Abstract
Here we report a case of a 40-year-old man who visited the emergency room with severe chest pain. He showed a Stanford type B aortic dissection on chest-computed tomography. Despite medical treatment and malperfusion of lower extremities, acute renal failure developed; hence thoracic endovascular aortic repair (TEVAR) was considered under general anaesthesia. After endotracheal intubation, ventilation with low tidal volume required high inspiratory airway pressure. An arterial blood gas analysis showed PaCO2 of 61.8mmHg and PaO2 of 26.4mmHg, indicating a status asthmaticus of hypoxaemia and hypercarbia, which did not respond to bronchodilator or mechanical ventilation. Impending cardiac arrest was treated using venovenous extracorporeal life support, which was administered by percutaneous femoral cannulation. Surgical procedure was completed without any complications. Extracorporeal life support was weaned at one day after the operation. The patient was discharged without any complications.
1 Introduction
Status asthmaticus, a reversible respiratory failure, does not respond to conventional bronchodilator. It presents mild dyspnea to severe bronchospastic asphyxia with potential disaster during anaesthetic induction. It is usually developed during anaesthetic induction. However, it can be detected any time during perioperative period. Prompt recognition of this situation and appropriate management are very important to avoid morbidity and mortality [1]. Extracorporeal life support is characterized by drainage of venous blood, removal of carbon dioxide, adding oxygen in oxygenator, and returning blood by centrifugal pump. It is widely used for acute respiratory failure with pneumonia, acute respiratory distress syndrome (ARDS), bridge to lung transplantation, and primary graft dysfunction after lung transplantation [2]. A few cases of extracorporeal life support for severe status asthmaticus patient have been reported [3]. However, severe bronchospastic asphyxia during anaesthetic induction has not been reported yet.
2 Case report
A 40-year-old male (140kg, 165cm) patient was transferred to our emergency room with chest pain. He had hypertension, coronary artery disease, and bronchial asthma that were not treated. He visited the pulmonology department with exertional dyspnea one year before surgery. On pulmonary function test, he had mild obstructive airway disease and allergen skin prick test revealed bronchial asthma to specific allergen. On chest X-ray, there was no abnormal finding (Figure 1). Contrast-enhanced computed tomography scan revealed Stanford type B aortic dissection from descending thoracic aorta to iliac arteries (Figure 2). Despite medical treatment with labetalol (120mg/h) and nicardipine (2.5mg/h), lower limb ischaemia and acute renal failure developed due to malperfusion at HAD #2 (Figure 3). Urgent surgical intervention was needed. Thoracic endovascular aortic repair (TEVAR) followed. Before transferring him to the operating room, 0.2mg glycopyrrolate was injected intramuscularly. For anaesthetic induction, 2% propofol and remifentanyl were used. The patient was paralyzed with 50mg rocuronium. Anaesthesiologist had a difficult time in endotracheal intubation with poor laryngoscopic view. After endotracheal intubation, expiratory tidal volume was 100ml with high inspiratory airway pressure (70cmH2O). On arterial blood gas analysis after 100% oxygen inhalation, severe hypoxemia and respiratory acidosis were found (pH 7.198, PCO2 61.8mmHg, PaO2 26.4mmHg, O2 Saturation 36.1%). The anaesthesiologist performed flexible bronchoscopy. There was no endotracheal or endobronchial obstruction. Severe bronchospastic asphyxia was suspected and epinephrine 0.5 mg was given subcutaneously. Then 