Abstract
Context
A variety of manual manipulation techniques are utilized in clinical practice to alleviate pain and improve musculoskeletal function. Many manual practitioners analyze gait patterns and asymmetries in their assessment of the patient, and an increasing number of gait motion capture studies are taking place with recent improvements in motion capture technology. This study is the first systematic review of whether these manual modalities have been shown to produce an objectively measurable change in gait mechanics.
Objectives
This study was designed to perform a systematic review of the literature to assess the impact of manual medicine modalities on biomechanical parameters of gait.
Methods
A master search term composed of keywords and Medical Subject Headings (MeSH) search terms from an initial scan of relevant articles was utilized to search six databases. We screened the titles and abstracts of the resulting papers for relevance and then assessed their quality with the Cochrane Risk of Bias Tool. Clinical trials that featured both a manual manipulation intervention and multiple mechanical gait parameters were included. Case reports and other studies that only measured gait speed or other subjective measures of mobility were excluded.
Results
We included 20 studies in our final analysis. They utilize manipulation techniques primarily from osteopathic, chiropractic, massage, and physiotherapy backgrounds. The conditions studied primarily included problems with the back, knee, and ankle, as well as healthy patients and Parkinson’s patients. Control groups were highly variable, if not absent. Most studies measured their gait parameters utilizing either multicamera motion capture systems or force platforms.
Conclusions
Twelve of 20 papers included in the final analysis demonstrated a significant effect of manipulation on gait variables, many of which included either step length, walking speed, or sagittal range of motion (ROM) in joints of the lower extremity. However, the results and study design are too heterogeneous to draw robust conclusions from these studies as a whole. While there are initial indications that certain modalities may yield a change in certain gait parameters, the quality of evidence is low and there is insufficient evidence to conclude that manual therapies induce changes in biomechanical gait parameters. Studies are heterogeneous with respect to the populations studied and the interventions performed. Comparators were variable or absent across the studies, as were the outcome variables measured. More could be learned in the future with consistent methodology around blinding and sham treatment, and if the gait parameters measured were standardized and of a more robust clinical significance.
Manual manipulation is an adjunctive therapy utilized by many practitioners to help relieve pain, improve physical function, and decrease disease burden for patients with a variety of musculoskeletal and systemic conditions. Manual manipulation has been shown to be cost-effective and efficacious for musculoskeletal conditions when compared with general practitioner care [1]. Prominent schools of manual manipulation include osteopathic manipulative treatment (OMT), chiropractic manipulation, massage, and physiotherapy joint mobilization, all of which have been shown to have efficacy for a variety of conditions. OMT has been shown to provide clinical benefit for patients with chronic low back pain (n=433) [2], neck pain (n=90) [3], and patellofemoral pain syndrome (n=82) [4]. Systematic reviews have shown the clinical benefits of chiropractic manipulation for patients with low back pain [5] and neck pain [6]. Massage is efficacious for patients with knee osteoarthritis (OA) (n=175) [7, 8] and has been shown to reduce delayed-onset muscle soreness after exercise (n=78) [9]. Finally, systematic reviews have demonstrated clinical benefits of joint mobilization therapy in patients with frozen shoulder [10], lateral ankle sprain [11], and knee OA [12].
Gait, or the steady state of walking, requires the integration of multiple types of sensory information from somatosensory, vestibular, and visual systems in addition to the active engagement of cortical integration of sensory input with motor output, central pattern generators, reflex systems, and complex executive functions [13]. Manual therapy can improve overall posture including head position, thoracic kyphosis, and pelvic position [14]. It has also been demonstrated to improve postural stability, balance, strength, and range of motion (ROM) [15], [16], [17], [18]. These improvements may be mediated through changes that manipulation can affect in motor unit behavior, cortical drive, cortical processing, sensorimotor integration, motor control, joint position sense, and central integration [19], [20], [21], [22], [23], [24], [25], [26]. Manipulative treatment may also improve pain conditions, such as knee OA, that may alter gait [27]. It is therefore reasonable to expect that manual therapy intervention could influence gait by means of changing any or all of these factors.
Historically, decreased gait speed has been identified as a useful clinical indicator of poor long-term health outcomes in elderly patients [28, 29]. Slower gait speed has also been associated with impaired activities of daily living and is an important predictor of health-related quality of life [30, 31]. Poor mobility, with gait speed as the most commonly reported mobility measure, has been associated with depressive symptoms [32]. In addition, there is significant evidence to support that variability in gait is associated and may be predictive of future fall risk, especially in elderly patients [32], [33], [34], [35], [36], [37], [38], [39], [40], [41], [42]. The impacts of falls in this population include high morbidity and mortality as well as poor overall health, stress, depression, and loss of independence [43], [44], [45]. Gait also plays a role in injury progression in the lower extremity, hips, and back, all of which are affected by symmetry and magnitude of forces that impact the body during each step [46], [47], [48]. Finally, gait disturbance due to concussion has been demonstrated, and although we identified no trials studying the effect of manipulation on gait in concussion patients, this represents an emerging field of study [49].
With the improvement in motion capture camera technology, gait analysis has become a popular area of study for medical researchers in a variety of fields. Many manual medicine practitioners have identified objective gait analysis systems as a tool that could provide additional evidence basis for the efficacy, and potentially an underlying mechanism of action, of their treatments. In theory, identifying gait parameters that reliably predict clinical health outcomes in a certain population and then demonstrate an ability to consistently improve that parameter with manipulation could provide robust evidence of the efficacy of the treatment.
In this study, we assess all available research investigating the impact of a manual manipulation intervention on a patient’s gait utilizing mechanical gait analysis variables as their primary outcome measure.
Methods
An initial search was performed in PubMed with the following terms along with “gait”: osteopathic, chiropractic, manual medicine, manipulative medicine, manual therapy, massage, and manual-therapy physical therapy (PT). Relevant papers were reviewed for Medical Subject Headings (MESH) search terms and keywords, and after compiling an initial list, the research team (SY, SF, BH, TM, AF) agreed on a final list of search terms to be utilized in each database search (Figure 1). The following databases were searched on June 21, 2022 utilizing our keywords: CINAHL (Cumulative Index to Nursing and Allied Health Literature), PubMed, Scopus, SPORTDiscus, Trip Database Pro, Embase (Excerpta Medica dataBASE).
The master search terms.
Search results yielded 5,532 total results that were aggregated in Rayyan. The software automatically removed 220 duplicates and flagged an additional 570 papers as potential duplicates. The research team scanned the titles and abstracts for relevance, excluding case reports and any study that did not include both a manual therapy intervention and a stated outcome measure involving gait. Review papers were excluded, but their references were scanned for relevant studies. This narrowed the initial search results down to 115 papers for consideration. Of that group, 27 were selected for further analysis as they demonstrated both a manual manipulation intervention and a mechanical measurement of gait parameters in their outcome data. Of note, functional assessments of gait such as the Western Ontario and McMaster Universities Arthritis (WOMAC) Index, which is a 24-point questionnaire utilized to assess pain, stiffness, and function in knee and hip OA, were insufficient for inclusion. Papers utilizing gait speed as their only gait parameter were also excluded. Within the final inclusion group, three papers were excluded because they were not available in English, and four were excluded due to insufficient description of their methods, bringing the final count of papers for analysis to 20 (Figure 2). Included papers were assessed for risk of bias utilizing the Cochrane Risk of Bias Tool for Randomized Trials. Disagreements among the research team were addressed through whole-group discussion until a consensus was reached.
