Abstract
Background and purpose
Local infiltration anaesthesia is frequently painful due to low pH of the used anaesthetics, such as lidocaine. Usually pH of the solution is near 4.0, which causes tissue irritation and excitation of the pain mediating nerve endings. Warming and buffering the local anaesthetic solution have been shown to reduce the patient’s experience of pain and unpleasantness during infiltration. Buffering reduces the dissociation of the local anaesthetic molecule and may enhance the anaesthetic’s entrance into nerve cells. In this randomized placebo-controlled trial warmed and buffered lidocaine with adrenaline was compared to room temperature unbuffered lidocaine with adrenaline infiltrated before bone marrow aspiration and/or biopsy (BMAB). The aim was to find out to what extent warming and buffering would diminish pain during infiltration and whether this would be reflected in less pain also during subsequent steps of the BMAB procedure.
Methods
One hundred patients scheduled to undergo BMAB were interviewed regarding subjective experiences from previous medical procedures, current chronic and temporary medications, and their present state of anxiety before the BMAB procedure. They received local anaesthetic infiltration of lidocaine prior to BMAB. The solution used was either warmed lidocaine 20 mg/ml with adrenaline buffered with sodium bicarbonate 75 mg/ml (warmed and buffered group, 50 patients, pH approximately 7.3, 32°C) or unbuffered lidocaine 20 mg/ml with adrenaline mixed with NaCl 0.9% solution (control group, 50 patients, pH approximately 3.7, room temperature). The lidocaine concentration was similar in both groups. The bone marrow sampling needle was inserted 2 min after local anaesthetic infiltration. The grade of preprocedural anxiety, and pain sensations during the BMAB, both rated on NRS (numeral rating scale, 0–10) were compared between the groups.
Results
In comparison with the use of an unbuffered solution at room temperature warmed and buffered lidocaine with adrenaline caused less pain during infiltration (median NRS 4.0 vs. 2.0, P < 0.002) but it did not make performing the other phases of BMAB any less painful. As expected, painful experiences from previous medical, other than BMAB, or dental procedures and anxiety were associated with local anaesthetic infiltration pain during BMAB. Patients’ own pain or anxiolytic medication did not lessen pain during BMAB.
Conclusions
By warming and buffering the lidocaine solution containing adrenaline it is possible to make the pain during infiltration less intense. Unfortunately, such benefit was not detected during the following steps of BMAB, initiated 2 min later. Preprocedural anxiety made procedural pain more intense including that of the local anaesthetic infiltration.
Implications
Warming and buffering the local anaesthetic prior to its administration is an effective and simple way of diminishing pain during infiltration. This benefit seems to be underutilized in the BMAB procedure. However, warming and buffering are not sufficient enough to diminish pain during bone marrow sampling and thus additional pain alleviating methods should be used, particularly in patients showing preprocedural anxiety.
1 Introduction
Bone marrow aspiration and/or biopsy (BMAB) in adults is usually performed after local anaesthetic infiltration, occasionally supplemented with a sedative or an opioid. In spite of infiltration of adequate amount and concentration of the local anaesthetic (usually lidocaine) the subsequent sampling procedures can be painful [1,2,3]. Since the local anaesthetic solutions are acidic, the subcutaneous and periosteal infiltration may itself cause discomfort and pain. For BMAB, adrenaline containing local anaesthetic solutions are preferred because the vasoconstrictor may reduce the size of postpuncture haematomas, in particular in patients with disturbed coagulation. However, the commercial adrenaline containing solutions are manufactured very acidic (approximately pH 4) by adding hydrochloric acid for adequate preservation of adrenaline, resulting in even more tissue irritation than with plain solutions (pH 5–7). Buffering the acidic local anaesthetic solution to near physiological pH by adding sodium bicarbonate just prior to administration has been found to reduce the pain from infiltration in a variety of clinical situations [4,5,6] as well as in one BMAB study [7]. In addition, by reducing the dissociation of the basic local anaesthetic molecule (pKa 7.9) through a pH rise, the molecules can enter into nerve cells more easily and act more rapidly and strongly [8,9].
