Abstract
Introduction
Childhood exposure to lead has severe health consequences including long-term physical, behavioral, and learning problems. Lead poisoning often occurs in the home and persists as a form of environmental injustice, disparately impacting certain children based on factors such as socioeconomic status, immigration status, and race. Because abatement is costly, many prevention programs rely on educational interventions. We conducted a systematic review to assess the effectiveness of educational interventions on reducing blood lead levels (BLL) in children.
Content
Following PRISMA-P guidelines, a librarian-guided search strategy incorporated database-specific subject headings and keywords related to lead poisoning and education, and encompassed four databases: Ovid MEDLINE, Scopus, Web of Science Core Collection and CINAHL. Two reviewers screened the results for those that met inclusion criteria (original research, study population of children under 18 years, inclusion of an educational intervention, outcome of BLL).
Summary and Outlook
We screened the titles of 2,062 non-duplicate studies, the abstracts of 78 studies, and full texts of 23 articles, resulting in 17 articles that met eligibility criteria. Thirteen studies used multi-pronged interventions, which precluded comprehensive assessment of the effectiveness of the educational component. Interventions that had success in lowering BLL included some notable elements: longevity of intervention, consideration of culture and ethnicity; use of a community or home-based approach; and provision of supplies or assistance with cleaning. Of the four of studies that used solely educational interventions, three were successful in reducing BLL. Among the 12 studies that used a control group, six found their interventions to be successful in reducing BLL. This review found that educational interventions, either alone or as part of a multi-pronged approach, do not consistently reduce BLL in children. However, educational interventions may decrease severity of lead poisoning in children when more robust interventions are not feasible.
Introduction
Lead is a heavy metal that has been used in a variety of industries, commonly used for waterworks and pipes, solders, pottery glazes, paints, battery casings, bullets, and more [1]. Despite its utility, lead is a known environmental toxin, exposure to which results in negative health consequences . While adults and children alike are vulnerable to the negative impacts of lead, children are especially vulnerable [5]. Due to behavioral factors, such as frequent hand-to-mouth movements or mouthing, children are more likely to ingest lead dust, chew on toys prepared with lead paint, or eat paint chips from deteriorating surfaces. Additionally, biological factors also put children at an increased risk. Children absorb a greater amount of lead once ingested than adults [6]. Once in the bloodstream, children are at higher risk of poor neurological outcomes when compared to adults, due to the still developing blood brain barrier and central nervous system [7].
Most human lead exposure occurs through ingestion or inhalation of lead dust or material containing lead [8], 9]. Common ways that children are exposed to lead is through lead-containing paint (particularly mouthing a painted surface, ingestion of chipping paint, or exposure to contaminated dust from deteriorating paint), through consuming contaminated water, and through lead deposited in the soil or environment, such as through the use of leaded gasoline [2], 10], 11].
Lead exposures can have serious consequences, ranging from abdominal pain and fatigue to kidney and brain damage [2], 3], 12], 13]. In very severe cases high level exposures can lead to death [4], 14], 15]. Even low level exposures in children can damage the brain and nervous system, slow growth and delay development, cause speech and hearing problems, and result in behavioral and learning problems [3], 16], 17].
In recent decades, the dramatic decrease in levels of lead poisoning in the United States has been notable, some considering it one of the top 10 modern public health achievements [18], 19]. Despite this, the number of children who continue to be poisoned by lead and is unacceptable. Some reports indicate that globally, one third of all children may have elevated blood lead levels (BLL)s [2], 20], 21]. As reported by the World Health Organization, lead exposure may account for 1.06 million deaths and 24.4 million years of healthy life lost worldwide and may account for over 60 % of the global burden of idiopathic developmental intellectual disability [2]. Prevalence of elevated BLL is not equal among all groups, with research demonstrating disparities based on race [22], 23], poverty [23], 24], immigration or refugee status [25], residing in racially segregated neighborhoods, or in neighborhoods with lower socioeconomic status [26].
Historically, it is evident that removing sources of exposure will lead to dramatic declines in incidence of lead poisoning. In 1973 the Environmental Protection Agency required that tetraethyllead be phased out from gasoline [27] and was ultimately banned in 1990 through the Clean Air Act amendments, with full effectiveness in 1996 [28]. During the phase-out of lead from gasoline from 1976 to 1991, the overall estimated geometric mean BLL of the US population aged 1–74 years decreased 78 %, from 12.8 to 2.8 μg/dL; much of this dramatic decrease is believed to be due to the banning of lead in gasoline as well as removal of lead soldering from food-containing cans [29].
The removal of the source of exposure is an extremely effective means of primary prevention. Unfortunately, the most common sources of exposure for children are not easily removed. Layers of leaded paint has been spread through millions [30] of homes, and is costly [7], difficult, and potentially dangerous [31] to abate. Lead laterals bringing contaminated water to houses are costly to update. Mass abatement of lead paint or updating of antiquated plumbing infrastructure would require large financial commitments from federal, state, or city governments, grant-providing institutions, property owners, and the public. As the United States has not yet been able to coordinate the effort or funds to do so (despite intentions to accelerate some lead hazard removal efforts) [32] many public health efforts to prevent lead poisoning lean heavily on smaller-scale education and health promotion efforts.
Efforts to reduce lead poisoning often incorporate education into their intervention, sometimes combined with testing or assistance in abating or cleaning the source of exposure. Educational programs typically address parents’ knowledge and awareness of concepts related to sources of exposure, hygiene measures, and cleaning techniques to prevent exposure to lead contaminated soil, dust, and paint [33]. While such efforts are important and should continue [34], it is critical that public health professionals understand the value and limitations of such measures, elements that influence their effectiveness, and how they are best utilized. With this goal in mind, we conducted a systematic review of the literature surrounding the effectiveness of educational interventions in reducing BLL in children.
Methods
Literature search
This review followed the Preferred Reporting Items for Systematic review and Meta-Analysis Protocols (PRISMA-P) guidelines [35], a set of evidence-based standards for reporting systematic reviews. A search strategy was created in partnership with a medical librarian, incorporating database specific subject headings and keywords related to the topics of lead poisoning and education. Search terms related to lead included “lead”, “blood lead level”, and the elemental form of lead, “Pb”. Search terms related to education included: “health education”, “promotion”, and “health fair”. Searches were conducted in June of 2021 on four databases: Ovid MEDLINE, Scopus, Web of Science Core Collection, and CINAHL (EBSCO). Search results were updated November 2023 to incorporate results from the most recent two years, at that time one additional article met criteria for inclusion. See Appendix A for full search strategy.
Article selection process
Duplicates were removed and search results were exported to a web-based application for systematic reviews, Rayyan [36]. Two independent reviewers (JSB, JCB) screened the results, iteratively applying a systematic PICOS criterion [37] for inclusion/exclusion:
| P (Population) | Children <18, and parents/caregivers (any country, only articles in English). |
| I (Intervention) | Individual or community level education-based interventions for primary or secondary prevention of lead poisoning in children. Target of the intervention could be children directly, or parents/guardians/caregivers of children. |
| C (Comparison) | Between an intervention/non-intervention group, or same population pre/post intervention. |
| O (Outcome) | Childhood BLL. |
| S (Study Design) | Original research, observational or experimental. |
Eligibility criteria
Studies were included if they were an experimental or quasi-experimental design. Studies were included if they described an educational intervention, even if education was just one component of a multi-arm intervention. Studies were excluded if they were not original research, such as systematic reviews. Studies were excluded if they did not describe an educational intervention aimed at reducing or preventing lead poisoning in children. Finally, studies were excluded if the outcome was not BLL in children.
Results
For the original search, a total of 2,769 references resulted, and 1,624 remained after eliminating duplicates. During the title screening phase 1,562 studies were excluded, and 62 remained. During the abstract screening phase, 40 studies were excluded, and 22 studies remained for complete review of methods section/full text. Upon screening the full text, nine additional studies that did not meet eligibility criteria were excluded. Three studies were identified and included from the references of included articles that had been screened out in the title-screening round but met the PICOS criteria for inclusion, resulting in a total of 16 articles originally included in this review. For the November 2023 update, an additional 438 titles were screened, 16 abstracts reviewed, and one full text reviewed and included, resulting in 17 included studies (Figure 1 this figure reflects the combined results from the original search and the update). The results are summarized in Table 1.
