Abstract
Nail-patella syndrome is a genetic disorder with some characteristic features (nail dysplasia, patellar hypoplasia, elbow dysplasia, iliac horns and renal symptoms). Renal involvement of these patients requires close follow-up in pregnancy to avoid complications like preeclampsia. In this report, we have presented two consecutive successful pregnancies of a patient with nail-patella syndrome. The first pregnancy resulted with a newborn with nail-patella syndrome and the second pregnancy resulted in a healthy newborn without any obstetric complications. Renal functions were closely followed-up during both pregnancies, and basal renal functions were normal in the pregestational period, which seems to be the most important predictor of obstetric hypertensive complications. Prenatal diagnosis of nail-patella disease is also challenging due to several possible mutations and a wide range of phenotypes of the disease. Ultrasonographic examination findings may be suspicious for the disease in the fetus like patellar hypoplasia or joint contractures.
Introduction
Nail-patella syndrome, also known as hereditary onychosteodysplasia, is a genetic disorder characterized by nail dysplasia, patellar hypoplasia, elbow dysplasia, iliac horns and renal symptoms. This syndrome is rare, with an incidence of 1/50,000 and is inherited in an autosomal dominant pattern [1]. Apart from the characteristic skeletal problems, renal involvement of the patients requires careful follow-up during pregnancy to avoid complications such as preeclampsia [2]. Renal involvement of the disease may have a wide spectrum ranging from trace proteinuria to end-stage renal disease. Thus, close follow-up of renal functions and avoiding complications like preeclampsia in patients with nail-patella syndrome is the key point in follow-up of the disease. Due to the autosomal dominant inheritance, prenatal diagnosis and ultrasonographic examinations are also key points for the outcome of these pregnancies.
In this report, we present the case of two consecutive successful pregnancies in a patient with nail-patella syndrome.
Case report
The patient was diagnosed as having nail-patella syndrome at the age of 12 years after admission to the hospital for symptoms related to rib deformities and nail hypoplasia. The syndrome-related symptoms included nail hypoplasia in the upper extremities, decreased flexibility at the elbow joints, contractures at both ankles and slight deformity of the cranial bones. The patient was admitted to our hospital for her first pregnancy at the age of 27 years. The baseline renal functions were normal. A first trimester urine analysis revealed 245 mg/24 h proteinuria. The patient’s follow-up was performed by the nephrology and perinatology departments of our institution. Blood pressure levels were found to be normal during the entire antenatal period. Routine follow-up was performed and no additional medication was given to the patient for any obstetric complication. Fetal ultrasonograms were normal. At the 39th gestational week, the patient delivered by cesarean section due to acute fetal distress, with a birthweight of 3590 g and APGAR scores of 9 and 10 at the 1st and 5th min, respectively. Examination of the newborn revealed the presence of nail hypoplasia (Figure 1). Patellar hypoplasia (Figure 2), joint contracture at the elbow and clinodactyly were observed in the newborn at the age of 2 years. Due to these symptoms, the newborn was also diagnosed as having nail-patella syndrome. Regular follow-ups performed during the next 7 years showed no additional symptoms.

Nail hypoplasia of affected child and mother.
