Chronic Benign Paroxysmal Positional Vertigo (BPPV): A possible cause of chronic, otherwise unexplained neck-pain, headache, and widespread pain and fatigue, which may respond positively to repeated particle repositioning manoeuvres (PRM)
In this issue of the Scandinavian Journal of Pain, Wenche Iglebekk. Carsten Tjell, and Peter Borenstein [1] report on pain and other symptoms in patients with chronic benign paroxysmal positional vertigo (BPPV).
1 BPPV is a common health problem
Vertigo from BPPV, which is the most common form of vertigo, can be a major handicap for the patient and cause great expenses for the society. Lifetime prevalence is 2.4% [2], indicating 120 000 cases in Norway.
If also dizziness and balance problems are included, 10% of Norwegians claim to have experienced such health problems the last three months [3].
The diagnosis of BPPV is usually based on a history of brief attacks of spinning vertigo and nystagmus provoked by changes in head position [4]. The cause is believed to be otoconia (otoliths) or debris thereof that have loosened from macula utriculi and fallen into one of the semicircular canals (canalolithiasis), most often the posterior canal (80%) of labyrinthus vestibularis in the inner ear (Fig. 1).
Less commonly, the otoconia may be fixed to cupula of crista ampullaris – cupulolithiasis, with somewhat different symptoms and signs.
When the head is moved in a manner that places the semicircular canal in question vertically, the loose otoconia will move downwards by the force of gravity and cause turbulence in the endolymph. This again will cause the stereocilia of the sensory cells at crista ampullaris to deflect, trigging an afferent signal through the vestibular part of the eighth cranial nerve mimicking an angular acceleration of the head. The brain interprets this as if the person is spinning, trigging the vestibulo-ocular reflex which is the cause of the observed nystagmus. In addition to the acute, spinning vertigo, the patient usually is nauseated and may vomit.
Usually acute BPPV can be treated effectively by manipulating the patient in a way that removes the displaced otoconia from the semicircular canal, i.e. particle repositioning manoeuvre (PRM). However, recurrences are common, and sometimes the condition becomes chronic (Fig. 1).
2 Some patients with chronic BPPV may also have incapacitating pain and fatigue
In the present report [1], the authors found that in chronic BPPV, dizziness is more common than spinning vertigo, which is at variance with the usual criterion for the diagnosis BPPV [5]. However, they still observed nystagmus from provocative changes in head position (Dix-Hallpike’s test and PRM).
By extending the observation period for nystagmus after provocative movements, the authors observed nystagmus also in patients that would not be diagnosed with BPPV when following classical diagnostic procedures. The nystagmus was atypical, though, interpreted as caused by displaced otoconia present in more than one semicircular canal.
Almost all of their patients (87%) reported varying types of pain-conditions as a major symptom, and 85% experienced fatigue as well [1]. The authors speculate that pain and fatigue are caused by muscular tension due to a constant challenge of keeping their balance when feeling dizzy, due to conflicting afferent signals from the vestibular system, through vision, and from proprioception. The majority of their patients (75%) were on sick leave [1].
If the authors’ observations and interpretations are correct, the diagnostic criteria of chronic BPPV must possibly be modified.
3 Curative treatment of chronic BPPV also reduces the associated chronic pain
Treatment for chronic BPPV, according to the present report [1] can often be beneficial for the patient’s total situation, including their chronic pain condition as shown by one illustrative case-report of a patient who had chronic pain as his major problem.