Another simple and inexpensive manoeuver to make the local anaesthetic infiltration more comfortable is warming the solution to a temperature near body temperature [10]. Warming and buffering may act synergistically in alleviating infiltration pain [11,12], but experience from this combination for BMAB seems to be lacking. A pleasant experience from the first step of the BMAB procedure, i.e. local anaesthetic infiltration, may be reflected in reduced discomfort from the following steps of BMAB.
Therefore, in the present study we warmed the adrenaline containing lidocaine solution (32 °C) and added warm bicarbonate just before infiltration. The primary outcome was the intensity of pain during infiltration in comparison with the infiltration of the nonbuffered solution at room temperature. The secondary aim was to find out whether pain during the subsequent steps (puncture, aspiration, biopsy) would be influenced by the pain experience from the local anaesthetic infiltration performed 2 min earlier.
2 Methods
The ethics committee of Helsinki and Uusimaa hospital district accepted the protocol (diary number 306/13/03/01/11). All patients gave informed consent before recruitment.
2.1 Patients
We included 100 patients in this randomized study; 50 patients received warmed and buffered lidocaine with adrenaline and the other 50 patients received non-buffered lidocaine with adrenaline at room temperature. The power analysis was based on a study comparing intradermal infiltration of unmanipulated lidocaine to warmed and buffered lidocaine in volunteers [11]. In that study, the VAS score for unmanipulated lidocaine infiltration was 44.2, and for warmed, buffered lidocaine it was 29.2. Thus, warming and buffering decreased the VAS score by 34%. In our previous study [2] mean NRS score for local anaesthetic infiltration was 3.5 (SD 2.08). A reduction in pain intensity during infiltration by 34% would be expected to yield a NRS score of 2.3 in our BMAB patients. When the alfa is set to 0.05 and power to 80%, we need 44 patients to both study groups. Due to the medical complexity of haematological patients we decided to recruit 100 patients to the study. Half of the patients were randomized to receive warmed and buffered lidocaine and the other half served as a control group receiving nonwarmed and non-buffered lidocaine. Furthermore, approximately half of patients in each group had the bone marrow sampling performed from the sternum and the other half from the posterior iliac crest. The exclusion criteria were allergy to local anaesthetics, obesity (BMI, body mass index > 32 kg/m2) and unstable coronary heart disease. The flow chart is presented in Fig. 1.