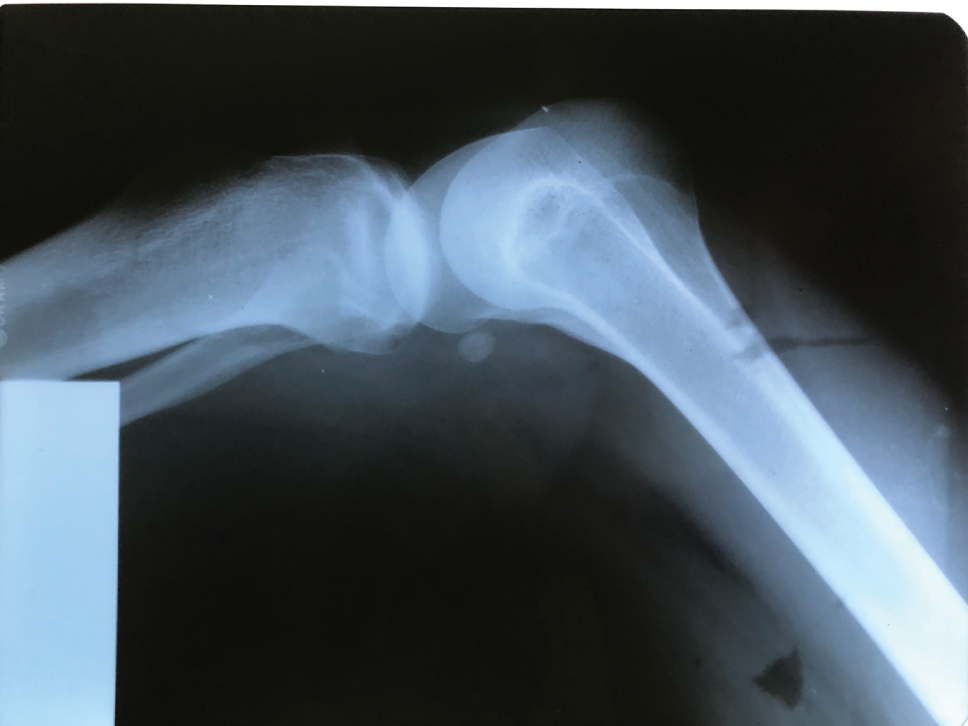
X-ray of the knee joint of the affected child.
The patient was admitted for her second pregnancy at the age of 34 years (the patient’s follow-up was performed by the nephrology department between the two gestations and reported no complications). A first trimester spot urine analysis revealed trace proteinuria with normal blood pressure levels. During antenatal follow-ups, amniocentesis was performed due to the increased risk at the first trimester screening. The chromosomal analysis reported a normal karyotype, but no other tests for nail-patella syndrome were performed due to the lack of information concerning the exact mutation in our patient. Ultrasonographic examinations showed patellar structures in both fetal joints. Third trimester urine analysis yielded 14.2 mg albumin and 63.1 mg protein in a spot urine sample. After routine antenatal care performed by the perinatology and nephrology departments without any medical intervention, the patient delivered via cesarean section due to past uterine surgery at the 38th gestational week with a birthweight of 3150 g. Examination of the newborn revealed normal nail structure and skeletal anatomy. The patient’s second child was evaluated as disease-free by the neonatology and genetics departments. The required informed consent was acquired from the patient.
Discussion
Nail-patella syndrome is inherited as an autosomal dominant disease. Despite its autosomal dominant inheritance, expression of the gene is variable even within affected families [3]. The disease-related gene is named LMX1B and is located on the distal end of the long arm of chromosome 9 in the region 9q34. The LMX1B gene is a transcription factor involved in limb and kidney development [4]. Nail-patella syndrome is mostly identified by skeletal system findings. Nail dysplasia, patellar hypoplasia, elbow dysplasia and iliac horns are the most common and characteristic symptoms of this disease. According to the literature, nail involvement is the most common symptom, present in nearly all cases [3]. Renal involvement is another important feature of the disease and may occur in 60% of all cases [5]. The most frequent renal finding is asymptomatic proteinuria, which occurs in 40% of cases [6]. Most patients had a silent course of renal disesase, but this syndrome may lead to end stage renal disease in 1–5% of cases [5]. Renal involvement is highly critical in terms of achieving a successful pregnancy because of the risks related to preeclampsia and increased proteinuria.
We have presented the case study of a patient with two consecutive successful pregnancies. Our patient had normal renal function with only minimal proteinuria during the pregestational period. Having normal renal function seems to be one of the most important points for preserving renal function during the pregnancy and avoiding complications such as preeclampsia or gestational hypertension. The existance of massive proteinuria in the early periods of pregnancy has been shown to complicate pregnancies and result in intrauterine demise [7]. It has also been reported that preeclampsia may occur in patients without proteinuria [2]. Pathognomonic findings in cases of renal involvement present as cross-banded collagen fibrils within the glomerular basement membrane under electron microscopy [7].
Despite our patient’s successful consecutive pregnancies, it is difficult to predict the course of renal function in such pregnancies, and a close follow-up must be performed for every pregnant patient with nail-patella syndrome. The most important prognostic factor seems to be pregestational renal function and abnormalities for pregnancy outcomes and complications, as shown in our case. It has also been shown that increased amounts of proteinuria in the patients with preeclampsia leads to obstetric complications such as preterm labor which also demonstrates the significance of renal functions in the pregestational or antepartum period [8]. It is critical to maintain normal pregestational renal function to avoid complications such as preeclampsia which is predisposed by nail-patella syndrome.