0.5ml albuterol of 0.5% formulation was inhaled into the endotracheal tube. Methylprednisolone (1mg/Kg) was also given intravenously. After conventional therapy for severe bronchospasm, his hypoxemia and respiratory acidosis were slightly improved (pH 7.264, PCO2 56.7mmHg, PaO2 43.2mmHg, O2 Saturation 71.3%). However, his blood pressure dropped down (systolic blood pressure<70mmHg) and bradycardia (40/min) developed. Conventional therapy was ineffective for him and cardiac arrest caused by persistent hypoxemia was impending. At 12 minutes after bronchospastic attack, emergent venovenous extracorporeal life support (VV ECLS) was initiated. A 21 French drainage cannula (Bio-Medicus™ Multi-Stage Femoral Venous Cannula, Medtronic, Minneapolis, MN, USA) was inserted into the right common femoral vein and advanced into right atrium. A 17 French return cannula (Bio-Medicus™Femoral Arterial Cannula, Medtronic, Minneapolis, MN, USA) was placed at the left external iliac vein. The anaesthesiologist already inserted central venous catheter into the right internal jugular vein. Only both groins were cleansed and draped for TEVAR. Therefore, we planned secondary cannulation via the right internal jugular vein if needed after emergency VV ECLS via femoral venous cannulation. All procedures were done percutaneously with fluoroscopic guidance (Figure 4). Quadrox oxygenator and rotaflow pump (Maquet, Hirrlingen, Germany) were connected to extracorporeal circuit. Extracorporeal circulatory blood flow rate was 4.5L/min. Peripheral O2 saturation raised up to 80%. He was stabilized haemodynamically. We changed the mode of mechanical ventilation from volume controlled to pressure controlled ventilation. Limitation of inspiratory airway pressure was 40cmH2O. Expiratory tidal volume was less than 70ml. After VV ECLS, hypoxemia and hypercarbia were improved on arterial blood gas analysis (pH 7.305, PCO2 49.6mmHg, PaO2 56.2 mmHg, O2 Saturation 86.2%). Intimal tearing portion of thoracic aorta was sealed with stent graft (Valiant thoracic stent graft with the Captiva delivery system, Medtronic) on VV ECLS. The patient was transferred to intensive care unit after surgery without any problem. Bronchodilator was used for inhalation every 4 hours. After 12 hours after VV ECLS, his expiratory tidal volume was increased up to 450ml with appropriate inspiratory airway pressure (less than 40cmH2O). VV ECLS was weaned at POD#1 and decannulation was done without haemorrhagic complication. Patient could be weaned from mechanical ventilator and extubated at POD#2. He could be discharged at POD#7 without any respiratory or cognitive dysfunction. Malperfusions of left kidney and left iliac artery were resolved and there was no abnormal finding of lung parenchyma and pulmonary vessels on contrast-enhanced computed tomography scan at POD#14 (Figure 5). The patient has been treated with a bronchodilator at the Pulmonology Department. He has no more episode of bronchospastic asphyxia.

Preoperative chest X-ray without abnormal finding

Contrast-enhanced computed tomography scan showing Stanford type B aortic dissection.

Contrast-enhanced computed tomography scan showing malperfusions of left kidney (white arrow) and left iliac artery (blue arrow)
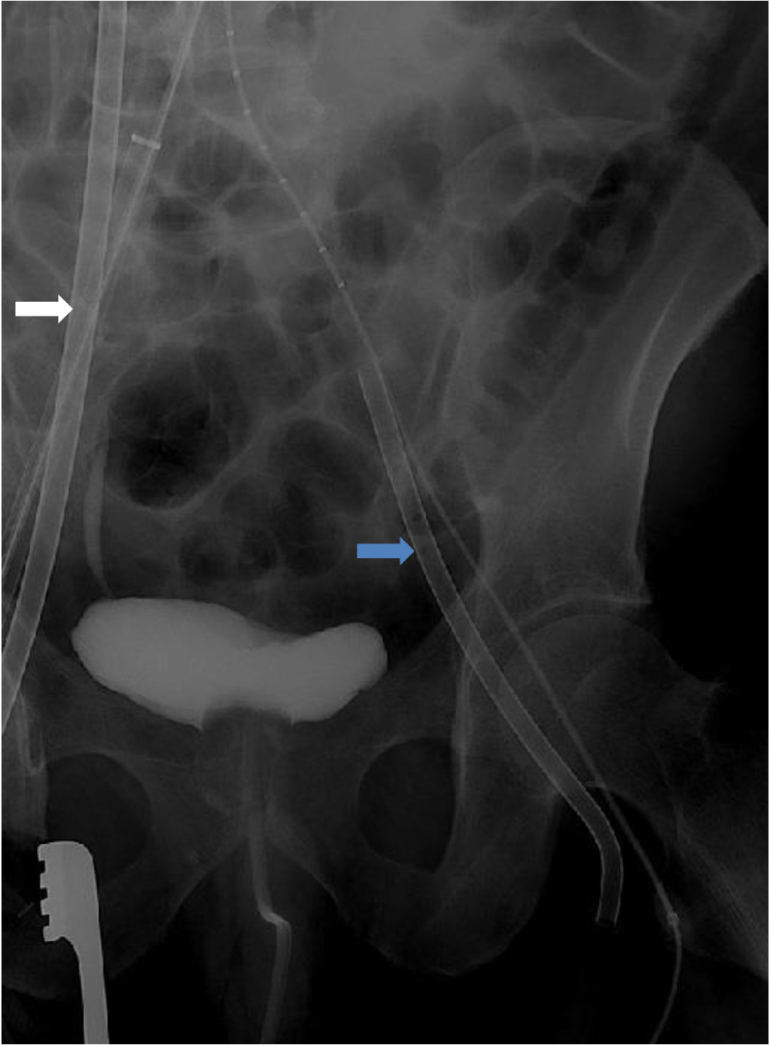
Venous cannulations for extracorporeal life support under fluoroscopic guidance. A 21 French venous cannula was inserted into the right common femoral vein for venous drainage (white arrow). A 17 French arterial cannula was inserted into the left common femoral vein for return (blue arrow).

Malperfusions of left kidney and left iliac artery were resolved after operation at POD#14.
Ethical approval
