Abstract
Context
Osteopathic listening tests are diagnostic tools utilized in manual therapies, but their impact on physiological markers of the autonomic nervous system (ANS), such as heart rate (HR) and heart rate variability (HRV), remains unclear. This study examines these effects to clarify the role of listening tests within osteopathic practice.
Objectives
This study aims to evaluate the influence of osteopathic listening tests on HR and HRV markers, including the root mean square of successive differences (rMSSD) and the low-frequency/high-frequency (LF/HF) ratio, in healthy participants, and to contextualize the findings within existing osteopathic research on ANS modulation.
Methods
51 osteopathic students were randomized into three groups: (1) an osteopathic test group (OTG) receiving listening tests; (2) a light pressure group (LPG) experiencing non-therapeutic light pressure; and (3) a control group (CG) receiving no intervention. Measurements of HR, rMSSD, and LF/HF ratio were collected during the first and last 30 s of the protocol utilizing validated software. Data from 48 participants were analyzed after excluding artifacts.
Results
No significant changes in HR, rMSSD, or LF/HF ratio were observed in any group during the protocol. For OTG, the HR changed minimally (69.17 ± 9.58 beats per minute [bpm] to 69.10 ± 10.24 bpm; p=0.884), while the rMSSD and LF/HF ratio also showed no significant alterations (p=0.064 and p=0.106, respectively). Similar null findings were observed in the LPG and CG, suggesting that neither osteopathic tests nor light pressure induced measurable effects on the ANS markers chosen.
Conclusions
This study found no evidence that osteopathic listening tests influence HR or HRV markers in healthy participants. Although listening tests serve as diagnostic tools for identifying somatic dysfunctions, they do not appear to exert therapeutic effects on ANS regulation. These findings contrast with previous studies on osteopathic manipulative treatment (OMT), which have demonstrated significant modulation of ANS activity. Future studies should investigate the differential effects of diagnostic tests and therapeutic techniques to better define the scope of the osteopathic interventions.
Osteopathy is a care method based on the therapeutic actions of osteopathic manipulation [1]. Before treatment, an osteopathic physician performs a physical and structural examination to assist in diagnosis and treatment [2], 3]. Touch, a key communication tool in manual therapies, helps to identify somatic dysfunctions [2]. It provides the initial physical contact that patients expect and appreciate in manual therapies [4]. Touch can serve different purposes, such as providing therapeutic intervention or gathering information [5]. Touch can also play a role in reducing negative emotions, decreasing stress biomarkers [6], and increasing relaxation and feelings of safety [7]. During osteopathic training, students progressively develop their sense of touch and learn various diagnostic techniques, including osteopathic listening tests. These tests are introduced early in the curriculum and continue to be refined throughout their education, forming part of their diagnostic toolkit [8]. Regarding the physiological basis of listening tests, the work of Biel et al. [9] on the reproducibility of palpation and Vincent et al. [10] on the quantification of tissue responses provide essential insights into the reliability of listening tests in osteopathy. Listening tests in osteopathy rely on the osteopath’s ability to perceive information transmitted by mechanoreceptors and proprioceptors, which detect mechanical changes in tissues, such as pressure and movement [11]. Additionally, research by Bland et al. [12] on the thixotropy of tissues adds an important dimension to understanding tissue responses during these tests. Research on the autonomic nervous system (ANS) has highlighted the impact of osteopathic manipulative treatment (OMT) on its function. The ANS, which regulates involuntary bodily functions, comprises the sympathetic nervous system (SNS) and parasympathetic nervous system (PNS). These systems influence heart rate (HR) and heart rate variability (HRV), both of which serve as markers for ANS activity [13]. HR, measured in beats per minute (bpm) [14], reflects ANS activity, increasing with SNS dominance and decreasing with PNS activation [15], 16]. It is a straightforward marker that can reflect potential influences of osteopathic interventions on the ANS [16]. For instance, the study by Henley et al. [17] demonstrated parasympathetic activation during cervical myofascial release. HRV, which measures the variability in time between successive heartbeats, provides deeper insights into ANS function. The root mean square of successive differences (rMSSD), a time-domain HRV measure, reflects vagal tone (PNS activity) and is independent of breathing rate [18], 19] and measured in milliseconds (ms) [14]. Frequency analysis of HRV, utilizing the low-frequency/high-frequency (LF/HF) ratio, is also a reliable measure, provided the analysis lasts at least 5 min [20]. RMSSD reflects vagal tone (PNS activity), whereas the LF/HF ratio measures sympathovagal balance [18], 21].
In this study, rMSSD serves as the primary marker for cardiac vagal tone, whereas HR and the LF/HF ratio are secondary measures. The objective is to determine whether osteopathic listening tests, widely taught but underexplored in terms of physiological effects, induce measurable changes in these markers. Specifically, do HR and HRV significantly change during a listening test session? Beyond their diagnostic role, could these tests elicit physiological responses in the patient?
Methods
This observational study was carried out from November 2022 to February 2023. It took place in the clinic of an osteopathic school. The study investigates the effect of listening tests. A protocol of these tests on the right knee, the digestive system, and the cranium was carried out. These areas were selected to explore the three main fields of osteopathy: musculoskeletal, visceral, and cranial, which have shown the effects of OMT on HR and HRV in prior studies [22], [23], [24], [25]. Data on HR, rMSSD, and LF/HF ratio were collected from subjects before and after a listening test session and compared with those from a control group (CG). A third group, involving light pressure application without therapeutic intent, was also included as a placebo. In the light pressure group (LPG), an object simulating light touch pressure (0.8 N [N], equivalent to 81.58 g [g]) was utilized [26], although it has no therapeutic intent [27]. The protocol, it is materialized by an object close to the weight defined for light touch, i.e., 0.8 N, which is equivalent to 81.58 g [26]. To isolate the effect of human contact, no practitioner touch was involved in this group. The CG participants underwent no interventions but were asked to lie on their back for the same duration as the other groups.