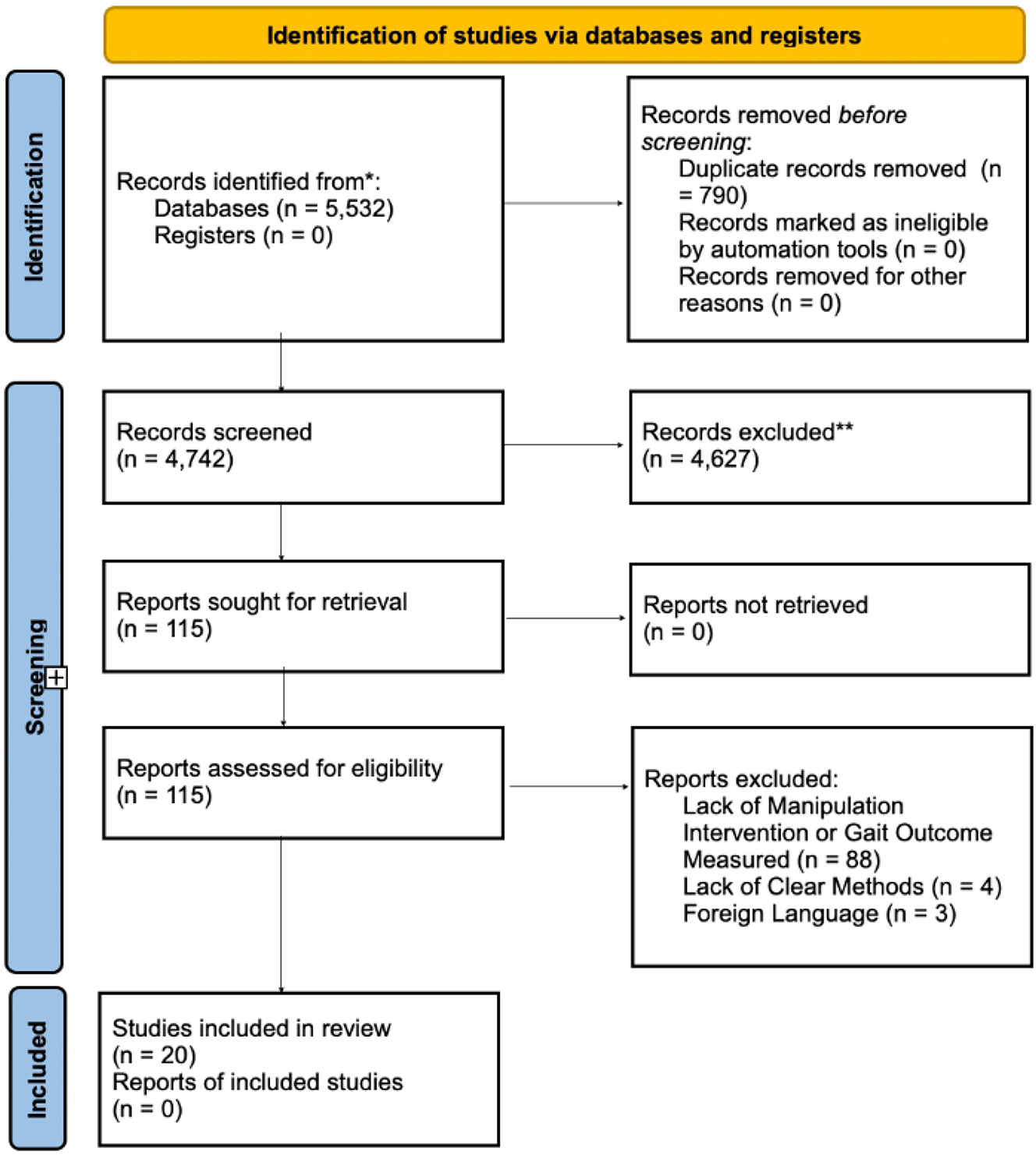
The study flow throughout the review of search results.
Results
Full PICO (P – Patient, problem, or population; I – Intervention; C – Comparison, control or comparator; O – Outcome[s]) breakdown of the included studies can be seen in Table 1. The 20 studies ranged in size from 9 to 100 subjects, with two studying women only, one men only, and 17 all sexes. The studies involved 787 subjects in total, 419 men and 331 women, and 37 sex not specified. Ages studied ranged from 15 to 70. The conditions studied included healthy subjects, knee OA, Parkinson’s disease, low back pain, chronic sacroiliac (SI) joint problems, acute-inversion ankle sprain, restriction in knee extension after ACL surgery, and abnormal gait after stroke.
PICO+ results from 20 analyzed studies.
