To the Editor,
Possibly lethal infections must be recognized immediately and readily-available characteristic laboratory findings could speed up essential decision making. Here, we present two cases of lethal infection with Clostridium perfringens. This anaerobic, gram-positive, rod shaped bacterium, which can be found in soil as well as the intestinal and genital microbiome of healthy individuals [1], [2], is most commonly known for its ability to cause food-poisoning. While uncommon, infection may lead to lethal sepsis with complications such as gas gangrene, necrotic myositis, and most notably, massive intravascular hemolysis. With a mortality rate of 70–100%, timely recognition of C. perfringens sepsis is of utmost importance [1]. Several clinical case reports have been published [1], [3], [4], [5], but none have focused on the laboratory’s perspective. Here, we emphasize on characteristic and readily-available laboratory findings that could support the clinician in timely identification and diagnosis.
Case A, a 61-year-old male, presented with progressive lower back pain, nausea and vomiting. Physical examination showed a perceptive but restless man with scleral icterus, fever, tachycardia, and tachypnea. Computed tomography revealed one large (∼4.6 cm) and multiple smaller gas-containing hepatic lesions. A single dose of cefuroxime was administered and blood sampling was performed for routine clinical chemistry, hematology and microbiology tests. Due to excessive hemolytic plasma, clinical chemistry results could not be provided. His hemoglobin (Hb) level was 1.6 mmol/L and the direct antiglobulin test (DAT) was negative. The patient’s condition deteriorated rapidly and he was transferred to the ICU. He died within 5 h of presentation due to multiple organ failure. Later, blood culture tests came back positive for C. perfringens. Autopsy also revealed C. perfringens in the liver lesions.
Case B, a 71-year-old female, presented with acute abdominal pain, vomiting, and diarrhea. Physical examination revealed tenderness in the right upper quadrant of the abdomen, but no clinical signs of cholecystitis. There were no other complaints or fever and her vital signs were normal. Laboratory results showed a normal Hb concentration (9.2 mmol/L), increased leukocyte count, normal C-reactive protein, elevated hepatobiliary enzymes and bilirubin, and markedly elevated amylase. Suspecting biliary pancreatitis, she was admitted for treatment. The next day, medical ultrasound showed signs of cholangitis, for which she received cefuroxime and tobramycin. 36 h later, she developed a fever, hematuria, icterus and tachypnea. Laboratory results showed an Hb concentration of 2.0 mmol/L, a negative DAT and a high thrombocyte count of 1060 × 109/L. Clinical chemistry results could not be provided due to excessive hemolysis. She was admitted to the ICU where she received several units of plasma, thrombocytes, and erythrocytes, raising her Hb to 4.8 mmol/L. Because blood cultures came back positive for C. perfringens and gram-positive cocci, ceftriaxone was added. During the night, her Hb dropped to 2.3 mmol/L and the patient unexpectedly died from circulatory failure. Upon autopsy, 2 L of blood were found in the abdominal and thoracic cavities resulting from perforation of the right atrium due to necrosis. Additionally, gas lesions were found in the liver, most likely due to C. perfringens infection.
The pathophysiology of C. perfringens infection results from release of alpha-toxin (phospholipase C), which binds to phospholipid membranes [6], hydrolyzing phospholipids into fatty acids, leading to membrane damage and cell lysis. In vascular smooth muscle and endothelium, the released free fatty acids induce leukotriene, prostaglandin, and thromboxane production, causing local vasoconstriction and coagulation to create an anaerobic environment for bacterial proliferation. Additional anaerobic fermentation enzymes lead to gas gangrene [7]. Immediate treatment is of utmost importance for a chance of survival [1]. Treatment includes antimicrobial therapy and support of vital functions, and preferentially also surgical removal of the focus, if known [1], [4].