The research related to human use has been complied with all the relevant national regulations, institutional policies and in accordance the tenets of the Helsinki Declaration, and has been approved by the authors’ institutional review board or equivalent committee.
Informed consent
Informed consent has been obtained from all individuals included in this study.
3 Discusion
Acute asthma is characterized by spasm of bronchial muscle, edema of bronchial wall, and increase of mucosal secretion. The goal of therapy for acute attack is to reverse obstructed airflow [4]. Bronchospasm is a severely exacerbated form of acute asthma. This usually leads to anaesthetic disaster. Such disaster encountered during anaesthetic induction period might involve IgE mediated anaphylaxis or nonallergic mechanism triggered by pharmacological and mechanical factors. A total of 4,000 bronchospasm events were reported in Australia, including 103 cases during the perioperative period. It might be triggered by pharmacological or mechanical stimulus [1]. A nonallergic mechanism (79%) is more frequently involved than an allergic mechanism. Among these nonallergic cases, most (44%) events occurred during the induction of anaesthesia [5]. In pharmacological factors, succinylcholine-induced anaphylaxis is the most common etiology. Cardiovascular shock is the hallmark of severe IgE mediated anaphylaxis. This sign might be associated with bronchospasm in 19-40% of patients with asthma or chronic obstructive pulmonary disease [6]. Perioperative bronchospasm commonly occurs during or after endotracheal instrumentation. Endotracheal tube is the irritant for well-innervated upper airway. It increases airway responsiveness [5]. Subcutaneously injection of epinephrine and inhalation of bronchodilator such as albuterol can be effective for rapid control of bronchospasm. Theophylline can increase intracellular cyclic adenosine monophosphate (cAMP) level, resulting in relaxation of bronchial smooth muscle. Corticosteroid can decrease inflammation of bronchial wall. Short-term therapy of corticosteroid is recommended when patient does not respond to bronchodilator therapy. However, its therapeutic effect will occur after 6 to 12 h. Inhalation of halothane as an anaesthetic agent is useful for bronchodilating effect. But, it has adverse effects such as increasing myocardial sensitization and cerebrospinal fluid pressure. Therefore, it is not commonly used. Despite these therapies, severe asthma attack can cause morbidity and mortality during anaesthesia. For hypoxic brain damage and death during anaesthesia, respiratory events accounted for 28% of claims in the United States [7]. Extracorporeal life support could promptly restore gas oxygenation, resolve respiratory acidosis, and avoid haemodynamic deterioration. Excellent CO2 removal, oxygenation, and rapid correction of respiratory acidosis for severe refractory asthma attack not responding to conventional therapy could be achieved by using extracorporeal life support. This could decrease intrinsic positive end expiratory pressure (PEEP) and prevent haemodynamic collapse and ventilator induced lung injury [3]. A total of 1,257 adult respiratory failure extracorporeal life support cases were reported to the international Extracorporeal Life Support Organization (ELSO) registry between January 1986 and September 2006. Asthma was the primary indication in 24 patients. They were treated by extracorporeal life support. Mean hours for mechanical ventilation until initiation of extracorporeal life support is 65.2±67.7h. Despite mechanical ventilation due to respiratory failure, mean pH is 7.17±0.16 mmHg, PaCO2 is 119±58.1mmHg, and PaO2/FiO2 ratio is 244±180 before administration of extracorporeal life support. Extracorporeal life support was provided 111.9±71.2h and 83.3% of patients