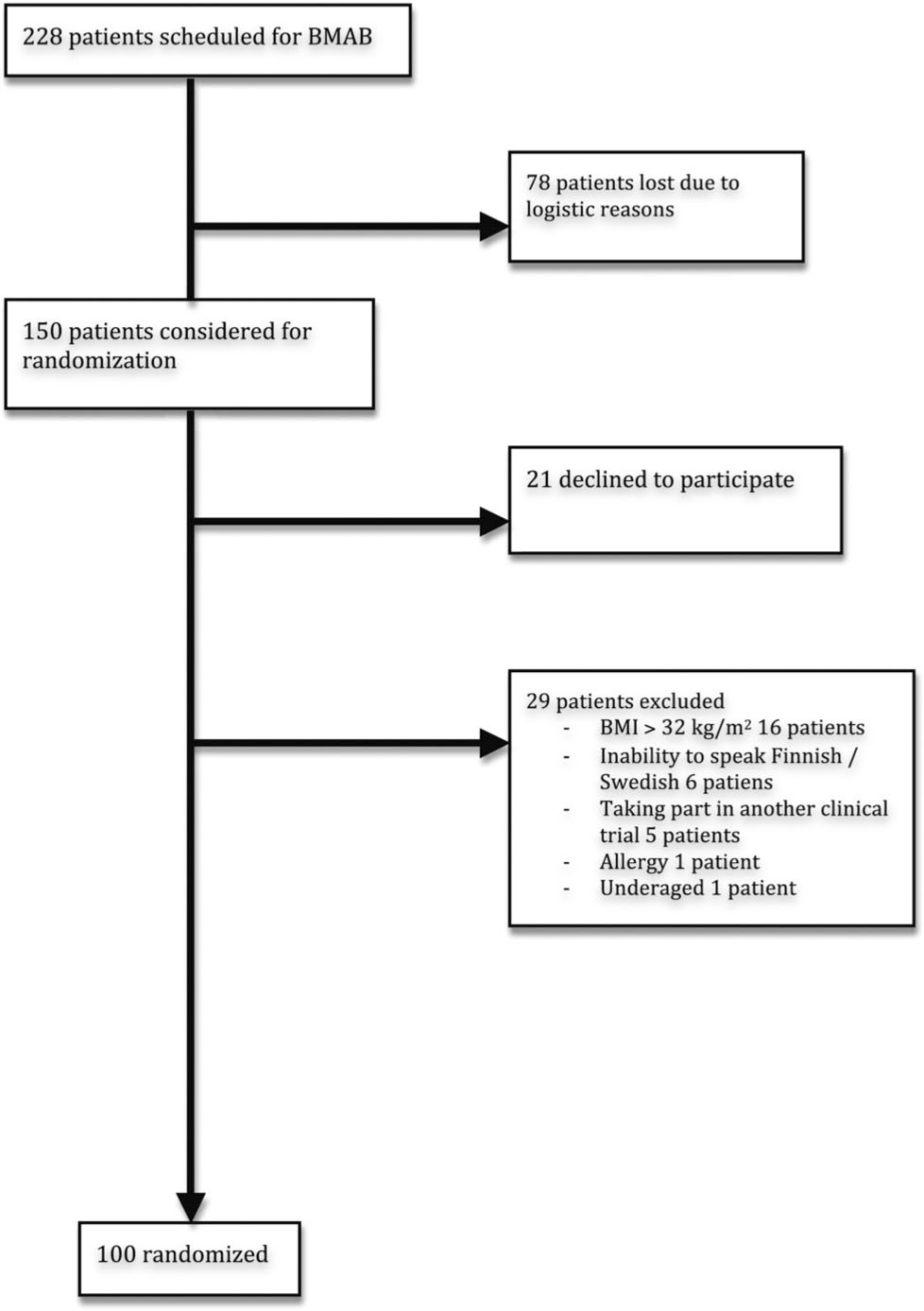
Flow chart.
2.2 Blinding
This study was single-blinded. The randomization was performed beforehand with sealed envelopes. Before the BMAB begun, the research assistant opened the envelope and prepared the local anaesthetic solution for the patient. The physician performing the BMAB was not told which group the patient belonged to. The nonblinded research assistant performed interviews using a designated questionnaire after the BMAB on the procedure day. One of the blinded researchers performed the telephone interviews on the following day.
2.3 Interview before BMAB
During the pre-procedural interview the research assistant recorded the participants’ regular or temporary use of pain, anxiolytic or sleep medication. The patients were asked to grade their pre-procedural anxiety on NRS 0–10 (numeral rating scale, 0 = no anxiety, 10 = worst anxiety imaginable). Possible pre-existing pain and its intensity on NRS (0 = no pain, 10 = worst pain imaginable) was recorded. The patients also graded the pain experience during previous BMABs or other minor medical procedures (e.g. visit to the dentist). On the patient’s request, diazepam or intramuscular alfentanil was given before the BMAB procedure.
2.4 Local anaesthetic solutions
The local anaesthetic solution for control group was made from 8 ml of room temperature lidocaine 20 mg/ml with adrenaline 5 μg/ml (Lidocain c adrenalin, Orion Corporation, Espoo, Finland) and 2 ml NaCl 0.9% solution, totaling 10 ml. The pH of the control group solution had been measured (Radiometer PHM 83 Autocal pH Meter, Denmark) in our separate preceding laboratory tests and was approximately 3.7. The buffered and warmed local anaesthetic solution was made from 8 ml of lidocaine 20 mg/ml with adrenaline 5 μg/ml and 2.0 ml of 7.5% sodium bicarbonate (Natriumbicarbonate Braun 75 mg/ml, B. Braun, Melsungen, Germany). The lidocaine and sodium bicarbonate solutions were first warmed in separate syringes for 4–5 min under a heating lamp to 32 °C. This temperature was chosen because in normal conditions it is near the temperature of the subcutaneous tissue [13]. A thermometer was used to control adequate warming, after which the lidocaine and sodium bicarbonate were mixed in a syringe and handed out to the haematologist. The pH of this buffered and warmed solution was approximately 7.3.
