Abstract
Objectives
The effect of stretching on joint range of motion is well documented, and although sensory perception has significance for changes in the tolerance to stretch following stretching the underlining mechanisms responsible for these changes is insufficiently understood. The aim of this study was to examine the influence of endogenous pain inhibitory mechanisms on stretch tolerance and to investigate the relationship between range of motion and changes in pain sensitivity.
Methods
Nineteen healthy males participated in this randomized, repeated-measures crossover study, conducted on 2 separate days. Knee extension range of motion, passive resistive torque, and pressure pain thresholds were recorded before, after, and 10 min after each of four experimental conditions; (i) Exercise-induced hypoalgesia, (ii) two bouts of static stretching, (iii) resting, and (iv) a remote, painful stimulus induced by the cold pressor test.
Results
Exercise-induced hypoalgesia and cold pressor test caused an increase in range of motion (p<0.034) and pressure pain thresholds (p<0.027). Moderate correlations in pressure pain thresholds were found between exercise-induced hypoalgesia and static stretch (Rho>0.507, p=0.01) and exercise-induced hypoalgesia and the cold pressor test (Rho=0.562, p=0.01). A weak correlation in pressure pain thresholds and changes in range of motion were found following the cold pressor test (Rho=0.460, p=0.047). However, a potential carryover hypoalgesic effect may have affected the results of the static stretch.
Conclusions
These results suggest that stretch tolerance may be linked with endogenous modulation of pain. Present results suggest, that stretch tolerance may merely be a marker for pain sensitivity which may have clinical significance given that stretching is often prescribed in the rehabilitation of different musculoskeletal pain conditions where reduced endogenous pain inhibition is frequently seen.
Introduction
Stretching is known to increase joint range of motion and is extensively used in relation to both rehabilitation and exercise to improve function or prevent injury [1], [, 2]. Moreover, increasing soft tissue temperature using active warm-up or local heat application is often used as an adjunct to therapeutic or developmental stretching employed to treat restrictions in range of movement [3]. Stretching has been considered primarily a mechanical phenomenon and previous hypotheses have attributed increases in range of motion following stretching to mechanical changes in the muscle-tendon unit, such as increased muscle length, or a reduction in muscle activity [4], [, 5]. However, these theories have been negated [4], [, 6] hence the underlying mechanisms responsible for the acute changes in joint range of motion following stretching are still largely undisclosed [4].
Current evidence suggests that changes in joint range of motion following stretching are caused by modifications in the person’s sensations (i.e. stretch, tightness, pain, etc.) resulting in changes in the tolerance to stretch [4], [, 5], thus indicating an important sensory component. Moreover, increases in range of motion following stretching have lately been positively associated with reduced pain sensitivity [7]. Stretch tolerance is commonly characterized by the changes in range of motion and peak passive moment recorded at end range [8] and is defined as the ability to tolerate stretch-related discomfort [9] suggesting that an increase in stretch tolerance may explain improved joint range of motion following stretching [10]. An increase in stretch tolerance following stretching may depend on an analgesic effect, allowing for higher tolerance to passive tension [11], [, 12], possibly due to changes in the sensitivity of peripheral nociceptors in the joint or muscle-tendon unit (e.g. type Ia and Ib afferents) via gate control [9], [, 10] or neurotransmitter modulation [13].
Recent findings from our group suggest that there may be a link between the tolerance to stretch and endogenous inhibitory pain mechanisms indicating that central pain mechanisms can to some extent modulate joint range of motion following stretching [12]. However, it is still unknown to what extent pain affects the tolerance to stretch. Taken together, this may indicate that the tolerance to stretch is linked with endogenous modulation of somatosensory input.
The conductance of nociceptive afferent signals can be modulated via descending inhibition [14], [, 15] which, in a healthy system, commonly reduces pain sensitivity and thereby increases the tolerance to nociceptive stimuli [16], [, 17]. However, endogenous modulation of pain is often impaired in populations with chronic pain, resulting in reduced inhibitory capacity. Endogenous modulation of pain sensitivity can be induced with e.g. exercise, resulting in exercise-induced hypoalgesia (EIH) and by applying a conditioning nociceptive stimulus distant to the area being investigated, (conditioned pain modulation, CPM) [18]. This causes an acute heterotopic decrease in pain sensitivity, although homotopic hypoalgesia has also been reported [19]. Both methods are known to increase pain tolerance in healthy adults although activating a CPM response seems to induce a greater inhibitory response compared with exercise [20].
Stretching is broadly recommended for patients with chronic pain [9] and can be a feasible option as part of rehabilitation, considering its non-invasiveness, low cost and potential for self-management. Investigating the interactions between the sensitivity of pain mechanisms, the tolerance to stretch and range of motion is warranted, considering the importance such an understanding may have for rehabilitation strategies. The purpose of this study was, therefore, 1) to investigate the potential influence of endogenous pain inhibitory mechanisms on stretch tolerance and 2) to investigate the relationship between range of motion and changes in pain sensitivity. The hypotheses were that i) the tolerance to stretch increases when endogenous pain inhibitory mechanisms are engaged, ii) the effect is greater when a CPM response is induced as compared to EIH and iii) changes in pain-free range of motion are associated with changes in pain sensitivity.
Materials and methods
Nineteen healthy male participants were recruited for this randomized, repeated-measures cross-over study. The participants had a mean ± standard deviation (range) age, 25.5 ± 3.5 [22], [23], [24], [25], [26], [27], [28], [29], [30], [31], [32], [33], [34] years, height 1.82 ± 0.08 (1.7–1.97) m, weight 85.5 ± 14.5 (73–130) kg, BMI 25.9 ± 4 (22.5–42) kg m−2. 16 out of 19 participants were right hand dominant. Only males were included to avoid the potential effect that fluctuations in gonadal hormone values across the menstrual cycle have on the endogenous inhibitory mechanisms [21]. In accordance with IKDC criteria, the sample size was determined to detect a difference in knee extension range of motion of at least 2°, as this must be distinguished to properly categorize knee function [13], (α=0:05, power=80%) between measures [12]. Based on these data, an n value of 16 participants was estimated to be necessary. However, 19 were included to account for possible technical errors or dropouts during the study. Eligibility for participation included the absence of any pain or other conditions which might affect the somatosensory system and pain perception. All participants were asked to refrain from physical exercise and caffeinated beverages on the day of participation. The participants entered the study after providing their written informed consent. The study was conducted in accordance with the declaration of Helsinki and approved by the local ethical committee (N-20160019). The study was registered at ClinicalTrials.gov with the registry ID NCT03886883.
