Abstract
Background
Joint deformities in juvenile idiopathic arthritis (JIA) are most common in children, are not defined in term of angular measurements. The study was aimed to evaluate the joint deformities in angular deviation of the afected joints in JIA patients.
Methods
This cross-sectional study was conducted at Pediatric Rheumatology Clinic, North Bengal Medical College, West Bengal. The children aged 2–16 years diagnosed with JIA according to the International League of Associations for Rheumatology (ILAR) criteria were included in the study. Patients with co-morbid disease, hemodynamic instability, and other acute conditions were excluded. Angular measurements were performed using goniometer.
Results
The mean age of children was (8.05 ± 3.20) years of which 57.5% was male and the disease duration associated with the deformities in JIA. The prevalent subtypes of JIA were Oligoarticular JIA (oligoJIA)(40%), followed by polyarticular JIA (pJIA) (35%) and systemic-onset JIA (sJIA) (12.5%). The commonly involved joint were knee (40%), followed by small joint of hand (32.5%), ankle (30%), wrist and foot (17.5% each), elbow (12.5%) and cervical joint (7.5%). In pJIA, duration of disease significantly (P = 0.017) associated with the number of affected joints. Mostly, wrist, knee and ankle deformities were observed in oligoJIA, pJIA and sJIA. The angular deviation (mean ± SD) of right and left knee were (2° ± 4.16°) and (1.87° ± 5.12°) in oligoJIA, (13.36° ± 17.03°) and (12.5° ± 15.08°) in pJIA and (3° ± 6.71°) and (2.4° ± 5.37°) in sJIA. Right ankle angular deviation were (2.62° ± 5.06), (5.43° ± 8.21°) and 4° ± 8.94° respectively in oligoJIA, pJIA and sJIA. The angular deviation of right and left wrist were (1.25° ± 3.41°) and (0.94° ± 3.75°) in oligoJIA, (4.07° ± 8.93°) and (4.14° ± 9.36°) in pJIA and (2.45° ± 5.37°) and (2° ± 4.47°) in sJIA.
Conclusion
This study is the first study from India to quantify the angular deviation of deformed joints in JIA. Angular deviation could serve as a valuable parameter for monitoring disease progression across various JIA subtypes.
Introduction
Juvenile idiopathic arthritis (JIA) is a chronic autoimmune disease that affects the children.[1] The prevalence of JIA varies widely across different populations. Globally, the prevalence of JIA has been reported to range from 7 to 401 cases per 100, 000 children. In India, the prevalence of JIA is lower than the global average, with an estimated rate of 48 cases per 100, 000 children.[2] In JIA, common skeletal abnormalities include joint deformity, discrepancy in limb length, valgus deformity of the knees and delay in growth, micrognathia, retrognathia, facial asymmetry, malocclusion (if temporomandibular joint involvement).[3,4] Decreased joint motion in inflamed joints can leads to deformities like Boutonniere deformity, swan neck deformity, Z-deformities of thumb, spindling of fingers, subluxations, deviations, fixed flexion deformities, valgus and varus deformities in various joints.[2,5,6] A few studies were performed on radiographic images of afected joints to monitor the JIA.[7,8] However, joint involvement is classically described to define deformities in available literature, it has not defined with exact angular measurement in degree. There is a clear lack of studies regarding specific measurement of joint movement in JIA patients. Hence, the present study was designed to add a new measurable parameter for monitoring disease which may be useful for clinical practice. In this context, the angular deviation of joints was evaluated in various sub-categories of JIA using a goniometer.
Materials and Methods
Study Design
This cross-sectional study was conducted on JIA patients who visited the Pediatric Rheumatology Clinic and Physical Medicine Department at North Bengal Medical College in West Bengal, India.
Patient Recruitment
A total of 40 children aged 2–16 years were recruited in the study both from indoor and outdoor of Pediatric Rheumatology Clinic and Physical medicine. Children with comorbid diseases, hemodynamic instability, congenital musculoskeletal anomalies, or joint deformities caused by other factors were excluded from the study. Newly diagnosed JIA patients were classified according to the International League of Associations for Rheumatology (ILAR) criteria. Patients were treated using standard monitoring and treatment approaches.
