Abstract
Background
The scarcity of oncology specialists poses a significant challenge globally, particularly in regions with limited healthcare resources. This leads to delayed diagnoses and disparities in care. The shortage of oncology services disproportionately affects vulnerable populations, leading to delays in diagnosis, treatment, and poorer outcomes.
Aim
This study investigates the implications of oncology resource scarcity, focusing on South Africa’s Eastern Cape province, aiming to analyse challenges, interventions, and lessons from other countries.
Method
This review study employed a mixed-method research design encompassing an empirical literature review and case study approach. It drew on existing research and data to analyse the impact of oncology resource scarcity on patient care.
Results
Cancer-related mortality in the province remains considerable, with lung cancer emerging as a leading cause, underscoring the need for comprehensive cancer control strategies. Infrastructure disparities between urban and rural areas compound the challenges, with limited access to oncology facilities and specialists in remote regions.
Conclusion
Urgent action is needed to address oncology resource scarcity to improve cancer care outcomes, particularly in underserved regions. Targeted interventions and lessons from other countries can enhance access to quality oncology services and reduce disparities in care.
Contribution
This study’s findings have significant implications for South African health policy, particularly regarding the urgent scarcity of oncology resources. The critical shortage of oncology specialists in underserved areas like the Eastern Cape underscores the necessity for a comprehensive strategy to enhance cancer care.
1 Introduction
1.1 Scarcity of oncology resources and human capital
The scarcity of oncology specialists poses a critical challenge in addressing the global burden of cancer, disproportionately impacting urban and rural communities across high-income and low-income countries (LICs) [1,2,3]. The distribution of the oncology workforce reveals significant disparities, particularly in the oncologist-to-population ratio across various regions.
A global study indicated that the lower bound for an optimal cancer surgical workforce in lower-middle-income countries, such as the Philippines, should be at least 166,000 professionals [4]. In stark contrast, LICs experience significantly lower ratios, with some regions reporting as few as 1 oncologist per 500,000 to 1 million individuals. This disparity results in acute shortages, particularly in rural areas [5,6]. For example, Zimbabwe has an oncologist-to-population ratio of 1 oncologist per 1.057 million people, while the United States has a ratio of approximately 1 oncologist per 26,418 individuals [7].
The situation is even more alarming in certain African nations, such as South Sudan, Lesotho, Benin, Gambia, and Sierra Leone, which lack trained oncologists altogether [8]. In LICs, the median ratio of clinical oncologists is alarmingly low, with only 0.006 oncologists per 100,000 population and 0.01 oncologists per 100 cancer patients [9]. This severe shortage underscores the urgent need for targeted interventions to strengthen the oncology workforce and improve access to cancer care in under-resourced regions. Furthermore, these disparities are exacerbated by socio-economic challenges, including inadequate healthcare funding, poverty, and a lack of oncology training programmes [10].
The shortage of oncologists has widespread consequences for cancer care, particularly in regions where specialists are sparse. Patients in such areas often experience delays in receiving diagnoses and beginning treatment, which can lead to late-stage cancer diagnoses and significantly poorer outcomes [11]. This situation is worsened by extended appointment waiting times, further prolonging the time between symptom onset and therapeutic intervention [2,5]. Delays in treatment initiation reduce the effectiveness of therapies, negatively impacting patient survival rates [12].
In addition to delayed care, oncology resource scarcity limits patients’ access to comprehensive treatment modalities. Cancer care often requires a multidisciplinary approach involving medical oncologists, radiation oncologists, surgical oncologists, and allied healthcare professionals [10]. However, in areas with insufficient specialists, patients may lack access to critical therapies such as chemotherapy, radiation, and immunotherapy [12]. Consequently, patients often travel significant distances to reach specialised cancer centres, placing financial and logistical burdens on them and their families [11,13].
This scarcity of oncology specialists also contributes to stark disparities in cancer care. Patients in rural and underserved regions face more significant challenges in accessing oncological services due to geographic isolation, inadequate healthcare infrastructure, and financial constraints [14]. Moreover, marginalised communities, often affected by socio-economic disparities such as low income, limited education, and lack of health insurance, experience further obstacles in obtaining timely and appropriate cancer care [2,13]. These inequities perpetuate health disparities and worsen cancer-related outcomes, highlighting the urgent need for equitable distribution of oncology resources and improved access to cancer care services across all populations [2,6].
Overall, the unequal distribution of oncology specialists, particularly in low-income and rural regions, underscores the need for targeted strategies to enhance access to cancer care. By addressing the systemic barriers that limit the availability of oncology services, healthcare systems can work towards mitigating the global burden of cancer and improving patient outcomes [3,15].
1.2 Rationale
The scarcity of oncology specialists is a critical issue that demands attention due to its profound impact on global patient outcomes and healthcare systems.
Public health impact: Insufficient oncology resources have a direct impact on the quality of patient care, resulting in delayed diagnosis, extended waiting periods for treatment, and restricted availability of specialist therapies [2,5]. This, in turn, contributes to poorer health outcomes and increased mortality rates among cancer patients.
Socio-economic implications: Regions facing oncology resource scarcity often exhibit socio-economic challenges, such as poverty, unemployment, and limited access to healthcare services [2]. These disparities further exacerbate the effects of oncology resource scarcity, disproportionately affecting underserved populations and marginalised communities [14].
1.3 Problem statement
The scarcity of oncology specialists presents a pressing challenge in addressing the burden of cancer diseases globally and in local communities, leading to delayed diagnosis, prolonged waiting times for appointments, and limited access to specialised treatments and therapies [17]. The Eastern Cape province of South Africa exhibits a notable dearth of resources, characterised mainly by socio-economic challenges and insufficient healthcare facilities (Morris-Paxton et al. [18,19]). These factors further exacerbate inequalities in cancer treatment and negatively impact patient outcomes. The combination of socio-economic challenges and limited healthcare infrastructure intensifies disparities in cancer care, ultimately hindering the effectiveness of treatment for patients [20].
1.4 Aim
This review study aims to raise awareness of the pressing challenge posed by the scarcity of oncology specialists in addressing the burden of cancer diseases, mainly in the Eastern Cape province of South Africa.
1.5 Research methods
This review employed a concurrent mixed-method research design, combining an empirical literature review with a case study approach (Creswell [21]; Fetters et al. [22]). Yin [23] described case study research as an in-depth investigation of a phenomenon within its real-world context, mainly when the distinction between the phenomenon and its setting is unclear. The case study in this research focused on oncology resource scarcity in the Eastern Cape province of South Africa, using existing data to evaluate its effects on patient care [18,24,25].
The data sources included peer-reviewed literature on oncology resource allocation, cancer-related mortality rates, and national healthcare reports. Cancer incidence and death rates were analysed to identify the challenges associated with timely diagnosis and treatment. The literature review provided a broader analysis of oncology care trends, while the case study examined specific regional dynamics in the Eastern Cape. Qualitative and quantitative data analysis techniques were applied (Creswell, 2009; Fetters et al. 2013). Qualitative thematic analysis uncovered recurring themes, such as barriers to healthcare access, resource limitations, and policy gaps. The quantitative analysis supported the case study findings, mainly cancer incidence and mortality rates. The eligibility criteria for the literature review focused on peer-reviewed studies, government reports, and epidemiological data published between 2000 and 2023 that addressed oncology resource allocation and healthcare access in South Africa.
