Abstract
Background and aims
Real-life data on laxative use in patients suffering from opioid-induced constipation (OIC) are very limited, and many OIC patients are only using over the counter laxatives to resolve their constipation. Our aim was to describe laxative utilization and quality of life in participants in Norway who ever experienced OIC.
Methods
This was a cross-sectional online survey conducted between 27th of June and 3rd of July 2014 among participants above 18 years with self-reported OIC and who had agreed to receive information from the pharmacy chain (Boots A/S, Norway). The questionnaire comprised a series of multiple choice, close-ended, and free text questions on abdominal symptoms, laxative use and health-related quality of life.
Results
A total of 417 participants met the study eligibility criteria: (1) treated with opioid for a minimum of 4 weeks, (2) actively accepted participation, and (3) confirmed ever experiencing OIC and in addition completed the survey. Among the eligible participants, 86% were females, 85% were younger than 60 years of age, and 57% were currently suffering OIC. More than half of the currently constipated participants were experiencing moderate to very severe abdominal bloating (63%), abdominal pain (55%) and/or pain during bowel movement (50%). Less than every fourth participant (23%) had consulted health care professionals (HCPs) about their constipation. Up to 39% reported that they handled their OIC by self-management, e.g., bought laxative, reduced the dose and/or changed opioid without consulting HCP or pharmacy. Less than half (48%) of the laxative users were satisfied with the laxative they were using to relieve their constipation. The EQ-5D health-related quality of life score was mean (SD): 0.587 (0.272). Although not statistically significant (p = 0.067), there was a tendency of lower quality of life among the participants who were currently constipated compared with those not currently constipated (difference of mean EQ-5D: 0.629-0.555 = 0.074). A significantly lower (p = 0.001) quality of life was found among participants who were dissatisfied with their laxative [mean (SD): 0.424 (0.350)] than among those who were satisfied or neither satisfied nor dissatisfied [mean (SD): 0.628 (0.235) and 0.673 (0.155), respectively].
Conclusions
The results suggest a high degree of moderate to very severe abdominal symptoms, a high degree of self-management of opioid-induced constipation, a low degree of satisfaction with laxative, and low health-related quality of life of patients suffering from chronic pain necessitating long-term opioid treatment, subsequent constipation and laxatives use.
Implications
Patients suffering from OIC with low quality of life and remaining symptoms despite use of two or more laxatives are a vulnerable patient group in need of optimized healthcare management, who also might benefit from more specific and innovative therapy.
1 Introduction
Constipation is a well-known and common side-effect of opioid treatment in patients with moderate-to-severe pain. Between 40 and 70% of chronic opioid users suffer from opioid induced constipation (OIC) [1, 2, 3, 4, 5].
A majority of patients experiencing symptoms of OIC, report that the OIC has negative impact on their general quality of life and every day activities [6, 7, 8]. In a recent study, more than 70% of the patients who receive opioids due to musculoskeletal pain, reported that they had not been informed about the risk of experiencing/developing OIC as a treatment side-effect [9]. Additionally, one-third of the patients had skipped doses, reduced or stopped their use of opioid therapy in order to resolve their gastrointestinal side effects, resulting in increased experience of pain for more than 90% of these patients [6].
Real-life data on laxative utilization among patients suffering from OIC are very limited, and many patients suffering from OIC are only using over the counter laxatives to resolve their constipation.
In this cross-sectional survey study, the aim was to describe laxative utilization and quality of life in participants who ever experienced OIC.
2 Method
2.1 Study design and sample
This is a cross-sectional survey study among participants experiencing self-reported OIC. The online survey was conducted in collaboration with a pharmacy chain (Boots A/S, Norway), administering the survey via e-mail to more than 82,000 individuals who had indicated an interest in receiving general information from the pharmacy. Participants had to (1) confirm that they had been on opioid therapy for a minimum of 4 weeks with an expectation to continue for at last 3 months (to ensure participants were consistently treated with opioid e.g. not acute injury or post-surgical use), (2) actively accept participation in the study to get online access to the self-reported questionnaire, and (3) the participants had to confirm ever experiencing constipation while on opioid therapy. The study eligibility criteria are presented in Table 1.
Study eligibility criteria.
| Opioid therapy ≥4 weeks with the expectation to continue for at last 3 months (target population) | Participants who confirmed used of one or more of the specified opioid therapies |
| Tramadol hydrochloride, tramadol hydrochloride/paracetamol | |
| Oxycodone hydrochloride | |
| Oxycodone hydrochloride, naloxone | |
| Morphine, hydromorphone | |
| hydrochloride, morphine sulphate, morphine sulphate pentahydrate | |
| Burprenorphine | |
| Methadone hydrochloride | |
| Codein/paracetamol | |
| Ketobemidone | |
| Pethidine hydrochloride | |
| Fentanyl | |
| OIC (criteria for confirmation ofstudy eligibility) | Participants who respond “yes” to the question “have you ever experienced constipations while on opioid therapy such as less than three BM pr. week, bloating or pain in abdomen, BM too hard or straining/squeezing BM” |
-
OIC: opioid induced constipation; BM: bowel movements
2.2 Data collection
All participants were informed that participation was voluntary and anonymous, and they gave consent to the collection, use, and disclosure of their online response. No data were collected that potentially could identify a person such as date of birth, name or personal identification number. The online survey took approximately 10 min to complete and comprised a series of multiple choice, close-ended, and free text questions which was divided in two parts, symptoms and treatment and health related quality of life. Data were collected between 27th of June 2014 and 3rd ofJuly 2014.
