee of University of KwaZulu-Natal (BREC) according to the WMA Helsinki declaration and good clinical practice (GCP).
-
Ethical approval: This study has been approved by the Biomedical Research Ethics Committee of the University of KwaZulu Natal (South Africa) (Ethics Number: BFC198/18) and by the Human Research Ethics Committee of the study hospital facilities i.e. Rasheed Shekoni Specialist Hospital (RSSH) (RSSH/GEN/226/V.II/7) and the Federal Medical Centre, Birnin-Kudu (FMC BKD) both Jigawa state Northwestern Nigeria where the study was conducted. The RSSH and FMC are 300 and 200-bed capacity tertiary health facilities respectively, serving patients from within and around the state.
-
Availability of data and materials: The datasets used and/or analyzed during the current study are available from the corresponding author (Usman AA) on reasonable request. However, the findings from the study would be made available to participating researchers as required by law. Also, the full trial protocol is available with the trial registry i.e. ClinicalTrial.gov (NCT3449810).
References
1. Hoy, D, March, L, Brooks, P, Blyth, F, Woolf, A, Bain, C, et al.. The global burden of low back pain: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis 2014;73:968–74. https://doi.org/10.1136/annrheumdis-2013-204428.Suche in Google Scholar PubMed
2. Wu, A, March, L, Zheng, X, Huang, J, Wang, X, Zhao, J, et al.. Global low back pain prevalence and years lived with disability from 1990 to 2017: estimates from the Global Burden of Disease Study 2017. Ann Transl Med 2020;8:299. https://doi.org/10.21037/atm.2020.02.175.Suche in Google Scholar PubMed PubMed Central
3. Woolf, AD, Erwin, J, March, L. The need to address the burden of musculoskeletal conditions. Best Pract Res Clin Rheumatol 2012;26:183–224. https://doi.org/10.1016/j.berh.2012.03.005.Suche in Google Scholar PubMed
4. Hoy, DG, Smith, E, Cross, M, Sanchez-Riera, L, Blyth, FM, Buchbinder, R, et al.. Reflecting on the global burden of musculoskeletal conditions: lessons learnt from the global burden of disease 2010 study and the next steps forward. Ann Rheum Dis 2015;74:4–7. https://doi.org/10.1136/annrheumdis-2014-205393.Suche in Google Scholar PubMed
5. Hartvigsen, J, Hancock, MJ, Kongsted, A, Louw, Q, Ferreira, ML, Genevay, S, et al.. What low back pain is and why we need to pay attention. Lancet 2018;391:2356–67. https://doi.org/10.1016/s0140-6736(18)30480-x.Suche in Google Scholar
6. Majid, K, Truumees, E. Epidemiology and natural history of low back pain. Semin Spine Surg 2008;20:87–92. https://doi.org/10.1053/j.semss.2008.02.003.Suche in Google Scholar
7. Woolf, AD, Brooks, P, Åkesson, K, Mody, GM. Prevention of musculoskeletal conditions in the developing world. Best Pract Res Clin Rheumatol 2008;22:759–72. https://doi.org/10.1016/j.berh.2008.07.003.Suche in Google Scholar PubMed
8. Morris, LD, Daniels, KJ, Ganguli, B, Louw, QA. An update on the prevalence of low back pain in Africa: a systematic review and meta-analyses. BMC Musculoskelet Disord 2018;19:1–15. https://doi.org/10.1186/s12891-018-2075-x.Suche in Google Scholar PubMed PubMed Central
9. Von Korff, M. Studying the natural history of back pain. Spine (Phila Pa 1976) 1994;19:2041S–6S. https://doi.org/10.1097/00007632-199409151-00005.Suche in Google Scholar PubMed
10. Foster, NE, Anema, JR, Cherkin, D, Chou, R, Cohen, SP, Gross, DP, et al.. Prevention and treatment of low back pain: evidence, challenges, and promising directions. Lancet 2018;391:2368–83. https://doi.org/10.1016/s0140-6736(18)30489-6.Suche in Google Scholar PubMed
11. Airaksinen, O, Brox, JI, Cedraschi, C, Hildebrandt, J, Klaber-Moffett, J, Kovacs, F, et al.. Chapter 4 European guidelines for the management of chronic nonspecific low back pain on behalf of the COST B13 working group on guidelines for chronic low back pain contributors. Eur Spine J 2006:192–300.10.1007/s00586-006-1072-1Suche in Google Scholar PubMed PubMed Central