| Author | Year | n= | Power analysis | Population/condition | Intervention | Frequency | Comparison | Measure | Outcome variables | Risk of bias | Result |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Green et al. | 2001 | 41 | No | Acute ankle sprain | Joint mobilization+RICE | 7 sessions in 2 weeks or until discharge | Taping+RICE | Single video camera | GS, SL, SST, GSym | High | Pos |
| Herzog et al. | 1991 | 37 | No | Chronic SI joint dysfunction | Chiropractic spinal manipulation | 10 sessions in 4 weeks | Back school | Force platform/treadmill | VGRF, APGRF, MLGRF | High | Pos |
| Wojtowicz et al. | 2017 | 57 | No | Healthy adults | Chiropractic SI joint manipulation | Single session | Waiting period | Force platform/treadmill | AFF, AFB, FR, SL, StrL, DSP%, ST, StrT, Cad, MPF, MPM, MPH | High | Pos |
| Ward et al. | 2013 | 12 | No | Healthy adults | Chiropractic SI joint manipulation | Not reported | No manipulation | MoCap | SHA, SKA, SAA, DST, StaT, SL, StrL | Low | Neg |
| Ward et al. | 2014 | 21 | No | Healthy adults | Chiropractic drop table SI joint manipulation | Not reported | No manipulation | MoCap | SHA, SKA, SAA, DST, StaT, SL, StrL | Moderate | Neg |
| Ditcharles et al. | 2017 | 22 | No | Healthy adults | T9 HVLA | Single session | Sham treatment | Force platform/treadmill | APCOGAcc, COGV, COGD, FC, TO, APAs | Moderate | Pos |
| Hill et al. | 2021 | 42 | Yes | Healthy adults | Whole body OMT | Single session | No control | MoCap | SL, StrL, StaT, VGRF, VGRFI, PKFA | High | Neg |
| Gopalswami et al. | 2021 | 100 | Yes | Knee DJD | Joint mobilization, MET, interferential therapy, exercise, education | 6 sessions in 2 weeks | Interferential therapy, exercises, education | Footprint method | StrL, SL, Cad | High | Neg |
| Robinson et al. | 1987 | 9 | No | Low back pain | Chiropractic SI joint manipulation | Single session | No control | Force platform/treadmill | Described 46 gait variables | High | Neg |
| Herzog et al. | 1988 | 11 | No | Low back pain | Chiropractic SI joint manipulation | 7 sessions in 2 weeks | No control | Force platform/treadmill | MLGRF, VGRF, APGRF | High | Pos |
| Krekoukias et al. | 2021 | 75 | Yes | Low back pain | Manual therapy | 5 sessions in 5 weeks | 1. Stretching, TENS unit, massage. 2. Sham treatment | MoCap | GRF, trunk and pelvis symmetry | Moderate | Pos |
| Kang et al. | 2015 | 24 | Yes | Men with <10 degrees of DF ROM of the ankle in knee extension | Joint mobilization+stretching | Single session | Stretching | MoCap | THO, ADFHO | Low | Pos |
| Wells et al. | 1999 | 28 | No | Parkinson’s disease | Standardized whole body OMT protocol | Single session | Sham treatment | MoCap | StrL, Cad, SV, AV, WV, HV, KV, AnV | Moderate | Pos |
| Terrell et al. | 2022 | 84 | Yes | Parkinson’s disease | Whole body OMT | Single session | 1. Neck down OMT 2. Sham treatment | 18 camera motion capture system with dual belt treadmill | SHA, SKA, SAA | Low | Neg |
| Hunt et al. | 2010 | 12 | No | Limited knee ext post ACL surgery | Anterio tibiofemoral glides | Single session | No control | MoCap | SL, StrL, GS, SKA | High | Pos |
| Vismara et al. | 2016 | 45 | No | Prader Willi syndrome | Whole body OMT | Single session | No manipulation | MoCap | GS, Cad, stance%, SL, SHA, SKA, SAA, ICAK, MinKFMS, MaxKFS, PADSt, MinAAS, PADSw, MaxAPFTS, MaxAPTS, MVF | High | Pos |
| Albin et al. | 2019 | 72 | Yes | Open reduction internal fixation of ankle fracture | Joint mobilization | 3 sessions in 10 days | Sham treatment | Force platform/treadmill | GS, StaT, stance% | Low | Neg |
| Cho et al. | 2020 | 45 | Yes | Stroke | Joint mobilization+stretching | Single session | 1. Joint mobilization 2. Stretching | G Walk gait sensor | Cad, StrL, GS | Low | Neg |
| Zhu et al. | 2015 | 20 | No | Women with knee OA | Chinese massage | 6 sessions in 2 weeks | No control | MoCap | GS, SL, SW, TST, IDST, SST, ICAA, ICAK, ICAH | High | Pos |
| Sabet et al. | 2021 | 30 | Yes | Women with knee OA | Swedish massage | 12 sessions in 4 weeks | No manipulation | MoCap | GS, StrL, SW, TST, IDST, SST | Moderate | Pos |
-
PICO, P – Patient, problem, or population; I – Intervention; C – Comparison, control or comparator; O – Outcome[s]; DGD, degenerative joint disease; MoCap, multicamera motion capture system with reflective markers; GS, gait speed; SL, step length; SST, single support time; GSym, gait symmetry; VGRF, vertical ground reaction force; VGRFI, vertical ground reaction force impulse; APGRF, anteroposterior ground reaction force; MLGRF, mediolateral ground reaction force; AFF, average force forefoot; AFB, average force backfoot; FR, foot rotation; StrL, stride length; DSP%, double stance phase%; ST, step time; StrT, stride time; Cad, cadence; MPF, max pressure forefoot; MPM, max pressure mid foot; MPH, max pressure heel; SHA, sagittal hip angle; SKA, sagittal knee angle; SAA, sagittal ankle angle; DST, double support time; StaT, stance time; APCOGAcc, anteroposterior center of gravity acceleration; COGV, center of gravity velocity; COGD, center of gravity displacement; FC, foot contact; TO, toe off; APAs, anticipatory postural adjustments; PKFA, peak knee flexion angle; THO, time to heel off; ADFHO, ankle dorsiflexion before heel off; SV, shoulder velocity; AV, arm velocity; WV, wrist velocity; HV, hip velocity; KV, knee velocity; AnV, ankle velocity; TST, total support time; IDST, initial double support time; ICAK, initial contact angle of knee; ICAH, initial contact angle of hip; ICAA, initial contact angle of ankle; SW, step width; MinKFMS, minimum knee flexion in mid stance; MaxKFS, maximum knee flexion in swing; PADSt, peak ankle dorsiflexion during stance; MinAAS, minimum ankle angle in stance; PADSw, peak ankle dorsiflexion in swing; MaxAPFTS, maximum ankle plantar flexion in terminal stance; MaxAPTS, maximum ankle power in terminal stance; MVF, maximum vertical force; MET, muscle energy technique; RICE, rest, ice, compression, and elevation; SI, sacroiliac; HVLA, high-velocity, low-amplitude; GRF, ground reaction force; DFROM, dorsiflexion range of motion; TENS, transcutaneous electrical nerve stimulation.
The interventions studied were PT, osteopathic, chiropractic, and massage. The interventions varied in number and length of treatment sessions, and in treatment of specific body part vs. whole-body treatment. The most commonly utilized interventions included whole-body OMT, ankle joint mobilization, and chiropractic manipulation to the SI joint.
Interventions were assessed against many different types of control conditions. Although some studies utilized sham manual treatment, stretching, or other well-established conservative treatments, many studies compared their manipulation group to a “no manipulation” control, whereas others did not include a control group at all.
Mechanical gait parameters were primarily measured utilizing either a multicamera motion capture system utilizing reflective markers placed on standardized body locations, or some variation of a force platform walkway or treadmill that measured forces transmitted from the subject into the floor during the gait cycle. Some studies utilized both technologies simultaneously. The most commonly assessed gait variables included stride length, step length, step width, walking speed (m/s), walking cadence (steps/minute), stance time, stance percentage, double support time, single support time, vertical ground reaction force (VGRF), and the sagittal angle of the ankle, knee, and hip throughout gait. Significant changes in mechanical gait parameters were reported in 12 out of the 20 included studies.
Risk of bias analysis yielded 10 papers with a high risk of bias, five with a moderate risk of bias, and five with a low risk of bias. Eight studies performed power analysis, whereas 12 did not describe power analysis methodology [50], [51], [52], [53], [54], [55], [56], [57], [58], [59], [60], [61], [62], [63], [64], [65], [66], [67], [68], [69]. Six studies were identified that were considered to have a low or moderate risk of bias and that also conducted a power analysis. Among those studies were four manual physiotherapy studies, one massage study on knee OA, and one whole-body OMT study in Parkinson’s patients.
