Abstract
Objectives
In our neonatal intensive care unit (NICU), patients are screened for colonization with Staphylococcus aureus (S. aureus) and decolonized if positive. During the COVID-19 pandemic, our NICU significantly limited its visitor policy. We assessed for a difference between S. aureus colonization rates before and after the visitor policy change, which coincided with the exponential rise of COVID-19 cases in New York City (NYC).
Methods
We calculated rates of newly S. aureus colonized NICU patients during January to June 2020 and compared rates pre- and post-implementation of the new visitor policy. Additionally, we obtained the weekly incidence of COVID-19 in NYC and assessed for a correlation between COVID-19 rates and S. aureus colonization.
Results
The number of newly colonized patients per thousand patient days was 4.65 pre- and 3.95 post-implementation of the new visitor policy. The difference was not statistically significant (p=0.66). Furthermore, there was no correlation between the incidence of COVID-19 in NYC and the rates of S. aureus colonization in our NICU (R2=0.02).
Conclusions
Our results suggest that limiting visitation of patients is not associated with a decrease in S. aureus colonization rate. Hospital unit leaders may need to focus on other strategies in order to reduce colonization.
New York City (NYC) is a metropolitan area with relatively high rates of Staphylococcus aureus (S. aureus) infection and colonization [1]. In our neonatal intensive care unit (NICU) in NYC, our policy is to test neonates for colonization with S. aureus weekly and decolonize them with mupirocin ointment and chlorhexidine baths if positive. This practice has become standard of care in many NICUs and other hospital units across the country, as there is evidence to suggest that decolonization reduces the risk for both methicillin-susceptible S. aureus (MSSA) and methicillin-resistant S. aureus (MRSA) infections [2, 3]. Furthermore, both clinical and culture-proven infections during neonatal hospitalizations, particularly in extremely low-birthweight infants, are associated with morbidity, including adverse neurodevelopmental outcomes and growth impairment, and mortality [4].
Newly S. aureus colonized patients per 1,000 patient days pre- and post-visitor policy change.
| 2-week period in 2020 | Patient-days | Newly S. aureus colonized patients | Newly colonized patients per 1,000 patient-days |
|---|---|---|---|
| January 6–19 | 566 | 1 | 1.77 |
| January 20–February 2 | 623 | 3 | 4.82 |
| February 3–16 | 620 | 3 | 4.84 |
| February 17–March 1 | 573 | 3 | 5.24 |
| March 2–15 | 626 | 4 | 6.39 |
| March 16–29 | 608 | 3 | 4.93 |
| March 30–April 12 | 560 | 2 | 3.57 |
| April 13–26 | 581 | 2 | 3.44 |
| April 27–May 10 | 473 | 2 | 4.23 |
| May 11–24 | 502 | 5 | 9.96 |
| May 25–June 7 | 498 | 1 | 2.01 |
| June 8–21 | 573 | 0 | 0 |
|
|
|||
| Total pre- and post- visitor policy | |||
|
|
|||
| January 6–March 15 | 3,008 | 14 | 4.65a |
| March 16–June 21 | 3,795 | 15 | 3.95a |
-
We modeled the number of biweekly colonization cases pre- and post-intervention using negative-binomial regression with a logistic link with SAS 9.04. The outcome was generated as a count variable representing a number of cases falling into each of the weeks over time. An alpha of 0.05 was used. The average number of newly colonized patients per thousand patient days was 4.65 from pre- and 3.95 post-visitation policy change. There was no significant difference between the pre- and post-colonization rates when they were modeled biweekly as discussed above (ap=0.66).
