Frequency of Serious Outcomes in Patients With Hypertension as a Chief Complaint in the Emergency Department
-
Steven P. Frei
Abstract
Context: Hypertension is a common incidental finding in the emergency department (ED). However, the authors noticed a segment of patients who present to the ED specifically because their blood pressure is found to be elevated outside of the hospital. Emergency medicine physicians are often unsure of the level of intervention that is required for these patients.
Objective: To determine if these patients have serious outcomes (ie, final diagnosis of myocardial infarction, angina, coronary syndrome, congestive heart failure, pulmonary edema, hypertensive encephalopathy, malignant hypertension, stroke, transient ischemic attack, subarachnoid hemorrhage, loss of vision, kidney failure, or aortic dissection) within 7 days of the initial ED visit.
Methods: The authors retrospectively reviewed ED medical records from 2008 with a chief complaint of high blood pressure or hypertension in the physician or nursing notes. Age, sex, blood pressure, history of hypertension, associated symptoms, tests, medications, admission or discharge information, final diagnoses, and return visits within 7 days were recorded.
Results: Of the 316 medical records that were reviewed, 149 met the study criteria and were included in analysis. Patient age range was 19 to 94 years (mean, 59.8 years; median, 61 years). Sixty patients (40%) were men and 89 (60%) were women. Of the 149 patients, 121 (81%) had a previous diagnosis of hypertension and 28 (19%) did not. Five patients (3%) had a normal initial blood pressure in the ED. Sixteen patients (11%) did not undergo diagnostic tests, and 77 patients (52%) received medication in the ED. Twenty-six patients (17%) were admitted to the hospital, and 123 (83%) were discharged or eloped. Four patients (2.7%; 95% confidence interval, 0.7-6.7) had a serious outcome noted within 7 days of initial presentation to the ED.
Conclusion: Among patients presenting to the ED with a chief complaint of hypertension or high blood pressure and no serious associated complaint, the risk of serious outcome within 7 days is low.
Abstract
In this retrospective medical record review, the authors studied characteristics of patients with hypertensive concern (ie, patients who present to the emergency department specifically because their blood pressure is found to be elevated outside of the hospital), particularly frequency of serious outcomes within 7 days of the initial emergency department visit.
Hypertension is a major public health concern; an estimated 68 million US adults have the disease.1 Many patients are found to have hypertension in the emergency department (ED), with the severity of the disease ranging from asymptomatic to critically ill. The broad spectrum of this disease makes it challenging for physicians to decide the level of intervention that is required for these patients.2
There is great variability within the emergency medicine community regarding the treatment of patients with elevated blood pressure in the ED.2-7 Prior research has concentrated on hypertension found incidentally in the emergency department. These studies8-11 revealed that although hypertension in the ED is often ascribed to patients' pain and anxiety, a substantial percentage of these patients may have chronic hypertension that needs to be identified and treated as a public health measure.
Hypertension is not always an incidental finding in the ED, however. At our institution, we have observed a subset of patients who present to the ED with blood pressure as a primary concern. Their blood pressure has been measured and found to be elevated before presentation to the ED either routinely or because of some nonspecific symptom. These patients have no other symptoms that would have prompted them to seek medical care. We have categorized these patients as having hypertensive concern.
To our knowledge, no studies have examined patients who present to the ED with hypertensive concern. Characterizing these patients would help establish best practices for treating these patients in an era of rising health care spending and increasing attention to establishing value for that spending.12 In the present study, we sought to characterize patients with hypertensive concern demographically and by medical history, as well as to determine if they suffered serious outcomes within 7 days of the initial ED visit.
Methods
We obtained institutional review board approval for the present retrospective medical record review study. Patients were included if they were aged 18 years or older and if they presented to 1 of the EDs in our health network during 2008 with a chief complaint of hypertension. Our network, in Pennsylvania, is composed of 1 tertiary care suburban hospital and 2 community hospitals (1 urban, 1 suburban), with a cumulative annual census of more than 130,000 ED visits. We identified these patients by searching our ED's electronic medical record system (T-system, Inc) for medical records from the year 2008 with the key words “hypertension,” “high blood pressure,” or “blood pressure” in the chief complaint section. We then manually reviewed all the identified records and verified age and if the words “hyper tension,” “high blood pressure,” or “elevated blood pressure” were written in the first part of the chief complaint in the registration, nursing, or physician notes.
