Socioeconomic status as a risk factor for SARS-CoV-2 infection in pregnant women
-
Julia Lastinger
, Joachim Gerich
, Philip Sebastian Trautner
Abstract
Objectives
Due to the association between COVID-19 and adverse pregnancy outcomes, pregnant women are considered to be a vulnerable patient group. Studies have shown that low socioeconomic status (SES) is a risk factor for SARS-CoV-2 infection. COVID-19 and low SES are likely to have a synergistic adverse effect. This study aimed to evaluate the socioeconomic background, indicated by self-reported SES, educational level, and financial situation, in pregnant women who were positive for SARS-CoV-2.
Methods
A case-control study was conducted, including all pregnant women with positive SARS-CoV-2 PCR tests at Kepler University Hospital Linz between May 2020 and August 2021 (n=150) and a control group matched 1:1 relative to gestational age at birth (n=150). Data were collected using written questionnaires and medical records from the hospital information system.
Results
Lower self-reported socioeconomic status (p=0.029) and lower education level (p=0.003) were detected in the COVID group. Mothers in the COVID group were significantly younger (p=0.024). However, after adjustment for educational attainment, younger age was not confirmed as a risk factor for SARS-CoV-2 infection during pregnancy (p=0.326). The social gradient was not explained by the assumed mediators and confounders.
Conclusions
These findings confirm an association between lower socioeconomic status and the risk of SARS-CoV-2 infection during pregnancy. Since both socioeconomic factors and COVID-19 impose negative effects on pregnancy outcomes, health inequalities should be taken into consideration when implementing SARS-CoV-2 prevention measures and when providing health care for pregnant women from disadvantaged communities.
Introduction
The outbreak of the coronavirus disease 2019 (COVID-19) pandemic in early-2020 has been challenging health-care systems worldwide. In order to establish prevention strategies, researchers attempted to identify patients who are at risk for infection with severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2). Observational studies soon found that older people and patients with comorbidities such as cardiovascular disease, immunodeficiency or cancer, smokers, and obese patients are more likely to develop COVID-19 1], [2], [3. Socioeconomic risk factors were also identified. Communities suffering from social disadvantage, poor education and housing, and low incomes have significantly higher infection rates. In addition, patients from ethnic minority backgrounds and those of male sex are at higher risk 1], [2], [3], [4], [5], [6], [7], [8], [9. In a British cohort, pregnant women suffering from COVID-19 were found to be more likely to live in deprived neighborhoods and to be of nonwhite ethnicity [10]. Patients who were more likely to develop severe infection with a need for admission to the intensive-care unit (ICU) included those of advanced age, patients from ethnic minority populations, and patients with a low socioeconomic background [2, 11]. Vaccine hesitancy is reported to be higher in communities from ethnic minority backgrounds [4].
In addition to correlating with negative health outcomes in general, a lower socioeconomic background similarly has an impact on pregnancy outcomes and fetal growth. Living in a deprived neighborhood leads to higher rates of adverse pregnancy outcomes, such as preterm birth and low birth weight [12].
Pregnant women are at higher risk for a severe course of SARS-CoV-2-infection with a need for ICU admission and invasive ventilation. Rates of preeclampsia, preterm birth, low birth weight, and even fetal death are higher in this group of patients [10, 11, 13, 14]. Although transmission from mothers to newborns during pregnancy and childbirth only occurs rarely, cases of SARS-CoV-2–positive neonates have been reported [15]. Pregnant women are therefore regarded as a vulnerable patient group.
Both COVID-19 and a low socioeconomic background have a severe impact on pregnancy outcomes [12, 13]. These effects are likely to amplify each other, leaving disadvantaged communities at high risk for poorer maternal and fetal health outcomes.
Over 400 women with SARS-CoV-2 infection during pregnancy or labor have been treated at Kepler University Hospital, one of Austria’s largest perinatal clinics, between the onset of the pandemic until the end of 2022. So far, three SARS-CoV-2–positive pregnant women have had to be admitted to the ICU. The present study aimed to analyze whether low socioeconomic status correlates with a higher risk for SARS-CoV-2 infection during pregnancy in this cohort and to determine which socioeconomic variables should be considered as risk factors in pregnant women at risk for SARS-CoV-2 infection.
In addition, the study aimed to identify possible pathways for the social gradient in the SARS-CoV-2 infection risk during pregnancy. The study takes into account migration status, age at childbirth, mothers’ and their partners’ working conditions, housing conditions, and health literacy as possible explanatory variables for the assumed social gradient.