Initially, eligible participants were asked if they were currently experiencing constipation while on opioid therapy, those who confirmed current constipation were then asked to evaluate the severity (no, mild, moderate, severe or very severe) of the following three common symptoms of OIC: abdominal pain, abdominal bloating, and pain on/during bowel movements.
Eligible participants were asked about management of their OIC, and their responses were categorized into: consulted health care professional (HCP; e.g., physician or nurse); consulted pharmacy without contacting HCP; self-management (e.g., bought over-the- counter laxative, reduced dose of opioid, changed opioid, or other) without contacting a HCP or pharmacy; or other/did nothing.
Participants who reported that they consulted a HCP or a pharmacy were then asked if they were advised to buy laxative with or without a prescription.
Prescribed laxative users were defined as those who were advised by a HCP or pharmacy to buy prescribed laxative.
Non-prescribed laxative users were defined as those who were advised by HCP or pharmacy to buy laxative without prescription and those who bought laxative without contacting a HCP or a pharmacy.
Both prescribed and non-prescribed laxative users were asked to specify what type of laxatives they bought: macrogol 3350/potassium chloride/sodium bicarbonate/sodium chloride, lactulose, bisacodyl, senna, ispaghula, other. Further, all laxative users were categorized according to number of different brands of laxatives used (one laxative, two or more laxatives), frequency of laxative use (daily; 6-3 days/week; 1-2 days/week; <1 day/week), and self-rated satisfaction with laxative on a 5-point scale from very satisfied to very dissatisfied.
Health related quality of life was assessed by means of the Euro- QOL 5 Dimensions (EQ-5D) [10] which is a validated 5-item health state descriptive system where full health is one, and zero is equivalent to death (EQ-5D index) and a visual analogue scale (EQ-5D VAS, range 0-100 from worst to best imaginable health state).
2.3 Statistical methods
Continuous variables are presented as means and standard deviations and categorical variables as absolute and relative frequencies. Statistical comparisons were made using analysis of variance (ANOVA) for continuous variables and chi-square test for categorical variables. The significance level is set at 5% but as no adjustment for multiplicity has been performed the p-values should be considered as exploratory.
2.4 Ethical conduct
An opinion was obtained from Regional Committees for Medical and Health Research Ethics (REC) in writing (reference number: 2013/2405 D) stating that the project did not need to be submitted to ethics Committee due to its design and purpose.
3 Results
A total of 910 participants confirmed that they had been treated with opioids for a minimum of 4 weeks with the expectation to continue for at least 3 months. About half of the participants (n = 445) confirmed that they had at some point experienced OIC and therefore were eligible for data analysis. Excluding 28 participants who did not complete the survey, this study counted 417 eligible participants who completed the first part of the survey.
Among the 417 eligible participants who reported ever experienced OIC, 86% were females and 85% were younger than 60 years old (Table 2). Further, more than half of the participants (57%) were currently suffering constipation while on opioid therapy (Table 2). The participants responded to questions regarding how they managed their OIC, and less than every fourth participant (23%) had consulted health care professional (i.e., physician or nurse). Thirty-nine percent reported that they handled their OIC by self-management, e.g., bought laxative, reduced the dose and/or changed opioid without consulting HCP or pharmacy. Twenty-three percent reported that they had used two or more laxatives, 34% had used one laxative, and 43% had not used laxative.
Characteristics of participants who have experienced OIC, n = 417.
| Total, n(%) | |
|---|---|
| Gender | |
| Males | 58 (13.9) |
| Females | 359 (86.1) |
| Age, years | |
| 18-39 | 165 (39.6) |
| 40-59 | 189 (45.3) |
| ≥60 | 63 (15.1) |
| Currently constipated | |
| Yes | 239 (57.3) |
| No | 178 (42.7) |
| Management of OIC | |
| Consulted HCP | 96 (23.0) |
| Consulted pharmacy | 41 (9.8) |
| Self-management | 162 (38.8) |
| Other or nothing | 118 (28.3) |
| Use of laxative | |
| No laxative | 181 (43.4) |
| One laxative | 142 (34.1) |
| Two or more laxatives | 94 (22.5) |
The most frequently used opioid therapy was codein/paracetamol followed by tramadol hydrochloride, tramadol hydrochloride/paracetamol (Fig. 1). The most frequently used laxative was lactulose followed by bisacodyl (Fig. 2).
