Intravenous acetaminophen vs. ketorolac for postoperative analgesia after ambulatory parathyroidectomy
-
Amrat Anand
Abstract
Background and methods
Minimally invasive parathyroidectomy requires limited analgesia and short recovery times. The preferred post-operative analgesic regimen for this patient population has not been established but non-narcotic components would be quite appropriate. The aim of the study was to determine whether intravenous (IV) acetaminophen (1 g) or ketorolac (30 mg) provide better pain control after parathyroidectomy. A parallel, randomized, double blind, comparative study was completed on 180 patients scheduled for outpatient parathyroidectomy utilizing general anesthesia. Patients were randomized to a blinded administration of either intravenous acetaminophen 1 g or ketorolac 30 mg intra-operatively. Upon arrival but before premedication, baseline pain scores were assessed in all patients. A consecutive series of postoperative pain scores were collected every 15 min using a 10 cm visual analog pain scale (VAS) upon arrival to the post anesthesia care unit (PACU) until discharge by blinded study personnel. Other data collected included: anesthesia time, surgical time, time to discharge, supplemental morphine and postoperative side effects.
Results
Overall mean postoperative VAS scores were not significantly different between the two treatment groups (p = 0.07). However, ketorolac produced significantly lower pain scores compared with acetaminophen in the later postoperative periods (3.9 ± 1.9 vs. 4.8 ± 2.4 at 45 min, p = 0.009; 3.4 ± 1.7 vs. 4.5 ± 2.1 at 60min, p = 0.04; and 3.2 ± 2.1 vs. 4.4 ± 2.1 at 75 min, p = 0.03). Supplemental morphine was administered to 3 patients in the ketorolac group and 9 patients in the acetaminophen group but total consumption was not significantly different between groups (p = 0.13). The occurrence of nausea was significantly lower in the ketorolac group compared with the IV acetaminophen group (3.4% vs. 14.6%, respectively; p = 0.02). The overall incidence of morphine supplementation, vomiting, headache, muscular pain, dizziness, and drowsiness were not significantly different when compared between the treatment groups.
Conclusions
Both postoperative regimens provided adequate analgesia but patients receiving ketorolac intraoperatively had significantly lower pain scores at later recovery time points and significantly lower occurrences of nausea.
Implications
The large volume of patients undergoing parathyroidectomies at our facility warranted a study to develop a standardized postoperative analgesic regimen. We conclude both medications can be utilized safely in this patient population, but there is a slight advantage in pain control with the usage of ketorolac for minimally invasive parathyroidectomies.
1 Introduction
The gold standard for treatment of primary hyperparathyroidism is parathyroidectomy [1, 2]. In our pioneered technique, minimally invasive and radio-guided parathyroid (MIRP) surgery, there is short operating times with cure rates over 99% [2, 3, 4]. Despite less perceived pain with MIRP compared with traditional parathyroidectomy techniques, the preferred regimen for postoperative pain relief has not been established and is often determined by the preference of the anesthesia provider or drug availability. This minimally invasive surgery lends itself well to an opioid-free pain regimen, benefiting the patient with less serious side effects and cheaper costs. Currently two non-opioid analgesics, intravenous acetaminophen (Ofirmev, Cadence Pharmaceuticals, Inc., San Diego, CA) or ketorolac (Toradol, Hospira, Baxter), are used intra-operatively for postoperative pain management in our ambulatory setting.
Ketorolac, a non-steroid anti-inflammatory drug (NSAID), is indicated for pain control, fever and inflammation and has shown to decrease narcotic usage and side effects [5]. Ketorolac however, has been shown to induce platelet dysfunction and increased incidence of hematoma after thyroid surgery [6, 7]. Recently FDA approved (USA), intravenous acetaminophen, an anti-pyretic, non-NSAID analgesic agent obtains a faster and more effective onset compared with orally or rectally administered acetaminophen [8]. Several studies have noted its clinical benefit by providing reduced pain scores, opioid consumption, and postoperative side effects when used as a postoperative analgesic [9].