Records were excluded if patients were pregnant, if a request for blood pressure medication refill was found in the nursing or physician notes, or if 1 of the following additional serious complaints was listed with the chief complaint: headache, chest pain, shortness of breath, abdominal pain, confusion, syncope, vomiting, epistaxis, or neurologic deficit. All exclusion criteria were identified manually.
Data Collection
Records were reviewed by 1 of 3 reviewers—2 emergency physicians (S.P.F. and D.B.B.) and 1 fourth-year emergency medicine resident (J.F.C.)—and data were entered into a standard form. Interrater reliability was not evaluated. Data collected included age, sex, initial blood pressure, number of blood pressure checks on the day of presentation, previous history of hypertension, serious and minor symptoms, tests or medications administered or prescribed in the ED, admission or discharge information, final diagnoses, and return visits. Blood pressure was considered normal if the systolic blood pressure was less than 140 mm Hg and diastolic blood pressure was less than 90 mm Hg. Final diagnoses were reviewed for ED visits, hospital stays, and ED revisits at any hospital in the network within 7 days of presentation. Outcome was defined as the presence or absence of 1 of the following acutely serious final diagnoses: myocardial infarction, angina, coronary syndrome, congestive heart failure, pulmonary edema, hypertensive encephalopathy, malignant hypertension, stroke, transient ischemic attack, subarachnoid hemorrhage, loss of vision, kidney failure, or aortic dissection. Accelerated hypertension or hypertensive urgency was not considered a serious diagnosis by itself. Hospital admission by itself was not considered a serious outcome, because patients might be admitted for blood pressure concerns (hypertensive urgency) only. Final diagnosis was considered the diagnosis in the ED medical record or, if the patient was admitted to the hospital, the diagnosis listed in the discharge summary of the patient's medical record.
Statistical Analysis
Descriptive and relative frequencies were used to describe the study population. Descriptive statistics such as means, medians, and ranges were used to describe the patient characteristics. Ninety-five percent confidence intervals (CIs) were used to demonstrate the precision around our prevalence estimate. All data management and analyses were performed using Stata statistical software (version 10, Stata Corporation).
Results
From our electronic search, 316 medical records were identified. Of these, 91 did not meet the study's inclusion criteria and 3 were duplicate records. In addition, 73 records met the exclusion criteria—primarily for having another serious symptom in the chief complaint section of the medical record—and were thus not included in the study. A total of 149 medical records were analyzed (Figure).
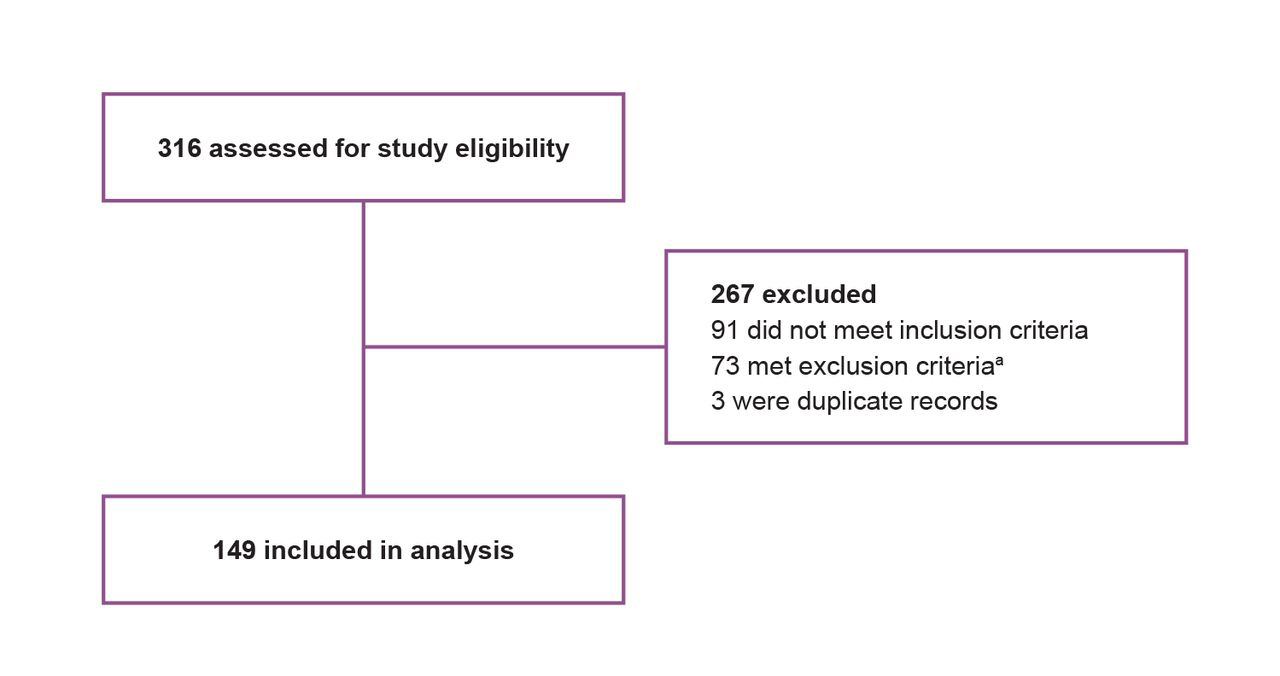