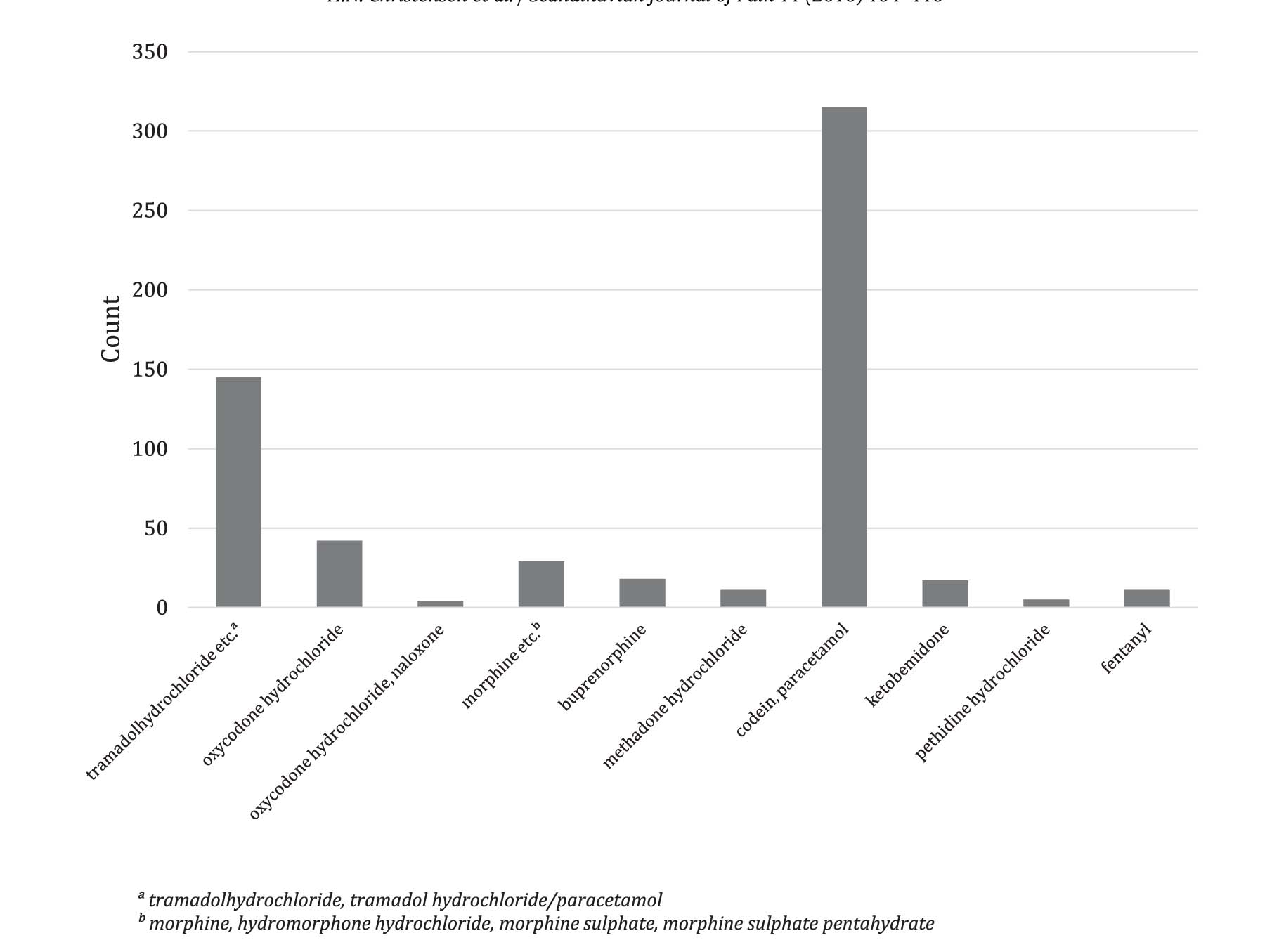
Frequency of different types of opioid therapy used among participants who ever experienced OIC, n = 417.a Tramadolhydrochloride, tramadol hydrochloride/paracetamol.b Morphine, hydromorphone hydrochloride, morphine sulphate, morphine sulphate pentahydrate.

Frequency of different types of laxatives used among participantswhoever experienced OIC and had used laxative, n = 236.a Macrogol 3350/potassium chloride/sodium bicarbonate/sodium chloride.
More than half of the 239 particpants on opioid therapy who were currently constipated were experiencing moderate to very severe symptoms related to OIC. Severe to very severe symptoms were observed in 16% suffering from abdominal bloating, 12% suffered from pain during bowel movement, and 8% who had abdominal pain. The symptom burden was more prevalent in currently constipated participants using laxatives compared to non-laxative users (Fig. 3). The most pronounced difference in prevalence of moderate to very severe symptom was found for abdominal bloating when comparing participants using no (46%), one (64%), and two or more laxatives (90%) (p < 0.05).
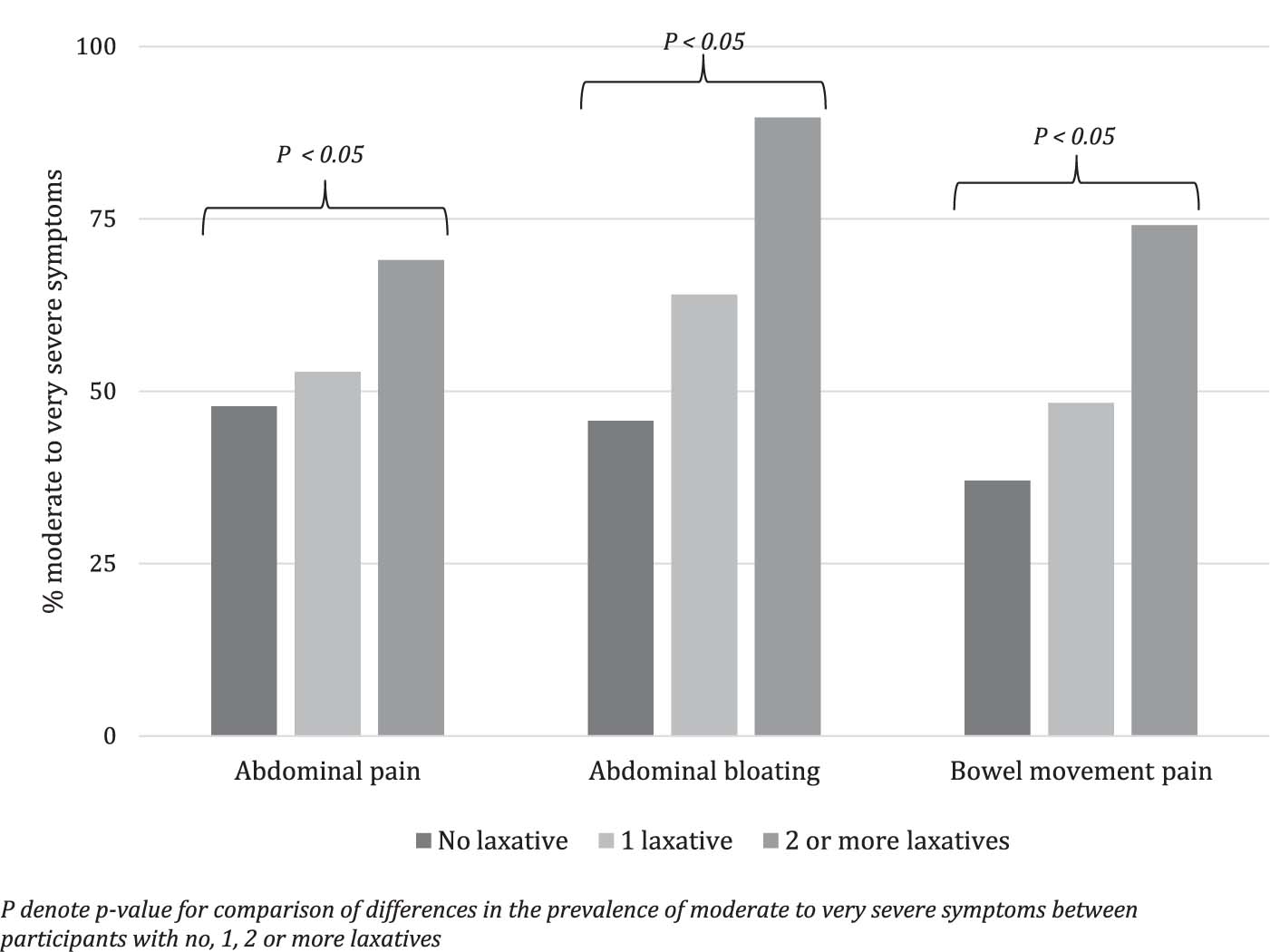
Prevalence of moderate to very severe symptoms in participants currently constipated while on opioid therapy according to laxative use, n = 239. p-Value give for comparison of differences in the prevalence of moderate to very severe symptoms between participants with no, one, two or more laxatives.
The laxative utilization among the 236 laxative users who ever experienced OIC is presented in Table 3. Twelve percent of the laxative users reported that they purchased laxative which was prescribed by their HCP. Almost two of three (62%) prescribed laxative users reported that they had tried only one laxative. However, it was reported that more than one-third (34%) of the prescribed laxatives users had previously tried non-prescribed laxative. Participants using two or more laxatives were generally using them more frequently than those using only one laxative (daily use of laxative: 21% and 6%, respectively). Less than half (48%) of the laxative users were satisfied with the laxative they were using, one-third (34%) were neither satisfied or dissatisfied, and about one-fourth (18%) reported that they were dissatisfied with the laxative they were using.