Materials and methods
A case-control study including pregnant women who gave birth at a tertiary obstetric clinic in Linz, Austria, between May 2020 and August 2021 was conducted. All pregnant women with a positive SARS-CoV-2 PCR test any time during pregnancy and delivery were included in the study. Due to routine testing upon hospital admission, most women were tested positively in the last trimester of pregnancy. To compare demographic data, a control group who gave birth during the same time period as the COVID group was matched 1:1 according to gestational age at birth. The control group was selected from a list of live births at the study center. All controls had a negative SARS-CoV-2 PCR at admission and no history of SARS-CoV-2 infection during pregnancy. Women in the control group gave birth at the same time points as women from the COVID group. Random selection of controls was performed by a member of the study team. Basic maternal characteristics were collected on the basis of a retrospective analysis of medical records using the hospital information system. A written questionnaire was used to collect individual data for socioeconomic status (financial situation, subjective estimation of socioeconomic status, level of education), mothers’ and their partners’ working conditions, migration status, housing conditions, and health literacy.
Socioeconomic status
Socioeconomic status was measured with three indicators (self-rated financial situation, subjective estimation of socioeconomic status, level of education). The self-rated financial situation was covered by the question “How do you rate your financial situation?” followed by a five-point Likert-type rating scale ranging from (1) very bad to (5) very good. The measure of subjective estimation of socioeconomic status was based on the style of a McArthur scale, in which respondents rate their own position in society between values of 1 (people at the lowest position in society) and 10 (people at the top position in society) [16, 17]. Educational level was considered as a binary variable (high-school diploma or university degree vs. lower educational levels).
Working conditions
The working conditions of women who were employed before childbirth are covered by mean ratings for three items (“My supervisor cares about the health of staff members,” “The firm makes sure that the current COVID safety guidelines are observed,” “It is possible to comply with COVID-related safety distance and hygiene rules at my workplace”), each followed by a four-point Likert-type scale ranging from 1 (“not at all”) to 4 (“fully applies”). Where applicable, the working conditions of the women’s employed partners were inquired into in the same format.
Migration status and housing conditions
The women’s migration status was taken into account using two indicators (whether respondents were born in Austria or another country, and whether German or another language is typically spoken at home). Two indicators for housing conditions were considered. The household occupancy rate was computed as the ratio between the reported apartment size, measured in square meters, and the number of persons living in the household. In addition, respondents were asked whether certain facilities are available in their home or neighborhood (balcony, green areas, garden, parks, playgrounds, opportunities for walking), where neighborhood facilities were computed as the sum of these features available.
Health literacy
Health literacy was covered using two dimensions. First, the six-item short version of the HLS-EU inventory was used to assess the subjectively rated level of health literacy [18, 19]. This inventory asks about individuals’ difficulty in accomplishing different health-related tasks in the domains of health care, disease prevention, and health promotion (sample item: “How easy would you say it is to understand information in the media on how to improve your health?”). All items were followed by a four-point Likert-type rating scale ranging from (1) very difficult to (4) very easy. As previous research has shown that high scores on the HLS-EU scale may be biased due to subjective overestimation, low critical awareness, or a lack of health-related experience [20], an alternative measure addressing health-related knowledge [21] was also implemented. Health-related knowledge was covered by six items consisting of statements for which the respondents have to indicate whether they are true, false, or whether they are not able to decide (sample item: “The term hepatitis refers to inflammation of the heart muscle”). Health-related knowledge was calculated as the number of correct answers to these six items.
All women were asked to participate in the study via telephone interviews, and information about their socioeconomic background and health literacy was obtained using written questionnaires delivered by mail. The participants gave their consent by signing the Informed Consent Form (ICF). A total of 300 women were included in the two groups, and they were contacted by a member of the study team. Only pseudonymized data were used for statistical analysis.
Statistical analysis
Descriptive analysis was performed for the total patient sample and separately in the COVID and control group. Nominal data are presented with absolute and relative frequencies. Ordinal and continuous quantitative variables are presented by their mean values and standard deviations. The t-test for independent samples and χ2 test were used to analyze differences between the COVID group and the control group. Binary logistic regression was used to analyze whether expected group differences with respect to socioeconomic status can be explained by the assumed mediators and confounders. Multiple logistic regression analysis has been performed in order to evaluate several factors simultaneously. The level of significance was set at 0.05. All analyses were performed with IBM SPSS Statistics, version 26 (IBM Corporation, Armonk, New York, 2019).
Results
Figure 1 shows the distribution of participants and returned questionnaires in the COVID group and control group. A total of 104 (69 %) of 150 women in the COVID group agreed to participate, and 41 (27 %) complete questionnaires were returned. Eighty-five (57 %) of 150 women in the control group agreed to participate, and 31 (21 %) complete questionnaires were returned.
