Abstract
Context
One of the two major pathways to become a physician in the United States is the Doctor of Osteopathic Medicine (DO) degree. A major distinctive feature is often perceived as the addition of manual training in osteopathic manipulative treatment (OMT) in the DO education. However, the profession also has a distinct philosophy imbedded in the curriculum of all osteopathic medical schools. Many medical schools offer professional degrees with graduates who may choose to continue their education in medicine, such as the Master of Science in Biomedical Sciences (MSBS). At our institution, there is no formal exposure to the differences between osteopathic and allopathic medicine in the MSBS curriculum, and most of this understanding is gained through out-of-classroom conversations. During the SARS-CoV-2 pandemic, virtual learning prohibited the usual gathering and discourse that occurs when students are learning on campus.
Objectives
The objective of this study is to create a curriculum in the form of a seminar series to assist premedical students in making an informed choice about which profession is the best fit for their own education and to gain an appreciation for osteopathic medicine. This appreciation could also aid in the future collaboration of premedical students with osteopathic providers, recommendations to patients, and potentially their own medical care. Questionnaires were utilized to determine if our osteopathic seminar series was effective at changing the preferences and understanding of MSBS students. We also sought to determine the effectiveness of virtual vs. in-person delivery of our curriculum.
Methods
A seminar series with pre-established objectives was developed and presented to MSBS students at an osteopathic institution during the Fall of 2020 and 2021. The 2020 seminar was delivered through a virtual conference platform, and the 2021 seminar was delivered in-person. An eight question pre-and postquestionnaire was given to participants to evaluate their preferences and understanding. Internal validity and differences between delivery formats were assessed.
Results
Both seminar series produced equally effective, significant changes in the preferences and perceptions of osteopathic medicine in both virtual and in-person delivery formats. Differences in pre-vs. post understanding across both seminar series were not consistently significant and were smaller than those observed in preferences and perceptions. Positive changes included an increased willingness to see a DO and to recommend a loved one see a DO as their personal physician. Preference changes between the in-person vs. virtual delivery platforms did not show significant differences; however, understanding did show some inconsistent differences.
Conclusions
This study demonstrates the utility of a virtual or in-person seminar to improve the preferences and perceptions of the osteopathic profession in MSBS students. The seminar series was successful in its goal of offering formal exposure to the osteopathic profession. The improved preferences and perceptions will have potential substantial benefits to the field of osteopathic medicine in the future. Further research is warranted to determine the most effective way to increase understanding of the osteopathic profession.
Doctors of Osteopathic Medicine (DOs) have worked for decades to be granted equal practicing rights to their allopathic (MD) counterparts. DOs trained in the United States were federally recognized as full practice physicians in 1966 and by all state governments by 1972. These efforts to prove equivalence were so effective that now there is little perceptible difference between the practice of the two types of physicians [1]. Despite achieving equivalence in licensure [2], the osteopathic profession promotes itself as distinct from their allopathic colleagues. This distinctiveness is emphasized twofold: first, through the philosophy of the osteopathic tenets; and second, in the application and practice of osteopathic manipulative medicine (OMM) as an adjunct to pharmacology, surgery, and other conservative measures. osteopathic manipulative treatment (OMT) is often perceived as the main difference between MDs and DOs as observed in studies evaluating the preferences of OMT in the medical student population [3], practicing physicians [4], hospital staff [5], and premedical undergraduate student populations [6, 7]. These studies revealed a lack of understanding of osteopathic philosophy beyond OMT, which are particularly important given a decline in the use of OMT [4].
In the United States, one in four medical students are training to become physicians as DOs. Medical school matriculation surveys from 2019 to 2021 reveal that at least 15% of medical school students participated in postbaccalaureate premedical programs (postbac), including non–degree-seeking and degree-seeking programs, such as a Master of Science in Biomedical Sciences (MSBS), making this an important population of premedical students [8]. MSBS programs have been established throughout the United States at multiple allopathic and osteopathic programs [9, 10]. Postbac programs are commonly an avenue for students to establish their academic readiness and enhance their applications when applying to terminal-degree medical programs [11]. Traditionally, postbacs are designed to assist applicant transition from alternate careers into medicine (“career changers”) and/or to improve the competitiveness of applicants (“enhancement”) [12]. The first-reported postbac program was established in 1969, and the number of postbac programs has grown to at least 250 postbacs in the United States, ranging from 9 months to 3 years, with a few having over 100 students, degree- or certificate-awarding, and with or without research components [13]. The typical curriculum for MSBS programs does not include learning about various medical school options [14]. Despite many MSBS programs being at institutions with DO schools [9], it is unclear what understanding the postbac and MSBS students at those institutions have of osteopathic vs. allopathic medicine. It is known that osteopathic medical students with prior exposure to OMT agree more with osteopathic philosophy statements and have a greater intention to utilize OMT [3]. This suggests that exposing students to these concepts can widen their preferences and open them to higher appreciation for these tools. The impacts of the education of OMM concepts for premedical students have not been well described, may provide a significant impact on the future generation of osteopathic physicians, and could additionally foster the development of educational strategies to educate other health professional students and providers about the osteopathic profession [5].