Study flow diagram of patient records assessed for hypertension as a chief complaint in the emergency department. a Another serious symptom in the chief complaint section of the medical record was the most common exclusion criterion met.
Sixty records (40%) were for men, and 89 records (60%) were for women (Table). The patient age range was 19 to 94 years, with a mean of 59.8 years and a median of 61 years. Of the 149 patients, 121 (81%) had a previous diagnosis of hypertension and 28 (19%) did not.
Characteristics of Patients Presenting to the Emergency Department With Hypertension as a Chief Complaint
| Characteristic | No. (%)a |
|---|---|
| Age, y, mean (range)b | 59.8 (19-94) |
| Sex | |
| Male | 60 (40) |
| Female | 89 (60) |
| Initial Blood Pressure, mm Hg, mean (range) | |
| Within normal limits | 5 (3) |
| Systolic | 180.8 (128-260) |
| Diastolic | 98.2 (60-148) |
| History of Hypertension | |
| Yes | 121 (81) |
| No | 28 (19) |
| Disposition | |
| Admitted | 26 (17) |
| Discharged or eloped | 123 (83) |
Five patients (3%) had a normal initial blood pressure in the ED. For initial measurement, systolic blood pressure ranged from 128 to 260 mm Hg (mean, 180.8 mm Hg; median, 178 mm Hg). Diastolic blood pressure ranged from 60 to 148 mm Hg (mean, 98.2 mm Hg; median, 98 mm Hg). Thirty-six records (24%) indicated that the patient's blood pressure had been checked frequently on the day of presentation to the ED (ie, >2 times before arrival).
In the ED, 16 patients (11%) did not undergo diagnostic tests; 13 (9%) underwent electrocardiography, 4 (3%) underwent a urine dipstick test, and 8 (5%) underwent both a urine dipstick test and electrocardiography. Other tests noted in the records included computed tomography of the head (22 patients [15%]) and chest radiography (44 patients [30%]). A total of 77 patients (52%) received medication while in the ED—44 received blood pressure medication and 33 received other medications, with acetaminophen and benzodiazepines being the most common (4 patients received potassium). Of all patients, 26 (17%) were admitted to the hospital and 123 (83%) were discharged or eloped.
Four patients (2.7%; 95% CI, 0.7-6.7) met our prespecified list of serious diagnoses: 3 had congestive heart failure, and 1 had kidney failure (worsening of chronic renal insufficiency). Two of the patients found to have congestive heart failure in the ED had a previous diagnosis of congestive heart failure; the new diagnosis was in a patient with a history of coronary artery disease, hypertension, and atrial fibrillation. Two patients with a serious diagnosis had a complaint of shortness of breath when probed, although no patients had shortness of breath as their chief complaint. Twelve patients (8%) returned to the ED within 7 days for a revisit. Many of these revisits were blood pressure rechecks. One patient had a serious diagnosis made at a revisit (exacerbation of congestive heart failure; found only at revisit).
