Abstract
There exists a need to research new diagnostic and therapeutic approaches that consider hemolytic disease of fetus and newborn (HDFN)’s physiopathology and focus not only on the pregnant person’s immune system but also on the fetal immune system. This implies, in the final sense, to view the fetus as our patient. In spite of having found a safe and efficient method of prevention of HDFN more than 50 years ago, HDFN continues to be a relevant cause of perinatal morbidity and mortality, due to lack of access to immunoprophylaxis. In light of the above, we should strive to prevent sensitization and HDFN by ensuring certain health policies across the globe, especially in countries and regions of high morbidity and mortality.
Where are we and where are we heading?
The traditional treatment for hemolytic disease of fetus and newborn (HDFN) is intrauterine (ITU) and neonatal transfusion [1]. However, transfusion addresses anemia, a consequence of HDFN, instead of attempting to solve its cause. Moreover, the pregnant person’s titers of antibodies are a universally accepted method of screening. Nonetheless, said technique is imprecise and focuses only on the pregnant person’s immune system, even though the responsible for fetal hemolysis and/or anemia is the fetal immune system.
There exists a need to research new diagnostic and therapeutic approaches that consider HDFN’s physiopathology and focus not only on the pregnant person’s immune system but also on the fetal immune system. This implies, in the final sense, to view the fetus as our patient [2]. From this point of view, an anti–neonatal Fc receptor blocker called Nipocalimab with a greater FcRn-binding affinity more than 1.000 times that of immune globulin has been developed and proven in a phase two study to delay or prevent fetal anemia and therefore intrauterine transfusions [3]. Additionally, the capacity of fetal phagocytosis is currently unknown, and new immunological tools could allow us to predict which fetal immune system will lead to HDFN.
Why should we continue to discuss HDFN?
In spite of having found a safe and efficient method of prevention of HDFN more than 50 years ago, HDFN continues to be a relevant cause of perinatal morbidity and mortality.
There are three key points that enable us to understand current HDFN’s global epidemiology.
First of all, the most clinically important blood group antigens are D, K and c [4], 5]. In addition, there are 50 other antigens capable of triggering HDFN [6]. Rarely do they cause HDFN, even so, some of them are frequent in certain populations.
On the other hand, 2 % of the general population and one in 80 pregnant people carry clinically significant antibodies [7]. As a result, one in 362 live births suffer HDFN across the world [8], [9], [10]. From 134 million world’s live births, 373,300 are estimated to suffer HDFN, leading to 114,100 deaths and neurological sequelae in 83 % of the survivors [10].
Finally, immunoprophylaxis fails in one in every 1,000 procedures [9]. Mostly, it is due to lack of access to immunoprophylaxis or administration of an insufficient dose. Less frequent causes include HDFN being triggered by other blood group antigens instead of D, incompatible transfusions in fertile people and sharing syringes in intravenous drug addicts.
There is a profound inequity in the access to immunoprophylaxis between regions and continents, leading to an enormous difference in HDFN’s prevalence, incidence and mortality between countries of high- and low-incomes.
Although annual doses required to prevent sensitization across the globe are 12.9 million, in 2020 only 3.6 million doses were applied. While high-income countries administer acceptable levels of anti-D, there are entire regions and continents such as South Asia and Africa that do not reach minimal thresholds (see Figure 1) [11], [12], [13].