Study protocol
The subjects participated in two 80-min-long sessions, (EIH session and CPM session) at approximately the same time of day with one-to-six days between sessions, to avoid the potential carry-over effect from one stimulation modality to the next. The order of sessions (EIH or CPM first) was randomized and counterbalanced. Before starting data collection, subjects were introduced to the study procedures.
In the EIH session, passive knee extension range of motion (ROM), passive resistive torque (PRT) and pressure pain thresholds (PPT) were assessed before (pre-test), 30 s after (post-test) and 10 min (10 min post-test) after the induction of an EIH response followed by static stretching (SS) of the knee flexors. In accordance with previous procedures, a 30 min wash-out period was maintained between EIH and SS to ensure that possible exercise-induced alterations in pain had subsided prior to commencing SS [22]. In the CPM session, the same variables as in the EIH session (ROM, PRT, and PPT) were assessed before (pre-test), 30 s after (post-test) and 10 min after (10 min post-test) two different conditions; rest/no stimuli and after the induction of the CPM response (Figure 1). To minimize the likelihood of pain-induced distraction on the measurements ROM, PRT and PPT measurements were performed 30 s later [34]. Participants were blinded to the results of all measurements and naïve to the research hypotheses.
![Figure 1:
Illustration of the experimental procedures performed in the two sessions; EIH and CPM. The order of sessions was randomized and counterbalanced. Passive knee extension range of motion [ROM], passive resistive torque [PRT] and pain sensitivity assessed with manual pressure algometry [pressure pain thresholds, PPT] at three assessment sites (dominant thigh, dominant upper arm, and non-dominant shoulder) was assessed before, immediately after and 10 min after each test condition. The EIH sessions consisted of isometric muscle contraction [EIH] and Static Stretch [SS]. The CPM session consisted of rest [Rest] and the cold pressor test [CPM].](/document/doi/10.1515/sjpain-2020-0010/asset/graphic/j_sjpain-2020-0010_fig_005.jpg)
Illustration of the experimental procedures performed in the two sessions; EIH and CPM. The order of sessions was randomized and counterbalanced. Passive knee extension range of motion [ROM], passive resistive torque [PRT] and pain sensitivity assessed with manual pressure algometry [pressure pain thresholds, PPT] at three assessment sites (dominant thigh, dominant upper arm, and non-dominant shoulder) was assessed before, immediately after and 10 min after each test condition. The EIH sessions consisted of isometric muscle contraction [EIH] and Static Stretch [SS]. The CPM session consisted of rest [Rest] and the cold pressor test [CPM].
Assessment of passive range of motion
Passive knee extension range of motion and passive resistive torque were quantified using a Biodex System 4 Pro isokinetic dynamometer (Biodex Medical Systems, Shirley, New York, USA). The Biodex system has a minimum detectable change (MDC95%) of 1.2° (range of motion) and 0.0 Nm (passive resistive torque) based on the standard error of measurement (SEM) reported by Drouin et al. [23]. The torque values were gravity corrected using the embedded software (System 4 Software v4.60). Participants were seated and fixed to the chair with restraining straps over the pelvis, trunk, thigh and lower leg with a hip flexion angle of 100°, a knee extension angle of 80° in accordance with previous procedures [24] (Figure 2). The dynamometer lever arm passively extended the knee at an angular velocity of 5°/s to exclude reflexive muscle activity [1]. The seated test position ensured that tension was placed on the proximal muscle-tendon unit of the hamstrings, which limited the amount of extension around the knee [25]. Participants were instructed to press a stop button when the sensation of stretch changed to pain, which instantaneously stopped the lever arm. This was defined as the stretch tolerance [26]. For each measurement, the test was performed once.

The picture illustrates the experimental set-up using the Biodex. The participant was comfortably seated with the trunk and lower extremities securely fastened with straps. The lever arm of the Biodex passively moved the lower leg towards extension at a speed of 5°/s.
Assessment of pain sensitivity
Pressure Pain Thresholds (PPTs) were assessed using a handheld pressure algometer (Somedic AB, Hörby, Sweden) with a stimulation area of 1 cm2. The rate of pressure increase was kept at 30 kPa/s, and the first time the sensation of pressure was perceived as pain, the subject pressed a button that stopped the stimulation. The pressure value at this time point was defined as the PPT [33]. PPTs were assessed at three different sites; The rectus femoris site was located in the middle of the dominant rectus femoris muscle, 20 cm proximal to the base of the patella. The biceps site was located in the middle of the dominant biceps brachii muscle, 10 cm proximal to the cubital fossa [20]. The shoulder site was located in the middle of the non-dominant middle deltoid muscle. The PPTs were assessed 3 times at each site and the average extracted for data analysis. For each experimental condition, the mean percentage difference in PPTs between pre-test and post-test were calculated and used for analysis.
Induction of exercise-induced hypoalgesia
Exercise-induced hypoalgesia is characterized by reduced pain intensity and pain sensitivity following exercise [27] and can effectively be induced by e.g. performing a submaximal, long-lasting isometric contraction [28]. In this study, an isometric handgrip protocol was employed, consisting of a 3-min trial of submaximal isometric handgrip exercise at 25% of maximal voluntary contraction (MVC). Prior to performing the exercise, the MVC of the hand flexor muscles was determined. Here, the participants were asked to squeeze a handheld dynamometer (Saehan DHD-1 Digital Hand Dynamometer, SH1001, Saehan Corporation, Changwon-City, S. Korea) with their dominant hand, squeezing it as hard as they could for 3 × 5 s with a 1-min interval between trials [29]. The average pressure values were extracted and used to determine the relative intensity (25% of MVC) for the isometric exercise protocol. While performing the isometric exercise, participants were seated with the dominant arm resting on a flat surface with the elbow flexed at 90°. Participants were able to see the dynamometer read-out and were instructed to maintain the force output at a level corresponding to 25% of their MVC. Ratings of perceived exertion (RPE) were assessed every 60 s during the isometric exercise using Borg’s 6–20 RPE scale [30] and ratings of muscle pain in the exercising forearm were assessed prior to completion of the exercise using the pain rating scale developed by Cook et al. (1997) [31].
Static stretch
The static stretch protocol consisted of two bouts of 30 second constant-angle static stretching of the knee flexors with a 1-min rest between bouts in a manoeuvre similar to the assessment of passive range of motion procedure. The stretching movements were stopped by the participants when they felt that the sensation of stretch changed to pain (stretch tolerance) [25], [26], [32] and this position was then kept constant for 30 s.
Quiet rest (no stimuli)
The participants were instructed to relax while comfortably seated in the Biodex.