12. Campbell, P, Bishop, A, Dunn, KM, Main, CJ, Thomas, E, Foster, NE. Conceptual overlap of psychological constructs in low back pain. Pain 2013;154:1783–91. https://doi.org/10.1016/j.pain.2013.05.035.Suche in Google Scholar PubMed PubMed Central
13. Jones, M, Edwards, I, Gifford, L. Conceptual models for implementing biopsychosocial theory in clinical practice. Man Ther 2002;7:2–9. https://doi.org/10.1054/math.2001.0426.Suche in Google Scholar PubMed
14. D’Hooge, R, Cagnie, B, Crombez, G, Vanderstraeten, G, Achten, E, Danneels, L. Lumbar muscle dysfunction during remission of unilateral recurrent nonspecific low-back pain: evaluation with muscle functional MRI. Clin J Pain 2013;29:187–94. https://doi.org/10.1097/AJP.0b013e31824ed170.Suche in Google Scholar PubMed
15. Goubert, D, Van Oosterwijck, J, Meeus, M, Danneels, L. Structural changes of lumbar muscles in non-specific low back pain. Pain Phys 2016;19:E985–99.10.36076/ppj/2016.19.E985Suche in Google Scholar
16. O’Sullivan, PB, Mitchell, T, Bulich, P, Waller, R, Holte, J. The relationship between posture and back muscle endurance in industrial workers with flexion-related low back pain. Man Ther 2006;11:264–71. https://doi.org/10.1016/j.math.2005.04.004.Suche in Google Scholar PubMed
17. Danneels, L, Coorevits, P, Cools, A, Vanderstraeten, G, Cambier, D, Witvrouw, E, et al.. Differences in electromyographic activity in the multifidus muscle and the iliocostalis lumborum between healthy subjects and patients with sub-acute and chronic low back pain. Eur Spine J 2002;11:13–9. https://doi.org/10.1007/s005860100314.Suche in Google Scholar PubMed PubMed Central
18. Linton, SJ. A review of psychological risk factors in back and neck pain. Spine (Phila Pa 1976) 2000;25:1148–56. https://doi.org/10.1097/00007632-200005010-00017.Suche in Google Scholar PubMed
19. Linton, SJ, Andersson, T. Can chronic disability be prevented? Spine (Phila Pa 1976) 2000;25:2825–31. https://doi.org/10.1097/00007632-200011010-00017.Suche in Google Scholar PubMed
20. Pincus, T, Burton, AK, Vogel, S, Field, AP. A systematic review of psychological factors as predictors of chronicity/disability in prospective cohorts of low back pain. Spine (Phila Pa 1976) 2002;27:109–20. https://doi.org/10.1097/00007632-200203010-00017.Suche in Google Scholar PubMed
21. Adnan, R, Van Oosterwijck, J, Cagnie, B, Dhondt, E, Schouppe, S, Van Akeleyen, J, et al.. Determining predictive outcome factors for a multimodal treatment program in low back pain patients: a retrospective cohort study. J Manip Physiol Ther 2017;40:659–67. https://doi.org/10.1016/j.jmpt.2017.09.001.Suche in Google Scholar PubMed
22. Dhondt, E, Van Oosterwijck, J, Cagnie, B, Adnan, R, Schouppe, S, Van Akeleyen, J, et al.. Predicting treatment adherence and outcome to outpatient multimodal rehabilitation in chronic low back pain. J Back Musculoskelet Rehabil 2020;33:277–93. https://doi.org/10.3233/bmr-181125.Suche in Google Scholar PubMed
23. Yannick, T-L, Marc, OM, Joshi, AB, Chad, EC. Rehabilitation management of low back pain – it’s time to pull it all together!. J Pain Res 2017;10:2373–85.10.2147/JPR.S146485Suche in Google Scholar PubMed PubMed Central
24. Geisser, ME, Haig, AJ, Wallbom, AS, Wiggert, EA. Pain-related fear, lumbar flexion, and dynamic EMG among persons with chronic musculoskeletal low back pain. Clin J Pain 2004;20:61–9. https://doi.org/10.1097/00002508-200403000-00001.Suche in Google Scholar PubMed
25. Geisser, ME, Wiggert, EA, Haig, AJ, Colwell, MO. A randomized, controlled trial of manual therapy and specific adjuvant exercise for chronic low back pain. Clin J Pain 2005;21:463–70. https://doi.org/10.1097/01.ajp.0000135237.89834.23.Suche in Google Scholar PubMed PubMed Central
26. Moon, HJ, Choi, KH, Kim, DH, Kim, HJ, Cho, YK, Lee, KH, et al.. Effect of lumbar stabilization and dynamic lumbar strengthening exercises in patients with chronic low back pain. Ann Rehabil Med 2013;37:110–7. https://doi.org/10.5535/arm.2013.37.1.110.Suche in Google Scholar PubMed PubMed Central