survived. Despite venoarterial extracorporeal life support (VA ECLS) was performed for only one because most cases were haemodynamically stable, mechanical, cardiovascular, and haemorrhagic complications developed in 19 (79.2%) patients [8]. In the current case, cardiac arrest impended due to hypoxemia and respiratory acidosis. We could not perform VA ECLS because cannulation into femoral artery could be dangerous. It might potentially aggravate aortic dissection in the patient. However, early administration of VV ECLS could correct hypoxemia and respiratory acidosis rapidly and haemodynamic stability could be achieved soon. Sudden resolution of severe asthma attack could occur after several days of pharmacologic therapy in some observational studies. However, we could not predict the exact time to recovery. Nevertheless, extracorporeal life support remains a reasonable therapy for treating adults with severe respiratory failure from status asthmaticus.
4 Conclusion
An obese patient with asthma developed severe status asthmaticus after endotracheal intubation. High oxygen mechanical ventilation, bronchodilator, or conventional medication including epinephrine was not effective. Early VV ECLS was initiated. The patient promptly recovered from hypoxemia. He was kept stable haemodynamically. To the best of our knowledge, this is the first case report of a patient with impending cardiac arrest from severe asthmatic attack during anaesthesia who is successfully treated by VV ECLS. This case shows the effectiveness of VV ECLS for an acute, severe, and refractory status asthmaticus patient not responsive to mechanical ventilation or conventional therapy during anaesthesia. Therefore, early administration of VV ECLS can prevent haemodynamic instability, reduce complication, and optimize patient’s outcome.
Acknowledgement
This work was supported by Soonchunhyang University Research Fund.
Conflict of interest
Conflict of interest statement: Authors state no conflict of interest
References
[1] Dewachter P, Mouton-Faivre C, Emala CW, et al. Case Scenario: Bronchospasm during Anesthetic induction. Anesthesiology 2011;114:1200-121010.1097/ALN.0b013e3182172cd3Search in Google Scholar PubMed
[2] Zapol WM, Snider MT, Hill JD, et al. Extracorporeal membrane oxygenation in severe acute respiratory failure. A randomized prospective study. JAMA 1979; 242:2193-219610.1001/jama.1979.03300200023016Search in Google Scholar
[3] Mikkelsen ME, Pugh ME, Hansen-Flaschen JH, et al. Emergency Extracorporeal Life Support for Asphyxic Status Asthmaticus. Respiratory Care 2007;52:1525-1529Search in Google Scholar
[4] Robin E, Lewiston N. Unexpected, unexplained sudden death in young asthmatic subjects. Chest 1989;96:790-79310.1378/chest.96.4.790Search in Google Scholar PubMed
[5] Westhorpe RN, Ludbrook GL, Helps SC. Crisis management during anesthesia: Bronchospasm. Qual Saf Health Care 2005;14:e710.1136/qshc.2002.004457Search in Google Scholar PubMed PubMed Central
[6] Dewachter P, Mouton-Faivre C, Emala CW. Anaphylaxis and anesthesia: Controversies and new insights. Anesthesiology 2009;111:1141-115010.1097/ALN.0b013e3181bbd443Search in Google Scholar PubMed
[7] Cheney FW, Posner KL, Lee LA, et al. Trends in anesthesia-related death and brain damage: A closed claims analysis. Anesthesiology 2006;105:1081-108610.1097/00000542-200612000-00007Search in Google Scholar PubMed
[8] Mikkelsen ME, Woo YJ, Sager JS, et al. Outcomes using extracorporeal life support for adult respiratory failure due to status asthmaticus. ASAIO J 2009;55:47-5210.1097/MAT.0b013e3181901ea5Search in Google Scholar PubMed PubMed Central
© 2018 Won Ho Chang, published by De Gruyter
This work is licensed under the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 License.