2.5 The BMAB procedure
After disinfection of the procedure site the physician performing the BMAB infiltrated the local anaesthetic using 22 G needle. The total volume of the local anaesthetic solution was 10 ml at the iliac crest, 8 ml at the sternal manubrium and 6 ml at the sternal body. One third of the local anaesthetic was infiltrated to the proximity of bony periosteum, one third to the subcutaneous tissue and the rest to the skin.
Two minutes after the local anaesthetic infiltration the haematologist tested the numbness of the procedure site with a puncture needle (14–16 G). If the patient sensed pain during testing, the haematologist infiltrated an additional dose of the anaesthetic solution, the volume being half of the original dose. If the patient suffered strong pain during BMAB, the patient received intramuscular alfentanil (Rapifen®, Janssen-Cilag corporation, 0.4–0.75 mg) or sublingual fentanyl (Abstral®, ProStrakan Ltd. 100–200 μg) as rescue medication. Immediately after each phase of the BMAB the research assistant asked the patient to grade the pain on the NRS (0–10).
2.6 Post-procedural interviews
After BMAB the patient walked to recovery room where the research assistant conducted the interview and recorded the general condition and possible complications such as pain or nausea. The patients were discharged after this interview if they felt well and no signs of BMAB related complications occurred. One of the blinded researchers telephoned the patient on the following day and recorded the general condition of the participant, pain at the puncture site and possible complications.
2.7 Statistics
Ordinal regression analysis stratified by phase of the procedure was used to measure differences between the study groups in regard to pain during BMAB. The variables considered to have a confounding effect were included in the analysis. PASW Statistics version 18.0 (Hong Kong) was used.
3 Results
The patient data collection was performed during January 2012 to April 2012. The demographic data of the participants are shown in Table 1. Eleven patients were on regular pain medication (paracetamol, ibuprofen, naproxen, paracetamol–codeine combination, tramadol, buprenorphine, oxycodone, pregabalin, gabapentin and amitriptyline). Ten patients were on regular anxiolytic or sleeping medication (zopiclone, benzodiazepines).
Demographic data of the patients. BMAB = Bone marrow aspiration and biopsy.
| Warmed and buffered group | Control group | |
|---|---|---|
| Gender (male/female) | 29/21 | 32/18 |
| Age (yrs), median (min, max) | 58 (19, 89) | 61 (29, 80) |
| Height (cm), median (min, max) | 176 (145, 190) | 175 (156, 190) |
| Weight (kg), median (min, max) | 77 (40, 111) | 76 (52, 106) |
| Diagnosis | ||
| Leukaemia acute/chronic | 18/3 | 17/6 |
| Lymphoma | 7 | 9 |
| Myeloma | 5 | 5 |
| Healthy donor | 3 | 0 |
| Other | 8 | 11 |
| Not known | 6 | 2 |
| Site of BMAB (n) | ||
| Sternal body | 14 | 14 |
| Sternal manubrium | 11 | 10 |
| Iliac crest | 25 | 26 |
The median preprocedural anxiety NRS score was 3.0 (range 0–10) with no difference between study groups. Twenty-three patients suffered from pre-existing pain in various regions (muscular pain, toothache, headache). The median NRS for patients having pre-existing pain was 3.0 (range 1–8). Eleven patients had taken temporary pain medication within 24 h before BMAB (paracetamol, paracetamol–codeine combination, oxycodone). Four patients had taken temporary anxiolytic or sleeping medication within 24 h prior BMAB.
3.1 Previous procedures
The majority of the patients (81.0%) had undergone BMAB before. The former BMABs had been painless in 10 patients (3 patients in warmed and buffered group and 7 patients in control group), slightly painful in 58 patients (27 patients in warmed and buffered group and 31 patients in control group) and painful in 10 patients (7 patients in warmed and buffered group and 3 patients in control group). Additionally, the patients were asked to grade the pain during other previous minor medical procedures (e.g. dental treatment). These procedures had been painless in 32 patients, slightly painful in 60 patients and painful in 7 patients, with no significant differences between study groups.
3.2 Pain during BMAB
The NRS scores during BMAB are shown in Table 2. Pain during local anaesthetic infiltration was significantly milder in patients receiving warmed and buffered lidocaine compared to the control group (P = 0.002, OR 0.29, 95% CI [0.13; 0.62]). The older the patient was the less pain the patient felt during local anaesthetic infiltration (P = 0.008, OR 0.96, 95% CI [0.94; 0.99]). The site of the procedure (sternal manubrium, sternal body or iliac crest) did not affect the pain ratings.