The most obvious laboratory finding in both cases was excessive hemolysis. The plasma had turned dark brown-red and samples were automatically flagged as immeasurable due to free hemoglobin interference. On the Roche Cobas and Siemens Vista platforms, this occurs when the ‘hemolytic index’ is higher than the allowed set value [8]. Hemolytic samples in itself are not rare and may occur in vitro in up to 1–10% of all samples due to pre-analytical factors related to blood drawing, specimen handling and storage, without any underlying disease [9]. However, extreme hemolysis is unlikely to be caused by pre-analytical factors. Hence, the occurrence of intravascular hemolysis of this magnitude should be reported to the clinician immediately.
Besides interference on clinical chemistry analyzers, free Hb also leads to erroneous results in hematology analyzers. Both Siemens Advia 2120i (Siemens Healthineers, Erlangen, Germany; Case A) and Sysmex XN1000 analyzers (Sysmex Corporation, Kobe, Japan; Case B) measure Hb after lysis of erythrocytes in vitro. By default, any free Hb already present due to in vivo hemolysis is indistinguishable from intracellular Hb. Recently, both Siemens and Sysmex introduced calculated intracellular Hb concentrations with proprietary algorithms via erythrocyte forward scatter characteristics [10]. In case A, the conventionally measured total Hb concentration was substantially different from the calculated intracellular Hb: 5.6 mmol/L vs. 1.6 mmol/L, respectively. After visually inspecting the hematocrit in a centrifuged tube, the result of 1.6 mmol/L was reported to the clinician. Similarly, in case B the Hb concentration as measured conventionally was 6.0 mmol/L, while the calculated intracellular Hb was 2.0 mmol/L after in vivo hemolysis had started. This low Hb was confirmed by replacing the hemolytic plasma with saline and subsequently measuring the total Hb. Hence, these calculated intracellular Hb results proved to be indispensable in assessing the severity of both patients’ conditions.
The free Hb originated from erythrocytes affected by the alpha-toxin, which causes profound morphologic changes and hemolysis [6]. Initially, erythrocytes start leaking, then lose their biconcave shape and ultimately fall apart. Both the leakage of cytoplasm and membrane rearrangement progressively lead to smaller cell diameters and a spherical cell shape [1], [4], [5]. In a blood smear, these changes can be spherocytes and marked anisocytosis can be recognized. Ultimately, small, Hb-deprived cells, may be seen as ‘ghost cells’ in a peripheral blood smear, although they are easily missed if not specifically paid attention to (Figure 2). Fortunately, these morphological changes can be recognized on hematology analyzers as well. Unusual microcytic populations where found in the RBC histograms of both patients (Figure 1A). These small erythrocytes, i.e., ghost cells, were counted as thrombocytes in patient B, leading to a falsely high platelet count of 1060 × 109/L. Additionally, spherocytes and ghost cells showed up in characteristic locations in the scattergrams for optical platelet and reticulocyte counts (Figure 1B and C). These cytometry results could help automated identification of ghost cells.
