Abstract
Objectives
Micro- and macrovascular endothelial deterioration has been mentioned in diabetic pregnants with critical clinical outcome for the fetus. Our aim was to measure serum and cord blood concentrations of methylated arginines in patients with gestational diabetes and find a relationship with endothelial dysfunction.
Materials and methods
Methylated arginines were detected with high performance liquid chromatography mass spectrometry via electrospray ionization positive technique with a chromatographic C18 column.
Results
Although gestational diabetes mellitus (GDM) groups’ asymmetric dimethylarginine (ADMA) levels were higher compared to control group, this difference was not significant. Control cord blood ADMA and N-monomethylarginine levels were significantly higher than insulin-regulated GDM cord blood ADMA and N-monomethylarginine levels (p=0.001; p=0.003, respectively). Diet-regulated GDM group’s cord blood N-monomethylarginine was significantly higher than insulin-regulated GDM group’s cord blood N-monomethylarginine (p=0.045). A negative correlation was found between cord blood symmetric dimethylarginine and oral glucose tolerance testing 0h glucose values (r=−0.453, p=0.002).
Conclusions
According to this study’s results, methylated arginine levels may not be associated with endothelial deterioration in GDM otherwise with preeclampsia risk.
Öz
Amaç
Diabetik gebelerde, fetüs için kritik klinik sonuçlara yol açacak mikro- ve makrovasküler endotelyal bozulma bildirilmiştir. Amacımız, gestasyonel diabeti olan hastalarda metilenmiş arjininlerin serum ve kord kanı konsantrasyonlarını ölçmek ve endotelyal disfonksiyon ile ilişkisini ortaya koymaktır.
Gereç ve Yöntemler
Metillenmiş arjinin türevleri, elektrosprey iyonizasyon pozitif mod tekniği ile kromatografik C18 kolon kullanılarak yüksek performanslı sıvı kromatografi kütle spektrometre yöntemi ile saptanmıştır.
Bulgular
Her ne kadar gestasyonel diabetes mellitus gruplarının asimetrik dimetilarjinin seviyeleri kontrol grubuna kıyasla yüksek olsa da, bu fark önemli bulunamamıştır. Kontrol kord kanı asimetrik dimetilarjinin ve N-monometilarjinin seviyeleri, insülin-regüle gestasyonel diabetes mellitus grubunun kord kanı asimetrik dimetilarjinin ve N-monometilarjinin seviyelerinden anlamlı olarak yüksek idi (Sırasıyla, p=0.001; p=0.003). Diet-regüle gestasyonel diabetes mellitus grubunun kord kanı N-monometilarjinin seviyeleri, insülin-regüle gestasyonel diabetes mellitus grubunun kord kanı N-monometilarjinin seviyelerinden anlamlı olarak yüksek idi (p=0.045). Kord kanı simetrik dimetilarjinin ve oral glukoz toleras testi 0.saat glukoz düzeyleri arasında negatif bir korelasyon saptandı (r=−0.453, p=0.002).
Sonuçlar
Bu çalışmanın sonuçlarına göre metilenmiş arjinin seviyeleri, preeklempsi riski olmadığı durumda gestasyonel diabetes mellitus hastalığında endotelyal bozulma ile birliktelik göstermeyebilir.
Introduction
Gestational diabetes mellitus (GDM), identified as glucose intolerance with the period of pregnancy, is one of widely acquired obstetrical complications, affecting 5–8% of all pregnancies. During last decade, the incidence of GDM was notified to rise up [1]. GDM represents a major risk for fetal development and outcome and is of importance for development of such metabolic and cardiovascular consequences [2]. Hyperglycaemia becomes evident after birth. These individuals are at high risk of developing type 2 diabetes and distinct cardiovascular disease (CVD). Therefore, early diagnosis of GDM might be useful for clinicians to identify a proportionally young individuals at high risk for cardiovascular outcomes and to respond promptly to reduce this possible consequences [3]. Vascular reactivity might be explained by many pathways such as locally generated vasoactive chemicals from the endothelium. Several pathological consitions are related with attenuated potential of endothelium to produce the efficient vasodilator nitric oxide (NO) [4]. NO is a potent vasodilator, and has an important role for the function of endothelial progenitor cells, which can immigrate to and fractionate at damage area to support the formation of new vessels in healthy subjects [5]. Lack of endothelial properties such as organization of vascular tonus means that deficiency of cellular functions, mentioned as endothelial dysfunction [6]. Methylated arginine derivaties are compounds synthesized via the action of enzymes called protein methyltransferases (PRMT) types I and II (PRMT I and II). Methylated arginines including asymmetric dimethylarginine (ADMA), symmetric dimethylarginine (SDMA) and N-monomethylarginine (L-NMMA) has a capacity of acting as inhibitor molecules for NO production by nitric oxide synthase (NOS). Whereas the structure of ADMA is similar to arginine, it competes with arginine for NOS binding, hereby blocking the formation of NO from arginine by NOS directly. NOS is mainly localized in the cell, thus the intracellular ADMA and arginine levels regulate NOS activity. In addition, extracellular ADMA is an antagonist to extracellular arginine on cell membrane transporter level, whereas they are both transported into the cell via the cell membrane by the cationic amino acid transporter (CAT). Since ADMA competes with arginine for NOS and for cell transport via CAT-2, the bioavailability of NO depends on the balance between the two, the so-called arginine/ADMA ratio. The arginine/ADMA ratio is an important indicator of NO bioavailability and therefore of the risk of formation of atherosclerotic plaques [7].
