Abstract
Objectives
This study has three purposes. First, we explore the percentage of the population that is vaccinated and the factors that contribute to whether or not an individual takes up COVID-19 vaccination. Second, we also look at how pregnant and lactating women (PLW) take up vaccination. Third, we reveal what the public think about PLW receiving vaccines.
Methods
Questionnaire data collection was carried out online using the quota method among Hungarians aged 18–65 with Internet access. The survey was carried out between 29th November and 11th December 2021. A total of 1,000 participants completed the questionnaire.
Results
A total of 66.4% of the respondents aged 18–65 received vaccination. There were significant differences across sociodemographic variables in vaccination: men and individuals with more education, better perceived financial status, and personal experience with COVID-19 were more likely to be vaccinated. PLW were less likely to be vaccinated, partly due to their fear of vaccines’ side-effects. More than one third of the participants do not agree with PLW having COVID-19 vaccination. In general, attitudes toward vaccination of PLW differed significantly by social group. Men and individuals with tertiary education and better financial situation, who knew somebody who had died of COVID-19 infection, and who had been vaccinated were more likely to accept vaccination for both pregnant women and lactating mothers.
Conclusions
Acceptance of receiving COVID-19 vaccination depends on social status; thus, targeted campaigns are required. In addition, PLW are afraid of vaccines’ side effects, so they should be provided information, just as there is a need to increase public information on this topic.
Introduction
In 2019, The World Health Organization (WHO) listed vaccine hesitancy among the top 10 threats to world health [1]. Vaccine hesitancy is defined as delay in acceptance or refusal of vaccination despite the availability of vaccination services [2].
COVID-19 vaccination started in Hungary in December 2020, at which time vaccines were only available to those at the highest risk. Since spring 2021, they have become widely available, and by 29 November 2021, the vaccination rate at least with one dose for Hungarians aged over 18 years was 63.6% [3], which was comparable with high-income countries, where rates of vaccination with at least one dose ranged from 60 to 80% in mid-October 2021 [4]. Nevertheless, according to the WHO, the COVID-19 pandemic can only be stopped globally when the vaccination rate exceeds 70% [5]; thus, Hungary still needs to increase its rate of vaccination.
Vaccine hesitancy is not evenly distributed among different social groups. Many studies have highlighted that women are less willing to have COVID-19 vaccines than men [6], [7], [8], [9], [10]. There are also factors such as income level, age and educational level that are associated with vaccine hesitancy [8, 10], [11], [12], [13]. One of the possible explanations for gender differences in COVID-19 vaccination is that women have a lower mortality rate than men following COVID-19 infection [14], thereby leading women to be more likely than men to consider vaccination to be less important [15]. A further explanation may be that women are afraid of the possible side-effects of vaccines on themselves and the possible negative effects on the fetus during pregnancy and the child or when breastfeeding [16], [17], [18], [19].
Vaccination was not initially recommended for pregnant and lactating women, and the WHO recommended that pregnancy should be avoided for 2–3 months after vaccination [20]. Now, however, a large body of evidence suggests that COVID-19 vaccination is effective and safe during pregnancy and breastfeeding [21, 22]. Most current recommendations support COVID-19 vaccination at any stage of pregnancy [20, 23]. In some countries, including Hungary, vaccination is offered at between 12 and 36 weeks’ gestation [20, 24].
We have not been able to identify on Google Scholar, PubMed, and Scopus between 2020 and 2022 studies that have focused on public opinion toward pregnant and lactating women being vaccinated against COVID-19. Since pregnant and lactating women may be influenced by opinions within their social environment, such as those of relatives, friends, and colleagues, regarding their decisions about COVID-19 vaccination, it is therefore important to ascertain the opinions of society as a whole. The aim of the study is to explore both the general attitudes and sociodemographic factors influencing the vaccination of pregnant and lactating women in Hungary. This topic has great importance because pregnant and postpartum women are at high risk for coronavirus and complications from it [25, 26].
Materials and methods
Study design and ethical approval
A representative sample was gathered through a nationwide, cross-sectional online survey on COVID-19 vaccine attitudes from 29 November to 11 December 2021. The sample included 1,000 participants aged 18 to 65 with internet access using a non-probabilistic quota method. The quota was determined on the basis of the population data of the Hungarian Statistical Office according to the dimensions of age, gender, type of settlement, and education. The participants had to fill out the questionnaire on a self-completion basis.
The project was granted ethical approval by the Ethics Committee of the Medical Research Council before the start of the research (ETT-TUKEB case number: IV/8531-1/2021/EKU).