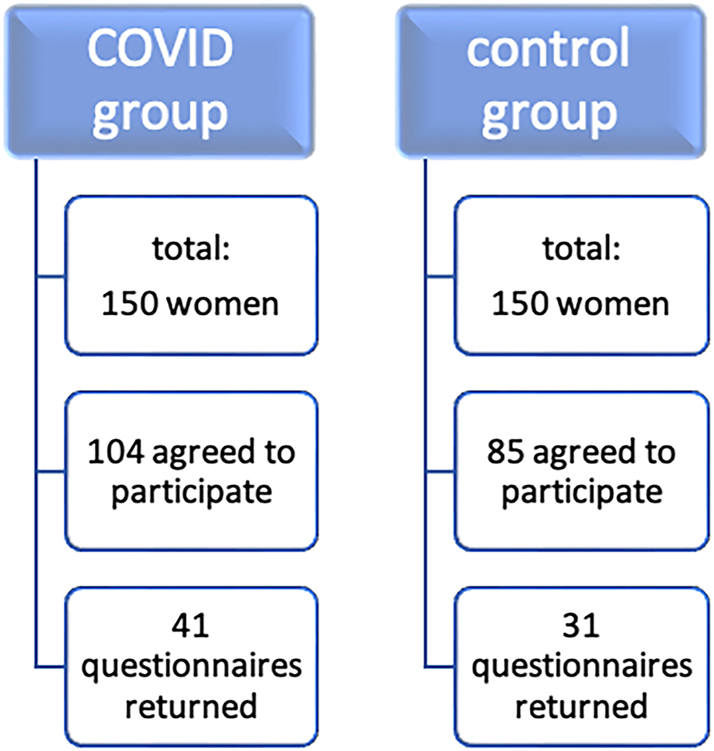
Participants and response rates in the COVID group and control group.
Descriptive variable information and corresponding group differences are shown in Table 1.
Descriptive characteristics and differences between the COVID group and control group.
| n | Scale | Mean/proportion (SD) | Group differences | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Total sample | COVID group | Control group | t (df) | χ2 (df) | p-Value | ||||
| Socioeconomic status | |||||||||
| Financial situation | 72 | 1 (very bad) – 5 (very good) | 3.10 (0.75) | 3.05 (0.82) | 3.17 (0.65) | 0.66 (70) | – | 0.513 | |
| Subjective SES | 71 | 1 (lowest) – 10 (highest) | 7.06 (1.36) | 6.76 (1.53) | 7.47 (0.97) | 2.23 (69) | – | 0.029 | |
| Higher education | 71 | 67.6 % | 53.7 % | 86.7 % | – | 8.62 (1) | 0.003 | ||
| Age at childbirth | 72 | years | 31.15 (4.52) | 30.14 (4.15) | 32.57 (4.70) | 2.31 (70) | – | 0.024 | |
| Working conditions | |||||||||
| Safe working conditions (respondent) | 55 | 1 (not safe) – 4 (very safe) | 3.53 (0.58) | 3.52 (0.57) | 3.56 (0.60) | 0.25 (53) | – | 0.804 | |
| Safe working conditions (partner) | 66 | 1 (not safe) – 4 (very safe) | 3.46 (0.72) | 3.43 (0.80) | 3.50 (0.63) | 0.41 (64) | – | 0.681 | |
| Migration status | |||||||||
| Not born in Austria | 71 | 19.7 % | 19.1 % | 20.7 % | – | 0.03 (1) | 0.864 | ||
| Foreign language spoken at home | 68 | 14.7 % | 15.8 % | 13.3 % | – | 0.08 (1) | 0.776 | ||
| Housing conditions | |||||||||
| Household occupancy rate | 72 | m2/number of persons | 16.79 (15.73) | 16.62 (15.09) | 17.04 (16.85) | 0.11 (70) | – | 0.912 | |
| Neighborhood facilities | 72 | 0 (none) – 6 (all) | 3.96 (1.27) | 4.07 (1.24) | 3.80 (1.32) | 0.89 (70) | – | 0.376 | |
| Health literacy | |||||||||
| HLS score | 68 | 1 (lowest) – 4 (highest) | 2.97 (0.55) | 2.96 (0.60) | 2.98 (0.50) | 0.17 (66) | – | 0.862 | |
| Health-related knowledge | 70 | 0 (lowest) – 6 (highest) | 4.94 (1.03) | 4.90 (0.98) | 5.00 (1.11) | 0.40 (68) | – | 0.692 | |
-
n, valid responses; p-values for group-differences based on chi-square/t-test; COVID-19, coronavirus disease 2019; SD, standard deviation; df, number of degrees of freedom; SES, socioeconomic status; HLS, health literacy score. Bold values indicate statistical significance (p-value < 0.05).