The purpose of this study was to establish an optimal postoperative pain regimen for patients undergoing minimally invasive parathyroidectomy while limiting associated side effects. The primary objective of this study was to a compare postoperative Visual Analog Scale (VAS) pain scores for two current analgesic regimens at our institution: intravenous administration of either ketorolac 30 mg or acetaminophen 1 g.
2 Methods
The study was approved by the Institutional Review Board (IRB) at the University of North Florida. Signed informed consent was obtained from each patient. This was a prospective, parallel, randomized, double-blinded, quantitative analysis study of 180 subjects scheduled for an ambulatory, minimally invasive parathyroidectomy procedure at a level 1 trauma hospital. All patients were screened and enrolled between February 2012 and June 2012.
All subjects that were scheduled to receive a primary parathy-roidectomy were evaluated for eligibility. Adults, older than 18 years of age, American Society of Anesthesiologists (ASA) physical status I-III were included in the study. Patients diagnosed with coagulopathy, liver or kidney impairment, allergy to NSAIDS, opioids, or local anesthetics, opioid/alcohol abuse, or recent infections were excluded from the study.
2.1 Randomization and blinding
On the day of admission, all patients were randomized in the preoperative holding area. Using a stratified random block design, the participants were stratified by age (≤60 or >60) and gender, and assigned randomly 1:1 to receive one of the following treatments for postoperative analgesia (90 patient/group): Acetaminophen 1 g given intravenously over 15 min at the start of the procedure or ketorolac 30 mg administered intravenously over 5 min at the time of closure of the inner fascia (approximately fifteen min before the end of surgery). The dosing time was based on the standard method of administration at out facility. The difference from the end of the acetaminophen infusion (15 min after the start of the case) and beginning of the ketorolac infusion (closing of the fascia) was calculated and averaged for each procedure.
The study pharmacist and administering anesthesiologist were the only unblinded staff for the study. A randomization schedule was provided by a biostatistician and delivered to the research pharmacist. The treatment allocation was completed by the research pharmacist who assigned the patient to the next available treatment on the randomization list according to age and gender and prepared the study drug. The study medications were delivered to the operating room by the study staff in blinded containers. No study members were in the operating room during the time of the procedure. Each study drug was administered intraoperatively as standard of care. Intraoperative notes in the electric medical records were listed as ‘ketorolac/ofirmev given’ in order to maintain the study blind.
2.2 Anesthetic regimen
Preoperatively, all patients were given 2 mg midazolam, and 4 mg of ondansetron intravenously. Anesthesia was induced with intravenous lidocaine 50 mg, followed by propofol 200 mg, fentanyl 50–100μg intravenously, and a laryngeal mask airway (LMA) was placed. General anesthesia was maintained with sevoflurane 1–3% in oxygen enriched air with 1.5–2 minimal alveolar concentration (MAC) and mean arterial pressure (MAP) was maintained at ≥65 mmHg in all patients.
2.3 Pain assessment
The participant’s pain level was assessed immediately upon PACU arrival by the study staff and was reassessed every 15 min until discharge using a 0–10 cm Visual Analog Pain Scale (VAS). Patients that complained of pain intensity >5 cm/10 cm, were given 2–4mg morphine IV up to a max dose of 10 mg as needed every 10min or until a VAS of <5 was obtained. Concurrently, any post-operative side effects or supplemental narcotic usage in the PACU were noted by study personnel with the assistance of the nursing staff.
2.4 Sample size and statistical analysis
The primary objective of the study was to determine if there was a difference in repeated, self-reported, postoperative VAS scores. A minimum of 180 patients (90 per group) was necessary to achieve 80% power to detect a difference of means of 0.5 on the 10 cm VAS scale in a design with 5 repeated time measurements, under the assumed common standard deviation of 1.3 [10], the correlation between observations on the same subject of 0.8, and the alpha level of 0.05. The secondary endpoints were to compare the following outcomes between the two study treatment arms: the total amount of supplemental analgesia consumed during the postoperative period, incidence of postoperative nausea, vomiting, bleeding, sedation and other adverse events.