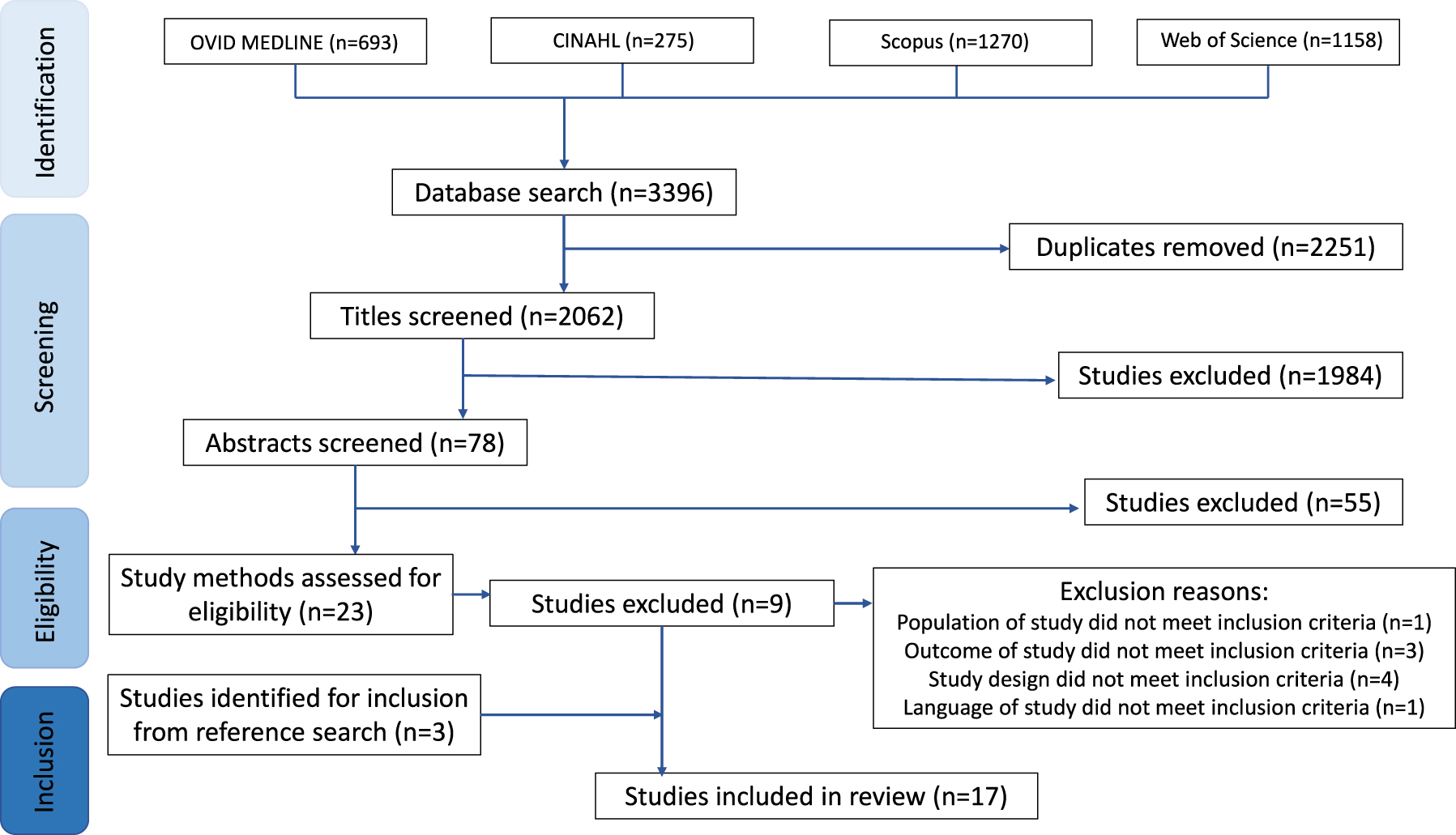
Flowchart describing results from article screening process.
Results.
| Article | Design | Population | Intervention | Educational intervention | Results | Conclusions |
|---|---|---|---|---|---|---|
| A randomized, community-based trial of home visiting to reduce blood lead levels in children [38], 2006 Brown, M. J., McLaine, P., Dixon, S., Simon, P. |
Randomized controlled | Children <28 months, identified by the RI department of health to have a BLL of 15–19 μg/dL who spoke English or Spanish (n=175) (92 intervention 83 control) | Educational interventions + additional interventions (dust/soil assessment, parent-child interaction and nutrition assessment, exposure assessment, individualized care plan) | Educational component included ‘comprehensive education’ and home visiting. An individualized care plan directed parent teaching by nurses and other services. Education was individualized to address specific risk factors, and was provided to families in five home visits. A control group received ‘customary care’, which consisted of 1–2 visits and environmental testing at end of study only |
Outcomes measured: dust lead levels, parent/child interactions, BLL.
Parents in the intervention group (n=92) decreased dust lead levels and significantly improved ‘parent-child interaction’ and family housekeeping practices when compared with the comparison group (n=83). BLLs declined 47 %, however the difference in BLL by group was not significant: 9 μg/dL for intervention group vs. 8.3 μg/dL for comparison group. After one year, almost half of enrolled children had BLLs ≥10 μg/dL. |
This study concluded that the education intervention of providing families with information may have a role in short-term efforts, especially in the absence of lead-safe house. Their overall findings suggest that this type of intervention has little benefit once BLLs are elevated. |
| Reducing lead exposure in children in Broken Hill [52], 2003 Burke, H., Balding, B., Lyle, D. |
Single cohort (pre/post comparison) | All children in Broken Hill (high-lead exposure area in Australia), specifically reinforced for children <5 years with high BLL (n=7,885 surveyed between 1991 and 2001 with estimated response rate between 41 and 75 %) | Educational interventions + additional interventions (monitoring and case finding; case management; public education and health promotion; remediation of public land; evaluation, research, and development) | The ‘lead management program’ was promoted through the media, with curriculum-based education in schools, and training for groups such as the local council, the water authority, nurseries, and businesses such as hardware stores. No control group identified. |
Outcomes measured: BLL
Results of this study found that the standardized mean BLL decreased from 16.7 μg/dL in 1991 to 7.0 μg/dL in 2002. |
BLLs dropped during the intervention, however, the multi-component makes it difficult to understand of the impact of the educational component specifically, and lack of a comparison group precludes understanding how much of the decrease in BLL can be attributed to the intervention vs. natural decline. |
| Primary prevention of lead exposure: the Philadelphia Lead safe homes Study [39], 2011 Campbell et al. |
Randomized controlled | Families of newborns recruited from outpatient practices in low-income neighborhoods in Philadelphia (n=314,110 completed study) | Educational interventions + additional interventions (parental education, home evaluation, lead remediation, parents given cleaning materials and supplies, specific cleaning instructions given, exposure assessment) | The Philadelphia Lead safe homes (LSH) study used parent education, home evaluation, and lead remediation for urban families with newborns. Two comparison groups: (1) standard: received lead-poisoning prevention education, and (2) maintenance: Received standard education + extensive education related to practices for maintaining a lead-safe property. | Outcomes measured: Visual environmental inspection, dust level, parental score on lead knowledge, BLL screening rate, BLL. This study found positive results in residential environmental conditions- in combined intervention groups, results positive for lead via visual inspections declined over 13 months from 97.0 to 90.6 %, p=0.007. At baseline, 36.9 % of homes exceeded the EPA’s lead dust standard, compared with 26.9 % at 12 months (p=0.032), with the primary improvement in window dust. Both parental groups had a significant score increase on a lead education test. Geometric mean BLLS in the intervention group (2.6 μg/dL) and control group (2.7 μg/dL), p=0.477 were similar. Mean BLLs at one year were not statistically different. | Education did significantly increase lead knowledge, but the study did not find that parental knowledge had an impact on child BLLs at one year of age. |
| Primary prevention of lead exposure--blood lead results at age two years [40], 2012 Campbell et al. |
Randomized controlled | Families of newborns recruited from outpatient practices in low-income neighborhoods in Philadelphia (n=314) (follow up from above) | Educational interventions + additional interventions (parental education, home evaluation, lead remediation, parents given cleaning materials and supplies, specific cleaning instructions given, exposure assessment) | The Philadelphia Lead safe homes (LSH) study offered parent education, home evaluation, and lead remediation to urban families with newborns. Two comparison groups: (1) standard: received lead-poisoning prevention education, and (2) maintenance: Received standard education + extensive education related to practices for maintaining a lead-safe property. This was a follow up study. | Outcomes measured: BLL (2 year follow up). Geometric mean BLLs between groups were 3.7 μg/dL vs. 3.5 μg/dL (p=0.4). The percentage of the cohort group with a BLLs ≥20 were 0.06 % and the controls 1.2 %. The percentage of the cohort group with BLL ≥10 was 5 and 6.6 % in the control. The percentage of the cohort group with BLL ≥5 μg/dL was 40 and 25 % in the control. The differences in these percentages were not statistically significant. | While the interventions did increase some aspects of parental knowledge of lead poisoning prevention and decreased dust levels in homes, it did not result in a significant decrease in BLLs. |
| Effect of interventions on children’s blood lead levels [53], 1998 Hilts, et al. |
Single cohort (pre/post comparison) | Children in trail, Canada, (which has been the site of an active lead/zinc smelter) (n=unspecified) | Educational interventions + additional interventions: screening, case management (in home education, testing, exposure reduction, testing, provision of supplies, assistance with paint abatement), dust abatement, environmental monitoring. | Messaging on decreasing lead exposure was given to children using puppets, a model house, demonstrations and schools/daycares. Messaging included hygiene, nutrition, and safe places to play. Educational messages were offered at fall screening on hygiene, nutrition, minimizing house dust. Nurses included education in well-baby visits. Lead exposure reduction messages were also distributed to the public through newsletters, local print, radio, billboards, and more. |
Outcomes measured: BLL. One-year follow-up of children whose families received the intervention of in-home educational visits and assistance with home-based dust control, found that these interventions resulted in average BLL changes of +0.5 to −4.0 μg/dL, with statistically significant declines in three out of five years. |
The authors reported that there did not appear to be an increase in the rate of BLL decline following the interventions. However, because there was no improvement in environmental conditions during the same time, they believe it’s possible that the decrease in BLL could be in part due to the implementation of their interventions. |
| A randomized trial of education to prevent lead burden in children at high risk for lead exposure: efficacy as measured by blood lead monitoring [45], 2003 Jordan, et al. |
Randomized controlled | Mothers and children 0–36 months of age in neighborhood with high risk for lead exposure in Minneapolis, MN (n=594 mothers, and their children) | Educational interventions only | Intervention and control groups both received brochures on basic lead prevention strategies, intervention group “were offered 20 bi-weekly educational sessions by same-ethnicity peer educators over the course of one year, and quarterly booster sessions for two years afterward. The intervention group’s educational curriculum included information on lead sources (e.g., paint, dust, water, soil, and risks from home repairs and remodeling), health consequences of lead burden, and strategies to reduce lead exposure, including household cleaning, hygiene, safe use of water, and nutritional recommendations.” | Outcomes measured: BLL. Results showed that of the 378 children with sufficient data for analysis, 23 % had BLL>10 μg/dL before three years of age. Intervention participants (81 %) were more likely to maintain BLL<10 μg/dL than were controls (73 %) p=0.08. Multivariate analyses found that the intervention reduced the risk of BLL>10 μg/dL by ∼34 %. | The authors concluded that while the educational intervention resulted in a decrease of children with elevated BLL, education alone is not enough for lead poisoning prevention. |