Discussion
Overall, 12 of the 20 studies found a significant effect of manipulation on their gait parameters. However, a high risk of bias, a small sample, and the presence of significant heterogeneity of design between studies makes it irresponsible to draw any robust conclusions from this group of studies as a whole or to perform a meta-analysis. Although some subgroups of studies do have notable overlap in the style of intervention, gait analysis methodology, and gait variables measured, significant variability still exists in terms of disease state of the population of interest, specifics of the intervention implemented, extent and nature of comparison groups, and outcome measures deemed to be most pertinent by the research groups. This prevailing heterogeneity would undermine the validity of any conclusions drawn from an analysis of any cluster of these studies.
Additionally, many of the studies included were either at high risk of bias, or failed to perform a power analysis, creating further barriers to drawing firm conclusions from their findings, whether positive or negative.
We identified six studies considered low or moderate risk of bias that also conducted a power analysis, including four manual physiotherapy studies, one massage study on knee OA, and one whole-body OMT study in Parkinson’s patients.
Krekoukias et al. [60] demonstrated a positive clinical effect of five sessions of manual therapy in patients with low back pain, along with a weak trend toward symmetrical gait. Albin et al. [66] found no significant changes in gait after three sessions of manual therapy to the ankles of patients postsurgical fixation of ankle or midfoot fracture. Cho and Park [67] demonstrated increases in cadence, stride length, and speed among stroke patients receiving a single session of joint mobilization and stretching, or just stretching, to the ankle joint. However, these treatment groups outperformed the group undergoing joint mobilization alone, pointing to stretching as the primary mediator of their findings [67]. Among healthy patients with limited ankle dorsiflexion range of motion (DF ROM), Kang et al. [61] demonstrated increased time to heel off and DF ROM before heel off after a single session of joint mobilization and stretching. In contrast to the stroke study by Cho and Park [67], Kang et al. [61] found that this treatment outperformed the stretching alone group, pointing to joint mobilization as the mediator of their observed effect.
Terrell et al. [63] compared the effect of one session of whole-body OMT, neck-down OMT, and sham treatment on gait in a population of Parkinson’s patients. Although they reported improved hip ROM in the whole-body OMT group, they found no significant difference in their gait parameters, including the sagittal angle of the hip, knee, and ankle throughout the gait cycle [63].
Finally, Sabet et al. [68] demonstrated significant changes in clinical measures and gait parameters in women with knee OA after 12 sessions of Swedish massage. They reported increases in speed, total support time, and single support time, along with decreases in step width and initial double support time [68]. This study was considered to have a moderate risk of bias, and utilized a “usual treatment” group as their control group, leaving open the possibility that a similar level of significance could have been found with a light touch or sham massage control group. Of note, Qingguang et al. [69] investigated the effect of six sessions of Chinese massage on women with knee OA. While they also reported significant increases in gait speed and total support time, they reported increases in step width [69], which contrasts with the findings of Sabet et al [68]. While interpretation of these studies taken together should be guarded because they include a study at high risk of bias, they may serve as an example for future gait and manipulation studies, because they utilized similar overall study design and gait analysis methodology. With a reduced risk of bias and increased sample size, studies like these could be analyzed together to make a stronger overall conclusion regarding the effect of massage on gait in women with knee OA.
Limitations
Of note, we only analyzed studies utilizing mechanical gait measurement systems, and we excluded many manipulation studies that utilized subjective, clinically oriented mobility indices like the timed up and go (TUG) test and the WOMAC Index. Although these indices may lack the precision of computer-generated data, they have a significant head start in terms of their established significance in the clinical setting [70]. By excluding these studies, we were left with a group of studies looking at a conglomeration of gait variables, very few of which were grounded with a clear description of clinical significance.
While certain gait variables have been shown to have a consistent clinical significance, the majority of common variables for analysis have poor or mixed results in the currently available literature. Gait changes associated with increased risk of falls in the elderly include increased double support time variability, double support time, and step length variability, and decreased stride length and gait speed, although these last two associations have been challenged by some authors [71], [72], [73], [74], [75], [76]. Knee OA has been associated with reduced gait speed and increased stride time variability, but these studies were not designed to establish directional causality [31]. In recreational runners, increased prospective injury risk was associated with increased stride length and flight time, and decreased contact time and ratio of contact time:stride time. VGRFs are commonly thought to mediate running-related injury. While two studies found a greater VGRF loading rate in runners with stress fracture and plantar fasciitis, the majority of the available evidence found no association between VGRFs and the risk for running-related injury [77], [78], [79].
Conclusions
While the literature demonstrates specific populations where gait analysis can provide reliable clinical utility, the majority of studies looking to establish clinical significance have yielded mixed or negative results. Additionally, very few of these studies have established directional causality, which weakens our ability to make claims about the benefits of a potential change in gait due to manipulation. Nevertheless, objective measurement of mechanical gait parameters represents an intriguing method for investigating the effect of manual manipulation on gait and the role of gait in overall health.
Further research and standardization of the measurement of motion capture collected gait variables seen across the studies in this review is needed in order to evaluate significance and assess clinical relevance and predictive values. Lack of concordance between clinical data like symptom and functionality questionnaires and the gait metrics that were reported in many of these studies further underlines the need for future studies in which gait variables can demonstrate a reliable association with improved clinical outcomes. The premise that a faster or more symmetric gait is associated with improved clinical outcomes was a working assumption for many of the authors reviewed in this study, but those premises need more investigation before being broadly accepted in larger populations of interest.
Lastly, creating a methodological consensus around blinding, sham treatment, and measurement of relevant gait variables will be crucial to create the conditions for higher-quality manipulation and gait studies. Future research will benefit from this standardization, because it will allow for larger-scale aggregation of data for high-powered meta-analysis, yielding more robust conclusions about the impact of manipulation on gait.
Acknowledgments
The authors would like to thank Adam Foster, PhD (Associate Professor of Anatomy, CUSOM) for assisting with the initial literature search and large-scale article review process; and Sarah Wade, MLS, AHIP (CUSOM Medical Librarian) for assisting with the literature search, organization of our sources, acquiring full text copies of studies, and ensuring adequacy of the paper’s citations.
-
Research ethics: Not applicable.
-
Informed consent: Not applicable.
-
Author contributions: The authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Competing interests: None declared.
-
Research funding: None declared.
-
Data availability: Not applicable.