Even though L-NMMA and ADMA has been concluded to have potential fundamental inhibitory effects on NO synthesis, SDMA is also known to prevent the uptake of basic NO substrate, arginine. Due to this property, SDMA has also effects to diminish NO production [8]. NO synthase activity is regulated by both negative feedback and availability of L-arginine. L-Arginine is a semi-essential amino acid obtained either from the diet or synthesized endogenously from L-citrulline. L-citrulline, in turn, can be derived from ornithine in the catabolism of proline or glutamine and glutamate, or from L-arginine via arginine–citrulline pathway. L-Citrulline can also be obtained during the degradation of ADMA, the process catalyzed by dimethylarginine dimethylaminohydrolase (DDAH), yielding dimethylamine (DMA) as a coproduct [9].
In this study, our aim was to measure cord blood and serum concentrations of methylated arginine levels in gestational diabetic subjects and find a relationship with endothelial dysfunction.
Materials and methods
Study design
Pregnant women admitting to the pregnancy outpatient units of Selcuk University Faculty of Medicine hospital between July 2017 and March 2018 were included in the present study. Participiants were classified into 36 diet-regulated GDM (mean age 33±5 years), 38 insulin-regulated GDM (mean age 33±5 years) and 31 control subjects (mean age 28±5 years). GDM was diagnosed via confirmation of at least two elevated serum glucose levels with 100 g 3 h oral glucose tolerance testing (OGTT) according to Carpenter and Cousten criteria (fasting serum glucose value: 95 mg/dL, first hour serum glucose value: 180 mg/dL, second hour serum glucose value: 155 mg/dL, third hour serum glucose value: 140 mg/dL). For 50 g glucose-loading test, a cut-off value of ≥140 mg/dL serum glucose levels were accepted as positive. According to The International Association of Diabetes in Pregnancy Study Groups (IADPSG) consensus paper, a 75 g OGTT in additon to the Carpenter and Coustan criteria should be performed to all pregnant subjects without a previous diagnosis of diabetes mellitus [10]. However, present study has been planned according to the routine follow up procedure of our hospital and Turkish Endocrinology Organization recommendations.
All participants was given written informed consent and this study was approved by Ethics Committe. The exclusion criteria of this study were to suffer from diabetes mellitus, chronic kidney disease, hypertension, and several chronic inflammatory diseases. There were three preeclampsia, four early delivery abortion and five intrauterine growth restriction (IUGR) patients. Demographic and clinical properties such as patient names, birth dates, week of gestation, the number of participiants, body mass index, weights on the onset and after birth, smoking status, family history of diabetes and weights of babies were collected for all subjects.
Biochemical measurements
Eight milliliters of venous blood samples were collected into plain tubes (BD Vacutainer, Franklin Lakes, NJ, USA) by phlebotomy from each participiants and analyzed according to stability procedures. After the centrifugation at 3500×g for 10 min at 4°C, sera were collected and stored at −80°C until the biochemical measurements. Methylated arginine derivatives such as SDMA, ADMA, L-NMMA and also arginine and citrulline (Sigma, Karlsruhe, Germany) of serum and cord blood were determined via high performance liquid chromatography (Shimadzu LC-20AD system (Tokyo, Japan) tandem mass spectrometry [Applied Biosystems MDS SCIEX (Foster City, CA, USA) API 3200]. This electrospray ionization (ESI) technique was operated in positive mode with a high resolution chromatography column [Phenomenex (Torrance, CA, USA) Luna C18] [11].
According to this prodecure, 100 μL of internal standard [(deuterated7-ADMA (Cambridge Isotopes, Tewksbury, MA, USA)] dissolved in methanol (Merck, Darmstadt, Germany) were added to 200 μL of sample and proteins were seperated after centrifugation via 6000 g for 10 min. The clear supernatant was taken and evaporated under a nitrogen gas flow at 60°C. Two hundred microliters of fresh butanol (Merck, Darmstadt, Germany) solution including 5% (vv−1) acetyl chloride (Merck, Darmstadt, Germany) were used for derivatizion of samples. The mixture was incubated at 60°C for 20 min. The mixture was dried under nitrogen flow at 60°C. The bulks were dissolved in 100 μL of water (Merck, Darmstadt, Germany) – methanol (Merck, Darmstadt, Germany) (90:10, vv−1) containing 0.1% (vv−1) formic acid (Sigma, Karlsruhe, Germany) and 40 μL were used for injection to chromatographic column. Mobile phase A and B consist of high performance liquid chromatography grade water containing 0.1% (vv−1) formic acid and methanol containing 0.1% (vv−1), respectively with a total binary flow of 0.8 mL. Chromatographic seperation was performed on Phenomenex Luna C18 column (Torrance, CA, USA) (250×4.6 mm, 5 μm, 100 Å) in 5 min analysis time. Mass spectrometric parameters were such as: ion source gas 1: 60; ion source gas 2: 60; entrance potential: 7.5; collision cell exit potential: 4; ion sprey voltage: 5500 V; declustering potential: 40; collision gas: 5; collision energy: 24; temperature: 550°C. Methylated arginine derivatives’ analysis was assessed by an optimisation procedure with an infusion of a 50 μM solution of each molecule. According to this method, either intra-day coefficient variation (CV) or inter-day CV values for methlated arginine molecules were both under 20%. The limit of detection and the limit of quantification were below or equal than the lowest calibration point: LOD was 0.01 μM for all compounds in serum. The LOQ was 0.05 μM for ADMA, SDMA, L-NMMA, citrulline and arginine. The observed bias for all added concentrations was <±17% and recoveries were between 80 and 92% (80% for L-NMMA).