27. Tsao, H, Druitt, TR, Schollum, TM, Hodges, PW. Motor training of the lumbar paraspinal muscles induces immediate changes in motor coordination in patients with recurrent low back pain. J Pain 2010;11:1120–8. https://doi.org/10.1016/j.jpain.2010.02.004.Suche in Google Scholar PubMed
28. Standaert, CJ, Weinstein, SM, Rumpeltes, J. Evidence-informed management of chronic low back pain with lumbar stabilization exercises. Spine J 2008;8:114–20. https://doi.org/10.1016/j.spinee.2007.10.015.Suche in Google Scholar PubMed
29. Moore, SD, Laudner, KG, Mcloda, TA, Shaffer, MA. The immediate effects of muscle energy technique on posterior shoulder tightness: a randomized controlled trial. J Orthop Sports Phys Ther 2011;41:400–7. https://doi.org/10.2519/jospt.2011.3292.Suche in Google Scholar PubMed
30. Gugliotti, M. The use of mobilization, muscle energy technique, and soft tissue mobilization following a modified radical neck dissection of a patient with head and neck cancer. Rehabil Oncol 2011;29:3–8. https://doi.org/10.1097/01893697-201129010-00001.Suche in Google Scholar
31. Szulc, P, Wendt, M, Waszak, M, Tomczak, M, Cieślik, K, Trzaska, T. Impact of McKenzie method therapy enriched by muscular energy techniques on subjective and objective parameters related to spine function in patients with chronic low back pain. Med Sci Monit 2015;21:2918–32. https://doi.org/10.12659/msm.894261.Suche in Google Scholar
32. Franke, H, Fryer, G, Ostelo, RW, Kamper, SJ. Muscle energy technique for non‐specific low‐back pain. Cochrane Database Syst Rev 2015:41–52. https://doi.org/10.1016/j.ijosm.2016.01.002.Suche in Google Scholar
33. Ahmed, U, Nadasan, T, Van Oosterwijck, J, Maharaj, SS. The effect of muscles energy technique in the management of chronic mechanical low back Pain : a scoping review. J Back Musculoskelet Rehabil 2020:20–57.Suche in Google Scholar
34. Wilson, E, Payton, O, Donegan-Shoaf, L, Dec, K. Muscle energy technique in patients with acute low back pain: a pilot clinical trial. J Orthop Sports Phys Ther 2003;33:502–12. https://doi.org/10.2519/jospt.2003.33.9.502.Suche in Google Scholar PubMed
35. Ellythy, MA. Efficacy of muscle energy technique versus myofascial release on function outcome measures in patients with chronic low back pain. Bull Fac Phys Ther 2012;17:29–35.Suche in Google Scholar
36. Delitto, A, George, SZ, Van Dillen, LR, Whitman, JM, Sowa, G, Shekelle, P, et al.. Low back pain. Clinical practice guidelines linked to the International classification of functioning, disability, and health from the orthopaedic section of the American physical therapy association. J Orthop Sports Phys Ther 2012;42:A1–57. https://doi.org/10.2519/jospt.2012.42.4.a1.Suche in Google Scholar
37. Mayer, TG, Neblett, R, Cohen, H, Howard, KJ, Choi, YH, Williams, MJ, et al.. The development and psychometric validation of the central sensitization inventory. Pain Pract 2012;12:276–85. https://doi.org/10.1111/j.1533-2500.2011.00493.x.Suche in Google Scholar PubMed PubMed Central
38. Vlaeyen, JWS, Kole-Snijders, AMJ, Boeren, RGB, van Eek, H. Fear of movement/(re)injury in chronic low back pain and its relation to behavioural performance. Pain 1995;62:363–72. https://doi.org/10.1016/0304-3959(94)00279-n.Suche in Google Scholar
39. Cohen, J. Statistical power analysis for the behavioral sciences, 2nd ed. [Internet], Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. Available from: https://books.google.com.ng/books/about/Statistical_Power_Analysis_for_the_Behav.html?id=cIJH0lR33bgC&printsec=frontcover&source=kp_read_button&redir_esc=y#v=onepage&q&f=false.Suche in Google Scholar
40. Childs, JD, Piva, SR, Fritz, JM. Responsiveness of the numeric pain rating scale in patients with low back pain. Spine (Phila Pa 1976) 2005;30:1331–4. https://doi.org/10.1097/01.brs.0000164099.92112.29.Suche in Google Scholar PubMed