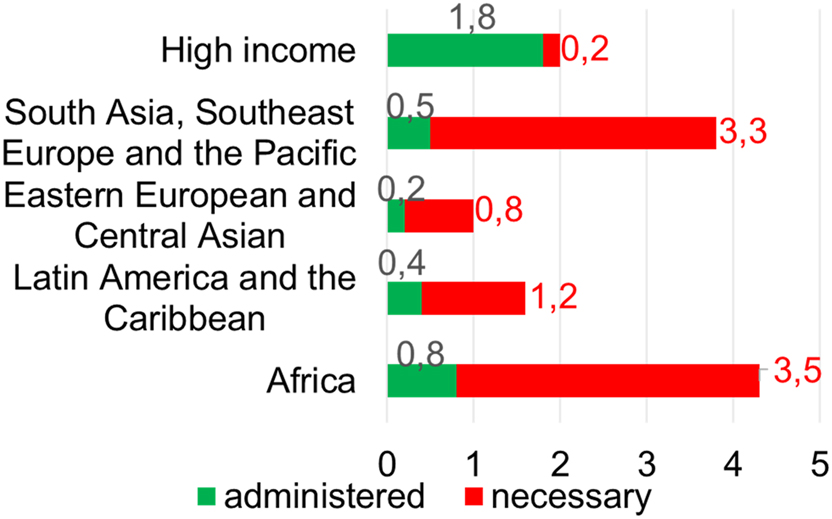
Representation of administered and necessary doses of immunoprophylaxis in different regions. Taken from Voto LS, Gonzalez CS. Enfermedad hemolítica perinatal. 1° edition. Buenos Aires: Acume; 2024. Data extracted from: Bhutani VK, Zipursky A, Blencowe H, Khanna R, Sgro M, Ebbesen F, et al. Neonatal hyperbilirubinemia and Rhesus disease of the newborn: incidence and impairment estimates for 2010 at regional and global levels. Pediatr Res. 2013;74 Suppl 1(Suppl 1):86–100. Ou Z, Yu D, Liang Y, He H, He W, Li Y, et al. Global trends in incidence and death of neonatal disorders and its specific causes in 204 countries/territories during 1990–2019. BMC Public Health. 2022;22(1):360.
As a consequence of access to anti-D, prevalence of HDFN dropped in high-income countries from one in 312 to initially one in 2,173 in 1969 and later on one in 40,000 in 2022; these data were extracted from the latest global prevalence epidemiological study. Because of this, HDFN has practically disappeared in those countries. In contrast, low-income countries hold 80 % of cases, maintaining same prevalence since 1940 (see Figure 2) [11], [12], [13].
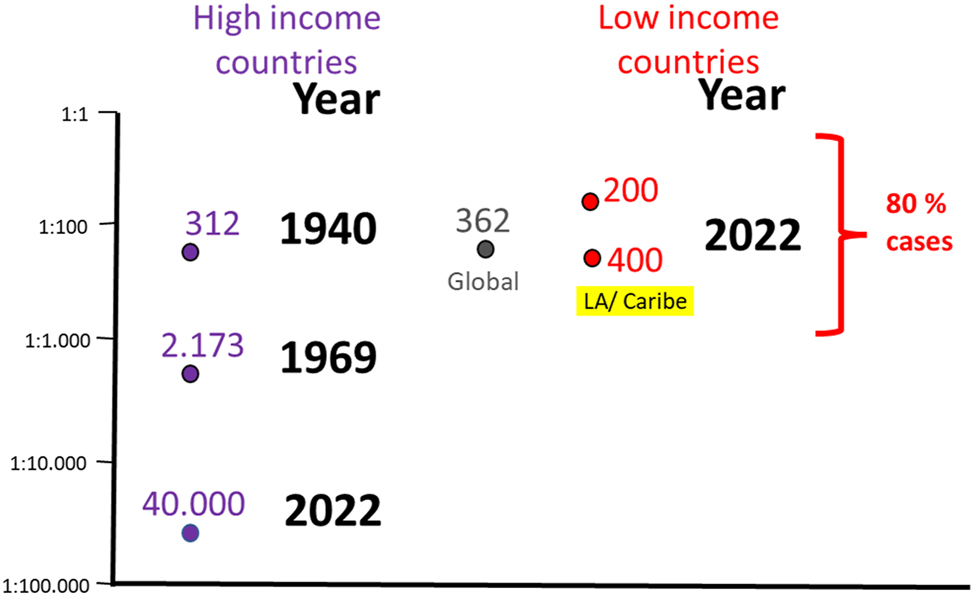
Representation of HDFN’ prevalence across time in high- and low-income countries, where LA stands for Latinoamerica. Taken from Voto LS, Gonzalez CS. Enfermedad hemolítica perinatal. 1° edition. Buenos Aires: Acume; 2024. Data extracted from: Bhutani VK, Zipursky A, Blencowe H, Khanna R, Sgro M, Ebbesen F, et al. Neonatal hyperbilirubinemia and Rhesus disease of the newborn: incidence and impairment estimates for 2010 at regional and global levels. Pediatr Res. 2013;74 Suppl 1(Suppl 1):86–100. Ou Z, Yu D, Liang Y, He H, He W, Li Y, et al. Global trends in incidence and death of neonatal disorders and its specific causes in 204 countries/territories during 1990–2019. BMC Public Health. 2022;22 (1):360.