Population
A total of 51 participants, recruited on a voluntary basis, were selected from osteopathy students (first to fifth year). An intervention was carried out before a class to introduce the study. The project was explained to them as an HR study, without mentioning the listening tests so that they would not know the different groups. The noninclusion criteria were also presented during this intervention. Several factors can influence HR and HRV, potentially affecting the results:
Presence of known cardiac pathology, because treatment may influence HRV measurements [36].
Having an acute illness (e.g., cold, fever), which contraindicates osteopathy [37].
Cardiac and noncardiac comorbidities, because their treatment may affect HR [38].
Volunteers were contacted by email or phone, and an appointment was scheduled. Students were asked to complete an informed consent form, according to French regulation. They also completed a document to affirm that they did not present a noninclusion criterion.
If the participant did not provide informed consent or had a noninclusion criterion, he was not selected for the study. For those selected, tests were carried out in a single session. Participants with artifacts rates that were too high during the software analysis were excluded. The percentage of ectopic beats considered too high for HRV measurements was greater than 1 %, and greater than 0.1 % for rMSSD [41], 42].
Randomization
The repartition between the osteopathic test group (OTG), LPG, and CG were done by blocks of six in Microsoft Excel. Participants remained unaware of the existence of other groups to reduce bias. Demographic information for each group is presented in Table 1.
Demographic information of the osteopathic test group, light pressure group, and control group.
| Osteopathic test group (n=17) | Light pressure group (n=17) | Control group (n=17) |
|
|---|---|---|---|
| Sex | |||
| Male | 5 (29.4 %) | 4 (23.5 %) | 4 (23.5 %) |
| Female | 12 (70.6 %) | 13 (76.5 %) | 13 (76.5 %) |
| Age, years | |||
| Mean ( ± SD) | 21.6 ± 1.5 | 21.8 ± 1.5 | 21.8 ± 1.6 |
| Range | 18–24 | 18–24 | 18–24 |
-
SD, standard deviation.
Each test session involved three investigators: one performed the tests, another reproduced the protocol, and a third conducted the measurements. Investigators rotated roles randomly between the participants to further minimize bias.
Protocol
The protocol was conducted in a room with controlled ambient temperature to prevent environmental variations that could influence HRV [41].
The protocol for each group, with the number of participants at each stage, is summarized in a flow chart, shown in Figure 1. The details of each test session are then explained in Figure 2 for all of the different groups. Each test session is described for the first practitioner, and the second one reproduces the same protocol. The test procedures for each group are summarized below:
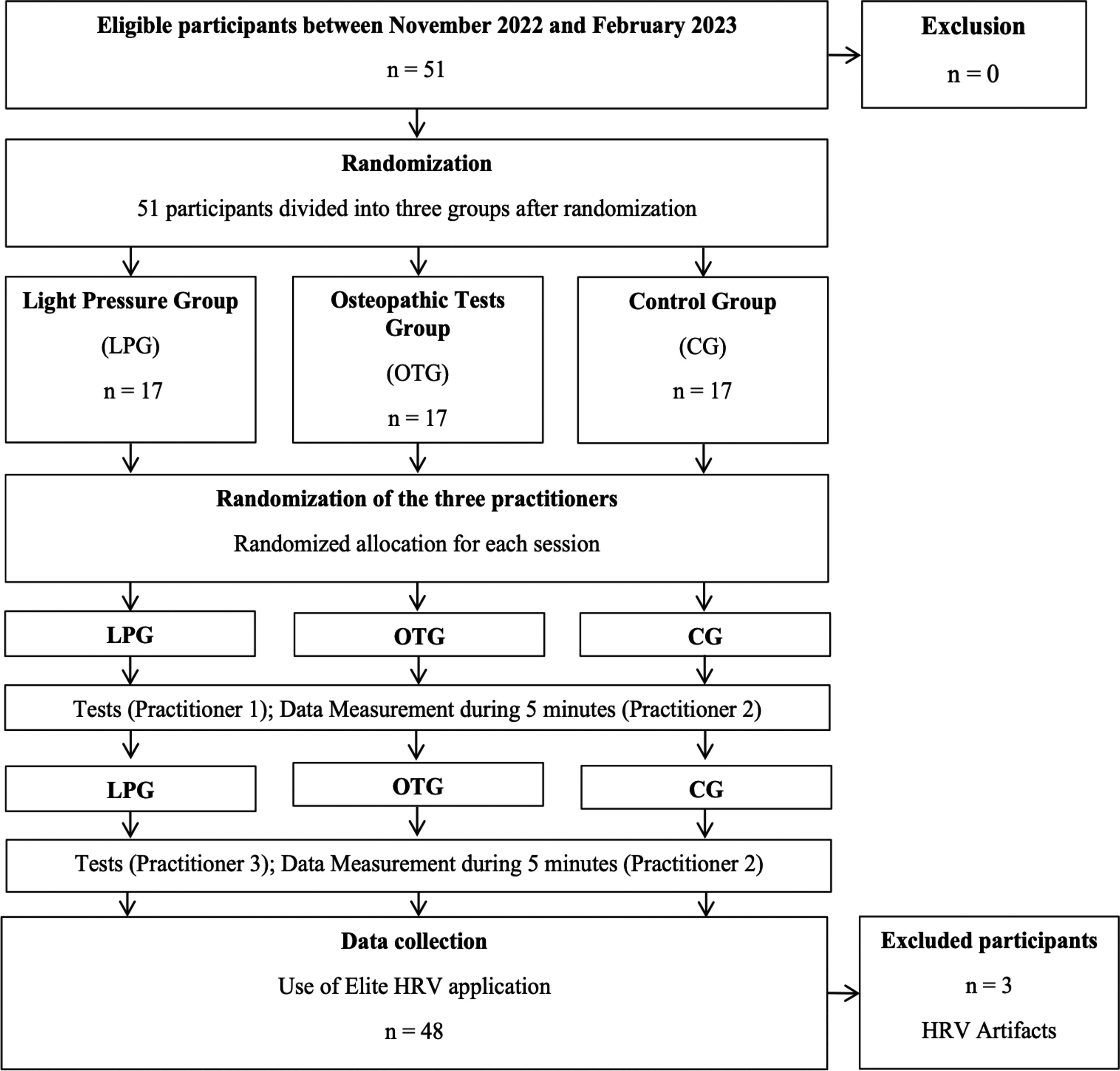
Flow chart for the observational study. CG, control group; HRV, heart rate variability; LPG, light pressure group; OTG, osteopathic test group.