Treatment utilization among laxative users who ever experienced OIC, n = 236.
| One laxative (n =142) | Two or more laxatives (n = 94) | Total (n = 236) | p-Value[*] | |
|---|---|---|---|---|
| Laxatives, n (row %) | 0.037 | |||
| Prescribed laxatives | 15 (78.9) | 4 (21.1) | 19 (100) | |
| Both prescribed and non-prescribed laxative | 3 (30.0) | 7 (70.0) | 10 (100) | |
| Non-prescribed laxatives | 124 (59.9) | 83 (40.1) | 207 (100) | |
| Laxative frequency, n (column %) | 0.001 | |||
| Daily | 9 (6.3) | 20 (21.3) | 29 (12.3) | |
| 6-3 days/week | 19 (l3.4) | 9 (9.6) | 28 (11.9) | |
| 1-2 days/week | 25 (l7.6) | 24 (25.5) | 49 (20.8) | |
| <1 day/week | 89 (62.7) | 41 (43.6) | 130 (55.1) | |
| Satisfaction with laxative, n (column %) | 0.388 | |||
| Satisfied | 72 (50.7) | 42 (44.7) | 114 (48.3) | |
| Neither satisfied or dissatisfied | 48 (33.8) | 31 (33.0) | 79 (33.5) | |
| Dissatisfied | 22 (15.5) | 21 (22.3) | 43 (18.2) |
The response rate for the second part of the survey decreased due to technical issues (users of iOS (Ipad and Iphone) were not able to get access to EQ5-D questionnaire), therefore only 188 of the eligible participants were able to answer the items on health- related quality of life. The EQ-5D index and the EQ-5D VAS score according to currently constipated, use of laxative, prescription, laxative frequency, and satisfaction are presented in Table 4. The mean EQ-5D index score was 0.587 (SD: 0.272) and the mean EQ-5D VAS score was 60.7 (SD: 22.6). Although not statistically significant (p = 0.067), there was a tendency of lower health-related quality of life among the participants who were currently constipated compared to those not currently constipated (difference of means: 0.629-0.555 = 0.074). The lowest health-related quality of life was found among participants who were dissatisfied with their laxative (mean EQ-5D index: 0.424; mean EQ-5D VAS score: 46.1), and statistically significant lower than for those who were satisfied and those who were neither satisfied nor dissatisfied with laxative (EQ-5D index: p = 0.001 and EQ-5D VAS score: p = 0.004).
