Effects of face masks on oxygen saturation at graded exercise intensities
-
Varnita Vishwanath
Abstract
Context
Mask wearing to mitigate the spread of COVID-19 and other viral infections may raise concerns on the effects of face masks on breathing and cardiopulmonary health. Non–evidence-based apprehensions may limit the use of masks in public.
Objectives
We will assess the parameters related to heart and lung physiology between healthy male and female adults exposed to wearing face masks (or not) under conditions of rest and graded exercise.
Methods
We performed a cross-sectional study including 20 male and 20 female adults who met our inclusion criteria. Adults with underlying respiratory and cardiac conditions were excluded. Physiologic parameters were measured while the participants underwent three activity levels (10 min each) in a randomly assigned order: rest, walking, and stair climbing. Each activity level was conducted under three mask conditions: no mask, surgical mask, and N95 respirator. Heart rate (HR) and blood oxygen saturation (SpO2) were recorded via pulse oximeter after each activity. Perceived exertion was recorded utilizing a Borg 15-point scale. A mixed-effects analysis of variance (ANOVA) was utilized to interpret the results.
Results
A significant increase in perceived exertion was reported for N95 users (p<0.0001). There was also a significant increase in mean HR for N95 users in comparison to no-mask users (p=0.0031). The mean SpO2 in females was higher than males under rest and walking conditions (p=0.0055). There was no change in SpO2 between mask type overall, nor between mask type vs. exercise intensity, nor between mask type and sex.
Conclusions
Our findings provide evidence that surgical masks and N95 respirators do not influence SpO2 at rest or during exercise.
COVID-19 (SARS-CoV-2) is a coronavirus that has progressed into an international concern to public health. The persistent global spread of the virus, primarily through respiratory droplet exposure [1], prompted the declaration of the COVID-19 pandemic on March 11, 2020, by the World Health Organization [2]. As a health initiative, the Centers for Disease Control and Prevention (CDC) recommended the use of face masks to prevent person-to-person spread of the virus. Two weeks after implementing statewide mask mandates in the United States, the weekly hospitalization growth rate declined by 2.9% among adults ages 40–64 years and declined by 5.5% among adults ages 18–39 years [1]. In a social survey that assessed mask usage among 19 million adults worldwide, global trends show an increase in mask usage from April 20, 2020, to February 17, 2021 [3], [4], [5]. Face masks control emissions of infected saliva and respiratory droplets, which substantiates a sustained public compliance to mask wearing to protect one another and slow the spread of COVID-19 [6, 7].
Numerous variations exist in the types of face masks available to the public, such as homemade cloth masks, surgical masks, cone-style masks, N95, and KN95. The lack of standardization results in a diversity of masks that may be perceived as discrepant in effectiveness. Existing differences in state regulations on mask mandates further raises public concern on whether masks affect our breathing and cardiorespiratory health [8]. A study by Gericke and Gupta [9] evaluated responses from 280 individuals from local gyms and social media outlets who had exercised with a mask, and found that perceived alterations to normal physiology while exercising with a mask were psychological in nature; masks inherently were not the cause of physiologic changes. Non–evidence-based apprehensions against masks may limit their use within the general population.
The comfort level of masks among healthcare workers (n=76) was evaluated by Nwosu et al. [10], via an 11-point Likert scale; they demonstrated that despite a greater perceived discomfort of the N95 mask compared to the surgical mask, neither mask affected arterial oxygen saturation [10]. Additionally, Fikenzer et al. [11] evaluated the perceived comfort of masks among 12 healthcare workers and showed that breathing resistance, heat, tightness, and overall discomfort have the greatest influence on the subjective discomfort of wearing masks. The goal of our study was to address public concerns on mask use by assessing the effects of surgical and N95 masks, in comparison to no-mask usage, on peripheral oxygen saturation (SpO2) during rest and graded exercise intensities. A relatively recent study evaluated the physiological effects of surgical masks and N95 masks, yet it was limited to a single-arm variable by solely examining two masks while only strenuously exercising and found no significant difference in SpO2 [12]. Our study aimed to conduct a comparative assessment of the effects of surgical masks and N95 masks in comparison to no mask at rest and graded exercise on heart rate (HR) and SpO2 among healthy adults. We aimed to highlight the comparative differences between males and females at all mask and exercise conditions that had not been reported in the literature to date. Our study also assessed the perceived level of physical exertion via the Borg 15-point scale to understand the participative experience of mask wearing during rest and exercise. By evaluating perceived exertion in addition to HR and SpO2, we aimed to provide evidence that mask wearing would not impose negative effects on cardiorespiratory function among healthy adults. The data from our study may provide a baseline of physiologic variables for comparison in future studies.
Materials and methods
Eligibility criteria
This study was approved by the Midwestern University (MWU) Institutional Review Board (IRB, AZ#1422). The inclusion criteria for this study included adults between 21 and 75 years of age with no underlying heart or respiratory illness. Participants who had knowledge of an existing medical condition that can hinder their ability to perform the study, such as hypertension, diabetes mellitus types I and II, and respiratory and cardiovascular illnesses, were excluded. The exclusion criteria were presented as a list to each individual participant. Data were collected from November 2020 to May 2021. Our study participants consisted of both males and females from MWU, including faculty and students. The health assessment was performed on a self-assessment basis. All participants provided written informed consent by signing paper consent forms that were collected by the study observers. In addition, participants filled out MWU’s COVID-19 health questionnaire upon enrollment into the study. The participant’s age, height, and BMI were collected prior to the start of the activity. HR and SpO2 via pulse oximeter were collected after every completion of each activity level. All experiments were performed on university campus grounds abiding by university and CDC guidelines on social distancing.
Study design
A cross-sectional study was performed where physiological parameters were measured while the participants participated in three activity levels (duration of 10 min each) in a randomly assigned order: rest (sitting), walking, and exercise (stair climbing), with a minimum of 30 min of rest between each exercise. Participants served as their own controls. Participants conducted every activity level wearing every face mask condition separately: no mask, surgical mask (Morestep, disposable medical mask, model 175 × 95 mm), and N95 respirator (3M 1860). Thus, a total of nine activities were completed by each participant (Figure 1). In the walking condition, participants walked at an average pace of 110 steps/minute, and in the stair-climbing condition, participants climbed stairs at an average pace of 122 steps/minute.
