Abstract
Background
To date, only 25 cases of cerebral infarction following a bee or wasp sting have been reported. Due to its rarity, undefined pathogenesis, and unique clinical features, we report a case of a 62-year-old man with progressive cerebral infarction following bee stings, possibly related to vasospasm. Furthermore, we review relevant literature on stroke following bee or wasp stings.
Case presentation
A 62-year-old retired male presented with progressive ischemic stroke after bee stings to the ear and face. Initial magnetic resonance imaging of the brain showed small punctate infarcts in the left medulla oblongata. Head and neck computed tomography angiography showed significant stenosis in the basilar artery and occlusion in the left V4 vertebral artery. The patient received intravenous alteplase (0.9 mg/kg) without symptomatic improvement. Digital subtraction angiography later demonstrated additional near occlusion in the left posterior cerebral artery (PCA). Thrombectomy was considered initially but was aborted due to hemodynamic instability. Repeated CT brain after 24 h showed acute infarcts in the left parieto-occipital region and left thalamus. The near occluded PCA was found to be patent again on magnetic resonance angiography (MRA) 25 days later. This reversibility suggests that vasospasm may have been the underlying mechanism. Unfortunately, the patient had persistent significant neurological deficits after rehabilitation one year later.
Conclusion
Cerebral infarction following bee stings is rare. There are several proposed pathophysiological mechanisms. While the natural course of this phenomenon is not well characterized, early diagnosis and treatment are essential. Furthermore, it is important to establish standardized care procedures for this unique entity.
1 Introduction
Wasp or bee stings are common around the world. Typical allergic symptoms include mild urticaria to severe anaphylaxis. Various unusual reactions after bee stings have been reported, involving neurological, renal, cardiac, pulmonary, and ocular systems [1]. To date, only 25 cases of cerebral infarction following a bee or wasp sting have been reported since the initial index case in 1962. Here, we report a case of a 62-year-old man with progressive cerebral infarction following bee stings and review relevant literature (Table 1) [2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26]. This rare phenomenon has unclear pathogenesis and clinical features, and there is no consensus on management.
Case reports of cerebral infarction following bee or wasp sting
| Author | Region/Year | Age/Sex | Wasp/Bee | Clinical features | CT/MR findings | Onset time | Angiography | Treatment | Prognosis |
|---|---|---|---|---|---|---|---|---|---|
| Day et al. [2] | US/1962 | 36/M | Wasp: neck, face, and arms | Headache, hemiplegia, seizure, coma | Necropsy: left hemorrhagic cortical infarction; pontine infarction | 15 min | NR | Anti-allergic phenobarbital | Died |
| Romano et al. [3] | US/1989 | 1.4/M | Wasp: inner upper lip | Hemiparesis, facial weakness | Left putamen and caudate infarctions | 4 days | Left ICA occlusion | Anti-allergic | Full recovery |
| Riggs et al. [4] | US/1993 | 38 y/M | Wasp: multiple; face and neck | Hemiplegia, aphasia | Left MCA infarction | 2 days | Left ICA occlusion | Unrecorded | NR |
| Riggs et al. [5] | US/1994 | 52/M | Wasp | Dysarthria, hemiparesis, quadriparesis | Left parietal and insular cortical infarctions | A few hours | Right ICA occlusion Left ICA near-complete occlusion | Anti-allergic | NR |
| Crawley et al. [6] | US/1994 | 30/F | Wasp: arm | Visual deficits, hypotension | Left occipital infarction | 45 min | NR | Anti-allergic | Full recovery |
| Bhat et al. [7] | India/2002 | 30/M | Bee: multiple; all over body | Dysarthria, vertigo, tinnitus, and bilateral cerebellar signs | Bilateral cerebellar hemorrhagic infarction | <1 day | NR | Anti-allergic reduced intracranial pressure | Died |
| Sachdev et al. [8] | India/2002 | 40/M | Wasp: face | Left hemiplegia, slurred speech | Right ventral pons and right cerebellum infarctions | 10 h | NR | Reduce cerebral edema aspirin | Improved |
| De-Meing Chen et al. [9] | Taiwan/2004 | 71/F | Wasp: head, face, and limbs | Facial palsy, paraplegia | Right MCA territory infarction | 1 day | Occlusion of the infrarenal aorta | Thrombectomy, anticoagulant plasmapheresis | The patient received rehabilitation programs and was discharged on the 56th day |
| Schiffman et al. [10] | US/2004 | 57/F | Bee: neck, head, eye, face, arm | Left homonymous hemianopia | Large right temporo-occipital hemorrhagic infarction | 2 days | Right PCA P1 occlusion | Anti-allergic antiemetics | Improved |
| Taurin et al. [11] | French/2006 | 36/M | Wasp: location NR | Vomiting, syncope | Left dorsal medulla infarction | 14 days | NR | Anti-allergic | Full recovery |
| Temizoz et al. [12] | Turkey/2009 | 60/M | Bee; head, face, limbs | Hemiplegia, dysarthria | Bilateral frontal lobe infarcts, right temporoparietal and bilateral centrum | 2 h | NR | Anti-allergic and aspirin | Improved slight left hemiparesis |