Pain during BMAB.
| Pain intensity (NRS 0–10) during BMAB phases, median (range) | Warmed and buffered group | Control group |
|---|---|---|
| Local anaesthetic infiltration | 2 (0–10) | 4 (0–10) |
| Puncture | 2 (0–10) | 3 (0–10) |
| Aspiration | 5 (0–10) | 3.5 (0–10) |
| Biopsy | 6 (0–10) | 5 (0–9) |
| Immediately after BMAB | 0 (0–7) | 0 (0–4) |
However, the use of warmed and buffered solution for the infiltration did not result in pain alleviation during other phases of the procedure. In fact, it seemed that processing the local anaesthetic resulted in increased pain during aspiration (not statistically significant, P = 0.052, OR 2.35, 95% CI [0.99; 5.25]) and pain felt immediately after BMAB (P = 0.017, OR 3.84, 95% CI [1.27; 11.62]).
Patients taking regular pain medication felt more pain during puncture (P = 0.047, OR 4.28, 95% CI [1.01; 18.07]) than those not having regular pain medication. Patients being on regular anxiolytic or sleeping medication suffered more pain during aspiration (P = 0.048, OR 3.91, 95% CI [1.01; 15.15]). That is, regular pain, anxiolytic or sleeping medication did not benefit the patients. Temporary use of pain medication (within 24 h prior to BMAB) was related to more pain during local anaesthetic infiltration (P = 0.006, OR 6.77, 95% CI [1.74; 26.29]). Temporary use of anxiolytic or sleeping medication did not affect the pain ratings. Pain medication given to 20 patients before or during BMAB on patient request did not alleviate pain during bone marrow sampling (NRS median during puncture 4.0 vs. 2.0, OR 2.406, 95% CI [0.937; 6.176]; NRS median during aspiration 4.0 vs. 4.0, OR 0.628, 95% CI [0.247; 1.593]; NRS median during biopsy 5.0 vs. 5.0, OR 0.471, 95% CI [0.064; 3.426]). Pain medication did lower the pain during local anaesthetic infiltration (NRS median 2.0 vs. 3.0, OR 0.269, 95% CI [0.099; 0.728]). Those five patients receiving benzodiazepines at the hospital 30–60 min prior to BMAB seem to have benefited from it, as their pain scores were somewhat lower during aspiration compared to those of the others (median NRS 2.0 vs. 4.0).
As expected, anxiety had a major influence on pain during BMAB. The more anxious the patient was just before BMAB, the more pain the patient suffered during local anaesthetic infiltration (P < 0.0001, OR 1.82, 95% CI [1.41; 2.34]), aspiration (P < 0.0001, OR 1.65, 95% CI [1.29; 2.11]) and immediately after BMAB (P = 0.006, OR 1.51, 95% CI [1.12; 2.03]).
Previous painful BMABs were not related to pain during the present BMAB apart from pain during biopsy. Biopsy pain was more intense if the patient recalled pain from previous BMABs (P = 0.029). Pain during previous other minor medical procedures such as a dental treatment predicted pain during local anaesthetic infiltration (P < 0.0001) and aspiration (P = 0.045).
3.3 Post-procedural interview
In the post-procedural telephone interview on the following day the median pain at the procedure site was 0 (range 0–6), with no difference between the study groups. Four patients (one in treatment and three in control group) reported of a small haematoma involving the puncture site. One patient from the warmed and buffered group reported minor haemorrhage from the puncture site. Three patients from the control group suffered from redness at the puncture site. No serious complications were reported.
4 Discussion
Warming and buffering the adrenaline-containing lidocaine solution made the infiltration pain less intense than in the control group. When lidocaine solution is buffered to near physiological pH, the equilibrium shifts to the nonionized form of the molecule. This is known to facilitate the anaesthetic effect of lidocaine on nerve cells [8,9]. However, in the present study no further clinical benefits of this phenomenon were gained as buffering proved to be similar in reducing pain during puncture, aspiration and biopsy compared to unbuffered lidocaine. However, letting the local anaesthetic properly take effect and traverse the bony periost and nerve cells might require more than 2 min, i.e. the time latency between infiltration and bone marrow puncture. The effect of buffering on procedural pain has varied in different studies and, e.g. in surgery for prominent ear correction it was found to be similar to unbuffered lidocaine [14], whereas during hernia repair [15] it was superior to unbuffered lidocaine and provided better local anaesthesia.