Articles in the same Issue
- Regular Articles
- Cleidocranial dysplasia-dental disorder treatment and audiology diagnosis
- A hybrid neural network – world cup optimization algorithm for melanoma detection
- Early administration of venovenous extracorporeal life support for status asthmaticus during anaesthetic induction: case report and literature review
- Assessment of maximal isometric hand grip strength in school-aged children
- Evaluation of a neurokinin-1 antagonist in preventing multiple-day cisplatin-induced nausea and vomiting
- Value of continuous video EEG and EEG responses to thermesthesia stimulation in prognosis evaluation of comatose patients after cardiopulmonary resuscitation
- Platelet-rich plasma protects HUVECs against oX-LDL-induced injury
- Pharmacoeconomics of three therapeutic schemes for anti-tuberculosis therapy induced liver injury in China
- Small-cell lung cancer presenting as fatal pulmonary hemorrhage
- Correlation of retinopathy of prematurity with bronchopulmonary dysplasia
- Prognosis of treatment outcomes by cognitive and physical scales
- The efficacy of radiofrequency hyperthermia combined with chemotherapy in the treatment of advanced ovarian cancer
- Arcuate Fasciculus in Autism Spectrum Disorder Toddlers with Language Regression
- Aesthetic dental procedures: legal and medico-legal implications
- Blood transfusion in children: the refusal of Jehovah’s Witness parents’
- Burnout among anesthetists and intensive care physicians
- Relationship of HS CRP and sacroiliac joint inflammation in undifferentiated spondyloarthritis
- Ethical and legal issues in gestational surrogacy
- Effects of arginine vasopressin on migration and respiratory burst activity in human leukocytes
- Associations of diabetic retinopathy with retinal neurodegeneration on the background of diabetes mellitus. Overview of recent medical studies with an assessment of the impact on healthcare systems
- Pituitary dysfunction from an unruptured ophthalmic internal carotid artery aneurysm with improved 2-year follow-up results: A case report
- Effectiveness of treatment with endostatin in combination with emcitabine, carboplatin, and gemcitabine in patients with advanced non-small cell lung cancer: a retrospective study
- Piercing and tattoos in adolescents: legal and medico-legal implications
- The central importance of information in cosmetic surgery and treatments
- Penile calciphylaxis in a patient with end-stage renal disease: a case report and review of the literature
- Serum CA72-4 as a biomarker in the diagnosis of colorectal cancer: A meta-analysis
- Association between uric acid and metabolic syndrome in elderly women
- Distinct expression and prognostic value of MS4A in gastric cancer
- MAPK pathway involved in epidermal terminal differentiation of normal human epidermal keratinocytes
- Association of central obesity with sex hormonebinding globulin: a cross-sectional study of 1166 Chinese men
- Successful endovascular therapy in an elderly patient with severe hemorrhage caused by traumatic injury
- Inflammatory biomarkers and risk of atherosclerotic cardiovascular disease
- Related factors of early mortality in young adults with cerebral hemorrhage
- Growth suppression of glioma cells using HDAC6 inhibitor, tubacin
- Post-stroke upper limb spasticity incidence for different cerebral infarction site