| Assessment of a lead management program for inner-city children [46], 2000 Kassa, H., Bisesi, M. S., Khuder, S. A., Park, P. C. |
Retrospective cohort (pre-post) | Children from low-income families residing in pre-1950s homes in Toledo, OH |
Educational interventions+ additional interventions. Environmental lead investigation was conducted with XRF, and paint and soil lead were abated following HUD guidelines. Children with BLL>45 μg/dL (and some with BLL>35 μg/dL) received chelation. |
Health care workers performed a single home visit to homes of children with BLL>10 μg/dL. Literature and instruction on prevention lead exposure was provided, focusing on hand washing, removal of peeling paint, and cleaning dust. |
Outcomes measured: BLL.
Children who received chelation therapy had a significantly (p<0.001) lower mean BLL when compared to pre-chelation, although it remained elevated. Children who did not receive chelation had a significantly (p<0.001) higher mean BLL than they did at the initial screenings. Children who did and did not receive chelation therapy continued to occupy lead-contaminated homes during the study. |
The authors concluded that chelation and education (a single health visit) do not consistently sufficiently lower BLL if there is a continuing exposure. They recommend parents receive frequent and comprehensive lead education, but conclude that residing in a lead-free home is the most effective way to control exposure to lead. |
| A randomized trial of the effect of dust control on children’s blood lead levels [42], 1996 Lanphear, et al. |
Randomized controlled | Children aged 12–31 months in Rochester, NY (n=104) | Educational interventions + additional interventions. Cleaning supplies distributed, information about commonly contaminated areas for cleaning, and a cleaning demonstration. | The intervention group received education about cleaning (particularly areas that are commonly sources of lead exposure) a demonstration, and were even provided with cleaning supplies. The control group was provided with an educational brochure on lead poisoning. |
Outcome measures: Dust lead level and BLL. Median BLL of children in the study was 6.7 μg/dL. No significant differences in BLLs or dust levels were found by group. Median decrease of BLL for children in the study group was −0.05 μg/dL, and −0.60 μg/dL for children in the control. |
The authors concluded that their findings imply that an educational and providing cleaning supplies and is not effective at reducing BLL in children with low/mild elevations after seven months. |
| Community health services and blood lead reduction in children, 2022 [54] Morales, et al. |
Single cohort interventional (pre-post comparison) | Preschool and school-age children in the “mi Peru” district of Peru (within the Callao region sources such as a smelter that can contaminate are and soil) with a BLL≥10 μg/dL (n=187 with 30 excluded for ‘noncompliance’) |
Educational interventions + additional interventions.
Intervention was described as ‘community health services’ with three components: comprehensive multidisciplinary care (medicine, nursing, nutrition, and psychology), health education, and house calls. |
Phase 1: Children in the study area were admitted for evaluation. Phase 2: Children received follow over the course of a year. Those with BLL>10 had labs every six months and those >20 had labs every three months, they received usual care as well as specialist evaluation. Phase 3: Children received comprehensive care from health professionals (including medicine, nutrition, psychology, nursing, social work) which included supplementation with calcium gluconate + vitamin D3. Parents received health education about risks of exposure, hygiene, cleanliness, and demonstration sessions on nutrition. Families received a home visit to reinforce counseling and deliver supplements. |
Outcomes measured: BLL
Mean BLL was 13.96 μg/dL at the start of the intervention and 8.96 μg/dL at the end of the intervention (p<0.001). At the start of the intervention 88.5 % (139) had ‘category II’ BLLs (10–19.99 μg/dL), and 11.5 % (18) had ‘category III’ BLLs (20–44.99 μg/dL). At the end of the intervention, 66.9 % (105) had BLL<10, 29.9 % (47) were category II, and 3.2 % (5) category III. |
The positive outcomes found in this study lead suggest that education with community health services may be effective in reducing BLL in children. However, the authors note that it is impossible to say which component of the study is the driver of this change, if all children received the same quality of care and education, or if pressure exerted by local authority may have reduced local lead emissions and therefore exposure. |
| A community-based intervention for low-income families to reduce children’s blood lead levels between 3 and 9.9 μg/dL [47], 2018 Nicholson, J. |
Randomized controlled | Children <6 years old from low-income families, with BLLs: 3–9.9 μg/dL, from a medium-sized midwestern city (n=84) | Educational interventions+ additional interventions. Intervention used environmental and educational components. | Participating families were put in one of eight different groups. All groups received an educational EPA brochure on lead exposure and how to reduce lead in homes; this was the only intervention provided to the control group. The intervention group received: a cleaning kit, (including a Riccar radiance HEPA vacuum with verbal/written instructions on how to clean), or a home inspection and consultation which outlined risks present and how to control them, or a combination of both the home assessment and the cleaning. | Outcomes measured: Lead knowledge, BLL. All groups showed a significant decrease in BLLs and increase in lead knowledge, but no main effects by group. Results suggest that all intervention groups reduced children’s BLLs. The authors report that this decrease can’t be definitively attributed to the intervention itself and could be inline with natural reduction trends. When compared to a passive control group post hoc, all intervention groups then had significant BLL reduction. | The authors concluded that educational, in combination with assistance from a health professional to help understand the content and respond to questions should be investigated further as a potential technique for prevention of lead poisoning. |
| The effect of dust lead control on blood lead in toddlers: A randomized Trial [43], 1999 Rhoads, et al. |
Randomized controlled “Field" trial | Urban children between the ages of 6 and 36 months in Jersey city, NJ (n=113) | Educational interventions + additional interventions. Education and biweekly assistance with household cleaning | Families assigned to the intervention group were asked to participate in a cleaning program in which two study staff trained in appropriate cleaning methods visited every two weeks to clean up potentially lead-contaminated dust, for ∼2 h/session. A control group received an “accident prevention” intervention. Both the intervention and control groups were invited to attend 4–5 educational sessions with information on lead and how to limit a child’s exposure. Flip charts were used in both groups, the lead group received a special educational card game in for last year. |
Outcomes measured: dust lead level, BLL. Among those in the intervention group, BLL fell by 17 % while it did not change among controls. Household dust/dust lead also fell in the intervention group. Children in homes cleaned ≥20 times had a 34 % average BLL decrease. There was a significant increase in knowledge in the intervention group as a whole, when compared to the baseline scores or the control group. The authors did not find a relationship between baseline maternal score on a lead knowledge test and the child’s initial BLL, nor with any change in BLL. Number of educational sessions attended was also not related to decline in BLL. |
The authors concluded that regular cleaning combined with education is a safe and somewhat effective intervention for children for whom are not able to relocate to a lead-safe location. |
| A community-developed, community-based lead poisoning prevention program: Lead awareness North Philly Style [41], 1999 Rothman, N. L., Lourie, R., Gaughan, J., White, N. |
Census tract based-cohort, prospective | The target population is an underserved, African American population in North Central Philadelphia at risk due to environmental lead. | Educational interventions + additional interventions. Cleaning supplies and lead testing swabs were provided to participants. | Educational program for children, educational programs for adults implemented at “block parties”. Census tracts that received the intervention were compared with census tracts that did not receive the intervention. |
Outcome measures: Knowledge of lead poisoning, surveillance, BLL