| Vidhate et al. [13] | India/2010 | 8/M | Wasp: eyebrow nasal bridge | Hemiplegia, altered sensorium | Infarcts in left frontoparietal region, right subcortical area, and posterior limb of the left internal capsule | 8 days | CTA normal | Systemic antibiotics, anticoagulants | Improved right-sided complete ophthalmoplegia |
| Dechyapirom et al. [14] | US/2011 | 64/M | Bee: face, neck, chest extremities | Hemiplegia, facial palsy, chest pain | Large right MCA territory infarction | 16 h | NR | Anti-allergic rt-PA | Recovery |
| Rajendiran et al. [15] | India/2012 | 25/M | Bee: head and neck | Vomiting, monoplegia, transient visual loss | Right frontoparieto-occipital infarct with hemorrhagic transformation | 1 day | NR | Anti-allergic antiemetics | Full recovery |
| Viswanathan et al. [16] | India/2012 | 59/M | Bee: face, neck, scalp, chest | Disorientation, dysarthria, facial palsy, hemiplegia, seizures, | Right perisylvian, peri-insular, and parietal cortices infarct | 2.5 h | NR | Anti-allergic aspirin, atorvastatin, and heparin | Improved |
| Jain et al. [17] | India/2012 | 70/M | Bee | Altered sensorium, hemiplegia | Left frontalparietooccipital infarction, lacunar infarcts of bilateral gangliocapsular | 6 h | MRA normal | Anti-allergic | Improved |
| Bilir et al. [18] | Turkey/2013 | 35 M | Bee: multiple; NR | Change in consciousness, dyspnea, hemiparesis | Left MCA infarction | 6 h | Neck MRA normal | Antiallergic | Residual right hemiparesis |
| Wani et al. [19] | India2014 | 40/M | Wasp: multiple; face, head, and neck | Deterioration in consciousness, hemiplegia, obtundation | Left thalamic, left parietooccipital, bilateral cerebellar hemispheres, and pontine infarction | 1 day | NR | Anti-allergic | vegetative state |
| An et al. [20] | Korea/2014 | 50/M | Bee | Left involuntary movements | Right temporal infarction | 27 h | Right M2 of MCA occlusion | Anti-allergic haloperidol aspirin | Recovery |
| Kulhari et al. [21] | US/2016 | 44/M | Wasp: leg | Hemiparesis, facial palsy, dysarthria | Multiple infarctions in right MCA | 1 h | Vasoconstriction in the bilateral proximal MCA arteries | Anti-allergic rt-PA | Recovery |
| Guzel et al. [22] | Turkey/2016 | 59/M | Bee | Mild shortness of breath left hemiplegia, | Right frontotemporoparietal infarction | A few hours | NR | Anti-allergic | Died |
| Dalugama and Gawarammana [23] | Sri Lanka/2018 | 69/F | Wasp: | Hemiplegia, aphasia | Left posterior frontal white matter infarction | NR | NR | Aspirin and atorvastatin | Improved |
| Gupta et al. [24] | India/2019 | 41/F | Honeybee: arm | Seizure, hemiparesis, dysarthria, unconscious | Bilateral thalami, left frontotemporoparietal infarctions, hemorrhage transformation | 3 h | NR | Antiepileptics, | Died |
| Elavarasi et al. [25] | India/2020 | 41/M | Bee | Hemiparesis, dysarthria | Massive right MCA territory infarction | 5 h | NR | Antiepileptics heparin, antiplatelets hemicraniectomy | Died |
| Ramlackhansingh and Seecheran [26] | Trinidad and Tobago/2020 | 70/M | Africanised honey bee: face, forearms, shoulders, and back | Dysphasia, hemiparesis | Left parietal lobe and left basal ganglia infarctions | 1 day | Normal | Antiallergic aspirin | Full recovery |
| Current study | China/2021 | 62/M | Honey bee face, neck | Speech disorder, hemiparesis | Left parieto-occipital lobe, basal ganglia, thalamus infarctions | 2 h | Stenosis of bilateral VA and BA Occlusion of P1 segment of right PCA | Anti-allergic rt-PA | Sequela |
Abbreviations: BA, basilar artery; CT, computerized tomography; CTA, computerized tomography angiography; DIC, disseminated intravascular coagulation; DSA, digital subtraction angiography; ECG, electrocardiogram; F, female; ICA, internal carotid artery; M, male; MCA, middle cerebral artery; MRA, magnetic resonance angiography; MRI, magnetic resonance imaging; NIHSS, National Institute of Health Stroke Scale; NR, not reported; PCA, posterior cerebral artery; rt-PA, recombinant tissue plasminogen activator; VA, vertebral artery.
2 Case presentation
A 62-year-old retired male with only mild hypertension was brought to the emergency department 1 h after bee stings to the ear and face. The initial symptoms were nausea, vomiting, and headache. On examination, he was found to have dysarthria, bulbar weakness, and right hemiparesis involving the arm and leg. The National Institutes of Health Stroke Scale score was 5. His blood pressure on presentation was 120/77 mmHg. The electrocardiogram showed sinus rhythm with a heart rate of 72 beats per minute. His initial non-contrast head CT was negative for hemorrhage or any acute processes. To treat a possible allergic reaction, he was given intravenous methylprednisolone and calcium gluconate. Given the possibility of acute stroke, intravenous alteplase (0.9 mg/kg) was also administered. Unfortunately, his symptoms did not improve.
Magnetic resonance imaging (MRI) of the brain was performed, which showed acute infarcts in the left medulla oblongata (Figure 1).

(a) Patent bilateral vertebral arteries (arrow) on CTA neck from three years prior to presentation; (b) admission head MRI (143 min after symptom onset) which showed small punctate infarction in the left medulla oblongata (arrow).