The main objective of our study was to investigate the preferences of MSBS students at an osteopathic institution regarding osteopathic medicine and to investigate whether an active intervention can change their preferences and understanding. This objective was evaluated utilizing a seminar series as an intervention and measuring change (pre-vs. post-) in preferences toward DOs and the understanding of OMM and OMT. We hypothesize that a seminar series would improve the understanding of MSBS students. Second, because the content had to be presented virtually during the COVID-19 pandemic, the second part of the study consisted of determining whether preferences can be changed effectively via a virtual vs. an in-person seminar series. We hypothesize that both delivery methods are equally as effective. Creating a lecture series that educates and positively affects the preferences of MSBS students toward osteopathic medicine could provide them a better appreciation of the option for their own potential careers in medicine, for their patients as collaborating providers, and as patients seeking care themselves.
Methods
Study overview
A three-part educational seminar series to discuss the history of osteopathic medicine, the definition and application of OMM, and lastly a demonstration of OMT was developed by Faculty and Predoctoral OPP (Osteopathic Principles and Practice) fellows at our osteopathic institution. This program was presented to Master of Science in Biomedical Sciences (MSBS) students at our institution. The main topics of the series included: “What is OMM?,” “How to utilize OMM to benefit patients,” and an OMM demonstration. Both virtual and in-person series were delivered because of ongoing COVID-19 restrictions. This allowed for the evaluation of the effectiveness of the delivery mode. Participation at the virtual presentations for the MSBS students was optional. Preference and understanding assessments were done pre-and postcompletion of the seminar series.
Participants
Participants included in this study were enrolled in our institution’s 9-month MSBS program during the 2020–2021 and 2021–2022 academic years. MSBS students have one shared course (Evidence-Based Medicine) with the College of Osteopathic Medicine (COM) students with no other overlapping curriculum and no formal education about osteopathic medicine. Participation in the study was voluntary, and results were kept confidential. Only students who attended the sessions and who completed the consent were included in the study. The study was vetted by the Rocky Vista University Institutional Review Board and approved as exempt. No demographic information was collected to maintain anonymity with the small class size and minimize potential social desirability bias.
Intervention description
The first part of the project took place during the 2020–2021 academic year and was utilized to identify if preferences toward OMM change effectively after a virtual seminar series. The virtual presentations were held via a video conferencing platform. Participants were asked to consent and complete the presurvey prior to the beginning of the presentation. The presentations were approximately 50 min in length and covered predetermined objectives as developed by the research team. The virtual presentations were delivered in October-November 2020. The second part of the project took place during the 2021–2022 academic year and was utilized to identify the effectiveness of virtual seminar series in comparison to in-person seminar series with the same objectives. The in-person presentations were held in classrooms and clinical skills labs on campus. The same format was utilized for the in-person series as the virtual series in the fall of 2020. The in-person presentations were delivered in October-November 2021.
The general topics covered in these seminars are summarized in Figure 1A. Slide presentations were created for both arms of the project. The presentations each covered the same objectives but differed in the presentation format: either virtually or in-person. Both presentations included student interactions. Virtual participants were able to type or verbally respond to the questions asked, whereas in-person participants were able to verbally respond. Participants were given opportunities to ask for clarification or to discuss confusing topics.