The study reports that 45 % of the children in the control and 57 % in the experimental group had BLLs ≥10 μg/dL at baseline. They reported that post intervention (one year) that 42 % of the control group and 46 % tested ≥10 μg/dL, representing a 3 % decline in the control areas and 9 % decline in the intervention areas. |
The authors concluded that this was a successful community intervention. They conclude that community-based prevention/intervention strategies ‘imposed by outsiders’ do not work, but are successful when developed ‘by and for the community’. |
| Primary prevention of childhood lead poisoning through community outreach [49], 2001 Schlenker, T. L. et al. |
Geographic cohort | Children 6–71 months of age with elevated BLL from 10 to 19 μg/dL, in a Milwaukee neighborhood with older housing stock (n=1850) | Educational interventions + additional interventions. Home visits, environmental assessments, demonstration of cleaning were also performed. | Bilingual outreach workers from the community were trained on blood draws and lead risk assessment. During home visits, capillary BLL samples were drawn, environmental assessments were performed, lead education provided and repair/cleaning of lead hazards demonstrated. This study used a comparison group comprised of BLL data for the entire city. |
Outcomes measured: environmental scores, screening rates, BLL. For children with BLLs 10–19 μg/dL enrolled in the community lead outreach program (CLOP) mean BLL was 12.9 μg/dL and showed a decline of 3.1 μg/dL or 24 % during the intervention. At the first follow-up, 97 % were <20 μg/dL while 76 % were <10 μg/dL. At the second follow-up, 100 % were <20 μg/dL. Odds ratios showed the target population of the intervention had a decrease in rate of elevated BLL 1.6 times that of the city-wide average (p=0.016). |
The authors concluded that the intervention successfully intervened to reduce BLLs of children who had been missed in traditional screening programs. They concluded that this program demonstrated how community outreach workers can access high-risk populations and reduce lead exposure. They suggest that this strategy may be useful in other geographic areas, to patients of private physicians, and for addressing other health problems. |
| Prevention of lead paint poisoning among Baltimore children. A hard-sell program [44], 1965 Schucker, G. W., Vail, E. H., Kelley, E. B., Kaplan, E. |
Cohort | Directed to parents and others responsible for the care of children under four years of age living in selected census tracts of the city where a high potential existed for lead paint poisoning, in Baltimore, MD (n=1,517 families) | Educational only | Painted surfaces that were accessible to children were inspected alongside the caregivers, instruction on lead paint poisoning was provided. A brochure on lead poisoning was discussed and left with the caregiver. A total of five visits were made every six months, and six letters were sent in between the visits. |
Outcomes measured: BLL.
During the three year intervention, the annual rate of elevated BLL among children <4 years of age was 4.5 per 1,000 in the intervention area and 5.4 per 1,000 in the control. In the previous three-years, the rate was 7.4 per 1,000 in the intervention area and 10.4 per 1,000 in the control. No significant reduction in lead poisoning in the action area was demonstrated against the control tracts. |
The authors concluded that high mobility among residents created instability, with only one-third of families remaining in their residence for the entire intervention- decreasing the opportunity for continued/repetitive outreach. They conclude educational interventions would have the most effect if held large-scale, where a mobile population would not be lost due to participants moving within the area. |
| A retrospective examination of in-home educational visits to reduce childhood lead levels [48], 1999 Schultz, B., Pawel, D., murphy, A |
Retro-spective cohorts- paper does not specify that they were randomly assigned. | Children who had elevated BLLs between 20 and 24 μg/dL in Milwaukee, WI (n=413 in experimental and reference group) | Educational only | The study group received an hour-long in-home educational visit by a health department paraprofessional, focused on the importance of reducing lead exposure, nutrition, and dust clean-up, and behavioral changes. Outreach workers described sources, why lead a problem, the health impacts, personal hygiene factors, and cleaning procedures. Pictures were used. Potential sources of lead were discussed, at times with a walk-through of the home with the caregiver to highlight specific sources. Importance of diet was discussed, examples and pictures given. A control group received no intervention. |
Outcomes measured: BLL.
Post-intervention, average BLL declined by 4.2 μg/dL (21 %). Average BLLs in the control group (no home visit) declined by 1.2 μg/dL (6 %). The intervention group had a decline in BLLs 3.1 μg/dL (15 %) greater than the reference group, p<0.001. |
The authors suggest that the BLL decline in the reference group may be partially due to education at the clinics while taking blood samples. The authors conclude that in-home education for families may be an effective component of interventions to decrease lead poisoning. |
| Effectiveness of cleaning and health education in reducing childhood lead poisoning among children residing near superfund sites in Missouri [51], 2004 Sterling, D. A. et al. |
Randomized controlled | Children between the ages of 6 and 72 months with a BLL between 10 and 20, in two former lead mining areas in Missouri (n=134) | Educational + additional interventions. There were multiple comparison groups, one group also received professional cleaning services. | Participants were randomized to receive “standard care” or one of two intervention groups: tailored newsletters only or tailored newsletters and specialized cleaning. The “standard care” group received one health education session on lead exposure reduction by a nurse educator; a letter reporting the results of the environmental lead assessment of the home; and generic educational information in the form of pamphlets. The ‘tailored newsletters only’ group received everything that the standard care group received + quarterly visits by a public health nurse educator and six tailored newsletters. The tailored newsletters and specialized cleaning group received everything that the tailored newsletters only group received + quarterly house cleaning by trained cleaners. | The authors found that BLLs declined during the intervention with an average decrease of 1.54 μg/dL (12.1 %), p< 0.001. However, no statistically significant differences were found between the different study groups. ∼40 % of children in all three groups who originally had BLLs>10 μg/dL reduced to <10 μg/dL. |
The authors found that tailored newsletters and specialized cleaning resulted in the greatest decline in BLLs, but no statistical differences were found among the study groups. |
| Management of children with slightly elevated blood lead levels [50], 1994 Kimbrough, R. D., LeVois, M., Webb, D. R.a |
Single cohort (pre-post comparison) | Families in Illinois, in the vicinity of a former lead smelter (n=827 volunteers, 490 children <6 years) | Educational only | Home visits and counseling of parents of children on lead exposure prevention and behavioral factors. Specific risks discussed. Topics included hygiene, housekeeping, paint removal, nutrition. Literature was provided. |
Outcomes measured: BLL. In children with initial BLL of ≥10 μg/dL, the BLL test was repeated four months later. The arithmetic mean BLL at four months decreased from 15 to 7.8 μg/dL. The lack of comparison group made it difficult to attribute the change to the educational intervention. An additional follow-up blood sample was taken at one year in a subset of children (n=30). These children had a mean BLL of 9 μg/dL at the one-year follow-up, although their mean BLL at four months had been 8 μg/dL. |
The authors reported that parental education was an effective tool, but that further studies are needed with larger populations to evaluate further. |
-
Abbreviation key: BLL, Blood lead level; CLOP, Community Lead Outreach Program; EPA, United States Environmental Protection Agency; HUD, Office of Housing and Urban Development; LSH, Lead Safe Homes; MD, Maryland; MN, Minnesota; NJ, New Jersey; NY, New York; RI, Rhode Island; WI, Wisconsin; XRF, X-ray flourescense.
Demographics
Most of the articles (12/17) studied children residing in the United States. Seven of the studies were based in the east/northeast areas of the country: Brown et al. looked at a sample of 175 children <28 months of age in Rhode Island [38]. Two studies (and a follow-up) were based in Philadephphia, PA: Campbell’s original and follow-up study looked at a sample of 314 newborns, and the Rothman et al. study of an underserved African-American population [39], [40], [41]. Lanphear et al. analyzed a group of 104 families with children aged 12–31 months in Rochester, NY [42]. Rhoads et al. studied a sample of 113 children from Jersey City, NJ [43]. The study by Schucker et al. of children <4 years old took place in Baltimore, MD [44].