Fetus as a patient
Pregnancy signifies an extraordinary situation from an immunohematological perspective: it implies the existence of two immune systems in one body, the fetal and pregnant person’s immune systems. Furthermore, not only do both systems exist within one body, but also they interact with one another, achieving a certain balance.
In other words, for pregnancy to occur normally, fetal immune system must not reject its own mother causing a graft vs. host disease [14], 15]. At the same time, the pregnant person must not recognise paternal antigens as foreign and therefore reject the fetus, which could be considered an incompatible hemitransplantation or semigraft. To this effect, interaction between both immune systems leads to an immune response that results in immune tolerance [13], 14], 16].
This involves a bidirectional passage of molecules and cells through placenta. For antibodies to cross, they require to go through syncytiotrophoblast, fetal endothelium and stroma. An Fc receptor known as FcRn binds to IgG and they are transported via pinocytosis. In stroma, there are fetal macrophages called Hofbauer cells which interact with IgG through different receptors (see Figure 3) [17]. Said macrophages could hold the key for future treatments.
![Figure 3:
Bidirectional transfer of molecules and cells between and fetus. Taken from: Gonzalez C, Gonzalez S, González J. One body, two immune systems. 1° edition. Moldavia: Eliva Press; 2024 [17].](/document/doi/10.1515/jpm-2024-0438/asset/graphic/j_jpm-2024-0438_fig_003.jpg)
Bidirectional transfer of molecules and cells between and fetus. Taken from: Gonzalez C, Gonzalez S, González J. One body, two immune systems. 1° edition. Moldavia: Eliva Press; 2024 [17].
Future challenges
As mentioned above, there exists a need to research new diagnostic and therapeutic possibilities that take into consideration HDFN’s physiopathology and therefore fetal immune system. Detection of fetal immune cells in pregnant person’s blood could enable to study Fc receptor’s affinity towards IgG, by transforming fetal neutrophils into fetal macrophages through already existing technology. As previously stated, an anti–neonatal Fc receptor blocker called Nipocalimab has been proven to prevent fetal anemia and intrauterine transfusions in pregnancies at high risk for recurrent early-onset severe HDFN [3]. Still, fetal immune system’s role in HDFN could benefit from more evidence-based support.
In light of the above, we should strive to prevent sensitization and HDFN by ensuring the following health policies across the globe, especially in countries and regions of high morbidity and mortality [13], 18]:
Equity in access to immunoprophylaxis with anti-D
Equity in access to monoclonal antibodies as they become available
Equity in access to antenatal care, including blood group test and antiglobulin test, with early referral of high-risk cases to higher complexity care during first trimester of pregnancy
Interdisciplinary approach of pregnant person, fetus and newborn
Blood transfusion as compatible as possible in phenotype in people capable of pregnancy particularly for D, K, c and E.
Development of drugs that enable to prevent production of clinically relevant antibodies other than anti-D
Implementation of platforms, laboratory studies and reagents with higher sensitivity and specificity
Detection of clinically important antibodies in milk banks
Creation of antibody databases at a local, national and regional level
-
Research ethics: Not applicable.
-
Informed consent: Not applicable.
-
Author contributions: All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Use of Large Language Models, AI and Machine Learning Tools: None declared.
-
Conflict of interest: The authors state no conflict of interest.
-
Research funding: None declared.
-
Data availability: Not applicable.