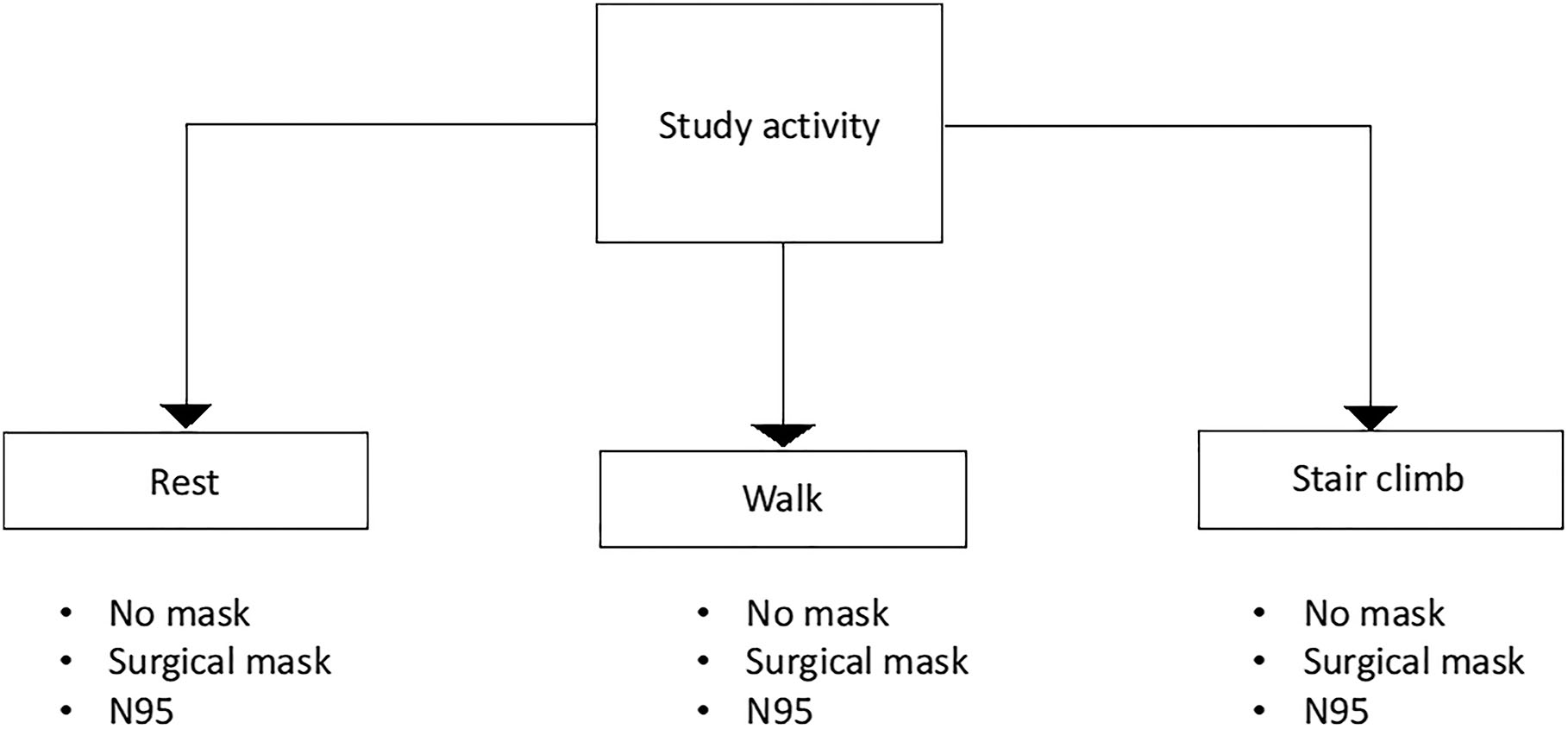
Representative diagram of study activities. Participants performed each activity (rest, walk, stair climb) under every mask condition (no mask, surgical mask, N95). Each activity was performed for 10 min. For rest, the subject remained seated. For walk, the subject walked a designated course. For stair climbing, the subject climbed a designated three-flight stair set.
Physical assessment and pulse oximetry
To quantify physical activity difficulty, the Borg 15-point scale of perceived exertion was utilized. This scale is a participative analysis of the perceived intensity experienced by the participants. The scale ranges from 6 to 20 (Figure 2). The device utilized to measure SpO2 was the McKesson Fingertip Pulse Oximeter (MFR#16-93651, McKesson, Richmond, VA), which provides rapid, non-invasive assessment of the participant’s SpO2 and pulse rate. Per the manufacturer’s website, the McKesson Pulse Oximeter has the following sensitivities: measures pulse rates between 30 and 235 bpm with an accuracy of ±2%, measures SpO2 levels ranging from 70 to 99% with an accuracy of ±3%, and requires no calibration. Pulse oximeter SpO2 measurements were taken immediately at completion of each timed activity.
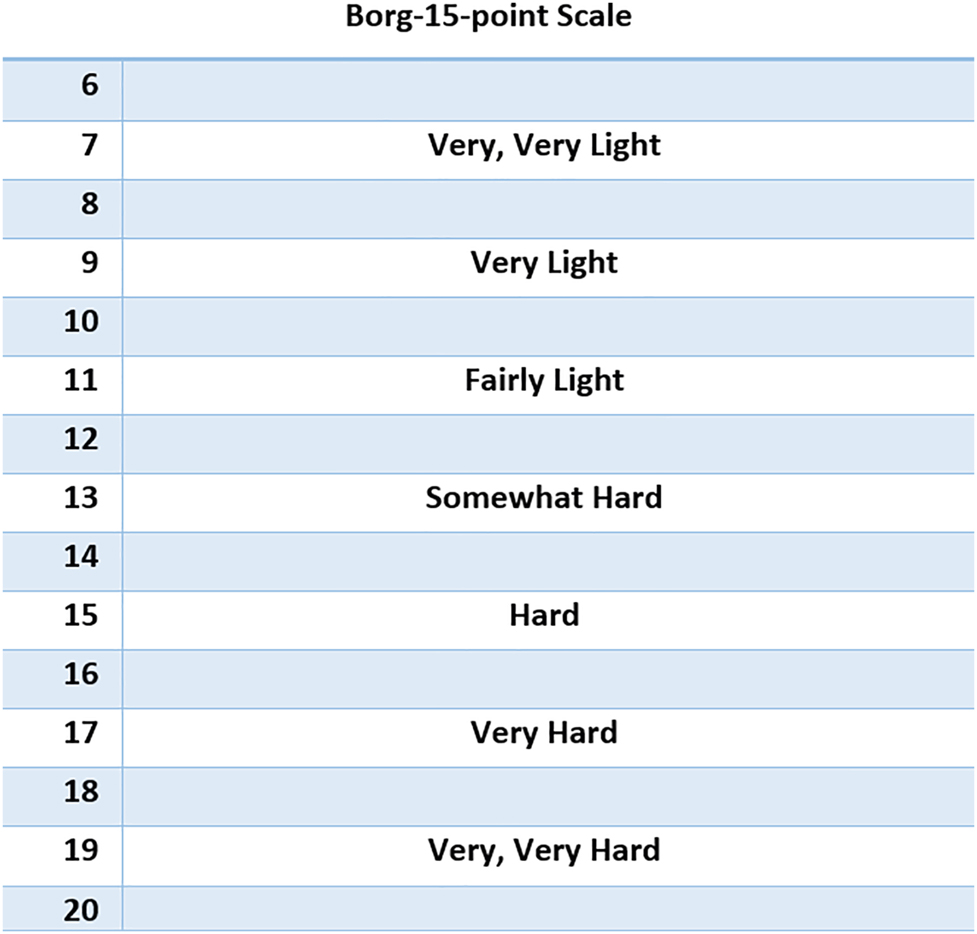
The Borg 15-point scale was utilized to evaluate the participants’ perceived exertion after each study activity.
The scale ranges from 6 to 20, reflecting a range between very light exertion to very hard.