Five studies were conducted in the midwest: The Jordan et al. study looked at a sample of mothers with children aged 0–36 months in Minneapolis, MN [45]. Kassa et al. looked at a sample of children in Toledo, OH [46]. The Nicholson study looked at a group of 84 children from low income families from a “medium-sized midwestern city” [47]. Two studies took place in Milwaukee, WI: The Schlenker et al. study of 1850 children aged 6 months–6 years, and the Schultz et al. study of 413 children [48], 49]. The Kimbrough et al. study took place in Illinois in the vicinity of a former lead smelting site [50].
Only one study was conducted in the southern region of the United States: the study by Sterling et al. of 134 children aged 6–72 months took place in two counties in Missouri, both former lead mining areas [51]. No studies or samples from the western region United States were represented.
Three studies were conducted outside of the United States. The study by Burke et al. surveyed 7,885 children (with estimated response rate between 41 and 75 %) living in a former lead mining/high exposure area took place in Broken Hill, Australia [52]. The Hilts et al. study took place in Trail, Canada-also a site of an active lead/zinc smelter and high risk area [53]. The study by Morales et al. took place in the Callao region of Peru, and area also prone to contamination by local smelters [54].
In four of the studies, children were at environmental risk of lead exposure due to being located at sites or former sites of lead mining/smelting or other industries [50], [52], [53], [54].
Study design
Eight of the studies (including a follow-up study) compared their intervention group to a control group using a randomized controlled design. Brown et al. compared their study group with a group who received customary care (provided standard health education about lead poisoning with less visits and customization than intervention group) [38]. Sterling et al. compared their intervention group to a group receiving “standard” care which was comprised of one health education session on lead exposure reduction activities, given by a nurse educator; a letter reporting the results of the environmental lead assessment of the home; and generic educational information in the form of pamphlets produced by state and federal agencies [51]. In their study and follow up analysis, Campbell et al. compared their intervention group against a control group that also received standard lead education in their original and follow-up study [39], 40]. Jordan et al., Lanphear et al., and Nicholson compared their intervention group to a control group who received a brochure on basic lead prevention [42], 45], 47]. Rhoads et al. compared their intervention group to control group that received an ‘accident prevention’ intervention, which notably did include some lead education [43].
Four used prospective or retrospective cohort-style designs to test their intervention. Rothman et al. compared census tracts in which people received the intervention to similar census tracts that did not receive the intervention [41]. Schlenker et al. compared their intervention group to a comparison group of BLL data for the city by zip code [49]. Schucker et al. compared tracts in Baltimore that received the intervention with control tracts [44]. The study by Schultz et al. compared their intervention group to a non-intervention control group retrospectively. The reference group presumably was comprised of children who like the experiemental group had BLLs between 20 and 24 μg/dL in the Milwaukee Health department records, but did not receive the educational intervention [48].
Five studies used a single cohort with a pre/post test to study their intervention: Burke et al., Hilts et al., Kassa et al., and Kimbrough et al., and Morales et al. [46], 50], [52], [53], [54].
Interventions
As it was the focus of this review, all studies included an educational component, with or without additional intervention components. Four studies used a solely educational intervention. Jordan et al. provided a brochure and offered bi-weekly educational sessions by same-ethnicity peer educators over a year, with quarterly booster sessions thereafter [45]. Their bi-weekly curriculum included education on lead sources, strategies to reduce exposure, and nutrition. The intervention in the study by Schucker et al. provided in-home education by same language community health workers, during which surfaces were inspected with an adult in charge of the children’s care present, information on the dangers of lead poisoning was presented to the same adult, a leaflet was left with the family. An additional five visits at six months intervals were held to remind parents of lead poisoning dangers, details not provided on if the educator provided personalized education [44]. The intervention described in the Schultz et al. study included an hour-long educational visit from a paraprofessional emphasizing lead exposure, nutrition, and cleaning practices and printed materials were left with the family [48]. The Kimbrough et al. study provided in-home counseling for families in 30–45 min sessions on sources of lead, hygiene, housekeeping, and nutrition, and written educational materials were provided [50]. Kimbrough et al. also provided some environmental testing at baseline, though it is unclear if families received these results during the intervention period.
The remaining studies used a variety of additional interventions, such as: dust/soil testing [38], 51], exposure assessments/home evaluations [[38], [39], [40, 46], 47], 49], case finding/monitoring [52], remediation of public land [52], lead or lead dust remediation [39], 40], 46], 53], case management [53], chelation therapy [46], distribution of nutritional supplementation [54], distribution of cleaning supplies [[39], [40], [41], [42, 47], 51], 53], cleaning demonstrations [42], 49], 51], assistance with household cleaning or cleaning services [43], 53], provision of testing swabs for community members to test their residences [41], and assessment of parent child-interaction assessment [38] or occupational or recreational exposures [38], [39], [40]. In some cases where testing of soil, surfaces, or home evaluations were performed, the line between educational/non-educational interventions were blurry. For this review, inspections that appeared more formal, such as if the family was provided specific testing results so they knew with some certainty if there were hazards in their home and what they were specifically, were considered to be beyond education. Inspections that seemed less formal, or did not provided specific results but seemed to be used to personalize education, were considered educational.
Findings
Overall, findings on the success of educational interventions to reduce BLL in children were mixed. Four of five studies that used a pre/post design reported improvements in BLL during the treatment/intervention period. Burke et al. reported a decrease in age-sex standardized mean BLL from 16.7 to 7.0 μg/dL during the treatment period from 1999 to 2002 [52]. Hilts et al. reported changes in BLL of +0.5 to −4.0 μg/dL of those who received specific interventions, with statistically significant BLL decreases in three years out of five-although it is unclear how much decline can be attributed to the intervention vs. the overall decrease seen in general population [53]. Kimbrough et al. reported that for those who had a BLL ≥10 μg/dL at the start of the intervention, the arithmetic mean BLL four months later decreased from 15 to 7.8 μg/dL (although an additional sample a year later was taken of a subset that showed the mean increased again to 9 μg/dL) [50]. The study by Kassa et al. used a pre-post design and found that among the children in their study who received chelation therapy, the post-chelation mean BLL (expectedly) was lower although it remained elevated. Among nonchelated study participants who received the educational visit, the mean BLL was actually higher than their original screen [46]. Morales et al. reported a decline in mean BLL from 13.96 to 8.96 μg/dL. While it is promising that an initial decrease in BLL was demonstrated in these studies, none of these studies utilized control groups, and so it is difficult to discern if the decrease in BLL is due to the intervention, the general decline in BLL that has happened over time, or some other outside influence.
Jordan et al., Nicholson, Rhoads et al., Rothman et al., Schlenker et al., and Schultz et al. reported a decrease in BLL in their treatment group when compared to a control group. Jordan et al. reported that intervention participants were more likely to maintain BLL<10 μg/dL than the control group (81 vs. 73 % p=0.08), with multivariate analysis indicating that the intervention reduced the risk of BLL>10 μg/dL by 34 % [45]. Nicholson did not find significant differences between the different interventions in their study, but when they compared their intervention groups with a post-hoc passive control, there was a statistically significant improvement in BLL in all intervention groups [47]. Rhoads et al. reported that BLL fell 17 % in the intervention group but did not change in the control group that was given education unrelated to lead [43]. Schlenker et al. reported that those in their intervention group demonstrated a decreased rate in elevated BLL 1.6 times that of the city-wide average (p=0.016) [49]. Schultz reported that their intervention group had a decline in BLL 3.1 (15 %) higher than the reference group (p=0.001) [48]. The study by Rothman et al. reported that one-year post intervention there was a 9 % decline in BLL≥10 μg/dL in the intervention group, and only a 3 % decline in the control group [41].
Not all studies found that their interventions were effective. The studies by Brown et al., Campbell et al., the Campbell et al. two-year follow up study, Lanphear et al., Schucker et al. and Sterling et al. reported that there was no significant difference in BLL reduction between control/intervention groups [38], [39], [40, 42], 44], 51].
Some studies reported additional outcomes that may be mediating factors to the final outcome of decreased BLL, such as increased knowledge or improved environmental screening results (such as reduced lead dust). These mediating outcomes are not discussed further as they are not the focus of the review, but those findings are noted in Table 1.
Discussion
Conclusions
Lead poisoning is a completely preventable condition with irreversible impacts on children who experience it. While this review demonstrated that there is a potential benefit to educational and combined interventions in the prevention of lead poisoning, mixed outcomes found in this review indicate that these interventions are not consistently effective at decreasing BLL in children. Interventions that had some measure of success in lowering BLL when compared against control groups included some notable elements: repeated or frequent educational visits, consideration of language, culture, ethnicity, and literacy, use of a community-based approach, home-based or individualized education, and provision of supplies or actual assistance with cleaning. While these are notable elements of the successful studies, one must also consider that some of these elements were also incorporated in the less-successful studies, making identification of the key drivers of success in these interventions difficult. Table 2 provides a brief summary of key components of interventions with results.