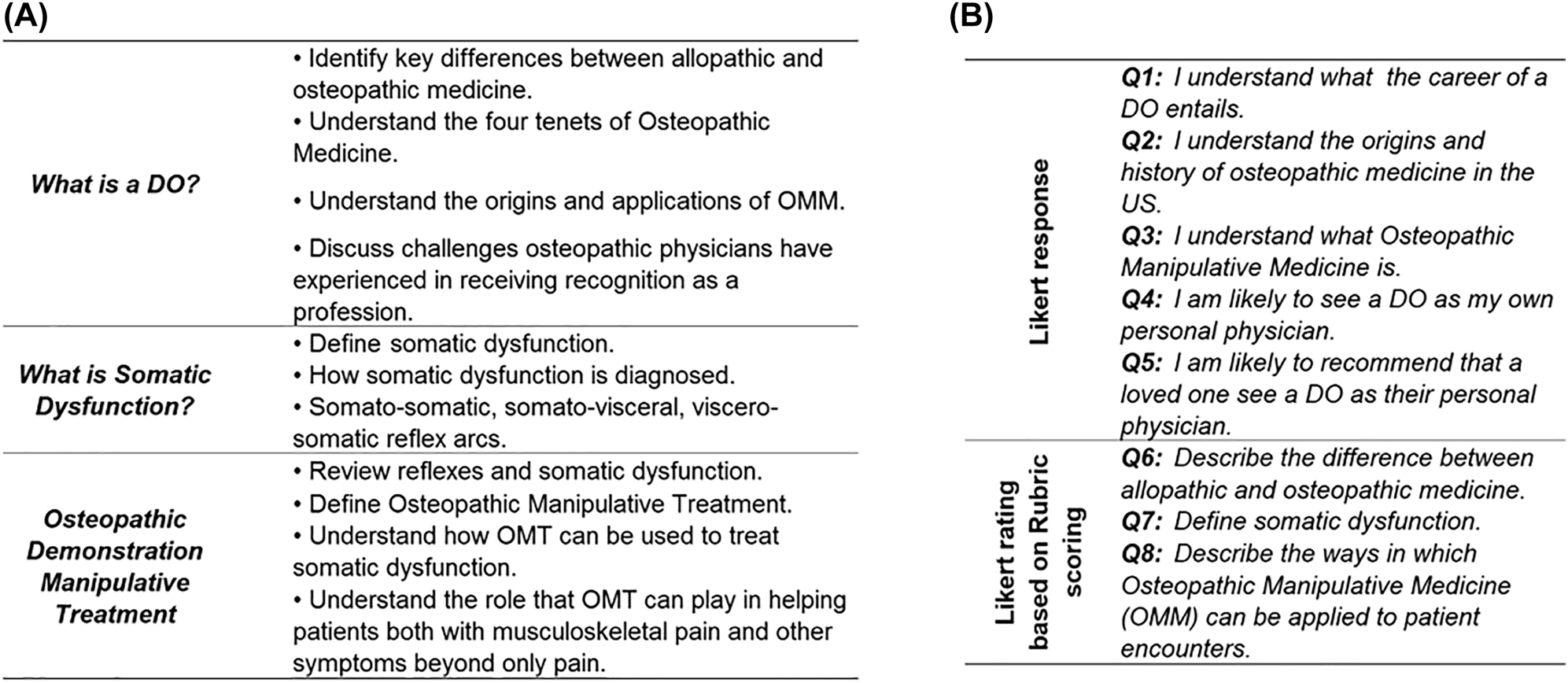
The osteopathic medicine topics covered and the assessment questionnaire. (A) The topics and subtopics covered in the lecture series. (B) The assessment questionnaire developed to evaluate the attitudes, preferences, and understanding of the osteopathic medicine concepts delivered.
Preference and understanding assessment
A survey questionnaire was utilized to determine if the information provided improved the students’ overall preferences and understanding of osteopathic medicine concepts. The assessment questionnaire is presented in Figure 1B. The first five questions gauged subjective preferences toward osteopathic medicine, in which students self-reported agreements with statements about osteopathic medicine from 1 (strongly disagree) to 5 (strongly agree). For the next three questions, one of the learning objectives from each lecture was chosen to create a short-answer test question gauging the students’ understanding of the presented material. This was included to reinforce a foundation of understanding about osteopathic medicine, which has been historically emphasized in the interview process for admission to our DO program. Short-answer questions were limited to 175 characters. Surveys were administered through Survey Monkey in 2020 and through Qualtrics in 2021. All pre-vs. postresponses by individual were matched utilizing a numerical identifier with no personal identifiers (Appendix A). The students took the survey a total of two times, once prior to the first presentation, and once after completion of the final presentation. Responses for the survey questionnaire were only collected during allocated times before and after the session.
A grading rubric for the short-answer question numbers 6, 7, and 8 was developed by the research team. Key terms and concepts were included in the rubric based on American Osteopathic Association’s descriptions of DOs [15], the Glossary of Osteopathic Terminology (3rd Edition), and consultation with a neuromusculoskeletal medicine and osteopathic manipulative medicine (NMM/OMM) board-certified DO attending physician and faculty at our institution. The rubric is available as Appendix B. Once the rubric was created to guide the qualitative analysis, each question was scored on a scale from 1 (demonstrates no understanding) to 4 (demonstrates advanced understanding). To prevent bias, each survey response was assigned a numerical identifier for blinding, and the pretest and posttest responses were deidentified and randomized. Responses for each question were compiled in random order and assigned to all graders. Graders consisted of three members of the research team including an NMM/OMM board-certified DO attending, an MD attending, and a Senior Pre-Doctoral OPP Fellow. Each grader scored every response individually and independently. Averages of the three scores were utilized for final quantitative analysis.
Statistical analysis
Preliminary power analysis determined that a sample of 34 participants (42 per group) was required to detect a 0.5 unit difference achieving 80% power at a significance threshold of 0.05. However, a post hoc power analysis revealed that our study was powered at an effective 93.7%. Descriptive statistics for participants and scores were estimated. The internal consistency assessment for the questionnaire utilized to assess the preferences and understanding of osteopathic medicine concepts was performed utilizing Cronbach’s alpha on the correlation matrix of the questionnaire answers. This assessment included all of the scores (preferences, as well as understanding as scored through the rubric).