Induction of conditioned pain modulation (CPM response)
The cold pressor test (CPT) was used to induce a CPM response and was performed with participants in the seated test position. Participants were instructed to immerse their non-dominant hand up to the wrist into a container with circulating water at 1–4 °C for 2 min keeping the hand open. Water temperature was controlled using a digital thermometer (Electronic Temperature Ltd. 810–930; Electronic Temperature Instruments Ltd., Worthing, UK) and a water pump (Aquadistri Aqua-Power 200–200 L; Aquadistri UK Ltd., Cambridgeshire, UK) was used to circulate the water, preventing local warming. The participants rated the cold-induced pain intensity from 0 to 10 on a numerical rating scale (NRS) where 0 was defined as ‘no pain’ and 10 as ‘maximal pain’ [17]. Following this procedure, the participants pulled their hands out of the water.
Statistical analysis
Data management and analysis were performed using SPSS 25 (SPSS Inc., Chicago, IL, USA). The normality of the data was assessed by the Shapiro–Wilks test and the homogeneity-of-variance assumption was assessed by testing for sphericity. Parameters that did not meet the assumption of sphericity were corrected using the Greenhouse–Geisser adjustment. To address the first and second hypotheses of the study, two-way repeated-measures analyses of variance were used to examine the absolute effect of condition (four levels: “EIH”, “Static Stretch”, “Rest” and “CPM”) and time (three levels: “Pre-test”, “Post-test” and “10 min post-test” for “EIH”, “Static Stretch” and “CPM”, and two levels “pre-test” and “10 min post-test” for “Rest”) on range of motion, pressure pain thresholds and passive resistive torque. In case of significant factors or interactions in the RM-ANOVAs, bonferroni corrected post hoc paired-comparisons of pairs of each independent factors were performed. To address the third hypothesis Spearman’s rank correlations were calculated to describe the association between pressure pain thresholds across each experimental condition (EIH, SS, Rest and CPM). Spearman’s rank correlations were also conducted to describe the association between the changes in pressure pain thresholds and changes in range of motion across experimental conditions. An alpha level of 0.05 was defined for the statistical significance of all tests.
Results
The average number of days between sessions was 2.2 ± 1.5 days. Mean (Standard Deviation) ratings of cold-induced pain during CPM, ratings of perceived muscle pain and ratings of perceived exertion during EIH are summarized in Table 1.
Mean (SD) rated pain intensity (NRS: 0–10) during the cold pressor test as well as ratings of perceived muscle pain (Borg 1–10) and ratings of perceived exertion (RPE: 6–20) during and after submaximal isometric handgrip exercise.
| Mean (SD) | ||
|---|---|---|
| Cold pressor test isometric exercise | Pain intensity, NRS (0–10) | 7.1 ± 1 |
| Rating of perceived muscle pain, (Borg CR10) | 6.2 ± 1.2 | |
| Rating of perceived exertion, RPE (6–20) at 60 s | 11.1 ± 2.1 | |
| Rating of perceived exertion, RPE (6–20) at 120 s | 14.3 ± 2 | |
| Rating of perceived exertion, RPE (6–20) at 180 s | 16.1 ± 2.5 |
Pre-test values for ROM, PRT and PPTs were comparable between EIH and CPM sessions (F[1, 18]=0.156, p=0.697), (F [1, 18]=0.058, p=0.812) and (Z>−0.563, p>0.573), respectively (Figures 3 and 4).

Mean (±SD) range of motion before (pre-test), immediately after (post-test) and 10 min after (10 min after) each test condition (e.g., EIH, SS, Rest and CPM). Significantly different compared with pre-test (*p<0.05).
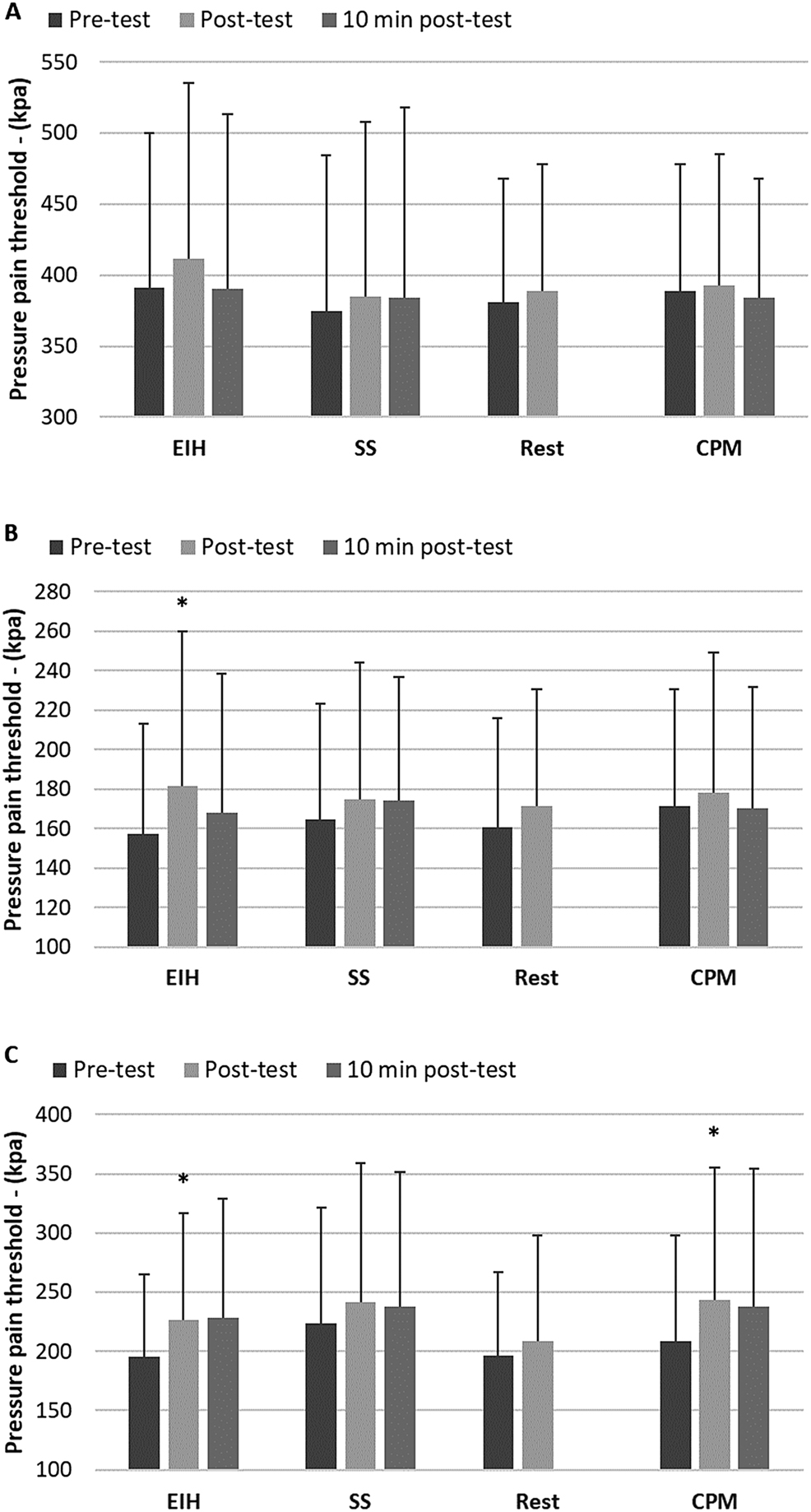
Mean (±SD) pressure pain threshold (PPT) recorded at the rectus femoris (A), biceps (B) and deltoid (C) muscles before (pre-test), immediately after (post-test) and 10 min after (10 min post-test) each test condition (e.g., EIH, SS, Rest and CPM). Significantly different compared with pre-test (*p<0.05).