Comment
As previously mentioned, to our knowledge our study is the first to examine patients who present to the ED with hypertensive concern. Although it has been shown that many patients with increased blood pressure in the ED are found to have chronic hypertension,7 we were surprised to find that more than 80% of patients in our study had hypertension that was already diagnosed. In this situation, physicians should arrange for better blood pressure control through discussion and follow-up with a primary physician. The ED visit may also present an opportunity for physicians to educate patients on their condition2; we have observed that, in an attempt to better manage hypertension, health care professionals sometimes frighten patients into concern over every temporary elevation in blood pressure.
Our primary purpose was to determine whether patients who present to the ED with a chief complaint of elevated blood pressure have serious outcomes. In our study, a low percentage (2.7%) of patients had serious outcomes within 7 days of ED presentation, despite some fairly extensive work-ups. Most serious outcomes were detected during clinical history and examination.
Our study had substantial limitations as a medical record review. The sample size was small, and some serious diagnoses may not have been included in the records. Also, some records indicated that treatment was provided in the ED. This treatment may have prevented some serious outcomes.
The strength of our findings must factor the lack of evaluation for interrater reliability in record abstraction and the choices the investigators made defining symptoms and whether to include or exclude them. For instance, had the 2 patients who complained of shortness of breath (not in the chief complaint) been excluded, the serious outcome percentage (even low as it was) would have been halved. In addition, although we believe the 7-day time frame for serious outcomes was realistic (most patients could schedule a visit with a primary care physician within that time), we made no attempt to independently contact these patients to determine if they had a serious outcome diagnosed after the 7-day period or at a hospital outside of our network. A prospective study would be required to address these concerns.
Future studies should examine if specific ED tests can safely be eliminated for patients with hypertension concern.
Conclusion
In patients who presented to the ED with elevated blood pressure as the chief complaint and with no other serious symptoms, the risk of a serious outcome was low. Future studies should address the usefulness of extensive workups in this patient population.
Acknowledgment
Statistical assistance was provided by research epidemiologist Stephen W. Dusza, DrPH.
-
Financial Disclosures: None reported.
References
1 Centers for Disease Control and Prevention (CDC) . Vital signs: prevalence, treatment, and control of hypertension—United States, 1999-2002 and 2005-2008. MMWR Morb Mortal Wkly Rep.2011;60(4):103-108. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6004a4.htm. Accessed August 15, 2013.Suche in Google Scholar
2 Shayne PH Pitts SR . Severely increased blood pressure in the emergency department. Ann Emerg Med.2003;41(4):513-529. http://www.ferne.org/lectures/ema_2007_pdfs/htn_%20references/ferne_htn_emerg_shayne_2003.pdf. Accessed February 11, 2013.10.1067/mem.2003.114Suche in Google Scholar PubMed
3 Karras DJ Kruus LK Cienke JJ et al. . Evaluation and treatment of patients with severely elevated blood pressure in academic emergency departments: a multicenter study. Ann Emerg Med.2006;47(3):230-236.10.1016/j.annemergmed.2005.11.001Suche in Google Scholar PubMed
4 Bender SR Fong MW Heitz S Bisognano JD . Characteristics and management of patients presenting to the emergency department with hypertensive urgency. J Clin Hypertens (Greenwich). 2006;8(1):12-18. http://onlinelibrary.wiley.com/doi/10.1111/j.1524-6175.2005.04898.x/pdf. Accessed February 8, 2013.10.1111/j.1524-6175.2005.04898.xSuche in Google Scholar PubMed PubMed Central