Comparison of repeated VAS scores between groups was analyzed using a mixed model adjusted for stratified variables. Nominal data were analyzed with χ2 or Fisher’s exact test. Student’s t-test was used for continuous data (expressed as mean standard deviation (SD)), and Wilcoxon rank sum test was used for non-normally distributed data. A p-value of less than 0.05 was considered statistically significant. All data were analyzed using Stata 11.2 (StataCorp LP, College Station, TX).
3 Results
A total of 180 patients were enrolled into the study. Fig. 1 presents the CONSORT flow diagram [11] on patient participation and reasons for non-participation. Five patients were withdrawn for the following reasons: admittance to the hospital following a required total thyroidectomy for concomitant thyroid cancer (1), wrong medication given (3), and re-operation (1). Demographic data such as age, weight, and height are displayed in Table 1. The comparability of the groups was found to be adequate as there were no statistically significant differences in preoperative VAS scores, length of anesthesia, or length of surgery (Table 1). The removal of one or more thyroid nodules during the parathyroid operation via nodulectomy, partial thyroid lobectomy, or total lobectomy occurred in 24% of patients at a rate which was similar for each group (Table 1). The mean time between the intraoperative administration of the two analgesics was 14.6 min. Concomitant thyroid resection increased the duration of the operation an equal amount in both groups (mean 5.5 ± 3.1 min), but had no effect on postoperative pain measurement compared with those not having any thyroid resection.

CONSORT recommended description of patient recruitment to analgesic efficacy of ketorolac vs. acetaminophen randomized, double-blind, active-controlled trial at Tampa General Hospital, Tampa, Florida, USA. *Patients were given both study medications.
Patient demographics and surgical time points.
| Ketorolac (N =86) | Acetaminophen (N =89) | |
|---|---|---|
| Age (years) | 60.8 ± 9.8 | 58.8±10.5 |
| Gender (female) | 68 (75.5) | 67 (74.4) |
| Height (cm) | 168.9±9.4 | 166.9±9.4 |
| Weight (kg) | 79.9±16.3 | 80.2±20.4 |
| BMI (kg/m2) | 28.1 ± 6.0 | 28.7±7.0 |
| Length ofsurgical procedure (min) | 40.2±16.4 | 41.5±18.2 |
| Thyroid nodule removal (N) | 21 | 22 |
| Anesthesia time (min) | 68.5±14.8 | 70.6±18.5 |
| Length ofPACU stay (min) | 70.5±32.7 | 72.2±30.7 |
-
Data presented as N (%) or mean SD.
The main objective of this study was to assess a series of repeated VAS scores measured over the length of the entire recovery period to determine if one analgesic was superior to the other in regards to pain relief. The VAS scores are depicted in Fig. 2. Although there was a significant interaction between time and drug administered (p = 0.001), there were no overall significant differences between VAS scores in the ketorolac and acetaminophen groups across the time points (p = 0.07). The VAS scores at postoperative time points 0, 15, and 30 min were not significantly different between the ketorolac and acetaminophen groups. However, the postoperative VAS scores reported at the 45, 60 and 75 min time points were significantly lower in patients who received ketorolac (3.9 ± 1.9 vs. 4.8 ± 2.4 at 45 min, p = 0.009; 3.4± 1.7 vs. 4.5 ± 2.1 at 60 min, p = 0.04; and 3.2 ± 2.1 vs. 4.4 ± 2.1 at 75 min, p = 0.03). The differences in repeated VAS scores were assessed using a mixed model.