Data Collection
Institutional ethical clearance (IEC/NBMC/2018–19/40) and consent from parents/caregivers/Legal guardians were taken prior to the study. Clinical details and exact angular measurement of affected joints were measured in degree using a Goniometer (Therapy-plusTM 824, India) and recorded on predesigned proforma. Angle deviations were measured by goniometer with a range of 1º to180º. Detailed joint angle assessments were conducted as follows: Patients were positioned supine with their head and eyes directed upwards, upper limbs at their sides with elbows extended and palms facing upwards, hips and knees extended, and feet perpendicular to the horizontal plane. In this position, joint angles were measured with a goniometer placed laterally to the joints. The data was collected from May 2019 to April 2020.
Statistical Analysis
Descriptive analysis was done in the form of proportion for categorical variables, mean or median for continuous variables. Data were checked for normality using tests for normality. Nonparametric tests were performed for variables that were not normally distributed. Differences between proportions were analyzed using the Chi-square test, and Spearman’s rank correlation coefficient (rho) was used to assess the correlation between variables. A P-value of less than 0.05 was considered statistically significant. All the data were analyzed using the SPSS (IBM Corp., Armonk, N.Y., USA) version 20.
Results
A total of 63 patients were screened and 40 patients with JIA were recruited for the assessment of joint deformities. The demographic data of the patients depicted in Table 1. The average age of the patients was 8.05 ± 3.2 years, of which majority was within the age group of 5–10 years (67.5%) followed by 11–15 years (15%) and < 5 years (12.5 %). JIA was more prevalent in males (57.5%) than females. The patients (57.5%) were diagnosed with JIA within 12 months of disease onset, 37.5% within 12–36 months, and 5% diagnosed more than 36 months after disease onset. The median (IQR) duration of disease was 6 months. Joint deformities were found in 72.5% patients, while 27.5% of were reported no deformities. The most prevalent subtype of JIA in the present study was Oligoarticular JIA (oligoJIA) (40%), followed by Polyarticular JIA (pJIA)(35%) and systemic-onset JIA (sJIA)(12.5%). The angular deviation of the other JIA subtypes were measured but not presented in the result. Most commonly involved joints were knee (40%), followed by small joint of hand (32.5%), ankle (30%), wrist and foot (17.5% each), elbow (12.5%) and cervical joint (7.5%)(Figure 1). Majority of the patients had oligoJIA (40%), followed by pJIA (35%) and sJIA (12.5%). Maximum involvement of joints was observed in pJIA and had a positive correlation (Spearman’s coefficient of rank correlation [rho]= 0.623, P = 0.017) with duration of the disease (Figure 2). Commonly, knee, right ankle and wrist deformities were observed in oligoJIA, pJIA and sJIA. The angular measurements and of different joint and their prevalence are depicted in Table 2. The angular deviation of right and left knee were 2° ± 4.16° and 1.87° ± 5.12° in oligoJIA, 13.36° ± 17.03° and 12.5° ± 15.08° in pJIA and 3° ± 6.71° and 2.4° ± 5.37° in sJIA. The prevalence of deformities of right and left knee were 25% and 18.75% in oligoJIA, 57.14% and 64.29% in pJIA and 20% in both joints of sJIA. Right ankle angular deviations in oligoJIA, pJIA, and sJIA were found to be 2.62° ± 5.06°, 5.43° ± 8.21°, and 4° ± 8.94°, respectively, with a prevalence of 25%, 42.86%, and 20%. Left ankle angular deviation were observed only in oligoJIA, pJIA, with deviation of 0.94° ± 2.72°and 5.29° ± 8.26°, respectively and a prevalence of 12.5% and 35.71%. The angular deviation of right and left wrist were 1.25° ± 3.41° and 0.94° ± 3.75° in oligo-JIA, 4.07° ± 8.93° and 4.14° ± 9.36°in pJIA and 2.45° ± 5.37° and 2° ± 4.47° in sJIA. The prevalence of right and left wrist angular deviation was 12.5% and 6.25% in oligoJIA, 21.43% in both wrists of pJIA, and 20% in both wrists of sJIA. Elbow, metatarsophalangeal (MTP), and proximal interphalangeal (PIP) joints were deviated only in oligoJIA and pJIA. In oligo-JIA, the angular deviations of the right and left elbows were 0.094° ± 2.72° and 5.00° ± 2.00°, respectively, with a prevalence of 12.5% and 6.25%. In pJIA, the angular deviations of the right and left elbows were 7.14° ± 13.26° and 5.64° ± 9.92°, respectively, with a prevalence of 28.57% in both. The angular deviations of the right and left MTP joints were 0.94° ± 3.75° and 0.62° ± 2.50° in oligoJIA, and 2.50° ± 1.00° and 2.43° ± 4.85° in pJIA, respectively. The angular deviations of the right and left foot PIP joints were 2.81° ± 11.25° and 2.5° ± 10° in oligoJIA, and 6.21° ± 11.53° and 6.07° ± 10.69° in pJIA, respectively. Angular deviations of the right and left hand PIP and distal interphalangeal (DIP) joints were observed only in pJIA. However, only right hand PIP joint deviation was noted in sJIA.