Statistical analysis
Statistical analyses were assessed by Statistical Package for the Social Sciences (SPSS) v 15.0. Distrubition of parameters were controlled via Shapiro–Wilk test.
The descriptive properties of methlated arginine and demographic data were given as mean±standard deviation or median (minimum-maximum). Student t-test and Mann-Whitney U-tests were used for parametric and non-parametric distrubitions to identify the statistical difference of groups, respectively. Spearman correlation test was performed. p<0.05 was accepted as statistically significant.
Results
In this study, no significant difference was found for pregnants’ serum methylated arginine values (for all groups p>0.05). The demographic data and methylated arginine levels were expressed in Table 1. No significant difference was found between diet-regulated GDM cord blood SDMA [2.47 (1.25–7.49) μmol/L] and insulin-regulated GDM cord blood SDMA levels [2.03 (1.22–6.63) μmol/L] (p=0.200). (Figure 1). Maternal serum L-NMMA positively correlated with 3 h OGTT serum glucose level (r=0.294, p=0.043).
Maternal and cord blood methylated arginine levels and demographic data of all groups.
| Control (n=31) | Diet regulated GDM (n=36) | Insulin regulated GDM (n=38) | p-Value | |
|---|---|---|---|---|
| Maternal serum ADMA (μmol/L) | 0.37±0.13 | 0.39±0.16 | 0.37±0.11 | 0.808 |
| Maternal serum SDMA (μmol/L) | 0.44 (0.28–1.02) | 0.46 (0.19–1.01) | 0.47 (0.15–0.87) | 0.647 |
| Maternal serum L-NMMA (μmol/L) | 0.05 (0.02–0.4) | 0.05 (0.006–0.19) | 0.04 (0.01–0.2) | 0.501 |
| Maternal serum arginine (μmol/L) | 149 (30–272) | 145 (14–270) | 164 (22–898) | 0.233 |
| Maternal serum citrulline (μmol/L) | 29 (6–62) | 35 (4–76) | 34 (4–59) | 0.165 |
| Maternal arginine/ADMA ratio | 422 (73–776) | 404 (82–836) | 422 (73–1448) | 0.311 |
| Cord blood arginine (μmol/L) | 174±120 | 170±101 | 154±72 | 0.673 |
| Cord blood arginine/ADMA ratio | 79±51 | 94±44 | 107±54 | 0.084 |
| Cord blood ADMA (μmol/L) | 2.28±0.80 | 1.93±0.86 | 1.61±0.62 | 0.001a |
| Cord blood SDMA (μmol/L) | 3.68 (1.65–6.39) | 2.47 (1.25–7.49) | 2.03 (1.22–6.63) | <0.001a |
| Cord blood L-NMMA (μmol/L) | 0.23±0.09 | 0.19±0.06 | 0.17±0.03 | 0.045a |
| Cord blood citrulline (μmol/L) | 41 (8–125) | 44 (23–149) | 37 (9–103) | 0.016a |
| Maternal age (years) | 28±5 | 33±5 | 33±5 | <0.001a |
| Maternal height (cm) | 160±6 | 160±8 | 159±4 | 0.745 |
| Maternal weight (kg) | 77±10 | 81±11 | 81±11 | 0.205 |
| Weight of birth (g) | 3419±408 | 3397±591 | 3240±515 | 0.237 |
| BPD (mm) | 38 (35–41) | 38 (32–84) | 38 (34–41) | 0.189 |
| AC (mm) | 38.2±1.41 | 38.0±2.0 | 37.7±1.68 | 0.309 |
| FL (mm) | 38 (36–41) | 38 (33–78) | 38 (33–41) | 0.017a |
Parameters were expressed as median (minimum-maximum) and mean±SD, respectively. n=number of participiants. aConsidered as significant. GDM, gestational diabetes mellitus; BPD, biparietal diameter; AC, abdominal circumference; FL, femur length; ADMA, asymmetric dimethylarginine; SDMA, symmetric dimethylarginine; L-NMMA, N-monomethylarginine.