References
1. Tsertsvadze, A, Clar, C, Court, R, Clarke, A, Mistry, H, Sutcliffe, P. Cost-effectiveness of manual therapy for the management of musculoskeletal conditions: a systematic review and narrative synthesis of evidence from randomized controlled trials. J Manip Physiol Ther 2014;37:343–62. https://doi.org/10.1016/j.jmpt.2014.05.001.Suche in Google Scholar PubMed
2. Licciardone, JC, Gatchel, RJ, Aryal, S. Recovery from chronic low back pain after osteopathic manipulative treatment: a randomized controlled trial. J Osteopath Med 2016;116:144–55. https://doi.org/10.7556/jaoa.2016.031.Suche in Google Scholar PubMed
3. Groisman, S, Malysz, T, De Souza Da Silva, L, Rocha Ribeiro Sanches, T, Camargo Bragante, K, Locatelli, F, et al.. Osteopathic manipulative treatment combined with exercise improves pain and disability in individuals with non-specific chronic neck pain: a pragmatic randomized controlled trial. J Bodyw Mov Ther 2020;24:189–95. https://doi.org/10.1016/j.jbmt.2019.11.002.Suche in Google Scholar PubMed
4. Zago, J, Amatuzzi, F, Rondinel, T, Matheus, JP. Osteopathic manipulative treatment versus exercise program in runners with patellofemoral pain syndrome: a randomized controlled trial. J Sport Rehabil 2020;30:609–18. https://doi.org/10.1123/jsr.2020-0108.Suche in Google Scholar PubMed
5. Blanchette, MA, Stochkendahl, MJ, Borges Da Silva, R, Boruff, J, Harrison, P, Bussières, A. Effectiveness and economic evaluation of chiropractic care for the treatment of low back pain: a systematic review of pragmatic studies. PLoS One 2016;11:e0160037. https://doi.org/10.1371/journal.pone.0160037.Suche in Google Scholar PubMed PubMed Central
6. Chaibi, A, Stavem, K, Russell, MB. Spinal manipulative therapy for acute neck pain: a systematic review and meta-analysis of randomised controlled trials. J Clin Med 2021;10:5011. https://doi.org/10.3390/jcm10215011.Suche in Google Scholar PubMed PubMed Central
7. Perlman, A, Fogerite, SG, Glass, O, Bechard, E, Ali, A, Njike, VY, et al.. Efficacy and safety of massage for osteoarthritis of the knee: a randomized clinical trial. J Gen Intern Med 2019;34:379–86. https://doi.org/10.1007/s11606-018-4763-5.Suche in Google Scholar PubMed PubMed Central
8. Wu, Q, Zhao, J, Guo, W. Efficacy of massage therapy in improving outcomes in knee osteoarthritis: a systematic review and meta-analysis. Complement Ther Clin Pract 2022;46:101522. https://doi.org/10.1016/j.ctcp.2021.101522.Suche in Google Scholar PubMed
9. Naderi, A, Aminian-Far, A, Gholami, F, Mousavi, SH, Saghari, M, Howatson, G. Massage enhances recovery following exercise-induced muscle damage in older adults. Scand J Med Sci Sports 2021;31:623–32. https://doi.org/10.1111/sms.13883.Suche in Google Scholar PubMed
10. Rahbar, M, Ranjbar Kiyakalayeh, S, Mirzajani, R, Eftekharsadat, B, Dolatkhah, N. Effectiveness of acromioclavicular joint mobilization and physical therapy vs physical therapy alone in patients with frozen shoulder: a randomized clinical trial. Clin Rehabil 2022;36:669–82. https://doi.org/10.1177/02692155211070451.Suche in Google Scholar PubMed
11. Loudon, JK, Reiman, MP, Sylvain, J. The efficacy of manual joint mobilisation/manipulation in treatment of lateral ankle sprains: a systematic review. Br J Sports Med 2014;48:365–70. https://doi.org/10.1136/bjsports-2013-092763.Suche in Google Scholar PubMed
12. Tsokanos, A, Livieratou, E, Billis, E, Tsekoura, M, Tatsios, P, Tsepis, E, et al.. The efficacy of manual therapy in patients with knee osteoarthritis: a systematic review. Medicina 2021;57:696. https://doi.org/10.3390/medicina57070696.Suche in Google Scholar PubMed PubMed Central
13. Mirelman, A, Shema, S, Maidan, I, Hausdorff, JM. Chapter 7 – gait. In: Day, BL, Lord, SR, editors. Handbook of clinical neurology. Vol 159. Balance, gait, and falls. Tel Aviv, Israel: Elsevier; 2018:119–34 pp.10.1016/B978-0-444-63916-5.00007-0Suche in Google Scholar PubMed
14. Santos, TS, Oliveira, KKB, Martins, LV, Vidal, APC. Effects of manual therapy on body posture: systematic review and meta-analysis. Gait Posture 2022;96:280–94. https://doi.org/10.1016/j.gaitpost.2022.06.010.Suche in Google Scholar PubMed
15. Holt, KR, Haavik, H, Elley, CR. The effects of manual therapy on balance and falls: a systematic review. J Manip Physiol Ther 2012;35:227–34. https://doi.org/10.1016/j.jmpt.2012.01.007.Suche in Google Scholar PubMed
16. Galindez-Ibarbengoetxea, X, Setuain, I, Andersen, LL, Ramírez-Velez, R, González-Izal, M, Jauregi, A, et al.. Effects of cervical high-velocity low-amplitude techniques on range of motion, strength performance, and cardiovascular outcomes: a review. J Altern Complement Med 2017;23:667–75. https://doi.org/10.1089/acm.2017.0002.Suche in Google Scholar PubMed
17. Lo, CN, Ng, J, Au, CK, Lim, ECW. The effectiveness of spinal manipulation in increasing muscle strength in healthy individuals: a systematic review and meta-analysis. J Manip Physiol Ther 2019;42:148–58. https://doi.org/10.1016/j.jmpt.2018.10.003.Suche in Google Scholar PubMed
18. Wong, CK, Conway, L, Fleming, G, Gopie, C, Liebeskind, D, Xue, S. Immediate effects of a single spinal manipulation on lower-limb strength in healthy individuals: a critically appraised topic. J Sport Rehabil 2020;30:161–5. https://doi.org/10.1123/jsr.2019-0372.Suche in Google Scholar PubMed
19. Christiansen, TL, Niazi, IK, Holt, K, Nedergaard, RW, Duehr, J, Allen, K, et al.. The effects of a single session of spinal manipulation on strength and cortical drive in athletes. Eur J Appl Physiol 2018;118:737–49. https://doi.org/10.1007/s00421-018-3799-x.Suche in Google Scholar PubMed PubMed Central
20. Robinault, L, Holobar, A, Crémoux, S, Rashid, U, Niazi, IK, Holt, K, et al.. The effects of spinal manipulation on motor unit behavior. Brain Sci 2021;11:105. https://doi.org/10.3390/brainsci11010105.Suche in Google Scholar PubMed PubMed Central
21. Haavik, H, Murphy, B. The role of spinal manipulation in addressing disordered sensorimotor integration and altered motor control. J Electromyogr Kinesiol 2012;22:768–76. https://doi.org/10.1016/j.jelekin.2012.02.012.Suche in Google Scholar PubMed
