A 39-year-old female was admitted due to bilateral temporomandibular joint (TMJ) pain, more severe on the left side than the left dise, accompanied by a clicking sound for 3 months. These symptoms were more noticeable during eating, occasionally leading to chewing difficulties. The patient denied any history of trauma or gum disease and reported no discomfort in other joints. She was positive for high titers of anticyclic citrullinated peptide (CCP) antibodies ( > 200 U/mL) and anti-mutant citrullinated vimentin (MCV) antibodies ( > 1000 U/mL). Her rheumatoid factor (RF), erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) levels were all within the normal range. The cone-beam computed tomography (CBCT) of TMJ showed osteophyte and surface erosion of the anterior bevel of the right condyle (Figure 1 A-B). Magnetic resonance imaging (MRI) of the TMJ revealed subcortical cyst at the anterior bevel of the right condyle, along with deformities of both articular discs and irreducible anterior internal displacement (Figure 1C). She was given a probable diagnosis of rheumatoid arthritis (RA) and was initially treated with methotrexate (15 mg/wk). Six months later, her TMJ pain and clicking sound improved significantly. MRI showed reduced cystic degeneration of the right condyle compared to previous scans (Figure 1D).
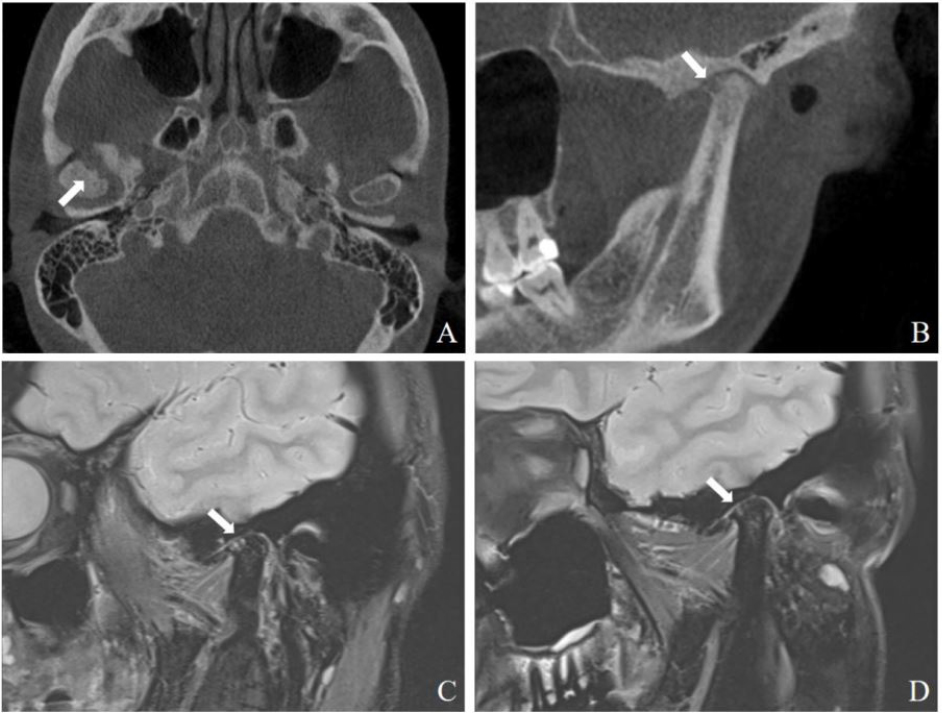
A: Axial view of CBCT shows osteophyte and surface erosion in the anterior bevel of the right condyle (arrow). B: Oblique sagittal view of CBCT shows osteophyte and surface erosion in the anterior bevel of the right condyle (arrow). C: MRI shows subcortical cyst in the right joint fossa and condyle (arrow). D: MRI shows reduction of cystic lesions in the right articular fossa and condyle after treatment (arrow).
Involvement of the TMJ in patients with RA is common, ranging between 45% and 92%.[1] However, temporomandibular disorder (TMD) related to RA is underestimated, largely due to its non-specific clinical manifestations and was not routinely examed.[2,3] MRI is currently the gold standard for diagnosing TMD because of its high resolution to differentiate joint and its surrounding soft tissue. CBCT can clearly display bone details. Therefore, MRI combined with CBCT can provide a more comprehensive assessment of TMD in patients with RA. TMJ involvement in RA can cause abnormalities in bone, joint space, and surrounding soft tissue, resulting in diverse clinical manifestations.[1] The destruction or absorption of condylar bone and cysts of the condyle may be specific imaging features of RA-TMJ, helping in distinguishing from other conditions like osteoarthritis (OA).[4,5]
Funding statement: None.