Head and neck CT angiography (CTA) was performed, which showed significant stenosis in the basilar artery, and occlusion in the V4 segment of the left vertebral artery (Figure 2). Digital subtraction angiography (DSA) showed significant stenosis in the V4 segment of the right vertebral artery, occlusion in the V4 segment of the left vertebral, and left posterior cerebral arteries (Figure 3). Thrombectomy was initially considered, but it was aborted due to hemodynamic instability. CT brain the next day showed acute infarcts in the left parieto-occipital region and the left thalamus (Figure 4). Repeat magnetic resonance angiography (MRA) head and neck was performed 25 days after presentation, which showed persistent stenosis in the V4 segments of the bilateral vertebral arteries, but patent bilateral posterior cerebral arteries (Figure 5).

Admission CTA (225 min after symptom onset) showed significant stenosis in the basilar artery, and occlusion of the left V4 segment of the vertebral artery(arrow). Both bilateral posterior cerebral arteries were patent at this time (arrow).

DSA (8 h after symptom onset) showed (a) significant stenosis in the right V4 segment of the vertebral artery and occlusion in the left PCA (arrow); (b) occlusion in the left V4 segment of the vertebral artery (arrow).

Head CT (18 h after symptom onset) showed ischemic infarcts in the left parieto-occipital lobe and thalamus (arrow).
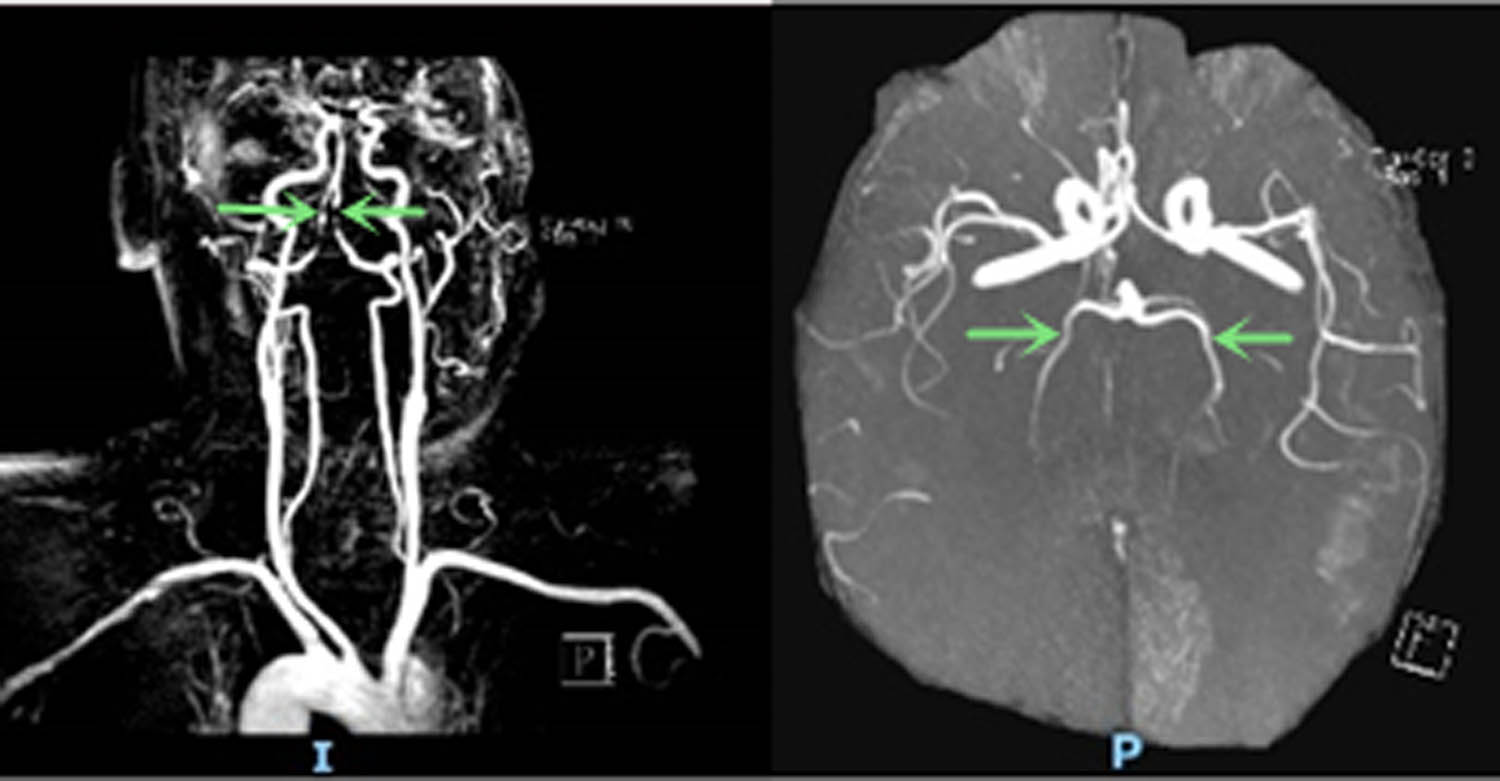
Repeat head and neck MRA (25 days after symptom onset) showed persistent stenosis in the bilateral V4 segments of the vertebral arteries and patency in bilateral posterior cerebral arteries (arrow).
He had a normal hepatorenal function, interleukin-6, fibrinogen, urine analysis, erythrocyte sedimentation rate, and coagulation testing. He was discharged to an acute rehabilitation facility. Unfortunately, at a one-year clinical follow-up, he had persistent neurologic deficits. He required percutaneous endoscopic gastrostomy due to dysphasia and tracheostomy. He was also unable to ambulate independently.