22. Holt, KR, Haavik, H, Lee, ACL, Murphy, B, Elley, CR. Effectiveness of chiropractic care to improve sensorimotor function associated with falls risk in older people: a randomized controlled trial. J Manip Physiol Ther 2016;39:267–78. https://doi.org/10.1016/j.jmpt.2016.02.003.Suche in Google Scholar PubMed
23. Daligadu, J, Haavik, H, Yielder, PC, Baarbe, J, Murphy, B. Alterations in cortical and cerebellar motor processing in subclinical neck pain patients following spinal manipulation. J Manip Physiol Ther 2013;36:527–37. https://doi.org/10.1016/j.jmpt.2013.08.003.Suche in Google Scholar PubMed
24. Haavik, H, Niazi, IK, Jochumsen, M, Sherwin, D, Flavel, S, Türker, KS. Impact of spinal manipulation on cortical drive to upper and lower limb muscles. Brain Sci 2017;7:2. https://doi.org/10.3390/brainsci7010002.Suche in Google Scholar PubMed PubMed Central
25. Taylor, HH, Murphy, B. The effects of spinal manipulation on central integration of dual somatosensory input observed after motor training: a crossover study. J Manip Physiol Ther 2010;33:261–72. https://doi.org/10.1016/j.jmpt.2010.03.004.Suche in Google Scholar PubMed
26. Haavik, H, Murphy, B. Subclinical neck pain and the effects of cervical manipulation on elbow joint position sense. J Manip Physiol Ther 2011;34:88–97. https://doi.org/10.1016/j.jmpt.2010.12.009.Suche in Google Scholar PubMed
27. Tsokanos, A, Livieratou, E, Billis, E, Tsekoura, M, Tatsios, P, Tsepis, E, et al.. The efficacy of manual therapy in patients with knee osteoarthritis: a systematic review. Medicina 2021;57:696. https://doi.org/10.3390/medicina57070696.Suche in Google Scholar PubMed PubMed Central
28. Afilalo, J, Eisenberg, MJ, Morin, JF, Bergman, H, Monette, J, Noiseux, N, et al.. Gait speed as an incremental predictor of mortality and major morbidity in elderly patients undergoing cardiac surgery. J Am Coll Cardiol 2010;56:1668–76. https://doi.org/10.1016/j.jacc.2010.06.039.Suche in Google Scholar PubMed
29. Peel, NM, Kuys, SS, Klein, K. Gait speed as a measure in geriatric assessment in clinical settings: a systematic review. J Gerontol A Biol Sci Med Sci 2013;68:39–46. https://doi.org/10.1093/gerona/gls174.Suche in Google Scholar PubMed
30. Lee, M, Noh, Y, Youm, C, Kim, S, Park, H, Noh, B, et al.. Estimating health-related quality of life based on demographic characteristics, questionnaires, gait ability, and physical fitness in Korean elderly adults. Int J Environ Res Public Health 2021;18:11816. https://doi.org/10.3390/ijerph182211816.Suche in Google Scholar PubMed PubMed Central
31. Wang, DXM, Yao, J, Zirek, Y, Reijnierse, EM, Maier, AB. Muscle mass, strength, and physical performance predicting activities of daily living: a meta-analysis. J Cachexia Sarcopenia Muscle 2020;11:3–25. https://doi.org/10.1002/jcsm.12502.Suche in Google Scholar PubMed PubMed Central
32. Chan, LLY, Okubo, Y, Brodie, MA, Lord, SR. Mobility performance predicts incident depression: a systematic review and meta-analysis. Exp Gerontol 2020;142:111116. https://doi.org/10.1016/j.exger.2020.111116.Suche in Google Scholar PubMed
33. Marques, NR, Spinoso, DH, Cardoso, BC, Moreno, VC, Kuroda, MH, Navega, MT. Is it possible to predict falls in older adults using gait kinematics? Clin Biomech 2018;59:15–18. https://doi.org/10.1016/j.clinbiomech.2018.08.006.Suche in Google Scholar PubMed
34. Marques, NR, Camilo, GF, De Martini Lopes Dos Santos, AP, Cardoso, BC, Navega, MT, De Abreu, DCC. The ability of gait kinematic parameters to predict falls in older adults with cognitive impairments living in long term institutions. Clin Biomech 2019;65:123–7. https://doi.org/10.1016/j.clinbiomech.2019.04.011.Suche in Google Scholar PubMed
35. Taguchi, CK, Teixeira, JP, Alves, LV, Oliveira, PF, Raposo, OFF. Quality of life and gait in elderly group. Int Arch Otorhinolaryngol 2016;20:235–40. https://doi.org/10.1055/s-0035-1570313.Suche in Google Scholar PubMed PubMed Central
36. Masud, T, Morris, RO. Epidemiology of falls. Age Ageing 2001;30:3–7. https://doi.org/10.1093/ageing/30.suppl_4.3.Suche in Google Scholar PubMed
37. Adam, CE, Fitzpatrick, AL, Leary, CS, Hajat, A, Ilango, SD, Park, C, et al.. Change in gait speed and fall risk among community-dwelling older adults with and without mild cognitive impairment: a retrospective cohort analysis. BMC Geriatr 2023;23:328. https://doi.org/10.1186/s12877-023-03890-6.Suche in Google Scholar PubMed PubMed Central
38. Kyrdalen, IL, Thingstad, P, Sandvik, L, Ormstad, H. Associations between gait speed and well-known fall risk factors among community-dwelling older adults. Physiother Res Int J Res Clin Phys Ther 2019;24:e1743. https://doi.org/10.1002/pri.1743.Suche in Google Scholar PubMed
39. Verghese, J, Holtzer, R, Lipton, RB, Wang, C. Quantitative gait markers and incident fall risk in older adults. J Gerontol A Biol Sci Med Sci 2009;64:896–901. https://doi.org/10.1093/gerona/glp033.Suche in Google Scholar PubMed PubMed Central
40. Ganz, DA, Bao, Y, Shekelle, PG, Rubenstein, LZ. Will my patient fall? JAMA 2007;297:77–86. https://doi.org/10.1001/jama.297.1.77.Suche in Google Scholar PubMed
41. Auvinet, B, Berrut, G, Touzard, C, Moutel, L, Collet, N, Chaleil, D, et al.. Gait abnormalities in elderly fallers. J Aging Phys Act 2003;11:40–52. https://doi.org/10.1123/japa.11.1.40.Suche in Google Scholar
42. Weiss, A, Brozgol, M, Dorfman, M, Herman, T, Shema, S, Giladi, N, et al.. Does the evaluation of gait quality during daily life provide insight into fall risk? A novel approach using 3-day accelerometer recordings. Neurorehabil Neural Repair 2013;27:742–52. https://doi.org/10.1177/1545968313491004.Suche in Google Scholar PubMed
43. Jónsdóttir, HL, Ruthig, JC. A longitudinal study of the negative impact of falls on health, well-being, and survival in later life: the protective role of perceived control. Aging Ment Health 2021;25:742–8. https://doi.org/10.1080/13607863.2020.1725736.Suche in Google Scholar PubMed
44. Siracuse, JJ, Odell, DD, Gondek, SP, Odom, SR, Kasper, EM, Hauser, CJ, et al.. Health care and socioeconomic impact of falls in the elderly. Am J Surg 2012;203:335–8. https://doi.org/10.1016/j.amjsurg.2011.09.018.Suche in Google Scholar PubMed