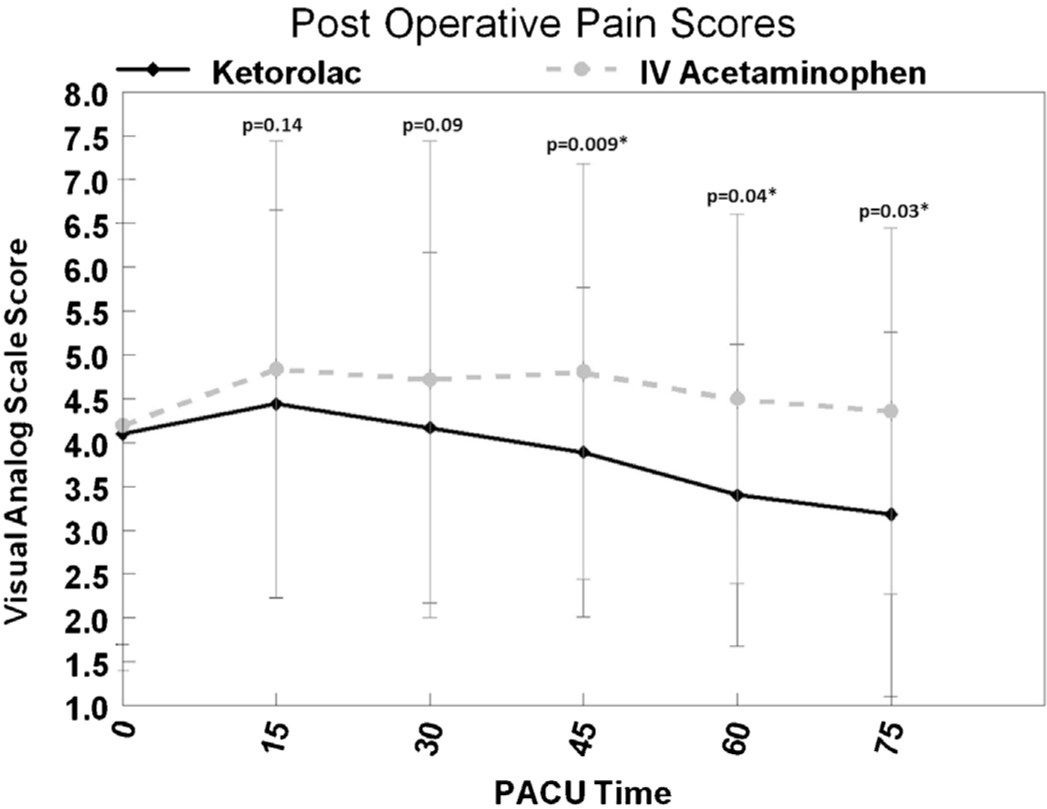
Change in mean postoperative VAS scores for patients treated with ketorolac (solid line) 30mg and or acetaminophen (dotted line) 1g from baseline (PACU arrival) to minute 75 (PACU discharge). Ap-value <0.05 was considered statistically significant (*). Data are represented as mean ± SD. The differences in repeated VAS scores were assessed using a mixed model.
Postoperative morphine requirements and complications are presented in Table 2. The number of patients that required postoperative morphine supplementation in the acetaminophen group (9 patients or 10.1%) compared with the ketorolac group (3 patients or 3.3%), was not significantly different (p = 0.13). The occurrence of nausea was significantly greater in the acetaminophen group compared with the ketorolac group (p = 0.02). Only two incidences of nausea were attributed to morphine use. The overall incidence of other postoperative side effects such as vomiting, headache, muscular pain, dizziness, and drowsiness were not significantly different when compared between the treatment groups.
Post-operative morphine requirements and incidence of side effects.
| Ketorolac (N = 86) | Acetaminophen (N =89) | p-Value | |
|---|---|---|---|
| Morphine requirements | 3(3.3) | 9(10.1) | 0.13 |
| Morphine consumed (mg) | 0(0–6.7) | 0(0–4) | 0.31 |
| Nausea | 3(3.4) | 13(14.6) | 0.02[*] |
| Vomiting | 3(3.4) | 3(3.4) | 1 |
| Headache | 5(5.8) | 7 (7.9) | 0.77 |
| Muscular pain | 3(3.4) | 2(2.2) | 0.68 |
| Dizzy | 2(2.3) | 1 (1.1) | 0.62 |
| Drowsy | 2(2.3) | 1 (1.1) | 0.62 |
| Confused | 0(0) | 1 (1.1) | 1 |
-
Data presented as N (%) or median (range).
4 Discussion
Our primary objective was to evaluate postoperative pain using non-opioid analgesics that are currently used in our practice. In the immediate postoperative period (0–30 min), pain scores were not significantly different between the ketorolac and intravenous acetaminophen groups; however pain scores were significantly lower in the later postoperative period (45, 60 and 75 min) in the group of patients who received ketorolac.