The evaluation of pre-vs. posteffects and virtual vs. in-person effects was performed utilizing a nonparametric test and Wilcoxon’s two-sample test. This was done because the distributions of the scores did not meet normality assumptions that would allow for parametric unpaired t tests. Normality assumptions were verified prior to analysis through univariate distribution plots. The tested hypothesis was a difference in the timepoint and delivery method vs. the null hypothesis of no difference. All descriptive statistics, correlation, internal consistency assessments, and association testing was performed utilizing SAS/STAT v.9.4 (SAS Institute Inc., Cary, NC). Statistical significance was declared at p≤0.05, although exact probabilities are provided.
Results
In the session delivered in 2020, a total of 86 MSBS students responded to the presurvey and 52 MSBS students responded to the postsurvey. For the session delivered in 2021, 83 MSBS students responded to the presurvey and 61 MSBS students responded to the postsurvey. Internal consistency, measured through a standardized Cronbach’s alpha, was 0.8067 for the virtual vs. in-person assessment. The 2020 cohort reported an internal consistency alpha value of 0.8373, and the 2021 cohort reported a value of 0.7770. All of the internal consistency values indicate a satisfactory level of internal consistency [16].
Delivery method average scores for the portion of the study comparing virtual vs in-person are presented in Figure 2, and formal testing outcomes of these comparisons are presented in Table 1. The average scores in this assessment indicate that preferences are higher than understanding. Only understanding questions displayed a significant difference (Q6 and Q7). This representation only evaluated the delivery model and does not distinguish pre- and postimprovements. This finding suggests that understanding is the only area where the delivery methods had an impact, thus no additional confounders were considered for this assessment. For the second part of our study evaluating the intervention effectiveness (pre-vs. post-) there is a strong effect observed in preferences. Average scores are presented in Figure 3 with formal testing presented in Table 1. The observed effect is larger among preferences as compared to understanding. The largest increase observed was on Q2 (understanding the origins and history of the osteopathic profession in the United States). The in-person delivery methods displayed no difference in the understanding sections (Q6 and Q8). Our findings in this part of the study indicate that the educational seminar provides a consistent benefit by consistently increasing the scores for preferences regardless of the delivery method. Our data suggest that increasing understanding of osteopathic medicine presents a higher challenge and our interventions were not sufficient for significantly increasing scores.
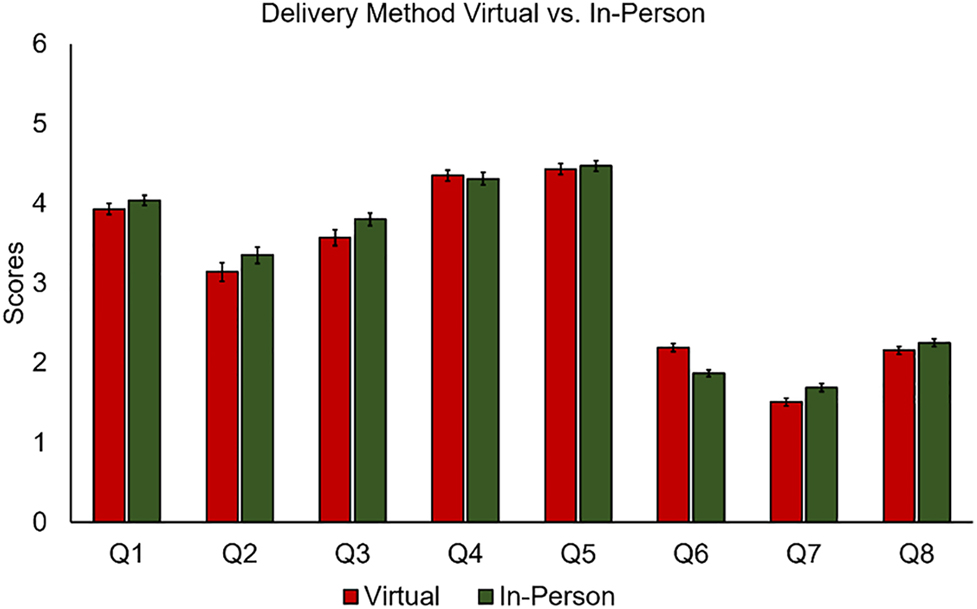
The average score responses between the delivery methods (virtual and in-person). Error bars represent the standard error of the mean (SEM).
