Abstract
Although laboratory tests are the most used diagnostic investigations for screening, diagnosing, prognosticating and therapeutic monitoring of most human diseases, laboratory medicine is currently seen as many other economic industries by some policymakers and administrators, and is hence subjected to scale economy and assessed accordingly, despite the incremental clinical value that laboratory tests can generate. According to a genuine economic perspective, the impact of diagnostic testing on a healthcare budget is lower than 2.5%, whilst its profitability is over 100%, a net profit margin over 7-fold larger than whatever other human industry. Even more importantly, the impact of laboratory tests on clinical outcomes is now clear and virtually incontestable, as their use will improve clinical pathways much more than any other diagnostic investigations. The many ongoing attempts to downsize the importance of laboratory medicine as costs centers, or even the concept that public laboratory services can be safely eliminated or outsourced to external private professional organizations, shall hence be challenged. Laboratory medicine not only is vital to patient care and patient flow, and will remain so for many years to come, but is also a valuable economical resource for the healthcare facilities.
Laboratory diagnostics is one of the most used diagnostic areas for screening, diagnosing, prognosticating and therapeutic monitoring of most human diseases. As is broadly acknowledged, the use of laboratory tests within clinical decision-making is much larger than that of any other diagnostic discipline. In a recent study published by Ngo and colleagues, for example, it was shown that 38% of patients living in a large geographic area of the US (Richmond, VA, USA, approximately 802,000 inhabitants) underwent laboratory testing, a much higher rate than in those who underwent radiological (22%) or cardiological (5%) examinations [1]. It was also emphasized that the vast majority of hospitalized patients (98%) had been subjected to at least one laboratory test, a percentage decreasing to 56% in those admitted to the emergency department and to 29% in outpatients. These important figures, which unquestionably confirm the essential role of laboratory diagnostics in the managed care, leads to some reflections on the current cost, profitability and value of in vitro diagnostics from the perspective of a hospital laboratory.
According to the English online Oxford Dictionary, cost, profitability and value are respectively defined as “the amount that needs to be paid to buy or obtain something”, “the degree to which a business or activity yields profit or financial gain” and “the importance, worth, or usefulness of something”. Translating these definitions within the context of laboratory diagnostics, the term cost underlies the real (overall) expenditure which is necessary to generate a laboratory test result (thus including costs for sample collection, transportation, preparation, analysis and result transmission). The term profitability, generally expressed in percentage as incremental revenue over costs, can instead be seen as the economic gain that the generation of a laboratory test grants to the provider. Finally, the term value consists in the clinical advantages (usually expressed as qualitative and quantitative improvement of outcomes) that the production of a laboratory test result has within a specific clinical pathway.
Albeit it may appear paradoxical, or even illogical and unreasonable, laboratory diagnostics is currently seen as many other economic industries by some policymakers and administrators, and is hence subjected to scale economy and assessed accordingly, despite the incremental clinical value that laboratory tests can generate [2]. However, even in this weird perspective, nothing is what it seems. Regarding the overall impact of diagnostic testing on the healthcare economy, recent evidence attests that in vitro diagnostic testing accounts for less than 2.5% of the total healthcare expenditures in many countries worldwide [3]. A recent cost-analysis carried out in an Italian healthcare facility, defined on the basis of the local diagnosis related groups (DRGs) and laboratory test reimbursement tariffs, has generated rather similar numbers, wherein the total annual cost of managing the hospital has been estimated at €606.5 million in the year 2017. The overall annual expenditure of the local laboratory, thus including reagents, wages of personnel, rental fees, maintenance, service costs, investments/depreciation as well as overhead expenditures (e.g. accounting, informational technology services) has been estimated at €10.6 million during the same year, thus impacting with a very modest 1.75% on the total hospital budget. This figure is very similar to that reported by Rohr et al., who estimated that approximately 1.4% of public healthcare expenditure is used for laboratory diagnostics in Germany [3]. Regarding profitability, the hospital revenue in 2017 has been estimated at €607.2 million (i.e. net profit of ~0.1%), whilst that of the local laboratory (i.e. considering direct payments of patients and insurances and public/tax support by governments or owners of the hospital) has been estimated at €21.7 million (i.e. net profit 104%) (Figure 1). Irrespective of the fact that the net profit of laboratory diagnostics is hence 4 orders of magnitude higher than that of the entire facility, this net profit margin is also over 7-fold larger than whatever other human industry [4]. Notably, these estimates only apply to the Italian economic scenario, so that it may be challenging to calculate the revenue in other settings, where the laboratory is not directly reimbursed but receives a share of a flat charge paid to the hospital.