Key outcomes and components of interventions. a
| Design | Study | Intervention | Outcome | Key elements |
|---|---|---|---|---|
| Randomized controlled | Brown 2006 | Education + additional interventions | Reduction in BLL noted among intervention group but was not significant against control group. | Five visits In-home education Individualized Environmental assessment |
| Campbell 2011 | Education + additional interventions | BLLs between comparison group and control group were not statistically different at one year. | Three visits In-home education Environmental assessment Remediation Distribution of cleaning supplies |
|
| Campbell 2013 | Education + additional interventions | BLLs between comparison group and control group were not statistically different at two years. | Four visits In-home education Environmental assessment Remediation Distribution of cleaning supplies |
|
| Jordan 2003 | Educational interventions only | Intervention participants were more likely to maintain BLL<10 μg/dL than the control group. | Up to 20 sessions bi-weekly Quarterly booster sessions for two years In home Culture, language or ethnicity was considered |
|
| Lanphear 1996 | Education + additional interventions | There was no significant difference in the change of children’s blood lead levels or dust lead levels by treatment group. | Educational visit Distribution of cleaning supplies Environmental assessment Cleaning demonstration |
|
| Nicholson 2018 | Education + additional interventions | No significant differences in BLL were found between treatment arms, but against a post hoc passive control all groups demonstrated a significant reduction. | Written education Verbal education Distribution of cleaning supplies Environmental assessment |
|
| Rhoads 1999 | Education + additional interventions | BLL fell by 17 % in intervention group and did not change among controls. | Biweekly educational visits Biweekly assistance with cleaning |
|
| Sterling 2004 | Education + additional interventions | The overall decrease was 1.54 μg/dL (12.1 %) with p<0.001. But there were no statistically significant differences among the three intervention groups. | In-home education Tailored newsletters Written and verbal education Environmental assessment Quarterly visits Assistance cleaning |
|
| Cohorts | Rothman 1999 | Education + additional interventions | A 3 % decline in BLL was found in control areas and 9 % decline in intervention areas. | Community-based education Education for adults and children Distribution of cleaning supplies Distribution of lead testing swabs Particular consideration on community, intervention by peers |
| Schlenker 2001 | Education + additional interventions | Comparison of odds ratios showed the target population had a decrease in rate of elevated BLL 1.6 times that of the city-wide average, p=0.016, and more than double that of the patients of area private providers. | In-home education Environmental assessments Cleaning demonstration Consideration of language and culture |
|
| Schucker 1965 | Educational interventions only | Compared with the previous experience in the study and control tracts, no significant reduction in lead paint poisoning in the action area was demonstrated. | In-home education Environmental assessment Five visits at six-month intervals Reminder letters between visits Consideration and adjustment for literacy levels of population |
|
| Schultz 1999 | Educational interventions only | The study group had a decline in BLLs 3.1 μg/dL (15 %) greater than the reference group, p=0.001. | In-home education 1 h-long visit Written and verbal education Environmental assessment |
|
| Pre-post | Burke 2003 | Education + additional interventions | Demonstrated reduction in BLL, but the multi-component intervention and lack of comparison group precludes understand of impact of educational intervention. | Environmental remediation Public health education Community based training |
| Hilts 1998 | Education + additional interventions | Found changes between +0.5 and −4.0, which were statistically significant three of five years. Does not appear to have been an increase in the rate of decline in BLL following the interventions. | In-home Community education Exposure reduction measures Distribution of cleaning supplies Abatement assistance |
|
| Kassa 2000 | Education + additional interventions | Mean BLL was statistically lower for those who received chelation therapy, but higher for those who only received educational interventions. | Single educational visit Chelation therapy |
|
| Kimbrough 1994 | Educational interventions only | The mean BLL at four months showed a decrease from 15–7.8 μg/dL. An additional blood sample was taken one year later in a subset of 30 children. These children showed a mean BLL of 9 μg/dL at the one-year follow-up, whereas their mean BLL at the four-month follow-up had been 8 μg/dL. | In-home education | |
| Morales 2022 | Education + additional interventions | Mean BLL reduced from 13.96 to 8.96 μg/dL over the course of the intervention which appeared to last at least one year. | Health education One or two home visits Medical/nursing/social work evaluation Distribution of supplements Nutritional demonstration |
- a
There is a level of subjectivity when determining if an intervention was successful or not, given the differing interventions and study designs represented. In this table, green represents a study that was or claimed to be successful, yellow represents studies that were or claimed to have some level of success, and red indicates studies that did not seem or claim to have success in decreasing BLL..
Comparison of effectiveness of educational interventions among studies was difficult due to the inability to assess the quality of the educational intervention (aside from studies who described potentially quality-impacting factors such as length of session or consideration of language, culture, and literacy). For interventions that were not exclusively educational, it is difficult to differentiate the impact of the educational component vs. the other components. The study populations were also varied, with differing age groups and differing baseline BLLs and among the children and differing study locations perhaps impacting outcomes.
Among the studies included, even the process of determining if a study was “successful” was somewhat subjective. While four of five studies that uses a pre-post design successfully demonstrated a decrease in BLL, it is hard to determine how much of the success can be attributed to the study intervention or simply the declining trend in BLL over time [55], or some other factor, such as local policy that reduced lead emissions in the local area [54]. Perhaps the same intervention compared to a control group would not have yielded a difference in rate or level of BLL decline. Additionally, among the randomized controlled studies, for ethical reasons, the control group often included some form of lead education, although to a lesser extent than the experimental arms. While many did not find significant differences between study groups, perhaps they would have found a significant different when compared to a group that received no intervention at all, as was the case in Nicholson’s 2008 study [47].
Limitations of this study include the potential to inadvertently exclude relevant articles during the search or screening process. Authors writing on this topic who did not have positive results when studying an intervention may have had more difficulty publishing, and therefore skewed the overall results of our review. Additionally, the results of this review are impacted by the overall burden of limitations among the articles, including lack of control group, variations in interventions and intervention quality, lack of statistical analysis, and the inability to precisely define the impact of the intervention vs. other outside influences.
Implications
This review has found that educational interventions do not consistently reduce BLL in children. Even the most effective interventions evaluated in this review did not decrease childhood lead exposure to an acceptable level: none. Although some studies did show some level of success in decreasing BLL through educational or multi-pronged approaches, the results from this review do not show a definitive path to lead poisoning prevention or reduction through education. Despite this, some interventions did show some measures of success in reducing BLL in children, and should be used when more robust options are not possible.
The evidence supporting the use of educational interventions, or how such interventions could be designed to maximize impact is not well-established. Further research on how to design and implement educational and other interventions for effective reduction childhood lead poisoning is needed. Research that examines the most effective and efficient way to disseminate education may be useful, such as in-home education vs. training health care providers to educate within the clinical setting. Due to ethical challenges, conducting a definitive study on the effectiveness of educational interventions for lead poisoning reduction is challenging (if one were to ‘control’ for the amount of lead a child is exposed to determine if education is effective, the only ethical control is to eliminate all known sources lead for all children in all study groups). Future research on this issue must take these challenges into consideration when trying to find a rigorous yet ethical study design.
The studies included in the review spanned over five decades, from 1965, and yet a consistent, improved, or reliable educational intervention did not develop. While this may reflect lack of a coordinated approach to improving and standardizing tested educational interventions, it likely is a stronger reflection the urgency of the need for thorough remediation of lead hazards, rather than reliance on educational lead poisoning prevention interventions. Children, including a disproportionate number of children of color or children from lower socio-economic backgrounds, continue to be poisoned in their own homes through exposure to lead. This poisoning and its lifelong impacts are completely preventable. Although prevention efforts such as full remediation come at a cost, it is imperative that they come. Policies and funding to support abatement of lead hazards are needed to fully remove this scourge from the environment and the bodies of children.
Acknowledgments
The authors would like to thank Liz Schulster, MLIS and Ori O’Malley, MLIS for their assistance in designing the search strategy and conducing the original search and performing the updated search, respectively.
-
Research ethics: Not applicable.
-
Informed consent: Not applicable.
-
Author contributions: The authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Competing interests: None declared.
-
Research funding: None declared.
-
Data availability: Not applicable.