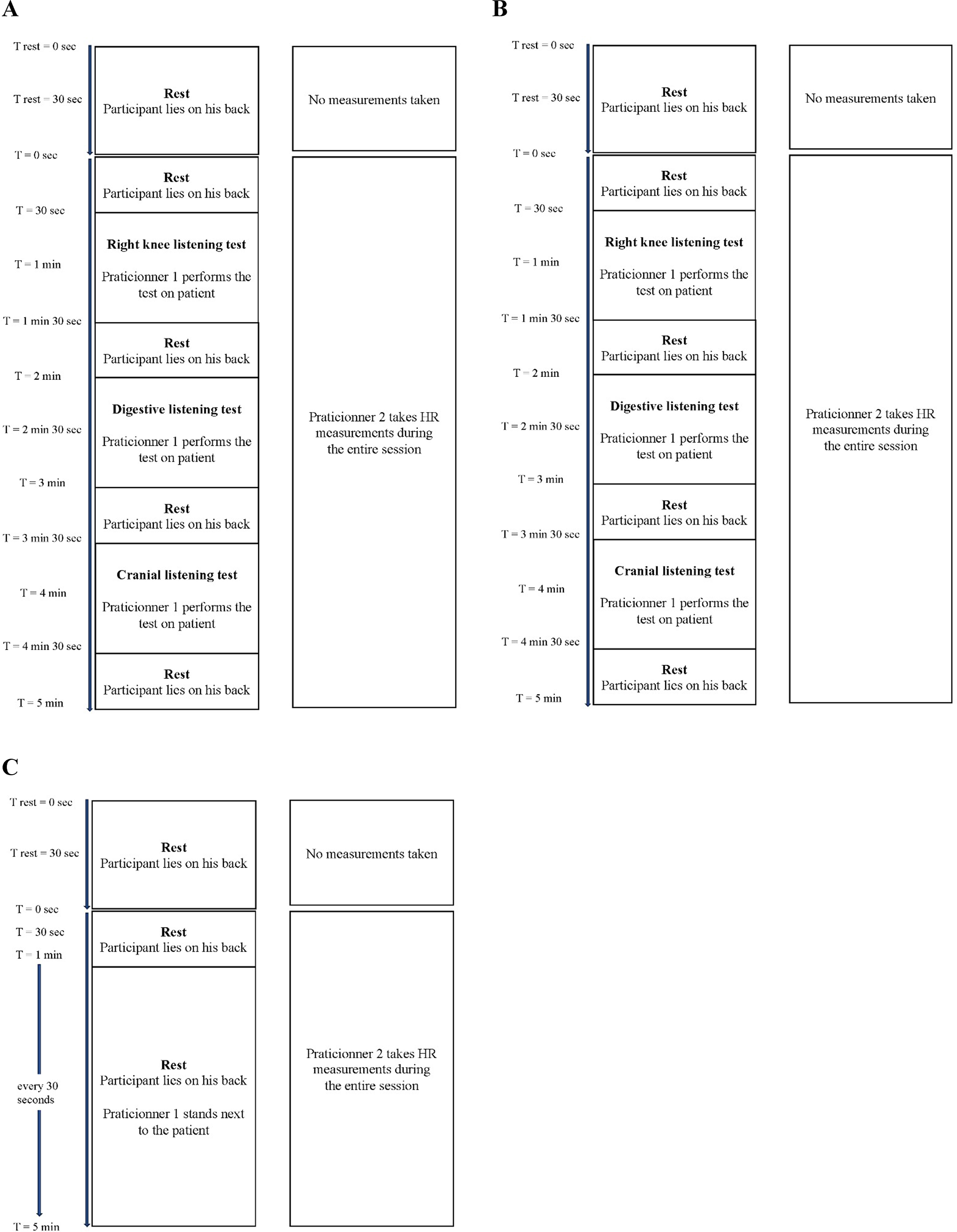
Test protocols for the different groups. (A) Protocol for the osteopathic test group session. (B) Protocol for the LPG session. (C) Protocol for the CG session. CG, control group; HR, heart rate; LPG, light pressure group.
Osteopathic test group (OTG)
The practitioner performed listening tests on the right knee (hands placed on femoral condyles and tibial plates), the digestive system (right hand positioned between the navel and xiphoid appendix), and the cranium (spheno-basilar symphysis with a four-finger grip).
Light pressure group (LPG)
A rice bag weighing 81.58 g was placed on the right femoral condyles, the area between the navel and xiphoid appendix, and the forehead, in sequence.
Control group (CG)
Participants lay supine for the same duration as the other groups without undergoing any tests or interventions.
Heart rate and heart rate variability measures
Participants were asked to remain still and silent throughout the measurements, because movement and speech can distort HRV analysis [43]. They lay on their back and rested for 1 min before the measurements began. HR and HRV measurements were then taken over a 5-min period. The tests and light pressures applied to the participants were always conducted with them in the supine position. It has been shown that body inclination increases HR [17], which is why no standing or sitting tests were performed.
For each group, a POLAR H10 chest strap was fitted by the first practitioner over the participant’s xiphoid process. The size of the strap was adjusted for each participant so that the sensor made contact with the skin. This strap enables noninvasive HR and HRV data collection for the student. The suitability of the strap for use was evaluated against electrocardiogram recordings, and it was recommended for practitioners [42]. Simultaneously, data were collected utilizing the Elite HRV mobile application, software designed for the chest strap [44]. The collected data were then analyzed utilizing the Kubios HRV software, which allows the study of HR, rMSSD, and the LF/HF ratio [45]. The validity and reliability of the three tools utilized were confirmed [19], 44], 46].
Statistical analysis
The first stage of the statistical analysis was to define if the values follow a normal distribution. The Shapiro–Wilk test was utilized to study the normality of the values of each measurement criterion. The results show that the HR values follow a normal distribution, although the rMSSD and LF/HF ratio values do not follow a normal distribution.