-
Ethical approval: The research related to human use has been complied with all the relevant national regulations, institutional policies and in accordance with the tenets of the Helsinki Declaration, and has been approved by the authors’ institutional review board or equivalent committee.
-
Informed consent: Informed consent has been obtained from all individuals included in this study.
3 Discussion
Adverse reactions to bee or wasp stings may present with neurological, cardiovascular, renal, pulmonary, and ocular symptoms [1,2]. Stings associated with cerebral infarction are extremely rare, and the underlying pathological mechanisms remain unclear. Furthermore, there are no guidelines for the management of stroke secondary to bee stings. We list documented cases of cerebral infarctions after bee or wasp stings (Table 1). Among all the reports, the stroke symptoms presented over a wide range of times after sting, from 15 min to 4–8 days and up to 14 days [2,3,11,13]. There were more males than females in the reviewed literature, with a ratio of 4.2:1. The ages of patients ranged from 34 months old to 71 years old [3,9]. Most individuals did not have classical stroke risk factors. Only two documented cases had a history of hypertension and smoking [10,21]. Given the rarity of this phenomenon, the TOAST classification of our case may be best described as “stroke of other determined etiology.” We believe that bee venom caused multifocal vasospasm involving different arteries. This likely resulted in the pattern of ischemic stroke confirmed on imaging. Alternatively, there could have been thrombus formation in the right V4 segment that subsequently embolized to the left posterior cerebral artery (PCA). Given the presentation with headache and vasoconstrictive trigger, a diagnosis of RCVS could also be considered [28]. The RCVS2 score for our case was 3. The features supportive of RCVS is a vasoconstrictive trigger, while the features inconsistent with RCVS is not thunderclap headache. Another possibility is secondary infarction related to rt-PA [29]. However, we believe this is less likely.
Most patients had favorable outcomes with immediate treatment; however, some had poor outcomes and four patients died [2,7,22,24]. The natural history of stroke following bee or wasp stings was, therefore, varied in the available literature. The youngest patient who died was 30 years old, and the mean age of death amongst cases was 41 years [7]. The locations of stings mainly involved the head, face, and neck. One case reported a near-global distribution of stings to the patient’s body; it was associated with bilateral hemorrhagic cerebellar infarctions [7]. Principal neurological manifestations following the sting included facial weakness, hemiplegia, slurred speech, seizures, involuntary movements, and coma [2,19,24]. Renal failure, acute coronary syndrome, and arrhythmias were also reported in some cases [1,14]. Two cases developed hypotension, and one had hypotensive syncope [6,18,20]. Thirteen patients underwent cerebral angiography, of which nine were found to have large artery stenosis or occlusion. Six cases were found to have bilateral infarctions [7,12,13,17,19,27]. Three cases were found to have bilateral large artery stenosis or occlusion [5,21]. Four cases had combined intracerebral or subarachnoid hemorrhage [2,7,10,15,24]. Currently, there is no evidence to suggest a particular vascular territory is more susceptible. In addition to stroke, bee stings have been associated with other neurologic signs and symptoms, such as trigeminal neuralgia [30] and Parkinsonism [31]. Future research is needed to better understand the relationship between stings and neurologic sequelae.
There are no specific guidelines or expert consensus on treating cerebral infarction associated with bee or wasp stings due to limited reported cases and variations in presentations. According to reported cases, it is reasonable to consider treatment with epinephrine, methylprednisolone, antihistamine, and other suitable anti-allergic drugs at an early stage. Bees generally leave their stinging apparatuses in patients’ lesions after envenomation; the Vespidae attached to the sting site often persistently inject venom. Prompt removal of such stinging apparatuses is likely beneficial [17]. Two patients obtained favorable outcomes after intravenous rt-PA. Prompt administration of intravenous rt-PA should be considered if there are no contraindications [14,21]. It is also essential to promptly correct hypotension or insufficient perfusion [6,18]. Attempts of mechanical thrombectomy have not yet been reported; our case abandoned this procedure due to hemodynamic instability. However, mechanical thrombectomy may be considered if affected individuals have large vessel occlusions and no contraindications. The possible clinical benefits require further validation alongside attention to detail concerning related comorbidities and complications. For certain patients in whom the mechanism is consistent with vasospasm, intra-arterial vasodilators are another consideration.
To date, the pathophysiological mechanisms of bee or wasp sting-associated cerebral infarction are not fully elucidated. Wasps are members of the order Hymenoptera, suborder apocrita. Sensitization to wasp venom requires only a few stings. Also, symptoms may occur after a single string [27], including a variety of reactions related to neurological, renal, pulmonary, ocular, muscular, and cardiovascular systems [1].
Postulated mechanisms include the following:
Immune system hyper-functionality: Riggs et al. [5] reported a patient who experienced a wasp sting 14 years prior to presentation. Upon being stung a second time, severe allergic reactions and bilateral occlusion of the internal carotid arteries were reported. Riggs et al. considered a possible mechanism of immune system hyper-functionality.
Global cerebral hypoperfusion: Hypotension post-sting may be attributed to histamine and prostaglandin-2 induction [19]. Vidhate et al. [13] reported an 8-year-old boy with no abnormalities of the cerebral vasculature. However, he suffered symmetrical watershed infarction bilaterally. Additionally, two patients [6,18] were also reported to have anaphylaxis-induced cerebral infarction related to hypotension and likely cerebral hypoperfusion.