- The esophageal manometry with gas-perfused catheters
- MMP-2 and TIMP-2 in patients with heart failure and chronic kidney disease
- Genetic testing: ethical aspects
- Intervention for physician burnout: A systematic review
- The melanin-concentrating hormone system in human, rodent and avian brain
- Clinical effects of piribedil in adjuvant treatment of Parkinson’s Disease: A meta-analysis
- Identification of a novel BRAF Thr599dup mutation in lung adenocarcinoma
- Adrenal incidentaloma – diagnostic and treating problem – own experience
- Common illnesses in tropical Asia and significance of medical volunteering
- Genetic risk in insurance field
- Genetic testing and professional responsibility: the italian experience
- The mechanism of mitral regurgitant jets identified by 3-dimensional transesophageal echocardiography
- Control of blood pressure and cardiovascular outcomes in type 2 diabetes
- Pseudomesotheliomatous primary squamous cell lung carcinoma: The first case reported in Turkey and a review of the literature
- Diagnostic efficacy of serum 1,3-β-D-glucan for invasive fungal infection: An update meta-analysis based on 37 case or cohort studies
- GPER was associated with hypertension in post-menopausal women
- Metabolic activity of sulfate-reducing bacteria from rodents with colitis
- Association of miRNA122 & ADAM17 with lipids among hypertensives in Nigeria
- The efficacy and safety of enoxaparin: a meta-analysis
- Cuffed versus uncuffed endotracheal tubes in pediatrics: a meta-analysis
- Thresholding for medical image segmentation for cancer using fuzzy entropy with level set algorithm
- Sleep deprivation in Intensive Care Unit – systematic review
- Benefits of computed tomography in reducing mortality in emergency medicine
- Ipragliflozin ameliorates liver damage in non-alcoholic fatty liver disease
- Limits of professional competency in nurses working in Nicu
- MDA-19 suppresses progression of melanoma via inhibiting the PI3K/Akt pathway
- The effect of smoking on posttraumatic pseudoarthrosis healing after internal stabilization, treated with platelet rich plasma (PRP)
- Partial deletion of the long arm of chromosome 7: a case report
- Meta-analysis of PET/CT detect lymph nodes metastases of cervical cancer
- High Expression of NLRC5 is associated with prognosis of gastric cancer
- Is monitoring mean platelet volume necessary in breast cancer patients?
- Resectable single hepatic epithelioid hemangioendothelioma in the left lobe of the liver: a case report
- Epidemiological study of carbapenem-resistant Klebsiella pneumoniae
- The CCR5-Delta32 genetic polymorphism and HIV-1 infection susceptibility: a meta-analysis
- Phenotypic and molecular characterisation of Staphylococcus aureus with reduced vancomycin susceptibility derivated in vitro
- Preliminary results of Highly Injectable Bi-Phasic Bone Substitute (CERAMENT) in the treatment of benign bone tumors and tumor-like lesions
- Analysis of patient satisfaction with emergency medical services
- Guillain-Barré syndrome and Low back pain: two cases and literature review
- HELLP syndrome complicated by pulmonary edema: a case report
- Pharmacokinetics of vancomycin in patients with different renal function levels
- Recurrent chronic subdural hematoma: Report of 13 cases
- Is awareness enough to bring patients to colorectal screening?