Significance testing for delivery mode (virtual vs. in person) and intervention effectiveness (pre-vs. post).
| Question | Delivery mode (virtual vs. in person) | Intervention effectiveness | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Difference | Test statistic | p-Value (Wilcoxon) | Virtual | In person | |||||
| Difference | Test statistic | p-Value (Wilcoxon) | Difference | Test statistic | p-Value (Wilcoxon) | ||||
| Q1 | 0.11 | 0.66 | NS | 1.02 | 54.32 | <0.001 | 0.61 | 33.94 | <0.001 |
| Q2 | 0.21 | 2.05 | NS | 2.15 | 77.88 | <0.001 | 1.66 | 62.39 | <0.001 |
| Q3 | 0.23 | 2.44 | NS | 1.57 | 64.49 | <0.001 | 1.06 | 52.67 | <0.001 |
| Q4 | −0.04 | 0.02 | NS | 0.71 | 25.17 | <0.001 | 0.32 | 5.71 | 0.0169 |
| Q5 | 0.04 | 0.25 | NS | 0.61 | 22.78 | <0.001 | 0.25 | 9.49 | 0.0021 |
| Q6 | −0.32 | 27.91 | <0.001 | 0.32 | 9.32 | 0.0023 | 0.22 | 3.04 | NS |
| Q7 | 0.18 | 15.30 | <0.001 | 0.61 | 26.76 | <0.001 | 1.22 | 7.58 | 0.0059 |
| Q8 | 0.09 | 1.21 | NS | 0.43 | 18.45 | <0.001 | 0.15 | 0.73 | NS |
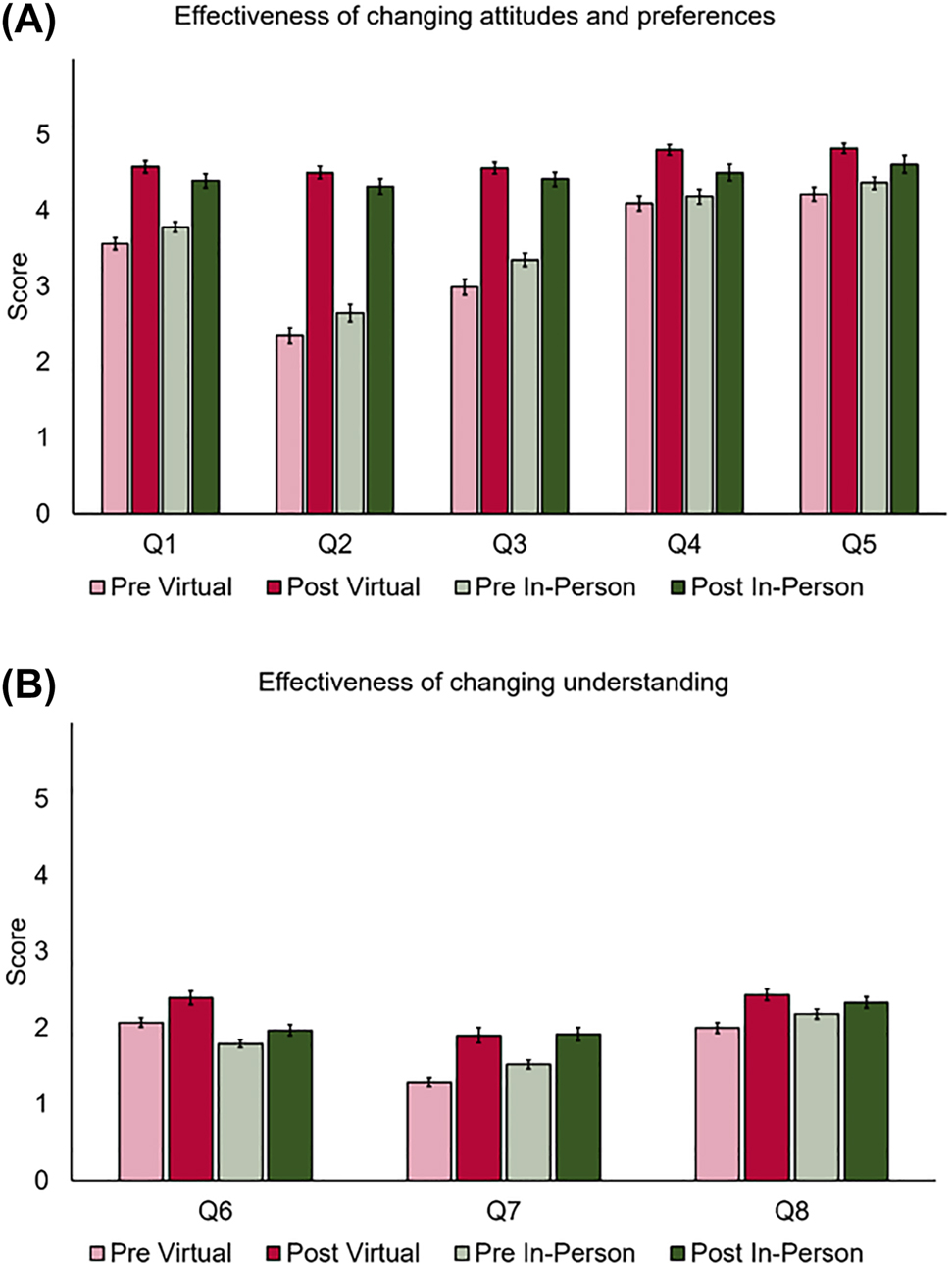
The average score responses for (A) effectiveness of changing attitudes and preferences, and (B) effectiveness of changing understanding. Error bars represent the standard error of the mean (SEM).