Treatment utilization among laxative users who ever experienced OIC, n = 236.
| n | EQ-5D index Mean (SD) | p-Value[*] | EQ-5D VAS score Mean (SD) | p-Valuee[*] | |
|---|---|---|---|---|---|
| Total | 188 | 0.587 (0.272) | 60.7 (22.6) | ||
| Currently constipated | 0.067 | 0.206 | |||
| Yes | 107 | 0.555 (0.296) | 58.9 (22.6) | ||
| No | 81 | 0.629 (0.231) | 63.1 (22.6) | ||
| Use of laxative | 0.422 | 0.057 | |||
| No laxative | 79 | 0.566 (0.292) | 61.7 (23.7) | ||
| One laxative | 70 | 0.621 (0.271) | 63.8 (21.9) | ||
| Two or more laxatives | 39 | 0.568 (0.228) | 53.3 (20.6) | ||
| Prescription | 0.775 | 0.153 | |||
| Prescribed | 10 | 0.636 (0.409) | 72.6 (26.8) | ||
| Both prescribed and non-prescribed | 4 | 0.671 (0.219) | 54.8 (34.1) | ||
| Non-prescribed | 95 | 0.596 (0.240) | 58.9 (20.7) | ||
| Laxative frequency | 0.448 | 0.004 | |||
| Daily | 13 | 0.497 (0.217) | 40.7 (22.2) | ||
| 6-3 days/week | 12 | 0.626 (0.240) | 59.5 (19.4) | ||
| 1-2 days/week | 20 | 0.636 (0.232) | 67.8 (21.7) | ||
| <1 day/week | 64 | 0.608 (0.273) | 61.6 (20.6) | ||
| Satisfaction with laxative | 0.001 | 0.004 | |||
| Satisfied with laxative | 56 | 0.628 (0.235) | 62.3 (22.6) | ||
| Neither satisfied or dissatisfied with laxative | 32 | 0.673 (0.155) | 65.2 (17.8) | ||
| Dissatisfied with laxative | 21 | 0.424 (0.350) | 46.1 (21.1) |
-
SD: standard deviation; VAS: Visual Analogue Scale (0-100), lower score indicate worse health state; EQ-5D: EuroQoL 5 dimension index (0-1, with 1 = full health), lower score indicates worse generic QoL
4 Discussion
The results from this cross-sectional survey study among participants experiencing OIC suggest a high degree of moderate to very severe abdominal symptoms, a high degree of self-management of OIC, a relatively low degree of satisfaction with laxatives, and low health-related quality of life, especially among those using more laxatives and using laxatives more often.
Our results show that more than half of the currently constipated participants reported having moderate to very severe abdominal symptoms (i.e., pain in abdomen, pain during bowel movement, and abdominal bloating). This finding was similar to the prevelence of these symptoms reported by Coyne et al. [7] in a sample of patients recruited from primary care clinics. Some of these common abdominal symptoms, particularly bloating, might also occur as side effects of several classes of laxatives [11]. The high usage of over-the-counter lactulose in Norway is especially an unfortunate tradition because of its high prevalence of its adverse effects bloating and abdominal discomfort and even abdominal pain. Indeed, the symptom burden was more prevalent in laxative users than in non-laxative users in our study, particulary abdominal bloating among participants who have used two or more laxatives. However, the relatively high prevalence of these symptoms might also suggest that for the participants who have used two or more laxatives the currently utilized laxative therapies may be lacking in efficacy and tolerability as well as there is a possibility that participants who are not using laxatives are undertreating their OIC. In a recent longitudinal study by Coyne et al. [12] with prospective data from US, Canada, Germany, and UK it was estimated that more than one of four participants was a sufficient laxative user but at the same time inadequate laxative responders, defined as <3 bowel movements or ≥1 moderate to very severe constipation symptom.
Self-management of OIC was frequent among the participants in our study. More than two out of five participants reported that in order to handle their OIC they had bought laxative, reduced the daily dose and/or changed opioid without consulting their HCP or pharmacy, which is consistent with the proportion reported by Bell et al. (35%) [6] and Cook et al. (27%) [13]. In a recent Danish crosssectional study among patients filling prescriptions for opioids at a community pharmacy, Pottegård et al. [9] concluded that only few of the participants (28%) recalled having had information on potential constipation caused by opioid and having received any recommendation on how to use laxatives to prevent constipation. The fact that relatively few (23%) of the participants in our study had consulted their physician or nurse regarding how to manage their OIC imply that they might be unaware of recent advances in therapeutic approaches for OIC to manage and prevent OIC without compromising analgesic efficacy [14].
Furthermore, our results show that less than half (48%) of the laxative users were satisfied with their laxative and almost one-quarter reported dissatisfaction with the laxative they were using, which is consistent with the proportion reported in Cook et al. [13].
Generally the health-related quality of life (QoL) reported by the participants in our study was relatively low with a mean EQ- 5D index score of 0.587. Our results support the finding reported by Brazier et al. [15] in a sample of seven different patient groups (chronic obstructive airways disease, osteoarthritis, irritable bowel syndrome, lower back pain, leg ulcers, post-menopausal women and elderly) in UK, in which the overall mean EQ-5D index score was 0.586. However, in that study the mean EQ-5D index score varied across the seven patient/population groups from 0.442 in osteoporosis patients to 0.729 in menopausal women. In the study by Coyne et al. [7] evaluating currently constipated opioid users, the mean EQ-5D index score varied across the four country-specific samples from 0.270 in UK to 0.610 in Canada. A number of studies have shown that patients with constipation report lower QoL than non-constipated individuals [16, 17, 18, 19] which is consistent with our results, although not statistically significant, participants who were currently constipated had a lower QoL than those who were not currently constipated (mean EQ-5D index score 0.555 and 0.629, respectively). In addition, our study adds to the literature, that the lowest QoL was found among participants who were dissatisfied with their laxative and participants who used laxatives every day (mean EQ-5D index score 0.424 and 0.497, respectively). Similar patterns were reflected by the mean EQ-5D VAS.
This patient group undoubtedly will benefit from more specific therapy that is now being introduced. Peripherally acting opioid receptor antagonist (PAMORAs) has recently been documented to be effective and safe for this group of unfortunate chronic pain patients needing opioid for their pain condition [20]. Such drugs will avoid the extra burden imposed on chronic pain patients who frequently have had to use two or more types of laxatives with extra burden of side-effects/adverse effects of such laxatives.