45. Bergen, G, Stevens, MR, Burns, ER. Falls and fall injuries among adults aged ≥65 years – United States, 2014. MMWR Morb Mortal Wkly Rep 2016;65:993–8. https://doi.org/10.15585/mmwr.mm6537a2.Suche in Google Scholar PubMed
46. Murray, KJ, Molyneux, T, Le Grande, MR, Castro Mendez, A, Fuss, FK, Azari, MF. Association of mild leg length discrepancy and degenerative changes in the hip joint and lumbar spine. J Manip Physiol Ther 2017;40:320–9. https://doi.org/10.1016/j.jmpt.2017.03.001.Suche in Google Scholar PubMed
47. Xu, Y, Yuan, P, Wang, R, Wang, D, Liu, J, Zhou, H. Effects of foot strike techniques on running biomechanics: a systematic review and meta-analysis. Sports Health 2021;13:71–7. https://doi.org/10.1177/1941738120934715.Suche in Google Scholar PubMed PubMed Central
48. Chan, ZYS, Zhang, JH, Au, IPH, An, WW, Shum, GL, Ng, GY, et al.. Gait retraining for the reduction of injury occurrence in novice distance runners: 1-year follow-up of a randomized controlled trial. Am J Sports Med 2018;46:388–95. https://doi.org/10.1177/0363546517736277.Suche in Google Scholar PubMed
49. Manaseer, TS, Gross, DP, Dennett, L, Schneider, K, Whittaker, JL. Gait deviations associated with concussion: a systematic review. Clin J Sport Med 2020;30:S11–28. https://doi.org/10.1097/JSM.0000000000000537.Suche in Google Scholar PubMed
50. Green, T, Refshauge, K, Crosbie, J, Adams, R. A randomized controlled trial of a passive accessory joint mobilization on acute ankle inversion sprains. Phys Ther 2001;81:984–94. https://doi.org/10.1093/ptj/81.4.984.Suche in Google Scholar
51. Herzog, W, Conway, PJ, Willcox, BJ. Effects of different treatment modalities on gait symmetry and clinical measures for sacroiliac joint patients. J Manip Physiol Ther 1991;14:104–9.Suche in Google Scholar
52. Herzog, W, Nigg, BM, Read, LJ. Quantifying the effects of spinal manipulations on gait using patients with low back pain. J Manip Physiol Ther 1988;11:151–7.Suche in Google Scholar
53. Wojtowicz, S, Sajko, I, Hadamus, A, Mosiolek, A, Bialoszewski, D. Effect of sacroiliac joint manipulation on selected gait parameters in healthy subjects. Ortop Traumatol Rehabil 2017;19:323–31. https://doi.org/10.5604/01.3001.0010.4640.Suche in Google Scholar PubMed
54. Ward, J, Sorrels, K, Coats, J, Pourmoghaddam, A, DeLeon, C, Daigneault, P. Pilot study of the impact that bilateral sacroiliac joint manipulation using a drop table technique has on gait parameters in asymptomatic individuals with a leg length inequality. J Can Chiropr Assoc 2014;58:85–95.Suche in Google Scholar
55. Ward, JS, Coats, J, Sorrels, K, Walters, M, Williams, T. Pilot study of the impact sacroiliac joint manipulation has on walking kinematics using motion analysis technology. J Chiropr Med 2013;12:143–52. https://doi.org/10.1016/j.jcm.2013.05.001.Suche in Google Scholar PubMed PubMed Central
56. Ditcharles, S, Yiou, E, Delafontaine, A, Hamaoui, A. Short-term effects of thoracic spine manipulation on the biomechanical organisation of gait initiation: a randomized pilot study. Front Hum Neurosci 2017;11:343. https://doi.org/10.3389/fnhum.2017.00343.Suche in Google Scholar PubMed PubMed Central
57. Hill, CN, Romero, M, Rogers, M, Queen, RM, Brolinson, PG. Effect of osteopathic manipulation on gait asymmetry. J Osteopath Med 2021;122:85–94. https://doi.org/10.1515/jom-2021-0046.Suche in Google Scholar PubMed
58. Gopalswami, AD, Kumar, SS, Sinha, AG. Gait parameters and functional performance following multi-factorial treatment among degenerative joint disease patients. Biomed India 2021;41:112–19. https://doi.org/10.51248/.v41i1.544.Suche in Google Scholar
59. Robinson, RO, Herzog, W, Nigg, BM. Use of force platform variables to quantify the effects of chiropractic manipulation on gait symmetry. J Manip Physiol Ther 1987;10:172–6.Suche in Google Scholar
60. Krekoukias, G, Sakellari, V, Anastasiadi, E, Gioftsos, G, Dimitriadis, Z, Soultanis, K, et al.. Gait kinetic and kinematic changes in chronic low back pain patients and the effect of manual therapy: a randomized controlled trial. J Clin Med 2021;10:3593. https://doi.org/10.3390/jcm10163593.Suche in Google Scholar PubMed PubMed Central
61. Kang, MH, Oh, JS, Kwon, OY, Weon, JH, An, DH, Yoo, WG. Immediate combined effect of gastrocnemius stretching and sustained talocrural joint mobilization in individuals with limited ankle dorsiflexion: a randomized controlled trial. Man Ther 2015;20:827–34. https://doi.org/10.1016/j.math.2015.03.016.Suche in Google Scholar PubMed
62. Wells, MR, Giantinoto, S, D’Agate, D, Areman, RD, Fazzini, EA, Dowling, D, et al.. Standard osteopathic manipulative treatment acutely improves gait performance in patients with Parkinson’s disease. J Am Osteopath Assoc 1999;99:92–8. https://doi.org/10.7556/jaoa.1999.99.2.92.Suche in Google Scholar PubMed
63. Terrell, ZT, Moudy, SC, Hensel, KL, Patterson, RM. Effects of osteopathic manipulative treatment vs. osteopathic cranial manipulative medicine on Parkinsonian gait. J Osteopath Med 2022;122:243–51. https://doi.org/10.1515/jom-2021-0203.Suche in Google Scholar PubMed
64. Hunt, MA, Di Ciacca, SR, Jones, IC, Padfield, B, Birmingham, TB. Effect of anterior tibiofemoral glides on knee extension during gait in patients with decreased range of motion after anterior cruciate ligament reconstruction. Physiother Can 2010;62:235–41. https://doi.org/10.3138/physio.62.3.235.Suche in Google Scholar PubMed PubMed Central
65. Vismara, L, Cimolin, V, Galli, M, Grugni, G, Ancillao, A, Capodaglio, P. Osteopathic manipulative treatment improves gait pattern and posture in adult patients with Prader-Willi syndrome. Int J Osteopath Med 2016;19:35–43. https://doi.org/10.1016/j.ijosm.2015.09.001.Suche in Google Scholar
66. Albin, SR, Koppenhaver, SL, Marcus, R, Dibble, L, Cornwall, M, Fritz, JM. Short-term effects of manual therapy in patients after surgical fixation of ankle and/or hindfoot fracture: a randomized clinical trial. J Orthop Sports Phys Ther 2019;49:310–19. https://doi.org/10.2519/jospt.2019.8864.Suche in Google Scholar PubMed
67. Cho, KH, Park, SJ. Effects of joint mobilization and stretching on the range of motion for ankle joint and spatiotemporal gait variables in stroke patients. J Stroke Cerebrovasc Dis 2020;29:104933. https://doi.org/10.1016/j.jstrokecerebrovasdis.2020.104933.Suche in Google Scholar PubMed