Data analysis
To examine the variability of HR, Borg 15-point scale, and SpO2 between groups (mask, exercise, and sex variables) and within participants, a mixed-effects analysis of variance (ANOVA) model was utilized. Each participant in the study provided multiple observations and the data were correlated with one another, thus the mixed-effects ANOVA model accounts for the variability of the outcome per participant. The mixed-effects ANOVA model has two types of effects: fixed and random. The fixed effects in the model were the explanatory variables of interest: mask, exercise, and sex. The random effect was the participant, which allows the model to handle non-independent observations by assuming a different baseline physiological parameter for each participant. In addition, interaction terms of mask by exercise, exercise by sex, and mask by sex were also included. A total of three mixed-effects models were utilized for each of the physiological parameters of HR, perceived exertion, and SpO2. The significance level utilized was alpha <0.05. If an interaction term was determined to be significant, the interaction term was interpreted rather than a significant main fixed effect. Post hoc comparisons utilizing least square means and standard errors were conducted with Tukey’s method for p value adjustment if a main fixed effect or interaction effect was statistically significant from the model for the mask or exercise variables, given that each variable had three categories. In addition, two-sample t tests were utilized to compare mean age and BMI between the males and females. Graphical displays such as boxplots were also created for relevant results from the mixed-effects ANOVA models. All data are expressed as mean ± SEM unless otherwise stated, and statistical analyses were conducted utilizing R version 4.0.3 [13].
Results
Study and patient characteristics
Forty participants who met the eligibility criteria successfully completed all nine study activities. In total, there were 20 females (mean age, 29.10 ± 10.67 years; range, 22–61 years) and 20 males (mean age, 28.35 ± 8.61 years; range, 24–64 years; Figure 3A). The mean age was found to be comparable between male and female cohorts (p=0.8081). However, the mean BMI was significantly higher in males (27.79 ± 4.26 kg/m2; range, 22.3–37.0 kg/m2) compared to females (24.01 ± 3.02 kg/m2 [range, 18.5–29.8 kg/m2], p=0.0027; Figure 3B). Table 1 contains mean Borg, HR, and SpO2 values under all mask and exercise conditions, and Table 2 contains results from the mixed-effects ANOVA model.
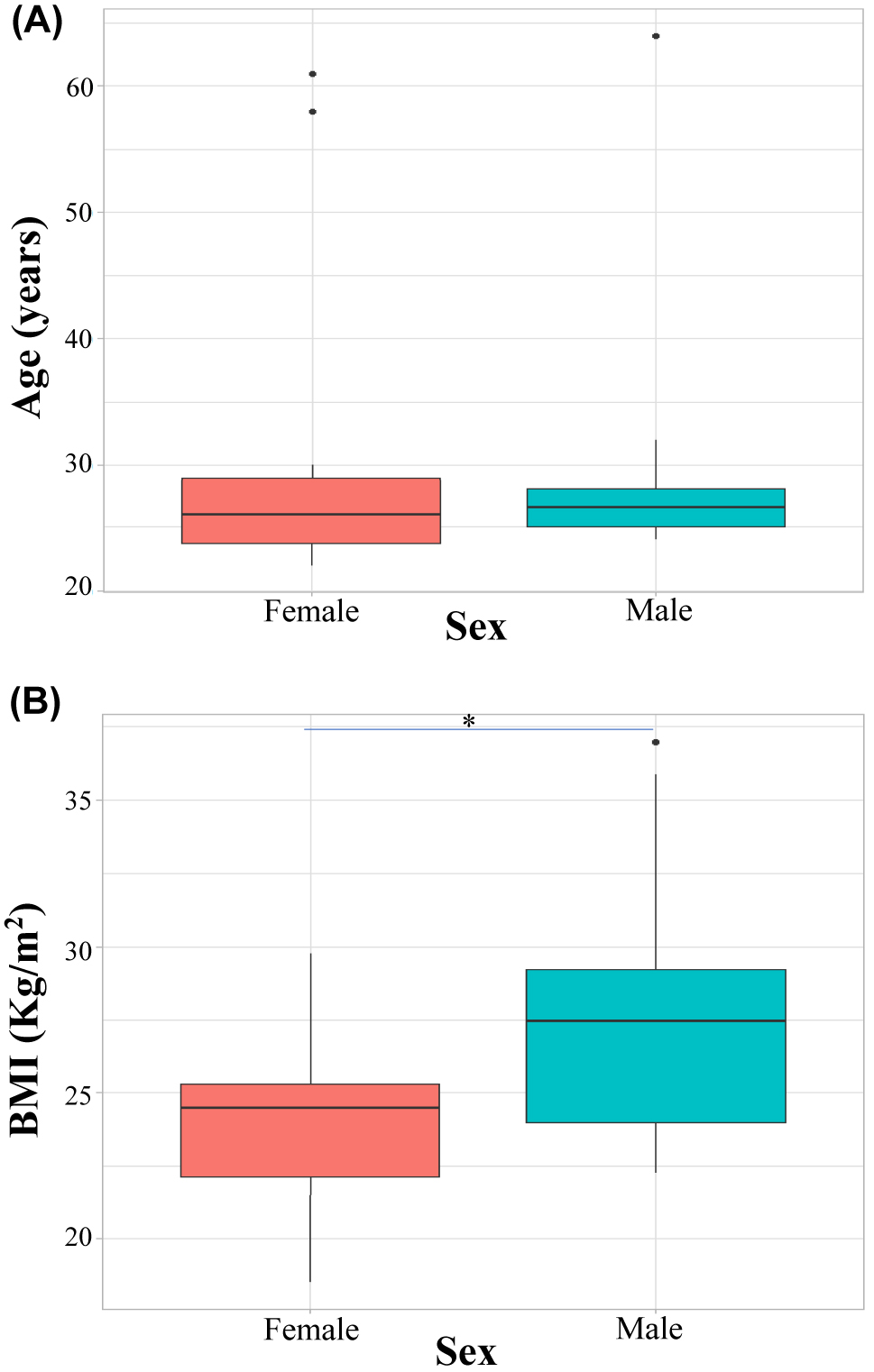
Comparative assessment of age and BMI between male and female participants. (A) Mean age and (B) BMI of subjects. There were 20 male and 20 female subjects. BMI, body mass index.
Average (SEM) Borg, HR, and SpO2 under all mask and exercise conditions.
| Rest Borg | Rest HR | Rest SpO2 | Walking Borg | Walking HR | Walking SpO2 | Exercise Borg | Exercise HR | Exercise SpO2 | |
|---|---|---|---|---|---|---|---|---|---|
| No mask | 6.28 (0.16) | 77.91 (2.15) | 97.28 (0.23) | 8.5 (0.36) | 93.47 (3.64) | 97.78 (0.26) | 13.22 (0.44) | 138.43 (3.83) | 97.06 (0.23) |
| Surgical mask | 6.34 (0.14) | 80.5 (2.62) | 96.72 (0.27) | 8.34 (0.31) | 99 (3.88) | 97.5 (0.32) | 13.25 (0.40) | 141.03 (4.29) | 96.91 (0.24) |
| N95 mask | 6.28 (0.10) | 84.19 (3.42) | 96.75 (0.25) | 8.69 (0.32) | 100.63 (3.68) | 97.63 (0.22) | 13.94 (0.44) | 143.31 (3.78) | 96.75 (0.19) |
-
HR, heart rate; SEM, standard error of the mean; SpO2, blood oxygen saturation.