References
1. The Royal Society of Chemistry. Lead: uses and properties [Internet]. Available from: https://www.rsc.org/periodic-table/element/82/lead. [cited 2021 Jun 26].Search in Google Scholar
2. World Health Organization. Lead poisoning and health [Internet]; 2019. Available from: https://www.who.int/news-room/fact-sheets/detail/lead-poisoning-and-health. [cited 1 Jul 2021].Search in Google Scholar
3. Centers for Disease Control and Prevention. Childhood lead poisoning prevention. Health effects of lead exposure. Available from: https://www.cdc.gov/nceh/lead/prevention/health-effects.htm. [cited 27 Jun 2021].Search in Google Scholar
4. The National Institute for Occupational Safety and Health. Centers for Disease Control and Prevention. Lead Information for Workers. Available from: https://www.cdc.gov/niosh/topics/lead/workerinfo.html.Search in Google Scholar
5. Bellinger, D. Lead. Pediatrics 2004;113:1016–22. https://doi.org/10.1542/peds.113.s3.1016.Search in Google Scholar
6. Heath, L, Soole, K, McLaughlin, M, McEwan, G, Edwards, J. Toxicity of environmental lead and the influence of intestinal absorption in children. Rev Environ Health 2003;18:231–50. https://doi.org/10.1515/reveh.2003.18.4.231.Search in Google Scholar PubMed
7. Needleman, H. Lead poisoning. Annu Rev Med 2004;55:209–22. https://doi.org/10.1146/annurev.med.55.091902.103653.Search in Google Scholar PubMed
8. Agency for Toxic Substances and Disease Registry. Centers for Disease Control. Environmental health and medicine education; 2019. Available from: https://www.atsdr.cdc.gov/csem/leadtoxicity/exposure_routes.html. [cited 27 Jun 2021].Search in Google Scholar
9. al osman, M, Yang, F, Massey, IY. Exposure routes and health effects of heavy metals on children. Biometals 2019;32:563–73. https://doi.org/10.1007/s10534-019-00193-5.Search in Google Scholar PubMed
10. Centers for Disease Control and Prevention. Sources of lead poisoning. Available from: https://www.cdc.gov/nceh/lead/prevention/sources.htm. [cited 2021 Jun 27].Search in Google Scholar
11. Kessel, I, O’Connor, J. Getting the lead out: the complete resource for preventing and coping with lead poisoning, Revised ed. Cambridge, MA: Perseus Publishing; 2001.Search in Google Scholar
12. Kopp, SJ, Barron, JT, Tow, JP. Cardiovascular actions of lead and relationship to hypertension: a review. Environ Health Perspect 1988;78:91–9.10.1289/ehp.887891Search in Google Scholar PubMed PubMed Central
13. Lilis, R, Gavrilescu, N, Nestorescu, B, Dumitriu, C, Roventa, A. Nephropathy in chronic lead poisoning. Occup Environ Med 1968;25:196–202. https://doi.org/10.1136/oem.25.3.196.Search in Google Scholar PubMed PubMed Central
14. Dooyema, CA, Neri, A, Lo, YC, Durant, J, Dargan, PI, Swarthout, T, et al.. Outbreak of fatal childhood lead poisoning related to artisanal gold mining in Northwestern Nigeria, 2010. Environ Health Perspect 2012;120:601–7. https://doi.org/10.1289/ehp.1103965.Search in Google Scholar PubMed PubMed Central
15. Kaufmann, RB, Staes, CJ, Matte, TD. Deaths related to lead poisoning in the United States, 1979–1998. Environ Res 2003;91:78–84. https://doi.org/10.1016/s0013-9351(02)00017-8.Search in Google Scholar PubMed
16. Evens, A, Hryhorczuk, D, Lanphear, BP, Rankin, KM, Lewis, DA, Forst, L, et al.. The impact of low-level lead toxicity on school performance among children in the Chicago Public Schools: a population-based retrospective cohort study. Environ Health 2015;14:21. https://doi.org/10.1186/s12940-015-0008-9.Search in Google Scholar PubMed PubMed Central
17. Vorvolakos, T, Arseniou, S, Samakouri, M. There is no safe threshold for lead exposure: a literature review. Psychiatriki 2016;27:204–14. https://doi.org/10.22365/jpsych.2016.273.204.Search in Google Scholar PubMed
18. United States Environmental Protection Agency. A public health approach to addressing lead. Available from: https://www.epa.gov/lead/public-health-approach-addressing-lead. [cited 27 Jun 2021].Search in Google Scholar
19. Centers for Disease Control and Prevention. Ten great public health achievements - United States, 2001–2010. Morb Mortal Wkly Rep 2011;60:619–23.Search in Google Scholar
20. Burki, T. Report says 815 million children have high blood lead levels. Lancet 2020:396:10248.10.1016/S0140-6736(20)31684-6Search in Google Scholar PubMed
21. Rees, N, Fuller, R. The toxic truth: children’s exposure to a lead pollution undermines a generation of future potential; 2020. Available from: https://www.unicef.org/media/73246/file/The-toxic-truth-children%E2%80%99s-exposure-to-lead-pollution-2020.pdf.Search in Google Scholar
22. White, BM, Bonilha, HS, Ellis, C. Racial/ethnic differences in childhood blood lead levels among children <72 months of age in the United States: a systematic review of the literature. J Racial Ethn Health Disparities 2016;3:145–53. https://doi.org/10.1007/s40615-015-0124-9.Search in Google Scholar PubMed
23. America’s Children and the Environment, 3rd ed. Washington, D.C: U.S. Environmental Protection Agency; 2013.Search in Google Scholar
24. Cureton, S. Environmental victims: environmental injustice issues that threaten the health of children living in poverty. Rev Environ Health 2011;26:141–7. https://doi.org/10.1515/reveh.2011.021.Search in Google Scholar PubMed
25. Balza, JS, Bikomeye, JC, Beyer, KMM, Rublee, C, Flynn, KE. Elevated blood lead levels of refugee children in the United States: a systematic review of recent literature (2011–2021). Rev Environ Health 2022;38:361–83. https://doi.org/10.1515/reveh-2022-0015.Search in Google Scholar PubMed
26. Moody, HA, Darden, JT, Pigozzi, BW. The relationship of neighborhood socioeconomic differences and racial residential segregation to childhood blood lead levels in metropolitan detroit. J Urban Health 2016;93:820–39. https://doi.org/10.1007/s11524-016-0071-8.Search in Google Scholar PubMed PubMed Central
27. US Environmental Protection Agency. EPA requires phase-out of lead in all grades of gasoline. EPA Press Release; 1973. Available from: https://www.epa.gov/archive/epa/aboutepa/epa-requires-phase-out-lead-all-grades-gasoline.html#:∼:text=On%20January%2010%2C%201973%2C%20EPA,control%20auto%20air%20pollution%20emissions.Search in Google Scholar
28. United States Environmental Protection Agency (EPA). The plain English guide to the clean air act; 2007. Available from: https://www.epa.gov/sites/default/files/2015-08/documents/peg.pdf.Search in Google Scholar
29. Pirkle, JL, Brody, DJ, Gunter, EW, Kramer, RA, Paschal, DC, Flegal, KM, et al.. The decline in blood lead levels in the United States. The National Health and Nutrition Examination Surveys (NHANES). JAMA 1994;272:284–91. https://doi.org/10.1001/jama.272.4.284.Search in Google Scholar
30. Woolf, AD, Goldman, R, Bellinger, DC. Update on the clinical management of childhood lead poisoning. Pediatr Clin North Am 2007;54:271–94. https://doi.org/10.1016/j.pcl.2007.01.008.Search in Google Scholar PubMed
31. Aschengrau, A, Beiser, A, Bellinger, D, Copenhafer, D, Weitzman, M. Residential lead-based-paint hazard remediation and soil lead abatement: their impact among children with mildly elevated blood lead levels. Am J Publ Health 1997;87:1698–702. https://doi.org/10.2105/ajph.87.10.1698.Search in Google Scholar PubMed PubMed Central
32. United States Environmental Protection Agency. Biden-Harris administration announces new get the lead out initiative to accelerate removal of lead service lines nationwide as part of investing in America agenda; 2023. Available from: https://www.epa.gov/newsreleases/biden-harris-administration-announces-new-get-lead-out-initiative-accelerate-removal.Search in Google Scholar
33. Campbell, C, Osterhoudt, KC. Prevention of childhood lead poisoning. Curr Opin Pediatr 2000;12:428–37. https://doi.org/10.1097/00008480-200010000-00002.Search in Google Scholar PubMed
34. Naranjo, VI, Hendricks, M, Jones, KS. Lead toxicity in children: an unremitting public health problem. Pediatr Neurol 2020;113:51–5.10.1016/j.pediatrneurol.2020.08.005Search in Google Scholar PubMed
35. Shamseer, L, Moher, D, Clarke, M, Ghersi, D, Liberati, A, Petticrew, M, et al.. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 2015:350:g7647.10.1136/bmj.g7647Search in Google Scholar PubMed
36. Ouzzani, M, Hammady, H, Fedorowicz, Z, Elmagarmid, A. Rayyan—a web and mobile app for systematic reviews. Syst Rev 2016;5:210. https://doi.org/10.1186/s13643-016-0384-4.Search in Google Scholar PubMed PubMed Central
37. Methley, AM, Campbell, S, Chew-Graham, C, McNally, R, Cheraghi-Sohi, S. PICO, PICOS and SPIDER: a comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv Res 2014;14:579. https://doi.org/10.1186/s12913-014-0579-0.Search in Google Scholar PubMed PubMed Central