68. Sabet, F, Ebrahimipour, E, Mohammadipour, F, Daneshjoo, A, Jafarnezhadgero, A. Effects of Swedish massage on gait spatiotemporal parameters in adult women with medial knee osteoarthritis: a randomized controlled trial. J Bodyw Mov Ther 2021;28:521–6. https://doi.org/10.1016/j.jbmt.2021.09.008.Suche in Google Scholar PubMed
69. Qingguang, Z, Min, F, Li, G, Shuyun, J, Wuquan, S, Jianhua, L, et al.. Gait analysis of patients with knee osteoarthritis before and after Chinese massage treatment. J Tradit Chin Med 2015;35:411–16. https://doi.org/10.1016/s0254-6272(15)30117-5.Suche in Google Scholar PubMed
70. You, Y, Liu, J, Tang, M, Wang, D, Ma, X. Effects of Tai Chi exercise on improving walking function and posture control in elderly patients with knee osteoarthritis: a systematic review and meta-analysis. Medicine 2021;100:e25655. https://doi.org/10.1097/MD.0000000000025655.Suche in Google Scholar PubMed PubMed Central
71. Modarresi, S, Divine, A, Grahn, JA, Overend, TJ, Hunter, SW. Gait parameters and characteristics associated with increased risk of falls in people with dementia: a systematic review. Int Psychogeriatr 2019;31:1287–303. https://doi.org/10.1017/S1041610218001783.Suche in Google Scholar PubMed
72. Boekesteijn, RJ, Van Gerven, J, Geurts, ACH, Smulders, K. Objective gait assessment in individuals with knee osteoarthritis using inertial sensors: a systematic review and meta-analysis. Gait Posture 2022;98:109–20. https://doi.org/10.1016/j.gaitpost.2022.09.002.Suche in Google Scholar PubMed
73. Thaler-Kall, K, Peters, A, Thorand, B, Grill, E, Autenrieth, CS, Horsch, A, et al.. Description of spatio-temporal gait parameters in elderly people and their association with history of falls: results of the population-based cross-sectional KORA-Age study. BMC Geriatr 2015;15:32. https://doi.org/10.1186/s12877-015-0032-1.Suche in Google Scholar PubMed PubMed Central
74. Bytyçi, I, Henein, MY. Stride length predicts adverse clinical events in older adults: a systematic review and meta-analysis. J Clin Med 2021;10:2670. https://doi.org/10.3390/jcm10122670.Suche in Google Scholar PubMed PubMed Central
75. Abellan Van Kan, G, Rolland, Y, Andrieu, S, Bauer, J, Beauchet, O, Bonnefoy, M, et al.. Gait speed at usual pace as a predictor of adverse outcomes in community-dwelling older people an International Academy on Nutrition and Aging (IANA) Task Force. J Nutr Health Aging 2009;13:881–9. https://doi.org/10.1007/s12603-009-0246-z.Suche in Google Scholar PubMed
76. Beck, JD, Robinson, K, Ogliari, G, Montero-Odasso, M, Kamkar, N, Ryg, J, et al.. Predicting falls in older adults: an umbrella review of instruments assessing gait, balance, and functional mobility. BMC Geriatr 2022;22:615. https://doi.org/10.1186/s12877-022-03271-5.Suche in Google Scholar PubMed PubMed Central
77. Ceyssens, L, Vanelderen, R, Barton, C, Malliaras, P, Dingenen, B. Biomechanical risk factors associated with running-related injuries: a systematic review. Sports Med 2019;49:1095–115. https://doi.org/10.1007/s40279-019-01110-z.Suche in Google Scholar PubMed
78. Malisoux, L, Gette, P, Delattre, N, Urhausen, A, Theisen, D. Spatiotemporal and ground-reaction force characteristics as risk factors for running-related injury: a secondary analysis of a randomized trial including 800+ recreational runners. Am J Sports Med 2022;50:537–44. https://doi.org/10.1177/03635465211063909.Suche in Google Scholar PubMed
79. van der Worp, H, Vrielink, JW, Bredeweg, SW. Do runners who suffer injuries have higher vertical ground reaction forces than those who remain injury-free? A systematic review and meta-analysis. Br J Sports Med 2016;50:450. https://doi.org/10.1136/bjsports-2015-094924.Suche in Google Scholar PubMed
© 2024 the author(s), published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.
Artikel in diesem Heft
- Frontmatter
- Medical Education
- Original Article
- Assessing nutrition literacy and nutrition counseling proficiency following an interdisciplinary culinary medicine elective
- Neuromusculoskeletal Medicine (OMT)
- Original Article
- Investigating Fryette’s mechanics in computed tomography scans: an analysis of vertebrae spinal physiology using open-sourced datasets and three-dimensional vertebral orientation
- Review Article
- Effect of manual manipulation on mechanical gait parameters
- Obstetrics and Gynecology
- Original Article
- The impact of prepregnancy body mass index on pregnancy and neonatal outcomes
- Public Health and Primary Care
- Original Article
- Associations of clinical personnel characteristics and telemedicine practices
- Clinical Image
- Davener’s dermatosis: a unique presentation of frictional hypermelanosis
- Letters to the Editor
- Fostering a research culture in osteopathic medical education
- Response to “Fostering a research culture in osteopathic medical education”
- Corrigendum
- Corrigendum to: A superficial dissection approach to the sphenopalatine (pterygopalatine) ganglion to emphasize osteopathic clinical relevance
Artikel in diesem Heft
- Frontmatter
- Medical Education
- Original Article
- Assessing nutrition literacy and nutrition counseling proficiency following an interdisciplinary culinary medicine elective
- Neuromusculoskeletal Medicine (OMT)
- Original Article
- Investigating Fryette’s mechanics in computed tomography scans: an analysis of vertebrae spinal physiology using open-sourced datasets and three-dimensional vertebral orientation
- Review Article
- Effect of manual manipulation on mechanical gait parameters
- Obstetrics and Gynecology
- Original Article
- The impact of prepregnancy body mass index on pregnancy and neonatal outcomes
- Public Health and Primary Care
- Original Article
- Associations of clinical personnel characteristics and telemedicine practices
- Clinical Image
- Davener’s dermatosis: a unique presentation of frictional hypermelanosis
- Letters to the Editor
- Fostering a research culture in osteopathic medical education
- Response to “Fostering a research culture in osteopathic medical education”
- Corrigendum
- Corrigendum to: A superficial dissection approach to the sphenopalatine (pterygopalatine) ganglion to emphasize osteopathic clinical relevance