Significant associations between indicators of mothers’ socioeconomic status and SARS-CoV-2 infection were confirmed. The women in the COVID group reported a significantly lower self-estimated socioeconomic status (measured on a scale from 1 to 10; p=0.029) and lower educational level (p=0.003).
Only one of the assumed mediators and confounders (age at childbirth) showed a significant difference between the groups, in that the mean age at childbirth among women in the COVID group was significantly lower in comparison with women in the control group (p=0.024).
No significant differences between the groups were confirmed in relation to working conditions, migration status, housing conditions, or indicators of health literacy.
The raw and adjusted ORs for the three indicators of socioeconomic status and mother’s age at childbirth are shown in Table 2.
Odds ratios for being in the non-COVID control group.
| Scale | Univariable | Multivariable | |
|---|---|---|---|
| Financial situation | 1 (very bad) – 5 (very good) | 1.24 (0.507) | 0.60 (0.245) |
| Subjective SES | 1 (lowest) – 10 (highest) | 1.53 (0.034) | 1.63 (0.061) |
| Higher education | Yes/no | 5.61 (0.006) | 4.58 (0.026) |
| Age at childbirth | years | 1.14 (0.030) | 1.067 (0.326) |
| R2 (Cox & Snell) | – | 0.18 |
-
Odds ratios from binary logistic regression (COVID, group=0; control group=1), p-values in parentheses; n=70; COVID-19, coronavirus disease 2019; SES, socioeconomic status. Bold values indicate statistical significance (p-value <0.05).
According to the univariable analysis, women with a high school or university diploma had a 5.6-fold chance of being in the control group rather than the COVID group in comparison with those with a lower educational level. Each additional step in the self-rated socioeconomic position (measured on a scale between one and ten) was associated with a 1.5-fold chance of being in the control instead of the COVID group. With regard to women’s age at childbirth, each additional year of life was related to a 1.14-fold increase in the chance of being in the control group rather than the COVID group.
The results of the multivariable analysis only confirmed a significant effect of women’s educational attainment after adjustment for the other predictors, explaining the multivariable model’s R2 value of 18 %. Hence, these results suggest that the higher risk of SARS-CoV-2 infection during pregnancy for women with lower socioeconomic status is predominately explained by the educational component of socioeconomic status. Moreover, although women with SARS-CoV-2 infection were younger at childbirth, a significant effect for the risk of a SARS-CoV-2 infection during pregnancy was not confirmed when the analysis was adjusted for socioeconomic status. Women with lower compared to higher socioeconomic status are thus younger at childbirth, but age was not confirmed a risk factor for SARS-CoV-2 infection during pregnancy after adjustment for socioeconomic status.
Discussion
Consistent with previous results regarding general health inequalities, these findings – based on the early days of the pandemic – confirm that there is an increased risk for SARS-CoV-2 infection during pregnancy associated with women’s lower socioeconomic status. Two out of three indicators of socioeconomic status considered (educational attainment and subjective status estimation) were found to be related to an increased risk for SARS-CoV-2 infection during pregnancy, with the strongest and most consistent effect being found for maternal education. However, significant associations were not confirmed with migration status, dense housing conditions and neighborhood characteristics, women’s and their partners’ working conditions, and women’s health literacy. Although an elevated risk for SARS-CoV-2 infection was confirmed for younger women, this was confounded with socioeconomic status. Higher educational status is related to higher age at childbirth, and women’s age is not related to a higher risk of SARS-CoV-2 infection after adjustment for educational attainment. This is consistent with prior results showing that later childbirth among women is related to higher educational attainment [22, 23] and findings indicating that higher educational status is related to greater use of and earlier entry into prenatal care [24].
With regard to working conditions, the questionnaire focused on subjective ratings of a COVID-related safety climate. It was inquired whether employers provided adequate resources and encouraged employees to comply with the recommended measures for reducing infection risks. However, the approach used here may have overlooked the possibility that some workplaces (for example, workplaces in the care and health-care sectors) present higher infection risks independently of the COVID-related safety climate.
Similarly, although validated measures were used, a relationship was not found between health literacy and the risk of SARS-CoV-2 infection during pregnancy.
All of these findings lead to the question how women with lower socioeconomic status can be protected from developing severe SARS-CoV-2 infection. Some studies suggest spreading relevant more information on the mitigation of COVID via the media and via social media in order to reach a broader audience [25]. In many cases language barriers are the reason for a lack of sufficient knowledge on SARS-CoV-2 and recommended safety measures. Various authors recommend to provide reliable multilingual information as well as culturally appropriate information in order to increase the protection of vulnerable patient groups 26], [27], [28. In Sweden, working groups aiming at the improvement of integration, health equity and social inclusion of immigrants have developed information specifically tailored to people with migration background [29]. The state of Upper Austria provides a homepage designated to recent news and information on SARS-CoV-2, which has been translated into languages most commonly spoken by immigrants in the region, including Dari and Pashto and SARS-CoV-2 online counselling has been offered for immigrants and refugees [30].