While the study employed a mixed-method approach, further details on integrating the case study with the broader literature review are required. The Eastern Cape’s selection as the case study site was justified by its high unemployment, widespread poverty, and significant socio-economic challenges, which worsened healthcare access issues. Additionally, the region experienced a substantial shortage of oncology practitioners, making it an important case for investigating the effects of oncology resource scarcity on patient care (Yin, 2018). The study drew from public and private sector reports, including data from Statistics South Africa, the Health District Information System, and the Council for Medical Schemes [26,27,28,29]. Data on oncology service providers were cross-referenced with Medpages and annual statutory returns submitted to the Council for Medical Schemes [30]. This triangulation of diverse data sources provided a comprehensive overview of oncology resource distribution across different healthcare settings. The combination of these datasets strengthened the study’s validity and reliability, enabling the identification of critical gaps in oncology service provision in the Eastern Cape province.
1.6 Clarification of concepts
The concepts shown in Table 1 have been considered and used in the analysis better to understand the setting and the study’s context.
Key concepts
| Oncology is a specialised field of medicine that involves the comprehensive examination and treatment of cancer, including its prevention, diagnosis, and therapeutic interventions. Providing comprehensive care for cancer patients involves a multidisciplinary approach that incorporates the expertise of medical oncologists, radiation oncologists, surgical oncologists, and other healthcare experts. Cancer is a collection of pathological conditions characterised by aberrant cellular growth and proliferation, which have the potential to infiltrate and inflict harm upon adjacent tissues and organs. One of the examples is breast cancer, which may present as a palpable lump or tumour in the breast, alterations in the breast’s shape or size, the release of fluid from the nipples, or modifications in the texture of the breast’s skin. |
Source: American Cancer Society [30].
-
Ethical considerations: Ensuring equitable access to oncology care is an ethical concern, as all individuals have the right to timely and quality healthcare services, regardless of their geographic location or socio-economic status. Addressing the scarcity of oncology specialists aligns with ethical principles of justice and benevolence, promoting fairness and maximising the well-being of all individuals affected by cancer.
2 Literature review
2.1 Eastern Cape case study – South Africa
The Eastern Cape province, located on the southeastern coast of South Africa, is characterised by its diverse landscapes, rich cultural heritage, and economic challenges. It covers an area of approximately 168,966 square kilometres. As counted in Census 2022, the Eastern Cape’s total population increased by 10.2% from 6.5 million more than a decade ago in Census 2011 to 7.2 million in the latest population and housing census [27]. The province’s economy is primarily agrarian, with agriculture, livestock farming, and forestry playing significant roles in employment generation and the gross domestic product (GDP). According to StatsSA [31], the province contributes 7.6% to the national GDP. The Eastern Cape faces numerous challenges, including high unemployment and widespread poverty, particularly in rural areas [32]. The province has the second highest prevalence of adult poverty, with a rate of 67.3%, and has the highest unemployment rate at 37.4% [33]. These socio-economic challenges significantly hinder access to essential health services in the region. Furthermore, the provinces face considerable obstacles in accessing screening services due to their distant locations, exacerbating the difficulties in obtaining critical healthcare interventions such as cancer screening and diagnosis for other life-threatening conditions.
2.2 Cancer incidence
Recent data reported by Ramaliba et al. [34] indicate a notable increase in new cancer cases, rising from 1193 in 2013 to 1666 in 2017, representing a 40% increase. This surge underscores a growing demand for cancer-related services and resources. The surveillance data further highlight regional disparities, with the southern part of the surveillance area consisting of five rural and one urban magisterial area. In contrast, the northern part comprises only three predominantly rural magisterial areas. Among females, the age group of 50–69 years accounts for approximately a quarter of cancer incidence, while 165 new cases were reported among males. The top three most prevalent cancers in males are prostate (C61), oesophagus (C15), and trachea, bronchus, and lung (C33–34). Conversely, among females, the leading cancers are cervix uteri (C53), breast (C50), and oesophagus (C15).
2.3 Morality cancer
This section presents data on the number of cancer-related deaths in the Eastern Cape province compared to the national figures. According to the table provided, the median number of cancer-related deaths in the province was 5,212 [28]. The data reveal that the number of deaths has consistently remained in this range, except for between 2011 and 2023, during which it dipped below 5,000. Over the 11-year review period, the Eastern Cape accounted for approximately 12.5% of the countrywide cancer-related deaths, with 2017 and 2018 representing 13% of the total (Table 2).
Number of cancer-related deaths in Eastern Cape Province
| Period | Eastern Cape | Other provinces | South Africa | Easter Cape, relative to population (%) |
|---|---|---|---|---|
| 2008 | 5,011 | 28,709 | 33,720 | 15 |
| 2009 | 5,118 | 30,020 | 35,138 | 15 |
| 2010 | 5,243 | 30,276 | 35,519 | 15 |
| 2011 | 4,937 | 31,583 | 36,520 | 14 |
| 2012 | 4,489 | 32,908 | 37,397 | 12 |
| 2013 | 4,577 | 33,837 | 38,414 | 12 |
| 2014 | 5,221 | 35,006 | 40,227 | 13 |
| 2015 | 5,121 | 36,679 | 41,800 | 12 |
| 2016 | 5,286 | 37,333 | 42,619 | 12 |
| 2017 | 5,460 | 37,397 | 42,857 | 13 |
| 2018 | 5,577 | 38,036 | 43,613 | 13 |
Source: Adapted from StatsSA [28].
Figure 1 presents information extracted from Statistics South Africa regarding the top 10 cancers contributing to mortality in the province in 2018 [28]. According to the data, bronchus and lung cancer emerge as the predominant cause, representing approximately 14% of cancer-related deaths. Following closely is oesophagus cancer, which accounted for approximately 12% of mortality cases. Oesophagus cancer was highest compared to the other eight provinces, with 386 in Gauteng, 459 in KwaZulu Natal, and 355 in the Western Cape.
![Figure 1
Cancers contributing to mortality in Eastern Cape, 2018 – Select the top 10. Source: Adapted from StatsSA [28].](/document/doi/10.1515/ohe-2025-0058/asset/graphic/j_ohe-2025-0058_fig_001.jpg)
Cancers contributing to mortality in Eastern Cape, 2018 – Select the top 10. Source: Adapted from StatsSA [28].
2.4 Facilities
Facilities with oncology departments in the Eastern Cape vary widely across urban and rural areas, as depicted in Table 3. While cities like Port Elizabeth, East London, and Mthatha boast modern infrastructure, including airports, ports, and major highways, rural communities often lack essential services such as electricity, clean water, and adequate healthcare facilities. Access to oncology services is also prevalent in these urban areas, as illustrated by the data in the private sector sourced from Medpages [30], which depict that most of the oncology departments/units are located in Gqebera (Gqeberha, was known as Port Elizabeth, Nelson Mandela Bay), according to Table 3. The radiation oncology department appears also to be based in Gqeberha.