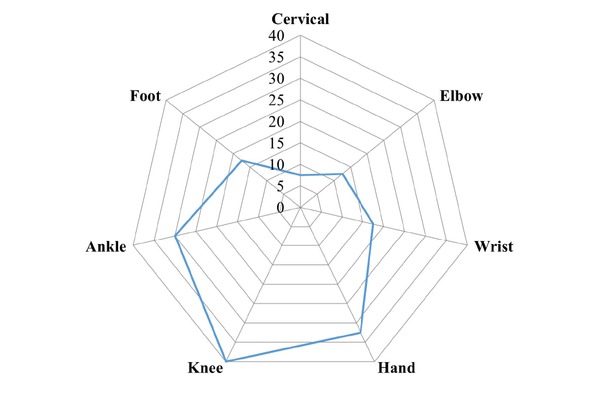
Distribution joint involvement of study subjects in juvenile idiopathic arthritis (JIA).
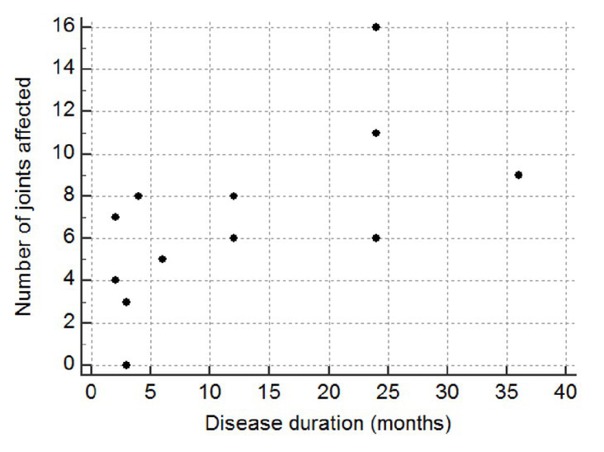
Spearman’s coefficient of rank correlation between disease duration and no. of joints affected in pJIA. Association was statistically significant where Spearman’s coefficient of rank correlation (rho) is 0.623, P = 0.017.