Retrograde stimulation of the superior cervical ganglion: [4,5] Riggs argued that venomous insect stings may lead to systemic immune responses and increased endothelial permeability of the distal ICA. Multiple ipsilateral facial or neck wasp stings can stimulate sympathetic innervation to the distal ICA via the superior cervical ganglion.
Disseminated intravascular coagulation (DIC): Jain [17] proposed that hemolysis and endothelial damage via toxins in honeybee venom contributed to DIC development resulting in the occlusion of blood vessels by widespread fibrin thrombi in the microcirculation.
Vasoconstriction: Bee venom contains vasoactive peptides such as thromboxane, leukotrienes, and other vasoactive mediators, causing vasoconstriction that can lead to ischemic stroke [10,21]. The patient we reported had previous MRA three years prior that was negative for intracranial vessel stenosis or occlusion. Furthermore, the PCA stenosis resolved on repeat MRA 25-days after the initial presentation. This suggests vasoconstriction may be a possible mechanism underlying cerebral infarction in our patient.
4 Conclusion
In summary, cerebral infarction following bee stings is rare. Various mechanisms have been proposed but there is no consensus on the most common pathophysiology or management approach. Further experiments, including in animal models, would be of great interest to elucidate the cellular responses to the venom that lead to vascular compromise and cerebral ischemia.
-
Funding information: The study is supported by Foshan Medical Technology Innovation Platform Construction Foundation (FS0AA-KJ218-1301-0012), China and Foshan the 14th Five-Year Plan Key Discipline Foundation, China.
-
Author contributions: Y.C, S.Y. and Z.H. drafted the manuscript, G.L. and Z.Y. determined the diagnosis and treated the patient. P.F. made radiology images, J.W., R.R.K.A.Y.C and J.C. analyzed the case and revised the study. All authors have read and approved the final version of the manuscript.
-
Conflict of interest: Authors state no conflict of interest.
-
Data availability statement: The data sets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
[1] Reisman RE. Unusual reactions to insect stings. Curr Opin Allergy Clin Immunol. 2005;5(4):355–8.10.1097/01.all.0000173782.35283.b6Suche in Google Scholar
[2] Day JM. Death due to cerebral infarction after wasp stings. Arch Neurol. 1962;7:184–6.10.1001/archneur.1962.04210030022003Suche in Google Scholar
[3] Romano JT, Riggs JE, Bodensteiner JB, Gutmann L. Wasp sting-associated occlusion of the supraclinoid internal carotid artery: implications regarding the pathogenesis of moyamoya syndrome. Arch Neurol. 1989;46(6):607–8.10.1001/archneur.1989.00520420025018Suche in Google Scholar
[4] Riggs JE, Ketonen LM, Bodensteiner JB, Benesch CG. Wasp sting-associated cerebral infarction: a role for cerebrovascular sympathetic innervation. Clin Neuropharmacol. 1993;16(4):362–5.10.1097/00002826-199308000-00009Suche in Google Scholar
[5] Riggs JE, Ketonen LM, Wymer JP, Barbano RL, Valanne LK, Bodensteiner JB. Acute and delayed cerebral infarction after wasp sting anaphylaxis. Clin Neuropharmacol. 1994;17(4):384–8.10.1097/00002826-199408000-00011Suche in Google Scholar
[6] Crawley F, Schon F, Brown MM. Cerebral infarction: a rare complication of wasp sting. J Neurol Neurosurg Psychiatry. 1999;66(4):550–1.10.1136/jnnp.66.4.550Suche in Google Scholar
[7] Bhat R, Bhat KR, Shivashankar, Pais R. Bilateral haemorrhagic cerebellar infarction following honey bee sting. J Assoc Phys India. 2002;50:721–2.Suche in Google Scholar
[8] Sachdev A, Mahapatra M, D’Cruz S, Kumar A, Singh R, Lehl SS. Wasp sting induced neurological manifestations. Neurol India. 2002;50(3):319–21.Suche in Google Scholar
[9] Chen DM, Lee PT, Chou KJ, Fang HC, Chung HM, Chen DM, et al. Descending aortic thrombosis and cerebral infarction after massive wasp stings. Am J Med. 2004;116(8):567–9.10.1016/j.amjmed.2003.08.036Suche in Google Scholar
[10] Schiffman JS, Tang RA, Ulysses E, Dorotheo N, Singh SS, Bahrani HM. Bilateral ischaemic optic neuropathy and stroke after multiple bee stings. Br J Ophthalmol. 2004;88(12):1596–8.10.1136/bjo.2004.042465Suche in Google Scholar
[11] Taurin G, Canneva-Bourel ML, Delafosse JM, Poirier J, Merienne M. Dorsal medulla oblongata stroke after a wasp sting. Rev Neurol (Paris). 2006;162(3):371–3.10.1016/S0035-3787(06)75024-XSuche in Google Scholar