Range of motion
There was a statistically significant two-way interaction between condition and time for range of motion (F [1,6] =3.092, p=0.008, partial η2=0.147). Therefore, analyses of simple main effects were run. Post-test ROM was significantly different between Rest (171.5 ± 9.7 deg.) and Stretch (178.2 ± 11.9 deg.) and Rest (171.5 ± 9.7 deg.) and CPM (175.6 ± 9.7 deg.) (F[1.891, 34.045]=4.472, p=0.02). ROM increased significantly during EIH (Pre-test: 170.3 ± 10.8 deg.; post-test: 174.2 ± 11 deg., p=0.002) and CPM (Pre-test: 171.3 ± 10.1 deg.; post-test: 175.6 ± 9.4 deg., p=0.001) (Figure 3).
Passive resistive torque
No significant interactions between condition and time were found for passive resistive torque (F[1, 18]=1.476, p=0.222, partial η2=0.054). A significant main effect of time was found for passive resistive torque (F[2.369]=5.444, p=0.09, partial η2=0.233). Post hoc test showed that passive resistive torque increased significantly during EIH (pre-test: 55.1 ± 11; post-test: 58.8 ± 11.2 N-m, p=0.049) and CPM (pre-test 55.1 ± 12.9 N-m; post-test 58.7 ± 14.8 N-m, p=0.018). There was no significant main effect of condition for passive resistive torque (F[3, 54]=1.422, p=0.246).
Pressure pain thresholds
No significant interactions between condition and time were found for pressure pain thresholds (p≥0.09).
A significant main effect of condition was found for the deltoid muscle (F[2.241, 40.631]=5.483, p=0.006) but not the biceps (F[3, 54]=0.353, p=0.787) or rectus femoris muscles (F[1.387, 24.966]=0.323, p=0.641). Post hoc test showed that pre-test pressure pain thresholds for the deltoid muscle were significantly different between EIH (197.7 ± 69.2 kpa) and Stretch (223.9 ± 97.2 kpa) (p=0.046). Post-test pressure pain thresholds for the deltoid muscle were significantly different between Stretch (241.5 ± 117.7 kpa) and Rest (209.1 ± 89.2 kpa) (p=0.05) and CPM (243.6 ± 111.9 kpa) and Rest (209.1 ± 89.2 kpa) (p=0.004).
A significant main effect of time was found for pressure pain thresholds for the deltoid muscle (F[1.153, 20.751]=12.688, p=0.001) and the biceps muscle (F[2, 36]=10.924, p=0.001) but not the rectus femoris muscle (F[1.384, 24.913]=2.465, p=0.120). Post hoc tests showed that pressure pain thresholds increased significantly during EIH for the biceps muscle (pre-test: 155.1 ± 57.8 kpa; post-test: 183.6 ± 77.8 kpa, p=0.003) and the deltoid muscle (pre-test: 195.7 ± 69.2 kpa; post-test: 227.0 ± 89.3 kpa, p=0.001). Likewise, pressure pain thresholds increased significantly during CPM for the deltoid muscle (pre-test: 209.1 ± 89.2 kpa; post-test: 243.6 ± 111.9 kpa, p=0.002) (Figure 4).
Associations between pressure pain thresholds
Moderate, significant correlations in post-test pressure pain thresholds were found between EIH and SS for the biceps muscle (Rho=0.586, p=0.01) and the deltoid muscle (Rho=0.535, p=0.01). A moderate, significant correlation in post-test pressure pain thresholds was found between EIH and CPM for the biceps muscle (Rho=0.562, p=0.01).
A weak, significant correlation was found between post-test pressure pain thresholds and changes in range of motion following CPM (Rho<0.460, p=0.047).
Discussion
This study set out with the preeminent aim of expanding our understanding of the underlining mechanisms related to stretch tolerance.
This is the first study to investigate the role of two endogenous inhibitory mechanisms; exercise-induced hypoalgesia and a conditioning painful stimulus on passive joint range of motion. The main findings were that engaging these endogenous pain modulatory systems results in a significant increase in range of motion. However, in contrast to our expectations, no differences were found in range of motion or changes in pressure pain thresholds when comparing EIH and CPM. The study findings and potential relevance will be discussed in the segments below.
Endogenous pain inhibition increases passive range of joint motion
Although stretching is used for the purpose of injury risk reduction [35], systematic reviews consistently show that stretching seemingly does not reduce the overall risk of exercise-related injury [36], [37], [38]. Considering the hypoalgesic effect of inducing a CPM [39] or an EIH response [27], it is possible that engaging these mechanisms can explain the increase in range of motion as seen here and elsewhere [2] and are known to reduce discomfort such as bothersome soreness [35], [, 40].
In this study, a conscious decision was made to induce an EIH response by activating upper extremity muscles as it has been suggested that increasing soft tissue temperature by way of sport-specific warm-up may increase range of motion [41]. On that note, it is important to consider that performing vigorous exercise close to exhaustion, only results in very small increases in body core temperature within a 3-min window [42] and that exercise must be specific to a particular muscle group in order to increase intramuscular temperature [43]. It is thus likely that the increase in range of motion following EIH can be attributed to exercise-induced endogenous pain inhibition and not an increase in intramuscular temperature in the knee flexors.
The analgesic effect of CPM has been shown to be greater than that of EIH [33] and therefore it was hypothesized that the effect on range of motion and pain sensitivity would be greater following CPM than EIH. This was however not supported by present findings where no difference in range of motion or changes in pain sensitivity was found when comparing EIH and CPM. In line with these findings, the present results revealed a moderate, significant correlation between the pain tolerance responses (CPM effect) following EIH and CPM for the biceps muscle. This contrasts the findings of Vaegter et al. [33] who found no correlation between these two phenomena.