Results from the mixed-effects ANOVA model (includes variables mask, exercise, sex, and all interactions) for the Borg scale, HR, and SpO2 outcomes.
| Variable | F value | p-Value | |
|---|---|---|---|
| Borg scale | |||
| Mask | 4.6585 | 0.0102 | |
| Exercise | 895.02 | <0.001 | |
| Sex | 1.1254 | 0.2954 | |
| Mask vs. exercise | 1.7757 | 0.1335 | |
| Exercise vs. sex | 5.4626 | 0.0047 | |
| Mask vs. sex | 0.0242 | 0.9761 | |
|
|
|||
| HR | |||
|
|
|||
| Mask | 5.5316 | 0.0044 | |
| Exercise | 737.70 | <0.001 | |
| Sex | 0.2192 | 0.6423 | |
| Mask vs. exercise | 0.2310 | 0.9208 | |
| Exercise vs. sex | 1.1989 | 0.3029 | |
| Mask vs. sex | 0.0090 | 0.9910 | |
|
|
|||
| SpO 2 | |||
|
|
|||
| Mask | 2.4806 | 0.0854 | |
| Exercise | 15.1531 | <0.001a | |
| Sex | 0.2192 | 0.6423a | |
| Mask vs. exercise | 0.9183 | 0.9208 | |
| Exercise vs. sex | 5.2851 | 0.0055 | |
| Mask vs. sex | 0.1416 | 0.8680 | |
-
aIndicates significant difference, p<0.05. ANOVA, analysis of variance; HR, heart rate; SpO2, blood oxygen saturation.
Perceived exertion
All participants reported their perceived exertion after every activity utilizing the Borg 15-point scale. Figure 4A displays the interaction effects between the mask type and the Borg 15-point scale score. The use of a post hoc test to evaluate perceived exertion by mask condition indicated a significant increase in mean Borg 15-point scale score in N95 users (9.77 ± 0.196) in comparison to no-mask users (9.23 ± 0.196, p=0.007, Figure 4A). Table 3 shows the mean Borg 15-point scale scores by exercise and sex. There was a significant difference for the interaction effect between exercise and sex (p=0.0047). A significant increase in the mean Borg 15-point scale score was observed separately among the male and female cohorts when walking compared to rest, stair climbing compared to rest, and stair climbing compared to walking (Figure 4B). While evaluating exertion by exercise intensity between sexes, however, no significant difference was found between males and females at rest (p=0.9997), walk (p=0.1225), or stair climbing (p=0.9971). There were no interaction effects found in perceived exertion between mask type and any exercise intensity (p=0.1335), nor between mask type and sex (p=0.9761).
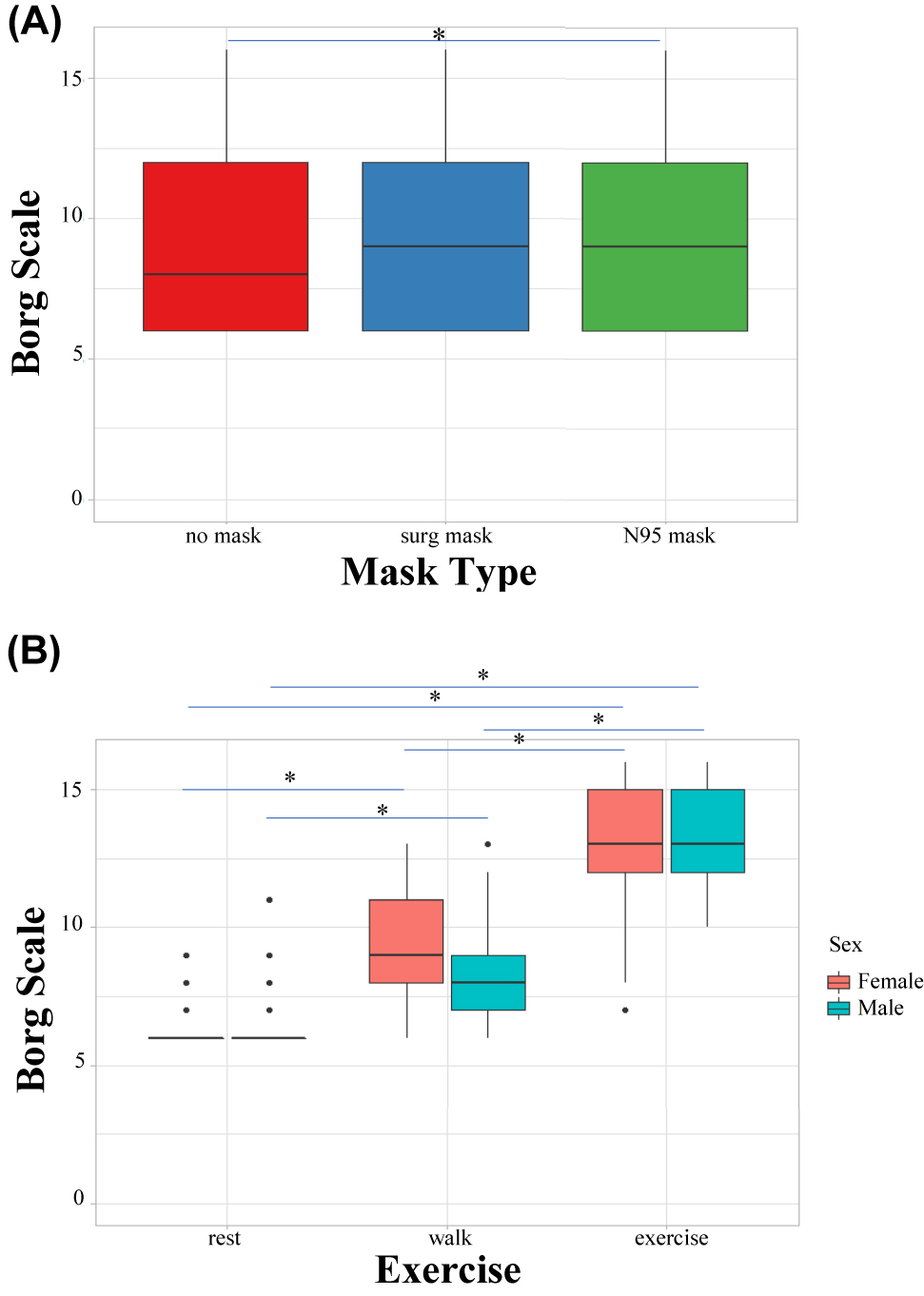
Comparative assessment of perceived exertion.
(A) The interaction effect of mask type on perceived exertion (Borg 15-point scale score). (B) The effect of exercise on perceived exertion. A comparison of both sexes is shown. Perceived exertion was evaluated by self-reported Borg 15-point scale scores. Significant differences are represented by significance lines.
Least-square means for Borg 15-point scale scores by exercise and sex.
| Exercise | Female | Male |
|---|---|---|
| Rest | 6.27 ± 0.28 | 6.38 ± 0.28 |
| Walk | 9.10 ± 0.28 | 8.10 ± 0.28 |
| Stairs | 13.65 ± 0.28 | 13.47 ± 0.28 |
Heart rate (HR)
HR was measured utilizing a pulse oximeter after each study activity was completed. There were statistically significant differences in the mean HR for mask type overall (p=0.0044). From post hoc tests, there was a significant increase in mean HR for N95 users (110 ± 2.51 beats/min) compared to no-mask users (104 ± 2.51 beats/min, p=0.0031, Figure 5A). There was also a significant difference in HR for exercise type overall for the main fixed effect (p<0.001). When comparing HR between exercise types utilizing post hoc tests (Figure 5B), there was a significant increase in mean HR with each sequential exercise intensity, from rest (80.9 ± 2.51 beats/min), to walk (98.1 ± 2.51 beats/min), to stair climbing (142.3 ± 2.51 beats/min, p<0.0001, for all comparisons between stairs vs. rest, stairs vs. walk, and rest vs. walk). No differences were found for any interaction effects when evaluating mean HR between mask types at any exercise intensity (p=0.9208), between mask type and sex (p=0.9910), or between exercise intensity and sex (p=0.3029).