Measures
Participants were asked about their attitudes toward and experiences with COVID-19, such as previous COVID-19 infection and knowing somebody who had died from COVID-19. They were also asked about their sociodemographic background, including gender, age, educational level, perceived financial status, intention to have children, and if they were breastfeeding a child. There were three outcome variables. The first was if the respondent was vaccinated (vaccination was defined as the respondent having at least two doses of a multiple-dose or one dose of a single-dose vaccine). For the other outcome variables, participants had to indicate their opinion toward vaccination of pregnant women and of lactating women on a five-point scale (1=strongly disagree, 2=disagree, 3=neither agree nor disagree, 4=agree, 5=strongly agree).
Data analysis
For the descriptive statistics, frequency and percentage were calculated. Chi-square statistics, two-sample t-test, and multivariate logistic regression were used to investigate factors associated with the respondents’ own vaccination and their attitudes toward the vaccination of pregnant and lactating women. A p-value less than 0.05 was considered significant. All the statistical analyses were performed using the Stata 16 software program.
Results
Sample characteristics
Table 1 details the sociodemographic characteristics of the participants. Regarding age, gender, type of settlement, and education, the sample represented the Hungarian population aged between 18 and 65 years. The mean ages of male and female participants were 45.4 and 39.6 years, respectively. The gender distribution was 53% female and 47% male. Regarding their perceived financial status, 58.6% of the participants stated that they could live comfortably or make ends meet, while 38.5% had some difficulty making ends meet.
Sociodemographic characteristics of the sample.
| Variable | Values | n | Percentage |
|---|---|---|---|
| Gender | Men | 470 | 47 |
| Women | 530 | 53 | |
| Age group | 18–29 | 203 | 20.3 |
| 30–39 | 243 | 24.3 | |
| 40–49 | 226 | 22.6 | |
| 50–65 | 328 | 32.8 | |
| Highest level of education | Primary | 252 | 25.2 |
| Secondary | 441 | 44.1 | |
| Tertiary | 307 | 30.7 | |
| Perceived financial status | Comfortable living on current income | 127 | 12.7 |
| Making ends meet | 459 | 45.9 | |
| Difficulty living on current income | 288 | 28.8 | |
| Very difficult living on current income | 97 | 9.7 | |
| No answer | 29 | 2.9 | |
| Know somebody who has died of COVID-19 infection? | Yes | 409 | 40.9 |
| No | 591 | 59.1 | |
| Have you been infected with COVID-19? | No | 727 | 72.7 |
| Yes, but I only had mild symptoms | 110 | 11 | |
| Yes, I had moderate symptoms | 87 | 8.7 | |
| Yes, I had severe symptoms | 76 | 7.6 | |
| Intention to have children | No | 675 | 67.5 |
| Yes, but later | 167 | 16.7 | |
| Yes, within 2 years | 136 | 13.6 | |
| Pregnant | 22 | 2.2 | |
| Breastfeeding | Yes | 50 | 5 |
| No | 950 | 9.5 |
As for personal experience with COVID-19, 40.9% of respondents had a relative or acquaintance who had died of COVID-19 infection and 27.3% reported that they had already had COVID-19 infection themselves. Of those who had previous COVID-19 infection, 40.3% reported that they suffered only mild symptoms during their infection, 31.9% had moderate symptoms, and 27.8% had serious symptoms. Regarding fertility plans, 13.6% of the respondents planned to have (further) children within 2 years, 2.2% were pregnant, and 5% would breastfeed their children during the survey period.
COVID-19 vaccine uptake
Table 2 shows that 66.4% had full protection against COVID-19 (at least two shots of a multiple-dose vaccine or one dose of a single-dose vaccine); 74.26% of men and 59.43% of women were vaccinated (χ2=38.1, p<0.0001).
COVID-19 vaccination rate by gender.
| All respondents | Men | Women | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Yes, all three doses | 320 | 32 | 181 | 38.51 | 139 | 26.23 |
| Yes, the single-dose vaccine | 13 | 1.3 | 8 | 1.7 | 5 | 0.94 |
| Yes, the second dose, and I am planning a third one | 182 | 18.2 | 100 | 21.28 | 82 | 15.47 |
| Yes, the second dose, but I am not planning a third one | 149 | 14.9 | 60 | 12.77 | 89 | 16.79 |
| Yes, the first dose, and I am planning another | 20 | 2 | 8 | 1.7 | 12 | 2.26 |
| Yes, the first dose, but I am not planning another | 9 | 0.9 | 3 | 0.64 | 6 | 1.13 |
| Not yet, but I plan to have them all | 18 | 1.8 | 5 | 1.061 | 13 | 2.45 |
| Not yet, but I plan to, but not all of them | 17 | 1.7 | 6 | 1.283 | 11 | 2.081 |
| No, and I do not plan to have any | 226 | 22.6 | 85 | 18.091 | 141 | 26.6 |
| I Do not want to answer | 46 | 4.6 | 14 | 2.97 | 32 | 6.04 |
| Total | 1000 | 100 | 470 | 100 | 530 | 100 |
-
The bold values are the sums of the columns (n= number of respondents).