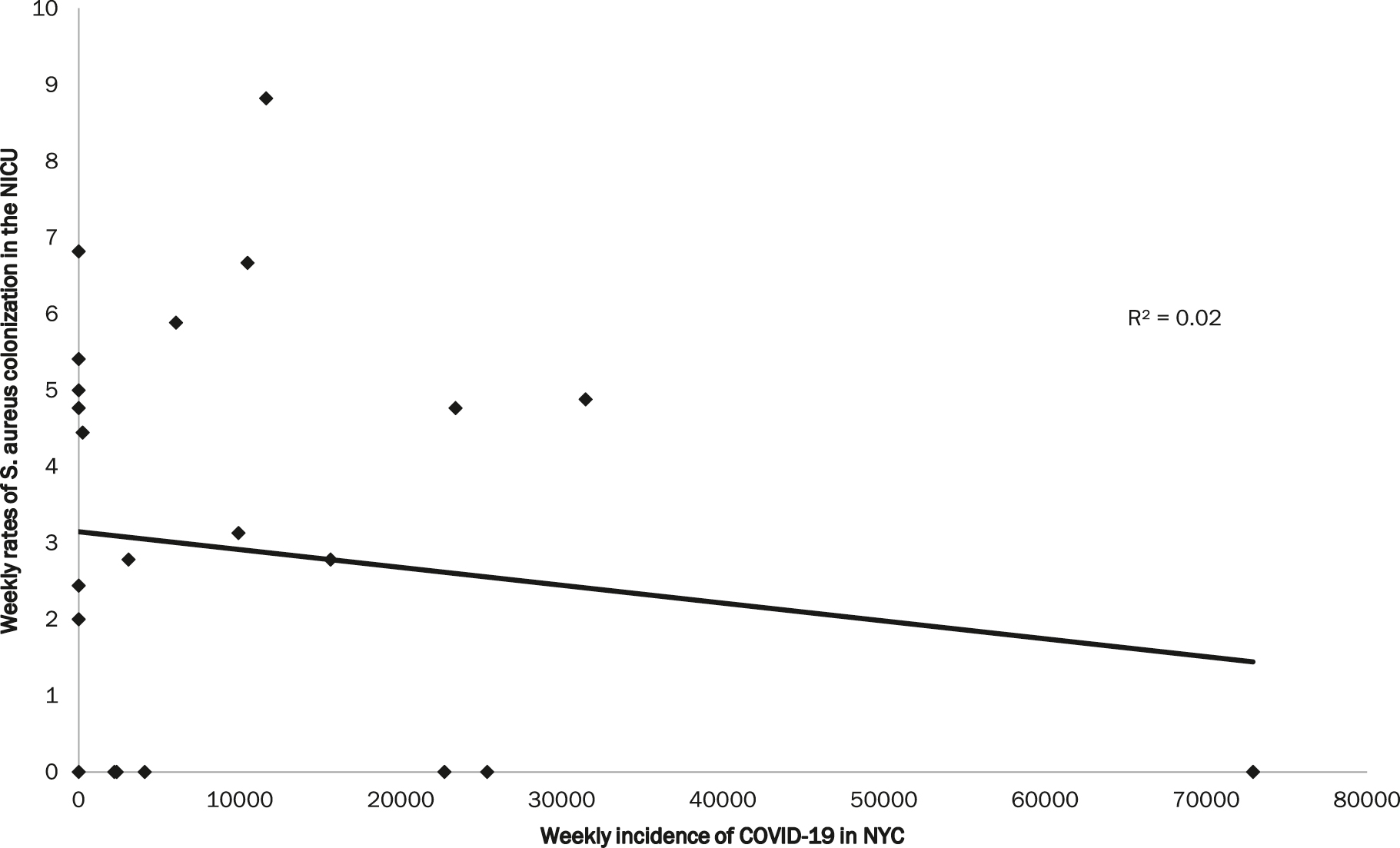
We collected data from the New York city department of health website and used linear regression to assess for a correlation between the number of new COVID-19 cases in NYC per week and weekly rates of S. aureus colonization in our NICU from January-June 2020. When we plotted weekly rates of S. Aureus colonization in the NICU vs. weekly incidence of COVID-19 cases in NYC, there was no correlation (R2=0.02).
Neonates have the potential to be exposed to S. aureus via numerous sources, including direct touch by healthcare workers and family members. In particular, early postnatal maternal-child transmission is thought to be a key mechanism of neonatal S. aureus colonization [5], though father-to-neonate transmission has also been described [6]. There is some data to suggest that decolonizing parents colonized with S. aureus may reduce risk of colonization in their newborns [7].
NYC was an epicenter of the novel coronavirus (COVID-19) global pandemic, especially during the period of March through June 2020. During the time of the COVID-19 pandemic, behaviors in our NICU changed. Our hospital required symptom screening prior to entering the facility and all visitors and staff were adhering to government-mandated social distancing and wearing face coverings. Throughout the city, people were more likely to be attending work and school from home and less likely to be gathering with individuals outside their households or taking public transportation. Additionally, our NICU implemented a strict visitation policy on March 16, 2020 that limited each patient to two visitors for the entirety of their NICU stay, only one of whom could visit the patient at a time. These two visitors had to be parents or other designated caregivers and could not be children below the age of 18 (unless they were the patient’s parent). This was a major change from our prior visitor policy, which had no restrictions limiting the number of people on each patient’s visitor list and had very few limitations on the type of visitors allowed. Any family member, friend, or sibling older than 13 years of age was permitted on the list. It also allowed two visitors to be present at the bedside at any given time. Our objective with this study was to assess for a difference between the rates of S. aureus colonization in our NICU before and after implementation of visitor restriction, which coincided with the exponential rise of COVID-19 cases in NYC.