Demographic data of the patients with JIA
| Age | Frequency | Percent (%) |
|---|---|---|
| <5 years | 05 | 12.5 |
| 5-10 years | 27 | 67.5 |
| 11-15 years | 06 | 15 |
| >15 years | 02 | 05 |
| Sex | ||
| Male | 23 | 57.5 |
| Female | 17 | 42.5 |
| Duration of JIA | ||
| <12 months | 23 | 57.5 |
| 12-36 months | 15 | 37.5 |
| >36 months | 02 | 05 |
| Any deformity | ||
| Absent | 11 | 27.5 |
| Present | 29 | 72.5 |
| JIA categories | ||
| pJIA | 14 | 35 |
| oJIA | 16 | 40 |
| SoJIA | 05 | 12.5 |
Angular deviation of the involved joints in degree
| Joints | Oligo JIA (n = 16) | Prevalence (%) | pJIA (n = 14) | Prevalence (%) | sJIA (n = 5) | Prevalence (%) |
|---|---|---|---|---|---|---|
| Knee Right | 2.00 ± 4.16 | 25 | 13.36 ± 17.03 | 57.14 | 3 ± 6.71 | 20 |
| Knee Left | 1.87 ± 5.12 | 18.75 | 12.5 ± 15.08 | 64.29 | 2.4 ± 5.37 | 20 |
| Ankle Right | 2.62 ± 5.06 | 25 | 5.43 ± 8.21 | 42.86 | 4.00 ± 8.94 | 20 |
| Ankle Left | 0.94 ± 2.72 | 12.5 | 5.29 ± 8.26 | 35.71 | 0 | 0 |
| Wrist Right | 1.25 ± 3.41 | 12.5 | 4.07 ± 8.93 | 21.43 | 2.4 ± 5.37 | 20 |
| Wrist Left | 0.94 ± 3.75 | 6.25 | 4.14 ± 9.36 | 21.43 | 2 ± 4.47 | 20 |
| Elbow Right | 0.094 ± 2.72 | 12.5 | 7.14 ± 13.26 | 28.57 | 0 | 0 |
| Elbow Left | 5.00 ± 2.00 | 6.25 | 5.64 ± 9.92 | 28.57 | 0 | 0 |
| MTP Right | 0.94 ± 3.75 | 6.25 | 2.50 ± 1.00 | 21.43 | 0 | 0 |
| MTP Left | 0.62 ± 2.50 | 6.25 | 2.43 ± 4.85 | 21.43 | 0 | 0 |
| Foot PIP joint Right | 2.81 ± 11.25 | 6.25 | 6.21 ± 11.53 | 35.71 | 0 | 0 |
| Foot PIP joint Left | 2.5 ± 10.00 | 6.25 | 6.07 ± 10.69 | 35.71 | 0 | 0 |
| Hand PIP joint Right | 0 | 0 | 16.93 ± 16.19 | 78.57 | 8 ± 10.95 | 40 |
| Hand PIP joint Left | 0 | 0 | 17.5 ± 18.53 | 78.57 | 8 ± 10.95 | 40 |
| Hand DIP joint Right | 0 | 0 | 1.79 ± 3.72 | 21.43 | 0 | 0 |
| Hand DIP joint Left | 0 | 0 | 1.79 ± 3.60 | 21.43 | 0 |
The data of angular deviation was represented as Mean ± SD. Involvement of joints in oJIA, pJIA, sJIA only represented. MTP: Metatarsophalangeal joints, PIP: Proximal interphalangeal, DIP: Distal interphalangeal.
Discussion
JIA is a multifactorial inflammatory disease and heterogeneous group of disorders. It is characterized by arthritis of unknown etiology that manifests before the age of 16 years, and persists for at least six weeks, and causes long-term morbidity.[9,10] Several factors, including the disease severity, genetic and environmental factors, and comorbidities play an important role in the treatment of JIA. Potential outcomes are remission, persistent joint involvement, joint damage and deformity, functional limitations and overall quality of life even with treatment.[11,12] Despite awareness and various modern treatments including biologics, about 50% of children suffer from JIA. It can cause joint deformities and limited joint movements, leading to limitation in daily activities and social participation in their adulthood.[13] Present study, showed that males outnumbered the females. Previous studies from the European and Latin American populations have shown that JIA is more prevalent in females.[10] Previous studies, have reported the mean age at onset ranged between 4.1 and 10.3 years. A previous study from India reported that JIA was common from the age of 12 years onwards. In present study, the average age was (8.05 ± 3.2) years, which was lower than reported in the previous Indian study.