Chi-square statics revealed that vaccine hesitancy significantly decreased by higher education (χ2=23.8, p<0.0001), perceived better financial status (χ2=17.21, p<0.01), knowing somebody who had died of COVID-19 infection (χ2=25.81, p<0.0001), and not planning to have (further) children (χ2=11.32, p<0.05). Meanwhile, age and own experience of COVID-19 infection did not have significant effects (χ2=14.88, p=0.0131; χ2=19.33, p=0.017; χ2=8.36, p=0.074).
Vaccination hesitancy among pregnant and lactating women
Pregnant women were less likely to be vaccinated (50%) than their non-pregnant counterparts (62.34%; χ2=3.5, p=0.061) in the fertile age groups; however, this result was not significant. The difference was even greater between lactating mothers (39.58%) and non-lactating women (65.6%; χ2=14.88, p<0.0001) in the 18–45 years age group (Figure 1).

Vaccination rate among pregnant and lactating women.
Public’s beliefs about vaccination of pregnant women and lactating mothers
In terms of vaccinating pregnant and lactating women, the public’s beliefs were very similar. More than one third of the respondents disagreed with the vaccination of pregnant women (33.7%) and lactating mothers (34.1%), while 28.6 and 25.74%, respectively, could not decide whether pregnant women and lactating mothers should be vaccinated. A little over a third agreed with the vaccination of pregnant women (37.7%) and lactating mothers (37.3%). There were no significant differences in attitudes towards the vaccination of pregnant and lactating women against COVID-19 (t=0.7686, p=0.615). Men were more likely to agree with the vaccination of both pregnant women and lactating mothers (χ2=41.66, p<0.0001) than women (χ2=38.12, p<0.0001).
Predictors of attitudes toward vaccination of pregnant women and lactating mothers
The multiple regression models concerning the vaccination of pregnant women and lactating mothers were significant (pregnant women: F=34.54, p=0.000; lactating mothers: F=33.31, p=0.000). The results showed that men (B=0.103, p<0.0001; B=0.107, p<0.0001), people with higher education (B=−0.104, p<0.0001; B=0.105, p<0.0001) and better financial situation (B=0.081, p=0.046; B=−0.105, p=0.010), those knowing somebody who had died of COVID-19 infection (B=0.098, p<0.0001; B=0.08, p=0.003), and people who were vaccinated (B=0.519, p<0.0001; B=0.523, p<0.0001) were more likely to accept vaccination of either pregnant women or lactating mothers. However, age and intention to have (further) children did not have significant effects on opinions toward vaccination of pregnant and lactating women (B=0.098, p<0.0001; B=0.08, p=0.003) (Table 3). Lactating mothers were more likely to reject vaccination of lactating mothers (B=0.107, p<0.0001), but breastfeeding did not have a negative effect on their opinion toward the vaccination of pregnant women (B=1.28, p=0.199) (Table 3).
Public’s beliefs toward vaccination of pregnant and lactating women against COVID-19.
| Items | Attitudes toward vaccination of pregnant women | Attitudes toward vaccination of lactating mothers | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Unstandardized coefficients | Standardized | t-Test | p-Value | Unstandardized coefficients | Standardized | t-Test | p-Value | |||
| Std. error | Beta | Std. error | Beta | |||||||
| Constant | 0.146 | 2.144 | 14.61 | 0.000 | 0.146 | 2.088 | 14.25 | 0.000 | ||
| Gender: Men | 0.071 | 0.265 | 0.103 | 3.70 | 0.000 | 0.071 | 0.279 | 0.107 | 3.90 | 0.000 |