This study was Institutional Review Board (IRB) approved and met the IRB standards of ethical conduction of research. All authors completed Collaborative Institutional Training Initiative (CITI) modules on research ethics through NYU and complied with the World Medical Association Declaration of Helsinki regarding ethical conduct of research involving human subjects and/or animals.
We utilized surveillance data that is routinely collected each week by the Department of Infection Prevention and Control to obtain a list of NICU patients colonized with S. aureus during a period between January and June 2020. We performed retrospective chart review of these infants to gather more data, including verifying completion of proper decolonization and information about previous colonization. We combined MRSA and MSSA colonized patients, as new MRSA colonization occurred only three times in the time period studied. We also only included patients who were colonized for the first time, as it was very common for patients to become recolonized even after proper decolonization. Unit census data allowed us to calculate the rate of newly S. aureus colonized NICU patients per 1,000 patient-days. All samples collected prior to March 16th were compared to the samples collected after March 16th (when visitation policy was changed). We chose to study a time period from January 2020 to June 2020, which encompasses approximately ten weeks prior to and 14 weeks following the visitor policy change and the initial rise and fall of COVID-19 in NYC.
We had a unique opportunity to assess for change in rates of S. aureus colonization after a visitor policy change in response to a global pandemic, which to our knowledge, has not been previously studied. Our results suggest that limiting visitation of NICU patients may not significantly affect colonization rates (Table 1) and that healthcare facilities may need to focus on other strategies to decrease S. aureus colonization among vulnerable patient populations. If limiting visitation has no impact on colonization rates, it is possible that primary caregivers, hospital staff, or both are the primary sources of S. aureus exposure for NICU patients.
With our strict visitor policy, only two caregivers were allowed to visit the patient, and the most commonly chosen caregivers were the parents. However, there were no restrictions on the length of time that could be spent with the patient. Visitors were required to wash their hands prior to entering the NICU, which is not a new policy, and all visitors and staff were required to wear a face covering at all times in the NICU. There were no other restrictions regarding handling the NICU patients. Some caregivers opted to wear gloves, but they were not required to do so. Additionally, skin-to-skin (kangaroo) care was still allowed and encouraged. Furthermore, our patient population encompasses several zip codes in Brooklyn where colonization and infection with S. aureus are very common [8].
Primary caregivers as a source of S. aureus exposure has been explored by other investigators [5, 6]. Maternal colonization with S. aureus was shown to increase the likelihood of neonatal colonization at birth by nearly five-fold and by two-fold later in infancy [5]. Paternal colonization with S. aureus has been less studied but still reported as a probable source [6]. Additionally, a randomized clinical trial demonstrated that decolonizing parents of NICU patients significantly reduces the likelihood of neonatal colonization with a S. aureus strain that matches their parents’ [7]. Thus, it is reasonable to conclude that limiting visitation of NICU patients may not significantly impact the rates of S. aureus colonization, so long as primary caretakers are allowed to visit and physically interact with their children.
It is also highly plausible that hospital staff members are a primary source of S. aureus colonization. There are case reports that suggest patients who are cared for by a S. aureus colonized healthcare provider are more likely to develop colonization and even infection [9, 10]. This may highlight the importance of staff cleanliness practices, including hand hygiene, in reducing S. aureus colonization and infection.
When we assessed for correlation between the incidence of COVID-19 in NYC and S. aureus colonization in our NICU, we did not find a significant association (Figure 1). This could suggest that pandemic-related changes in behavior (attending work and school from home, avoiding public transportation, wearing face coverings, social distancing, etc.) may not significantly reduce the likelihood of primary caregivers and hospital staff exposing hospitalized patients to S. aureus.
This study has limitations, most notably lack of power. We have baseline low rates of S. aureus colonization in our NICU, as evidenced by multiple weeks when there were zero newly colonized patients during our study period. Additionally, the study was designed with a single center approach and assessed a limited time period of approximately 5 months. We chose this time period to focus on the first several weeks of the pandemic when COVID-19 transmission and related behavior changes were most prominent. Additionally, this helped in minimizing impact of any confounding factors such as fluctuating rates of COVID-19 in the region and further changes to our evolving visitor and infection control policies.
Our study suggests that limiting visitation does not affect S. aureus colonization rates among NICU patients. Further directions could include assessing other hospital units, including those at other institutions. It also seems worthwhile to assess other potential strategies to reduce S. aureus colonization, including improving parent and staff hand hygiene and decolonizing primary caregivers.