In the present study it was found that the most commonly involved joints were knee (40%), followed by hand (32.5%), ankle (30%), wrist & foot (17.5% each), elbow (12.5%) and cervical joint (7.5%). These findings are consistent with those of Sen et al. and Menon et al., who reported that knees and ankles were the most commonly affected joints.[10,14] Although Naz S et al. reported that the hand and wrist joint were most commonly involved in their study, the present study found higher involvement of small joints of hand (32.5%), particularly in the pJIA categories.[6] In this category hand PIP joint involvement is most common (78.57%) followed by knee joint (64.29%).[14–16] Previously, a study on 105 patients found that articular damage was present in 48.6%, and extra-articular damage was 21.9% in children.[3]
Maximum joint involvement with deformities were observed in pJIA and had a positive correlation with the duration of disease.[17,18] Previously, it was reported that pJIA is an aggressive and erosive subtype that inhibits the growth of the affected joints and can lead to growth retardation.[9,19] However, there is no standardized method to quantify joint deformities using angular deviation. In the present study, knee was most affected major joint, particularly the left knee. The angular deviation (13.36° ± 17.03°) of the left knee was higher than the right knee (13.36° ± 17.03°), with a predominance of 64% and 57% respectively, in pJIA. Apart from major joints, right and left hand PIP were severally affected with a deviation of 16.93° ± 16.19° and 17.5° ± 18.53° respectively, and prevalence of 78.57%. In pJIA, monitoring angular deviation of the knee and hand PIP joints may be useful for monitoring the treatment response. In previous studies, it was observed that oligoJIA occurs in between 24%–60% of JIA patients. In the study, oligoJIA was observed as 40% and angular deviation of major and minor joints were less than pJIA. The children suffering from oligoJIA were more likely to respond to treatment than those with pJIA which may be co-related with lower angular deviation of the joints. The presentation of sJIA are variable compared to other JIA subtypes, with extra-articular features include fever, hepatosplenomegaly, rash and lymphadenopathy being more prominent than joint involvement.[20,21] In this study, 8.9% of patients were diagnosed with sJIA. The results was higher than those reported in India (8%) and South Africa (7.7%).[22] In this study, joint involvement and angular deviations (in degrees) were observed in the knee, right ankle, and hand PIP joints. These measurements can aid in monitoring and treatment progress in sJIA. Other potential confounding factors that could influence angular deviation and the improvement of angular deviation after treatment of JIA were not addressed in this study and should be considered in future research.
Conclusion
JIA is associated with single or multiple deformities in around 70% of patients, and disease duration is significantly associated with the presence of deformity and the number of joints in pJIA. In connection, the angular deviation of major and minor joints was higher in pJIA, followed by oligoJIA and sJIA, compared to other subtypes. This is the first study from India to understand the angular deviation in degree in deformed joints in JIAs. The angular deviation may be a parameters that can be used to monitor disease progression of various JIA subtypes.
Funding statement: None.
Acknowledgements
Authors acknowledge Multi-disciplinary Research Unit, Medical College and Hospital, Kolkata a scheme of Department of Health Research, Govt. of India for the support in this research.
-
Author contributions
All authors contributed to the study conception and design. Material method preparation, data collection was performed by S. Banerjee, D. Dutta and P.P. Pan. The data analysis was performed by A. Adak, S Banerjee, A Hazra and D. Dutta. The first draft of the manuscript was written by A. Adak. The manuscript was checked by M. Nandy, A. Hazra, R.K. Mondal and all authors commented on the final draft of the manuscript and approved the final manuscript. The research work was performed under the supervision of R.K. Mondal.
-
Informed consent
Written informed consent were taken from parents/caregivers/Legal guardians prior to the study.
-
Ethical approval
Ethical Committee of North Bengal Medical College, West Bengal, India approved the study with an approval no (IEC/NBMC/2018–19/40).
-
Conflict of interest
The authors declare no competing interest.
-
Data availability statement
No additional data is available.
-
Use of large language models, AI and machine learning tools
None declared.