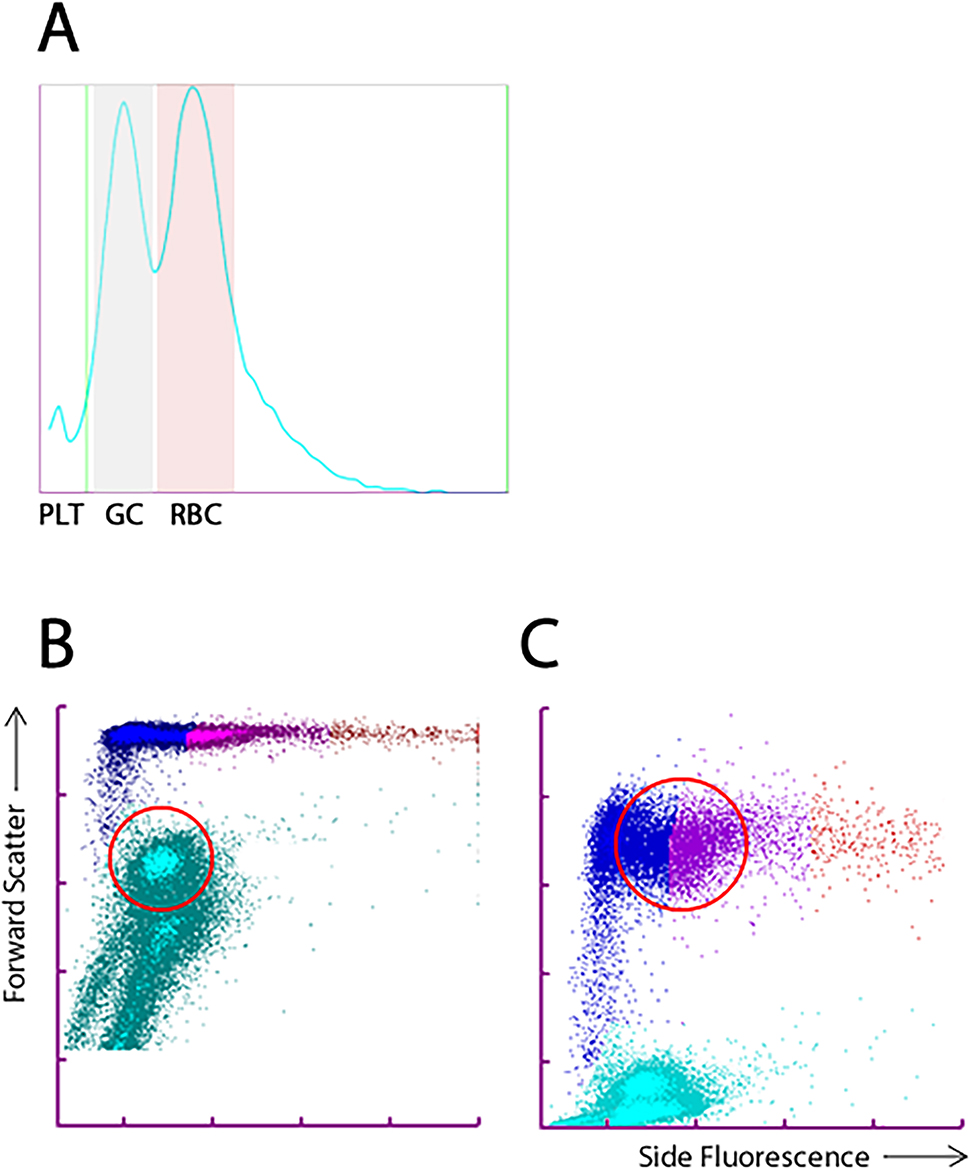
Sysmex XN1000 hematology analyzer results during Clostridium perfringens sepsis.
(A) Histograms illustrating a microcytic population of erythrocytes (ghost cells) in case B. Similar histograms were seen in case A on the Siemens Advia 2120i. (B) The ghost cells (encircled) were misidentified as platelets due to their reduced size in the optical platelet count. (C) The spherocytes (encircled) showed a marked interaction with the polymethine dye used in the reticulocyte channel, leading to misidentification as mature reticulocytes. One would normally expect to find predominantly young reticulocytes (orange population on the far right) in severe hemolysis. Abbreviations: PLT, platelets; GC, ghost cells; RBC, red blood cells.

Ghost cells as a result of the Clostridium perfringens alpha toxin in case B (arrows).
The picture on the right was edited to increase visibility of these perforated, microcytic erythrocytes.
Summarizing, massive hemolysis (e.g. dark-red plasma, interference on chemistry platforms), ghost cells in peripheral blood smears and distinct microcytic erythrocyte populations (resulting in falsely elevated platelet counts) may occur as indirect indicators of a C. Perfringens sepsis. Timely recognition of these telltale signs and contact with the physician may aid early diagnosis and treatment of C. perfringens sepsis long before blood culture results are available.