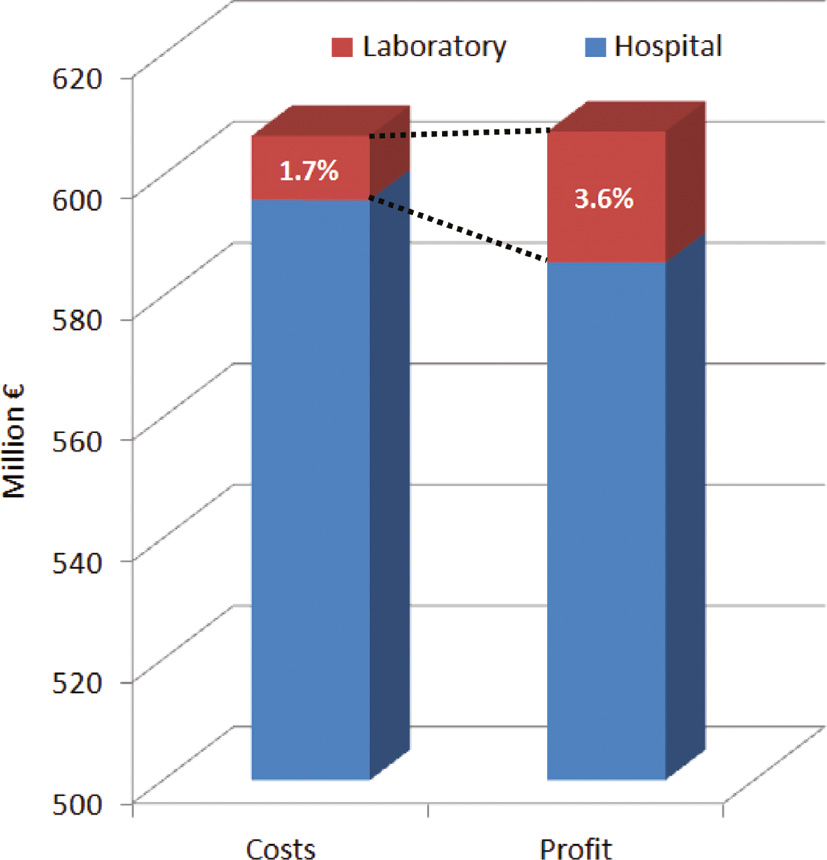
Costs and net profit of a general hospital and of its clinical laboratory.
The question is that little data are available in the literature based on an effective activity-based costing analysis and, in particular, no information has been published that effective cost-saving can be secured by only increasing test volumes. On the contrary, the relationship between volumes and costs is more multifaceted. Several variables impact on the final cost per test, especially for complex analyses. Even the distribution of prices paid per test in the same country varies widely, with the 95th percentile price exceeding the 5th percentile by an average factor of 10 in the USA [5]. Therefore, perceiving clinical laboratories as cost centers is not only misleading, but also somehow masochistic for both hospitals and healthcare systems.
Taking then a step forward out of the economical context, the impact of laboratory tests on improving clinical outcomes is now clear and virtually incontestable. A long debate has been raging on the real contribution of laboratory tests to patient care. Earliest claims have been published in the mid-1990s that nearly 60–70% of all critical medical decisions are somehow influenced by results of in vitro diagnostic testing [2]. Whilst intuitively straightforward, this concept has, however, been later disputed. The main reason behind this is that solid evidence on these figures was mostly lacking at that time and, especially, widespread generalization of this notion to all human pathologies is perhaps inappropriate [6]. The clinical setting is also problematic in itself. There are some circumstances in which the use of laboratory test results is virtually irreplaceable, such as for diagnosing non-ST elevation myocardial infarction (NSTEMI) [7] or monogenetic diseases [8]. Unlike these conditions, the contribution of diagnostic testing to the managed care of some other pathologies remains occasionally marginal such as, for example, for diagnosing spontaneous intracerebral hemorrhage [9]. Appropriateness is another immense drawback, which profoundly influence clinicians’ perception about the clinical significance of laboratory tests. The right test, with the right timing, to the right patient, at the right cost and for the right clinical purpose (i.e. the so-called “five R” paradigm) [10] will have a substantial impact on the clinical decision-making, whilst whenever these mainstream criteria cannot be thoughtfully fulfilled, the clinical usefulness of the same test will dramatically decrease. Irrespective of these considerations, no doubts remain that laboratory diagnostics contributes to improve clinical pathways much more than any other diagnostic area [1], [4].
In conclusion, the analysis of cost, profitability and value of in vitro diagnostic testing unquestionably attests that laboratory medicine should be regarded as an irreplaceable resource for modern healthcare systems. The many ongoing attempts to downsize the importance of laboratory medicine as costs centers, or even the concept that public laboratory services can be safely eliminated or outsourced to private external private diagnostic factories, often located far from the hospitals, must be compellingly challenged. We strongly believe that laboratory medicine not only is vital to patient care and patient flow, and will remain so for many years to come, but is also a valuable economical resource for the healthcare facilities, even without considering the paramount “profit” attributable to better outcomes for early/improved diagnosis. In this perspective, further studies shall be planned to investigate the monetary value of better/longer/healthier life attributable to high quality laboratory services. In essence, laboratory medicine is much more than just reporting numbers, and medical consultation by laboratory specialists provides added value throughout each step of the managed care [4], [11], [12].