References
1. Voto, LS, Mathet, ER, Zapaterio, JL, Orti, J, Lede, RL, Margulies, M. High-dose gammaglobulin (IVIG) followed by intrauterine transfusions (IUTs): a new alternative for the treatment of severe fetal hemolytic disease. J Perinat Med 1997;25:85–8. https://doi.org/10.1515/jpme.1997.25.1.85.Search in Google Scholar PubMed
2. Gonzalez, CA, Gonzalez, S, González, J. Who is our patient: the fetus or the mother? Int J Blood Transfus Immunohematol 2021;11.10.5348/100061Z02CG2021EDSearch in Google Scholar
3. Moise, KJJ, Ling, LE, Oepkes, D, Tiblad, E, Verweij, EJTJ, Lopriore, E, et al.. Nipocalimab in early-onset severe hemolytic disease of the fetus and newborn. N Engl J Med 2024;391:526–37. https://doi.org/10.1056/nejmoa2314466.Search in Google Scholar PubMed
4. Delaney, M, Wikman, A, Van de Watering, L, Schonewille, H, Verdoes, JP, Emery, SP, et al.. Blood group antigen matching influence on gestational outcomes (AMIGO) study. Transfusion 2017;57:525–32. https://doi.org/10.1111/trf.13977.Search in Google Scholar PubMed
5. Karafin, MS, Westlake, M, Hauser, RG, Tormey, CA, Norris, PJ, Roubinian, NH, et al.. Risk factors for red blood cell alloimmunization in the Recipient Epidemiology and Donor Evaluation Study (REDS-III) database. Br J Haematol 2018;181:672–81. https://doi.org/10.1111/bjh.15182.Search in Google Scholar PubMed PubMed Central
6. Smith, HM, Shirey, RS, Thoman, SK, Jackson, JB. Prevalence of clinically significant red blood cell alloantibodies in pregnant women at a large tertiary-care facility. Immunohematol 2013;29:127–30. https://doi.org/10.21307/immunohematology-2019-134.Search in Google Scholar
7. Evers, D, Middelburg, RA, De Haas, M, Zalpuri, S, De Vooght, KM, Van de Kerkhof, D, et al.. Red-blood-cell alloimmunisation in relation to antigens’ exposure and their immunogenicity: a cohort study. Lancet Haematol 2016;3:e284–92. https://doi.org/10.1016/s2352-3026(16)30019-9.Search in Google Scholar PubMed
8. Geifman-Holtzman, O, Wojtowycz, M, Kosmas, E, Artal, R. Female alloimmunization with antibodies known to cause hemolytic disease. Obstet Gynecol 1997;89:272–5. https://doi.org/10.1016/s0029-7844(96)00434-6.Search in Google Scholar PubMed
9. Koelewijn, JM, Vrijkotte, TG, Van der Schoot, CE, Bonsel, GJ, De Haas, M. Effect of screening for red cell antibodies, other than anti-D, to detect hemolytic disease of the fetus and newborn: a population study in The Netherlands. Transfusion 2008;48:941–52. https://doi.org/10.1111/j.1537-2995.2007.01625.x.Search in Google Scholar PubMed
10. Markham, KB, Rossi, KQ, Nagaraja, HN, O’Shaughnessy, RW. Hemolytic disease of the fetus and newborn due to multiple maternal antibodies. Am J Obstet Gynecol 2015;213:68.e1–5. https://doi.org/10.1016/j.ajog.2015.01.049.Search in Google Scholar PubMed
11. Bhutani, VK, Zipursky, A, Blencowe, H, Khanna, R, Sgro, M, Ebbesen, F, et al.. Neonatal hyperbilirubinemia and Rhesus disease of the newborn: incidence and impairment estimates for 2010 at regional and global levels. Pediatr Res 2013;74:86–100. https://doi.org/10.1038/pr.2013.208.Search in Google Scholar PubMed PubMed Central
12. Ou, Z, Yu, D, Liang, Y, He, H, He, W, Li, Y, et al.. Global trends in incidence and death of neonatal disorders and its specific causes in 204 countries/territories during 1990–2019. BMC Publ Health 2022;22:360. https://doi.org/10.1186/s12889-022-12765-1.Search in Google Scholar PubMed PubMed Central
13. Voto, LS, Gonzalez, CS. Enfermedad hemolítica perinatal, 1 ed. Buenos Aires: Ascune; 2024.Search in Google Scholar
14. Gonzalez, CA, Gonzalez, S, González, J. Can maternofetal transfusion provoke adverse outcomes akin to TA-GVHD? Transfus Apher Sci 2022;61:103409. https://doi.org/10.1016/j.transci.2022.103409.Search in Google Scholar PubMed
15. Schreiber, AR, Santos, J, McMahon, B, Buckner, TW, Olson, C, Alberti, MO, et al.. A case of fetal-induced graft-versus-host disease. N Engl J Med 2023;389:668–70. https://doi.org/10.1056/nejmc2307669.Search in Google Scholar
16. Gonzalez, CA, Gonzalez, S. Fetal and neonatal allo-immune response. Transfus Apher Sci 2020;59:102945. https://doi.org/10.1016/j.transci.2020.102945.Search in Google Scholar PubMed