Discussion
Within our institution, it has been assumed that our MSBS graduates attending DO schools have some concept of osteopathic medicine and optimally a positive outlook toward the field, but these assumptions have not been formally evaluated. MSBS students in this institution have historically relied on informal interactions with DO faculty and students on campus to learn about osteopathic philosophy, OMM, and OMT, with no program-level measurement of preferences and understanding of OMM. This lecture series was designed to accomplish the goals of offering formal exposure and optimally improving preferences and understanding about OMM in the MSBS students. In addition, this exposure to osteopathic concepts could provide benefits to MSBS graduates that attend nonosteopathic institutions because they would be able to act as liaisons for the osteopathic field.
Our intervention was also motivated in part by COVID-19 restrictions. During the COVID-19 pandemic, many educational institutions were required to give instruction virtually on topics that would traditionally only be given in-person. Although initially there were concerns with the effectiveness and practicality of online learning, studies have found that online learning is just as effective in developing understanding as compared to an in-person setting [17], [18], [19], although a combination of both methods is often preferred now [20]. The efficacy of online learning vs. the in-person modality of OMT teaching has not previously been explored. One aim of this study was to explore that efficacy. Our study found improved student preferences toward DO physicians and OMT, and this was successfully achieved with both delivery modalities. This was an encouraging finding because utilizing a virtual platform may be effective for teaching historically in-person content, such as labs. Even when the practical experience should still be provided in person, teaching these concepts through virtual delivery can be utilized to provide additional reinforcement.
An exciting and significant finding was an increased likelihood of recommending a family member to a DO. This suggests that interventions like the one presented have a strong potential to increase a patient’s desire to be seen by DOs and to develop premedical students into advocates for the osteopathic profession and the osteopathic philosophy regardless of their future careers. A study evaluating influences on medical school applicants found that those that concurred with a higher number of osteopathic understanding statements were more likely to apply to DO schools [21]. Therefore, changing the preferences of applicants could lead to an increase in applications to osteopathic medical schools.
This study did not provide evidence that specific understanding of OMT improved in either experimental arm. The reasons for this are not entirely clear. The lectures contained elements such as enthusiastic presenters, provided learning objectives (elements that increase the effectiveness of a lecture) [22], and included the repetition of key concepts that are important for increasing retention [23]. However, didactic content was delivered as traditional lecture, with intermittent active learning practices. Passive learning is known to be less effective in increasing knowledge than active learning but, interestingly, more effective in raising confidence about knowledge [24]. It is possible that the Dunning–Kruger effect [25] was observed in this study, because the surveys revealed an increase in confidence and fairly high confidence about the subject of OMT and DO physicians without a demonstratable increase in specific understanding and with rubric grades that we believe best correlate with a novice learner. Despite that, it is important to highlight that preferences toward osteopathic medicine were significantly improved following the seminar series, regardless of the delivery format. The opportunity for utilization of a seminar series in the MSBS curriculum to improve preferences toward osteopathic medicine is supported by our results. Our study was inconclusive as to whether change in understanding of osteopathic medicine was achieved. Understanding of osteopathic medicine is something that students matriculating into DO school will inevitably develop. For those students who will choose different career paths, further exploration into how to reliably increase understanding through participation in a seminar series is needed.
Some limitations in our study are that it was done in a single program within our institution, part of its approach was motivated by pandemic restrictions, and no control group was included. This acknowledges that an expansion of the study to other programs and institutions with the addition of a more defined experimental design format could provide more accurate findings. Of particular benefit would be collaboration with other osteopathic medical schools with MSBS-type programs. Bias mitigation consisted only in assuring the anonymity of the study and by making the participation voluntary. Expansion and collaboration would allow enough anonymity to collect robust demographic data, including participant background exposure to osteopathic medicine and participant journey to becoming a physician. Our study does not address whether improving preferences toward osteopathic medicine through a seminar series, such as the one utilized in our study, would directly result in increased application or matriculation rates to US osteopathic medical schools. This is something that could be answered with a larger cohort, wider institutional representations, and longer-term follow-up. The success of this seminar series in changing preferences through a virtual platform suggests the viability of an informational series targeted toward both healthcare and nonhealthcare populations. For example, this series could be tailored toward staff, faculty, and administrators employed at osteopathic institutions, undergraduate students interested in becoming physicians, those who would hire DO physicians, and the public who have a choice of selecting their providers. This could be a successful marketing opportunity for the osteopathic profession while empowering patients to make informed decisions regarding their healthcare team.