- Serum tumor marker carbohydrate antigen 125 levels and carotid atherosclerosis in patients with coronary artery disease
- Plastic treatment for giant pseudocyst after incisional hernia mesh repair: a case report and comprehensive literature review
- High expression levels of fascin-1 protein in human gliomas and its clinical relevance
- Thromboembolic complications following tissue plasminogen activator therapy in patients of acute ischemic stroke - Case report and possibility for detection of cardiac thrombi
- The effects of gastrointestinal function on the incidence of ventilator-associated pneumonia in critically ill patients
- A report of chronic intestinal pseudo-obstruction related to systemic lupus erythematosus
- Risk model in women with ovarian cancer without mutations
- Direct oral anticoagulants and travel-related venous thromboembolism
- How bispectral index compares to spectral entropy of the EEG and A-line ARX index in the same patient
- Henoch-schonlein purpura nephritis with renal interstitial lesions
- Cardiovascular risk estimated by UKPDS risk engine algorithm in diabetes
- CD5 and CD43 expression are associate with poor prognosis in DLBCL patients
- Combination of novoseven and feiba in hemophiliac patients with inhibitors
Articles in the same Issue
- Regular Articles
- Cleidocranial dysplasia-dental disorder treatment and audiology diagnosis
- A hybrid neural network – world cup optimization algorithm for melanoma detection
- Early administration of venovenous extracorporeal life support for status asthmaticus during anaesthetic induction: case report and literature review
- Assessment of maximal isometric hand grip strength in school-aged children
- Evaluation of a neurokinin-1 antagonist in preventing multiple-day cisplatin-induced nausea and vomiting
- Value of continuous video EEG and EEG responses to thermesthesia stimulation in prognosis evaluation of comatose patients after cardiopulmonary resuscitation
- Platelet-rich plasma protects HUVECs against oX-LDL-induced injury
- Pharmacoeconomics of three therapeutic schemes for anti-tuberculosis therapy induced liver injury in China
- Small-cell lung cancer presenting as fatal pulmonary hemorrhage
- Correlation of retinopathy of prematurity with bronchopulmonary dysplasia
- Prognosis of treatment outcomes by cognitive and physical scales
- The efficacy of radiofrequency hyperthermia combined with chemotherapy in the treatment of advanced ovarian cancer
- Arcuate Fasciculus in Autism Spectrum Disorder Toddlers with Language Regression
- Aesthetic dental procedures: legal and medico-legal implications
- Blood transfusion in children: the refusal of Jehovah’s Witness parents’
- Burnout among anesthetists and intensive care physicians
- Relationship of HS CRP and sacroiliac joint inflammation in undifferentiated spondyloarthritis
- Ethical and legal issues in gestational surrogacy
- Effects of arginine vasopressin on migration and respiratory burst activity in human leukocytes
- Associations of diabetic retinopathy with retinal neurodegeneration on the background of diabetes mellitus. Overview of recent medical studies with an assessment of the impact on healthcare systems
- Pituitary dysfunction from an unruptured ophthalmic internal carotid artery aneurysm with improved 2-year follow-up results: A case report
- Effectiveness of treatment with endostatin in combination with emcitabine, carboplatin, and gemcitabine in patients with advanced non-small cell lung cancer: a retrospective study
- Piercing and tattoos in adolescents: legal and medico-legal implications
- The central importance of information in cosmetic surgery and treatments
- Penile calciphylaxis in a patient with end-stage renal disease: a case report and review of the literature
- Serum CA72-4 as a biomarker in the diagnosis of colorectal cancer: A meta-analysis
- Association between uric acid and metabolic syndrome in elderly women
- Distinct expression and prognostic value of MS4A in gastric cancer
- MAPK pathway involved in epidermal terminal differentiation of normal human epidermal keratinocytes
- Association of central obesity with sex hormonebinding globulin: a cross-sectional study of 1166 Chinese men
- Successful endovascular therapy in an elderly patient with severe hemorrhage caused by traumatic injury
- Inflammatory biomarkers and risk of atherosclerotic cardiovascular disease
- Related factors of early mortality in young adults with cerebral hemorrhage
- Growth suppression of glioma cells using HDAC6 inhibitor, tubacin
- Post-stroke upper limb spasticity incidence for different cerebral infarction site