To begin the statistical analysis, it was necessary to compare the first 30 s of each group, for the three selected criteria, to make sure that there is no difference between the three groups at the beginning of the test session. A Student’s t-test allowed a comparison of the FC values between the three groups. Because the data are independent, a Mann–Whitney U test was utilized to compare the rMSSD and LF/HF ratio of the different groups.
To compare the different averages calculated before and after the protocol, a comparison of the means tests were carried out. The following tests were utilized for paired data. A Student’s t-test was utilized to compare the HR averages. The Wilcoxon signed-rank test was chosen to compare the means of the rMSSD and the LF/HF ratio. The significance threshold of the tests chosen is 5 %, or α=0.05.
Results
Population
Fifty-one participants were selected for the study. They were equally and randomly allocated to the osteopathic test, LPG, or CG. Each group was thus composed of 17 students, from the first to the fifth year of study (1Y to 5Y). After data analysis with the Kubios software, three participants in the LPG group were removed from the study because their values showed a percentage of artifacts greater than 5 %.
Main results
After comparing the first 30 s between each group, no significant difference was found. The p values between OTG and CG are p=0.293 for HR, p=0.158 for rMSSD, and p=0.811 for the LF/HF ratio. Between the OTG and LPG, they are p=0.315 for HR, p=0.861 for rMSSD, and p=0.799 for the LF/HF ratio. Concerning the last two groups, LPG and CG, the p values are p=0.968 for HR, p=0.063 for rMSSD, and p=0.591 for LF/HF ratio. Because there were no difference between the groups from the start, the rest of the statistical analysis could be carried out.
To compare the ANS markers before and after the test sequence, measurements were taken in the first 30 and last 30 s of each test session. Each criterion mean with their standard deviation (SD) are represented on Figure 3.
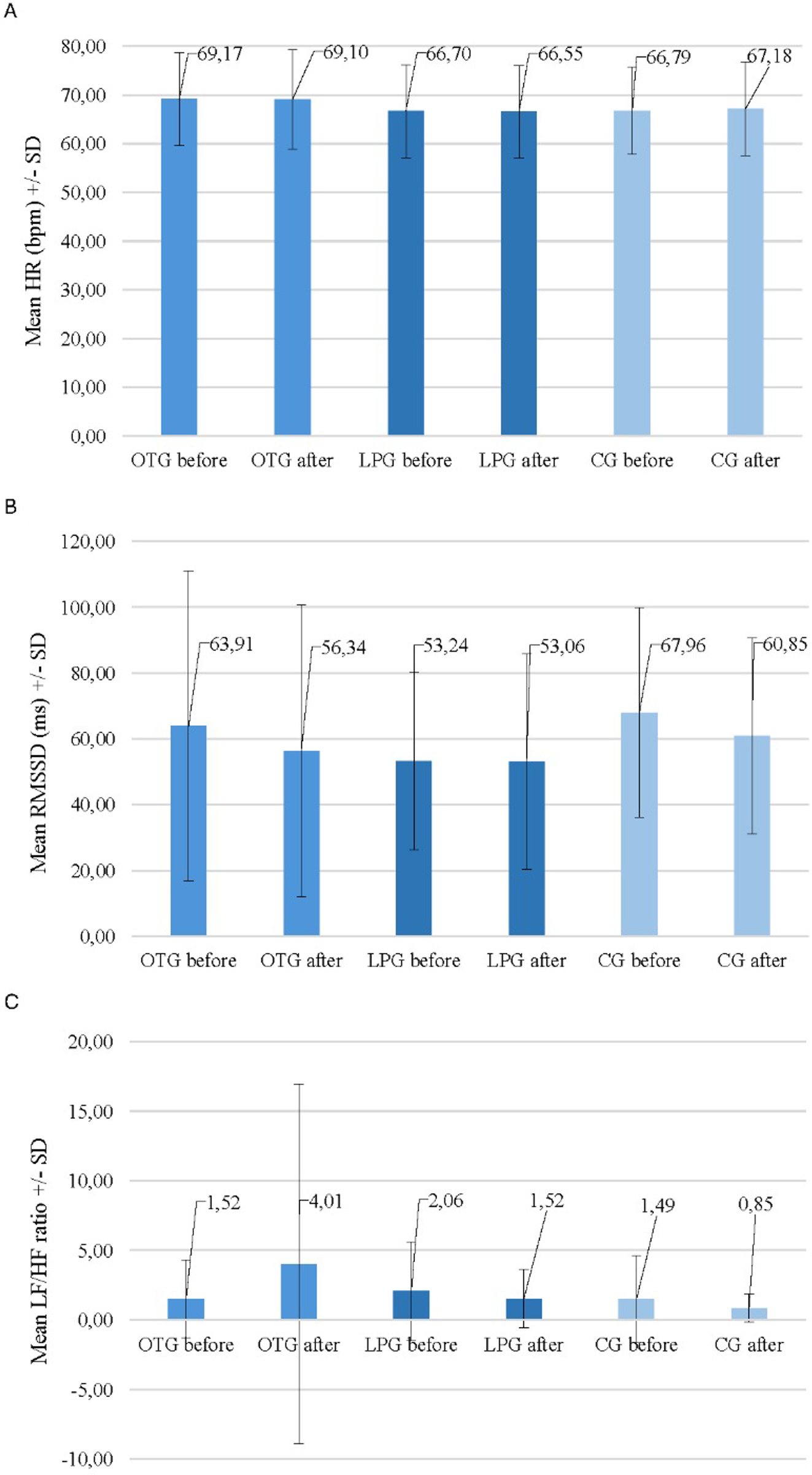
A histogram of the means of the different metrics before and after the protocol. (A) Heart rate before and after the protocol for each group. (B) rMSSD before and after the protocol for each group. (C) LF/HF ratio before and after the protocol for each group. CG, control group; LF/HF, low-frequency/high-frequency; LPG, light pressure group; OTG, osteopathic test group; rMSSD, root mean square of successive differences; SD, standard deviation.