In the early days of the pandemic, vaccination was limited to non-pregnant people only. However, potentially life-saving prophylaxis should be quickly made available for everyone. This is why some research groups suggest that pregnant people should be offered participation in clinical trials speed up access to novel therapeutic options [31]. In addition to in-person clinic visits, telemedicine offers new opportunities for patient care. Patient counselling and the spread of information regarding SARS-CoV-2 safety measures and implications for labor and delivery could be easily performed via telemedicine appointments. In this way, women from disadvantaged communities, who might have less options regarding mobility or childcare for their older children could benefit and be able to attend appointments they would have otherwise not have been able to attend [32].
In summary, the present results suggest that the social gradient in relation to SARS-CoV-2 infection during pregnancy may not be explained by any single identifiable determinants, but rather by the fact that a larger number of generalized resources are available to those with higher socioeconomic status, as suggested by the theory of fundamental causes [33, 34]. This theoretical approach argues that the flexible generalized resources available to those with higher socioeconomic status (such as money, knowledge, power, prestige, or those embedded in social networks) allow earlier recognition of newly emerging diseases and health risks and more adequate and faster reactions to new health-related challenges, and that the mechanisms related to this advantage cannot be assigned to single specific “surface” factors.
Limitations
Firstly, the study was based on a small sample size and the response rate of included patients was low. A response rate of approximately a third of the population is found commonly in questionnaire studies. Women with poor knowledge of the German language or the inability to read German texts are very likely not to respond to the survey. Especially these women might be affected by a poor socioeconomic background. The same number of women were first contacted via telephone in the COVID and control group. Certainly, women with little German language skills were also included in the control group. The number of women with migration background and of those who do not speak German at home were comparable between the two groups. However, selection bias cannot be ruled out completely. Due to the small number of questionnaires returned, the statistical power to reveal relevant predictors of SARS-CoV-2 infection is low. In addition, due to the low response rate, further selection effects may have occurred. It is possible, for instance, that individuals with higher risk behavior in both groups decided not to participate in the survey, and this may have reduced possible contrasts between the study groups. Moreover, as the measures were based on self-reporting, subjectivity bias or recall bias may have to be taken into account.
Conclusions
In line with the results of earlier international studies, these findings confirm that there is an association between indicators of socioeconomic status and SARS-CoV-2 infection in pregnant women. In particular, higher educational status with high-school or university qualifications was found to have a protective effect against the risk of acquiring a SARS-CoV-2 infection during pregnancy. Lower self-reported socioeconomic status was also found to be related to a higher risk of SARS-CoV-2 infection.
The negative consequences of COVID-19 on pregnancy complications, such as preterm birth, preeclampsia, or stillbirth, have long been acknowledged by researchers and clinicians. However, little attention has been paid to the influence of socioeconomic risk on mothers and their offspring. The detrimental effect of social inequality on pregnancy outcomes and health in general is not a new phenomenon solely caused by COVID-19 and was already being studied long before the onset of the SARS-CoV-2 pandemic [12]. It is recommended that health-care services should pay increased attention to mothers with lower socioeconomic status and provide additional social assistance for these vulnerable groups during pregnancy.
Funding source: Johannes Kepler University Linz
Award Identifier / Grant number: Grant for Covid Research
Acknowledgments
Sabine Enengl and Peter Oppelt received a grant for COVID-19 research from Johannes Kepler University Linz.
-
Research ethics: Ethics approval was obtained from the Ethics Committee of Johannes Kepler University Linz (EK – 1074/2020). This study was performed in accordance with the Declaration of Helsinki.
-
Informed consent: Informed consent was obtained from all individuals included in this study.
-
Author contributions: The authors have accepted responsibility for the entire content of this manuscript and approved its submission. JL: protocol development, data collection, manuscript writing; JG: protocol development, data management, statistical analysis, manuscript writing; MB-R: protocol development, manuscript writing; PS: data management; PST: data management; S-HE: manuscript editing; RA: data management; OS: manuscript editing; PO: protocol development, manuscript editing; SE: protocol development, data management, manuscript editing. All authors reviewed the manuscript.
-
Competing interests: Sabine Enengl and Peter Oppelt received a grant for COVID-19 research from Johannes Kepler University Linz. All other authors report no conflicts of interest.
-
Research funding: Sabine Enengl and Peter Oppelt received a grant for COVID-19 research from Johannes Kepler University Linz.