- The esophageal manometry with gas-perfused catheters
- MMP-2 and TIMP-2 in patients with heart failure and chronic kidney disease
- Genetic testing: ethical aspects
- Intervention for physician burnout: A systematic review
- The melanin-concentrating hormone system in human, rodent and avian brain
- Clinical effects of piribedil in adjuvant treatment of Parkinson’s Disease: A meta-analysis
- Identification of a novel BRAF Thr599dup mutation in lung adenocarcinoma
- Adrenal incidentaloma – diagnostic and treating problem – own experience
- Common illnesses in tropical Asia and significance of medical volunteering
- Genetic risk in insurance field
- Genetic testing and professional responsibility: the italian experience
- The mechanism of mitral regurgitant jets identified by 3-dimensional transesophageal echocardiography
- Control of blood pressure and cardiovascular outcomes in type 2 diabetes
- Pseudomesotheliomatous primary squamous cell lung carcinoma: The first case reported in Turkey and a review of the literature
- Diagnostic efficacy of serum 1,3-β-D-glucan for invasive fungal infection: An update meta-analysis based on 37 case or cohort studies
- GPER was associated with hypertension in post-menopausal women
- Metabolic activity of sulfate-reducing bacteria from rodents with colitis
- Association of miRNA122 & ADAM17 with lipids among hypertensives in Nigeria
- The efficacy and safety of enoxaparin: a meta-analysis
- Cuffed versus uncuffed endotracheal tubes in pediatrics: a meta-analysis
- Thresholding for medical image segmentation for cancer using fuzzy entropy with level set algorithm
- Sleep deprivation in Intensive Care Unit – systematic review
- Benefits of computed tomography in reducing mortality in emergency medicine
- Ipragliflozin ameliorates liver damage in non-alcoholic fatty liver disease
- Limits of professional competency in nurses working in Nicu
- MDA-19 suppresses progression of melanoma via inhibiting the PI3K/Akt pathway
- The effect of smoking on posttraumatic pseudoarthrosis healing after internal stabilization, treated with platelet rich plasma (PRP)
- Partial deletion of the long arm of chromosome 7: a case report
- Meta-analysis of PET/CT detect lymph nodes metastases of cervical cancer
- High Expression of NLRC5 is associated with prognosis of gastric cancer
- Is monitoring mean platelet volume necessary in breast cancer patients?
- Resectable single hepatic epithelioid hemangioendothelioma in the left lobe of the liver: a case report
- Epidemiological study of carbapenem-resistant Klebsiella pneumoniae
- The CCR5-Delta32 genetic polymorphism and HIV-1 infection susceptibility: a meta-analysis
- Phenotypic and molecular characterisation of Staphylococcus aureus with reduced vancomycin susceptibility derivated in vitro
- Preliminary results of Highly Injectable Bi-Phasic Bone Substitute (CERAMENT) in the treatment of benign bone tumors and tumor-like lesions
- Analysis of patient satisfaction with emergency medical services
- Guillain-Barré syndrome and Low back pain: two cases and literature review
- HELLP syndrome complicated by pulmonary edema: a case report
- Pharmacokinetics of vancomycin in patients with different renal function levels
- Recurrent chronic subdural hematoma: Report of 13 cases
- Is awareness enough to bring patients to colorectal screening?
- Serum tumor marker carbohydrate antigen 125 levels and carotid atherosclerosis in patients with coronary artery disease
- Plastic treatment for giant pseudocyst after incisional hernia mesh repair: a case report and comprehensive literature review
- High expression levels of fascin-1 protein in human gliomas and its clinical relevance
- Thromboembolic complications following tissue plasminogen activator therapy in patients of acute ischemic stroke - Case report and possibility for detection of cardiac thrombi
- The effects of gastrointestinal function on the incidence of ventilator-associated pneumonia in critically ill patients
- A report of chronic intestinal pseudo-obstruction related to systemic lupus erythematosus
- Risk model in women with ovarian cancer without mutations
- Direct oral anticoagulants and travel-related venous thromboembolism
- How bispectral index compares to spectral entropy of the EEG and A-line ARX index in the same patient
- Henoch-schonlein purpura nephritis with renal interstitial lesions
- Cardiovascular risk estimated by UKPDS risk engine algorithm in diabetes
- CD5 and CD43 expression are associate with poor prognosis in DLBCL patients
- Combination of novoseven and feiba in hemophiliac patients with inhibitors