Warming the local anaesthetic may make pain during infiltration less intense through various mechanisms. Warming shifts the equilibrium of the molecule towards uncharged form of the molecule [16], thus enhancing the movement trough cell membranes, as seen also with buffered local anaesthetics. Warmed lidocaine solution might also cause less tissue irritation and excitation of nerve endings. Processing the local anaesthetic did not lessen pain during other phases of BMAB, reflecting the fact that lidocaine – even if it is warmed and buffered – does not sufficiently traverse the periosteum and bone marrow to such an extent that it would provide anaesthesia for bone marrow sampling.
As seen in our previous BMAB studies [2,3], anxiety was related to pain also in this study population. Those few patients who received diazepam at the hospital had lower pain scores during BMAB, but due to small number of these patients it cannot be ruled out that this observation was coincidental. Furthermore, those patients having regular anxiolytic medication did not have any lower pain scores. Pain medication given before or during BMAB did not have any beneficial effect either. Those patients receiving intramuscular alfentanil did not have any lower pain scores than the rest of the study population. This was also seen in our previous studies [3,17] and thus, the use of intramuscular opioids during ongoing BMAB should be discouraged. A beneficial effect of benzodiazepines on procedural pain during BMAB has been noted [18]. However, the patient should receive the drug sufficiently early so that the drug has time to take effect. Benzodiazepines have some adverse effects such as sedation and the risks and benefits of the drug should each time be evaluated. Intravenous opioid or benzodiazepine may be useful to a selected group of patients (fearful patients, patients having painful memories from previous BMABs) but this medication demands careful monitoring after the procedure.
Dental procedures resemble BMABs as they often require local anaesthesia and are frequently associated with anxiety and pain. Pain associated with dental procedures has been shown to correlate with the level of anxiety and use of local anaesthetic infiltration [19]. Anxiety also prolongs pain during local anaesthetic infiltration [20]. Thus anxiolytic premedication may be used with fearful patients [21]. It seems that local anaesthetic infiltration is a major source of pain in this patient population and should thus be targeted more intensively. Buffering the used lidocaine solution during dental procedures has been shown to decrease pain during infiltration and to shorten the onset of anaesthesia [22].
This study has some limitations. The protocol was only single-blinded as the research assistant who prepared the local anaesthetic solutions conducted the patient reviews as well. The physicians performing the BMAB probably recognized the warm syringe but since the investigators did not distract the haematologists to report how the syringe felt, they seemed to perform the procedure in the usual way. The infiltration anaesthesia might probably have been more profound if the local anaesthetic had been let to take effect longer.
In conclusion, warming and buffering of the local anaesthetic solution made the pain during lidocaine infiltration less intense but processing the solution did not have an effect on the subsequent painful phases of BMAB. Preprocedural anxiety correlated with pain during all procedural steps, including local anaesthetic infiltration.
Highlights
Bone marrow aspiration and biopsy is a painful procedure despite local infiltration anaesthesia.
Warming and buffering the local anaesthetic solution alleviates pain during infiltration.
Processed solution does not ease pain during next steps of bone marrow sampling.
Especially anxious patients may benefit from additional pain relieving methods.
DOI of refers to article: http://dx.doi.org/10.1016/j.sjpain.2013.11.005.
-
Conflict of interest
Conflict of interest statement: The authors do not have any actual or potential conflict of interest including any financial, personal or other relationships with other people or organizations.
Acknowledgements
We wish to thank our research assistant Päivi Turunen, R.N, for her valuable work in collecting the patient material. One of the authors (PR) received a research grant for the study from the Finska Läkaresällskapet foundation.