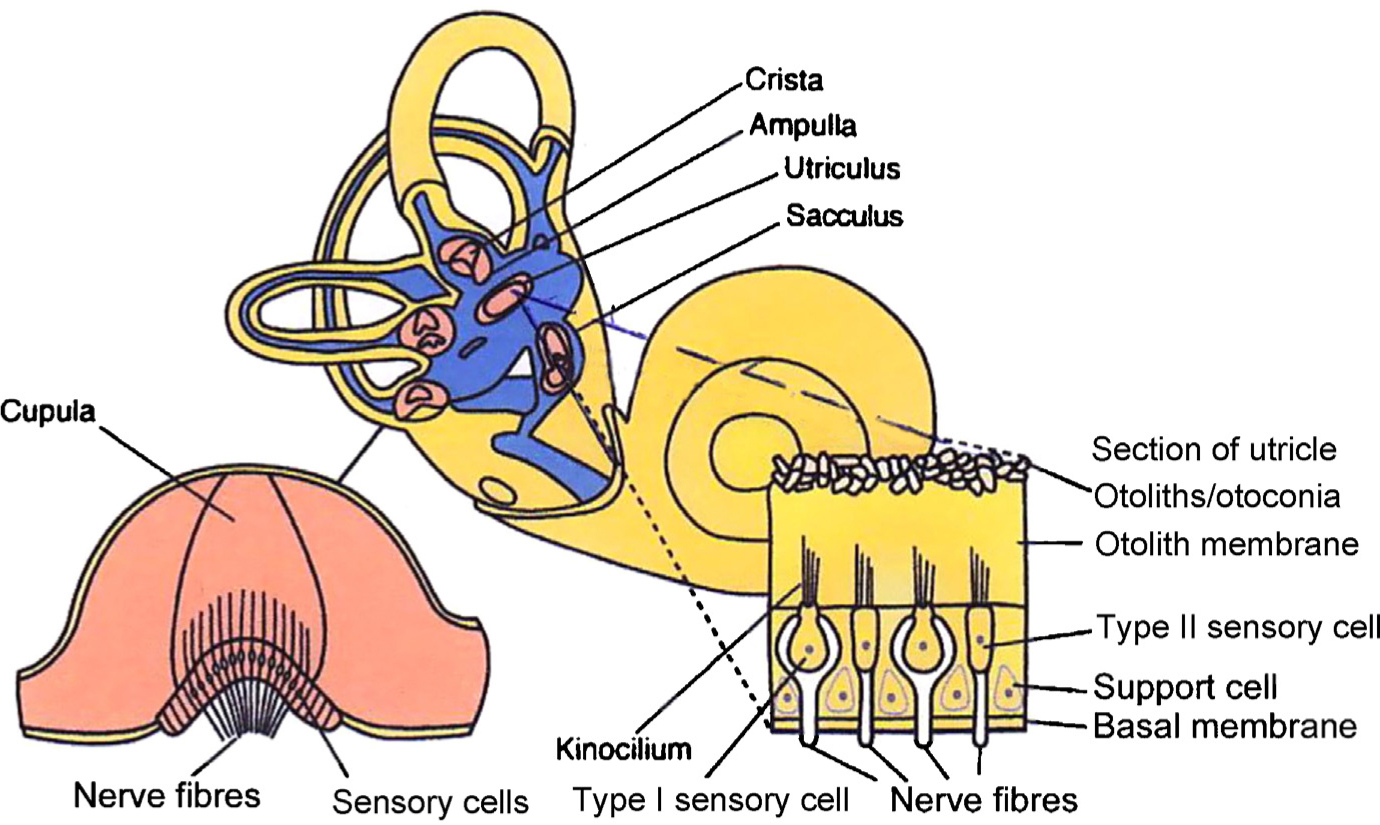
The vestibular labyrinth of auris interna.
Therefore, Iglebekk and co-workers’ results strongly indicate that health care providers should include search for chronic dizziness in their investigation of patients with chronic, unexplained pain [1].
4 Conclusions
The present report suggests an extension of the classical diagnostic criteria for chronic BPPV, the treatment of which benefited their patients with chronic dizziness, chronic pain, fatigue, and other symptoms.
The possibly causative association between vertigo or dizziness and chronic pain is subject to further investigation by Iglebekk and co-workers and is also in progress elsewhere. This shows that there is now much interest in this fairly common condition of treatable benign paroxysmal positional vertigo causing severe pain and other disabling symptoms.
DOI of refers to article: http://dx.doi.org/10.1016/j.sjpain.2013.06.004.
References
[1] Iglebekk W, Tjell C, Borenstein P. Pain and other symptoms in patients with chronic benign paroxysmal positional vertigo. Scand J Pain 2013;4:233–40.Suche in Google Scholar
[2] Von Breven M, Radtke A, Lezius F, Ziese T, Lempert T, Neuhauser H. Epidemiology of benign paroxysmal positional vertigo: a population based study.J Neurol Neurosurg Psychiatry 2007;78:710–5.Suche in Google Scholar
[3] Goplen FK. Svimmelhet. Diagnostikk og behandling. Kompetansesenter for vestibulære sykdommer. Øre-Nese-Halsavdelingen: Haukeland Universitetssykehus; 2009.Suche in Google Scholar
[4] Brandt T, Daroff RB. Physical therapy for benign paroxysmal positional vertigo. Arch Otolaryngol 1980;106:484–5.Suche in Google Scholar
[5] Bhattacharyya N, Baugh RF, Orvides L, Barrs D, Bronston LJ, Cass S, Chalian AA, Desmond AL, Earll JM, Fife TD, Fuller DC, Judge JO, Mann NR, Rosenfeld RM, Schuring LT, Steiner RW, Whitney SL, Haidari J. American academy of otolaryngology-head and neck surgery foundation, clinical practical guideline: benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg 2008;139:S47–81.Suche in Google Scholar
© 2013 Scandiavian Association for the Study of Pain
Artikel in diesem Heft
- Editorial comment
- Chronic pain – The invisible disease? Not anymore!