Hospitals with oncology departments/unit
| City (municipality) | Area | Hospital |
|---|---|---|
| East London (or Tambo District Municipality) | Amalinda | Frere Hospital - Radiation Oncology Dept |
| Southernwood | Life St Dominic’s Hospital - Oncology (St Agatha Ward) | |
| Gqeberha (Nelson Mandela Bay Metropolitan Municipality) | Central | Life St George’s Hospital - Oncology Dept |
| Korsten | Livingstone Hospital - Oncology Dept | |
| Mount Croix | Port Elizabeth Provincial Hospital - Oncology Unit | |
| Mthatha (or Tambo District Municipality) | Fort Gale | Nelson Mandela Academic Hospital - Oncology Dept |
Source: Adapted from Medpages [30].
2.5 Access and availability of oncology services
The scarcity of oncology medical service providers presents a pressing concern that directly impacts patient care and outcomes. Like many others in South Africa, the region grapples with significant disparities in access to specialised healthcare services, particularly in oncology. The shortage of oncologists and cancer treatment facilities has profound implications for our community’s well-being. The limited number of oncologists and treatment centres translates into long waiting times for appointments, delays in diagnosis, and restricted access to vital treatments and therapies. The issue becomes further exacerbated by the fact that most oncology services in South Africa are centralised within the private sector, which only serves a fraction of the population, estimated to be less than 15%. This concentration of services creates a significant disparity in access to cancer care between those who can afford private healthcare and the majority who rely on public services. South Africa has little over 200 clinical or radiation oncologists, with 80% in the commercial sector and 20% in the public health sector, according to van Eeden et al. [35]. This resource gap makes radiation harder for many patients. The nationwide deployment of radiation units complicates matters. Nearly 77% (64 units) of the nation’s 83 teletherapy units are in three of its nine provinces.
Patients in rural and underserved areas are most vulnerable, where geographic barriers compound the difficulties of accessing quality oncology care. Figure 2 depicts the count of claiming Independent Practice Specialist Radiation Oncologists in the medical schemes. The graph illustrates a pronounced concentration of oncologists in the Nelson Mandela Bay/Gqeberha and Buffalo City areas. Conversely, no practising oncologists were in the Chris Hani District Municipality and Joe Gqabi District in 2022. In addition, there were no more than three independent practice specialist radiation oncologists in these areas, which mirrors the situation in the OR Tambo and Sarah Baartman districts, which are mainly rural.
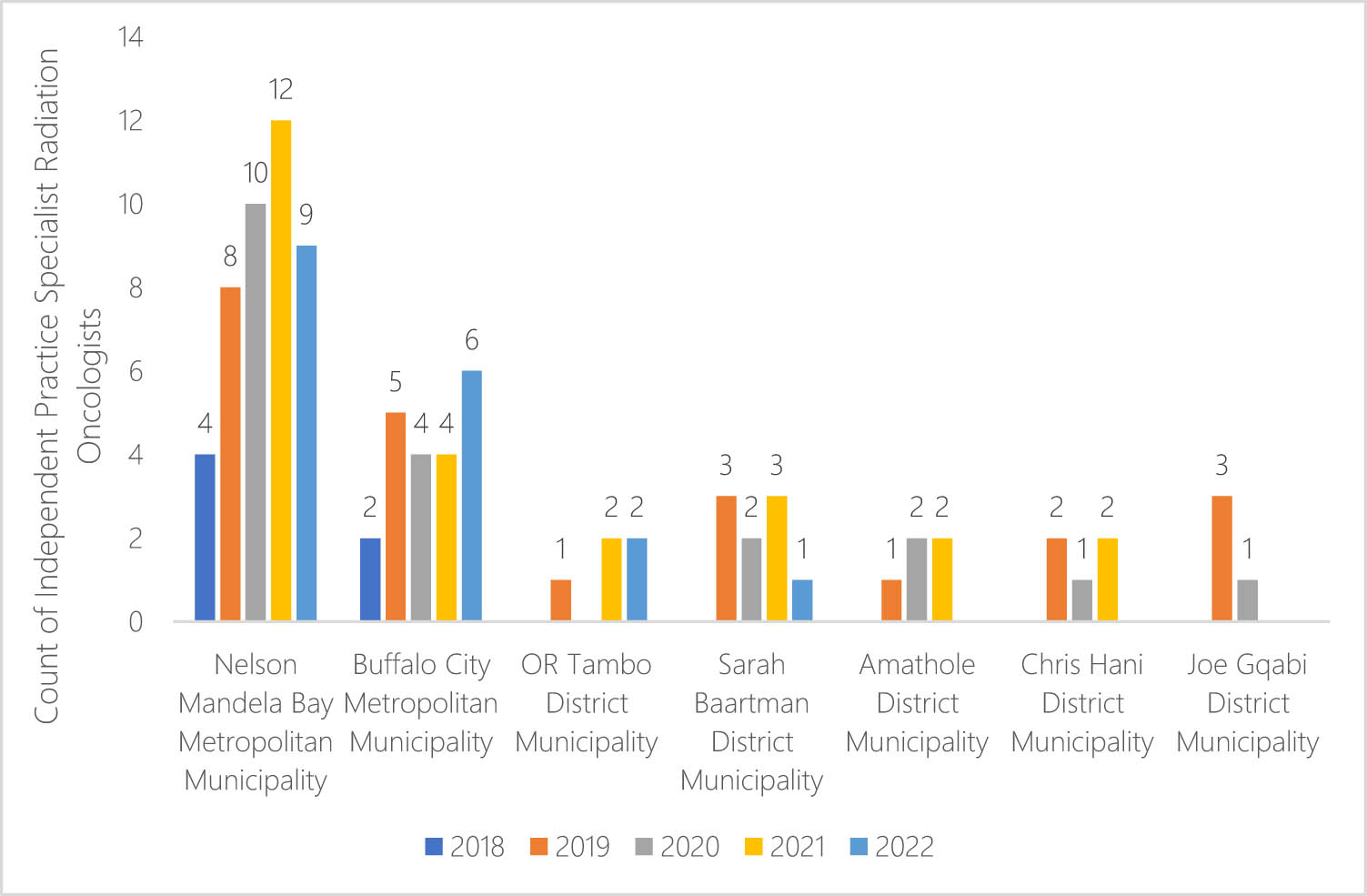
Count of Independent Practice Specialist Radiation Oncologists claiming from medical schemes for 2018–2022 by Eastern Cape district. Source: Generated from the CMS (2024) unpublished report.
2.6 Select screening services: Cervical screening coverage
This section discusses cervical screening coverage, defined as the proportion of eligible individuals who undergo screening within a specified timeframe. For individuals aged 25–49 years, screening should occur within 3.5 years, while for those aged 50–64 years, it should occur within 5.5 years [36]. Cervical cancer screening coverage serves as a critical monitoring indicator for the World Health Organization’s (WHO) cervical cancer elimination plan. Figure 3 illustrates an increase in coverage ratios at both provincial and national levels, with the province showing slightly higher coverage compared to the national average, reaching 50% relative to 46.8% nationally in 2019, which is both below and below the target of 70% set by the WHO [26,37,38]. The data presented demonstrate a significant decline in screening rates due to the influence of the COVID-19 pandemic in 2020. The substantial decrease in screening rates from 2020 to 2022 may potentially have an adverse impact on the number of related deaths.