[12] Temizoz O, Celik Y, Asil T, Balci K, Unlu E, Yilmaz A. Stroke due to bee sting. Neurologist. 2009;15(1):42–3.10.1097/NRL.0b013e31818c7251Suche in Google Scholar PubMed
[13] Vidhate MR, Sharma P, Verma R, Yadav R. Bilateral cavernous sinus syndrome and bilateral cerebral infarcts: A rare combination after wasp sting. J Neurol Sci. 2011;301(1–2):104–6.10.1016/j.jns.2010.10.020Suche in Google Scholar PubMed
[14] Dechyapirom W, Cevik C, Nugent K. Concurrent acute coronary syndrome and ischemic stroke following multiple bee stings. Int J Cardiol. 2011;151(2):e47–52.10.1016/j.ijcard.2010.04.085Suche in Google Scholar PubMed
[15] Rajendiran C, Puvanalingam A, Thangam D, Ragunanthanan S, Ramesh D, Venkatesan S, et al. Stroke after multiple bee sting. J Assoc Phys India. 2012;60:122–4.Suche in Google Scholar
[16] Viswanathan S, Muthu V, Singh AP, Rajendran R, George R. Middle cerebral artery infarct following multiple bee stings. J Stroke Cerebrovasc Dis. 2012;21(2):148–50.10.1016/j.jstrokecerebrovasdis.2010.06.003Suche in Google Scholar PubMed
[17] Jain J, Banait S, Srivastava AK, Lodhe R. Stroke intracerebral multiple infarcts: Rare neurological presentation of honey bee bite. Ann Indian Acad Neurol. 2012;15(2):163–6.10.4103/0972-2327.95008Suche in Google Scholar PubMed PubMed Central
[18] Bilir O, Ersunan G, Kalkan A, Ozmen T, Yigit Y. A different reason for cerebrovascular disease. Am J Emerg Med. 2013;31(5):891.e5–6.10.1016/j.ajem.2012.12.040Suche in Google Scholar PubMed
[19] Wani M, Saleem S, Verma S, Yousuf I, Wani M, Asimi R, et al. Multiple cerebral infarctions with severe multi-organ dysfunction following multiple wasp stings. Ann Indian Acad Neurol. 2014;17(1):125–7.10.4103/0972-2327.128581Suche in Google Scholar PubMed PubMed Central
[20] An JY, Kim JS, Min JH, Han KH, Kang JH, Park JS, et al. Hemichorea after multiple bee stings. Am J Emerg Med. 2014;32(2):196.e1–2.10.1016/j.ajem.2013.09.024Suche in Google Scholar PubMed
[21] Kulhari A, Rogers A, Wang H, Kumaraswamy VM, Xiong W, DeGeorgia M. Ischemic stroke after wasp sting. J Emerg Med. 2016;51(4):405–10.10.1016/j.jemermed.2016.06.016Suche in Google Scholar PubMed
[22] Guzel M, Akar H, Erenler AK, Baydin A, Kayabas A. Acute ischemic stroke and severe multiorgan dysfunction due to multiple bee stings. Turk J Emerg Med. 2016;16(3):126–8.10.1016/j.tjem.2015.02.002Suche in Google Scholar PubMed PubMed Central
[23] Dalugama C, Gawarammana IB. Ischemic stroke following a wasp sting – a rare complication: a case report. J Med Case Rep. 2018;12(1):294.10.1186/s13256-018-1839-0Suche in Google Scholar PubMed PubMed Central
[24] Gupta A. Acute fatal stroke associated with honeybee sting. J Neurol Neuromed. 2020;5(1):18–21.10.29245/2572.942X/2019/1.1262Suche in Google Scholar
[25] Elavarasi A, Haq TM, Thahira T, Bineesh C, Kancharla LB. Acute ischemic stroke due to multiple bee stings – a delayed complication. Ann Indian Acad Neurol. 2020;23(1):135–6.10.4103/aian.AIAN_118_19Suche in Google Scholar
[26] Ramlackhansingh AF, Seecheran N. Africanised honey bee sting-induced ischaemic stroke. BMJ Case Rep. 2020;13(5):e234877.10.1136/bcr-2020-234877Suche in Google Scholar PubMed PubMed Central
[27] Ewan PW. Venom allergy. BMJ. 1998;316(7141):1365–8.10.1136/bmj.316.7141.1365Suche in Google Scholar PubMed PubMed Central
[28] Rocha EA, Topcuoglu MA, Silva GS, Singhal AB. RCVS2 score and diagnostic approach for reversible cerebral vasoconstriction syndrome. Neurology. 2019;92(7):e639–47.10.1212/WNL.0000000000006917Suche in Google Scholar PubMed
[29] Matsuzono K, Nagaoka L, Suzuki M, Kim Y, Ozawa T, Mashiko T, et al. Catastrophic secondary infarctions with onset seizure following tissue plasminogen activator therapy. J Stroke Cerebrovasc Dis. 2019;28(4):e24–6.10.1016/j.jstrokecerebrovasdis.2018.12.045Suche in Google Scholar PubMed
[30] Kahilogullari G, Ugur HC, Tatli M, Kanpolat Y. Trigeminal neuropathic pain following honeybee sting: a case report. Turk Neurosurg. 2010;20(2):261–4.10.5137/1019-5149.JTN.1761-09.1Suche in Google Scholar PubMed
[31] Mittal R, Munjal S, Khurana D, Gupta A. Parkinsonism following bee sting: a case report. Case Rep Neurol Med. 2012;2012:476523–2.10.1155/2012/476523Suche in Google Scholar PubMed PubMed Central
© 2022 Shuiquan Yang et al., published by De Gruyter
This work is licensed under the Creative Commons Attribution 4.0 International License.