Figure 3A shows the HR mean before and after the protocol for each group. Figure 3B represents the rMSSD means before and after protocol in the three groups. The same goes for Figure 3C, but with the LF/HF ratio mean. The values shown on this figure are represented below for each group.
Osteopathic test group (OTG)
Averages with their SD of 30 first seconds of OTG were 69.17 ± 9.58 bpm for the HR, 63.91 ± 47.09 m s for the rMSSD and 1.52 ± 2.80 for the LF/HF ratio. Over the last 30 s, the averages and their SD were 69.10 ± 10.24 bpm for the HR, 56.34 ± 44.44 m s for rMSSD, and 4.01 ± 12.93 for LF/HF ratio. When comparing the means before and after the tests, there was no significant difference emphasis for HR (p=0.884), rMSSD (p=0.064), or LF/HF ratio (p=0.106).
Light pressure group (LPG)
The LPG also showed no significant difference before and after the pressures. The averages and their SD for the first 30 s were 66.70 ± 9.55 bpm for the HR, 53.24 ± 26.94 m s for the rMSSD, and 2.06 ± 3.55 for the LF/HF ratio. The comparison of the averages did not show a significant difference for HR (p=0.812), rMSSD (p=0.814), or LF/HF ratio (p=0.981).
Control group (CG)
For the CG, the averages and their SD were 66.70 ± 9.55 bpm for HR, 53.24 ± 26.94 m s for rMSSD, and 2.06 ± 3.55 for LF/HF ratio. No significant differences were found in the comparisons between the protocol start and end averages for HR (p=0.495), rMSSD (p=0.209), or the LF/HF ratio (p=0.675).
Discussion
Interpretation
The results indicate that there were no significant changes in HR or HRV metrics (rMSSD and LF/HF ratio) following the osteopathic listening tests or light pressure application. Therefore, the hypothesis that these tests could influence ANS markers is not supported by the data. The findings suggest that the selected osteopathic listening tests do not have a measurable therapeutic effect on HR or HRV. The results suggest that these tests remain diagnostic tools utilized by osteopaths to detect somatic dysfunctions rather than interventions that produce therapeutic effects on the ANS. They do not induce significant changes in HR and HRV, and thus do not have a measurable physiological impact on the markers we selected.
Previous studies have shown that OMT can influence the ANS, especially by modulating the sympathovagal balance through HRV metrics like the LF/HF ratio [23]. Another study proposes the HRV as a useful method for developing simulated controls during studies on osteopathic manipulations [17]. While OMT has been associated with changes in HR and HRV, the results of our study suggest that listening tests themselves do not elicit similar physiological effects. It would be worthwhile to investigate whether comparing listening tests to actual OMTs would yield different results. Future studies could focus on treatment techniques rather than just diagnostic tests to explore their potential effects on the ANS. Regarding the LPG, our data show that a simple application of light pressure (utilizing a rice bag without therapeutic intent) did not lead to any significant changes in HR, rMSSD, or LF/HF ratio. This suggests that touch alone, when not combined with a therapeutic intent, does not appear to influence the ANS.
The lack of therapeutic effect observed in the osteopathic listening tests can be attributed to their primary diagnostic purpose. These tests are designed to detect somatic dysfunctions through palpation and are not intended to provide therapeutic interventions or stimulate physiological changes. Unlike OMT, which involves intentional and targeted interventions to influence physiological processes, the listening tests employ light touch primarily for assessment purposes. Furthermore, the light pressure applied during the listening tests may not constitute a sufficient stimulus to elicit a measurable autonomic response. Studies that have observed changes in HRV following osteopathic treatments often involve more dynamic manipulations that engage the musculoskeletal and nervous systems to a greater extent. In contrast, the listening tests do not involve sustained or intentional therapeutic interventions, which could explain their lack of impact on ANS markers such as HR and HRV. Another factor is the role of intentionality in therapeutic touch. Previous research suggests that the therapeutic intent behind an intervention can influence its physiological effects. In this study, the tests were explicitly diagnostic, and the absence of therapeutic intent may have contributed to the lack of observable changes in HR and HRV. This finding is supported by the results of the LPG, in which nontherapeutic touch also failed to produce significant effects on ANS markers.
These findings emphasize the need for future studies to distinguish between diagnostic and therapeutic interventions in osteopathy. Investigating the physiological effects of treatment techniques, rather than the diagnostic tests, may provide more insight into the mechanisms by which osteopathic interventions influence the ANS.
Limitations
This study has several limitations. The participants were osteopathy students, who were familiar with listening tests and were aware of their own group’s procedures, but not those of the other groups. Their prior experience with these tests may have influenced their perception of touch compared to the general population. As a result, our sample may yield different results from those that could be expected in the general population. Furthermore, because the participants were not seeking treatment, their readiness to receive touch in a therapeutic context could have been affected [47].
Another limitation is that the practitioners were students. As the quality of palpation improves with training [47], [48], [49], it is expected that the quality of touch would differ between practitioners and, moreover, between students and experienced osteopaths. Investigating whether practitioners of different experience levels, such as newly graduated osteopaths or students from various years, produce different physiological effects could provide useful insights.
The testing protocol followed a fixed sequence (knee, digestive area, and skull), which may have influenced the outcomes. Testing these sequences in different orders could potentially yield different results and insights.
Generalizability
This study is repeatable and reproducible, because the protocol and hand positions for the listening tests are easily replicable by those trained in osteopathy. However, this study could be expanded by exploring other markers of the ANS to provide a more comprehensive understanding of the potential effects of listening tests.
HRV is a simple, non-invasive method for measuring sympathovagal balance [50]. By exploring additional HRV metrics, valuable insights could be gained, because HRV is easily measurable and carries minimal risk for participants. Furthermore, a more thorough investigation of osteopathic listening tests is warranted. This could include assessing other physiological markers beyond the ANS to ensure that there are no unintended physiological effects that could be attributed to these tests as treatments. Such examinations could serve as important reference points for clinical trials. It would also be interesting to generalize this study to other osteopathic tests. Different physiological markers may yield different results, and perhaps other osteopathic tests would demonstrate modifications in these markers. The statistical analysis part could also be modified by adding other data as confidence intervals (CIs), or other statistical tests that could bring more information.