![Figure 3
Cervical cancer screening coverage (%) (2020 NIDS): Eastern Cape Province and National: Source Ntshangase and Sebitloane [26].](/document/doi/10.1515/ohe-2025-0058/asset/graphic/j_ohe-2025-0058_fig_003.jpg)
Cervical cancer screening coverage (%) (2020 NIDS): Eastern Cape Province and National: Source Ntshangase and Sebitloane [26].
2.7 Key interventions and learnings from other countries
Due to the scarcity of these services in the province, immediate intervention is needed to partner with the private sector, as a more significant majority of oncology service providers operate in the private sector. Addressing the scarcity of oncology resources and human capital requires a multifaceted approach encompassing various interventions and drawing lessons from successful strategies implemented in other countries (Table 4).
Interventions and key lessons from other countries
| Intervention | Key lessons from other Countries |
|---|---|
| Optimisation of technology | Utilising telemedicine and digital health platforms has emerged as a key intervention to overcome barriers to oncology care. Lessons from countries like the United States and Canada emphasise the importance of integrating telemedicine into oncology practice to reach patients who face geographic and logistical challenges in accessing care [39,40,41] |
| Collaboration among African countries | Establishing partnerships and networks among African countries is crucial for sharing resources, expertise, and best practices in oncology care. The lessons derived from efforts such as the African Access Initiative highlight the significance of cross-border collaborations in enhancing access to cancer prevention, diagnosis, and treatment services [38,42,43] |
| Interventions in rural provinces | Implementing mobile clinics, telehealth initiatives, and capacity-building programmes for nurses and primary healthcare providers is essential to improving rural provinces’ access to basic oncology services. Lessons from countries like Australia and Brazil highlight the effectiveness of mobile cancer screening units and telemedicine networks in reaching rural populations and reducing disparities in cancer care [38,41] |
| Partnering with donors | Collaborating with international donors is vital to secure funding and equipment for oncology facilities and treatment centres. The significance of sustained collaborations with donors in enhancing health systems and accessibility to cancer care is underscored by the lessons derived from programmes supported by esteemed organisations such as the WHO and the Bill & Melinda Gates Foundation [44] |
| Revisit budgeting and planning | Reviewing and reallocating healthcare budgets to prioritise oncology services is essential for adequate staffing, equipment, and infrastructure funding. Lessons from countries like the United Kingdom and Sweden underscore the need for long-term planning and investment in cancer services to meet the evolving needs of populations and achieve equitable access to care [45,46] |
| Optimisation of partnerships | Strengthening partnerships with medical schools in provinces with higher concentrations of oncology services, such as Gqeberha, is crucial for enhancing training and workforce development. Lessons from academic partnerships in countries like India and South Korea demonstrate the value of integrating oncology training into medical curricula and establishing mentorship programmes to groom the next generation of cancer care providers [47,48,49] |
3 Discussion
The scarcity of oncology resources and human capital presents a formidable challenge globally, affecting patient care, healthcare systems, and socio-economic well-being [1,2,3]. Oncologists are pivotal in diagnosing, treating, and providing ongoing care for cancer patients. However, the scarcity of these resources contributes to the postponement of diagnoses, extended waiting periods for consultations, and restricted availability of specialised therapies, ultimately leading to inferior health outcomes and heightened mortality rates among those diagnosed with cancer [3,15]. The difficulties are further intensified in the Eastern Cape province of South Africa, which is distinguished by elevated levels of poverty and unemployment, inadequate healthcare infrastructure, and geographical obstacles that hinder the availability of oncology services [32]. Efforts to address this scarcity require multifaceted approaches, including decentralising oncology services, expanding training programmes for oncologists, and addressing socio-economic disparities in cancer care [6]. Aligning with ethical principles of justice and beneficence, prioritising efforts to address oncology resource scarcity can improve patient outcomes, promote health equity, and strengthen healthcare systems globally [11].
This review underscores the urgent need to address oncology resource scarcity, highlighting the unique challenges faced in underserved regions like the Eastern Cape province in South Africa. This work offers valuable insights for stakeholders aiming to enhance cancer care globally. It highlights key interventions, lessons learned from other African nations, and international experiences, with a particular focus on the Eastern Cape province of South Africa.
Countries like Kenya and Uganda have implemented community health worker programmes to extend the reach of oncology services into rural areas, facilitating early detection and referral for cancer patients [50,51,52]. These programmes leverage local resources and knowledge, reducing geographic barriers to care. Additionally, Rwanda has successfully integrated telemedicine into its healthcare system, improving access to oncologists and specialised treatments for patients in remote areas (Kok et al. [53,54]). This model can be adapted to the Eastern Cape to enhance service delivery in under-resourced settings.
Optimisation of technology, such as telemedicine and digital health platforms, has emerged as a crucial intervention, drawing insights from experiences in the United States and Canada, where integrating telemedicine into oncology practice has improved access for patients facing geographic and logistical barriers [40,41]. Collaboration among African countries is also essential, with initiatives like the African Access Initiative emphasising the value of cross-border partnerships in improving access to cancer prevention, diagnosis, and treatment services [6,43]. For instance, the African Cancer Registry Network has facilitated data sharing and collaboration among countries like Ghana, Nigeria, and Botswana to improve cancer surveillance and resource allocation [55]. Experts from Ghana, Kenya, South Africa, and Zimbabwe have recently shared their knowledge and expertise in developing Botswana’s inaugural National Cancer Control Programme. This initiative supports the IAEA’s efforts to improve national cancer control planning across Africa and promote South-South cooperation (Nobile [56]). However, collective efforts are still required to address and prioritise under-resourced, rural communities where access to oncology medical service providers is limited due to their scarcity.
In rural provinces, implementing mobile clinics, telehealth initiatives, and capacity-building programmes for healthcare providers are vital interventions, drawing lessons from successful strategies in countries like Australia and Brazil [38]. Partnering with donors is emphasised to secure funding and equipment for oncology facilities, with lessons from initiatives by organisations like the WHO and the Bill & Melinda Gates Foundation underscoring the importance of sustainable partnerships [44]. For instance, partnerships have proven effective in mobilising resources for cancer care, thereby improving access to both treatment and diagnostic services.
Revisiting budgeting and planning is essential to secure sufficient funding for oncology services, with valuable insights from countries such as the United Kingdom and Sweden underscoring the importance of long-term investment to ensure equitable access to care [45]. Strengthening partnerships with medical schools is also essential for workforce development, drawing lessons from academic collaborations in countries like India and South Korea to groom the next generation of cancer care providers [48,49].