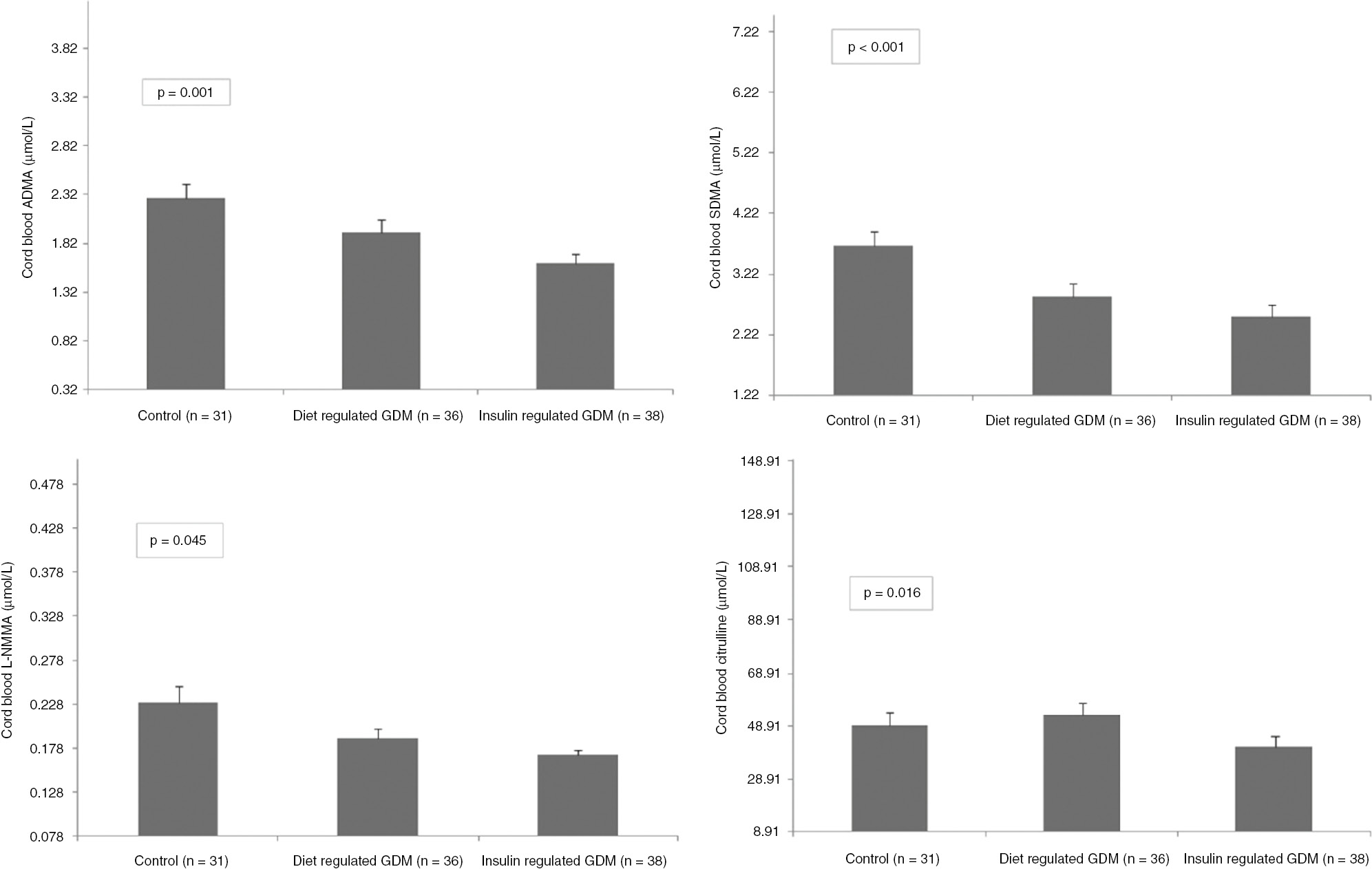
Cord blood ADMA, SDMA, L-NMMA, citrulline levels of control and GDM groups.
Subjects with preeclampsia (n=3) were found to have two-fold increase in ADMA (0.75 vs. 0.36 μmol/L) and two-fold decrease in Arginine/ADMA ratios (429 vs. 207).
Cord blood SDMA negatively correlated with 0 h OGTT serum glucose levels (r=−0.453, p=0.002) (Figure 2).
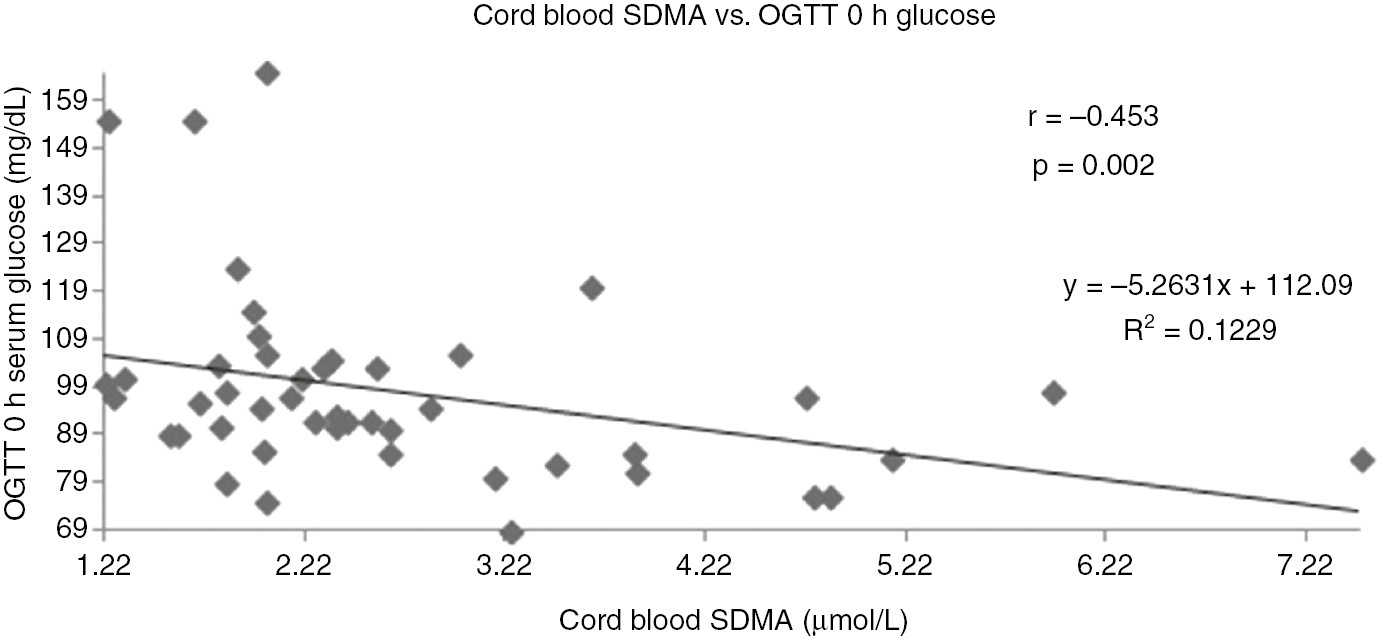
Correlation between cord blood SDMA and OGTT 0 h glucose.