38. Brown, MJ, McLaine, P, Dixon, S, Simon, P. A randomized, community-based trial of home visiting to reduce blood lead levels in children. Pediatrics 2006;117:147–53. https://doi.org/10.1542/peds.2004-2880.Search in Google Scholar PubMed
39. Campbell, C, Tran, M, Gracely, E, Starkey, N, Kersten, H, Palermo, P, et al.. Primary prevention of lead exposure: the Philadelphia lead safe homes study. Public Health Rep 2011;126(1 Suppl):76–88. https://doi.org/10.1177/00333549111260s111.Search in Google Scholar PubMed PubMed Central
40. Campbell, C, Gracely, E, Tran, M, Starkey, N, Kersten, H, Palermo, P, et al.. Primary prevention of lead exposure—blood lead results at age two years. Int J Environ Res Publ Health 2012;9:1216–26. https://doi.org/10.3390/ijerph9041216.Search in Google Scholar PubMed PubMed Central
41. Rothman, NL, Lourie, R, Gaughan, J, White, N. A community-developed, community-based lead poisoning prevention program: lead awareness North Philly style. Holist Nurs Pract 1999;14:47–58. https://doi.org/10.1097/00004650-199910000-00008.Search in Google Scholar PubMed
42. Lanphear, BP, Winter, NL, Apetz, L, Eberly, S, Weitzman, M. A randomized trial of the effect of dust control on children’s blood lead levels. Pediatrics 1996;98:35–40. https://doi.org/10.1542/peds.98.1.35.Search in Google Scholar
43. Rhoads, GG, Ettinger, AS, Weisel, CP, Buckley, TJ, Goldman, KD, Adgate, J, et al.. The effect of dust lead control on blood lead in toddlers: a randomized trial. Pediatrics 1999;103:551–5. https://doi.org/10.1542/peds.103.3.551.Search in Google Scholar PubMed
44. Schucker, GW, Vail, EH, Kelley, EB, Kaplan, E. Prevention of lead paint poisoning among Baltimore children. A hard-sell program. Public Health Rep 1965;80:969–74. https://doi.org/10.2307/4592586.Search in Google Scholar
45. Jordan, CM, Yust, BL, Robison, LL, Hannan, P, Deinard, AS. A randomized trial of education to prevent lead burden in children at high risk for lead exposure: efficacy as measured by blood lead monitoring. Environ Health Perspect 2003;111:1947–51. https://doi.org/10.1289/ehp.6352.Search in Google Scholar PubMed PubMed Central
46. Kassa, H, Bisesi, MS, Khuder, SA, Park, PC. Assessment of a lead management program for inner-city children. J Environ Health 2000;62:15–9.Search in Google Scholar
47. Nicholson, JS. A community-based intervention for low-income families to reduce children’s blood lead levels between 3-9.9 μg/Dl. Child Health Care 2018;47:379–96. https://doi.org/10.1080/02739615.2017.1370673.Search in Google Scholar
48. Schultz, B, Pawel, D, Murphy, A. A retrospective examination of in-home educational visits to reduce childhood lead levels. Environ Res 1999;80:364–8. https://doi.org/10.1006/enrs.1998.3922.Search in Google Scholar PubMed
49. Schlenker, TL, Baxmann, R, McAvoy, P, Bartkowski, J, Murphy, A. Primary prevention of childhood lead poisoning through community outreach. Wis Med J 2001;100:48–54.Search in Google Scholar
50. Kimbrough, RD, LeVois, M, Webb, DR. Management of children with slightly elevated blood lead levels. Pediatrics 1994;93:188–91.Search in Google Scholar
51. Sterling, DA, Evans, RG, Shadel, BN, Serrano, F, Arndt, B, Chen, JJ, et al.. Effectiveness of cleaning and health education in reducing childhood lead poisoning among children residing near superfund sites in Missouri. Arch Environ Health 2004;59:121–31. https://doi.org/10.3200/aeoh.59.3.121-131.Search in Google Scholar
52. Burke, H, Balding, B, Lyle, D. Reducing lead exposure in children in Broken Hill. N S W Public Health Bull 2003;14:52–4. https://doi.org/10.1071/nb03016.Search in Google Scholar PubMed
53. Hilts, SR, Bock, SE, Oke, TL, Yates, CL, Copes, RA. Effect of interventions on children’s blood lead levels. Environ Health Perspect 1998;106:79–83. https://doi.org/10.2307/3433782.Search in Google Scholar
54. Morales, J, Yovera-Sandoval, EM, Basilio-Rojas, MR. Community health services and blood lead reduction in children. Univers J Public Health 2022;10:590–5. https://doi.org/10.13189/ujph.2022.100606.Search in Google Scholar
55. Dignam, TA, Lojo, J, Meyer, PA, Norman, E, Sayre, A, Flanders, WD. Reduction of elevated blood lead levels in children in North Carolina and Vermont, 1996–1999. Environ Health Perspect 2008;116:981–5. https://doi.org/10.1289/ehp.10548.Search in Google Scholar PubMed PubMed Central
Supplementary Material
This article contains supplementary material (https://doi.org/10.1515/reveh-2023-0108).
© 2024 Walter de Gruyter GmbH, Berlin/Boston
Articles in the same Issue
- Frontmatter
- Reviews
- Mercury and cadmium-induced inflammatory cytokines activation and its effect on the risk of preeclampsia: a review
- Prevalence of chronic obstructive pulmonary disease in Indian nonsmokers: a systematic review & meta-analysis
- Beyond the outdoors: indoor air quality guidelines and standards – challenges, inequalities, and the path forward
- Cadmium exposure and thyroid hormone disruption: a systematic review and meta-analysis
- New generation sequencing: molecular approaches for the detection and monitoring of bioaerosols in an indoor environment: a systematic review
- Concentration of Tetrabromobisphenol-A in fish: systematic review and meta-analysis and probabilistic health risk assessment
- The association between indoor air pollution from solid fuels and cognitive impairment: a systematic review and meta-analysis
- Phthalates and uterine disorders
- Effectiveness of educational interventions for the prevention of lead poisoning in children: a systematic review
- Association between exposure to per- and polyfluoroalkyl substances and levels of lipid profile based on human studies
- Summary of seven Swedish case reports on the microwave syndrome associated with 5G radiofrequency radiation
- Expanding the focus of the One Health concept: links between the Earth-system processes of the planetary boundaries framework and antibiotic resistance
- Exploring the link between ambient PM2.5 concentrations and respiratory diseases in the elderly: a study in the Muang district of Khon Kaen, Thailand
- Standards for levels of lead in soil and dust around the world
- Tributyltin induces apoptosis in mammalian cells in vivo: a scoping review
- The influence of geology on the quality of groundwater for domestic use: a Kenyan review
- Biological concentrations of DDT metabolites and breast cancer risk: an updated systematic review and meta-analysis
- Letter to the Editor
- Ancient medicine and famous iranian physicians
Articles in the same Issue
- Frontmatter
- Reviews
- Mercury and cadmium-induced inflammatory cytokines activation and its effect on the risk of preeclampsia: a review
- Prevalence of chronic obstructive pulmonary disease in Indian nonsmokers: a systematic review & meta-analysis
- Beyond the outdoors: indoor air quality guidelines and standards – challenges, inequalities, and the path forward
- Cadmium exposure and thyroid hormone disruption: a systematic review and meta-analysis
- New generation sequencing: molecular approaches for the detection and monitoring of bioaerosols in an indoor environment: a systematic review
- Concentration of Tetrabromobisphenol-A in fish: systematic review and meta-analysis and probabilistic health risk assessment
- The association between indoor air pollution from solid fuels and cognitive impairment: a systematic review and meta-analysis
- Phthalates and uterine disorders
- Effectiveness of educational interventions for the prevention of lead poisoning in children: a systematic review
- Association between exposure to per- and polyfluoroalkyl substances and levels of lipid profile based on human studies
- Summary of seven Swedish case reports on the microwave syndrome associated with 5G radiofrequency radiation
- Expanding the focus of the One Health concept: links between the Earth-system processes of the planetary boundaries framework and antibiotic resistance
- Exploring the link between ambient PM2.5 concentrations and respiratory diseases in the elderly: a study in the Muang district of Khon Kaen, Thailand
- Standards for levels of lead in soil and dust around the world
- Tributyltin induces apoptosis in mammalian cells in vivo: a scoping review
- The influence of geology on the quality of groundwater for domestic use: a Kenyan review
- Biological concentrations of DDT metabolites and breast cancer risk: an updated systematic review and meta-analysis
- Letter to the Editor
- Ancient medicine and famous iranian physicians