While the review underscores the urgent need to address oncology resource scarcity and highlights the unique challenges faced in underserved regions like the Eastern Cape province, it is essential to contrast these findings with existing literature. Prior research has indicated that the scarcity of oncology resources and human capital indeed presents significant challenges globally, affecting patient care, healthcare systems, and socio-economic well-being [1,2,3]. The scarcity of oncologists contributes to the postponement of diagnoses, extended waiting periods for visits, and restricted availability of specialised therapies, ultimately leading to inferior health outcomes and heightened mortality rates among those diagnosed with cancer [3,15]. Efforts to address this scarcity necessitate multifaceted approaches, including decentralising oncology services, expanding training programmes for oncologists, and addressing socio-economic disparities in cancer care [6].
The review highlights the importance of key interventions and valuable insights from international and African experiences to address the challenge of limited oncology resources, particularly in the Eastern Cape region. However, it is imperative to acknowledge the obstacles and constraints associated with the local implementation of these strategies. Therefore, future research should focus on assessing the feasibility and effectiveness of these interventions within the specific sociocultural, economic, and healthcare system contexts of the Eastern Cape province to ensure their successful implementation and impact on improving cancer care outcomes [3,32,40].
4 Recommendations
The review underscores the urgent need to address oncology resource scarcity, particularly in underserved regions like the Eastern Cape province of South Africa. Based on global experiences and acquired knowledge, several recommendations arise to address this difficulty and enhance the results of cancer treatment:
Optimisation of technology: Leveraging telemedicine and digital health platforms can enhance access to oncology services, particularly for patients facing geographical and logistical barriers. Lessons from the United States and Canada suggest that integrating telemedicine into oncology practice can facilitate remote consultations and monitoring and improve patient access and convenience.
Collaboration among African countries: Initiatives like the African Access Initiative emphasise the importance of cross-border partnerships in improving access to cancer prevention, diagnosis, and treatment services. Strengthening collaboration among African nations can foster knowledge sharing, resource pooling, and capacity building in oncology care.
Implementation of mobile clinics and telehealth initiatives: Drawing from successful strategies in countries like Australia and Brazil, establishing mobile clinics and telehealth initiatives in rural provinces can enhance access to oncology services and facilitate early detection and treatment of cancer.
Partnerships with donors: Partnering with donors, such as the WHO and the Bill & Melinda Gates Foundation, is essential to secure funding and equipment for oncology facilities. Lessons from successful initiatives underscore the importance of sustainable partnerships in addressing resource scarcity.
Revisiting budgeting and planning: Ensuring adequate funding for oncology services requires revisiting budgeting and planning processes. Insights from countries like the United Kingdom and Sweden emphasise the need for long-term investment in oncology care to achieve equitable access and improve patient outcomes.
Strengthening partnerships with medical schools: Collaborating with medical schools is vital for workforce development in oncology care. Lessons from academic collaborations in countries like India and South Korea highlight the importance of grooming the next generation of cancer care providers through training programmes and research initiatives.
These recommendations provide a framework for addressing oncology resource scarcity and improving cancer care in the Eastern Cape province and similar underserved regions. Implementing multifaceted approaches that consider local contexts and challenges is crucial for achieving meaningful and sustainable improvements in oncology care outcomes.
5 Conclusion
The scarcity of oncology medical specialists presents a critical challenge in addressing the burden of cancer diseases, both globally and within local communities. Oncologists play a pivotal role in diagnosing, treating, and providing ongoing care for cancer patients, making their shortage a pressing concern for healthcare systems worldwide. Regions lacking oncology specialists face numerous obstacles in accessing timely and quality care, leading to delayed diagnosis, prolonged appointment waiting, and limited access to specialised treatments and therapies. These challenges are further exacerbated by disparities in cancer care, particularly among underserved populations and marginalised communities. The Eastern Cape province of South Africa exemplifies these challenges, with high poverty rates, unemployment, and limited access to essential healthcare services. The shortage of oncology specialists in the area has significant consequences for patient outcomes, resulting in delays in diagnosis and treatment commencement.
Moreover, it restricts patients’ access to comprehensive cancer care services. The data presented highlights the urgent need for strategies to address the shortage of oncology specialists and improve access to cancer care services in the Eastern Cape province. Efforts to decentralise oncology services, expand training programmes for oncologists, and invest in healthcare infrastructure in rural and underserved areas are essential to achieving equitable access to oncology care for all individuals in the region.
6 Contribution of the study
The findings of this study have important implications for health policy in South Africa, particularly in addressing the pressing issue of oncology resource scarcity. The severe shortage of oncology specialists, particularly in underserved areas like the Eastern Cape, highlights the need for a comprehensive strategy to improve cancer care. South African health policymakers must prioritise decentralising oncology services to ensure broader geographical coverage, especially in rural and remote areas. Telemedicine and mobile clinics are critical interventions that can mitigate the challenges posed by geographic barriers and improve access to oncology services. Furthermore, there is an urgent need to increase the number of trained oncologists through targeted educational programmes and partnerships with academic institutions. The government must also address the socio-economic disparities that disproportionately affect low-income and rural populations, ensuring that cancer care is accessible and affordable for all citizens. Sustainable investment in healthcare infrastructure and workforce development, alongside partnerships with international donors and African regional collaborations, could significantly enhance South Africa’s healthcare system’s capacity to meet the growing cancer burden. This approach aligns with the ethical principles of equity and justice, promoting fair access to life-saving care nationwide.
Acknowledgements
The author is grateful Sipho Kabane and Toko Potelwa for their invaluable contributions and feedback in completing this article.
-
Funding information: The author states no funding involved.
-
Author contribution: MMW produced the concept note and text. MMW supervised the data preparation, cleaning, and analysis processes. MMW assumed additional responsibilities in literature review compilation, formal analysis, project administration, supervision, visualisation, and manuscript writing.
-
Conflict of interest: The author states no conflict of interest.
-
Data availability statement: Since this study cited public domain data, data sharing is not applicable.
-
Disclaimer: The author of this article offer his views and ideas, which may not necessarily align with the official stance or position of any agency linked to the authors with whom they are affiliated.