Although isometric exercise can induce EIH with both painful and non-painful contractions, it is known that the magnitude of the analgesic effect is greater with intensities that generally induce more pain [44]. Therefore, the relationship between the CPM and EIH responses seen here may be related to the intensity of perceived muscle pain during EIH in the present study which was greater than that of comparable studies [29], [, 45].
At present, the mechanisms responsible for EIH are insufficiently understood. The endogenous opioid system has received significant attention [27] where both opioid and nonopioid mechanisms have been implicated. This indicates that there are likely multiple mechanisms responsible for EIH [46], including increased secretion of β-endorphins, attention mechanisms, activation of diffuse noxious inhibitory controls, or an interaction of the cardiovascular and pain regulatory systems [47]. The hypoalgesic effect of the isometric exercise and the CPT seen in the present study were multisegmental which suggests that central widespread inhibitory mechanisms were activated by both static muscle contractions and CPT. It is therefore likely, that a great part of the EIH effect seen in the present study could be related to endogenous inhibitory pain mechanisms.
The present results showed a weak but significant correlation between the changes in range of motion and the magnitude of endogenous analgesia following CPM. The results thus suggest that the changes in range of motion are associated but not linearly dependent on the magnitude of endogenous analgesia. This finding broadly supports the postulation that pain inhibition is likely a saturable phenomenon [48] indicating that these mechanisms can only reduce the sensitivity to nociceptive stimuli up to a certain level. The moderate correlations between post-test pain tolerance responses, suggests that a static muscle stretch may reduce the sensitivity of central pain mechanisms. Present findings thus warrant further investigations on the potential effect muscle stretching has on overall pain sensitivity.
Practical implications
Stretching is commonly used in relation to sport as part of pre- and post-activity routines as well as in rehabilitation to increase function and improve flexibility. The present findings suggest that stretch tolerance is, to some degree dependent on endogenous inhibition. With the current findings in mind, and considering that reduced endogenous pain inhibition is commonly seen in various musculoskeletal pain conditions [49], stretch tolerance may simply be a marker for the overall pain sensitivity. Given that stretch tolerance seems to depend on endogenous pain inhibition it may therefore be likely that patients with chronic pain may respond differently to stretching.
In rehabilitation, stretching has been shown effective to improve function in patients with musculoskeletal pain and has therefore been advocated for in multidisciplinary pain management programs [9]. Interestingly though, Law et al. [9] did not find that their stretching program affected muscle extensibility which is supported by the current findings where the acute effect of stretching did neither increase range of motion nor reduce pain sensitivity.
Methodological considerations
Previous findings suggest that the EIH effect following isometric exercise is short-lasting [50]. For this reason, the 30-min wash-out period was implemented between the two conditions (EIH and SS) to ensure that possible exercise-induced alterations in pain had subsided prior to commencing SS. Nevertheless, the present findings indicate that the hypoalgesic effect did not fully attenuate in the 30 min following EIH (Figure 3) which is in contrast to the findings of Kosek & Lundberg [47] who found that the EIH effect attenuated within 30 min after cessation of isometric exercise. These differences may, however, relate to methodological variations in the isometric protocols, used to induce the EIH effect [50].
In contrast to previous findings, the current study did not show an acute effect of static stretch on knee extension range of motion [12]. This discrepancy is however likely attributed to a potential carry-over hypoalgesic effect from the EIH protocol that may have influenced subsequent responses to SS given that pain inhibition is potentially a saturable phenomenon [48]. The result was that the ‘pre-test’ stretch results for range of motion were higher (although not significantly) than the ‘pre-test’ values for the EIH and CPM conditions. This should, therefore, be considered when interpreting present findings regarding the effect of static stretching.
Current evidence demonstrates gender differences in hamstring extensibility and although gender differences in the intensity of pain elicited during stretching have been suggested as an explanatory variable [51], the contribution of gender on the magnitude of endogenous analgesia has provided inconsistent findings [15] with no apparent gender differences in thermal pain sensitivity following stretching [7]. Accordingly, further research assessing whether men and women differ in stretch tolerance responses is warranted.
Conclusion
By engaging the endogenous pain inhibitory mechanisms similar to what was done here with, either through exercise or by introducing a competing painful stimulus, the tolerance to stretch increases. This pain inhibitory response then increases passive knee extension range of motion. The results imply that the tolerance to stretch is associated with pain sensitivity but not linearly dependent on the magnitude of endogenous analgesia.
Funding source: University College of Northern Denmark (UCN)
Award Identifier / Grant number: 24000160
Acknowledgments
The authors wish to thank Marte Ingebrigtsen Sverdrup, BPt; Jesper Pedersen, BPt; Jens Roding Grunnet Dahlgaard, BPt; and Rikke Roskær Axelsen. BPt. for their assistance during data collection.
-
Research funding: This project was funded by the Department of Physiotherapy, University College of Northern Denmark (UCN) [grant number 24000160].
-
Author contributions: All authors contributed to the design of the study, the analysis and interpretation of the data, as well as making intellectual contributions to its content. Morten Pallisgaard Støve collected data.
-
Competing interests: Authors state no conflict of interest.
-
Informed consent: Informed consent has been obtained from all individuals included in this study.
-
Ethical approval: The research related to human use complies with all the relevant national regulations, institutional policies and was performed in accordance with the tenets of the Helsinki Declaration, and has been approved by the local ethical committee (N-20160019).