There was a negative correlation between cord blood L-NMMA and OGTT 1 h serum glucose levels (r=−0.401, p=0.006) (Figure 3). There was no significant correlation between other maternal or cord blood methylated arginines and OGTT glucose levels.
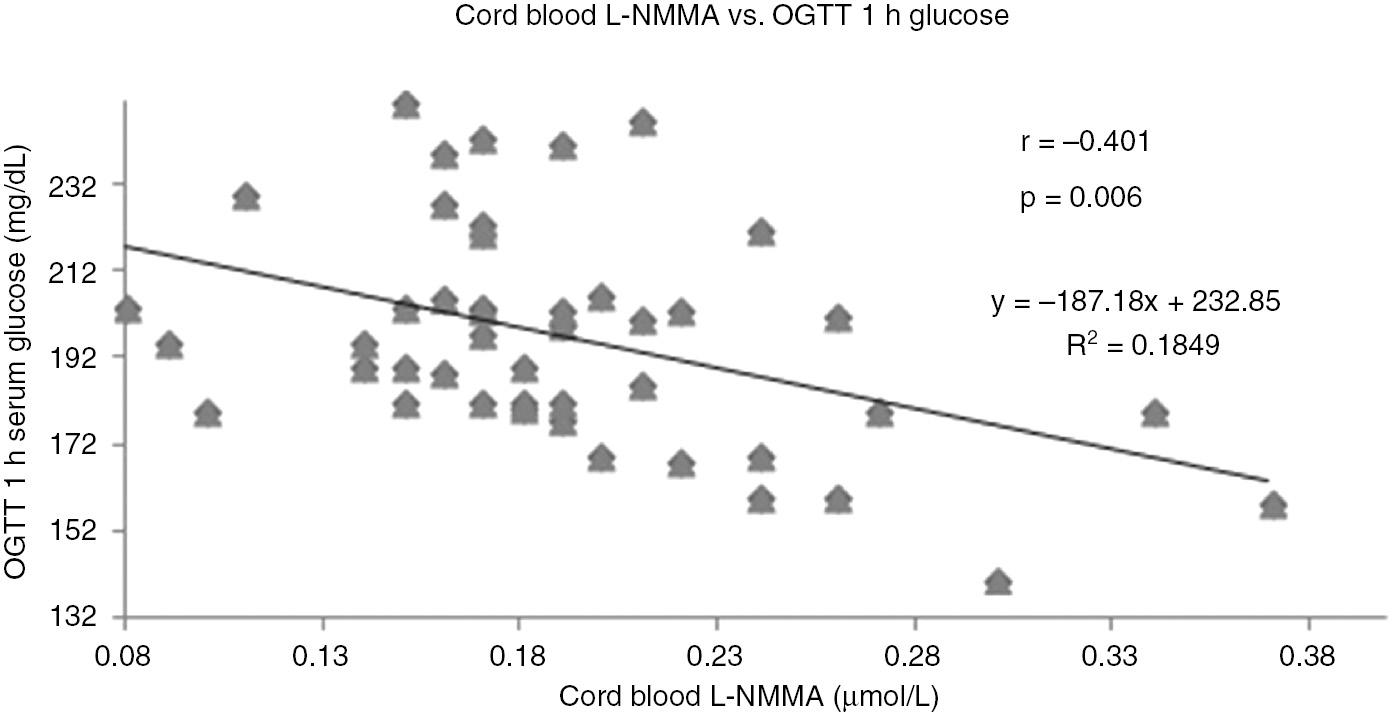
Correlation between cord blood L-NMMA and OGTT 1 h glucose.
Discussion
Gestational diabetes is a syndrome that occurs during pregnancy and associated with impaired glucose metabolism leading to endothelial deterioration and improper organization of vascular tonus. One important local mechanism involved in the control of vascular tonus is endothelial NO synthesis, a process that could require membrane transport of L-arginine, the substrate for eNOS [12].
In recent years, alterations in methylated arginine metabolites have been suggested as a early onset predictor of endothelial deterioration and proved to be a unique, distinct risk factor of several cardiovascular and metabolic conditions.
There are contradictious ADMA and SDMA results in patients with GDM in the literature. Telejko et al. reported the levels of ADMA in 56 patients with gestational diabetes (GDM), 68 pregnant subjects with normal glucose tolerance (NGT) and 36 healthy non-pregnant participiants. ADMA concentrations were found to be substantially lower in NGT (0.48 μmol/L) compared to GDM (0.50 μmol/L) and healthy non-pregnant (0.57 μmol/L) groups and reported that a decrease in circulating ADMA concentrations might be associated with physiological adaptation process [13]. In their study an enzyme linked immunosorbent assay commercial kit was used for the detection of ADMA and Arginine/ADMA ratio was not calculated. A multimarker approach by determining serum methylated arginines might provide useful information about the all parameters related to NO synthesis. Thus, a single step and more sensitive measurement of these molecules by liquid chromatography tandem mass spectrometry offers us to have more accurate results of this NO-related pathway. In this study, accurate and precise measurement of ADMA and arginine was performed with tandem mass spectrometry and there was no difference for serum ADMA levels and Arginine/ADMA ratios for all groups (Table 1).