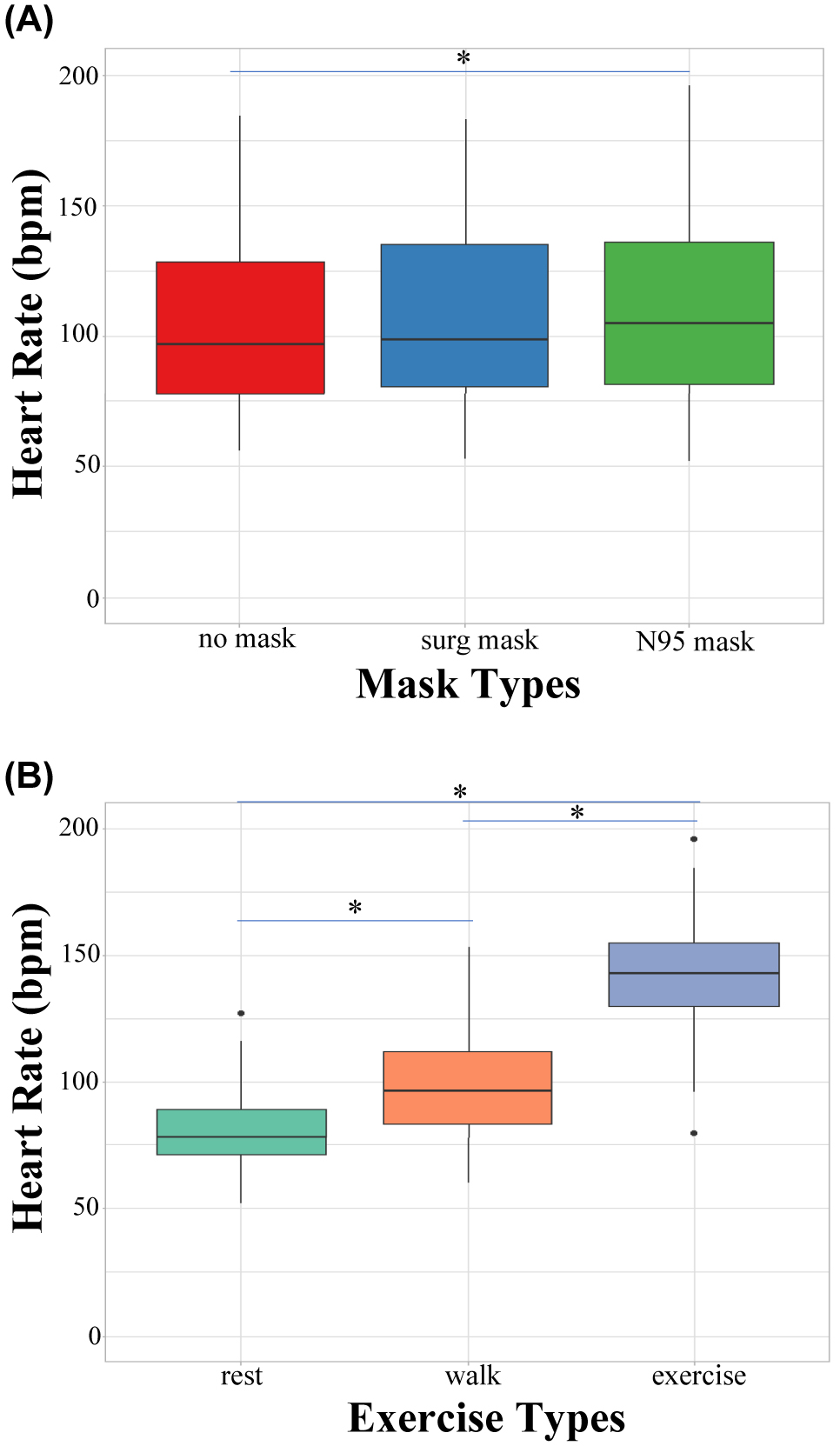
Comparative assessment of HR (beats per minute).
(A) The influence of mask type on HR. (B) The influence of exercise type on HR. HR was evaluated via pulse oximeter. Significant differences are represented by significance lines. HR, heart rate.
Blood oxygen saturation (SpO2)
Oxygen saturation was measured utilizing a pulse oximeter after every activity level. There was no difference in mean SpO2 when evaluating mask type overall for the fixed effect (p=0.0854), or between the interaction effects of mask type at any exercise intensity (p=0.9208), or between mask type and sex (p=0.8680). The mean SpO2 values in males and females at each exercise condition is shown in Table 2. There was a significant difference in mean SpO2 for the interaction effect of sex and exercise intensity (p=0.0055, Figure 6, Table 4). The mean SpO2 in females at rest was significantly higher than in their male counterparts at rest. The mean SpO2 in females while walking was significantly higher than in males walking. There was, however, no difference in mean SpO2 between males and females in high-intensity stair climbing. A significant difference in mean SpO2 was also found within sexes for some comparisons in exercise intensity. Mean SpO2 in females while walking was significantly higher than in females during stair climbing. Mean SpO2 was significantly higher in males while walking compared to males at rest, as well as in males while stair climbing compared to males at rest.