References
1. Herda, TJ, Costa, PB, Walter, AA, Ryan, ED, Hoge, KM, Kerksick, CM, et al. Effects of two modes of static stretching on muscle strength and stiffness. Med Sci Sports Exerc 2011;43:1777–84. Available from: http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00005768-201109000-00022.10.1249/MSS.0b013e318215cda9Suche in Google Scholar PubMed
2. Behm, DG, Blazevich, AJ, Kay, AD, Mchugh, M. Acute effects of muscle stretching on physical performance, range of motion, and injury incidence in healthy active individuals: a systematic review. Appl Physiol Nutr Metabol 2016;11:1–11. https://doi.org/10.1139/apnm-2015-0235.Suche in Google Scholar PubMed
3. Bleakley, CM, Costello, JT. Do thermal agents affect range of movement and mechanical properties in soft tissues? A systematic review. Arch Phys Med Rehabil 2013;94:149–63. https://doi.org/10.1016/j.apmr.2012.07.023.Suche in Google Scholar PubMed
4. Weppler, CH, Magnusson, SP. Increasing muscle extensibility: a matter of increasing length or modifying sensation? Phys Ther 2010;90:438–49. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20075147.10.2522/ptj.20090012Suche in Google Scholar PubMed
5. Marshal, WMP, Lovell, R, Siegler, CJ. Changes in passive tension of the hamstring muscles during a simulated soccer match authors. Int J Sports Physiol Perform 2015;25:594–601. doi:https://doi.org/10.1123/ijspp.2015-0009.Suche in Google Scholar PubMed
6. Chaouachi, A, Padulo, J, Kasmi, S, Othmen, AB, Chatra, M, Behm, DG. Unilateral static and dynamic hamstrings stretching increases contralateral hip flexion range of motion. Clin Physiol Funct Imag 2017;37:23–9. https://doi.org/10.1111/cpf.12263.Suche in Google Scholar PubMed
7. Bishop, MD, George, SZ. Pain sensitivity and torque used during measurement predicts change in range of motion at the knee. J Pain Res 2017;10:2711–6. https://doi.org/10.2147/jpr.s150775.Suche in Google Scholar PubMed PubMed Central
8. Blazevich, AJ, Cannavan, D, Waugh, CM, Miller, SC, Thorlund, JB, Aagaard, P, et al. Range of motion, neuromechanical, and architectural adaptations to plantar flexor stretch training in humans. J Appl Physiol 2014;117:452–62. Available from: http://jap.physiology.org/cgi/doi/10.1152/japplphysiol.00204.2014.10.1152/japplphysiol.00204.2014Suche in Google Scholar PubMed
9. Law, RY, Harvey, LA, Nicholas, MK, Tonkin, L, De Sousa, M, Finniss, DG. Stretch exercises increase tolerance to stretch in patients with chronic musculoskeletal pain: a randomized controlled trial. Phys Ther 2009;89:1016–26. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=19696119.10.2522/ptj.20090056Suche in Google Scholar PubMed
10. Magnusson, SP, Simonsen, EB, Aagaard, P, Boesen, J, Johannsen, F, Kjaer, M. Determinants of musculoskeletal flexibility: viscoelastic properties, cross-sectional area, EMG and stretch tolerance. Scand J Med Sci Sports 1997;7:195–202. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=9241023.10.1111/j.1600-0838.1997.tb00139.xSuche in Google Scholar PubMed
11. Knudson, D. The biomechanics of stretching. J Exerc Sci Physiother 2006;2:3–12.Suche in Google Scholar
12. Støve, MP, Hirata, RP, Palsson, TS. Muscle stretching – the potential role of endogenous pain inhibitory modulation on stretch tolerance. Scand J Pain 2019;19:415–22.10.1515/sjpain-2018-0334Suche in Google Scholar PubMed
13. Cabido, CET, Bergamini, JC, Andrade, AGP, Lima, FV, Menzel, HJ, Chagas, MH. Acute effect of constant torque and angle stretching on range of motion, muscle passive properties, and stretch discomfort perception. J Strength Cond Res 2013;28:1050–7. Available from: http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00124278-900000000-97643.10.1519/JSC.0000000000000241Suche in Google Scholar PubMed
14. Yarnitsky, D. Conditioned pain modulation (the diffuse noxious inhibitory control-like effect): its relevance for acute and chronic pain states. Curr Opin Anaesthesiol 2010;23:611–5. https://doi.org/10.1097/aco.0b013e32833c348b.Suche in Google Scholar
15. Pud, D, Granovsky, Y, Yarnitsky, D. The methodology of experimentally induced diffuse noxious inhibitory control (DNIC)-like effect in humans. Pain 2009;144:16–9. https://doi.org/10.1016/j.pain.2009.02.015.Suche in Google Scholar PubMed
16. Moont, R, Pud, D, Sprecher, E, Shavrit, G, Yarnitsky, D. “Pain inhibits pain” mechanisms: is pain modulation simply due to distraction? Pain 2010;150:113–20. https://doi.org/10.1016/j.pain.2010.04.009.Suche in Google Scholar PubMed
17. Vaegter, HB, Handberg, G, Graven-Nielsen, T. Hypoalgesia after exercise and the cold pressor test is reduced in cronic musculoskeletal pain patients with high pain sensitivity. Clin J Pain 2016;32:58–69. https://doi.org/10.1097/ajp.0000000000000223.Suche in Google Scholar PubMed
18. Lewis, GN, Rice, DA, McNair, PJ. Conditioned pain modulation in populations with chronic pain: a systematic review and meta-analysis. [cited 2020 Feb 19]. J Pain 2012;13:936–44. Available from: http://sfx.dbc.dk/dbc-45DBC_UCN-45DBC_UCN?ctx_enc=info%3Aofi%2Fenc%3AUTF-8&ctx_ver=Z39.88-2004&req.language=dan&rfr_id=info%3Asid%2FElsevier%3ASD&rft.atitle=Conditioned+Pain+Modulation+in+Populations+With+Chronic+Pain%3A+A+Systematic+Review+and+Meta-Analy.Suche in Google Scholar
19. Pud, D, Sprecher, E, Yarnitsky, D. Homotopic and heterotopic effects of endogenous analgesia in healthy volunteers. Neurosci Lett 2005;380:209–13. https://doi.org/10.1016/j.neulet.2005.01.037.Suche in Google Scholar PubMed
20. Vaegter, HB, Handberg, G, Jørgensen, MN, Kinly, A, Graven-nielsen, T. Aerobic exercise and cold pressor test induce hypoalgesia in active and inactive men and women. Pain Med 2015;16:923–33. https://doi.org/10.1111/pme.12641.Suche in Google Scholar PubMed
21. Rezaii, T, Hirschberg, AL, Carlström, K, Ernberg, M. The influence of menstrual phases on pain modulation in healthy women. J Pain 2012;13:646–55. https://doi.org/10.1016/j.jpain.2012.04.002.Suche in Google Scholar PubMed
22. Jones, MD, Taylor, JL, Booth, J, Barry, BK. Exploring the mechanisms of exercise-induced hypoalgesia using somatosensory and laser evoked potentials. Front Physiol 2016;7. https://doi.org/10.3389/fphys.2016.00581.Suche in Google Scholar PubMed PubMed Central
23. Drouin, BJM, Valovich-mcleod, TC, Shultz, SJ, Gansneder, BM, Perrin, DH. Reliability and validity of the biodex system 3 pro isokinetic dynamometer velocity, torque and postition measurements. Eur J Appl Physiol 2004;91:22–9.10.1007/s00421-003-0933-0Suche in Google Scholar PubMed
24. Støve, MP, Palsson, TS, Hirata, RP. Smartphone-based accelerometry is a valid tool for measuring dynamic changes in knee extension range of motion. Knee 2018;25:66–72. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0968016017302983.10.1016/j.knee.2017.11.001Suche in Google Scholar PubMed
25. Magnusson, SP, Simonsen, EB, Aagaard, P, Dyhre-Poulsen, P, McHugh, MP, Kjaer, M. Mechanical and physical responses to stretching with and without preisometric contraction in human skeletal muscle. Arch Phys Med Rehabil 1996;77:373–8. https://doi.org/10.1016/s0003-9993(96)90087-8.Suche in Google Scholar PubMed