41. Bernhard, MPM, Saur PM, M. Lumbar range of Motion : reliability and validity of the inclinometer technique in the clinical measurement of trunk flexibility [diagnostic Imaging and testing]. Spine (Phila Pa 1976) 1996;21:1332–8. http://doi.org/10.1.1.621.2434&rep=rep1&type=pdf.10.1097/00007632-199606010-00011Suche in Google Scholar PubMed
42. Yoshida, G, Hasegawa, T, Yamato, Y, Kobayashi, S, Shin, O, Banno, T, et al.. Minimum clinically important differences in Oswestry Disability Index domains and their impact on adult spinal deformity surgery. Asian Spine J 2019;13:35–44. https://doi.org/10.31616/asj.2018.0077.Suche in Google Scholar PubMed PubMed Central
43. Frost, H, Lamb, SE, Stewart-Brown, S. Responsiveness of a patient-specific outcome measure compared with the Oswestry disability index v2.1 and Roland and Morris disability questionnaire for patients with subacute and chronic low back pain. Spine (Phila Pa 1976) 2008;33:2450–7. https://doi.org/10.1097/brs.0b013e31818916fd.Suche in Google Scholar
44. Adamu, AS, Ibrahim, AA, Ahmad, RY, Akindele, MO, Kaka, B, Mukhtar, NB. Cross-cultural adaptation and validation of the Hausa version of the Oswestry disability index 2.1a for patients with low back pain. Spine (Phila Pa 1976) 2019;44:E1092–102. https://doi.org/10.1097/brs.0000000000003068.Suche in Google Scholar
45. Linton, SJ, Halldén, K. Can we screen for problematic back pain? A screening questionnaire for predicting outcome in acute and subacute back pain. Clin J Pain 1998;14:209–15. https://doi.org/10.1097/00002508-199809000-00007.Suche in Google Scholar PubMed
46. Boersma, K, Linton, SJ. Screening to identify patients at risk: profiles of psychological risk factors for early intervention. Clin J Pain 2005;21:38–43. https://doi.org/10.1097/00002508-200501000-00005.Suche in Google Scholar PubMed
47. Linton, SJ, Boersma, K. Early identification of patients at risk of developing a persistent back problem: the predictive validity of the Örebro musculoskeletal pain questionnaire. Clin J Pain 2003;19:80–6. https://doi.org/10.1097/00002508-200303000-00002.Suche in Google Scholar PubMed
48. Hill, JC, Dunn, KM, Main, CJ, Hay, EM. Subgrouping low back pain: a comparison of the STarT back tool with the Örebro musculoskeletal pain screening questionnaire. Eur J Pain 2010;14:83–9. https://doi.org/10.1016/j.ejpain.2009.01.003.Suche in Google Scholar PubMed PubMed Central
49. Gabel, CP, Melloh, M, Burkett, B, Osborne, J, Yelland, M. The Örebro Musculoskeletal Screening Questionnaire: validation of a modified primary care musculoskeletal screening tool in an acute work injured population. Man Ther 2012;17:554–65. https://doi.org/10.1016/j.math.2012.05.014.Suche in Google Scholar PubMed
50. Ahmed, UA, Maharaj, SS, Nadasan, T, Kaka, B. Cross-cultural adaptation and psychometric validation of the Hausa version of the Örebro Musculoskeletal Pain Screening Questionnaire in patients with non-specific low back pain. Scand J Pain 2021;21:103–11.10.1515/sjpain-2020-0071Suche in Google Scholar PubMed
51. Jaeschke, R, Singer, J, Guyatt, GH. Measurement of health status: ascertaining the minimal clinically important difference. Control Clin Trials 1989;10:407–15. https://doi.org/10.1016/0197-2456(89)90005-6.Suche in Google Scholar PubMed
52. Kamper, SJ, Maher, CG, Mackay, G. Global rating of change scales: a review of strengths and weaknesses and considerations for design. Aust J Physiother 2009;55:289. https://doi.org/10.1179/jmt.2009.17.3.163.Suche in Google Scholar PubMed PubMed Central
53. Ahmed, UA, Maharaj, SS, Thaya, N, Kaka, B, Akodu, AK. Knowledge of physiotherapists on the use of muscle energy technique in the management of non-specific low back pain. BMC Health Serv Res 2020:20–63.10.21203/rs.2.17864/v1Suche in Google Scholar
54. Odebiyi, D, Aweto, H, Igbari, T, Tella, B. Factors Influencing number of physiotherapy treatment sessions for patients with low back pain. African J Physiother Rehabil Sci 2012;4:23–8. https://doi.org/10.4314/ajprs.v4i1-2.4.Suche in Google Scholar