Mittermayer et al. conducted a study with 46 obese, 31 non-obese GDM patients and 17 healthy women. ADMA concentrations were similiar for obese and non-obese GDM subjects (0.58±0.02 and 0.57±0.02 μmol/L, respectively), and the levels were found to be elevated compared to control group (0.47±0.03 μmol/L). Although SDMA levels and ADMA/SDMA ratios were found to be higher in obese GDM, SDMA concentrations were higher in GDM groups than controls [14]. In another study with 77 subjects with GDM who carried out a 75 g OGTT and follow-up, they reported a correlation between serum ADMA levels and blood pressure without a correlation with metabolic parameters (body-mass index, fasting glucose levels and lipid levels). In their study, Arginine and symmetrical dimethyl arginine were not associated with glucose values. During the follow-up period, Arginine and ADMA were found to diminish. Glucose tolerance was affected in 36% of GDM patients over 0.56 μmol/L median ADMA values [15].
These results are in consistency with previous data. Such that Pettersson et al. analyzed serum concentrations of arginine and ADMA that were collected at 32–39 weeks of gestation, 3–5 days and 3 months after birth from 12 pregnant subjects with advanced preeclampsia and from pregnant participiants without hypertension (n=12). In their study, it was found that at the course of third trimester, serum ADMA levels tended to be higher (p<0.05) in the preeclampsia patients (0.55±0.02 μmol/L) compared to the control group (0.36±0.01 μmol/L). There was no stastistically significant difference between both groups for arginine levels (80.7±5.8 μmol/L) and 74.5±3.8 μmol/L, respectively), arginine/ADMA ratio was found to be decreased (p<0.05) in the preeclamptic group (145.6±10.5) compared to controls (211.0±14.3) [16]. These findings suggest a link between high blood pressure and circulating methlated arginine levels. Also, in this study there were three preeclampsia, four early delivery abortion and five IUGR patients. Patients with preeclampsia were found to have two-fold increase in ADMA levels (0.75 vs. 0.36 μmol/L) and two-fold decrease in Arginine/ADMA ratios (429 vs. 207). In this study, although not statistically significant (p=0.084), the cord blood of patients with GDM regulated by diet or insulin has a trend to increase the ratio of Arginine/ADMA. This may be a condition that develops in response to decreased NO synthesis due to gestational diabetes (Table 1).
Pleiner et al. performed a research with seven overweight and five non-overweight women with GDM. They found that there was no significant difference between non-overweight participiants and healthy subjects for serum ADMA levels. SDMA and ADMA levels were found to be elevated in obese GDM than non-obese group (0.58±0.04 and 0.55±0.03 vs. 0.46±0.07 and 0.40±0.07 μmol/L, respectively) [17].
Gumus et al. performed a study with 30 subjects with GDM and 40 healthy controls participiants with similiar age and body-mass index values. According to their study’s results, serum ADMA levels were elevated in patients with GDM rather than control group (0.45±0.11 vs. 0.31±0.13 μmol/L, respectively; p=0.01) [18].
Sertkaya et al. compared plasma concentrations of ADMA in 58 GDM, 30 pregnant subjects with positive glucose challange test but negative OGTT (AGCT) and 50 healthy pregnant individuals. ADMA values were significantly elevated compared to control subjects (3.60±1.21; 4.00±1.70; 2.65±0.82 μmol/L, respectively, p=0.001). They concluded that the rise of ADMA values in pregnant subjects with glucose intolerance might probably be by virtue of higher insulin values [19]. Interestingly, there was a 10-fold increase in ADMA levels in this study’s control group compared to other studies at all. In this study, while the methylated arginine derivatives that indirectly block NO synthase, play an important role in vascular pathologies due to hyperglycaemia and endothelial dysfunction, especially in the chronic basis, the negative correlation between OGTT 0 and 3-h glucose levels and concentrations of these molecules might not be considered as clinically significant. The decrease in the levels of methylated arginine derivatives that inhibit the uptake of arginine, such as SDMA and L-NMMA, can be considered as a dilution effect since the sudden increase in glucose values does not reflect exactly whether glucose’s endotoxic effects occur.
Akturk et al. analyzed plasma ADMA levels in 54 gestational diabetic subjects and 69 participiants with normal glucose tolerance (NGT) between 32 and 39 weeks. They reported the elevation of serum ADMA levels in GDM subjects compared to NGT controls (p=0.03). The ADMA concentrations in the third trimester were positively correlated with the glucose levels the 50-g glucose challenge test (GCT) during 24–28 weeks in the whole group (r=0.21, p=0.02) [20]. In our study, ADMA, SDMA and L-NMMA levels, which are antagonists of NO synthesis, were found to be significantly lower in cord blood of insulin- or diet-regulated gestational diabetic patients compared to control group. This can be explained by the fact that there is a decrease in the level of inhibitory molecules in the patient group regulated with insulin or diet. However, due to the low molecular stability and difficulty of measuring NO, NO levels could not be analyzed as a limitation of this study. The net effect of insulin or dietary therapy on NO production could be observed if NO levels were measured and could be assessed in all three groups.
Conclusion
According to this study’s results, methylated arginine levels may not be associated with endothelial deterioration in GDM otherwise with preeclampsia risk.