26. Laessøe, U, Voigt, M. Modification of stretch tolerance in a stooping position. Scand J Med Sci Sports 2004;14:239–44. Available from: http://www3.interscience.wiley.com/journal/118785899/abstract.10.1111/j.1600-0838.2003.00332.xSuche in Google Scholar PubMed
27. Koltyn, KF, Brellenthin, AG, Cook, DB, Sehgal, N, Hillard, C. Mechanisms of exercise-induced hypoalgesia. J Pain 2014;15:1294–304.10.1016/j.jpain.2014.09.006Suche in Google Scholar PubMed PubMed Central
28. Naugle, KM, Naugle, KE, Fillingim, RB, Samuels, B, Joseph, LRIII. Intensity thresholds for aerobic exercise – induced hypoalgesia. Med Sci Sports Exerc 2014;46:817–25. https://doi.org/10.1249/mss.0000000000000143.Suche in Google Scholar
29. Naugle, KM, Naugle, KE, Fillingim, RB, Riley, JL. Isometric exercise as a test of pain Modulation: effects of experimental pain test, psychological variables, and sex. Pain Med 2013;15:692–701. https://doi.org/10.1111/pme.12312.Suche in Google Scholar PubMed PubMed Central
30. Borg, G. Borg’s perceived exertion and pain scales. Human Kinetics 1998;110. ISBN 0880116234.Suche in Google Scholar
31. Cook, DB, O’Connor, PJ, Eubanks, SA, Smith, JC, Lee, M. Naturally occurring muscle pain during exercise: assessment and experimental evidence. Med Sci Sports Exerc 1997;29:999–1012. Available from: http://www.ncbi.nlm.nih.gov/pubmed/9268956.10.1097/00005768-199708000-00004Suche in Google Scholar PubMed
32. Iwata, M, Yamamoto, A, Matsuo, S, Hatano, G, Miyazaki, M, Fukaya, T, et al. Dynamic stretching has sustained effects on range of motion and passive stiffness of the hamstring muscles. J Sports Sci Med 2019;18:13–20.Suche in Google Scholar
33. Vaegter, HB, Handberg, G, Graven-Nielsen, T. Similarities between exercise-induced hypoalgesia and conditioned pain modulation in humans. Pain 2013;155:158–67.10.1016/j.pain.2013.09.023Suche in Google Scholar PubMed
34. Defrin, R, Tsedek, I, Lugasi, I, Moriles, I, Urca, G. The interactions between spatial summation and DNIC: effect of the distance between two painful stimuli and attentional factors on pain perception. Pain 2010;151:489–95. Available from: http://journals.lww.com/pain/Fulltext/2010/11000/The_interactions_between_spatial_summation_and.33.aspx.10.1016/j.pain.2010.08.009Suche in Google Scholar PubMed
35. Herbert, RD, de Noronha, M, Kamper, S. Stretching to prevent or reduce muscle soreness after exercise. Cochrane Database Syst Rev 2007:CD004577. Available from: http://www.ncbi.nlm.nih.gov/pubmed/17943822.10.1002/14651858.CD004577.pub2Suche in Google Scholar PubMed
36. Leppänen, M, Aaltonen, S, Parkkari, J, Heinonen, A, Kujala, UM. Interventions to prevent sports related injuries: a systematic review and meta-analysis of randomised controlled trials. Sports Med 2014;44:473–86. https://doi.org/10.1007/s40279-013-0136-8.Suche in Google Scholar PubMed
37. Lauersen, JB, Bertelsen, DM, Andersen, LB. The effectiveness of exercise interventions to prevent sports injuries: a systematic review and meta-analysis of randomised controlled trials. Br J Sports Med 2014;48:871–7. https://doi.org/10.1136/bjsports-2013-092538.Suche in Google Scholar PubMed
38. Small, K, Mc Naughton, L, Matthews, M. A systematic review into the efficacy of static stretching as part of a warm-up for the prevention of exercise-related injury. Res Sports Med 2008;16:213–31. https://doi.org/10.1080/15438620802310784.Suche in Google Scholar PubMed
39. Nir, R-R, Yarnitsky, D. Conditioned pain modulation. Curr Opin Support Palliat Care 2015;9:131–7. Available from: https://journals.lww.com/co-supportiveandpalliativecare/Fulltext/2015/06000/Conditioned_pain_modulation.9.aspx.10.1097/SPC.0000000000000126Suche in Google Scholar PubMed
40. Jamtvedt, G, Herbert, RD, Flottorp, S, Odgaard-Jensen, J, Håvelsrud, K, Barratt, A, et al. A pragmatic randomised trial of stretching before and after physical activity to prevent injury and soreness. Br J Sports Med 2010;44:1002–9. https://doi.org/10.1136/bjsm.2009.062232.Suche in Google Scholar PubMed
41. Smith, CA. The warm-up procedure: to stretch or not to stretch. A breif review. J Orthop Sports Phys Ther 1994;19:12–7. https://doi.org/10.2519/jospt.1994.19.1.12.Suche in Google Scholar PubMed
42. González-Alonso, J, Quistorff, B, Krustrup, P, Bangsbo, J, Saltin, B, Gonzalez-Alonso, J, et al. Heat production in human skeletal muscle at the onset of intense dynamic exercise. J Physiol 2000;524:603–15. Available from: http://view.ncbi.nlm.nih.gov/pubmed/10766936%5Cnhttp://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2269891&tool=pmcentrez&rendertype=abstract.10.1111/j.1469-7793.2000.00603.xSuche in Google Scholar PubMed PubMed Central
43. Wirth, VJ, Van Lunen, BL, Mistry, D, Saliba, E, McCue, FC. Temperature changes in deep muscles of humans during upper and lower extremity exercise. J Athl Train 1998;33:211–5.Suche in Google Scholar
44. Law, LAF, Lee, JE, McMullen, TR, Xia, T. Relationships between maximum holding time and ratings of pain and exertion differ for static and dynamic tasks. Appl Ergon 2011;42:9–15.10.1016/j.apergo.2010.03.007Suche in Google Scholar PubMed PubMed Central
45. Umeda, M, Newcomb, LW, Ellingson, LD, Koltyn, KF. Examination of the dose-response relationship between pain perception and blood pressure elevations induced by isometric exercise in men and women. Biol Psychol 2010;85:90–6.10.1016/j.biopsycho.2010.05.008Suche in Google Scholar PubMed
46. Koltryn, KF. Analgesia following exercise: a review. Sports Med 2000;29:85–98.10.2165/00007256-200029020-00002Suche in Google Scholar PubMed
47. Kosek, E, Lundberg, L. Segmental and plurisegmental modulation of pressure pain thresholds during static muscle contractions in healthy individuals. Eur J Pain 2003;7:251–8. https://doi.org/10.1016/s1090-3801(02)00124-6.Suche in Google Scholar PubMed
48. Granot, M, Weissman-Fogel, I, Crispel, Y, Pud, D, Granovsky, Y, Sprecher, E, et al. Determinants of endogenous analgesia magnitude in a diffuse noxious inhibitory control (DNIC) paradigm: do conditioning stimulus painfulness, gender and personality variables matter? Pain 2008;136:142–9. https://doi.org/10.1016/j.pain.2007.06.029.Suche in Google Scholar PubMed
49. Staud, R. Abnormal endogenous pain modulation is a shared characteristic of many chronic pain conditions. Expert Rev Neurother 2013;12:577–85.10.1586/ern.12.41Suche in Google Scholar PubMed PubMed Central
50. Naugle, KM, Fillingim, RB, Riley, JI. A meta-analytic review of the hypoalegsic effects of exercise. J Pain 2012;13:1139–50. https://doi.org/10.1016/j.jpain.2012.09.006.Suche in Google Scholar PubMed PubMed Central
51. Marshall, PW, Siegler, JC. Lower hamstring extensibility in men compared to women is explained by differences in stretch tolerance. BMC Musculoskelet Disord 2014;15:223. Available from: http://www.biomedcentral.com/1471-2474/15/223.10.1186/1471-2474-15-223Suche in Google Scholar PubMed PubMed Central
© 2020 Walter de Gruyter GmbH, Berlin/Boston
Artikel in diesem Heft
- Frontmatter
- Editorial
- Salami-slicing and duplicate publication: gatekeepers challenges
- Editorial Comment
- Risk for persistent post-delivery pain – increased by pre-pregnancy pain and depression. Similar to persistent post-surgical pain in general?