There are some differences in the pharmacological characteristics of ketorolac and intravenous acetaminophen. The peak plasma concentration (Cmax) of ketorolac occurs within forty five min, and a mean terminal elimination half-life (t1/2) of 5 h [3]. Intravenous acetaminophen is administered over 15 min with an onset of action in ten min, a Cmax of less than thirty min, and t1/2 of 2–4 h [12].
Hong et al. conducted a prospective, randomized, double blinded study, and evaluated postoperative pain in 124 women undergoing an endoscopic thyroidectomy [13]. A placebo group was compared with a group who received one gram of acetaminophen (paracetamol) as a 100 ml solution infused over 15 min 1 h before the induction of anesthesia and then at 6 h intervals for the following 24 h. Pain scores were significantly lower at postoperative hours 1, 3, 6, and 24 in the acetaminophen group when compared with the placebo group. The results also indicated that intravenous acetaminophen reduced overall opioid requirements and provided effective analgesia [13].
Gehling et al. performed a randomized, double blinded, study of 140 patients which compared the effects of intravenous acetaminophen and parecoxib, or their combination for treatment of postoperative pain in patients who underwent thyroid surgery [14]. The results of this study indicated no differences in postoperative pain when the study groups were compared with placebo. Both medications effectively decreased the use of opioid requirements in the postoperative setting. When these medications were given in combination, no further decline in opioid use was observed [14].
Lee et al. performed a randomized, prospective, active, and placebo controlled trial [10]. The study included 80 participants who underwent parathyroidectomies; twenty patients received 1g intravenous acetaminophen, 20 patients received 30 mg IV ketorolac, 20 patients received 700 mg intravenous acetaminophen with 3 mg IV morphine, and 20 patients received a placebo. The results revealed significantly lower VAS scores as well as less rescue opioid administration in all groups except the placebo group. No statistical differences in patient satisfaction regarding pain relief in the three active drug study groups were observed [10].
Achieving pain management without opioid induced side effects of postoperative nausea and vomiting is one major advantage of non-opioid analgesics. Although noted as an observed side effect with its use, most clinical trials studying intravenous acetaminophen state a reduction of postoperative nausea and vomiting when compared with opioids [15]. The observed postoperative complications in the present study revealed a significantly greater occurrence of nausea in the cohort that received intra-venous acetaminophen compared with ketorolac (14% vs. 3%; p < 0.02). Morphine consumption in the current study was minimal and no correlation was found between the occurrences of nausea and its use for supplemental analgesia.
A limitation in this study is the administration times of the two intraoperative analgesics. These however were based on standard practices of care and were administered less than 15 min apart. The timing and dose of ketoralac administered might explain the later onset of postoperative analgesia in these patients, vs. the earlier onset of analgesia after intravenous acetaminophen. Another limitation was short postoperative recovery times, however the minimally invasive nature of our procedure allows patients to be discharged the same day (within 75 min after surgery), reducing the observable timeframe for postoperative analgesia. Additionally, the combination of both analgesics may be superior to either ketorlac or acetaminophen alone, but the adequate pain scores observed with this procedure do not warrant further studies evaluating this.
5 Conclusions and implications
Despite these limitations, our results show previously unknown data regarding two non-opioid analgesics. The adequate analgesia observed in both groups confirms that non-opioid treatment is effective for this ambulatory procedure. In conclusion, we observed analgesia with both postoperative regimens, with slight superiority for ketorolac which provided better pain relief at later time points and less nausea compared with intravenous acetaminophen.
Highlights
Pain scores were collected after minimally invasive radio-guided parathyroidectomy.
Overall analgesic efficacy of intravenous acetaminophen (1 g) and ketorolac (30 mg) were similar.
Patients receiving ketorolac had lower pain scores than those receiving acetaminophen between 45 and 75 min postoperatively.
Lower occurrence of nausea was experienced in the ketorolac group.
DOI of refers to article: http://dx.doi.org/10.1016/j.sjpain.2013.07.018.
Acknowledgements
Tampa General Hospital Research Pharmacy helped randomize and maintain the study blind. The nurses in the parathyroid suite at Tampa General Hospital helped administer rescue medication in the recovery room and maintain patient comfort. This project was funded by a grant from the University Foundation for Education & Research, Tampa, Florida.