| Age: 18–29 (ref: 40–49) | 0.119 | −0.162 | −0.049 | −1.36 | 0.175 | 0.119 | −0.172 | −0.052 | −1.44 | 0.150 |
| Age: 30–39 | 0.103 | −0.023 | −0.007 | −0.23 | 0.819 | 0.102 | −0.032 | −0.011 | −0.31 | 0.753 |
| Age: 50–65 | 0.091 | 0.088 | 0.032 | 0.96 | 0.337 | 0.091 | 0.085 | 0.031 | 0.94 | 0.349 |
| Education: Secondary (ref: low) | 0.087 | 0.075 | 0.029 | 0.086 | 0.388 | 0.087 | 0.149 | 0.057 | 1.71 | 0.087 |
| Education: Tertiary | 0.095 | 0.289 | 0.104 | 3.03 | 0.003 | 0.095 | 0.416 | 0.149 | 4.36 | 0.000 |
| Financial status: Comfortable (ref: make ends meet) | 0.105 | −0.210 | −0.081 | −1.99 | 0.046 | 0.105 | −0.272 | −0.105 | −2.58 | 0.010 |
| Financial status: Difficult | 0.114 | −0.251 | −0.087 | −2.20 | 0.028 | 0.113 | −0.255 | −0.089 | −2.24 | 0.025 |
| Financial status: Very difficult | 0.147 | −0.404 | −0.091 | −2.75 | 0.006 | 0.146 | −0.501 | −0.113 | −3.42 | 0.001 |
| Financial status: No answer | 0.379 | −0.073 | −0.005 | −0.19 | 0.846 | 0.289 | −0.017 | −0.012 | −0.45 | 0.650 |
| Knowing someone who had died of COVID-19 | 0.069 | 0.257 | 0.098 | 3.70 | 0.000 | 0.069 | 0.210 | 0.08 | 3.03 | 0.003 |
| Intention to have child later (ref: no intention) | 0.107 | 0.088 | 0.026 | 0.083 | 0.407 | 0.107 | 0.048 | 0.013 | 0.45 | 0.650 |
| Intention to have child within 2 years | 0.107 | −0.170 | −0.045 | −1.59 | 0.112 | 0.107 | −0.107 | −0.028 | −1 | 0.317 |
| Intention to have child: Pregnant | 0.046 | 0.46 | 0.005 | 0.19 | 0.846 | 0.236 | 0.043 | 0.005 | 0.18 | 0.853 |
| Breastfeeding | 0.160 | 0.206 | 0.035 | 1.28 | 0.199 | 0.160 | 0.626 | 0.107 | 3.91 | 0.000 |
| Vaccinated | 2.144 | 1.486 | 0.519 | 19.06 | 0.000 | 0.078 | 1.105 | 0.523 | 0.000 | 0.000 |
Reasons for willingness to take vaccines
We found significant difference by gender: 19.25% of women vs. 8.09% of men stated that they feared the consequences of vaccination (χ2=5.79, p<0.0001), and 20.75% of women vs. 15.96% of men stated that they did not trust vaccines (χ2=3.82, p=0.005).
There were no significant differences between pregnant and non-pregnant women (χ2=1.553, p=0.213) and lactating mothers and non-lactating women (χ2=0.603, p=0.427) in the 18–45 age group in terms of the reasons why they were not vaccinated against COVID-19. However, more than 45% of pregnant women indicated that they had not vaccinated themselves due to fear of the side-effects of the vaccination, compared with 21.1% of those women who did not intend to have children. Further, 32.7% of lactating women indicated that they did not trust vaccines, compared with 20.4% of those women who did not intend to have children (Figure 2).
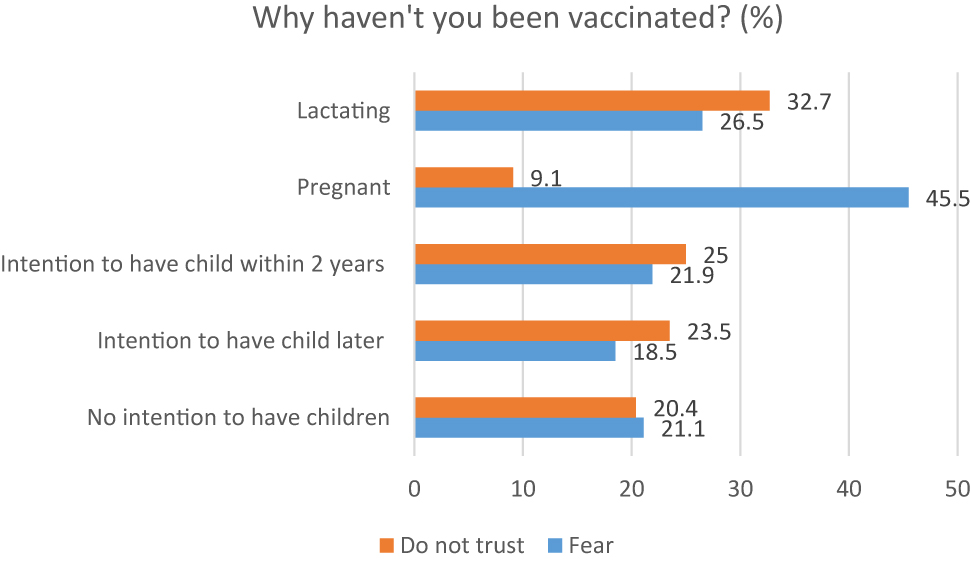
Reasons for vaccine hesitancy among different groups of women aged 18–45.
Discussion
This study examined hesitancy toward COVID-19 vaccination among different sociodemographic groups and attitudes toward the vaccination of pregnant and lactating women. We found that approximately two thirds of the participants had been vaccinated by receiving at least two doses of a multiple-dose COVID-19 vaccine or one dose of a single-dose vaccine. A further 2% in our sample had received only one shot of a multiple-dose vaccine, but they planned to have more. We did not consider them to be vaccinated, since the third dose had become widely available by end of November 2021 in Hungary, and our consideration was their behavior and not their intention.