-
Data availability: The raw data can be obtained on request from the corresponding author.
-
Clinical trial registration: The study was retrospectively registered at the German Clinical Trials Register (DRKS00021208) on March 31th, 2020.
References
1. Chadeau-Hyam, M, Bodinier, B, Elliott, J, Whitaker, MD, Tzoulaki, I, Vermeulen, R, et al.. Risk factors for positive and negative COVID-19 tests: a cautious and in-depth analysis of UK biobank data. Int J Epidemiol 2020;49:1454–67. https://doi.org/10.1093/ije/dyaa134.Search in Google Scholar PubMed PubMed Central
2. Anesi, G. COVID-19: epidemiology, clinical features, and prognosis of the critically ill adult (30.03.2022) UpToDate. https://www.uptodate.com/contents/covid-19-epidemiology-clinical-features-and-prognosis-of-the-critically-ill-adult?search=covid%20risk%20factors&source=search_result&selectedTitle=4∼150&usage_type=default&display_rank=2. [Accessed 22 May 2022].Search in Google Scholar
3. Bein, BBM, Huggett, S, Wegermann, P. SARS-CoV-2/COVID-19: evidence-based recommendations on diagnosis and therapy. Geburtshilfe Frauenheilkd 2020;80:491–8. https://doi.org/10.1055/a-1156-3991.Search in Google Scholar PubMed PubMed Central
4. Hussain, B, Latif, A, Timmons, S, Nkhoma, K, Nellums, LB. Overcoming COVID-19 vaccine hesitancy among ethnic minorities: a systematic review of UK studies. Vaccine 2022;S0264-410X:00446–7.10.1016/j.vaccine.2022.04.030Search in Google Scholar PubMed PubMed Central
5. Liao, TF, De Maio, F. Association of social and economic inequality with coronavirus disease 2019 incidence and mortality across US counties. JAMA Netw Open 2021;4:e2034578. https://doi.org/10.1001/jamanetworkopen.2020.34578.Search in Google Scholar PubMed PubMed Central
6. Bambra, C, Riordan, R, Ford, J, Matthews, F. The COVID-19 pandemic and health inequalities. J Epidemiol Community Health 2020;74:964. https://doi.org/10.1136/jech-2020-214401.Search in Google Scholar PubMed PubMed Central
7. Wachtler, B, Michalski, N, Nowossadeck, E, Diercke, M, Wahrendorf, M, Santos-Hövener, C, et al.. Socioeconomic inequalities and COVID-19 – a review of the current international literature. J Health Manag 2020;3–17. https://doi.org/10.25646/7059.Search in Google Scholar PubMed PubMed Central
8. Khanijahani, A, Iezadi, S, Gholipour, K, Azami-Aghdash, S, Naghibi, D. A systematic review of racial/ethnic and socioeconomic disparities in COVID-19. Int J Equity Health 2021;20:248. https://doi.org/10.1186/s12939-021-01582-4.Search in Google Scholar PubMed PubMed Central
9. Hoebel, J, Michalski, N, Wachtler, B, Diercke, M, Neuhauser, H, Wieler, LH, et al.. Socioeconomic differences in the risk of infection during the second sars-Cov-2 wave in Germany. Dtsch Arztebl Int 2021;118:269–70. https://doi.org/10.3238/arztebl.m2021.0188.Search in Google Scholar PubMed PubMed Central
10. Gurol-Urganci, I, Jardine, JE, Carroll, F, Draycott, T, Dunn, G, Fremeaux, A, et al.. Maternal and perinatal outcomes of pregnant women with SARS-CoV-2 infection at the time of birth in England: national cohort study. Am J Obstet Gynecol 2021;225:522.e1–11. https://doi.org/10.1016/j.ajog.2021.05.016.Search in Google Scholar PubMed PubMed Central
11. Allotey, J, Stallings, E, Bonet, M, Yap, M, Chatterjee, S, Kew, T, et al.. Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: living systematic review and meta-analysis. BMJ 2020;370:m3320. https://doi.org/10.1136/bmj.m3320.Search in Google Scholar PubMed PubMed Central
12. Gootjes, DV, Posthumus, AG, Jaddoe, VWV, Steegers, EAP. Association between neighbourhood deprivation, fetal growth, small-for-gestational age and preterm birth: a population-based prospective cohort study. BMJ Open 2021;11:e049075. https://doi.org/10.1136/bmjopen-2021-049075.Search in Google Scholar PubMed PubMed Central
13. Marchand, G, Patil, AS, Masoud, AT, Ware, K, King, A, Ruther, S, et al.. Systematic review and meta-analysis of COVID-19 maternal and neonatal clinical features and pregnancy outcomes up to June 3, 2021. AJOG Glob Rep 2022;2:100049. https://doi.org/10.1016/j.xagr.2021.100049.Search in Google Scholar PubMed PubMed Central