5 Preston RA Baltodano NM Cienki J Materson BJ . Clinical presentation and management of patients with uncontrolled, severe hypertension: results from a public teaching hospital. J Hum Hypertens.1999;13(4):249-255.10.1038/sj.jhh.1000796Suche in Google Scholar PubMed
6 Nishijima DK Paladino L Sinert R . Routine testing in patients with asymptomatic elevated blood pressure in the ED. Am J Emerg Med.2010;28(2):235-242.10.1016/j.ajem.2008.11.015Suche in Google Scholar PubMed
7 Baumann BM Cline DM Pimenta E . Treatment of hypertension in the emergency department. J Am Soc Hypertens.2011;5(5): 366-377.10.1016/j.jash.2011.05.002Suche in Google Scholar PubMed
8 Karras DJ Ufberg JW Heilpern KL et al. . Elevated blood pressure in urban emergency department patients. Acad Emerg Med.2005;12(9):835-843. http://onlinelibrary.wiley.com/doi/10.1197/j.aem.2005.04.015/pdf. Accessed February 8, 2013.10.1197/j.aem.2005.04.015Suche in Google Scholar PubMed
9 Baumann BM Abate NL Cowan RM Chansky ME Rosa K Boudreaux ED . Characteristics and referral of emergency department patients with elevated blood pressure. Acad Emerg Med.2007;14(9):779-784. http://onlinelibrary.wiley.com/doi/10.1111/j.1553-2712.2007.tb02351.x/pdf. Accessed February 8, 2013.10.1197/j.aem.2007.05.008Suche in Google Scholar PubMed
10 Svenson JE Repplinger M . Hypertension in the ED: still an unrecognized problem. Am J Emerg Med.2008;26(8):913-917.10.1016/j.ajem.2007.11.024Suche in Google Scholar PubMed
11 Shah T Aronow WS Peterson SJ Goldwag D . Diagnosis, treatment, and referral of hypertension or prehypertension in an emergency department after an educational program: preliminary results. J Clin Hypertens (Greenwich). 2011;13(6):413-415. http://onlinelibrary.wiley.com/doi/10.1111/j.1751-7176.2010.00423.x/pdf. Accessed February 8, 2013.10.1111/j.1751-7176.2010.00423.xSuche in Google Scholar PubMed PubMed Central
12 Garber A Goldman DP Jena AB . The promise of health care cost containment. Health Affairs (Millwood). 2007;26(6):1545-1547. http://content.healthaffairs.org/content/26/6/1545.full.pdf+html. Accessed February 11, 2013.10.1377/hlthaff.26.6.1545Suche in Google Scholar PubMed
© 2013 The American Osteopathic Association
This work is licensed under the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Artikel in diesem Heft
- Special Report
- 2013-2022 Strategic Plan for Research: A Role for Everyone in Promoting Research in the Osteopathic Medical Profession
- Letters to the Editor
- Osteopathic Manual Treatment and Ultrasound Therapy for Chronic Low Back Pain: An Illustration of Osteopathic Semantic Confusion
- Response
- Correction
- Correction
- Original Contribution
- Frequency of Serious Outcomes in Patients With Hypertension as a Chief Complaint in the Emergency Department
- Leg Length Discrepancy and Osteoarthritic Knee Pain in the Elderly: An Observational Study
- Evidence-Based Clinical Review
- Fibromyalgia: A Clinical Update
- Medical Education
- Frequency of Counterstrain Tender Points in Osteopathic Medical Students
- Special Communication
- The 2012-2013 Influenza Epidemic and the Role of Osteopathic Manipulative Medicine
- Case Report
- Mucormycosis in a Patient With AIDS Receiving Systemic Steroids
- Clinical Images
- Mammary Paget Disease
Artikel in diesem Heft
- Special Report
- 2013-2022 Strategic Plan for Research: A Role for Everyone in Promoting Research in the Osteopathic Medical Profession
- Letters to the Editor
- Osteopathic Manual Treatment and Ultrasound Therapy for Chronic Low Back Pain: An Illustration of Osteopathic Semantic Confusion
- Response
- Correction
- Correction
- Original Contribution
- Frequency of Serious Outcomes in Patients With Hypertension as a Chief Complaint in the Emergency Department
- Leg Length Discrepancy and Osteoarthritic Knee Pain in the Elderly: An Observational Study
- Evidence-Based Clinical Review
- Fibromyalgia: A Clinical Update
- Medical Education
- Frequency of Counterstrain Tender Points in Osteopathic Medical Students
- Special Communication
- The 2012-2013 Influenza Epidemic and the Role of Osteopathic Manipulative Medicine
- Case Report
- Mucormycosis in a Patient With AIDS Receiving Systemic Steroids
- Clinical Images
- Mammary Paget Disease