References
[1] Vanhelleputte P, Nijs K, Delforge M, Evers G, Vanderschueren S. Pain during bone marrow aspiration: prevalence and prevention. J Pain Symptom Manage 2003;26:860–6.Search in Google Scholar
[2] Kuivalainen AM, Niemi-Murola L, Widenius T, Elonen E, Rosenberg PH. Comparison of articaine and lidocaine for infiltration anaesthesia in patients undergoing bone marrow aspiration and biopsy. Eur J Pain 2010;14:160–3.Search in Google Scholar
[3] Kuivalainen AM, Pitkäniemi J, Widenius T, Elonen E, Rosenberg PH. Anxiety and pain during bone marrow aspiration and biopsy. Scand J Pain 2012;3:92–6.Search in Google Scholar
[4] Xia Y, Chen E, Tibbits DL, Reilley TE, McSweeney TD. Comparison of effects of lidocaine hydrochloride, buffered lidocaine, diphenhydramine, and normal saline after intradermal injection. J Clin Anesth 2002;14:339–43.Search in Google Scholar
[5] Carvalho B, Fuller A, Brummel C, Cohen SE. Local infiltration of epinephrine-containing lidocaine with bicarbonate reduces superficial bleeding and pain during labor epidural catheter insertion: a randomized trial. Int J Obstet Anesth 2007;16:116–21.Search in Google Scholar
[6] Narváez J, Wessels I, Bacon G, Chin VR, Baqai WK, Zimmerman GJ. Prospective randomized evaluation of short-term complications when using buffered or unbuffered lidocaine 1% with epinephrine for blepharoplasty surgery. Ophthal Plast Reconstr Surg 2010;26:33–5.Search in Google Scholar
[7] Ruegg TA, Curran CR, Lamb T. Use of buffered lidocaine in bone marrow biopsies: a randomized, controlled study. Oncol Nurs Forum 2009;36:52–60.Search in Google Scholar
[8] Coventry DM, Todd G. Alkalinisation of bupivacaine for sciatic nerve blockade. Anaesthesia 1989;44:467–70.Search in Google Scholar
[9] Quinlan JJ, Oleksey K, Murphy FL. Alkalinization of mepivacaine for axillary block. Anesth Analg 1992;74:371–4.Search in Google Scholar
[10] Hogan ME, vanderVaart S, Perampaladas K, Machado M, Einarson TR, Taddio A. Systematic review and meta-analysis of the effect of warming local anesthetics on injection pain. Ann Emerg Med 2011;58:86–98, e1.Search in Google Scholar
[11] Colaric KB, Overton DT, Moore K. Pain reduction in lidocaine administration through buffering and warming. Am J Emerg Med 1998;16:353–6.Search in Google Scholar
[12] Hsu CH, YangF H.C., ShenF S.C., Juan WH, Hong HS, Chen CH. Warm and neutral tumescent anesthetic solutions are essential factors for a less painful injection. Dermatol Surg 2006;32:1119–23.Search in Google Scholar
[13] Heavner JE, Leinonen L, Haasio J, Kyttä J, Rosenberg PH. Interaction of lidocaine and hypothermia in Bier blocks in volunteers. Anesth Analg 1989;69:53–9.Search in Google Scholar
[14] Fitton AR, Ragbir M, Milling MAP. The use of pH adjusted lignocaine in controlling operative pain in the day surgery unit: a prospective, randomized trial. Br J Plast Surg 1996;49:404–8.Search in Google Scholar
[15] Ball EL, Sanjay P, Woodward A. Comparison of buffered and unbuffered local anaesthesia for inguinal hernia repair: a prospective study. Hernia 2006;10:175–8.Search in Google Scholar
[16] Kamaya H, Hayes JJ, Ueda I. Dissociation constants of local anesthetics and their temperature dependence. Anesth Analg 1983;62:1025–30.Search in Google Scholar
[17] Kuivalainen AM, Ebeling F, Rosenberg PH. Pre-medication with sublingual fentanyl did not relieve pain associated with bone marrow aspiration and biopsy: a randomized feasibility trial. Eur J Pain 2013;17:1357–64.Search in Google Scholar
[18] Park SH, Bang SM, Nam E, Cho EK, Shin DB, Lee JH, Ahn JY. A randomized double-blind placebo-controlled study of low-dose intravenous lorazepam to reduce procedural pain during bone marrow aspiration and biopsy. Pain Med 2008;9:249–52.Search in Google Scholar
[19] Tickle M, Milsom K, Crawford FIJ, Aggarwal VR. Predictors of pain associated with routine procedures performed in general dental practise. Community Dent Oral Epidemiol 2012;40:343–50.Search in Google Scholar
[20] van Wijk AJ, Hoogstraten J. Anxiety and pain during dental injections. J Dent 2009;37:700–4.Search in Google Scholar