Artikel in diesem Heft
- Research Articles
- Mice can recognise water depths and will avoid entering deep water
- CLSPCOL rescues Alzheimer’s disease mouse models
- Ischemic stroke following STA–MCA double bypass
- Relationship between subclasses low-density lipoprotein and carotid plaque
- Construction and effect evaluation of different sciatic nerve injury models in rats
- Effects of propofol on neuroblastoma cells via the HOTAIRM1/miR-519a-3p axis
- Effects of Goldblatt hypertension on rats’ hippocampal cholinergic system
- Longitudinal PET studies of mGluR5 in FXS using an FMR1 knockout mouse model
- Molecular recognition of the interaction between ApoE and the TREM2 protein
- Remimazolam induced cognitive dysfunction in mice via glutamate excitotoxicity
- Hybrid 18F-florbetapir PET/MRI for assessing myelin recovery in GFAP-A patients
- Preliminary study on pathogenic mechanism of first Chinese family with PNKD
- Aged rats learn Morris Water maze using non-spatial search strategies evidenced by a parameter-based algorithm
- Embelin and levodopa combination therapy for improved Parkinson’s disease treatment
- The roles and diagnostic value of miRNA-1246 in the serum of patients with intracranial aneurysms
- Predictors of high dose of massed practice following stroke
- The effect of stimulation frequency on transcranial evoked potentials
- Increased levels of neurofilament light chain in suicide attempters’ serum
- Propofol ameliorates ischemic brain injury by blocking TLR4 pathway in mice
- Single-cell analysis of gene expression in the substantia nigra pars compacta of a pesticide-induced mouse model of Parkinson’s disease
- Psychobiotics improve propionic acid-induced neuroinflammation in juvenile rats, rodent model of autism
- Isoliquiritigenin attenuates neuroinflammation in mice model of Parkinson’s disease by promoting Nrf2/NQO-1 pathway
- Ketamine alleviating depressive-like behaviors is associated with regulation of nNOS–CAPON–Dexras1 complex in chronic unpredictable mild stress rats
- The association of anxiety and other clinical features with CACNA1C rs1006737 in patients with depression
- Outcomes of acute ischemic stroke in kidney transplant recipients: An analysis of US Nationwide inpatient sample
- Brain atrophy pattern in patients with mild cognitive impairment: MRI study
- Correlation of serum RBP4 level with oxidative stress and unstable carotid plaque in patients with cerebral infarction
- Prevalence of neurodegenerative/demyelinating disorders in patients with achalasia
- Protection against H2O2-evoked toxicity in HT22 hippocampal neuronal cells by geissoschizine methyl ether via inhibiting ERK pathway
- Alteration in NMDAR subunits in different brain regions of chronic unpredictable mild stress (CUMS) rat model
- Acacetin improves cognitive function of APP/PS1 Alzheimer’s disease model mice via the NLRP3 inflammasome signaling pathway
- Assessment of malformations, variations and diameters of vessels forming the circle of Willis – An autopsy study in a non-cerebrovascular cohort
- Singular versus combinatory glucose-sensitive signal control of metabolic sensor protein profiles in hypothalamic astrocyte cultures from each sex
- Mild acute stress prevents the memory impairment induced by long-term isoflurane anesthesia
- Esketamine improves propofol-induced brain injury and cognitive impairment in rats
- Correlations between EEG and intestinal electrical stimulation
- Factors influencing recovery of upper limb motor function during constraint-induced movement therapy for people with stroke
- Application of auditory mismatch negativity in tinnitus patients based on high-resolution electroencephalogram signals
- The value of transcranial Doppler monitoring of cerebral blood flow changes during carotid endarterectomy performed under regional anesthesia – A case series
- Acacetin alleviates neuroinflammation and oxidative stress injury via the Nrf2/HO-1 pathway in a mouse model of spinal cord injury
- Pre-ischemic exercise prevents inflammation and apoptosis by inhibiting MAPK pathway in ischemic stroke
- Fronto-parietal single-trial brain connectivity benefits successful memory recognition
- Review Articles
- Machine learning approaches for diagnosing depression using EEG: A review
- Perinatal diet and offspring anxiety: A scoping review
- Brain and gut microbiota disorders in the psychopathology of anorexia nervosa
- Nanotechnology-based drug delivery for the treatment of CNS disorders
- Case Reports
- A rare giant intracranial arachnoid cyst confused the diagnosis and treatment of Wilson disease
- Cerebral infarction following bee stings: Case report and literature review
- Neurosarcoidosis presenting as longitudinally extensive myelitis: Diagnostic assessment, differential diagnosis, and therapeutic approach
- Long-acting paliperidone in Ekbom’s syndrome in Lewy body dementia: A case report
- Patients with post-COVID-19 vaccination facial palsy: To boost or not to boost?