-
Conflict of interest
None.
References
[1] Suliburk JW, Perrier ND. Primary hyperparathyroidism. Oncologist 2007;12:644–53.Suche in Google Scholar
[2] Silverberg SJ, Shane E, Jacobs TP, Siris E, Bilezikian JP. A 10-year prospective study of primary hyperparathyroidism with or with out parathyroid surgery. N Engl J Med 1999;341:1249–55.Suche in Google Scholar
[3] Norman J, Politz D. Measuring individual parathyroid gland hormone production in real-time during radioguided parathyroidectomy. Experience in over 8,000 operations. Minerva Endocrinol 2008;33:147–57.Suche in Google Scholar
[4] Norman J, Lopez J, Politz D. Abandoning unilateral parathyroidectomy: why we reversed our position after 15,000 parathyroid operations. J Am Coll Surg 2012;214:260–9.Suche in Google Scholar
[5] Gillis JC, Brogden RN, Ketorolac. A reappraisal of its pharmacodynamic and pharmacokinetic properties and therapeutic use in pain management. Drugs 1997;53:139–88.Suche in Google Scholar
[6] Niemi TT, Backman JT, Syrjälä MT, Viinikka LU, Rosenberg PH. Platelet dysfunction after intravenous ketorolac or propacetamol. Acta Anaesthesiol Scand 2000;44:69–74.Suche in Google Scholar
[7] Chin CJ, Franklin JH, Turner B, Sowerby L, Fung K, Yoo JH. Ketorolac in thyroid surgery: quantifying the risk of hematoma. J Otolaryngol Head Neck Surg 2011 Jun;40(3):196–9.Suche in Google Scholar
[8] Brett CN, Barnett SG, Pearson J. Postoperative plasma paracetamol levels following oral or intravenous paracetamol administration: a double-blind randomised controlled trial. Anaesth Intensive Care 2012;40:166–71.Suche in Google Scholar
[9] Macario A, Royal MA. A literature review of randomized clinical trials of intravenous acetaminophen (paracetamol) for acute postoperative pain. Pain Pract 2011;11:290–6.Suche in Google Scholar
[10] Lee SY, Lee WH, Lee EH, Han KC, Ko YK. The effects of paracetamol, ketorolac, and paracetamol plus morphine on pain control after thyroidectomy. Korean J Pain 2010;23:124–30.Suche in Google Scholar
[11] Schulz KF, Altman DG, Moher D, CONSORT Group. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ 2010;340:c332.Suche in Google Scholar
[12] Jahr J, Lee V. Intravenous acetaminophen. Anesthesiology Clin 2010;28:619–24.Suche in Google Scholar
[13] Hong JY, Kim WO, Chung WY, Yun JS, Kil HK. Paracetamol reduces postoperative pain and rescue analgesic demand after robot-assisted endoscopic thyroidectomy by the transaxillary approach. World J Surg 2010;34:521–6.Suche in Google Scholar
[14] Gehling M, Arndt C, Eberhart LH, Koch T, Kruger T, Wulf H. Postoperative analgesia with parecoxib, acetaminophen, and the combination of both: a randomized, double-blind, placebo-controlled trial in patients undergoing thyroid surgery. Br J Anaesth 2010;104:761–7.Suche in Google Scholar
[15] Sonner JM, Hynson JM, Clark O, Katz JA. Nausea and vomiting following thyroid and parathyroid surgery. J Clin Anesth 1997;9:398–402.Suche in Google Scholar
© 2013 Scandinavian Association for the Study of Pain
Artikel in diesem Heft
- Editorial comment
- Chronic pain – The invisible disease? Not anymore!
- Clinical pain research
- New objective findings after whiplash injuries: High blood flow in painful cervical soft tissue: An ultrasound pilot study
- Editorial comment
- Chronic pain is strongly associated with work disability
- Observational studies
- Chronic pain: One year prevalence and associated characteristics (the HUNT pain study)
- Editorial comment
- Pain rehabilitation in general practice in rural areas? It works!