Finally, the small sample size (17 participants in each of the three groups) may limit the generalizability of the findings. Because this is an observational study presenting preliminary results, further investigation with a larger sample size would be an important next step to confirm or challenge these conclusions.
Conclusions
This study aimed to investigate the impact of osteopathic listening tests on markers of the ANS, focusing on HR, rMSSD, and the LF/HF ratio. The primary hypothesis posited that these tests would influence the ANS. However, the analysis of results did not support this hypothesis, because no significant differences were observed in the selected ANS markers before and after the listening test sessions.
To expand on these findings, it would be beneficial to conduct additional studies. Previous studies have demonstrated the impact of OMT on the ANS [17], 23], 51], and comparing these effects with those of osteopathic listening tests could provide valuable insights into the differential impacts of testing vs. treatment.
-
Research ethics: This study did not require ethical approval in accordance with local/national guidelines.
-
Informed consent: Informed consent was obtained for this case series.
-
Author contributions: All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Use of Large Language Models, AI and Machine Learning Tools: None declared.
-
Conflict of interest: None declared.
-
Research funding: None declared.
-
Data availability: All data generated or analyzed during this study are included in this article. Further inquiries can be directed to the corresponding author.
References
1. Paulus, S. The core principles of osteopathic philosophy. Int J Osteopath Med 2013:11–6. https://doi.org/10.1016/j.ijosm.2012.08.003.Search in Google Scholar
2. Baroni, F, Ruffini, N, D’Alessandro, G, Consorti, G, Lunghi, C. The role of touch in osteopathic practice: a narrative review and integrative hypothesis. Compl Ther Clin Pract 2021;42:101277. https://doi.org/10.1016/j.ctcp.2020.101277.Search in Google Scholar PubMed
3. Vaucher, P. Ostéopathie et rationalité scientifique: la place des tests dans le traitement ostéopathique. Mains Libres 2016;33:33–7.10.55498/MAINSLIBRES.2016.33.1.0033Search in Google Scholar
4. Murthy, V, Sibbritt, D, Broom, A, Kirby, E, Frawley, J, Refshauge, KM, et al.. Back pain sufferers’ attitudes toward consultations with CAM practitioners and self- prescribed CAM products: a study of a nationally representative sample of 1310 Australian women aged 60-65 years. Compl Ther Med 2015;23:782–8. https://doi.org/10.1016/j.ctim.2015.09.003.Search in Google Scholar PubMed
5. Testa, M, Rossettini, G. Enhance placebo, avoid nocebo: how contextual factors affect physiotherapy outcomes. Man Ther 2016;24:65–74. https://doi.org/10.1016/j.math.2016.04.006.Search in Google Scholar PubMed
6. Maratos, FA, Duarte, J, Barnes, C, McEwan, K, Sheffield, D, Gilbert, P. The physiological and emotional effects of touch: assessing a hand-massage intervention with high self-critics. Psychiatry Res 2017;250:221–7. https://doi.org/10.1016/j.psychres.2017.01.066.Search in Google Scholar PubMed
7. Walker, SC, Trotter, PD, Swaney, WT, Marshall, A, Mcglone, FP. C-tactile afferents: cutaneous mediators of oxytocin release during affiliative tactile interactions? Neuropeptides 2017;64:27–38. https://doi.org/10.1016/j.npep.2017.01.001.Search in Google Scholar PubMed
8. Référentiel de formation en ostéopathie. Bulletin officiel santé - protection sociale - solidarité 2014:233–300.Search in Google Scholar
9. Biel, A. Reproducibility of manual palpation in musculoskeletal diagnosis: a systematic review. Man Ther 2015;20:653–60.Search in Google Scholar
10. Vincent, L. Quantitative assessment of manual palpation in osteopathy: measuring the impact of force application on tissue reactivity. J Osteopath Med 2019;13:91–8.Search in Google Scholar
11. Gordon, AM. The role of mechanoreceptors in tactile and proprioceptive feedback in manual therapy. J Manipulative Physiol Therapeut 2016;39:512–9.Search in Google Scholar
12. Bland, J. Thixotropy and the human connective tissue response: implications for osteopathic diagnosis. J Bodyw Mov Ther 2012;16:236–42.Search in Google Scholar
13. Korr, I. Bases physiologiques de l’ostéopathie. Paris: Frison Roche; 2000:237 p.Search in Google Scholar
14. Besson, C, Saubade, M, Gremeaux, V, Millet, GP, Schmitt, L. [Heart rate variability: methods, limitations and clinical examples]. Rev Med Suisse 2020;16:1432–7. https://doi.org/10.53738/revmed.2020.16.701.1432.Search in Google Scholar
15. Bankenahally, R, Krovvidi, H. Autonomic nervous system: anatomy, physiology, and relevance in anaesthesia and critical care medicine. BJA Education 2016:381–7. https://doi.org/10.1093/bjaed/mkw011.Search in Google Scholar
16. Marsac, J. Variabilité de la fréquence cardiaque: un marqueur de risque cardiométabolique en santé publique. Bull Acad Natl Med (Paris) 2013:175–86. https://doi.org/10.1016/s0001-4079(19)31635-8.Search in Google Scholar
17. Henley, CE, Ivins, D, Mills, M, Wen, FK, Benjamin, BA. Osteopathic manipulative treatment and its relationship to autonomic nervous system activity as demonstrated by heart rate variability: a repeated measures study. Osteopath Med Prim Care 2008;2:7. https://doi.org/10.1186/1750-4732-2-7.Search in Google Scholar PubMed PubMed Central
18. Laborde, S, Mosley, E, Thayer, JF. Heart rate variability and cardiac vagal tone in psychophysiological research - recommendations for experiment planning, data analysis, and data reporting. Front Psychol 2017;8:213. https://doi.org/10.3389/fpsyg.2017.00213.Search in Google Scholar PubMed PubMed Central