[21] Donaldson M, Gizzarelli G, Chanpong B. Oral sedation: a primer on anxiolysis for the adult patient. Anesth Prog 2007;54:118–28.Search in Google Scholar
[22] Kashyap VM, Desai R, Reddy PB, Menon S. Effect of alkalinisation of lignocaine for intraoral nerve block on pain during injection, and speed of onset of anaesthesia. Br J Oral Maxillofac Surg 2011;49:e72–5.Search in Google Scholar
© 2013 Scandinavian Association for the Study of Pain
Articles in the same Issue
- Scandinavian Journal of Pain
- Editorial comment
- High risk of depression and suicide attempt among chronic pain patients: Always explore catastrophizing and suicide thoughts when evaluating chronic pain patients
- Clinical pain research
- Suicide attempts in chronic pain patients. A register-based study
- Editorial comment
- Polymorphism in the μ-opioid receptor gene OPRM1 A118G —An example of the enigma of genetic variability behind chronic pain syndromes
- Original experimental
- A118G polymorphism in the μ-opioid receptor gene and levels of β-endorphin are associated with provoked vestibulodynia and pressure pain sensitivity
- Editorial comment
- Genital pain related to sexual activity in young women: A large group who suffer in silence
- Original experimental
- Living with genital pain: Sexual function, satisfaction, and help-seeking among women living in Sweden
- Editorial comment
- The Norwegian version of the Neck Disability Index (NDI) is reliable and sensitive to changes in pain-intensity and consequences of pain-in-the-neck
- Clinical pain research
- Reliability and responsiveness of the Norwegian version of the Neck Disability Index
- Editorial comment
- Quality of life in low back pain patients with MRI-lesions in spinal bone marrow and vertebral endplates (Modic-changes): Clinical significance for outcome of spinal surgery?
- Clinical pain research
- Association of Modic changes with health-related quality of life among patients referred to spine surgery
- Editorial comment
- Warming and alkalinisation of lidocaine with epinephrine mixture: Some useful aspects at first glance, but not so simple?
- Clinical pain research
- Warmed and buffered lidocaine for pain relief during bone marrow aspiration and biopsy. A randomized and controlled trial
- Acknowledgement of Reviewers
Articles in the same Issue
- Scandinavian Journal of Pain
- Editorial comment
- High risk of depression and suicide attempt among chronic pain patients: Always explore catastrophizing and suicide thoughts when evaluating chronic pain patients
- Clinical pain research
- Suicide attempts in chronic pain patients. A register-based study
- Editorial comment
- Polymorphism in the μ-opioid receptor gene OPRM1 A118G —An example of the enigma of genetic variability behind chronic pain syndromes
- Original experimental
- A118G polymorphism in the μ-opioid receptor gene and levels of β-endorphin are associated with provoked vestibulodynia and pressure pain sensitivity
- Editorial comment
- Genital pain related to sexual activity in young women: A large group who suffer in silence
- Original experimental
- Living with genital pain: Sexual function, satisfaction, and help-seeking among women living in Sweden
- Editorial comment
- The Norwegian version of the Neck Disability Index (NDI) is reliable and sensitive to changes in pain-intensity and consequences of pain-in-the-neck
- Clinical pain research
- Reliability and responsiveness of the Norwegian version of the Neck Disability Index
- Editorial comment
- Quality of life in low back pain patients with MRI-lesions in spinal bone marrow and vertebral endplates (Modic-changes): Clinical significance for outcome of spinal surgery?
- Clinical pain research
- Association of Modic changes with health-related quality of life among patients referred to spine surgery
- Editorial comment
- Warming and alkalinisation of lidocaine with epinephrine mixture: Some useful aspects at first glance, but not so simple?
- Clinical pain research
- Warmed and buffered lidocaine for pain relief during bone marrow aspiration and biopsy. A randomized and controlled trial
- Acknowledgement of Reviewers