- Autosomal dominant sleep-related hypermotor epilepsy associated with a novel mutation of KCNT1
- A rare brainstem anaplastic astrocytoma
- A singular case of hyposmia and transient audiovestibular post-vaccine disorders: case report and literature review
- A rare lymphoplasmacyte-rich meningioma involving the dura of the skull base and cervical spinal cord: A case report
- Communication
- The system’s genetics of depression and its somatic and mental comorbidities
- Commentary
- The possible association between neurodegenerative/demyelinating neurological disorders in achalasia patients
- Letter to the Editor
- A patient with hereditary transthyretin amyloidosis involving multiple cranial nerves due to a rare p.(Phe84Ser) variant
- Erratum
- Erratum to “Spinocerebellar ataxia type 40: A case report and literature review”
- Erratum to “Construction and effect evaluation of different sciatic nerve injury models in rats”
- Retraction
- Nervonic acid amends motor disorder in a mouse model of Parkinson’s disease
- Retraction of “Isovitexin modulates autophagy in Alzheimer’s disease via miR-107 signalling”
Artikel in diesem Heft
- Research Articles
- Mice can recognise water depths and will avoid entering deep water
- CLSPCOL rescues Alzheimer’s disease mouse models
- Ischemic stroke following STA–MCA double bypass
- Relationship between subclasses low-density lipoprotein and carotid plaque
- Construction and effect evaluation of different sciatic nerve injury models in rats
- Effects of propofol on neuroblastoma cells via the HOTAIRM1/miR-519a-3p axis
- Effects of Goldblatt hypertension on rats’ hippocampal cholinergic system
- Longitudinal PET studies of mGluR5 in FXS using an FMR1 knockout mouse model
- Molecular recognition of the interaction between ApoE and the TREM2 protein
- Remimazolam induced cognitive dysfunction in mice via glutamate excitotoxicity
- Hybrid 18F-florbetapir PET/MRI for assessing myelin recovery in GFAP-A patients
- Preliminary study on pathogenic mechanism of first Chinese family with PNKD
- Aged rats learn Morris Water maze using non-spatial search strategies evidenced by a parameter-based algorithm
- Embelin and levodopa combination therapy for improved Parkinson’s disease treatment
- The roles and diagnostic value of miRNA-1246 in the serum of patients with intracranial aneurysms
- Predictors of high dose of massed practice following stroke
- The effect of stimulation frequency on transcranial evoked potentials
- Increased levels of neurofilament light chain in suicide attempters’ serum
- Propofol ameliorates ischemic brain injury by blocking TLR4 pathway in mice
- Single-cell analysis of gene expression in the substantia nigra pars compacta of a pesticide-induced mouse model of Parkinson’s disease
- Psychobiotics improve propionic acid-induced neuroinflammation in juvenile rats, rodent model of autism
- Isoliquiritigenin attenuates neuroinflammation in mice model of Parkinson’s disease by promoting Nrf2/NQO-1 pathway
- Ketamine alleviating depressive-like behaviors is associated with regulation of nNOS–CAPON–Dexras1 complex in chronic unpredictable mild stress rats
- The association of anxiety and other clinical features with CACNA1C rs1006737 in patients with depression
- Outcomes of acute ischemic stroke in kidney transplant recipients: An analysis of US Nationwide inpatient sample
- Brain atrophy pattern in patients with mild cognitive impairment: MRI study
- Correlation of serum RBP4 level with oxidative stress and unstable carotid plaque in patients with cerebral infarction
- Prevalence of neurodegenerative/demyelinating disorders in patients with achalasia
- Protection against H2O2-evoked toxicity in HT22 hippocampal neuronal cells by geissoschizine methyl ether via inhibiting ERK pathway
- Alteration in NMDAR subunits in different brain regions of chronic unpredictable mild stress (CUMS) rat model
- Acacetin improves cognitive function of APP/PS1 Alzheimer’s disease model mice via the NLRP3 inflammasome signaling pathway
- Assessment of malformations, variations and diameters of vessels forming the circle of Willis – An autopsy study in a non-cerebrovascular cohort
- Singular versus combinatory glucose-sensitive signal control of metabolic sensor protein profiles in hypothalamic astrocyte cultures from each sex
- Mild acute stress prevents the memory impairment induced by long-term isoflurane anesthesia
- Esketamine improves propofol-induced brain injury and cognitive impairment in rats
- Correlations between EEG and intestinal electrical stimulation
- Factors influencing recovery of upper limb motor function during constraint-induced movement therapy for people with stroke
- Application of auditory mismatch negativity in tinnitus patients based on high-resolution electroencephalogram signals
- The value of transcranial Doppler monitoring of cerebral blood flow changes during carotid endarterectomy performed under regional anesthesia – A case series
- Acacetin alleviates neuroinflammation and oxidative stress injury via the Nrf2/HO-1 pathway in a mouse model of spinal cord injury
- Pre-ischemic exercise prevents inflammation and apoptosis by inhibiting MAPK pathway in ischemic stroke
- Fronto-parietal single-trial brain connectivity benefits successful memory recognition
- Review Articles
- Machine learning approaches for diagnosing depression using EEG: A review
- Perinatal diet and offspring anxiety: A scoping review
- Brain and gut microbiota disorders in the psychopathology of anorexia nervosa
- Nanotechnology-based drug delivery for the treatment of CNS disorders
- Case Reports
- A rare giant intracranial arachnoid cyst confused the diagnosis and treatment of Wilson disease
- Cerebral infarction following bee stings: Case report and literature review
- Neurosarcoidosis presenting as longitudinally extensive myelitis: Diagnostic assessment, differential diagnosis, and therapeutic approach
- Long-acting paliperidone in Ekbom’s syndrome in Lewy body dementia: A case report
- Patients with post-COVID-19 vaccination facial palsy: To boost or not to boost?
- Autosomal dominant sleep-related hypermotor epilepsy associated with a novel mutation of KCNT1
- A rare brainstem anaplastic astrocytoma
- A singular case of hyposmia and transient audiovestibular post-vaccine disorders: case report and literature review
- A rare lymphoplasmacyte-rich meningioma involving the dura of the skull base and cervical spinal cord: A case report
- Communication
- The system’s genetics of depression and its somatic and mental comorbidities
- Commentary
- The possible association between neurodegenerative/demyelinating neurological disorders in achalasia patients
- Letter to the Editor
- A patient with hereditary transthyretin amyloidosis involving multiple cranial nerves due to a rare p.(Phe84Ser) variant
- Erratum
- Erratum to “Spinocerebellar ataxia type 40: A case report and literature review”
- Erratum to “Construction and effect evaluation of different sciatic nerve injury models in rats”
- Retraction
- Nervonic acid amends motor disorder in a mouse model of Parkinson’s disease
- Retraction of “Isovitexin modulates autophagy in Alzheimer’s disease via miR-107 signalling”