Due to the autosomal dominant inheritance of nail-patella syndrome, prenatal diagnosis is very important for the accurate follow-up of these pregnancies and for prenatal counseling. The syndrome is strictly related with mutations of the LMX1B gene, which provides an opportunity to diagnose affected fetuses via molecular techniques. The most challenging issue in molecular prenatal diagnosis is the existance of several deletions or variations [9]. Because of that fact and the absence of an exact mutation in our patient, we could not perform any invasive procedure for the prenatal diagnosis of nail-patella syndrome. Ultrasonographic examination may also be useful for the prenatal diagnosis of nail-patella syndrome. Absence of the patellae, presence of deformities of the femoral neck and congenital talipes may be used for the diagnosis of nail-patella syndrome [10]. Due to the variable phenotypes of the syndrome, such as hypoplastic or normal patellae, prenatal misdiagnosis is also possible. In the second pregnancy in our case, we observed a normal skeletal anatomy. Ultrasound seems to be crucial for prenatal counseling of families without recourse to molecular diagnosis.
In conclusion, despite the evident risk of preeclampsia in pregnancy, patients with nail-patella syndrome may have good obstetric outcomes with regular and strict follow-up performed at a tertiary center. The most important predictors seem to be normal renal function and the absence of marked proteinuria during the pregestational period.
Author’s Statement
-
Conflict of interest: Authors state no conflict of interest.
Material and Methods
-
Informed consent: Informed consent has been obtained from all individuals included in this study.
-
Ethical approval: The research related to human subject use has complied with all the relevant national regulations, and institutional policies, and is in accordance with the tenets of the Helsinki Declaration, and has been approved by the authors’ institutional review board or equivalent committee.
References
[1] Wynne-Davies R, Hall CM, Apley AG. Atlas of skeletal dysplasias. Edinburgh: Churchill Livingstone, 1985.Search in Google Scholar
[2] Casellas M, Tey RR, Segura A, Cerqueira MJ, Romero F, Codina S, et al. Nail-patella syndrome and pre-eclampsia. Eur J Obstet Gynecol Reprod Biol. 1993;52:219–22.10.1016/0028-2243(93)90076-OSearch in Google Scholar
[3] Bongers EM, Huysmans FT, Levtchenko E, de Rooy JW, Blickman JG, Admiraal RJ, et al. Genotype-phenotype studies in nail-patella syndrome show that LMX1B mutation location is involved in the risk of developing nephropathy. Eur J Hum Genet. 2005;13:935–46.10.1038/sj.ejhg.5201446Search in Google Scholar PubMed
[4] Vollrath D, Jaramillo-Babb VL, Clough MV, McIntosh I, Scott KM, Lichter PR, et al. Loss-of-function mutations in the LIM-homeodomain gene, LMX1B, in nail-patella syndrome. Hum Mol Genet. 1998;7:1091–8.10.1093/hmg/7.7.1091Search in Google Scholar PubMed
[5] Knoers NV, Bongers EM, Van Beersum SE, Lommen EJ, Van Bokhoven H, Hol FA. Nail-patella syndrome identification of mutations in the LMX1B gene in Dutch families. J Am Soc Nephrol. 2000;11:1762–6.10.1681/ASN.V1191762Search in Google Scholar PubMed
[6] Granata A, Nori G, Ravazzolo R, Marini M, Castellino S, Sicurezza E, et al. Nail-patella syndrome and renal involvement. Description of three cases and literature review. Clin Nephrol. 2008;69:377–82.10.5414/CNP69377Search in Google Scholar PubMed
[7] Aboobacker I, Krishnakumar A, Narayanan S, Hafeeque B, Gopinathan J, Aziz F. Nail-patella syndrome: A rare cause of nephrotic syndrome in pregnancy. Ind J Nephrol. 2018;28:76–8.10.4103/ijn.IJN_362_16Search in Google Scholar PubMed PubMed Central
[8] Parlakgümüş HA, Şimşek E, Çok T, Tarım E. The relationship between proteinuria in severe preeclampsia and maternal and fetal outcomes. Gynecol Obstet Reprod Med. 2012;18:7–11.Search in Google Scholar