Similar to previous studies [6], [7], [8], [9], we found women to be less likely to be vaccinated than men (59.43 vs. 74.26%). One of the potential reasons for this seems to be they were more afraid about the side-effects of vaccination and less likely to trust in vaccines than men. Besides gender, other factors had a significant effect on vaccine hesitancy, such as higher education and higher income, which were positively associated with receiving vaccination, which is in line with the results of other studies [27], [28], [29]. Additionally, we examined personal experiences of COVID-19, such as personally knowing someone who had died of COVID-19 and the respondents’ own previous infections. Our findings showed that personally knowing someone who had died of COVID-19 was likely to decrease vaccine hesitancy, which is consistent with Piltch-Loeb et al.’s [29] findings in the USA; however, own COVID-19 infection experience did not have a significant effect, which was different from their findings [29]. This may be due to the fact that Piltch-Loeb et al. [29] measured own COVID-19 experience with a dummy variable, had or not had, whereas we measured it across four categories. It seems that different experiences of COVID-19 infections can lead to differences in vaccine behavior. Since the number of those infected with COVID-19 will increase, it is important to examine this issue in more detail in the future.
Regarding pregnant and lactating women, we found that they were less likely to be vaccinated than their non-pregnant or non-lactating counterparts in the 18–45 years age group. It seems that they were more likely to fear unfavorable side-effects from vaccination; however, this result was not significant, which might be due to the low number of cases of pregnant and lactating women in the sample. This result is consistent with findings from the USA [19] and Turkey [30] but contradicts the results from Poland [31], where pregnant and lactating women were more likely to be vaccinated than their counterparts in the same age group. This may be due to Poles’ stronger trust in the health system overall, compared with that specifically of non-pregnant and not lactating women. The results partly coincide with the results from Czechia, where lactating women were resistant to being vaccinated, but pregnant women were not; however, the respondents were asked about their intention to be vaccinated, and not about their actual vaccination.
Our findings point out that general attitudes are not supportive toward the vaccination of pregnant and lactating women, since only 37.7 and 37.3% of the respondents agreed with vaccinating pregnant women and lactating mothers, respectively. We found that the same factors influenced attitudes toward the vaccination of pregnant and lactating women as those influencing own vaccination: men, higher education and better financial situation, and knowing somebody who had died of COVID-19 infection were associated with supportive attitudes. Additionally, those who were vaccinated were more likely to also support the vaccination of both pregnant women and lactating mothers.
Strengths and limitations
This is the first study in Hungary that discusses the attitudes of pregnant and lactating women toward vaccination against COVID-19. Likewise, previous research has not so far examined the public’s beliefs toward the vaccination of pregnant and lactating women. This may be an important factor, since pregnant and lactating women may adjust their vaccination behavior according to the dominant social norms and not just based on the suggestions of medical doctors.
One of the limitations of the research is that very few pregnant women (22) and lactating mothers (50) participated in a sample that was representative of the population aged 18–65 in Hungary. The other limitation is that the survey did not ask about the type of vaccines so we cannot measure the different attitudes toward different types of vaccines, although several types of vaccines are available in Hungary. Further studies should be conducted with larger number of pregnant and lactating women and asking about the type of vaccines the respondents took.
Conclusions
Women have a lower vaccination rate than men. Moreover, we found that pregnant and lactating women have a significantly lower vaccination rate than non-pregnant, non-lactating women of fertile age. Men are more likely to support the vaccination of pregnant and lactating women than women. A possible significant reason for hesitancy toward COVID-19 vaccination among pregnant and lactating women seems to be the fear of side-effects on themselves or harmful effects on their fetuses or newborns. Awareness campaigns about COVID-19 vaccination are needed, particularly among those with a lower level of education, people in poor financial circumstances, and women. Furthermore, these campaigns should also emphasize that COVID-19 vaccination is not harmful either to pregnant and lactating women or to their fetuses and newborns.
Acknowledgments
The research conducted by the MTA TK Lendület “Momentum” Reproductive Sociology Research Group.
-
Research funding: None declared.
-
Author contributions: All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Competing interests: Authors state no conflict of interest.
-
Informed consent: Informed consent was obtained from all individuals included in this study.
-
Ethical approval: The project was granted ethical approval by the Ethics Committee of the Medical Research Council before the start of the research (ETT-TUKEB case number: IV/8531-1/2021/EKU).