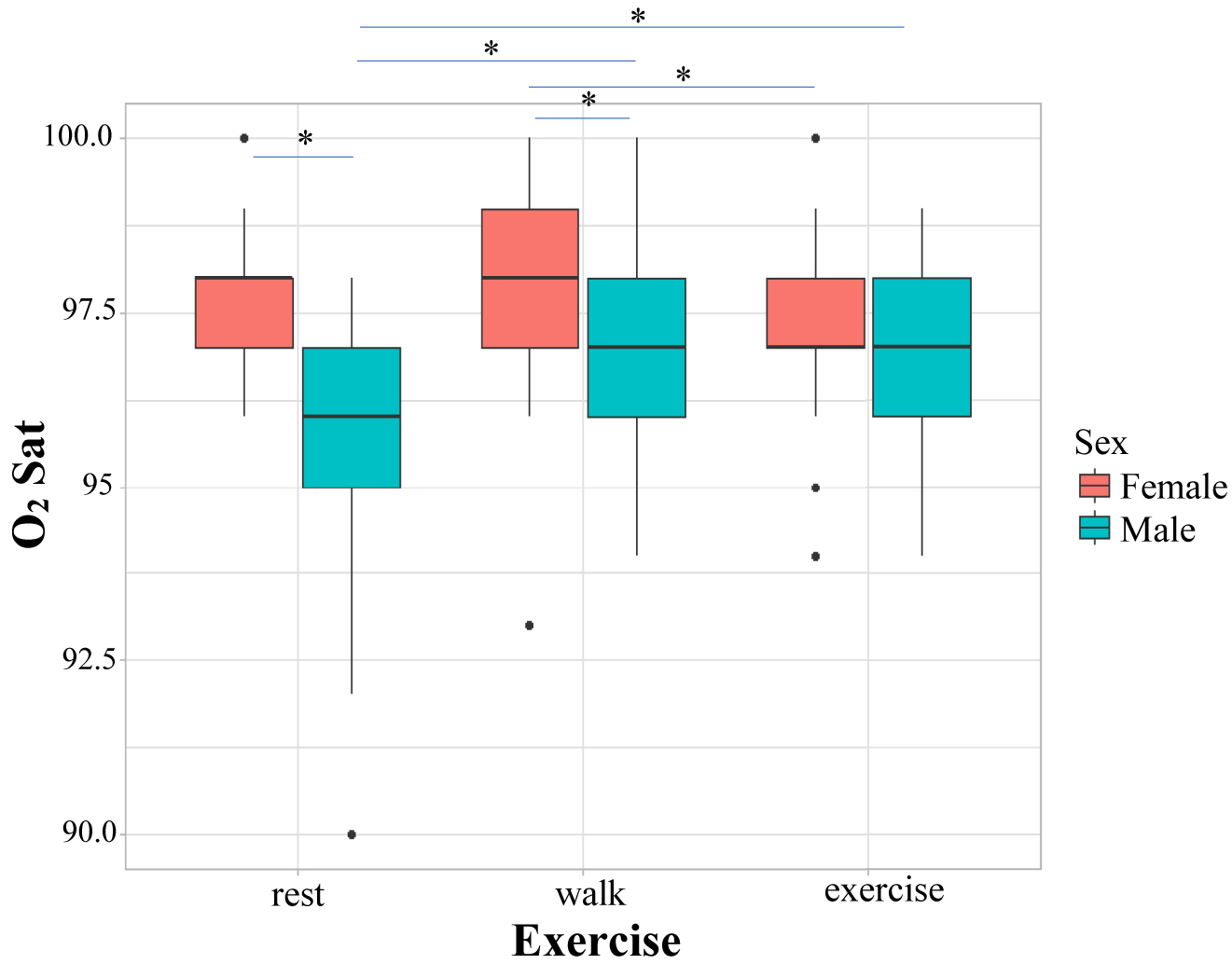
A comparative assessment of mean SpO2 and the interaction effects between sex and exercise type. SpO2 was recorded via pulse oximeter. Significant differences are represented by significance lines.
Least-square means for SpO2 by exercise and sex.
| Exercise | Female | Male |
|---|---|---|
| Rest | 97.48 ± 0.20 | 95.92 ± 0.20 |
| Walk | 98.02 ± 0.20 | 97.03 ± 0.20 |
| Stairs | 97.22 ± 0.20 | 96.65 ± 0.20 |
-
SpO2, blood oxygen saturation.
Discussion
To our knowledge, this is one of the first observational studies that compares SpO2, HR, and perceived exertion between a total of 40 healthy males and females at graded exercise intensities under three mask conditions. Our study demonstrated that mean SpO2 had remained above the physiologically healthy standard of 95% in all mask and exercise conditions. As expected, physical activity was associated with a greater HR, which was also correlated to an increased perceived exertion in N95 users. During the COVID-19 pandemic, measures to mitigate transmission were pertinent. The CDC recommended mask wearing among other protective measures such as social distancing and vaccination [3]. However, with abundant variation in mask material (cloth, surgical, N95), concerns arose about the comparative effects of masks on our work of breathing at rest and during exercise. Thus, differentiating a healthy blood oxygen level is necessary (identified with SpO2) to further utilize blood oxygen level as a key indicator of good health and/or a diseased state.
It is generally accepted that saturation levels above 95% are considered normal, with values under 90% considered hypoxemic [14]. When hypoxemia occurs, patients often first complain of shortness of breath. An increased breathing effort (i.e., altered rate and depth of breathing) is an indication of a normal acute compensatory physiological response [15]. Individuals may also experience headaches and mental status changes. The neurologic effects are largely because the brain is most sensitive to hypoxemia and is often the first to illicit symptoms [14]. Without corrective intervention, aerobic metabolism is replaced with anaerobic metabolism, leading to lactic acidosis and reduced cellular function, and can lead ultimately to cell death [15]. Our data indicate that there was no significant decrease in SpO2 in our participants (i.e., hypoxemia was not a consequence). Although the current study was unable to measure the work of breathing directly due to COVID-19–related restrictions, a prior study by Ade et al. [16] demonstrated in 11 adult males and females that masks significantly increased end-expired peri-oral %CO2 and reduced %O2, each by ∼0.8–2% during exercise (p<0.05). Interestingly, despite those changes, Ade et al. [16] found that masks did not reduce exercise arterial O2 saturation, and neither compromised max respiratory effort nor significantly altered the primary cardiovascular response during submaximal exercise.
Perceived exertion
A common concern among the general population relating to mask wearing is the increased perception of discomfort and perceived claustrophobia when wearing a mask. According to our data, there was an increase in perceived exertion in N95 users in comparison to no-mask users. The increased perceived exertion in N95 users may be attributed to mask discomfort rather than a change in physiological parameters such as SpO2 and HR. A previous study by Li et al. [17], evaluated the subjective experience of mask wearing during intermittent treadmill exercise, and reported that N95 users (n=11) reported the mask feeling tight, unfit, itchy, odorous, and salty, with an increased perception of fatigue in comparison to no-mask users during aerobic exercise. Additionally, masks may increase inspiratory and expiratory resistance with increased facial temperature and humidity during exercise, thereby increasing perceived respiratory effort [18]. Cloth masks, although widely utilized, were not evaluated in our study due to their diversity and lack of standardization, which hinders generalizability. However, Doherty et al. [19] (n=12) compared participant-owned two-ply cloth masks against surgical masks and no-mask controls and reported significantly greater perceived exertion in cloth mask users. The findings by Doherty et al. [19] are in contrast with a study by Shaw et al. [20] (n=14) that evaluated a three-ply cloth mask and found no increase in perceived exertion in comparison to surgical masks and no-mask controls. The discrepancies between these two studies may be attributed to differences in the cloth masks themselves, participant fitness, or the method of testing. Neither of those two studies made comparisons to the N95. Future studies conducting direct comparisons between multi-ply cloth, surgical, and N95 masks could provide valuable insight on their effects on perceived exertion.
Heart rate (HR)
Our study found a significant increase in HR with each sequential exercise intensity in all mask conditions, as expected to occur with incremental levels of exertion. An unexpected outcome of our study was a significant increase in HR for N95 users in comparison to no-mask users in the main fixed effect. The increased HR in N95 users may be due to the constrictive and claustrophobic nature of the N95 having the potential to increase the sympathetic nervous system response and its sequelae such as elevated HR [21]. The increased HR in N95 users is corroborated by Li et al. [17] and Kim et al. [22], both of which report peak HR in healthy N95 users (n=20) during aerobic exercise. On the other hand, Epstein et al. [12] reports no significant difference in HR between healthy no-mask and N95 users (n=16), whereas Kampert et al. [23] found a significant decrease in HR in healthy N95 users (n=20) in comparison to no-mask users during aerobic exercise. The evidence on the effects of N95 on HR is inconsistent and should be considered in future studies while evaluating HR between mask conditions with or without underlying heart or lung conditions.