References
[1] Abujam B, Mishra R, Aggarwal A. Prevalence of musculoskel-etal complaints and juvenile idiopathic arthritis in children from a developing country: a school-based study. Int J Rheum Dis. 2014;17:256–260.10.1111/1756-185X.12276Suche in Google Scholar PubMed
[2] Agarwal M, Freychet C, Jain S, et al. Factors impacting referral of JIA patients to a tertiary level pediatric rheumatology center in North India: a retrospective cohort study. Pediatr Rheumatol Online J. 2020;18:21.10.1186/s12969-020-0408-4Suche in Google Scholar PubMed PubMed Central
[3] Sidhique R, Bagri NK, Jana M, et al. Disease Damage in Juvenile Idiopathic Arthritis. Indian J Pediatr. Published online August 30, 2024.10.1007/s12098-024-05239-2Suche in Google Scholar PubMed
[4] Tangcheewinsirikul S, Sukharomana M, Charuvanij S. Disability and disease-related damage in Thai children and adolescents with juvenile idiopathic arthritis. Pediatr Rheumatol Online J. 2023;21:68.10.1186/s12969-023-00852-5Suche in Google Scholar PubMed PubMed Central
[5] Oen K, Malleson PN, Cabral DA, et al. Disease course and outcome of juvenile rheumatoid arthritis in a multicenter cohort. J Rheumatol. 2002;29:1989-1999.Suche in Google Scholar
[6] Naz S, Asif M, Naz F, et al. Spectrum of Joint Deformities in Children with Juvenile Idiopathic Arthritis. J Coll Physicians Surg Pak. 2018;28:470–473.10.29271/jcpsp.2018.06.470Suche in Google Scholar PubMed
[7] Augdal TA, Angenete OW, Shi X-Q, Säll M, Fischer JM, Nordal E, et al. Cone beam computed tomography in the assessment of TMJ deformity in children with JIA: repeatability of a novel scoring system. BMC Oral Health. 2023;23:12.10.1186/s12903-022-02701-5Suche in Google Scholar PubMed PubMed Central
[8] Ključevšek D, Potočnik Tumpaj V, Gazikalović A. The role of radiography in diagnosing, monitoring and prognosing juvenile idiopathic arthritis. Pediatr Radiol. 2024;54:481–489.10.1007/s00247-023-05742-2Suche in Google Scholar PubMed
[9] Zak M, Pedersen FK. Juvenile chronic arthritis into adulthood: a long-term follow-up study. Rheumatology (Oxford). 2000;39:198–204.10.1093/rheumatology/39.2.198Suche in Google Scholar PubMed
[10] Şen V, Ece A, Uluca Ü, et al. Evaluation of children with juvenile idiopathic arthritis in southeastern Turkey: a single center experience. Hippokratia. 2015;19:63-68.Suche in Google Scholar
[11] Bansal N, Pasricha C, Kumari P, et al. A comprehensive overview of juvenile idiopathic arthritis: From pathophysiology to management. Autoimmun Rev. 2023;22:103337.10.1016/j.autrev.2023.103337Suche in Google Scholar PubMed
[12] La Bella S, Rinaldi M, Di Ludovico A, et al. Genetic Background and Molecular Mechanisms of Juvenile Idiopathic Arthritis. Int J Mol Sci. 2023;24:1846.10.3390/ijms24031846Suche in Google Scholar PubMed PubMed Central
[13] Sarma PK, Misra R, Aggarwal A. Physical disability, articular, and extra-articular damage in patients with juvenile idiopathic arthritis. Clin Rheumatol. 2008;27:1261–1265.10.1007/s10067-008-0901-5Suche in Google Scholar PubMed
[14] Menon NVB, Peethambaran G, Puthiyapurayil AT, et al. Clinical profile and juvenile arthritis damage index in children with juvenile idiopathic arthritis: A study from a tertiary care center in south India. Int J Rheum Dis. 2018;21:871–879.10.1111/1756-185X.12886Suche in Google Scholar PubMed
[15] Farr S, Girsch W. The Hand and Wrist in Juvenile Rheumatoid Arthritis. J Hand Surg Am. 2015;40:2289–2292.10.1016/j.jhsa.2015.06.111Suche in Google Scholar PubMed
[16] Horsten NC, Ursum J, Roorda LD, et al. Prevalence of hand symptoms, impairments and activity limitations in rheumatoid arthritis in relation to disease duration. J Rehabil Med. 2010;42:916–921.10.2340/16501977-0619Suche in Google Scholar PubMed