References
[1] Mao JJ, Pillai GG, Andrade CJ, Ligibel JA, Basu P, Cohen L, et al. Integrative oncology: Addressing the global challenges of cancer prevention and treatment. CA: A Cancer J Clinicians. 2022;72(2):144–64. 10.3322/caac.21706.Search in Google Scholar PubMed
[2] Ramutumbu NJ, Ramathuba DU, Maputle MS. Barriers to accessing oncology services for effective cancer care in the public health institutions in Limpopo Province, South Africa: a qualitative study. Nurs Rep. 2023;13(3):956–68. 10.3390/nursrep13030084.Search in Google Scholar PubMed PubMed Central
[3] Roques T. Addressing the capacity crisis in oncology, progress and ongoing concerns. London, United Kingdom: Clinical Oncology Blog; 2024. https://www.rcr.ac.uk/news-policy/latest-updates/addressing-the-capacity-crisis-in-oncology-progress-and-ongoing-concerns/.Search in Google Scholar
[4] Perera SK, Jacob S, Wilson BE, Ferlay J, Bray F, Sullivan R, et al. Global demand for cancer surgery and an estimate of the optimal surgical and anaesthesia workforce between 2018 and 2040: A population-based modelling study. Lancet Oncol. 2021;22(2):182–9. 10.1016/S1470-2045(20)30349-0.Search in Google Scholar
[5] Lombe DC, Mwamba M, Msadabwe S, Bond V, Simwinga M, Ssemata AS, et al. Original research: Delays in seeking, reaching and access to quality cancer care in sub-Saharan Africa: A systematic review. BMJ Open. 2023;13(4):e067715. 10.1136/bmjopen-2022-067715.Search in Google Scholar PubMed PubMed Central
[6] Omotoso O, Teibo JO, Atiba FA, Oladimeji T, Paimo OK, Ataya FS, et al. Addressing cancer care inequities in sub-Saharan Africa: current challenges and proposed solutions. Int J Equity Health. 2023;22:189. 10.1186/s12939-023-01962-y.Search in Google Scholar PubMed PubMed Central
[7] Naicker S, Eastwood JB, Plange-Rhule J, Tutt RC. Shortage of healthcare workers in sub-Saharan Africa: A nephrological perspective. Clin Nephrology. 2010;74(Suppl 1):S129–33. 10.5414/cnp74s129.Search in Google Scholar PubMed
[8] Mathew A. Global survey of clinical oncology workforce. JCO Glob Oncol. 2018;2018(4):1–12. 10.1200/JGO.17.00188.Search in Google Scholar PubMed PubMed Central
[9] Trapani D, Murthy S, Boniol M, Booth C, Simensen V, Kasumba M, et al. Distribution of the workforce involved in cancer care: A systematic review of the literature. ESMO Open. 2021;6(6):100292. 10.1016/j.esmoop.2021.100292.Search in Google Scholar PubMed PubMed Central
[10] Silbermann M, Pitsillides B, Al-Alfi N, Omran S, Al-Jabri K, Elshamy K, et al. Multidisciplinary care team for cancer patients and its implementation in several Middle Eastern countries. Ann Oncol. 2013;24(Suppl 7):vii41. 10.1093/annonc/mdt265.Search in Google Scholar PubMed PubMed Central
[11] Kibudde S, Namisango E, Nakaganda A, Atieno M, Bbaale J, Nabwana M, et al. Turnaround time and barriers to treatment of newly diagnosed cancer in Uganda: A mixed-methods longitudinal study. Afr Health Sci. 2022;22(1):327–37. 10.4314/ahs.v22i1.40.Search in Google Scholar PubMed PubMed Central
[12] Taberna M, Moncayo FG, Jané-Salas E, Antonio M, Arribas L, Vilajosana E, et al. The multidisciplinary team (MDT) approach and quality of care. Front Oncol. 2020;10:85. 10.3389/fonc.2020.00085.Search in Google Scholar PubMed PubMed Central
[13] Walsh J, Harrison JD, Young JM, Butow PN, Solomon MJ, Masya L. What are the current barriers to effective cancer care coordination? A qualitative study. BMC Health Serv Res. 2010;10:132. 10.1186/1472-6963-10-132.Search in Google Scholar PubMed PubMed Central
[14] Kale S, Hirani S, Vardhan S, Mishra A, Ghode DB, Prasad R, et al. Addressing cancer disparities through community engagement: lessons and best practices. Cureus. 2023;15(8):e43445. 10.7759/cureus.43445.Search in Google Scholar PubMed PubMed Central
[15] Baird R, Banks I, Cameron D, Chester J, Earl H, Flannagan M, et al. An association of cancer physicians’ strategy for improving services and outcomes for cancer patients. Ecancermedicalscience. 2016;10:608. 10.3332/ecancer.2016.608.Search in Google Scholar PubMed PubMed Central
[16] Maphumulo WT, Bhengu BR. Challenges of quality improvement in the healthcare of South Africa post-apartheid: A critical review. Curationis. 2019;42(1):1–9. http://www.scielo.org.za/scielo.php?script=sci_arttext&pid=S2223-62792019000100012&lng=en&nrm=iso. 10.4102/curationis.v42i1.1901.Search in Google Scholar PubMed PubMed Central
[17] Somaroo H, Ramiah D. Maternal and neonatal health. Beyond diagnosis: using a futurist approach to improve access to radiation oncology services in South Africa. South African Health Review. South Africa: Health Systems Trust. 2024;26. 10.61473/001c.118826.Search in Google Scholar
[18] Willie MM, Maqbool M. Access to public health services in South Africa’s rural Eastern Cape Province. Appl Sci Res Periodicals. 2023;1(2):35–54.10.2139/ssrn.4405870Search in Google Scholar
[19] Morris-Paxton AA, Reid S, Ewing RG. Primary healthcare services in the rural Eastern Cape, South Africa: Evaluating a service-support project. Afr J Prim Health Care Fam Med. 2020;12(1):1–7. http://www.scielo.org.za/scielo.php?script=sci_arttext&pid=S2071-29362020000100020&lng=en&nrm=iso. 10.4102/phcfm.v12i1.2207.Search in Google Scholar PubMed PubMed Central
[20] Bourgeois A, Horrill T, Mollison A, Stringer E, Lambert LK, Stajduhar K. Barriers to cancer treatment for people experiencing socioeconomic disadvantage in high-income countries: a scoping review. BMC Health Serv Res. 2024;24:670. 10.1186/s12913-024-11248-1.Search in Google Scholar
[21] Creswell JW. Research design: Qualitative, quantitative, and mixed methods approaches. 3rd ed. Thousand Oaks (CA): SAGE Publications; 2009.Search in Google Scholar
[22] Fetters MD, Curry LA, Creswell JW. Achieving integration in mixed methods designs – principles and practices. Health Serv Res. 2013;48(6 Pt 2):2134–56. 10.1111/1475-6773.12117.Search in Google Scholar PubMed PubMed Central
[23] Yin RK. Case study research and applications: Design and methods. 6th edn. Thousand Oaks (CA): SAGE Publications; 2018.Search in Google Scholar
[24] Chitha W, Swartbooi B, Jafta Z, Funani I, Maake K, Hongoro D, et al. Model of delivery of cancer care in South Africa’s Eastern Cape and Mpumalanga provinces: A situational analysis protocol. BMJ Open. 2022;12(2):e058377. 10.1136/bmjopen-2021-058377.Search in Google Scholar PubMed PubMed Central
[25] Willie MM, Noutchang T, Molatseli M, Kabane S. Funding of oncology benefits by medical schemes, South Africa: A focus on breast and cervical cancer. London, United Kingdom: IntechOpen; 2023. 10.5772/intechopen.107418.Search in Google Scholar
[26] Ntshangase NP, Sebitloane H. Cervical cancer screening coverage. District Health Barometer. Durban, South Africa: Health Systems Trust; 2024. https://www.hst.org.za/publications/District%20Health%20Barometers/DHB%202022-23%20Section%20A,%20chapter%203%20-%20Non-communicable%20diseases.pdf.Search in Google Scholar