Conclusions
In this study, we showed that our curriculum was successful in changing preferences regarding the osteopathic profession in a MSBS student population based on our rubric. Both a virtual and in-person delivery platform successfully improved preferences; however, neither platform was effective in increasing the understanding of osteopathic medicine. Improving the preferences of prehealth students, like the MSBS students, could hopefully encourage application to osteopathic medical schools, although more research is needed ideally collaborating with other osteopathic medical schools and MSBS-type programs. While specific study of the impact for those that enter other health professions must be pursued, we are hopeful that the positive change in preferences toward osteopathic medicine observed in this study could possibly have an impact on the awareness, collaboration, and utilization of the osteopathic profession in their future practice.
-
Research funding: None reported.
-
Author contributions: All authors provided substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; all authors drafted the article or revised it critically for important intellectual contact; all authors gave final approval of the version of the article to be published; all authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
-
Competing interests: None reported.
References
1. Howell, JD. The paradox of osteopathy. N Engl J Med 1999;341:1465–8. https://doi.org/10.1056/NEJM199911043411910.Search in Google Scholar PubMed
2. Barnum, S, Craig, B, Wang, X, et al.. A concordance study of COMLEX-USA and USMLE Scores. J Grad Med Educ 2022;14:53–9. https://doi.org/10.4300/JGME-D-21-00499.1.Search in Google Scholar PubMed PubMed Central
3. Draper, BB, Johnson, JC, Fossum, C, Chamberlain, NR. Osteopathic medical students’ beliefs about osteopathic manipulative treatment at 4 colleges of osteopathic medicine. J Am Osteopath Assoc 2011;111:615–30.Search in Google Scholar
4. Healy, CJ, Brockway, MD, Wilde, BB. Osteopathic manipulative treatment (OMT) use among osteopathic physicians in the United States. J Osteopath Med 2021;121:57–61. https://doi.org/10.1515/jom-2020-0013.Search in Google Scholar PubMed
5. Smith-Kelly, JB, Cardenas, A. Assessment of hospital staff’s knowledge of osteopathic manipulative medicine: a survey-based study. J Am Osteopath Assoc 2016;116:764–9. https://doi.org/10.7556/jaoa.2016.151.Search in Google Scholar PubMed
6. Beverly, EA, Wietecha, DA, Nottingham, K, Rush, LJ, Law, TD. Premedical students’ attitudes toward primary care medicine. J Am Osteopath Assoc 2016;116:302–9. https://doi.org/10.7556/jaoa.2016.060.Search in Google Scholar PubMed
7. Collins, PB, Collins, L, Darrow, GB, Sepede, J. Undergraduate knowledge of osteopathic medicine: what premedical students know about osteopathic medicine and its effect on burnout. J Osteopath Med 2020;120:855–64. https://doi.org/10.7556/jaoa.2020.149.Search in Google Scholar PubMed
8. AAMC. Matriculating student questionnaire (MSQ); 2021. Available from: https://www.aamc.org/data-reports/students-residents/report/matriculating-student-questionnaire-msq [Accessed 23 Aug 2022].Search in Google Scholar
9. AACOM. Post baccalaurate premedical programs; 2022. Available from: https://www.aacom.org/become-a-doctor/how-to-apply-to-osteopathic-medical-college/preparing-for-do-school/post-baccalaureate-premedical-programs [Accessed 22 Aug 2022].Search in Google Scholar
10. AAMC. Postbac; 2022. Available from: https://mec.aamc.org/postbac/#/index [Accessed Aug 23 2022].Search in Google Scholar
11. Sadik, A, Woldemariam, B, Wang, X. Master students’ cGPA is a good predictor of success in medical school. Med Sci Educ 2017;27:193–9. https://doi.org/10.1007/s40670-016-0366-0.Search in Google Scholar
12. AAMC. Postbac; 2022. Available from: https://mec.aamc.org/postbac/#/index [Accessed Aug 23 2022]. 12.2.0-20220628.120412.Search in Google Scholar
13. Teisberg, E, Wallace, S, O’Hara, S. Defining and implementing value-based health care: a strategic framework. Acad Med 2020;95:682–5. https://doi.org/10.1097/acm.0000000000003122.Search in Google Scholar PubMed PubMed Central
14. Ingoglia, NA. A proposal to establish master’s in biomedical sciences degree programs in medical school environments. Acad Med 2009;84:464–7. https://doi.org/10.1097/ACM.0b013e31819a7dd8.Search in Google Scholar PubMed
15. AOA. What is a DO? 2022. Available from: https://osteopathic.org/what-is-osteopathic-medicine/what-is-a-do/ [Accessed 22 Aug 2022].Search in Google Scholar
16. Bland, JM, Altman, DG. Statistics notes: Cronbach’s alpha. BMJ 1997;314:572. https://doi.org/10.1136/bmj.314.7080.572.Search in Google Scholar PubMed PubMed Central