[9] Ghoumid J, Petit F, Holder-Espinasse M, Jourdain AS, Guerra J, Dieux-Coeslier A, et al. Nail-patella syndrome: clinical and molecular data in 55 families raising the hypothesis of a genetic heterogeneity. Eur J Hum Genet. 2016;24:44–50.10.1038/ejhg.2015.77Search in Google Scholar PubMed PubMed Central
[10] Pinette MG, Ukleja M, Blackstone J. Early prenatal diagnosis of nail-patella syndrome by ultrasonography. J Ultrasound Med. 1999;18:387–9.10.7863/jum.1999.18.5.387Search in Google Scholar PubMed
©2018 Walter de Gruyter GmbH, Berlin/Boston
Articles in the same Issue
- Case Reports – Obstetrics
- Trisomy 9 presenting in the first trimester as a fetal lateral neck cyst and increased nuchal translucency
- A case of intrauterine closure of the ductus arteriosus and non-immune hydrops
- Pregnancy luteoma: a rare presentation and expectant management
- A pregnant woman with an operated bladder extrophy and a pregnancy complicated by placenta previa and preterm labor
- Consecutive successful pregnancies of a patient with nail-patella syndrome
- A multidisciplinary management approach for patients with Klippel-Trenaunay syndrome and multifetal gestation with successful outcomes
- A uterus didelphys with a spontaneous labor at term of pregnancy: a rare case and a review of the literature
- Case Reports – Fetus
- Prenatal diagnosis of ring chromosome 13: a rare chromosomal aberration
- Case Reports – Newborn
- Late-onset pubic-phallic idiopathic edema in premature recovering infants
- An unusual cause of neonatal shock: a case report
- Early ultrasonographic follow up in neonatal pneumatocele. Two case reports
- Nonsyndromic extremely premature eruption of teeth in preterm neonates – a report of three cases and a review of the literature
- Successful outcome of a preterm infant with severe oligohydramnios and suspected pulmonary hypoplasia following premature rupture of membranes (PPROM) at 18 weeks’ gestation
- Onset of Kawasaki disease immediately after birth
- Short rib-polydactyly syndrome (Saldino-Noonan type) undetected by standard prenatal genetic testing
- Severe congenital autoimmune neutropenia in preterm monozygotic twins: case series and literature review
- Verona integron-encoded metallo-β-lactamase-producing Klebsiella pneumoniae sepsis in an extremely premature infant
Articles in the same Issue
- Case Reports – Obstetrics
- Trisomy 9 presenting in the first trimester as a fetal lateral neck cyst and increased nuchal translucency
- A case of intrauterine closure of the ductus arteriosus and non-immune hydrops
- Pregnancy luteoma: a rare presentation and expectant management
- A pregnant woman with an operated bladder extrophy and a pregnancy complicated by placenta previa and preterm labor
- Consecutive successful pregnancies of a patient with nail-patella syndrome
- A multidisciplinary management approach for patients with Klippel-Trenaunay syndrome and multifetal gestation with successful outcomes
- A uterus didelphys with a spontaneous labor at term of pregnancy: a rare case and a review of the literature
- Case Reports – Fetus
- Prenatal diagnosis of ring chromosome 13: a rare chromosomal aberration
- Case Reports – Newborn
- Late-onset pubic-phallic idiopathic edema in premature recovering infants
- An unusual cause of neonatal shock: a case report
- Early ultrasonographic follow up in neonatal pneumatocele. Two case reports
- Nonsyndromic extremely premature eruption of teeth in preterm neonates – a report of three cases and a review of the literature
- Successful outcome of a preterm infant with severe oligohydramnios and suspected pulmonary hypoplasia following premature rupture of membranes (PPROM) at 18 weeks’ gestation
- Onset of Kawasaki disease immediately after birth
- Short rib-polydactyly syndrome (Saldino-Noonan type) undetected by standard prenatal genetic testing
- Severe congenital autoimmune neutropenia in preterm monozygotic twins: case series and literature review
- Verona integron-encoded metallo-β-lactamase-producing Klebsiella pneumoniae sepsis in an extremely premature infant