References
1. WHO. Ten threats to global health in 2019; 2019. Available from: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019.Search in Google Scholar
2. MacDonald, NE, SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: definition, scope and determinants. Vaccine 2015;33:4161–4. https://doi.org/10.1016/j.vaccine.2015.04.036.Search in Google Scholar PubMed
3. Medve, F. Share of Hungarians vaccinated against COVID-19 2020–2022; 2022. Available from: https://www.statista.com/statistics/1197351/hungary-share-of-population-vaccinated-against-covid-19/.Search in Google Scholar
4. Ritchie, H, Mathieu, E, Rhodés-Guirao, L, Appel, C, Giattino, C, Ortiz-Ospina, E, et al.. Coronavirus pandemic (COVID-19); 2020. Available from https://ourworldindata.org/coronavirus.Search in Google Scholar
5. WHO. Strategy to achieve global Covid-19 vaccination by mid-2022; 2021. Available from: https://cdn.who.int/media/docs/default-source/immunization/covid-19/strategy-to-achieve-global-covid-19-vaccination-by-mid-2022.pdf.Search in Google Scholar
6. Zintel, S, Flock, C, Arbogast, AL, Forster, A, von Wagner, C, Sieverding, M. Gender differences in the intention to get vaccinated against COVID-19: a systematic review and meta-analysis. J Public Health 2022. [Epub ahead of print]. https://doi.org/10.1007/s10389-021-01677-w.Search in Google Scholar PubMed PubMed Central
7. Dombrádi, V, Joó, T, Palla, G, Pollner, P, Belicza, É. Comparison of hesitancy between COVID-19 and seasonal influenza vaccinations within the general Hungarian population: a cross-sectional study. BMC Publ Health 2021;21:2317. https://doi.org/10.1186/s12889-021-12386-0.Search in Google Scholar PubMed PubMed Central
8. Schwarzinger, M, Watson, V, Arwidson, P, Alla, F, Luchini, S. COVID-19 vaccine hesitancy in a representative working-age population in France: a survey experiment based on vaccine characteristics. Lancet Public Health 2021;6:210–21. https://doi.org/10.1016/s2468-2667(21)00012-8.Search in Google Scholar
9. Ogilvie, GS, Gordon, S, Smith, LW, Albert, A, Racey, CS, Booth, A, et al.. Intention to receive a COVID-19 vaccine: results from a population-based survey in Canada. BMC Publ Health 2021;21:1017–31. https://doi.org/10.1186/s12889-021-11098-9.Search in Google Scholar PubMed PubMed Central
10. Brys, Z, Albert, F, Pénzes, E. COVID–19 vaccination refusal in the active Hungarian adult population in December, 2021. Orv Hetil 2021;163:1135–43.10.1556/650.2022.32531Search in Google Scholar PubMed
11. Abuhammad, S. Attitude of pregnant and lactating women toward COVID-19 vaccination in Jordan: a cross-sectional study. J Perinat Med 2022;50:896–903. https://doi.org/10.1515/jpm-2022-0026.Search in Google Scholar PubMed
12. Riad, A, Jouzova, A, Üstün, B, Lagová, E, Hruban, L, Janku, P, et al.. COVID-19 vaccine acceptance of pregnant and lactating women (PLW) in Czechia: an analytical cross-sectional study. Int J Environ Res Publ Health 2021;18:13373–97. https://doi.org/10.3390/ijerph182413373.Search in Google Scholar PubMed PubMed Central
13. Viswanath, K, Bekalu, M, Dhawan, D, Pinnamaneni, R, Lang, J, McLoud, R. Individual and social determinants of COVID-19 vaccine uptake. BMC Publ Health 2021;21:818–28. https://doi.org/10.1186/s12889-021-10862-1.Search in Google Scholar PubMed PubMed Central
14. Tazerji, SS, Shahabinejad, F, Tokasi, M, Rad, AM, Khan, MS, Safdar, M, et al.. Global data analysis and risk factors associated with morbidity and mortality of COVID-19. Gene Rep 2022;26:101505. https://doi.org/10.1016/j.genrep.2022.101505.Search in Google Scholar PubMed PubMed Central
15. Petravić, L, Arh, R, Gabrovec, T, Jazbec, L, Rupčić, N, Starešinič, N, et al.. Factors affecting attitudes towards COVID-19 vaccination: an online survey in Slovenia. Vaccines 2021;9:247–62. https://doi.org/10.3390/vaccines9030247.Search in Google Scholar PubMed PubMed Central
16. Hsu, AL, Johnson, T, Phillips, L, Nelson, TB. Sources of vaccine hesitancy: pregnancy, infertility, minority concerns, and general skepticism. Open Forum Infect Dis 2021;9:ofab433. https://doi.org/10.1093/ofid/ofab433.Search in Google Scholar PubMed PubMed Central
17. Diaz, P, Reddy, P, Ramasahayam, R, Kuchakulla, M, Ramasamy, R. COVID-19 vaccine hesitancy linked to increased internet search queries for side effects on fertility potential in the initial rollout phase following Emergency Use Authorization. Andrologia 2021;53:e14156. https://doi.org/10.1111/and.14156.Search in Google Scholar PubMed PubMed Central