19. Rogers, B, Schaffarczyk, M, Gronwald, T. Estimation of respiratory frequency in women and men by Kubios HRV software using the polar H10 or movesense medical ECG sensor during an exercise ramp. Sensors 2022;22. https://doi.org/10.3390/s22197156.Search in Google Scholar PubMed PubMed Central
20. Roura, S, Álvarez, G, Solà, I, Cerritelli, F. Do manual therapies have a specific autonomic effect? An overview of systematic reviews. PLoS One 2021;16:e0260642. https://doi.org/10.1371/journal.pone.0260642.Search in Google Scholar PubMed PubMed Central
21. Heart rate variability. Standards of measurement, physiological interpretation, and clinical use. Task force of the European society of cardiology and the North American society of pacing and electrophysiology. Eur Heart J 1996;17:354–81.Search in Google Scholar
22. Codandamourty, M. Evolution des fondements de l’Ostéopathie : comparaison des modèles et principes édités par A.T Still (XIXe siècle) et l’OMS (2010). Grenoble: Centre hospitalier universitaire de Grenoble; 2014.Search in Google Scholar
23. Ruffini, N, D’Alessandro, G, Mariani, N, Pollastrelli, A, Cardinali, L, Cerritelli, F. Variations of high frequency parameter of heart rate variability following osteopathic manipulative treatment in healthy subjects compared to control group and sham therapy: randomized controlled trial. Front Neurosci 2015;9:272. https://doi.org/10.3389/fnins.2015.00272.Search in Google Scholar PubMed PubMed Central
24. Christina, CCA, Alex, SMA, Julio, GS. Cardiac autonomic response after cranial technique of the fourth ventricle (cv4) compression in systemic hypertensive subjects. J Bodyw Mov Ther 2017;22:666–72.10.1016/j.jbmt.2017.11.013Search in Google Scholar PubMed
25. Verena, R, Michael, B, Jan, P. Effectiveness of an osteopathic treatment on the autonomic nervous system: a systematic review of the literature. Eur J Med Res 2019:24–36.10.1186/s40001-019-0394-5Search in Google Scholar PubMed PubMed Central
26. Hanley, MA, Coppa, D, Shields, D. A practice-based theory of healing through therapeutic touch : advancing holistic nursing practice. J Holist Nurs 2017;35:369–81. https://doi.org/10.1177/0898010117721827.Search in Google Scholar PubMed
27. Gas, V. Light touch study. In: T, G, editor. Estimation de l’effet de la pression légère utilisée comme placebo dans les essais cliniques contrôlés en ostéopathie – étude pilote2014:1–5 pp.Search in Google Scholar
28. Gonzaga, LA, Vanderlei, LCM, Gomes, RL, Valenti, VE. Caffeine affects autonomic control of heart rate and blood pressure recovery after aerobic exercise in young adults: a crossover study. Sci Rep 2017;7:14091. https://doi.org/10.1038/s41598-017-14540-4.Search in Google Scholar PubMed PubMed Central
29. Sarshin, A, Naderi, A, da Cruz, CJG, Feizolahi, F, Forbes, SC, Candow, DG, et al.. The effects of varying doses of caffeine on cardiac parasympathetic reactivation following an acute bout of anaerobic exercise in recreational athletes. J Int Soc Sports Nutr 2020;17:44. https://doi.org/10.1186/s12970-020-00373-6.Search in Google Scholar PubMed PubMed Central
30. Benjamim, CJR, Monteiro, LRL, Pontes, YMM, Silva, A, Souza, TKM, Valenti, VE, et al.. Caffeine slows heart rate autonomic recovery following strength exercise in healthy subjects. Rev Port Cardiol 2021;40:399–406. https://doi.org/10.1016/j.repce.2020.07.021.Search in Google Scholar PubMed
31. Kim, CS, Kim, MK, Jung, HY, Kim, MJ. Effects of exercise training intensity on cardiac autonomic regulation in habitual smokers. Ann Noninvasive Electrocardiol 2017;22. https://doi.org/10.1111/anec.12434.Search in Google Scholar PubMed PubMed Central
32. Gronwald, T, Hoos, O. Correlation properties of heart rate variability during endurance exercise: a systematic review. Ann Noninvasive Electrocardiol 2020;25:e12697. https://doi.org/10.1111/anec.12697.Search in Google Scholar PubMed PubMed Central
33. Sumartiningsih, S, Lin, HF, Lin, JC. Cigarette smoking blunts exercise-induced heart rate response among young adult male smokers. Int J Environ Res Publ Health 2019;16. https://doi.org/10.3390/ijerph16061032.Search in Google Scholar PubMed PubMed Central
34. Gonzalez, JE, Cooke, WH. Acute effects of electronic cigarettes on arterial pressure and peripheral sympathetic activity in young nonsmokers. Am J Physiol Heart Circ Physiol 2021;320:H248–h55. https://doi.org/10.1152/ajpheart.00448.2020.Search in Google Scholar PubMed
35. Guo, QN, Wang, J, Liu, HY, Wu, D, Liao, SX. Nicotine ingestion reduces heart rate variability in young healthy adults. BioMed Res Int 2022;2022:4286621. https://doi.org/10.1155/2022/4286621.Search in Google Scholar PubMed PubMed Central
36. Galaasen Bakken, A, Eklund, A, Hallman, DM, Axén, I. The effect of spinal manipulative therapy and home stretching exercises on heart rate variability in patients with persistent or recurrent neck pain: a randomized controlled trial. Chiropr Man Ther 2021;29:48. https://doi.org/10.1186/s12998-021-00406-0.Search in Google Scholar PubMed PubMed Central
37. Chabot, F, Tillie-Leblond, I, Cuvelier, A, Maitre, B, Jouniteaux, V, Marquette, CH. Référentiel de sémiologie respiratoire. Nancy; 2009:141 p.Search in Google Scholar
38. Böhm, M, Robertson, M, Ford, I, Borer, JS, Komajda, M, Kindermann, I, et al.. Influence of cardiovascular and noncardiovascular Co-morbidities on outcomes and treatment effect of heart rate reduction with ivabradine in stable heart failure (from the SHIFT trial). Am J Cardiol 2015;116:1890–7. https://doi.org/10.1016/j.amjcard.2015.09.029.Search in Google Scholar PubMed
