Osteopathic manipulative treatment in the management of headaches associated with musculoskeletal dysfunction: systematic review and meta-analysis
-
Yasir Rehman
, Jonathon Kirsch
Abstract
Context
Osteopathic manipulative treatment (OMT) can be utilized as a primary or adjunctive treatment for headaches associated with musculoskeletal disorders. Although previous systematic reviews investigated the effectiveness of manual therapies for treating headaches, they did not focus specifically on OMT or perform a pooled meta-analysis to evaluate the effectiveness of outcomes.
Objectives
The aim of this study is to systematically evaluate the effectiveness of OMT for managing headaches associated with musculoskeletal dysfunction and to assess the associated harm outcomes.
Methods
In September 2023, the following databases were searched for randomized controlled trials (RCTs) of adult patients with headaches associated with musculoskeletal dysfunction who were treated with OMT: Allied and Complementary Medicine Database, ClinicalTrials.gov, Cochrane Central Register of Controlled Trials (CENTRAL), Cumulative Index of Nursing and Allied Health Literature (CINAHL), Excerpta Medica (EMBASE), Osteopathic Medicine Digital Library (OSTMED), Ovid Emcare, Ovid MEDLINE, Physiotherapy Evidence Database (PEDro), PsycINFO, and PubMed. The search terms included osteopathic manipulative medicine, manual therapy, osteopath, headache, concussion, and head injury. The studies had to compare OMT techniques (e.g., articulatory [ART]; high-velocity, low-amplitude [HVLA]; soft tissues [ST]) to another form of treatment or a different type of OMT technique. Our primary outcomes included headache severity, headache frequency, disability associated with headaches, quality of life, and return to work (RTW); harm outcomes included all-cause dropout (ACD) rates, dropouts due to inefficacy, and adverse effects. The Cochrane Risk of Bias (ROB) tool was utilized to assess the ROB in the reviewed studies, and the quality of evidence was assessed utilizing the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) system. Outcomes data were pooled for analysis and reported as standardized mean difference (SMD) and 95 % confidence interval (CI).
Results
Our search identified 11,657 RCTs. After removing duplicates and screening titles and abstracts, 167 underwent full-text review, and 18 were included in our review. None of the reviewed RCTs met all of the Cochrane ROB criteria. Moderate-quality evidence indicated that combined ART-HVLA (SMD=−0.61, 95 % CI=−1.0 to −0.23) and ST HVLA-ART (SMD=−0.48, 95 % CI=−0.83 to −0.13) effectively reduced the severity of headache. Moderate-quality evidence also indicated that the combined techniques of ART-HVLA (SMD=−0.43, 95 % CI=−0.74 to −0.13) and ST-ART-HVLA (SMD=−0.62, 95 % CI=−0.89 to −0.35) effectively reduced the frequency of headaches. Moderate-quality evidence indicated that quality of life was improved with combined ART-HVLA (SMD=0.57, 95 % CI=0.14 to 0.99). Low-quality evidence indicated no significant associations of OMT with disability or harm outcomes (all p>0.26).
Conclusions
Results of our systematic review and meta-analysis suggested that a combination of multiple types of OMT techniques effectively reduced the frequency and severity of headaches and improved quality of life. However, high-quality RCTs with large sample sizes utilizing a variety of technique modalities and combinations of technique modalities are necessary to better evaluate the effectiveness of OMT for managing headaches.
Headaches are among the most common complaints when seeking medical care, and 52 % of the global population experiences an active headache every year [1]. On any given day, 15.8 % of people have a headache [1]. Headaches associated with musculoskeletal dysfunction, such as tension and migraine headaches, can significantly impact activities of daily living (ADLs), work-related activities, and quality of life (QOL) [2]. In 2019, missed workdays from migraines in the United States cost $19.3 billion [3]. In 2014, the annual combined direct and indirect costs for a single migraine patient were estimated at over $8,000 [4], 5]. People with migraines are approximately half as effective at work and miss an average of 2 h of work per day and 3 days of work every 3 months [6], 7]. Although over half of the adult population will complain about headaches during their lifetime, most do not receive optimal treatment [8]. Given these substantial impacts associated with headache disorders, the World Health Organization started a global campaign in 2003 to increase awareness and reduce the burden of treatment costs and loss of productivity [9], 10].
The inclusion of osteopathic manipulative treatment (OMT) in the management of headaches was assessed in previous systematic reviews [11], [12], [13], [14], but these reviews did not focus on osteopathic manipulation or perform a meta-analysis because of high heterogeneity in the reviewed studies. The results of earlier reviews were also limited by their search criteria for eligible studies, such as the inclusion of quasi-randomized trials [11], 13], focused on a specific manipulative technique [13], or a literature search restricted to a few databases and to a 12-year range [12]. Therefore, the purpose of the current study was to systematically evaluate the effectiveness of OMT for treating headaches associated with musculoskeletal dysfunction and to assess the associated harm outcomes, including all-cause dropout (ACD) rates, dropout rates associated with adverse events, and dropout rates due to inefficacy.