18. Bíró-Nagy, A, Szászi, ÁJ. The roots of COVID-19 vaccine hesitancy: evidence from Hungary. J Behav Med 2022;14:1–16. https://doi.org/10.1007/s10865-022-00314-5.Search in Google Scholar PubMed PubMed Central
19. Sutton, D, D’Alton, M, Zhang, Y, Kahe, K, Cepin, A, Goffman, D, et al.. COVID-19 vaccine acceptance among pregnant, breast-feeding, and nonpregnant reproductive-aged women. Am J Obstet Gynecol 2021;3:100403. https://doi.org/10.1016/j.ajogmf.2021.100403.Search in Google Scholar PubMed PubMed Central
20. Brillo, E, Tosto, V, Gerli, S, Buonomo, E. COVID-19 vaccination in pregnancy and postpartum. J Matern Fetal Neonatal Med 2021;16:1–20. https://doi.org/10.1080/14767058.2021.1920916.Search in Google Scholar PubMed
21. Gray, KJ, Bordt, EA, Atyeo, C, Deriso, E, Akinwunmi, B, Young, N, et al.. Coronavirus disease 2019 vaccine response in pregnant and lactating women: a cohort study. Am J Obstet Gynecol 2021;225:303.e1–17. https://doi.org/10.1016/j.ajog.2021.03.023.Search in Google Scholar PubMed PubMed Central
22. Razzaghi, H, Yankey, D, Vashist, K, Lu, PJ, Kriss, JL, Nguyen, KH, et al.. COVID-19 vaccination coverage and intent among women aged 18-49 years by pregnancy status, United States. Vaccine 2022 40:4554–63. https://doi.org/10.1016/j.vaccine.2022.06.029.Search in Google Scholar PubMed PubMed Central
23. WHO. Frequently asked questions: COVID-19 vaccines and breastfeeding based on WHO interim recommendations; 2021. Available from: https://www.who.int/publications/i/item/WHO-2019-nCoV-FAQ-Breast_feeding-Vaccines-2021.1.Search in Google Scholar
24. COVID-19 Maternal Immunization Tracker; 2022. Available from: https://www.comitglobal.org/vaccines/matrix/pregnancy.Search in Google Scholar
25. Phoswa, WN, Khaliq, OP. Is pregnancy a risk factor of COVID-19? Eur J Obstet Gynecol Reprod Biol 2020;252:605–9. https://doi.org/10.1016/j.ejogrb.2020.06.058.Search in Google Scholar PubMed PubMed Central
26. Pietrasanta, C, Ronchi, A, Crippa, BL, Artieri, G, Ballerini, C, Crimi, R, et al.. Coronavirus disease 2019 vaccination during pregnancy and breastfeeding: a review of evidence and current recommendations in Europe, North America, and Australasia. Front Pediatr 2022;10:883953. https://doi.org/10.3389/fped.2022.883953.Search in Google Scholar PubMed PubMed Central
27. Skjefte, M, Ngirbabul, M, Akeju, O, Escudero, D, Hernandez-Diaz, S, Wyszynski, DF, et al.. COVID-19 vaccine acceptance among pregnant women and mothers of young children: results of a survey in 16 countries. Eur J Epidemiol 2021;36:197–211. https://doi.org/10.1007/s10654-021-00728-6.Search in Google Scholar PubMed PubMed Central
28. Mappa, I, Luviso, M, Distefano, FA, Carbone, L, Maruotti, GM, Rizzo, G. Women perception of SARS-CoV-2 vaccination during pregnancy and subsequent maternal anxiety: a prospective observational study. J Matern Fetal Neonatal Med 2021; 11:1–4. https://doi.org/10.1080/14767058.2021.1910672.Search in Google Scholar PubMed
29. Piltch-Loeb, R, Silver, DR, Kim, Y, Norris, H, McNeill, E, Abramson, DM. Determinants of the COVID-19 vaccine hesitancy spectrum. PLoS One 2022;17:e0267734. https://doi.org/10.1371/journal.pone.0267734.Search in Google Scholar PubMed PubMed Central
30. Ayhan, GS, Oluklu, D, Atalay, A, Beser, DM, Tanacan, A, Tekin, OM, et al.. COVID-19 vaccine acceptance in pregnant women. Int J Gynaecol Obstet 2021;154:291–6. https://doi.org/10.1002/ijgo.13713.Search in Google Scholar PubMed PubMed Central
31. Kuciel, N, Mazurek, J, Hap, K, Marciniak, D, Biernat, K, Sutkowska, E. COVID-19 Vaccine acceptance in pregnant and lactating women and mothers of young children in Poland. Int J Womens Health 2022;14:415–24. https://doi.org/10.2147/ijwh.s348652.Search in Google Scholar
© 2022 the author(s), published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Frontmatter
- Reviews
- Placenta Accreta Spectrum Part I: anesthesia considerations based on an extended review of the literature
- Placenta Accreta Spectrum Part II: hemostatic considerations based on an extended review of the literature
- Corner of Academy
- The impact of lateral placenta on preeclampsia and small for gestational age neonates: a systematic review and meta-analysis
- Original Articles – Obstetrics