Blood oxygen saturation (SpO2)
In our study, mean SpO2 was higher in our female cohort in comparison to the male cohort under the rest and walking conditions. There were no significant age differences, underlying medical conditions, or differences in SpO2 contributed by mask type in either sex. The main differentiating characteristic was mean BMI, which was greater in males than in females. A study by Petrofsky et al. [24] evaluated SpO2 and BMI in 81 healthy subjects undergoing graded exercise and showed an inverse relationship between BMI >30 kg/m2 and SpO2. Although mean BMI did not exceed 30 kg/m2 in our participants, our findings agree with the inverse relationship between BMI and SpO2. The relationship between BMI and SpO2 may be attributed to breathing technique rather than oxygen delivery because a higher BMI may correlate with increased abdominal adiposity that restricts diaphragmatic movement and lung perfusion [24]. Additional mechanisms of sex-related SpO2 differences reported in the literature highlight reproductive hormones such as progesterone, a known respiratory stimulant, which may account for higher SpO2 in females [25]. A previous study whose primary goal was to evaluate the relationship between sex and SpO2 (n=207) found a significant difference in mean SpO2 between males (97.1 ± 1.7%) and females (98.1 ± 1.0%), and interpreted this finding as the result of stimulatory effects of progesterone on central and peripheral chemoreceptors, leading to increased respiratory rate [25]. The same study also evaluated data on the phase of the female menstrual cycle and found that female SpO2 was unaffected by menstrual phase. It may be beneficial in future studies to collect data on the phase of the female menstrual cycle to corroborate the relationship between reproductive hormones and SpO2. An additional finding in our study was that mean SpO2 was not significantly different between males and females in the high-intensity stair-climbing phase under any mask condition. A potential reason for this finding is the equal and maximal effort of breathing by all participants at high intensity. Differences in SpO2 in our study were contributed only by sex and BMI. SpO2 was not changed by masks at any exercise intensity and indeed remained consistently above 95% in all conditions of our study for both sexes. The main findings of our study support that surgical masks and N95 respirators do not affect SpO2 at rest and exercise.
Limitations
Because our study was performed during the pandemic, the experimental design was modified to meet federal, state, and university health mandates at the time. Due to the social distancing mandate, data collection was limited to the outdoor setting where strict intensity controls could not be implemented, such as utilizing a treadmill. These restrictions hindered the ability to standardize the activity level achieved by participants during exercise, which otherwise may have helped strengthen the perceived exertion findings in our study. We also limited our testing conditions to 10 min each to account for the length of the study in which participants were required to perform a total of nine 10-min exercise conditions. We chose 10 min to more closely mimic clinical testing; however, time to exhaustion may be better representative of the real world for future studies. However, time to exhaustion may have been largely different among each participant, which could not be controlled. Additionally, HR and SpO2 data were obtained immediately postactivity, which could produce different values in comparison to HR and SpO2 during the midst of the activity. We lacked the means to obtain said values during activity bouts in a controlled environment because our study was conducted outdoors on campus grounds. Future studies should consider implementing means to measure HR and SpO2 during activity to obtain real-time values. Similarly, the tools we selected to obtain data were those that required the least amount of contact with participants in compliance with state/university mandates. Such tools included the pulse oximeter, for which the sensitivity is not calibrated, potentially impacting the detection of differences in SpO2 at different exercise and mask conditions. Despite this, we chose the pulse oximeter to measure SpO2 because it is utilized in clinical practice. Our study excluded participants with known medical conditions that could impact their ability to perform the activities of this study. However, the overall fitness level of the participants in our study may only be interpreted with the average BMI. The participants were recruited from a healthcare professions institution, which may impact the generalizability to the public. Additionally, as noted in our study, females had a higher SpO2 than males in two out of the three activity levels, possibly because of the stimulatory effects of progesterone on respiration. We had not collected data on female menstrual stage to corroborate this interpretation, which may be beneficial in future studies.
Future studies would benefit largely from including data on additional parameters such as blood pressure, partial pressure of CO2, respiratory rate, and work of breathing, which were not collected in our study because our study design was modified to meet state and university mandates for social distancing. Such parameters would provide insight as to whether the surgical mask or N95 mask impaired breathing and increased the work of breathing compared to the subject’s perceived difficulty in breathing. Future studies should also focus on evaluating the effects of face masks on physiological parameters to perform a comparative assessment in those with and without medical conditions. Additionally, to our knowledge, our study includes the largest sample size inclusive of males and females in this topic of research; however, future studies with even larger sample sizes could generalize the data to greater degrees.
Conclusions
Our findings provide supportive evidence of adequate oxygen intake while wearing a mask at rest and during exercise, and this study found no evidence to support a change in SpO2. Future studies on the effects of masks on HR and SpO2 in a larger sample population (including those with health issues) and on multi-ply cloth masks, are needed for a comparative assessment. Studies that compare additional parameters, such as the partial pressure of carbon dioxide (PCO2), work of breathing, and perceived discomfort, would also contribute greatly to the assessment of mask wearing during exercise.
-
Research funding: None reported.
-
Author contributions: All authors provided substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; all authors drafted the article or revised it critically for important intellectual content; all authors gave final approval of the version of the article to be published; and all authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. V.V. and C.L.F. contributed equally to this work.
-
Competing interests: None reported.
References
1. Joo, H, Miller, GF, Sunshine, G, Gakh, M, Pike, J, Havers, FP, et al.. Decline in COVID-19 hospitalization growth rates associated with statewide mask mandates - 10 states, March-October 2020. MMWR Morb Mortal Wkly Rep 2021;70:212–6. https://doi.org/10.15585/mmwr.mm7006e2.Suche in Google Scholar PubMed PubMed Central
2. National Center for Health Statistics. CDC calls on Americans to wear masks to prevent COVID-19 spread. Center for Disease Control and Prevention; 2020. Available from: https://www.cdc.gov/media/releases/2020/p0714-americans-to-wear-masks.html.Suche in Google Scholar
3. University of Washington. Maps of mask use. IHME; 2021. Available from: https://www.healthdata.org/acting-data/covid-19-maps-mask-use [Accessed 17 Mar 2021].Suche in Google Scholar