Acknowledgments
Annemarieke Loot and Cock Bank (Admiraal De Ruyter Ziekenhuis, Goes) are gratefully acknowledged for fruitful discussions and review of the manuscript. Claudia Wienefoet (Product Manager Hematology, Sysmex Netherlands) is gratefully acknowledged for helping with hematology data interpretation.
-
Research funding: None declared.
-
Author contributions: BS and MWH wrote the first draft of the manuscript. All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Competing interests: Authors state no conflict of interest.
-
Informed consent: Both patients involved passed away, therefore no written informed consent was obtained.
-
Ethical approval: Research involving human subjects complied with all relevant national regulations, institutional policies and is in accordance with the tenets of the Helsinki Declaration (as revised in 2013), and has been approved by the authors’ Institutional Review Board (NLx) or equivalent committee.
References
1. Simon, TG, Bradley, J, Jones, A, Carino, G. Massive intravascular hemolysis from clostridium perfringens septicemia: a review. J Intensive Care Med 2014. https://doi.org/10.1177/0885066613498043.Suche in Google Scholar PubMed
2. Kocarev, M, Girn, Z, Collyer, TC, Swindells, S. Uterine clostridial myonecrosis after thermal balloon endometrial ablation. Obstet Gynecol 2012. https://doi.org/10.1097/aog.0b013e31825a725d.Suche in Google Scholar PubMed
3. Leeda, M, van der Sloot, JAP. Massive haemolysis: a rare manifestation of sepsis due to Clostridium perfringens. Ned Tijdschr Geneeskd 2006.Suche in Google Scholar
4. van Bunderen, CC, Bomers, MK, Wesdorp, E, Peerbooms, P, Veenstra, J. Clostridium perfringens septicaemia with massive intravascular haemolysis: a case report and review of the literature. Neth J Med 2010.Suche in Google Scholar
5. Ohtani, S, Watanabe, N, Kawata, M, Harada, K, Himei, M, Murakami, K. Massive intravascular hemolysis in a patient infected by Clostridium perfringens. Acta Med Okayama 2006. http://doi.org/10.18926/AMO/30725.Suche in Google Scholar
6. Jewell, SA, Titball, RW, Huyet, J, Naylor, CE, Basak, AK, Gologan, P, et al. Clostridium perfringens α-toxin interaction with red cells and model membranes. Soft Matter 2015. https://doi.org/10.1039/c5sm00876j.Suche in Google Scholar PubMed
7. Awad, MM, Ellemor, DM, Boyd, RL, Emmins, JJ, Rood, JI. Synergistic effects of alpha-toxin and perfringolysin O in Clostridium perfringens-mediated gas gangrene. Infect Immun 2001. https://doi.org/10.1128/iai.69.12.7904-7910.2001.Suche in Google Scholar
8. Lippi, G, Favaloro, EJ, Franchini, M. Haemolysis index for the screening of intravascular haemolysis: a novel diagnostic opportunity? Blood Transfus 2018;16:433–7. https://dx.doi.org/10.2450/2018.0045-18.Suche in Google Scholar
9. Liu, D, Li, YX, Huang, Y. The prevalence of hemolysis - A survey using hemolysis index. Clin Chem Lab Med 2017;55:e90–1. https://dx.doi.org/10.1515/cclm-2016-0698.10.1515/cclm-2016-0698Suche in Google Scholar PubMed
10. Bauer, N, Moritz, A. Evaluation of three methods for measurement of hemoglobin and calculated hemoglobin parameters with the ADVIA 2120 and ADVIA 120 in dogs, cats, and horses. Vet Clin Pathol 2008. https://doi.org/10.1111/j.1939-165X.2008.00039.x.Suche in Google Scholar PubMed
© 2020 Bob Smit et al., published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.