- Clinical pain research
- New objective findings after whiplash injuries: High blood flow in painful cervical soft tissue: An ultrasound pilot study
- Editorial comment
- Chronic pain is strongly associated with work disability
- Observational studies
- Chronic pain: One year prevalence and associated characteristics (the HUNT pain study)
- Editorial comment
- Pain rehabilitation in general practice in rural areas? It works!
- Clinical pain research
- Effectiveness of multidisciplinary rehabilitation treatment for patients with chronic pain in a primary health care unit
- Editorial comment
- Mirror-therapy: An important tool in the management of Complex Regional Pain Syndrome (CRPS)
- Topical review
- Mirror therapy for Complex Regional Pain Syndrome (CRPS)—A literature review and an illustrative case report
- Editorial comment
- New insight in migraine pathogenesis: Vasoactive intestinal peptide (VIP) and pituitary adenylate cyclase-activating polypeptide (PACAP) in the circulation after sumatriptan
- Original experimental
- Vasoactive intestinal peptide (VIP) and pituitary adenylate cyclase-activating polypeptide (PACAP) in the circulation after sumatriptan
- Editorial comment
- Statistical pearls: Importance of effect-size, blinding, randomization, publication bias, and the overestimated p-values
- Topical review
- Significance tests in clinical research—Challenges and pitfalls
- Editorial comment
- Biomarkers of pain – Zemblanity?
- Topical review
- Mechanistic, translational, quantitative pain assessment tools in profiling of pain patients and for development of new analgesic compounds
- Editorial comment
- Chronic Benign Paroxysmal Positional Vertigo (BPPV): A possible cause of chronic, otherwise unexplained neck-pain, headache, and widespread pain and fatigue, which may respond positively to repeated particle repositioning manoeuvres (PRM)
- Observational studies
- Pain and other symptoms in patients with chronic benign paroxysmal positional vertigo (BPPV)
- Editorial comment
- The most important step forward in modern medicine, “a giant leap for mankind”: Insensibility to pain during surgery and painful procedures
- Topical review
- In praise of anesthesia: Two case studies of pain and suffering during major surgical procedures with and without anesthesia in the United States Civil War-1861–65
- Editorial comment
- Intravenous non-opioids for immediate postop pain relief in day-case programmes: Paracetamol (acetaminophen) and ketorolac are good choices reducing opioid needs and opioid side-effects
- Clinical pain research
- Intravenous acetaminophen vs. ketorolac for postoperative analgesia after ambulatory parathyroidectomy
- Editorial comment
- Scandinavian Association for the Study of Pain 2013—Annual scientific meeting abstracts of pain research presentations and greetings from incoming President
- Abstracts
- Why does the impact of multidisciplinary pain management on quality of life differ so much between chronic pain patients?
- Abstracts
- Health care utilization in chronic pain—A population based study
- Abstracts
- Pain treatment in rural Ghana—A qualitative study
- Abstracts
- Pain psychology specialist training 2012–2014
- Abstracts
- Pain assessment, documentation, and management in a university hospital
- Abstracts
- Promising effects of donepezil when added to patients treated with gabapentin for neuropathic pain
- Abstracts
- A pediatric patients’ pain evaluation in the emergency unit
- Abstracts
- Proteomic analysis of cerebrospinal fluid gives insight into the pain relief of spinal cord stimulation
- Abstracts
- The DQB1(*)03:02 HLA haplotype is associated with increased risk of chronic pain after inguinal hernia surgery and lumbar disc herniation
- Abstracts
- On the pharmacological effects of two lidocaine concentrations tested on spontaneous and evoked pain in human painful neuroma: A new clinical model of neuropathic pain
- Abstracts
- The mineralocorticoid receptor antagonist spironolactone enhances morphine antinociception
- Abstracts
- Expression of calcium/calmodulin-dependent protein kinase II in dorsal root ganglia in diabetic rats 6 months and 1 year after diabetes induction
- Abstracts
- Histamine in the locus coeruleus attenuates neuropathic hypersensitivity
- Abstracts
- Pronociceptive effects of a TRPA1 channel agonist methylglyoxal in healthy control and diabetic animals
- Abstracts
- Human inducible pluripotent stem cell-derived sensory neurons express multiple functional ion channels and GPCRs
Artikel in diesem Heft
- Editorial comment
- Chronic pain – The invisible disease? Not anymore!