14. Papageorghiou, AT, Deruelle, P, Gunier, RB, Rauch, S, García-May, PK, Mhatre, M, et al.. Preeclampsia and COVID-19: results from the INTERCOVID prospective longitudinal study. Am J Obstet Gynecol 2021;225:289.e1–17. https://doi.org/10.1016/j.ajog.2021.05.014.Search in Google Scholar PubMed PubMed Central
15. Enengl, S, Pecks, U, Oppelt, P, Stelzl, P, Trautner, PS, Shebl, O, et al.. Antibody response and maternofetal antibody transfer in SARS-CoV-2-positive pregnant women: a multicenter observational study. Geburtshilfe Frauenheilkd 2022;82:501–9. https://doi.org/10.1055/a-1768-0415.Search in Google Scholar PubMed PubMed Central
16. Adler, NE, Epel, ES, Castellazzo, G, Ickovics, JR. Relationship of subjective and objective social status with psychological and physiological functioning: preliminary data in healthy, White women. Health Psychol 2000;19:586–92. https://doi.org/10.1037/0278-6133.19.6.586.Search in Google Scholar
17. Hoebel, J, Müters, S, Kuntz, B, Lange, C, Lampert, T. Messung des subjektiven sozialen Status in der Gesundheitsforschung mit einer deutschen Version der MacArthur Scale. Bundesgesundheitsblatt – Gesundheitsforsch – Gesundheitsschutz 2015;58:749–57. https://doi.org/10.1007/s00103-015-2166-x.Search in Google Scholar PubMed
18. Sørensen, K, Van den Broucke, S, Pelikan, JM, Fullam, J, Doyle, G, Slonska, Z, et al.. Measuring health literacy in populations: illuminating the design and development process of the European health literacy survey questionnaire (HLS-EU-Q). BMC Publ Health 2013;13:948. https://doi.org/10.1186/1471-2458-13-948.Search in Google Scholar PubMed PubMed Central
19. Pelikan, JM, Ganahl, K. Measuring health literacy in general populations: primary findings from the HLS-EU Consortium’s health literacy assessment effort. In: Logan, RA, Siegel, ER, editors. Health literacy: new directions in research, theory and practice. Amsterdam: IOS Press; 2017.Search in Google Scholar
20. Gerich, J, Moosbrugger, R, Heigl, C. Health literacy and age-related health-care utilisation: a multi-dimensional approach. Ageing Soc 2022;42:1538–59. https://doi.org/10.1017/s0144686x20001609.Search in Google Scholar
21. Gerich, J, Moosbrugger, R. Subjective estimation of health literacy-what is measured by the HLS-EU scale and how is it linked to empowerment? Health Commun 2018;33:254–63. https://doi.org/10.1080/10410236.2016.1255846.Search in Google Scholar PubMed
22. Berrington, A, Pattaro, S. Educational differences in fertility desires, intentions and behaviour: a life course perspective. Adv Life Course Res 21. https://doi.org/10.1016/j.alcr.2013.12.003. [Epub ahead of print 1 January 2013].Search in Google Scholar PubMed
23. Nitsche, N, Brückner, H. Late, but not too late? Postponement of first birth among highly educated US women. Eur J Popul 2021;37:371–403. https://doi.org/10.1007/s10680-020-09571-z.Search in Google Scholar PubMed PubMed Central
24. Feijen-de Jong, EI, Jansen, DE, Baarveld, F, van der Schans, CP, Schellevis, FG, Reijneveld, SA. Determinants of late and/or inadequate use of prenatal healthcare in high-income countries: a systematic review. Eur J Publ Health 2012;22:904–13. https://doi.org/10.1093/eurpub/ckr164.Search in Google Scholar PubMed
25. Hayes, J, Clerk, L. Fatalism in the early days of the COVID-19 pandemic: implications for mitigation and mental health. Front Psychol 2021;12. https://doi.org/10.3389/fpsyg.2021.560092.Search in Google Scholar PubMed PubMed Central
26. Mheidly, N, Fares, J. Leveraging media and health communication strategies to overcome the COVID-19 infodemic. J Publ Health Pol 2020;41:410–20. https://doi.org/10.1057/s41271-020-00247-w.Search in Google Scholar PubMed PubMed Central
27. Elisabeth, M, Maneesh, P-S, Michael, S. Refugees in Sweden during the COVID-19 pandemic – the need for a new perspective on health and integration. Front Public Health 2020;8. https://doi.org/10.3389/fpubh.2020.574334.Search in Google Scholar PubMed PubMed Central
28. Roble, S, Wångdahl, J, Warner, G. COVID-19 Information in Sweden: opinions of immigrants with limited proficiency in Swedish. Health Commun 2022;37:1510–19. https://doi.org/10.1080/10410236.2022.2050005.Search in Google Scholar PubMed
29. Partnership Skåne. Information films of COVID-19 – in multiple languages; 2021. https://reginproject.eu/resources-for-regions/integration-lab/skane/ [Accessed 31 July 2024].Search in Google Scholar