Acknowledgements
No funding from any pharmaceutical firm was received for this project, and the authors’ time on this project was supported by their respective employers.
Authors’ conflict of interest disclosure: The authors stated that there are no conflicts of interest regarding the publication of this article.
Employment or leadership: None declared.
Honorarium: None declared.
References
1. Stanley JL, Cheung CC, Rueda-Clausen CF, Sankaralingam S, Baker PN, Davidge ST. Effect of gestational diabetes on maternal artery function. Reprod Sci 2011;18:342–52.10.1177/1933719110393029Search in Google Scholar PubMed
2. Capobianco E, Martínez N, Fornes D, Higa R, Di Marco I, Basualdo MN, et al. PPAR activation as a regulator of lipid metabolism, nitric oxide production and lipid peroxidation in the placenta from type 2 diabetic patients. Mol Cell Endocrinol 2013;377:7–15.10.1016/j.mce.2013.06.027Search in Google Scholar PubMed
3. Brewster S, Zinman B, Retnakaran R, Floras JS. Cardiometabolic consequences of gestational dysglycemia. J Am Coll Cardiol 2013;62:677–84.10.1016/j.jacc.2013.01.080Search in Google Scholar PubMed
4. Guzmán-Gutiérrez E, Arroyo P, Salsoso R, Fuenzalida B, Sáez T, Leiva A, et al. Role of insulin and adenosine in the human placenta microvascular and macrovascular endothelial cell dysfunction in gestational diabetes mellitus. Microcirculation 2014;21:26–37.10.1111/micc.12077Search in Google Scholar PubMed
5. Mordwinkin NM, Ouzounian JG, Yedigarova L, Montoro MN, Louie SG, Rodgers KE. Alteration of endothelial function markers in women with gestational diabetes and their fetuses. J Matern Fetal Neonatal Med 2013;26:507–12.10.3109/14767058.2012.736564Search in Google Scholar PubMed PubMed Central
6. Sobrevia L, Abarzúa F, Nien JK, Salomón C, Westermeier F, Puebla C, et al. Differential placental macrovascular and microvascular endothelial dysfunction in gestational diabetes. Placenta 2011;32:159–64.10.1016/j.placenta.2010.12.011Search in Google Scholar PubMed
7. Brinkmann SJ, Wörner EA, Buijs N, Richir M, Cynober L, van Leeuwen PA, et al. The Arginine/ADMA ratio ıs related to the prevention of atherosclerotic plaques in hypercholesterolemic rabbits when giving a combined therapy with atorvastatine and arginine. Int J Mol Sci 2015;16:12230–42.10.3390/ijms160612230Search in Google Scholar PubMed PubMed Central
8. Di Gangi IM, Pirillo P, Carraro S, Gucciardi A, Naturale M, Baraldi E, et al. Online trapping and enrichment ultra performance liquid chromatography-tandem mass spectrometry method for sensitive measurement of “arginine-asymmetric dimethylarginine cycle” biomarkers in human exhaled breath condensate. Anal Chim Acta 2012;754:67–74.10.1016/j.aca.2012.09.032Search in Google Scholar PubMed
9. Fleszar MG, Wiśniewski J, Krzystek-Korpacka M, Misiak B, Frydecka D, Piechowicz J, et al. Quantitative analysis of l-arginine, dimethylated arginine derivatives, L-citrulline, and dimethylamine in human serum using liquid chromatography-mass spectrometric method. Chromatographia 2018;81:911–21.10.1007/s10337-018-3520-6Search in Google Scholar PubMed PubMed Central
10. International Association of Diabetes and Pregnancy Study Groups Consensus Panel, Metzger BE, Gabbe SG, Persson B, Buchanan TA, Catalano PA, et al. International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diab Care 2010;33:676–82.10.2337/dc10-0719Search in Google Scholar
11. Di Gangi IM, Chiandetti L, Gucciardi A, Moret V, Naturale M, Giordano G. Simultaneous quantitative determination of N(G),N(G)-dimethyl-L-arginine or asymmetric dimethylarginine and related pathway’s metabolites in biological fluids by ultrahigh-performance liquid chromatography/electrospray ionization-tandem mass spectrometry. Anal Chim Acta 2010;677:140–8.10.1016/j.aca.2010.08.011Search in Google Scholar PubMed
12. Vásquez G, Sanhueza F, Vásquez R, González M, San Martín R, Casanello P, et al. Role of adenosine transport in gestational diabetes-induced L-arginine transport and nitric oxide synthesis in human umbilical vein endothelium. J Physiol 2004;560(Pt 1): 111–22.10.1113/jphysiol.2004.068288Search in Google Scholar PubMed PubMed Central
13. Telejko B, Zonenberg A, Kuzmicki M, Modzelewska A, Niedziolko-Bagniuk K, Ponurkiewicz A, et al. Circulating asymmetric dimethylarginine, endothelin-1 and cell adhesion molecules in women with gestational diabetes. Acta Diabetol 2009;46:303–8.10.1007/s00592-008-0088-xSearch in Google Scholar PubMed
14. Mittermayer F, Mayer BX, Meyer A, Winzer C, Pacini G, WagnerOF, et al. Circulating concentrations of asymmetrical dimethyl-L-arginine are increased in women with previous gestational diabetes. Diabetologia 2002;45:1372–8.10.1007/s00125-002-0916-4Search in Google Scholar PubMed
15. Mittermayer F, Kautzky-Willer A, Winzer C, Krzyzanowska K, Prikoszovich T, Demehri S, et al. Elevated concentrations of asymmetric dimethylarginine are associated with deterioration of glucose tolerance in women with previous gestational diabetes mellitus. J Intern Med 2007;261:392–8.10.1111/j.1365-2796.2007.01772.xSearch in Google Scholar PubMed