-
Research funding: None declared.
-
Author contributions: Drs. Evans and Cicalese conceptualized and designed this study, wrote and submitted the IRB, performed data collection and analysis, drafted the initial manuscript, and reviewed and revised the manuscript. Drs Bailey and Verma assisted with data collection and analysis and critically reviewed and suggested edits to the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work. There are no additional acknowledgements for this study. All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Competing interests: Authors state no conflict of interest.
-
Informed consent: Not applicable.
-
Ethical approval: The local Institutional Review Board deemed the study exempt from review.
References
1. Pardos de la Gandara, M, Raygoza Garay, JA, Mwangi, M, Tobin, JN, Tsang, A, Khalida, C, et al.. Molecular types of methicillin-resistant Staphylococcus aureus and methicillin-sensitive S. aureus strains causing skin and soft tissue infections and nasal colonization, identified in community Health centers in New York city. J Clin Microbiol 2015;53:2648–58. https://doi.org/10.1128/jcm.00591-15.Search in Google Scholar PubMed PubMed Central
2. Popoola, VO, Colantuoni, E, Suwantarat, N, Pierce, R, Carroll, KC, Aucott, SW, et al.. Active surveillance cultures and decolonization to reduce Staphylococcus aureus infections in the neonatal intensive care unit. Infect Control Hosp Epidemiol 2016;37:381–7. https://doi.org/10.1017/ice.2015.316.Search in Google Scholar PubMed PubMed Central
3. Voskertchian, A, Akinboyo, IC, Colantuoni, E, Johnson, J, Milstone, AM. Association of an active surveillance and decolonization program on incidence of clinical cultures growing Staphylococcus aureus in the neonatal intensive care unit. Infect Control Hosp Epidemiol 2018;39:882–4. https://doi.org/10.1017/ice.2018.81.Search in Google Scholar PubMed PubMed Central
4. Stoll, BJ, Hansen, NI, Adams-Chapman, I, Fanaroff, AA, Hintz, SR, Vohr, B, et al.. Neurodevelopmental and growth impairment among extremely low-birth-weight infants with neonatal infection. JAMA 2004;292:2357–65. https://doi.org/10.1001/jama.292.19.2357.Search in Google Scholar PubMed
5. Jimenez-Truque, N, Tedeschi, S, Saye, EJ, McKenna, BD, Langdon, W, Wright, JP, et al.. Relationship between maternal and neonatal Staphylococcus aureus colonization. Pediatrics 2012;129:e1252–9. https://doi.org/10.1542/peds.2011-2308.Search in Google Scholar PubMed PubMed Central
6. Al-Tawfiq, JA. Father-to-infant transmission of community-acquired methicillin-resistant Staphylococcus aureus in a neonatal intensive care unit. Infect Control Hosp Epidemiol 2006;27:636–7. https://doi.org/10.1086/505097.Search in Google Scholar PubMed
7. Milstone, AM, Voskertchian, A, Koontz, DW, Khamash, DF, Ross, T, Aucott, SW, et al.. Effect of treating parents colonized with Staphylococcus aureus on transmission to neonates in the intensive care unit: a randomized clinical trial. JAMA 2020;323:319–28. https://doi.org/10.1001/jama.2019.20785.Search in Google Scholar PubMed PubMed Central
8. Lighter-Fisher, J, Phillips, MS, Stachel, A, Chopra, A, Rosman, I, Fisher, JC, et al.. Geographic cluster of community-acquired methicillin-resistant Staphylococcus aureus infections among pediatric patients from Brooklyn, New York. Open Forum Infect Dis 2016;3:278. https://doi.org/10.1093/ofid/ofw172.144.Search in Google Scholar
9. Bertin, ML, Vinski, J, Schmitt, S, Sabella, C, Danziger-Isakov, L, McHugh, M, et al.. Outbreak of methicillin-resistant Staphylococcus aureus colonization and infection in a neonatal intensive care unit epidemiologically linked to a healthcare worker with chronic otitis. Infect Control Hosp Epidemiol 2006;27:581–5. https://doi.org/10.1086/504933.Search in Google Scholar PubMed
10. Brown, NM, Reacher, M, Rice, W, Roddick, I, Reeve, L, Verlander, NQ, et al.. An outbreak of methicillin-resistant Staphylococcus aureus colonization in a neonatal intensive care unit: use of a case-control study to investigate and control it and lessons learnt. J Hosp Infect 2019;103:35–43. https://doi.org/10.1016/j.jhin.2019.05.009.Search in Google Scholar PubMed
© 2022 Walter de Gruyter GmbH, Berlin/Boston
Articles in the same Issue
- Frontmatter
- Reviews
- Placenta Accreta Spectrum Part I: anesthesia considerations based on an extended review of the literature
- Placenta Accreta Spectrum Part II: hemostatic considerations based on an extended review of the literature
- Corner of Academy