[27] Statistics South Africa. Eastern Cape home to over 7.2 million people. [Press release] Pretoria, South Africa: Improving Lives Through Data Ecosystems; 2023a. https://www.statssa.gov.za/?p=16760.Search in Google Scholar
[28] Statistics South Africa. Cancer in South Africa, 2008 – 2019 (Report No. 03-08-00). Pretoria: Statistics South Africa; 2023b. https://www.statssa.gov.za/publications/03-08-00/03-08-002023.pdf.Search in Google Scholar
[29] Statistics South Africa. Provincial gross domestic product: experimental estimates, 2013–2022 (Discussion Document No. D0441.1). Pretoria: Statistics South Africa; 2023c. https://www.statssa.gov.za/publications/D04411/D044112022.pdf.Search in Google Scholar
[30] American Cancer Society. What is oncology? Atlanta, GA: American Cancer Society; [date unknown]. Available from: https://www.cancer.org.medpages.info/hospital-depts-oncology-eastern-cape-south-africa.Search in Google Scholar
[31] StatsSA. Gross domestic product (GDP) statistics. Pretoria: Statistics South Africa; 2022. https://www.statssa.gov.za.Search in Google Scholar
[32] Ngumbela X, Khalema E, Nzimakwe T. Local worlds: Vulnerability and food insecurity in the Eastern Cape province of South Africa. Jàmbá: J Disaster Risk Stud. 2020;12(1):10. 10.4102/jamba.v12i1.830.Search in Google Scholar PubMed PubMed Central
[33] Statistics South Africa. Men, women and children: Findings of the living conditions survey 2014/15. Pretoria: Statistics South Africa; 2018. https://www.statssa.gov.za/publications/Report-03-10-02%20/Report-03-10-02%202015.pdf.Search in Google Scholar
[34] Ramaliba TM, Sithole N, Ncinitwa A. Cancer incidence in selected municipalities of the Eastern Cape Province, 2013–2017. Eastern Cape Cancer Registry Technical Report. Cape Town: South African Medical Research Council; 2020. https://www.samrc.ac.za/sites/default/files/attachments/2022-08/CancerIncidenceEasternCape2013-2017.pdf.Search in Google Scholar
[35] van Eeden R, Tunmer M, Nayler S. Lung cancer in South Africa. J Thorac Oncol. 2019;15(1):22–8. 10.1016/j.jtho.2019.06.032.Search in Google Scholar PubMed
[36] Judah G, Dilib F, Darzi A, Huf S. A population survey on beliefs around cervical cancer screening: Determining the barriers and facilitators associated with attendance. BMC Cancer. 2022;22:522. 10.1186/s12885-022-09529-w.Search in Google Scholar PubMed PubMed Central
[37] Bruni L, Serrano B, Roura E, Alemany L, Cowan M, Herrero R, et al. Cervical cancer screening programmes and age-specific coverage estimates for 202 countries and territories worldwide: a review and synthetic analysis. J Glob Health. 2022;10(8):E1115–27. 10.1016/S2214-109X(22)00241-8.Search in Google Scholar PubMed PubMed Central
[38] Henderson JT, Webber EM, Sawaya GF. Screening for ovarian cancer: Updated evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2018;319(6):595–606. 10.1001/jama.2017.21421.Search in Google Scholar PubMed
[39] Elder AJ, Alazawi H, Shafaq F, Ayyad A, Hazin R. Teleoncology: Novel approaches for improving cancer care in North America. Cureus. 2023;15(8):e43562. 10.7759/cureus.43562.Search in Google Scholar PubMed PubMed Central
[40] Haleem A, Javaid M, Singh RP, Suman R. Telemedicine for healthcare: Capabilities, features, barriers, and applications. Sens Int. 2021;2:100117. 10.1016/j.sintl.2021.100117.Search in Google Scholar PubMed PubMed Central
[41] Tang M, Reddy A. Telemedicine and its past, present, and future roles in providing palliative care to advanced cancer patients. Cancers. 2022;14(8):1884. 10.3390/cancers14081884.Search in Google Scholar PubMed PubMed Central
[42] Blanchard C, Lubuzo B, Asirwa FC, Dlamini X, Msadabwe-Chikuni SC, Mwachiro M, et al. Multisector collaborations and global oncology: The only way forward. JCO Glob Oncol. 2021;7:153–61. 10.1200/GO.20.00492.Search in Google Scholar PubMed PubMed Central
[43] Bryce J, Boschi-Pinto C, Shibuya K, Black RE. The WHO Child Health Epidemiology Reference Group. WHO estimates of the causes of death in children. Lancet. 2005;365:1147–52. 10.1016/S0140-6736(05)71877-8.Search in Google Scholar PubMed
[44] Morhason-Bello IO, Odedina F, Rebbeck TR, Harford J, Dangou JM, Denny L, et al. Challenges and opportunities in cancer control in Africa: A perspective from the African Organisation for Research and Training in Cancer. Lancet Oncol. 2013;14(4):e142–51. 10.1016/S1470-2045(12)70482-5.Search in Google Scholar PubMed
[45] Albers P, Albrecht W, Algaba F, Bokemeyer C, Cohn-Cedermark G, Fizazi K, et al. Guidelines on testicular cancer: 2015 update. Eur Urol. 2015 Dec;68(6):1054–68. 10.1016/j.eururo.2015.07.044. Epub 2015 Aug 18. PMID: 26297604.Search in Google Scholar PubMed
[46] Soliman R, Heneghan C, Boylan AM, Oke J, Eweida W, Elhaddad A. Barriers and facilitators to implementing cost-effective evidence-based childhood cancer treatment in a resource-limited setting in Egypt: A qualitative interview study. JCO Glob Oncol. 2023;9:e2200424. 10.1200/GO.22.00424.Search in Google Scholar PubMed PubMed Central
[47] Angel MO, Bonadio RC, Harada G, Waisberg F, Enrico D, Arrieta O, et al. Mentoring as an opportunity to improve research and cancer care in Latin America (AAZPIRE project). ESMO Open. 2020;5(6):e000988. 10.1136/esmoopen-2020-000988.Search in Google Scholar PubMed PubMed Central
[48] Dedeilia A, Sotiropoulos MG, Hanrahan JG, Janga D, Dedeilias P. Medical and surgical education challenges and innovations in the COVID-19 era: a systematic review. In Vivo. 2020;34(3_suppl):1603–11.10.21873/invivo.11950Search in Google Scholar PubMed PubMed Central
[49] Hui D, Paiva CE, Del Fabbro EG, Steer C, Naberhuis J, Fernández-Ortega P, et al. Prognostication in advanced cancer: update and directions for future research. Supportive Care Cancer. 2019;27(6):1973. 10.1007/s00520-019-04727-y.Search in Google Scholar PubMed PubMed Central
[50] Jatho A, Mugisha NM, Kafeero J, Holoya G, Okuku F, Niyonzima N, et al. Capacity building for cancer prevention and early detection in the Ugandan primary healthcare facilities: Working toward reducing the unmet needs of cancer control services. Cancer Med. 2021;10(2):745–56. 10.1002/cam4.3659.Search in Google Scholar PubMed PubMed Central
[51] O’Donovan J, Newcomb A, MacRae MC, Vieira D, Onyilofor C, Ginsburg O. Community health workers and early detection of breast cancer in low-income and middle-income countries: A systematic scoping review of the literature. BMJ Glob Health. 2020;5(5):e002466. 10.1136/bmjgh-2020-002466.Search in Google Scholar PubMed PubMed Central
[52] Pandya S, Hamal M, Abuya T, Kintu R, Mwanga D, Warren CE, et al. Understanding factors that support community health worker motivation, job satisfaction, and performance in three Ugandan districts: Opportunities for strengthening Uganda’s community health worker program. Int J Health Policy Manag. 2022;12(1):1–13. 10.34172/ijhpm.2022.6219.Search in Google Scholar PubMed PubMed Central