- Clinical pain research
- Effectiveness of multidisciplinary rehabilitation treatment for patients with chronic pain in a primary health care unit
- Editorial comment
- Mirror-therapy: An important tool in the management of Complex Regional Pain Syndrome (CRPS)
- Topical review
- Mirror therapy for Complex Regional Pain Syndrome (CRPS)—A literature review and an illustrative case report
- Editorial comment
- New insight in migraine pathogenesis: Vasoactive intestinal peptide (VIP) and pituitary adenylate cyclase-activating polypeptide (PACAP) in the circulation after sumatriptan
- Original experimental
- Vasoactive intestinal peptide (VIP) and pituitary adenylate cyclase-activating polypeptide (PACAP) in the circulation after sumatriptan
- Editorial comment
- Statistical pearls: Importance of effect-size, blinding, randomization, publication bias, and the overestimated p-values
- Topical review
- Significance tests in clinical research—Challenges and pitfalls
- Editorial comment
- Biomarkers of pain – Zemblanity?
- Topical review
- Mechanistic, translational, quantitative pain assessment tools in profiling of pain patients and for development of new analgesic compounds
- Editorial comment
- Chronic Benign Paroxysmal Positional Vertigo (BPPV): A possible cause of chronic, otherwise unexplained neck-pain, headache, and widespread pain and fatigue, which may respond positively to repeated particle repositioning manoeuvres (PRM)
- Observational studies
- Pain and other symptoms in patients with chronic benign paroxysmal positional vertigo (BPPV)
- Editorial comment
- The most important step forward in modern medicine, “a giant leap for mankind”: Insensibility to pain during surgery and painful procedures
- Topical review
- In praise of anesthesia: Two case studies of pain and suffering during major surgical procedures with and without anesthesia in the United States Civil War-1861–65
- Editorial comment
- Intravenous non-opioids for immediate postop pain relief in day-case programmes: Paracetamol (acetaminophen) and ketorolac are good choices reducing opioid needs and opioid side-effects
- Clinical pain research
- Intravenous acetaminophen vs. ketorolac for postoperative analgesia after ambulatory parathyroidectomy
- Editorial comment
- Scandinavian Association for the Study of Pain 2013—Annual scientific meeting abstracts of pain research presentations and greetings from incoming President
- Abstracts
- Why does the impact of multidisciplinary pain management on quality of life differ so much between chronic pain patients?
- Abstracts
- Health care utilization in chronic pain—A population based study
- Abstracts
- Pain treatment in rural Ghana—A qualitative study
- Abstracts
- Pain psychology specialist training 2012–2014
- Abstracts
- Pain assessment, documentation, and management in a university hospital
- Abstracts
- Promising effects of donepezil when added to patients treated with gabapentin for neuropathic pain
- Abstracts
- A pediatric patients’ pain evaluation in the emergency unit
- Abstracts
- Proteomic analysis of cerebrospinal fluid gives insight into the pain relief of spinal cord stimulation
- Abstracts
- The DQB1(*)03:02 HLA haplotype is associated with increased risk of chronic pain after inguinal hernia surgery and lumbar disc herniation
- Abstracts
- On the pharmacological effects of two lidocaine concentrations tested on spontaneous and evoked pain in human painful neuroma: A new clinical model of neuropathic pain
- Abstracts
- The mineralocorticoid receptor antagonist spironolactone enhances morphine antinociception
- Abstracts
- Expression of calcium/calmodulin-dependent protein kinase II in dorsal root ganglia in diabetic rats 6 months and 1 year after diabetes induction
- Abstracts
- Histamine in the locus coeruleus attenuates neuropathic hypersensitivity
- Abstracts
- Pronociceptive effects of a TRPA1 channel agonist methylglyoxal in healthy control and diabetic animals
- Abstracts
- Human inducible pluripotent stem cell-derived sensory neurons express multiple functional ion channels and GPCRs
Artikel in diesem Heft
- Editorial comment
- Chronic pain – The invisible disease? Not anymore!