- Clinical pain research
- New objective findings after whiplash injuries: High blood flow in painful cervical soft tissue: An ultrasound pilot study
- Editorial comment
- Chronic pain is strongly associated with work disability
- Observational studies
- Chronic pain: One year prevalence and associated characteristics (the HUNT pain study)
- Editorial comment
- Pain rehabilitation in general practice in rural areas? It works!
- Clinical pain research
- Effectiveness of multidisciplinary rehabilitation treatment for patients with chronic pain in a primary health care unit
- Editorial comment
- Mirror-therapy: An important tool in the management of Complex Regional Pain Syndrome (CRPS)
- Topical review
- Mirror therapy for Complex Regional Pain Syndrome (CRPS)—A literature review and an illustrative case report
- Editorial comment
- New insight in migraine pathogenesis: Vasoactive intestinal peptide (VIP) and pituitary adenylate cyclase-activating polypeptide (PACAP) in the circulation after sumatriptan
- Original experimental
- Vasoactive intestinal peptide (VIP) and pituitary adenylate cyclase-activating polypeptide (PACAP) in the circulation after sumatriptan
- Editorial comment
- Statistical pearls: Importance of effect-size, blinding, randomization, publication bias, and the overestimated p-values
- Topical review
- Significance tests in clinical research—Challenges and pitfalls
- Editorial comment
- Biomarkers of pain – Zemblanity?
- Topical review
- Mechanistic, translational, quantitative pain assessment tools in profiling of pain patients and for development of new analgesic compounds
- Editorial comment
- Chronic Benign Paroxysmal Positional Vertigo (BPPV): A possible cause of chronic, otherwise unexplained neck-pain, headache, and widespread pain and fatigue, which may respond positively to repeated particle repositioning manoeuvres (PRM)
- Observational studies
- Pain and other symptoms in patients with chronic benign paroxysmal positional vertigo (BPPV)
- Editorial comment
- The most important step forward in modern medicine, “a giant leap for mankind”: Insensibility to pain during surgery and painful procedures
- Topical review
- In praise of anesthesia: Two case studies of pain and suffering during major surgical procedures with and without anesthesia in the United States Civil War-1861–65
- Editorial comment
- Intravenous non-opioids for immediate postop pain relief in day-case programmes: Paracetamol (acetaminophen) and ketorolac are good choices reducing opioid needs and opioid side-effects
- Clinical pain research
- Intravenous acetaminophen vs. ketorolac for postoperative analgesia after ambulatory parathyroidectomy
- Editorial comment
- Scandinavian Association for the Study of Pain 2013—Annual scientific meeting abstracts of pain research presentations and greetings from incoming President
- Abstracts
- Why does the impact of multidisciplinary pain management on quality of life differ so much between chronic pain patients?
- Abstracts
- Health care utilization in chronic pain—A population based study
- Abstracts
- Pain treatment in rural Ghana—A qualitative study
- Abstracts
- Pain psychology specialist training 2012–2014
- Abstracts
- Pain assessment, documentation, and management in a university hospital
- Abstracts
- Promising effects of donepezil when added to patients treated with gabapentin for neuropathic pain
- Abstracts
- A pediatric patients’ pain evaluation in the emergency unit
- Abstracts
- Proteomic analysis of cerebrospinal fluid gives insight into the pain relief of spinal cord stimulation
- Abstracts
- The DQB1(*)03:02 HLA haplotype is associated with increased risk of chronic pain after inguinal hernia surgery and lumbar disc herniation
- Abstracts
- On the pharmacological effects of two lidocaine concentrations tested on spontaneous and evoked pain in human painful neuroma: A new clinical model of neuropathic pain
- Abstracts
- The mineralocorticoid receptor antagonist spironolactone enhances morphine antinociception
- Abstracts
- Expression of calcium/calmodulin-dependent protein kinase II in dorsal root ganglia in diabetic rats 6 months and 1 year after diabetes induction
- Abstracts
- Histamine in the locus coeruleus attenuates neuropathic hypersensitivity
- Abstracts
- Pronociceptive effects of a TRPA1 channel agonist methylglyoxal in healthy control and diabetic animals
- Abstracts
- Human inducible pluripotent stem cell-derived sensory neurons express multiple functional ion channels and GPCRs