55. Ayanniyi, O, Lasisi, O, Adegoke, BO, Oni-Orisan, M. Management of low back pain: attitudes and treatment preferences of physiotherapists in Nigeria. Afr J Biomed Res 2009;10:41–9. https://doi.org/10.4314/ajbr.v10i1.48970.Suche in Google Scholar
56. Opara, J, Kucio, C, Małecki, A, Pilch, J. Methods of blinding clinical trials in physiotherapy. Physiotherapy 2013;21:62–4. https://doi.org/10.2478/physio-2013-0006.Suche in Google Scholar
57. Bang, H, Flaherty, SP, Kolahi, J, Park, J. Blinding assessment in clinical trials: a review of statistical methods and a proposal of blinding assessment protocol. Clin Res Regul Aff 2010;27:42–51. https://doi.org/10.3109/10601331003777444.Suche in Google Scholar
58. Lawrence, JP, Greene, HS, Grauer, JN. Back pain in athletes. J Am Acad Orthop Surg 2006;14:726–35. https://doi.org/10.5435/00124635-200612000-00004.Suche in Google Scholar PubMed
59. França, FR, Burke, TN, Caffaro, RR, Ramos, LA, Marques, AP. Effects of muscular stretching and segmental stabilization on functional disability and pain in patients with chronic low back pain: a randomized, controlled trial. J Manip Physiol Ther 2012;35:279–85. https://doi.org/10.1016/j.jmpt.2012.04.012.Suche in Google Scholar PubMed
60. Zafereo, J, Wang-price, S, Roddey, T, Brizzolara, K, Zafereo, J, Wang-price, S, et al.. Regional manual therapy and motor control exercise for chronic low back pain: a randomized clinical trial. J Man Manip Ther 2018;9817:1–13. https://doi.org/10.1080/10669817.2018.1433283.Suche in Google Scholar
61. Bindra, S. A study on the efficacy of muscle energy technique as compared to conventional therapy on lumbar spine range of motion in chronic low back pain of sacroiliac origin. Hum Biol Rev 2013;2:336–48.Suche in Google Scholar
62. Lamberth, L, Hansen, KL, Bloch-Thomsen, M, Silbye, P, Remvig, L. Muscle energy technique: a useful aid to the manual treatment of low back pain? J Orthop Med 2005;27:17–21. https://doi.org/10.1080/1355297X.2005.11736248.Suche in Google Scholar
63. Balthazard, P, de, GP, Rivier, G, Demeulenaere, P, Ballabeni, P, Deriaz, O. Manual therapy followed by specific active exercises versus a placebo followed by specific active exercises on the improvement of functional disability in patients with chronic non-specific low back pain: a randomized controlled trial. BMC Muscoskel Disord 2012;13:162. https://doi.org/10.1186/1471-2474-13-162.Suche in Google Scholar PubMed PubMed Central
64. Niemistö, L, Lahtinen-Suopanki, T, Rissanen, P, Lindgren, KA, Sarna, S, Hurri, H. A randomized trial of combined manipulation, stabilizing exercises, and physician consultation compared to physician consultation alone for chronic low back pain. Spine (Phila Pa 1976) 2003;28:2185–91. https://doi.org/10.1097/01.brs.0000085096.62603.61.Suche in Google Scholar PubMed
65. Ellythy, MA. Efficacy of muscle energy technique versus strain counter strain on low back dysfunction. Bull Fac Phys Ther 2012;17:29–35.Suche in Google Scholar
66. Dhinkaran, M, Sareen, A, Arora, T. Comparative analysis of Muscle Energy Technique and conventional physiotherapy in the treatment of sacroiliac joint dysfunction. Indian J Physiother Occup Ther An Int J 2011;5:127–30.Suche in Google Scholar
© 2021 Walter de Gruyter GmbH, Berlin/Boston
Artikel in diesem Heft
- Frontmatter
- Editorial Comment
- Some controversies related to questionable clinical uses of methadone for chronic non-cancer pain and in palliative care
- Systematic Reviews
- Heart rate variability in patients with low back pain: a systematic review
- Prevalence of musculoskeletal chest pain in the emergency department: a systematic review and meta-analysis
- Clinical Pain Research
- When driving hurts: characterizing the experience and impact of driving with back pain
- Sensitization in office workers with chronic neck pain in different pain conditions and intensities
- Do chronic low back pain subgroups derived from dynamic quantitative sensory testing exhibit differing multidimensional profiles?