4.1 Limitations and strengths
As with other survey based evaluations, the present study comes with some limitations to be taken into account when interpreting the results.
First, we were unable to compare the observed use of laxative among patients treated with opioids to an age-matched control group not treated with opioids.
Second, our study sample was drawn from an online database established by a pharmacy chain (Boots A/S, Norway) which could have biased the sample towards participants having a greater familiarity with the Internet and interest in receiving information from the pharmacy. Although, the age and gender distribution were skewed in favour of younger and female participants, potentially inferring low generalizability and external validity, the results still are well in accordance with previous studies on symptom burden, self-management, and quality of life in relation to OIC.
Third, the questions, except of EQ-5D, were defined for the present study only, and were thus not validated or standardized. Also, data analyzed in this study was based exclusively on self-report and may be subject to inaccuracy or recall bias.
Fourth, the participants may be taking other medications, have limited mobility or have dietary habits that contribute to constipation. Therefore, it may not be certain that the OIC symptoms found in this study are only related to opioids.
This study also comes with strengths, not the least the use of an anonymized self-administration questionnaire. This may have allowed a more honest response to sensitive questions related to symptoms and self-management of constipation as opposed to an interviewer-administration questionnaire, which may induce a social desirability response bias where the respondent seeks to please the interviewer. Further, since there are no registries in the Nordic countries capturing over the counter drug use, conducting the study via a pharmacy chain database enabled assessment of utilization of these types of easily accessible laxatives. In addition, this study not only sheds light on the prevalence and use of laxative but also explore aspects of symptoms and health-related quality of life in both non-laxative and laxative users.
5 Conclusions and implications
The results from this cross-sectional survey study among participants experiencing OIC suggest a high degree of moderate to very severe abdominal symptoms, a high degree of self-management of OIC, a low degree of satisfaction with laxatives, and low health-related quality of life of patients suffering from chronic pain necessitating long-term opioid treatment. This implies that patients suffering from OIC with low quality of life and remaining symptoms despite use of two or more laxative are a vulnerable patient group in need of optimized healthcare management, who also might benefit from more specific and innovative therapy.
Highlights
We studied laxative use and quality of life in persons with opioid-induced constipation (OIC).
417 opioid treated patients with OIC self-administered a cross-sectional online survey.
Abdominal pain and bloating were frequent as was laxative self-management of OIC.
Quality of life was low among those using several laxatives and those using laxatives daily.
DOIs of original articles: http://dx.doi.org/10.1016/j.sjpain.2016.02.003, http://dx.doi.org/10.1016/j.sjpain.2015.12.005
-
Funding: This work was supported by AstraZeneca. Project management was provided by AstraZeneca. The statistical analysis was agreed on by the study steering committee, and data analysis was performed by an independent statistical consultant company, Statisticon, for which AZ is a client. AstraZeneca took part, as members of the study steering committee, in the interpretation of the data and the drafting of the manuscript.
-
Conflicts of interest: HNC and JF are employed by AstraZeneca. HB is a physician and received financial support from AZ for his scientific consultation in interpreting this study. UO is employed by an independent statistical consultant company, Statisticon, for which AZ is a client. The authors have no other conflicts of interest in this work.
References
[1] Droney J, Ross J, Gretton S, Welsh K, Sato H, Riley J. Constipation in cancer patients on morphine. Support Care Cancer 2008;16:453–9.Search in Google Scholar
[2] Hess B, Bernardi M, Klotz HP. Attitude of Swiss physicians towards opioidinduced constipation: a national survey. EurJ Intern Med 2011;22:527–31.Search in Google Scholar
[3] Kalso E, Edwards JE, Moore RA, McQuay HJ. Opioids in chronic non-cancer pain: systematic review of efficacy and safety. Pain 2004;112:372–80.Search in Google Scholar
[4] Panchal SJ, Muller-Schwefe P, Wurzelmann JI. Opioid-induced bowel dysfunction: prevalence, pathophysiologyand burden. Int J Clin Pract 2007;61:1181–7.Search in Google Scholar
[5] Rosti G, Gatti A, Costantini A, Sabato AF, Zucco F. Opioid-related bowel dysfunction: prevalence and identification of predictive factors in a large sample of Italian patients on chronic treatment. Eur Rev Med Pharmacol Sci 2010;14:1045–50.Search in Google Scholar
[6] Bell TJ, Panchal SJ, Miaskowski C, Bolge SC, Milanova T, Williamson R. The preva-lence, severity, and impact of opioid-induced bowel dysfunction: results of a US and European Patient Survey (PROBE 1). Pain Med 2009;10:35–42.Search in Google Scholar
[7] Coyne KS, LoCasale RJ, Datto CJ, Sexton CC, Yeomans K, Tack J. Opioidinduced constipation in patients with chronic noncancer pain in the USA, Canada, Germany, and the UK: descriptive analysis of baseline patient-reported outcomes and retrospective chart review. Clinicoecon Outcomes Res 2014;6:269–81.Search in Google Scholar
[8] Boswell K, Kwong WJ, Kavanagh S. Burden of opioid-associatedgastrointestinal side effects from clinical and economic perspectives: a systematic literature review. J Opioid Manag 2010;6:269–89.Search in Google Scholar