17. Su, C-Y, Guo, Y. Factors impacting university students’ online learning experiences during the COVID-19 epidemic. J Comput Assist Learn 2021;37:1578–90. https://doi.org/10.1111/jcal.12555.Search in Google Scholar PubMed PubMed Central
18. Berland, N, Lugassy, D, Fox, A, Goldfeld, K, Oh, SY, Tofighi, B, et al.. Use of online opioid overdose prevention training for first-year medical students: a comparative analysis of online versus in-person training. Subst Abuse 2019;40:240–6. https://doi.org/10.1080/08897077.2019.1572048.Search in Google Scholar PubMed PubMed Central
19. Caton, JB, Chung, S, Adeniji, N, Hom, J, Brar, K, Gallant, A, et al.. Student engagement in the online classroom: comparing preclinical medical student question-asking behaviors in a videoconference versus in-person learning environment. FASEB BioAdvances 2021;3:110–7. https://doi.org/10.1096/fba.2020-00089.Search in Google Scholar PubMed PubMed Central
20. Brockman, RM, Taylor, JM, Segars, LW, Selke, V, Taylor, TAH. Student perceptions of online and in-person microbiology laboratory experiences in undergraduate medical education. Med Educ Online 2020;25:1710324. https://doi.org/10.1080/10872981.2019.1710324.Search in Google Scholar PubMed PubMed Central
21. Kuizin, LA. Analysis of factors that influence pre-med undergraduate selection of osteopathic or allopathic medical school [Ed.D. dissertation]. Jonesboro, Arkansas: Arkansas State University; 2018. https://www.proquest.com/docview/2124416752.Search in Google Scholar
22. Babik, JM, Luther, VP. Creating and presenting an effective lecture. J Continuing Educ Health Prof 2020;40:36–41. https://doi.org/10.1097/ceh.0000000000000281.Search in Google Scholar PubMed
23. Kooloos, JGM, Bergman, EM, Scheffers, MAGP, Schepens-Franke, AN, Vorstenbosch, MATM. The effect of passive and active education methods applied in repetition activities on the retention of anatomical knowledge. Anat Sci Educ 2020;13:458–66. https://doi.org/10.1002/ase.1924.Search in Google Scholar PubMed PubMed Central
24. Mehrkam, LR, Wynne, CDL. Behavioral differences among breeds of domestic dogs (canis lupus familiaris): current status of the science. Appl Anim Behav Sci 2014;155:12–27. https://doi.org/10.1016/j.applanim.2014.03.005.Search in Google Scholar
25. Dunning, D. Chapter five – the dunning–kruger effect: on being ignorant of one’s own ignorance. In: Olson, JM, Zanna MPBT-A in ESP, editor. Academic Press; 2011, vol 44:247–96 pp.10.1016/B978-0-12-385522-0.00005-6Search in Google Scholar
Supplementary Material
The online version of this article offers Supplementary Material (https://doi.org/10.1515/jom-2022-0139).
© 2022 the author(s), published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Frontmatter
- Behavioral Health
- Original Article
- Adverse childhood experience categories and subjective cognitive decline in adulthood: an analysis of the Behavioral Risk Factor Surveillance System
- General
- Original Article
- Understanding and preference toward DOs and OMT before and after an osteopathic principles and practice fellow lecture series
- Musculoskeletal Medicine and Pain
- Original Article
- Revisiting chronic low back pain: evidence that it is not non-specific
- Neuromusculoskeletal Medicine (OMT)
- Original Article
- Connecting the dots: alterations in bioelectric activity at acupuncture Ting (Jing-Well) points following CV4 cranial manipulation
- Pediatrics
- Brief Report
- Evaluation of academic detailing to educate clinicians regarding childhood lead poisoning prevention: a pilot study
- Public Health and Primary Care
- Original Article
- Effects of face masks on oxygen saturation at graded exercise intensities
- Clinical Image
- Annular bullous lesions in a child from Uganda: chronic bullous disease of childhood
Articles in the same Issue
- Frontmatter
- Behavioral Health
- Original Article
- Adverse childhood experience categories and subjective cognitive decline in adulthood: an analysis of the Behavioral Risk Factor Surveillance System
- General
- Original Article
- Understanding and preference toward DOs and OMT before and after an osteopathic principles and practice fellow lecture series
- Musculoskeletal Medicine and Pain
- Original Article
- Revisiting chronic low back pain: evidence that it is not non-specific
- Neuromusculoskeletal Medicine (OMT)
- Original Article
- Connecting the dots: alterations in bioelectric activity at acupuncture Ting (Jing-Well) points following CV4 cranial manipulation
- Pediatrics
- Brief Report
- Evaluation of academic detailing to educate clinicians regarding childhood lead poisoning prevention: a pilot study
- Public Health and Primary Care
- Original Article
- Effects of face masks on oxygen saturation at graded exercise intensities
- Clinical Image
- Annular bullous lesions in a child from Uganda: chronic bullous disease of childhood