Artikel in diesem Heft
- Frontmatter
- Editorial
- Biotin interference in cardiac troponin immunoassay – where the wild things are?
- Review
- Laboratory-related issues in the measurement of cardiac troponins with highly sensitive assays
- Mini Review
- Chromatographic methods development for clinical practice: requirements and limitations
- Opinion Paper
- Harmonising EQA schemes the next frontier: challenging the status quo
- Genetics and Molecular Diagnostics
- Direct comparison study between droplet digital PCR and a combination of allele-specific PCR, asymmetric rapid PCR and melting curve analysis for the detection of BRAF V600E mutation in plasma from melanoma patients
- A novel mitochondrial m.14430A>G (MT-ND6, p.W82R) variant causes complex I deficiency and mitochondrial Leigh syndrome
- Obesity status modifies the association between rs7556897T>C in the intergenic region SLC19A3-CCL20 and blood pressure in French children
- General Clinical Chemistry and Laboratory Medicine
- Influence of reagent lots and multiple measuring systems on estimating the coefficient of variation from quality control data; implications for uncertainty estimation and interpretation of QC results
- Electrophoretic α1-globulin for screening of α1-antitrypsin deficient variants
- A continued method performance monitoring approach for the determination of pediatric renin samples – application within a European clinical trial
- Pilot study for cystic fibrosis neonatal screening: the Cuban experience
- Validation of the analytical performance of the NOVEOS™ System, a system which improves upon the third-generation in vitro allergy testing technology
- IgE cross-reactivity measurement of cashew nut, hazelnut and peanut using a novel IMMULITE inhibition method
- Sexual dimorphism in the cerebrospinal fluid total protein content
- Current state of the morphological assessment of urinary erythrocytes in The Netherlands: a nation-wide questionnaire
- Reference Values and Biological Variations
- Within-subject and between-subject biological variation of first morning void urine amino acids in 12 healthy subjects
- Proenkephalin as a new biomarker for pediatric acute kidney injury – reference values and performance in children under one year of age
- Hematology and Coagulation
- Quality performance for indirect Xa inhibitor monitoring in patients using international external quality data
- Cardiovascular Diseases
- Clinical risk assessment of biotin interference with a high-sensitivity cardiac troponin T assay
- Short- and long-term biological variation of cardiac troponin I in healthy individuals, and patients with end-stage renal failure requiring haemodialysis or cardiomyopathy
- Infectious Diseases
- Monocyte distribution width (MDW) as a screening tool for sepsis in the Emergency Department
- Performance of a Toxo IgM prototype assay for the diagnosis of maternal and congenital Toxoplasma infections
- Letters to the Editors
- Evaluation of an ELISA for SARS-CoV-2 antibody testing: clinical performances and correlation with plaque reduction neutralization titer
- Preliminary evaluation of Roche Cobas Elecsys Anti-SARS-CoV-2 chemiluminescence immunoassay
- Hypoalbuminemia and elevated D-dimer in COVID-19 patients: a call for result harmonization
- Total pathway to method validation
- Derivation of performance specifications for uncertainty of serum C-reactive protein measurement according to the Milan model 3 (state of the art)
- FGF23 measurement in burosumab-treated patients: an emerging treatment may induce a new analytical interference
- Use of a modified IDS-ISYS intact PTH assay for intraoperative PTH measurements
- Agreement of dried blood spot lyso-Gb3 concentrations obtained from different laboratories in patients with Fabry disease
- Influence of delayed separation of plasma from whole blood and centrifugation protocol on Zn plasma concentration
- A survey of order of draw on inpatient wards and adherence to EFLM-COLABIOCLI recommendations
- Successful implementations of automated minimum re-test intervals to overcome ferritin over-requesting in a Spanish hospital laboratory
- Remarkable pseudoleucocytosis induced by mild cryoglobulinemia
- Massive hemolysis due to Clostridium perfringens: a laboratory’s perspective
Artikel in diesem Heft
- Frontmatter
- Editorial
- Biotin interference in cardiac troponin immunoassay – where the wild things are?