30. Corona-Infos Oberösterreich. COVID-19 information in many languages. https://corona.ooe.gv.at/index.htm [Accessed 31 July 2024].Search in Google Scholar
31. Stock, SJ, Harmer, C, Calvert, C. COVID-19 variants of concern and pregnancy. BMJ Med 2022;1:e000151. https://doi.org/10.1136/bmjmed-2022-000151.Search in Google Scholar PubMed PubMed Central
32. Preis, H, Mahaffey, B, Heiselman, C, Lobel, M. Pandemic-related pregnancy stress and anxiety among women pregnant during the coronavirus disease 2019 pandemic. COVID-19 Pregnancy Update 2020;2:100155. https://doi.org/10.1016/j.ajogmf.2020.100155.Search in Google Scholar PubMed PubMed Central
33. Link, BG, Phelan, J. Social conditions as fundamental causes of disease. J Health Soc Behav 1995:80–94. https://doi.org/10.2307/2626958.Search in Google Scholar
34. Phelan, JC, Link, BG, Tehranifar, P. Social conditions as fundamental causes of health inequalities: theory, evidence, and policy implications. J Health Soc Behav 2010;51:S28–40. https://doi.org/10.1177/0022146510383498.Search in Google Scholar PubMed
© 2024 the author(s), published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Frontmatter
- Review
- Chorioamnionitis and respiratory outcomes in prematurely born children: a systematic review and meta analysis
- Opinion Paper
- Non-binary patients in ART: new challenges and considerations
- Corner of Academy
- KANET evaluation in patients with SARS-CoV-2
- Original Articles – Obstetrics
- Socioeconomic status as a risk factor for SARS-CoV-2 infection in pregnant women
- Social vulnerability and prenatal diagnosis
- Perinatal outcomes in pregnant women with ITP: a single tertiary center experience
- Ability of an obstetric hemorrhage risk assessment tool to predict quantitative peripartum blood loss
- Sensitive detection of hemodynamic changes after fetoscopic laser photocoagulation by assessing intraventricular pressure difference in fetuses with twin-to-twin transfusion syndrome
- Prevalence of restless legs syndrome during pregnancy and postpartum period
- Does atenolol use during pregnancy cause small for gestational age neonates? A meta-analysis
- Uterine isthmic tourniquet left in situ as a new approach for placenta previa-accreta surgery: a comparative study
- Maternal and newborn outcomes in pregnancies complicated by Guillain-Barré syndrome
- Original Articles – Fetus
- A customised fetal growth and birthweight standard for Qatar: a population-based cohort study
- Molecular analysis of 31 cases with fetal skeletal dysplasia
- Short Communication
- Current practice of ultrasound in the management of postpartum hemorrhage: a secondary analysis of a national survey
Articles in the same Issue
- Frontmatter
- Review
- Chorioamnionitis and respiratory outcomes in prematurely born children: a systematic review and meta analysis
- Opinion Paper
- Non-binary patients in ART: new challenges and considerations
- Corner of Academy
- KANET evaluation in patients with SARS-CoV-2
- Original Articles – Obstetrics
- Socioeconomic status as a risk factor for SARS-CoV-2 infection in pregnant women
- Social vulnerability and prenatal diagnosis
- Perinatal outcomes in pregnant women with ITP: a single tertiary center experience
- Ability of an obstetric hemorrhage risk assessment tool to predict quantitative peripartum blood loss
- Sensitive detection of hemodynamic changes after fetoscopic laser photocoagulation by assessing intraventricular pressure difference in fetuses with twin-to-twin transfusion syndrome
- Prevalence of restless legs syndrome during pregnancy and postpartum period
- Does atenolol use during pregnancy cause small for gestational age neonates? A meta-analysis
- Uterine isthmic tourniquet left in situ as a new approach for placenta previa-accreta surgery: a comparative study
- Maternal and newborn outcomes in pregnancies complicated by Guillain-Barré syndrome
- Original Articles – Fetus
- A customised fetal growth and birthweight standard for Qatar: a population-based cohort study
- Molecular analysis of 31 cases with fetal skeletal dysplasia
- Short Communication
- Current practice of ultrasound in the management of postpartum hemorrhage: a secondary analysis of a national survey