- Fetal intelligent navigation echocardiography (FINE) has superior performance compared to manual navigation of the fetal heart by non-expert sonologists
- Evaluation of fetal middle adrenal artery Doppler and fetal adrenal gland size in pregnancies with fetal growth restriction: a case-control study
- First trimester low maternal serum pregnancy associated plasma protein-A (PAPP-A) as a screening method for adverse pregnancy outcomes
- Time interval to delivery in asymptomatic twin pregnancies with a short cervix at 23–28 weeks’ gestation
- Hepatic arterial buffer response in monochorionic diamniotic pregnancies with twin-to-twin transfusion syndrome
- Healthcare of pregnant women with diabetes during the COVID-19 pandemic: a Southern Brazilian cross-sectional panel data
- Attitudes toward COVID-19 vaccination of pregnant and lactating women in Hungary
- Maternal vitamin D levels correlate with fetal weight and bone metabolism during pregnancy: a materno-neonatal analysis of bone metabolism parameters
- Removal of pregnancy categories and likelihood of prescribing: a randomized trial
- Prenatal prediction of Shone’s complex. The role of the degree of ventricular disproportion and speckle-tracking analysis
- Original Article – Fetus
- The effect of middle cerebral artery peak systolic velocity on prognosis in early and late-onset fetal growth restriction
- Original Articles – Neonates
- Assessment of salivary cortisol concentrations for procedural pain monitoring in newborns
- Impact on neonatal morbidities after a change in policy to administer antenatal corticosteroids to mothers at risk for late preterm delivery
- The Apgar score in clinical research: for what, how and by whom it is used
- Short Communication
- Visitor restriction during the COVID-19 pandemic did not impact rates of Staphylococcus aureus colonization in the NICU patients
- Letter to the Editor
- Knowledge and attitudes of pregnant women on maternal immunization against COVID-19: correspondence
Articles in the same Issue
- Frontmatter
- Reviews
- Placenta Accreta Spectrum Part I: anesthesia considerations based on an extended review of the literature
- Placenta Accreta Spectrum Part II: hemostatic considerations based on an extended review of the literature
- Corner of Academy
- The impact of lateral placenta on preeclampsia and small for gestational age neonates: a systematic review and meta-analysis
- Original Articles – Obstetrics
- Fetal intelligent navigation echocardiography (FINE) has superior performance compared to manual navigation of the fetal heart by non-expert sonologists
- Evaluation of fetal middle adrenal artery Doppler and fetal adrenal gland size in pregnancies with fetal growth restriction: a case-control study
- First trimester low maternal serum pregnancy associated plasma protein-A (PAPP-A) as a screening method for adverse pregnancy outcomes
- Time interval to delivery in asymptomatic twin pregnancies with a short cervix at 23–28 weeks’ gestation
- Hepatic arterial buffer response in monochorionic diamniotic pregnancies with twin-to-twin transfusion syndrome
- Healthcare of pregnant women with diabetes during the COVID-19 pandemic: a Southern Brazilian cross-sectional panel data
- Attitudes toward COVID-19 vaccination of pregnant and lactating women in Hungary
- Maternal vitamin D levels correlate with fetal weight and bone metabolism during pregnancy: a materno-neonatal analysis of bone metabolism parameters
- Removal of pregnancy categories and likelihood of prescribing: a randomized trial
- Prenatal prediction of Shone’s complex. The role of the degree of ventricular disproportion and speckle-tracking analysis
- Original Article – Fetus
- The effect of middle cerebral artery peak systolic velocity on prognosis in early and late-onset fetal growth restriction
- Original Articles – Neonates
- Assessment of salivary cortisol concentrations for procedural pain monitoring in newborns
- Impact on neonatal morbidities after a change in policy to administer antenatal corticosteroids to mothers at risk for late preterm delivery
- The Apgar score in clinical research: for what, how and by whom it is used
- Short Communication
- Visitor restriction during the COVID-19 pandemic did not impact rates of Staphylococcus aureus colonization in the NICU patients
- Letter to the Editor
- Knowledge and attitudes of pregnant women on maternal immunization against COVID-19: correspondence