4. Kreuter, F, Barkay, N, Bilinski, A, Bradford, S, Chiu, R, Eliat, J, et al.. Partnering with a global platform to inform research and public policy making. Surv Res Methods 2000;14:159–63.Suche in Google Scholar
5. Chang, TH, Goicoechea, EB, Stuart, E, Kim, E, Morris, K, LaRocca, S, et al.. Global trends in mask usage in 19 million adults. Social Data Science Center; 2020. Available from: https://socialdatascience.umd.edu/global-trends-of-mask-usage-in-19-million-adults [Accessed 17 Mar 2021].Suche in Google Scholar
6. Liang, M, Gao, L, Cheng, C, Zhou, Q, Uy, JP, Heiner, K, et al.. Efficacy of face mask in preventing respiratory virus transmission: a systematic review and meta-analysis. Travel Med Infect Dis 2020;36:101751. https://doi.org/10.1016/j.tmaid.2020.101751.Suche in Google Scholar PubMed PubMed Central
7. Balazy, A, Toivola, M, Adhikari, A, Sivasubramani, SK, Reponen, T, Grinshpun, SA. Do N95 respirators provide 95% protection level against airborne viruses, and how adequate are surgical masks? Am J Infect Control 2006;34:51–7. https://doi.org/10.1016/j.ajic.2005.08.018.Suche in Google Scholar PubMed
8. Howard, MC. Understanding face mask use to prevent coronavirus and other illnesses: development of a multidimensional face mask perceptions scale. Br J Health Psychol 2020;25:912–24. https://doi.org/10.1111/bjhp.12453.Suche in Google Scholar PubMed PubMed Central
9. Gericke, RC, Gupta, AK. The effects of wearing a mask on an exercise regimen. J Osteopath Med 2022;122:545–552. https://doi.org/10.1515/jom-2022-0045.Suche in Google Scholar PubMed
10. Nwosu, ADG, Ossai, EN, Onwuasoigwe, O, Ahaotu, F. Oxygen saturation and perceived discomfort with face mask types, in the era of COVID-19: a hospital-based cross-sectional study. Pan Afr Med 2021;39. https://doi.org/10.11604/pamj.2021.39.203.28266.Suche in Google Scholar PubMed PubMed Central
11. Fikenzer, S, Uhe, T, Lavall, D, Rudolph, U, Falz, R, Busse, M, et al.. Effects of surgical and FFP2/N95 face masks on cardiopulmonary exercise capacity. Clin Res Cardiol 2020;109:1522–30. https://doi.org/10.1007/s00392-020-01704-y.Suche in Google Scholar PubMed PubMed Central
12. Epstein, D, Korytny, A, Isenberg, Y, Marcusohn, E, Zukermann, R, Bishop, B, et al.. Return to training in the COVID-19 era: the physiological effects of face masks during exercise. Scand J Med Sci Sports 2021;31:70–5. https://doi.org/10.1111/sms.13832.Suche in Google Scholar PubMed PubMed Central
13. Team, RC. R: a language and environment for statistical computing. V Austria: R Foundation for Statistical Computing; 2020. Available from: https://www.R-project.org/.Suche in Google Scholar
14. Hafen, BB, Sharma, S. Oxygen saturation. Treasure Island, FL: StatPearls; 2021. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430685/.Suche in Google Scholar
15. Samuel, J, Franklin, C. Hypoxemia and hypoxia. In: Myers, JA, Millikan, KW, Saclarides, TJ, eds. Common surgical diseases: an algorithmic approach to problem solving. New York: Springer; 2008:391–4 pp.10.1007/978-0-387-75246-4_97Suche in Google Scholar
16. Ade, CJ, Turpin, VG, Parr, SK, Hammond, ST, White, Z, Weber, RE, et al.. Does wearing a facemask decrease arterial blood oxygenation and impair exercise tolerance? Respir Physiol Neurobiol 2021;294:103765. https://doi.org/10.1016/j.resp.2021.103765.Suche in Google Scholar PubMed PubMed Central
17. Li, Y, Tokura, H, Guo, YP, Wong, ASW, Wong, T, Chung, J, et al.. Effects of wearing N95 and surgical facemasks on heart rate, thermal stress and subjective sensations. Int Arch Occup Environ Health 2005;78:501–9. https://doi.org/10.1007/s00420-004-0584-4.Suche in Google Scholar PubMed PubMed Central
18. Zhang, G, Li, M, Zheng, M, Cai, X, Yang, J, Zhang, S, et al.. Effect of surgical masks on cardiopulmonary function in healthy young subjects: a crossover study. Front Physiol 2021;12:710573. https://doi.org/10.3389/fphys.2021.710573.Suche in Google Scholar PubMed PubMed Central
19. Doherty, CJ, Mann, LM, Angus, SA, Chan, JS, Molgat-Seon, Y, Dominelli, PB. Impact of wearing a surgical and cloth mask during cycle exercise. Appl Physiol Nutr Metab 2021;46:753–62. https://doi.org/10.1139/apnm-2021-0190.Suche in Google Scholar PubMed
20. Shaw, K, Butcher, S, Ko, JW, Zello, GA, Chilibeck, PD. Wearing of cloth or disposable surgical face masks has no effect on vigorous exercise performance in healthy individuals. Int J Environ Res Public Health 2020;17:8110. https://doi.org/10.3390/ijerph17218110.Suche in Google Scholar PubMed PubMed Central
21. Tian, Z, Kim, BY, Bae, MJ. A study on the effect of wearing masks on stress response. Int J Eng Res Technol 2020;13:807–13. https://doi.org/10.37624/ijert/13.4.2020.807-813.Suche in Google Scholar
22. Kim, JH, Benson, SM, Roberge, RJ. Pulmonary and heart rate responses to wearing N95 filtering facepiece respirators. Am J Infect Control 2013;41:24–7. https://doi.org/10.1016/j.ajic.2012.02.037.Suche in Google Scholar PubMed
23. Kampert, M, Singh, T, Sahoo, D, Han, X, Van Iterson, EH. Effects of wearing an N95 respirator or cloth mask among adults at peak exercise: a randomized crossover trial. JAMA Netw Open 2021;4:e2115219. https://doi.org/10.1001/jamanetworkopen.2021.15219.Suche in Google Scholar PubMed PubMed Central
24. Petrofsky, JS, Laymon, MS, Khowailed, IA, Fisher, S, Mills, A. The effect of BMI on oxygen saturation at rest and during mild walking. J Appl Med Sci 2015;4:1–8.Suche in Google Scholar
25. Levental, S, Picard, E, Mimouni, F, Joseph, L, Samuel, TY, Bromiker, R, et al.. Sex-linked difference in blood oxygen saturation. Clin Respir J 2018;12:1900–4. https://doi.org/10.1111/crj.12753.Suche in Google Scholar PubMed
© 2022 the author(s), published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.
Artikel in diesem Heft
- Frontmatter
- Behavioral Health
- Original Article
- Adverse childhood experience categories and subjective cognitive decline in adulthood: an analysis of the Behavioral Risk Factor Surveillance System
- General
- Original Article
- Understanding and preference toward DOs and OMT before and after an osteopathic principles and practice fellow lecture series
- Musculoskeletal Medicine and Pain
- Original Article
- Revisiting chronic low back pain: evidence that it is not non-specific
- Neuromusculoskeletal Medicine (OMT)
- Original Article
- Connecting the dots: alterations in bioelectric activity at acupuncture Ting (Jing-Well) points following CV4 cranial manipulation
- Pediatrics
- Brief Report
- Evaluation of academic detailing to educate clinicians regarding childhood lead poisoning prevention: a pilot study
- Public Health and Primary Care
- Original Article
- Effects of face masks on oxygen saturation at graded exercise intensities
- Clinical Image
- Annular bullous lesions in a child from Uganda: chronic bullous disease of childhood
Artikel in diesem Heft
- Frontmatter
- Behavioral Health
- Original Article
- Adverse childhood experience categories and subjective cognitive decline in adulthood: an analysis of the Behavioral Risk Factor Surveillance System
- General
- Original Article
- Understanding and preference toward DOs and OMT before and after an osteopathic principles and practice fellow lecture series
- Musculoskeletal Medicine and Pain
- Original Article
- Revisiting chronic low back pain: evidence that it is not non-specific
- Neuromusculoskeletal Medicine (OMT)
- Original Article
- Connecting the dots: alterations in bioelectric activity at acupuncture Ting (Jing-Well) points following CV4 cranial manipulation
- Pediatrics
- Brief Report
- Evaluation of academic detailing to educate clinicians regarding childhood lead poisoning prevention: a pilot study
- Public Health and Primary Care
- Original Article
- Effects of face masks on oxygen saturation at graded exercise intensities
- Clinical Image
- Annular bullous lesions in a child from Uganda: chronic bullous disease of childhood