- Systematic Review
- Acute experimentally-induced pain replicates the distribution but not the quality or behaviour of clinical appendicular musculoskeletal pain. A systematic review
- Topical Review
- Unwillingly traumatizing: is there a psycho-traumatologic pathway from general surgery to postoperative maladaptation?
- Clinical Pain Research
- Translation, cross-cultural adaptation and psychometric evaluation of the Thai version of the fear-avoidance beliefs questionnaire in patients with non-specific neck pain
- Pain management in patients undergoing radiation therapy for head and neck cancer – a descriptive study
- Do intensity of pain alone or combined with pain duration best reflect clinical signs in the neck, shoulder and upper limb?
- Different pain variables could independently predict anxiety and depression in subjects with chronic musculoskeletal pain
- Symptoms of central sensitization in patients with inflammatory bowel diseases: a case-control study examining the role of musculoskeletal pain and psychological factors
- Acceptability of psychologically-based pain management and online delivery for people living with HIV and chronic neuropathic pain: a qualitative study
- Determinants of pain occurrence in dance teachers
- Observational Studies
- A retrospective observational study comparing somatosensory amplification in fibromyalgia, chronic pain, psychiatric disorders and healthy subjects
- Utilisation of pain counselling in osteopathic practice: secondary analysis of a nationally representative sample of Australian osteopaths
- Effectiveness of ESPITO analgesia in enhancing recovery in patients undergoing open radical cystectomy when compared to a contemporaneous cohort receiving standard analgesia: an observational study
- Shoulder patients in primary and specialist health care. A cross-sectional study
- The tolerance to stretch is linked with endogenous modulation of pain
- Pain sensitivity increases more in younger runners during an ultra-marathon
- Original Experimental
- DNA methylation changes in genes involved in inflammation and depression in fibromyalgia: a pilot study
- Participants with mild, moderate, or severe pain following total hip arthroplasty. A sub-study of the PANSAID trial on paracetamol and ibuprofen for postoperative pain treatment
- Exploring peoples’ lived experience of complex regional pain syndrome in Australia: a qualitative study
- Although tapentadol and oxycodone both increase colonic volume, tapentadol treatment resulted in softer stools and less constipation: a mechanistic study in healthy volunteers
- Educational Case Report
- Updated management of occipital nerve stimulator lead migration: case report of a technical challenge
Artikel in diesem Heft
- Frontmatter
- Editorial
- Salami-slicing and duplicate publication: gatekeepers challenges
- Editorial Comment
- Risk for persistent post-delivery pain – increased by pre-pregnancy pain and depression. Similar to persistent post-surgical pain in general?
- Systematic Review
- Acute experimentally-induced pain replicates the distribution but not the quality or behaviour of clinical appendicular musculoskeletal pain. A systematic review
- Topical Review
- Unwillingly traumatizing: is there a psycho-traumatologic pathway from general surgery to postoperative maladaptation?
- Clinical Pain Research
- Translation, cross-cultural adaptation and psychometric evaluation of the Thai version of the fear-avoidance beliefs questionnaire in patients with non-specific neck pain
- Pain management in patients undergoing radiation therapy for head and neck cancer – a descriptive study
- Do intensity of pain alone or combined with pain duration best reflect clinical signs in the neck, shoulder and upper limb?
- Different pain variables could independently predict anxiety and depression in subjects with chronic musculoskeletal pain
- Symptoms of central sensitization in patients with inflammatory bowel diseases: a case-control study examining the role of musculoskeletal pain and psychological factors
- Acceptability of psychologically-based pain management and online delivery for people living with HIV and chronic neuropathic pain: a qualitative study
- Determinants of pain occurrence in dance teachers
- Observational Studies
- A retrospective observational study comparing somatosensory amplification in fibromyalgia, chronic pain, psychiatric disorders and healthy subjects
- Utilisation of pain counselling in osteopathic practice: secondary analysis of a nationally representative sample of Australian osteopaths
- Effectiveness of ESPITO analgesia in enhancing recovery in patients undergoing open radical cystectomy when compared to a contemporaneous cohort receiving standard analgesia: an observational study
- Shoulder patients in primary and specialist health care. A cross-sectional study
- The tolerance to stretch is linked with endogenous modulation of pain
- Pain sensitivity increases more in younger runners during an ultra-marathon
- Original Experimental
- DNA methylation changes in genes involved in inflammation and depression in fibromyalgia: a pilot study
- Participants with mild, moderate, or severe pain following total hip arthroplasty. A sub-study of the PANSAID trial on paracetamol and ibuprofen for postoperative pain treatment
- Exploring peoples’ lived experience of complex regional pain syndrome in Australia: a qualitative study
- Although tapentadol and oxycodone both increase colonic volume, tapentadol treatment resulted in softer stools and less constipation: a mechanistic study in healthy volunteers
- Educational Case Report
- Updated management of occipital nerve stimulator lead migration: case report of a technical challenge