Author contributions: All the authors have accepted responsibility for the entire content of this submitted manuscript and approved submission.
Research funding: None declared.
Employment or leadership: None declared.
Honorarium: None declared.
Competing interests: The funding organization(s) played no role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the report for publication.
References
1. Ngo A, Gandhi P, Miller WG. Frequency that laboratory tests influence medical decisions. J Appl Lab Med 2017;1:410–4.10.1373/jalm.2016.021634Suche in Google Scholar PubMed
2. Forsman RW. Why is the laboratory an afterthought for managed care organizations? Clin Chem 1996;42:813–6.10.1093/clinchem/42.5.813Suche in Google Scholar
3. Rohr U-P, Binder C, Dieterle T, Giusti F, Messina CG, Toerien E, et al. The value of in vitro diagnostic testing in medical practice: a status report. PLoS One 2016;11:e0149856.10.1371/journal.pone.0149856Suche in Google Scholar PubMed PubMed Central
4. Lippi G, Plebani M. The add value of laboratory diagnostics: the many reasons why decision-makers should actually care. J Lab Precis Med 2017;2:100.10.21037/jlpm.2017.12.07Suche in Google Scholar
5. Plebani M. Bigger is not always better. Diagnosis 2018;5: 41–6.10.1515/dx-2018-0019Suche in Google Scholar PubMed
6. Hallworth MJ. The “70% claim”: what is the evidence base? Ann Clin Biochem 2011;48:487–8.10.1258/acb.2011.011177Suche in Google Scholar PubMed
7. Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, et al. Fourth universal definition of myocardial infarction. J Am Coll Cardiol 2018;72:2231–64.10.1016/j.jacc.2018.08.1038Suche in Google Scholar PubMed
8. Ozgüç M. Genetic testing: predictive value of genotyping for diagnosis and management of disease. EPMA J 2011;2:173–9.10.1007/s13167-011-0077-ySuche in Google Scholar PubMed PubMed Central
9. Naidech AM. Diagnosis and management of spontaneous intracerebral hemorrhage. Continuum (Minneap Minn) 2015;21:1288–98.10.1212/CON.0000000000000222Suche in Google Scholar PubMed
10. Plebani M. Towards a new paradigm in laboratory medicine: the five rights. Clin Chem Lab Med 2016;54:1881–91.10.1515/cclm-2016-0848Suche in Google Scholar PubMed
11. Plebani M, Lippi G. Closing the brain-to-brain loop in laboratory testing. Clin Chem Lab Med 2011;49:1131–3.10.1515/CCLM.2011.617Suche in Google Scholar PubMed
12. Plebani M, Laposata M, Lippi G. A manifesto for the future of laboratory medicine professionals. Clin Chim Acta 2019;489:49–52.10.1016/j.cca.2018.11.021Suche in Google Scholar PubMed
©2019 Walter de Gruyter GmbH, Berlin/Boston
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Artikel in diesem Heft
- Frontmatter
- Opinion Paper
- Cost, profitability and value of laboratory diagnostics: in God we trust, all others bring data
- Review
- Interleukin-13 in the pathogenesis of pulmonary artery hypertension
- Infectiology and Microbiology
- Prospective evaluation study on the benefit of the simultaneous detection of seven sexually transmitted pathogens for the clinical management of patients suffering from sexually transmitted diseases
- Prevalence and genotyping of Helicobacter pylori in endoscopic biopsy samples from a Chinese population
- Original Articles
- Retinol-binding protein 4 better correlates with metabolic syndrome than cystatin C
- Effect of age and gender differences on high-sensitive troponin T measurement in the diagnosis of acute myocardial infarction
- Laboratory Case Report
- False high testosterone of unknown reason in a clinically inconspicuous female
Artikel in diesem Heft
- Frontmatter
- Opinion Paper
- Cost, profitability and value of laboratory diagnostics: in God we trust, all others bring data
- Review
- Interleukin-13 in the pathogenesis of pulmonary artery hypertension
- Infectiology and Microbiology
- Prospective evaluation study on the benefit of the simultaneous detection of seven sexually transmitted pathogens for the clinical management of patients suffering from sexually transmitted diseases
- Prevalence and genotyping of Helicobacter pylori in endoscopic biopsy samples from a Chinese population
- Original Articles
- Retinol-binding protein 4 better correlates with metabolic syndrome than cystatin C
- Effect of age and gender differences on high-sensitive troponin T measurement in the diagnosis of acute myocardial infarction
- Laboratory Case Report
- False high testosterone of unknown reason in a clinically inconspicuous female