- The impact of lateral placenta on preeclampsia and small for gestational age neonates: a systematic review and meta-analysis
- Original Articles – Obstetrics
- Fetal intelligent navigation echocardiography (FINE) has superior performance compared to manual navigation of the fetal heart by non-expert sonologists
- Evaluation of fetal middle adrenal artery Doppler and fetal adrenal gland size in pregnancies with fetal growth restriction: a case-control study
- First trimester low maternal serum pregnancy associated plasma protein-A (PAPP-A) as a screening method for adverse pregnancy outcomes
- Time interval to delivery in asymptomatic twin pregnancies with a short cervix at 23–28 weeks’ gestation
- Hepatic arterial buffer response in monochorionic diamniotic pregnancies with twin-to-twin transfusion syndrome
- Healthcare of pregnant women with diabetes during the COVID-19 pandemic: a Southern Brazilian cross-sectional panel data
- Attitudes toward COVID-19 vaccination of pregnant and lactating women in Hungary
- Maternal vitamin D levels correlate with fetal weight and bone metabolism during pregnancy: a materno-neonatal analysis of bone metabolism parameters
- Removal of pregnancy categories and likelihood of prescribing: a randomized trial
- Prenatal prediction of Shone’s complex. The role of the degree of ventricular disproportion and speckle-tracking analysis
- Original Article – Fetus
- The effect of middle cerebral artery peak systolic velocity on prognosis in early and late-onset fetal growth restriction
- Original Articles – Neonates
- Assessment of salivary cortisol concentrations for procedural pain monitoring in newborns
- Impact on neonatal morbidities after a change in policy to administer antenatal corticosteroids to mothers at risk for late preterm delivery
- The Apgar score in clinical research: for what, how and by whom it is used
- Short Communication
- Visitor restriction during the COVID-19 pandemic did not impact rates of Staphylococcus aureus colonization in the NICU patients
- Letter to the Editor
- Knowledge and attitudes of pregnant women on maternal immunization against COVID-19: correspondence
Articles in the same Issue
- Frontmatter
- Reviews
- Placenta Accreta Spectrum Part I: anesthesia considerations based on an extended review of the literature
- Placenta Accreta Spectrum Part II: hemostatic considerations based on an extended review of the literature
- Corner of Academy
- The impact of lateral placenta on preeclampsia and small for gestational age neonates: a systematic review and meta-analysis
- Original Articles – Obstetrics
- Fetal intelligent navigation echocardiography (FINE) has superior performance compared to manual navigation of the fetal heart by non-expert sonologists
- Evaluation of fetal middle adrenal artery Doppler and fetal adrenal gland size in pregnancies with fetal growth restriction: a case-control study
- First trimester low maternal serum pregnancy associated plasma protein-A (PAPP-A) as a screening method for adverse pregnancy outcomes
- Time interval to delivery in asymptomatic twin pregnancies with a short cervix at 23–28 weeks’ gestation
- Hepatic arterial buffer response in monochorionic diamniotic pregnancies with twin-to-twin transfusion syndrome
- Healthcare of pregnant women with diabetes during the COVID-19 pandemic: a Southern Brazilian cross-sectional panel data
- Attitudes toward COVID-19 vaccination of pregnant and lactating women in Hungary
- Maternal vitamin D levels correlate with fetal weight and bone metabolism during pregnancy: a materno-neonatal analysis of bone metabolism parameters
- Removal of pregnancy categories and likelihood of prescribing: a randomized trial
- Prenatal prediction of Shone’s complex. The role of the degree of ventricular disproportion and speckle-tracking analysis
- Original Article – Fetus
- The effect of middle cerebral artery peak systolic velocity on prognosis in early and late-onset fetal growth restriction
- Original Articles – Neonates
- Assessment of salivary cortisol concentrations for procedural pain monitoring in newborns
- Impact on neonatal morbidities after a change in policy to administer antenatal corticosteroids to mothers at risk for late preterm delivery
- The Apgar score in clinical research: for what, how and by whom it is used
- Short Communication
- Visitor restriction during the COVID-19 pandemic did not impact rates of Staphylococcus aureus colonization in the NICU patients
- Letter to the Editor
- Knowledge and attitudes of pregnant women on maternal immunization against COVID-19: correspondence