- Clinical pain research
- New objective findings after whiplash injuries: High blood flow in painful cervical soft tissue: An ultrasound pilot study
- Editorial comment
- Chronic pain is strongly associated with work disability
- Observational studies
- Chronic pain: One year prevalence and associated characteristics (the HUNT pain study)
- Editorial comment
- Pain rehabilitation in general practice in rural areas? It works!
- Clinical pain research
- Effectiveness of multidisciplinary rehabilitation treatment for patients with chronic pain in a primary health care unit
- Editorial comment
- Mirror-therapy: An important tool in the management of Complex Regional Pain Syndrome (CRPS)
- Topical review
- Mirror therapy for Complex Regional Pain Syndrome (CRPS)—A literature review and an illustrative case report
- Editorial comment
- New insight in migraine pathogenesis: Vasoactive intestinal peptide (VIP) and pituitary adenylate cyclase-activating polypeptide (PACAP) in the circulation after sumatriptan
- Original experimental
- Vasoactive intestinal peptide (VIP) and pituitary adenylate cyclase-activating polypeptide (PACAP) in the circulation after sumatriptan
- Editorial comment
- Statistical pearls: Importance of effect-size, blinding, randomization, publication bias, and the overestimated p-values
- Topical review
- Significance tests in clinical research—Challenges and pitfalls
- Editorial comment
- Biomarkers of pain – Zemblanity?
- Topical review
- Mechanistic, translational, quantitative pain assessment tools in profiling of pain patients and for development of new analgesic compounds
- Editorial comment
- Chronic Benign Paroxysmal Positional Vertigo (BPPV): A possible cause of chronic, otherwise unexplained neck-pain, headache, and widespread pain and fatigue, which may respond positively to repeated particle repositioning manoeuvres (PRM)
- Observational studies
- Pain and other symptoms in patients with chronic benign paroxysmal positional vertigo (BPPV)
- Editorial comment
- The most important step forward in modern medicine, “a giant leap for mankind”: Insensibility to pain during surgery and painful procedures
- Topical review
- In praise of anesthesia: Two case studies of pain and suffering during major surgical procedures with and without anesthesia in the United States Civil War-1861–65
- Editorial comment
- Intravenous non-opioids for immediate postop pain relief in day-case programmes: Paracetamol (acetaminophen) and ketorolac are good choices reducing opioid needs and opioid side-effects
- Clinical pain research
- Intravenous acetaminophen vs. ketorolac for postoperative analgesia after ambulatory parathyroidectomy
- Editorial comment
- Scandinavian Association for the Study of Pain 2013—Annual scientific meeting abstracts of pain research presentations and greetings from incoming President
- Abstracts
- Why does the impact of multidisciplinary pain management on quality of life differ so much between chronic pain patients?
- Abstracts
- Health care utilization in chronic pain—A population based study
- Abstracts
- Pain treatment in rural Ghana—A qualitative study
- Abstracts
- Pain psychology specialist training 2012–2014
- Abstracts
- Pain assessment, documentation, and management in a university hospital
- Abstracts
- Promising effects of donepezil when added to patients treated with gabapentin for neuropathic pain
- Abstracts
- A pediatric patients’ pain evaluation in the emergency unit
- Abstracts
- Proteomic analysis of cerebrospinal fluid gives insight into the pain relief of spinal cord stimulation
- Abstracts
- The DQB1(*)03:02 HLA haplotype is associated with increased risk of chronic pain after inguinal hernia surgery and lumbar disc herniation
- Abstracts
- On the pharmacological effects of two lidocaine concentrations tested on spontaneous and evoked pain in human painful neuroma: A new clinical model of neuropathic pain
- Abstracts
- The mineralocorticoid receptor antagonist spironolactone enhances morphine antinociception
- Abstracts
- Expression of calcium/calmodulin-dependent protein kinase II in dorsal root ganglia in diabetic rats 6 months and 1 year after diabetes induction
- Abstracts
- Histamine in the locus coeruleus attenuates neuropathic hypersensitivity
- Abstracts
- Pronociceptive effects of a TRPA1 channel agonist methylglyoxal in healthy control and diabetic animals
- Abstracts
- Human inducible pluripotent stem cell-derived sensory neurons express multiple functional ion channels and GPCRs