[53] Kok J, Smith R, Nkosi T, et al. Integration of telemedicine into healthcare systems in Rwanda: Enhancing access to oncologists and specialized treatments in remote areas. J Telemed Telecare. 2023;29(4):223–31. 10.1177/1357633X23100123.Search in Google Scholar
[54] Kok MO, Terra T, Tweheyo R, van der Hoeven M, Ponce MC, van Furth MT, et al. Using telehealth to support community health workers in Uganda during COVID-19: a mixed-method study. BMC Health Serv Res. 2023 Mar;23(1):284. 10.1186/s12913-023-09217-w. PMID: 36973681; PMCID: PMC10040915.Search in Google Scholar PubMed PubMed Central
[55] Omonisi AE, Liu B, Parkin DM. Population-based cancer registration in Sub-Saharan Africa: Its role in research and cancer control. JCO Glob Oncol. 2020;6:1721–8. 10.1200/GO.20.00294.Search in Google Scholar PubMed PubMed Central
[56] Nobile M. Advancing cancer control plans in Africa through South-South cooperation. International Atomic Energy Agency, Vienna, Austria. https://www.iaea.org/newscenter/news/advancing-cancer-control-plans-in-africa-through-south-south-cooperation.Search in Google Scholar
© 2025 the author(s), published by De Gruyter
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Research Articles
- Relationship between body mass index and quality of life, use of dietary and physical activity self-management strategies, and mental health in individuals with polycystic ovary syndrome
- Evaluating the challenges and opportunities for diabetes care policy in Nigeria
- Body mass index is associated with subjective workload and REM sleep timing in young healthy adults
- Prediction of hypoglycaemia in subjects with type 1 diabetes during physical activity
- Investigation by the Epworth Sleepiness Scale of daytime sleepiness in professional drivers during work hours
- Understanding public awareness of fall epidemiology in the United States: A national cross-sectional study
- Impact of Covid-19 stress on urban poor in Sylhet Division, Bangladesh: A perception-based assessment
- Impact of the COVID-19 pandemic on mental health, relationship satisfaction, and socioeconomic status: United States
- Psychological factors influencing oocyte donation: A study of Indian donors
- Cervical cancer in eastern Kenya (2018–2020): Impact of awareness and risk perception on screening practices
- Older LGBTQ+ and blockchain in healthcare: A value sensitive design perspective
- Trends and disparities in HPV vaccination among U.S. adolescents, 2018–2023
- Do cell towers help increase vaccine uptake? Evidence from Côte d’Ivoire
- In search of the world’s most popular painkiller: An infodemiological analysis of Google Trend statistics from 2004 to 2023
- Brain fog in chronic pain: A concept analysis of social media postings
- Association between multidimensional poverty intensity and maternal mortality ratio in Madagascar: Analysis of regional disparities
- A “disorder that exacerbates all other crises” or “a word we use to shut you up”? A critical policy analysis of NGOs’ discourses on COVID-19 misinformation
- Smartphone use and stroop performance in a university workforce: A survey-experiment
- Review Articles
- The management of body dysmorphic disorder in adolescents: A systematic literature review
- Navigating challenges and maximizing potential: Handling complications and constraints in minimally invasive surgery
- Examining the scarcity of oncology healthcare providers in cancer management: A case study of the Eastern Cape Province, South Africa
- Dietary strategies for irritable bowel syndrome: A narrative review of effectiveness, emerging dietary trends, and global variability
- The impact of intimate partner violence on victims’ work, health, and wellbeing in OECD countries (2014–2025): A descriptive systematic review
- Nutrition literacy in pregnant women: a systematic review
- Short Communications
- Experience of patients in Germany with the post-COVID-19 vaccination syndrome
- Five linguistic misrepresentations of Huntington’s disease
- Letter to the Editor
- PCOS self-management challenges transcend BMI: A call for equitable support strategies
Articles in the same Issue
- Research Articles
- Relationship between body mass index and quality of life, use of dietary and physical activity self-management strategies, and mental health in individuals with polycystic ovary syndrome
- Evaluating the challenges and opportunities for diabetes care policy in Nigeria
- Body mass index is associated with subjective workload and REM sleep timing in young healthy adults
- Prediction of hypoglycaemia in subjects with type 1 diabetes during physical activity
- Investigation by the Epworth Sleepiness Scale of daytime sleepiness in professional drivers during work hours
- Understanding public awareness of fall epidemiology in the United States: A national cross-sectional study
- Impact of Covid-19 stress on urban poor in Sylhet Division, Bangladesh: A perception-based assessment
- Impact of the COVID-19 pandemic on mental health, relationship satisfaction, and socioeconomic status: United States
- Psychological factors influencing oocyte donation: A study of Indian donors
- Cervical cancer in eastern Kenya (2018–2020): Impact of awareness and risk perception on screening practices
- Older LGBTQ+ and blockchain in healthcare: A value sensitive design perspective
- Trends and disparities in HPV vaccination among U.S. adolescents, 2018–2023
- Do cell towers help increase vaccine uptake? Evidence from Côte d’Ivoire
- In search of the world’s most popular painkiller: An infodemiological analysis of Google Trend statistics from 2004 to 2023
- Brain fog in chronic pain: A concept analysis of social media postings
- Association between multidimensional poverty intensity and maternal mortality ratio in Madagascar: Analysis of regional disparities
- A “disorder that exacerbates all other crises” or “a word we use to shut you up”? A critical policy analysis of NGOs’ discourses on COVID-19 misinformation
- Smartphone use and stroop performance in a university workforce: A survey-experiment
- Review Articles
- The management of body dysmorphic disorder in adolescents: A systematic literature review
- Navigating challenges and maximizing potential: Handling complications and constraints in minimally invasive surgery
- Examining the scarcity of oncology healthcare providers in cancer management: A case study of the Eastern Cape Province, South Africa
- Dietary strategies for irritable bowel syndrome: A narrative review of effectiveness, emerging dietary trends, and global variability
- The impact of intimate partner violence on victims’ work, health, and wellbeing in OECD countries (2014–2025): A descriptive systematic review
- Nutrition literacy in pregnant women: a systematic review
- Short Communications
- Experience of patients in Germany with the post-COVID-19 vaccination syndrome
- Five linguistic misrepresentations of Huntington’s disease
- Letter to the Editor
- PCOS self-management challenges transcend BMI: A call for equitable support strategies