[9] Pottegard A, Knudsen TB, van HK, Salmasi H, Schytte-Hansen S, Sondergaard J. Information on risk of constipation for Danish users of opioids, and their laxative use. Int J Clin Pharm 2014;36:291–4.Search in Google Scholar
[10] Oemar M, Janssen B. EQ-5D-5Luserguide: basic information on how to use the EQ-5D-5L instrument. Rotterdam, The Netherlands: The EuroQol Group; 2013.Search in Google Scholar
[11] Pappagallo M. Incidence prevalence, and management of opioid bowel dysfunction. AmJ Surg 2001;183:11S-8S.Search in Google Scholar
[12] Coyne KS, Margolis MK, Yeomans K, King FR, Chavoshi S, Payne KA, LoCasale RL. Opioid-induced constipation among patients with chronic noncancer pain in the United States, Canada, Germany, and the United Kingdom: laxative use, response, and symptom burden over time. Pain Med 2015.Search in Google Scholar
[13] Cook SF, Lanza L, Zhou X, Sweeney CT, Goss D, Hollis K, Mangel AW, Fehnel SE. Gastrointestinal side effects in chronic opioid users: results from a population-based survey.Aliment Pharmacol Ther 2008;27:1224–32.Search in Google Scholar
[14] Camilleri M, Drossman DA, Becker G, Webster LR, Davies AN, Mawe GM. Emerging treatments in neurogastroenterology: a multidisciplinary working group consensus statement on opioid-induced constipation. Neurogastroen- terol Motil 2014;26:1386–95.Search in Google Scholar
[15] Brazier J, Roberts J, Tsuchiya A, Busschbach J. A comparison of the EQ-5D and SF-6Dacross seven patientgroups. Health Econ 2004;13:873–84.Search in Google Scholar
[16] Dennison C, Prasad M, Lloyd A, Bhattacharyya S, Dhawan R, Coyne K. The health-related quality of life and economic burden of constipation. Pharmacoeconomics 2005;23:461–76.Search in Google Scholar
[17] Penning-van Beest FJ, van den Haak P, Klok RM, Prevoo YF, van der Peet DL, Herings RM. Quality of life in relation to constipation among opioid users. J Med Econ 2010;13:129–35.Search in Google Scholar
[18] Wald A, Scarpignato C, Kamm MA, Mueller-Lissner S, Helfrich I, Schuijt C, Bubeck J, Limoni C, Petrini O. The burden of constipation on quality of life: results of a multinational survey. Aliment Pharmacol Ther 2007;26:227–36.Search in Google Scholar
[19] Abramowitz L, Beziaud N, Labreze L, Giardina V, Causse C, Chuberre B, Allaert FA, Perrot S. Prevalence and impact of constipation and bowel dysfunction induced by strong opioids: a cross-sectional survey of 520 patients with cancer pain: DYONISOS study.J Med Econ 2013;16:1423–33.Search in Google Scholar
[20] Poulsen JL, Brock C, Olesen AE, Drewes AM. Clinical potential of naloxegol in the management of opioid-induced bowel dysfunction. Clin Exp Gastroenterol 2014;7:345–58.Search in Google Scholar
© 2016 Scandinavian Association for the Study of Pain
This work is licensed under the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Articles in the same Issue
- Editorial comment
- Psychophysiological effects of threatening a rubber hand that is perceptually embodied in healthy human subjects
- Original experimental
- A preliminary investigation into psychophysiological effects of threatening a perceptually embodied rubber hand in healthy human participants
- Editorial comment
- Analysis of C-reactive protein (CRP) levels in pain patients – Can biomarker studies lead to better understanding of the pathophysiology of pain?
- Clinical pain research
- Serum C-reactive protein levels predict regional brain responses to noxious cold stimulation of the hand in chronic whiplash associated disorders
- Editorial comment
- Importance of early diagnosis of complex regional pain syndrome (CRPS-1 and CRPS-2): Delayed diagnosis of CRPS is a major problem
- Clinical pain research
- Delayed diagnosis and worsening of pain following orthopedic surgery in patients with complex regional pain syndrome (CRPS)
- Editorial comment
- Associative learning mechanisms may trigger increased burden of chronic pain; unlearning and extinguishing learned maladaptive responses should help chronic pain patients
- Original experimental
- When touch predicts pain: predictive tactile cues modulate perceived intensity of painful stimulation independent of expectancy
- Editorial comment
- Low back pain among nurses: Common cause of lost days at work and contributing to the worldwide shortage of nurses
- Observational study
- Pain-related factors associated with lost work days in nurses with low back pain: A cross-sectional study
- Editorial comment
- Assessment of persistent pelvic pain after hysterectomy: Neuropathic or nociceptive?
- Clinical pain research
- Characterization of persistent pain after hysterectomy based on gynaecological and sensory examination
- Editorial comment
- Transmucosal fentanyl for severe cancer pain: Nasal mucosa superior to oral mucosa?
- Original experimental
- Facilitation of accurate and effective radiation therapy using fentanyl pectin nasal spray (FPNS) to reduce incidental breakthrough pain due to procedure positioning
- Editorial comment
- Why do we have opioid-receptors in peripheral tissues? Not for relief of pain by opioids
- Clinical pain research
- Peripheral morphine reduces acute pain in inflamed tissue after third molar extraction: A double-blind, randomized, active-controlled clinical trial
- Editorial comment
- Chronic pain and psychological distress among long-term social assistance recipients – An intolerable burden on those on the lowest steps of the socioeconomic ladder
- Clinical pain research
- The co-occurrence of chronic pain and psychological distress and its associations with salient socio-demographic characteristics among long-term social assistance recipients in Norway
- Editorial comment
- Fifty years on the Visual Analogue Scale (VAS) for pain-intensity is still good for acute pain. But multidimensional assessment is needed for chronic pain
- Clinical pain research
- Patient reported outcome measures of pain intensity: Do they tell us what we need to know?