17. Gonzalez, C, Gonzalez, S, González, J. One body, two immune systems, 1 ed. Moldavia: Eliva Press; 2024.Search in Google Scholar
18. Gupta, GK, Balbuena-Merle, R, Hendrickson, JE, Tormey, CA. Immunohematologic aspects of alloimmunization and alloantibody detection: a focus on pregnancy and hemolytic disease of the fetus and newborn. Transfus Apher Sci 2020;59:102946. https://doi.org/10.1016/j.transci.2020.102946.Search in Google Scholar PubMed
© 2025 the author(s), published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Frontmatter
- Editorial
- Perinatal responsibility in a fragmented world: reflections from the 2024 international academy of perinatal medicine New York meeting
- Corner of Academy
- Global education – impressive results of Ian Donald School
- Cicero’s universal law: a timeless guide to reproductive justice
- Enhancing patient understanding in obstetrics: the role of generative AI in simplifying informed consent for labor induction with oxytocin
- Faculty retention in academic OB/GYN: comprehensive strategies and future directions
- Hemolytic disease of the fetus and newborn: pregnant person’s and fetal immune systems interaction
- Viability of extremely premature neonates: clinical approaches and outcomes
- Reviews
- Standardizing cord clamping: bridging physiology and recommendations from leading societies
- Thrombotic thrombocytopenic purpura in pregnancy: a comprehensive review
- Mini Review
- Looking for a needle in a haystack: a case study of rare disease care in neonatology
- Opinion Paper
- Hemorrhagic placental lesions on ultrasound: a continuum of placental abruption
- Original Articles – Obstetrics
- Amnioreduction safety in singleton pregnancies; systematic review and meta-analysis
- Outpatient management of prelabour rupture of membranes (PROM) at term – a re-evaluation and contribution to the current debate
- Breastfeeding in HIV-positive mothers under optimized conditions: ‘real-life’ results from a well-resourced healthcare setting
- Intervention using the Robson classification as a tool to reduce cesarean section rates in six public hospitals in Brazil
- Short Communication
- Continuous positive airway pressure vs. high velocity nasal cannula for weaning respiratory support of preterm infants
Articles in the same Issue
- Frontmatter
- Editorial
- Perinatal responsibility in a fragmented world: reflections from the 2024 international academy of perinatal medicine New York meeting
- Corner of Academy
- Global education – impressive results of Ian Donald School
- Cicero’s universal law: a timeless guide to reproductive justice
- Enhancing patient understanding in obstetrics: the role of generative AI in simplifying informed consent for labor induction with oxytocin
- Faculty retention in academic OB/GYN: comprehensive strategies and future directions
- Hemolytic disease of the fetus and newborn: pregnant person’s and fetal immune systems interaction
- Viability of extremely premature neonates: clinical approaches and outcomes
- Reviews
- Standardizing cord clamping: bridging physiology and recommendations from leading societies
- Thrombotic thrombocytopenic purpura in pregnancy: a comprehensive review
- Mini Review
- Looking for a needle in a haystack: a case study of rare disease care in neonatology
- Opinion Paper
- Hemorrhagic placental lesions on ultrasound: a continuum of placental abruption
- Original Articles – Obstetrics
- Amnioreduction safety in singleton pregnancies; systematic review and meta-analysis
- Outpatient management of prelabour rupture of membranes (PROM) at term – a re-evaluation and contribution to the current debate
- Breastfeeding in HIV-positive mothers under optimized conditions: ‘real-life’ results from a well-resourced healthcare setting
- Intervention using the Robson classification as a tool to reduce cesarean section rates in six public hospitals in Brazil
- Short Communication
- Continuous positive airway pressure vs. high velocity nasal cannula for weaning respiratory support of preterm infants