[17] Elhai M, Bazeli R, Freire V, et al. Radiological peripheral involvement in a cohort of patients with polyarticular juvenile idiopathic arthritis at adulthood. J Rheumatol. 2013;40:520–527.10.3899/jrheum.121013Suche in Google Scholar PubMed
[18] Thatayatikom A, Modica R, De Leucio A. Juvenile Idiopathic Arthritis. In: StatPearls. Treasure Island (FL): StatPearls Publishing; January 16, 2023.Suche in Google Scholar
[19] Mahmud SA, Binstadt BA. Autoantibodies in the Pathogenesis, Diagnosis, and Prognosis of Juvenile Idiopathic Arthritis. Front Immunol. 2019;9:3168.10.3389/fimmu.2018.03168Suche in Google Scholar PubMed PubMed Central
[20] Foradori D, Rocha MEM. Arthritis Associated with Systemic Disease. Caring for the Hospitalized Child: A Handbook of Inpatient Pediatrics (3rd Edition), Edited by Gershel JC, Rauch DA, American Academy of Pediatrics, 2023: 56.10.1542/9781610026338-56Suche in Google Scholar
[21] Shenoi S, Horneff G, Aggarwal A, et al. Treatment of non-systemic juvenile idiopathic arthritis. Nat Rev Rheumatol. 2024;20:170–181.10.1038/s41584-024-01079-8Suche in Google Scholar PubMed
[22] Sabounji MM, Lissimo H, Deme A. Childhood-onset rheumatoid arthritis at a tertiary hospital in Senegal, West Africa. Pediatr Rheumatol Online J. 2023;21:98.10.1186/s12969-023-00889-6Suche in Google Scholar PubMed PubMed Central
© 2025 Sudip Banerjee, Atanu Adak, Debadyuti Dutta, Partha Pratim Pan, Manab Nandy, Avijit Hazra, Rakesh K Mondal, published by De Gruyter on behalf of NCRC-DID
This work is licensed under the Creative Commons Attribution 4.0 International License.
Artikel in diesem Heft
- Original Article
- Angular assessment of joints in juvenile idiopathic arthritis
- Circ_0088200 acts as a sponge for miR-127-5p to promote the migration and invasion of rheumatoid arthritis fibroblast-like synoviocytes
- Insights into familial Mediterranean fever: Chronic disease correlations with arthralgia and current health status of patients with familial Mediterranean fever in Jordan
- Nitazoxanide alleviates CFA-induced rheumatoid arthritis in Wistar rats by modulating the STAT-3 and NF-κB pathways
- The causal relationship between obstructive sleep apnea and rheumatic disease: A bidirectional Mendelian randomization study
- Efficacy and safety of 2% isosorbide cream in systemic sclerosis patients with digital ulcers and Raynaud’s phenomenon
- Letter to the Editor
- Insights into the clinical and immunological significance of anti-α-fodrin antibodies in systemic lupus erythematosus
- Images
- Antiphospholipid antibody-associated cystic lesion of the pancreatic head with concurrent acute pancreatitis
Artikel in diesem Heft
- Original Article
- Angular assessment of joints in juvenile idiopathic arthritis
- Circ_0088200 acts as a sponge for miR-127-5p to promote the migration and invasion of rheumatoid arthritis fibroblast-like synoviocytes
- Insights into familial Mediterranean fever: Chronic disease correlations with arthralgia and current health status of patients with familial Mediterranean fever in Jordan
- Nitazoxanide alleviates CFA-induced rheumatoid arthritis in Wistar rats by modulating the STAT-3 and NF-κB pathways
- The causal relationship between obstructive sleep apnea and rheumatic disease: A bidirectional Mendelian randomization study
- Efficacy and safety of 2% isosorbide cream in systemic sclerosis patients with digital ulcers and Raynaud’s phenomenon
- Letter to the Editor
- Insights into the clinical and immunological significance of anti-α-fodrin antibodies in systemic lupus erythematosus
- Images
- Antiphospholipid antibody-associated cystic lesion of the pancreatic head with concurrent acute pancreatitis