39. Alvares, GA, Quintana, DS, Hickie, IB, Guastella, AJ. Autonomic nervous system dysfunction in psychiatric disorders and the impact of psychotropic medications: a systematic review and meta-analysis. J Psychiatry Neurosci 2016;41:89–104. https://doi.org/10.1503/jpn.140217.Search in Google Scholar PubMed PubMed Central
40. Ide, T, Ohtani, K, Higo, T, Tanaka, M, Kawasaki, Y, Tsutsui, H. Ivabradine for the treatment of cardiovascular diseases. Circ J 2019;83:252–60. https://doi.org/10.1253/circj.cj-18-1184.Search in Google Scholar
41. Abellán-Aynés, O, Manonelles, P, Alacid, F. Cardiac parasympathetic withdrawal and sympathetic activity: effect of heat exposure on heart rate variability. Int J Environ Res Publ Health 2021;18. https://doi.org/10.3390/ijerph18115934.Search in Google Scholar PubMed PubMed Central
42. Schaffarczyk, M, Rogers, B, Reer, R, Gronwald, T. Validity of the polar H10 sensor for heart rate variability analysis during resting state and incremental exercise in recreational men and women. Sensors 2022;22. https://doi.org/10.3390/s22176536.Search in Google Scholar PubMed PubMed Central
43. Catai, AM, Pastre, CM, Godoy, MF, Silva, ED, Takahashi, ACM, Vanderlei, LCM. Heart rate variability: are you using it properly? Standardisation checklist of procedures. Braz J Phys Ther 2020;24:91–102. https://doi.org/10.1016/j.bjpt.2019.02.006.Search in Google Scholar PubMed PubMed Central
44. Chhetri, P, Shrestha, L, Mahotra, NB. Validity of elite-HRV smartphone application for measuring heart rate variability compared to polar V800 heart rate monitor. J Nepal Health Res Counc 2022;19:809–13. https://doi.org/10.33314/jnhrc.v19i04.3949.Search in Google Scholar PubMed
45. Kubios HRV User’s guide. Biosignal analysis and medical imaging group. Kuopio, Finland; 2014.Search in Google Scholar
46. Tarvainen, MP, Niskanen, JP, Lipponen, JA, Ranta-Aho, PO, Karjalainen, PA. Kubios HRV--heart rate variability analysis software. Comput Methods Progr Biomed 2014;113:210–20. https://doi.org/10.1016/j.cmpb.2013.07.024.Search in Google Scholar PubMed
47. Andersen, LM, Lundqvist, D. Somatosensory responses to nothing: an MEG study of expectations during omission of tactile stimulations. Neuroimage 2019;184:78–89. https://doi.org/10.1016/j.neuroimage.2018.09.014.Search in Google Scholar PubMed
48. Foster, IE, Bagust, J. Cutaneous two-point discrimination thresholds and palpatory sensibility in chiropractic students and field chiropractors. J Manip Physiol Ther 2004;27:466–71. https://doi.org/10.1016/j.jmpt.2004.06.005.Search in Google Scholar PubMed
49. Degenhardt, BF, Johnson, JC, Snider, KT, Snider, EJ. Maintenance and improvement of interobserver reliability of osteopathic palpatory tests over a 4-month period. J Am Osteopath Assoc 2010;110:579–86.Search in Google Scholar
50. Sztajzel, J. Heart rate variability: a noninvasive electrocardiographic method to measure the autonomic nervous system. Swiss Med Wkly 2004;134:514–22.Search in Google Scholar
51. Giles, PD, Hensel, KL, Pacchia, CF, Smith, ML. Suboccipital decompression enhances heart rate variability indices of cardiac control in healthy subjects. J Alternative Compl Med 2013;19:92–6.10.1089/acm.2011.0031Search in Google Scholar PubMed PubMed Central
© 2025 the author(s), published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Frontmatter
- Behavioral Health
- Original Article
- Bridging the gap: associations of provider enrollment in OKCAPMAP with social deprivation, child abuse, and barriers to access in the state of Oklahoma, USA
- Cardiopulmonary Medicine
- Original Article
- Impact of osteopathic tests on heart rate and heart rate variability: an observational study on osteopathic students
- General
- Review Article
- Comparing intubation techniques of Klippel–Feil syndrome patients in the last 10 years: a systematic review
- Medical Education
- Original Article
- Understanding COMLEX-USA Level-1 as a Pass/Fail examination: impact and opportunities
- Musculoskeletal Medicine and Pain
- Original Article
- Longitudinal outcomes among patients with fibromyalgia, chronic widespread pain, or localized chronic low back pain
- Neuromusculoskeletal Medicine (OMT)
- Original Article
- Carpal tunnel dimensions following osteopathic manipulation utilizing dorsal carpal arch muscle energy: a pilot study
- Corrigendum
- Corrigendum to: Carpal tunnel dimensions following osteopathic manipulation utilizing dorsal carpal arch muscle energy: a pilot study
Articles in the same Issue
- Frontmatter
- Behavioral Health
- Original Article
- Bridging the gap: associations of provider enrollment in OKCAPMAP with social deprivation, child abuse, and barriers to access in the state of Oklahoma, USA
- Cardiopulmonary Medicine
- Original Article
- Impact of osteopathic tests on heart rate and heart rate variability: an observational study on osteopathic students
- General
- Review Article
- Comparing intubation techniques of Klippel–Feil syndrome patients in the last 10 years: a systematic review
- Medical Education
- Original Article
- Understanding COMLEX-USA Level-1 as a Pass/Fail examination: impact and opportunities
- Musculoskeletal Medicine and Pain
- Original Article
- Longitudinal outcomes among patients with fibromyalgia, chronic widespread pain, or localized chronic low back pain
- Neuromusculoskeletal Medicine (OMT)
- Original Article
- Carpal tunnel dimensions following osteopathic manipulation utilizing dorsal carpal arch muscle energy: a pilot study
- Corrigendum
- Corrigendum to: Carpal tunnel dimensions following osteopathic manipulation utilizing dorsal carpal arch muscle energy: a pilot study