- Editorial comment
- Postoperative pain documentation 30 years after
- Topical review
- Postoperative pain documentation in a hospital setting: A topical review
- Editorial comment
- Aspects of pain attitudes and pain beliefs in children: Clinical importance and validity
- Observational study
- The Survey of Pain Attitudes: A revised version of its pediatric form
- Editorial comment
- The role of social anxiety in chronic pain and the return-to-work process
- Clinical pain research
- Social Anxiety, Pain Catastrophizing and Return-To-Work Self-Efficacy in chronic pain: a cross-sectional study
- Editorial comment
- Advances in understanding and treatment of opioid-induced-bowel-dysfunction, opioid-induced-constipation in particular Nordic recommendations based on multi-specialist input
- Topical review
- Definition, diagnosis and treatment strategies for opioid-induced bowel dysfunction–Recommendations of the Nordic Working Group
- Observational study
- Opioid-induced constipation, use of laxatives, and health-related quality of life
- Editorial comment
- Migraine headache and bipolar disorders: Common comorbidities
- Systematic review
- Migraine headache and bipolar disorder comorbidity: A systematic review of the literature and clinical implications
- Editorial comment
- The role of catastrophizing in the pain–depression relationship
- Clinical pain research
- The mediating role of catastrophizing in the relationship between pain intensity and depressed mood in older adults with persistent pain: A longitudinal analysis
- Announcement
- May 26-27, 2016 Scandinavian Association for the Study of Pain, Reykjavik, Iceland May 25, 2016 PhD course
Articles in the same Issue
- Editorial comment
- Psychophysiological effects of threatening a rubber hand that is perceptually embodied in healthy human subjects
- Original experimental
- A preliminary investigation into psychophysiological effects of threatening a perceptually embodied rubber hand in healthy human participants
- Editorial comment
- Analysis of C-reactive protein (CRP) levels in pain patients – Can biomarker studies lead to better understanding of the pathophysiology of pain?
- Clinical pain research
- Serum C-reactive protein levels predict regional brain responses to noxious cold stimulation of the hand in chronic whiplash associated disorders
- Editorial comment
- Importance of early diagnosis of complex regional pain syndrome (CRPS-1 and CRPS-2): Delayed diagnosis of CRPS is a major problem
- Clinical pain research
- Delayed diagnosis and worsening of pain following orthopedic surgery in patients with complex regional pain syndrome (CRPS)
- Editorial comment
- Associative learning mechanisms may trigger increased burden of chronic pain; unlearning and extinguishing learned maladaptive responses should help chronic pain patients
- Original experimental
- When touch predicts pain: predictive tactile cues modulate perceived intensity of painful stimulation independent of expectancy
- Editorial comment
- Low back pain among nurses: Common cause of lost days at work and contributing to the worldwide shortage of nurses
- Observational study
- Pain-related factors associated with lost work days in nurses with low back pain: A cross-sectional study
- Editorial comment
- Assessment of persistent pelvic pain after hysterectomy: Neuropathic or nociceptive?
- Clinical pain research
- Characterization of persistent pain after hysterectomy based on gynaecological and sensory examination
- Editorial comment
- Transmucosal fentanyl for severe cancer pain: Nasal mucosa superior to oral mucosa?
- Original experimental
- Facilitation of accurate and effective radiation therapy using fentanyl pectin nasal spray (FPNS) to reduce incidental breakthrough pain due to procedure positioning
- Editorial comment
- Why do we have opioid-receptors in peripheral tissues? Not for relief of pain by opioids
- Clinical pain research
- Peripheral morphine reduces acute pain in inflamed tissue after third molar extraction: A double-blind, randomized, active-controlled clinical trial
- Editorial comment
- Chronic pain and psychological distress among long-term social assistance recipients – An intolerable burden on those on the lowest steps of the socioeconomic ladder
- Clinical pain research
- The co-occurrence of chronic pain and psychological distress and its associations with salient socio-demographic characteristics among long-term social assistance recipients in Norway
- Editorial comment
- Fifty years on the Visual Analogue Scale (VAS) for pain-intensity is still good for acute pain. But multidimensional assessment is needed for chronic pain
- Clinical pain research
- Patient reported outcome measures of pain intensity: Do they tell us what we need to know?
- Editorial comment
- Postoperative pain documentation 30 years after
- Topical review
- Postoperative pain documentation in a hospital setting: A topical review
- Editorial comment
- Aspects of pain attitudes and pain beliefs in children: Clinical importance and validity
- Observational study
- The Survey of Pain Attitudes: A revised version of its pediatric form
- Editorial comment
- The role of social anxiety in chronic pain and the return-to-work process
- Clinical pain research
- Social Anxiety, Pain Catastrophizing and Return-To-Work Self-Efficacy in chronic pain: a cross-sectional study
- Editorial comment
- Advances in understanding and treatment of opioid-induced-bowel-dysfunction, opioid-induced-constipation in particular Nordic recommendations based on multi-specialist input
- Topical review
- Definition, diagnosis and treatment strategies for opioid-induced bowel dysfunction–Recommendations of the Nordic Working Group
- Observational study
- Opioid-induced constipation, use of laxatives, and health-related quality of life
- Editorial comment
- Migraine headache and bipolar disorders: Common comorbidities
- Systematic review
- Migraine headache and bipolar disorder comorbidity: A systematic review of the literature and clinical implications
- Editorial comment
- The role of catastrophizing in the pain–depression relationship
- Clinical pain research
- The mediating role of catastrophizing in the relationship between pain intensity and depressed mood in older adults with persistent pain: A longitudinal analysis
- Announcement
- May 26-27, 2016 Scandinavian Association for the Study of Pain, Reykjavik, Iceland May 25, 2016 PhD course