Acknowledgements
None.
-
Author contributions
Jun Li: Writing-Original draft preparation. Xin Gao and Haitao Dong: Writing-Reviewing and Editing. Jiuliang Zhao: Supervision. All authors have read and agreed to the published version of the manuscript.
-
Informed consent
Informed consent has been obtained. The patient has given her consent for her images and other clinical information to be reported in the journal.
-
Ethical approval
Not applicable.
-
Conflict of interest
Jiuliang Zhao is an Editorial Board Member of the journal. The article was subjected to the standard procedures of the journal, with a review process independent of the editor and his research group.
-
Data availability statement
No additional data is available.
References
[1] Pantoja LLQ, de Toledo IP, Pupo YM, et al. Prevalence of degenerative joint disease of the temporomandibular joint: a systematicreview. Clin Oral Investig. 2019;23:2475–2488.10.1007/s00784-018-2664-ySuche in Google Scholar PubMed
[2] Mustafa MA, Al-Attas BA, Badr FF, et al. Prevalence and Severity of Temporomandibular Disorders in Rheumatoid Arthritis Patients. Cureus. 2022;14:e2127610.7759/cureus.21276Suche in Google Scholar PubMed PubMed Central
[3] Schmidt C, Ertel T, Arbogast M, et al. The Diagnosis and Treatment of Rheumatoid and Juvenile Idiopathic Arthritis of the Temporomandibular Joint. Dtsch Arztebl Int. 2022;119:47–54.10.3238/arztebl.m2021.0388Suche in Google Scholar PubMed PubMed Central
[4] 4. Kretapirom K, Okochi K, Nakamura S, et al. MRI characteristics of rheumatoid arthritis in the temporomandibular joint. Dentomaxillofac Radiol. 2013;42:31627230.10.1259/dmfr/31627230Suche in Google Scholar PubMed PubMed Central
[5] Goupille P, Fouquet B, Cotty P, et al. Direct coronal computed tomography of the temporomandibular joint in patients with rheumatoid arthritis. Br J Radiol. 1992;65:955–960.10.1259/0007-1285-65-779-955Suche in Google Scholar PubMed
© 2024 Jun Li, Xin Gao, Haitao Dong, Jiuliang Zhao, published by De Gruyter on behalf of NCRC-DID
This work is licensed under the Creative Commons Attribution 4.0 International License.
Artikel in diesem Heft
- Editorial
- Enhancing standardized diagnosis and treatment to improve the prognosis of patients with rheumatoid arthritis in China
- The potential for biosimilars to address unmet clinical need — Is the developed world missing out?
- Guideline
- Chinese guidelines for the diagnosis and treatment of rheumatoid arthritis: 2024 update
- Review
- Therapeutic potential of CD20/CD3 bispecific antibodies in the treatment of autoimmune diseases
- Original Article
- 14-3-3 Eta protein as a novel biomarker in early detection of uveitis in Egyptian juvenile idiopathic arthritis and rheumatoid arthritis patients: Diagnostic and prognostic value
- Immunomodulatory effects of novel nano micelle based curcumin in rheumatoid arthritis patients: A double blind randomized clinical trial
- Letter to the Editor
- McArdle’s disease presents with multiple large vessel lesions
- Images
- “Bouncing temporomandibular joint”: Multiple temporomandibular lesions in a patient with rheumatoid arthritis
Artikel in diesem Heft
- Editorial
- Enhancing standardized diagnosis and treatment to improve the prognosis of patients with rheumatoid arthritis in China
- The potential for biosimilars to address unmet clinical need — Is the developed world missing out?
- Guideline
- Chinese guidelines for the diagnosis and treatment of rheumatoid arthritis: 2024 update
- Review
- Therapeutic potential of CD20/CD3 bispecific antibodies in the treatment of autoimmune diseases
- Original Article
- 14-3-3 Eta protein as a novel biomarker in early detection of uveitis in Egyptian juvenile idiopathic arthritis and rheumatoid arthritis patients: Diagnostic and prognostic value
- Immunomodulatory effects of novel nano micelle based curcumin in rheumatoid arthritis patients: A double blind randomized clinical trial
- Letter to the Editor
- McArdle’s disease presents with multiple large vessel lesions
- Images
- “Bouncing temporomandibular joint”: Multiple temporomandibular lesions in a patient with rheumatoid arthritis