- Review
- Laboratory-related issues in the measurement of cardiac troponins with highly sensitive assays
- Mini Review
- Chromatographic methods development for clinical practice: requirements and limitations
- Opinion Paper
- Harmonising EQA schemes the next frontier: challenging the status quo
- Genetics and Molecular Diagnostics
- Direct comparison study between droplet digital PCR and a combination of allele-specific PCR, asymmetric rapid PCR and melting curve analysis for the detection of BRAF V600E mutation in plasma from melanoma patients
- A novel mitochondrial m.14430A>G (MT-ND6, p.W82R) variant causes complex I deficiency and mitochondrial Leigh syndrome
- Obesity status modifies the association between rs7556897T>C in the intergenic region SLC19A3-CCL20 and blood pressure in French children
- General Clinical Chemistry and Laboratory Medicine
- Influence of reagent lots and multiple measuring systems on estimating the coefficient of variation from quality control data; implications for uncertainty estimation and interpretation of QC results
- Electrophoretic α1-globulin for screening of α1-antitrypsin deficient variants
- A continued method performance monitoring approach for the determination of pediatric renin samples – application within a European clinical trial
- Pilot study for cystic fibrosis neonatal screening: the Cuban experience
- Validation of the analytical performance of the NOVEOS™ System, a system which improves upon the third-generation in vitro allergy testing technology
- IgE cross-reactivity measurement of cashew nut, hazelnut and peanut using a novel IMMULITE inhibition method
- Sexual dimorphism in the cerebrospinal fluid total protein content
- Current state of the morphological assessment of urinary erythrocytes in The Netherlands: a nation-wide questionnaire
- Reference Values and Biological Variations
- Within-subject and between-subject biological variation of first morning void urine amino acids in 12 healthy subjects
- Proenkephalin as a new biomarker for pediatric acute kidney injury – reference values and performance in children under one year of age
- Hematology and Coagulation
- Quality performance for indirect Xa inhibitor monitoring in patients using international external quality data
- Cardiovascular Diseases
- Clinical risk assessment of biotin interference with a high-sensitivity cardiac troponin T assay
- Short- and long-term biological variation of cardiac troponin I in healthy individuals, and patients with end-stage renal failure requiring haemodialysis or cardiomyopathy
- Infectious Diseases
- Monocyte distribution width (MDW) as a screening tool for sepsis in the Emergency Department
- Performance of a Toxo IgM prototype assay for the diagnosis of maternal and congenital Toxoplasma infections
- Letters to the Editors
- Evaluation of an ELISA for SARS-CoV-2 antibody testing: clinical performances and correlation with plaque reduction neutralization titer
- Preliminary evaluation of Roche Cobas Elecsys Anti-SARS-CoV-2 chemiluminescence immunoassay
- Hypoalbuminemia and elevated D-dimer in COVID-19 patients: a call for result harmonization
- Total pathway to method validation
- Derivation of performance specifications for uncertainty of serum C-reactive protein measurement according to the Milan model 3 (state of the art)
- FGF23 measurement in burosumab-treated patients: an emerging treatment may induce a new analytical interference
- Use of a modified IDS-ISYS intact PTH assay for intraoperative PTH measurements
- Agreement of dried blood spot lyso-Gb3 concentrations obtained from different laboratories in patients with Fabry disease
- Influence of delayed separation of plasma from whole blood and centrifugation protocol on Zn plasma concentration
- A survey of order of draw on inpatient wards and adherence to EFLM-COLABIOCLI recommendations
- Successful implementations of automated minimum re-test intervals to overcome ferritin over-requesting in a Spanish hospital laboratory
- Remarkable pseudoleucocytosis induced by mild cryoglobulinemia
- Massive hemolysis due to Clostridium perfringens: a laboratory’s perspective