- Do people with acute low back pain have an attentional bias to threat-related words?
- Effects of dynamic stabilization exercises and muscle energy technique on selected biopsychosocial outcomes for patients with chronic non-specific low back pain: a double-blind randomized controlled trial
- Health-related quality of life and pain interference in two patient cohorts with neuropathic pain: breast cancer survivors and HIV patients
- Breast reconstruction after breast cancer surgery – persistent pain and quality of life 1–8 years after breast reconstruction
- Autonomic dysregulation and impairments in the recognition of facial emotional expressions in patients with chronic musculoskeletal pain
- Sleep disturbance in patients attending specialized chronic pain clinics in Denmark: a longitudinal study examining the relationship between sleep and pain outcomes
- The challenge of recognizing severe pain and autonomic abnormalities for early diagnosis of CRPS
- Military veterans with and without post-traumatic stress disorder: results from a chronic pain management programme
- Observational Studies
- Long-term postoperative opioid prescription after cholecystectomy or gastric by-pass surgery: a retrospective observational study
- Criterion validity and discriminatory ability of the central sensitization inventory short form in individuals with inflammatory bowel diseases
- Neural activity during cognitive reappraisal in chronic low back pain: a preliminary study
- Social deprivation and paediatric chronic pain referrals in Ireland: a cross-sectional study
- Original Experimental
- The inhibitory effect of conditioned pain modulation on temporal summation in low-back pain patients
- “Big girls don’t cry”: the effect of the experimenter’s sex and pain catastrophising on pain
- Short Communication
- Persistent pain relief following a single injection of a local anesthetic for neuropathic abdominal wall and groin pain
Artikel in diesem Heft
- Frontmatter
- Editorial Comment
- Some controversies related to questionable clinical uses of methadone for chronic non-cancer pain and in palliative care
- Systematic Reviews
- Heart rate variability in patients with low back pain: a systematic review
- Prevalence of musculoskeletal chest pain in the emergency department: a systematic review and meta-analysis
- Clinical Pain Research
- When driving hurts: characterizing the experience and impact of driving with back pain
- Sensitization in office workers with chronic neck pain in different pain conditions and intensities
- Do chronic low back pain subgroups derived from dynamic quantitative sensory testing exhibit differing multidimensional profiles?
- Do people with acute low back pain have an attentional bias to threat-related words?
- Effects of dynamic stabilization exercises and muscle energy technique on selected biopsychosocial outcomes for patients with chronic non-specific low back pain: a double-blind randomized controlled trial
- Health-related quality of life and pain interference in two patient cohorts with neuropathic pain: breast cancer survivors and HIV patients
- Breast reconstruction after breast cancer surgery – persistent pain and quality of life 1–8 years after breast reconstruction
- Autonomic dysregulation and impairments in the recognition of facial emotional expressions in patients with chronic musculoskeletal pain
- Sleep disturbance in patients attending specialized chronic pain clinics in Denmark: a longitudinal study examining the relationship between sleep and pain outcomes
- The challenge of recognizing severe pain and autonomic abnormalities for early diagnosis of CRPS
- Military veterans with and without post-traumatic stress disorder: results from a chronic pain management programme
- Observational Studies
- Long-term postoperative opioid prescription after cholecystectomy or gastric by-pass surgery: a retrospective observational study
- Criterion validity and discriminatory ability of the central sensitization inventory short form in individuals with inflammatory bowel diseases
- Neural activity during cognitive reappraisal in chronic low back pain: a preliminary study
- Social deprivation and paediatric chronic pain referrals in Ireland: a cross-sectional study
- Original Experimental
- The inhibitory effect of conditioned pain modulation on temporal summation in low-back pain patients
- “Big girls don’t cry”: the effect of the experimenter’s sex and pain catastrophising on pain
- Short Communication
- Persistent pain relief following a single injection of a local anesthetic for neuropathic abdominal wall and groin pain