16. Pettersson A, Hedner T, Milsom I. Increased circulating concentrations of asymmetric dimethyl arginine (ADMA), an endogenous inhibitor of nitric oxide synthesis, in preeclampsia. Acta Obstet Gynecol Scand 1998;77:808–13.10.1080/j.1600-0412.1998.770805.xSearch in Google Scholar
17. Pleiner J, Mittermayer F, Langenberger H, Winzer C, SchallerG, Pacini G, et al. Impaired vascular nitric oxide bioactivity in women with previous gestational diabetes. Wien Klin Wochenschr 2007;119:483–9.10.1007/s00508-007-0838-8Search in Google Scholar PubMed
18. Gumus II, Kargili A, Kaygusuz I, Derbent A, Karakurt F, KasapogluB, et al. The association between serum asymmetric dimethyl arginine levels and a history of gestational diabetes among healthy women. Blood Coagul Fibrinolysis 2012;23: 391–5.10.1097/MBC.0b013e3283468accSearch in Google Scholar PubMed
19. Sertkaya AC, Kafkasli A, Turkcuoglu I, Karabulut AB. Asymmetric dimethylarginine level in hyperglycemic gestation. Endocrine 2011;40:237–42.10.1007/s12020-011-9461-6Search in Google Scholar PubMed
20. Akturk M, Altinova A, Mert I, Dincel A, Sargin A, Buyukkagnici U, et al. Asymmetric dimethylarginine concentrations are elevated in women with gestational diabetes. Endocrine. 2010;38: 134–41.10.1007/s12020-010-9361-1Search in Google Scholar PubMed
©2019 Walter de Gruyter GmbH, Berlin/Boston
Articles in the same Issue
- Frontmatter
- Review Article
- Measurement uncertainty in laboratory medicine: the bridge between medical and industrial metrology
- Short Communication
- Investigation of beta globin gene mutations in Syrian refugee patients with thalassemia major
- Research Articles
- A practical ID-LC-MS/MS method for the most commonly analyzed steroid hormones in clinical laboratories
- Distribution of drug-metabolizing enzymes coding genes CYP2D6, CYP3A4, CYP3A5 alleles in a group of healthy Turkish population
- Molecular detection of Bacillus anthracis: evaluation of the efficiency of DNA extraction and a novel dry PCR
- Serum and cord blood-methylated arginine levels in gestational diabetic subjects
- Association of oxidative stress marker ischemia modified albumin and polycystic ovary syndrome in adolescent and young girls
- Influence of pegylated interferon and ribavirin on insulin resistance and metabolic factors in chronic hepatitis C
- Importance of biochemical parameters in order to predict clinical severity in patients diagnosed with Crimean-Congo haemorrhagic fever
- Evaluation of plasma VEGF and sVEGFR-1 levels in patients with diabetes mellitus receiving insulin treatment
- The effect of Ramadan fasting on renal functions in patients with chronic kidney disease
- Effect of food azo-dye tartrazine on physiological functions of pancreas and glucose homeostasis
- Ameliorating oxidative stress and inflammation by Hesperidin and vitamin E in doxorubicin induced cardiomyopathy
- Alteration in cholinesterases, γ-aminobutyric acid and serotonin level with respect to thiamine deficiency in Swiss mice
- Case Report
- Discordant troponin I value in a young woman: a case report with review of literature
- Letter to the editor
- Vitamin D test results in a public hospital in mid-January
Articles in the same Issue
- Frontmatter
- Review Article
- Measurement uncertainty in laboratory medicine: the bridge between medical and industrial metrology
- Short Communication
- Investigation of beta globin gene mutations in Syrian refugee patients with thalassemia major
- Research Articles
- A practical ID-LC-MS/MS method for the most commonly analyzed steroid hormones in clinical laboratories
- Distribution of drug-metabolizing enzymes coding genes CYP2D6, CYP3A4, CYP3A5 alleles in a group of healthy Turkish population
- Molecular detection of Bacillus anthracis: evaluation of the efficiency of DNA extraction and a novel dry PCR
- Serum and cord blood-methylated arginine levels in gestational diabetic subjects
- Association of oxidative stress marker ischemia modified albumin and polycystic ovary syndrome in adolescent and young girls
- Influence of pegylated interferon and ribavirin on insulin resistance and metabolic factors in chronic hepatitis C
- Importance of biochemical parameters in order to predict clinical severity in patients diagnosed with Crimean-Congo haemorrhagic fever
- Evaluation of plasma VEGF and sVEGFR-1 levels in patients with diabetes mellitus receiving insulin treatment
- The effect of Ramadan fasting on renal functions in patients with chronic kidney disease
- Effect of food azo-dye tartrazine on physiological functions of pancreas and glucose homeostasis
- Ameliorating oxidative stress and inflammation by Hesperidin and vitamin E in doxorubicin induced cardiomyopathy
- Alteration in cholinesterases, γ-aminobutyric acid and serotonin level with respect to thiamine deficiency in Swiss mice
- Case Report
- Discordant troponin I value in a young woman: a case report with review of literature
- Letter to the editor
- Vitamin D test results in a public hospital in mid-January