Methods
The current systematic review and meta-analysis was conducted according to the Cochrane Handbook for Systematic Reviews of Interventions [15], 16] and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [17]. The study protocol CRD42023449356 was registered with the International Prospective Register of Systematic Reviews (PROSPERO).
Search strategy
A detailed systematic search strategy was developed for the current review, and the following databases were searched from their inception to September 2023: Allied and Complementary Medicine Database, ClinicalTrials.gov, Cochrane Central Register of Controlled Trials (CENTRAL), Cumulative Index to Nursing and Allied Health Literature (CINAHL), Excerpta Medica (EMBASE), Osteopathic Medicine Digital Library (OSTMED), Ovid Emcare, Ovid MEDLINE, Physiotherapy Evidence Database (PEDro), PsycINFO, and PubMed. The search terms included osteopathic manipulative medicine, manual therapy, osteopath, headache, concussion, and head injury. The search strategy is reported in Supplementary Material Appendix 1.
Eligibility criteria
To be included in our review, eligible studies had to be randomized controlled trials (RCTs) of adult patients (≥18 years of age) with headaches associated with musculoskeletal dysfunction treated with OMT. Studies had to be published in English and compare OMT with placebo, treatment as usual, waitlist, a non-OMT intervention (e.g., medications), or another OMT technique type or protocol, but not the same as the experimental intervention. The following categories of studies and published articles were excluded: observational, quasi-randomized trials, qualitative studies, systematic reviews or narrative reviews, conference abstracts, animal studies, commentaries, and letters to the editor.
For the current systematic review, the types of headaches included were migraines and tension-type headaches cervicogenic headaches, headaches associated with temporomandibular joint disorder, concussion, traumatic brain injury, or whiplash-associated disorders; and headaches related to fibromyalgia [18]. Studies were excluded when the headaches were associated with hypoxia, infection, an elevation or depression in intracranial pressure, traumatic brain injury secondary to surgery or stroke, inflammation of the intracranial membranes, organic disorders of the central nervous system structures, headaches associated with medication use or withdrawal, or systemic dysfunctions.
Eligible OMT interventions included any OMT technique or modality described in the Glossary of Osteopathic Terminology [19] from the American Association of Colleges of Osteopathic Medicine (AACOM). Further, an osteopathically trained provider had to perform OMT interventions, which was confirmed by review of the author’s information or article text. The OMT interventions could be administered utilizing individual techniques or several techniques within a single modality. They could also be combined as part of a multimodality protocol, in which specific techniques were utilized in a predefined sequence of techniques. Finally, interventions could be based on a per-clinician protocol, in which multiple technique modalities were utilized as needed based on the physical examination. The OMT could be provided independently or with the standard of care [19]. Individual techniques utilized in the OMT interventions were divided into different OMT categories based on the modalities. For example, the articulatory (ART) technique category includes low-velocity, moderate-amplitude, and springing techniques [19]. Three authors (KS, JK, DS) who were experienced osteopathic educators determined the OMT categories through a blinded review process. To address the issue of high heterogeneity, which was a significant limitation in previous systematic reviews [20], [21], [22], the studies investigating the same OMT technique categories and comparator types were pooled for each outcome. We included this approach in our review because it has been previously validated for this kind of data [23], [24], [25].
For comparator interventions, the comparator treatment could include sham manipulation, waitlist or no treatment, treatment as usual, a different type of OMT technique or protocol that was not the same as the experimental intervention, or any standard of care intervention, such as exercise therapy or medication.
Study outcomes
The primary outcomes for the current systematic review and meta-analysis were headache severity and frequency. Data for these outcomes were measured with a validated measuring scale, such as a numerical rating scale (NRS), and/or with a headache frequency diary. Additionally, the outcomes included were disability associated with headaches, such as those measured with the Migraine Disability Assessment (MIDAS), QOL, such as those measured with the Headache Impact Test (HIT-6), and return to work (RTW). Harm outcomes included ACDs, dropouts due to inefficacy, and dropouts due to adverse effects. The Cochrane Risk of Bias (ROB) tool was utilized to assess the ROB in the reviewed studies, and quality of evidence was assessed utilizing the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) system.
Screening and data extraction
Our search strategy identified 11,657 RCTs (Figure 1), of which 18 were included in our review. Title and abstract screening, full-text screening, and data extraction, including ROB, were performed independently in duplicates. Any conflicts were resolved through consensus and, if necessary, arbitration by the third reviewer (YR). To ensure reliability of the full-text review, screening followed the guidelines proposed by Landis and Koch [26] for assessing agreement between reviewers. The following data were extracted from the included studies: demographic information of participants, intervention details, follow-up duration, and outcomes data. We also extracted data about the OMT technique categories utilized in the OMT protocols or included as part of a more extensive treatment protocol.
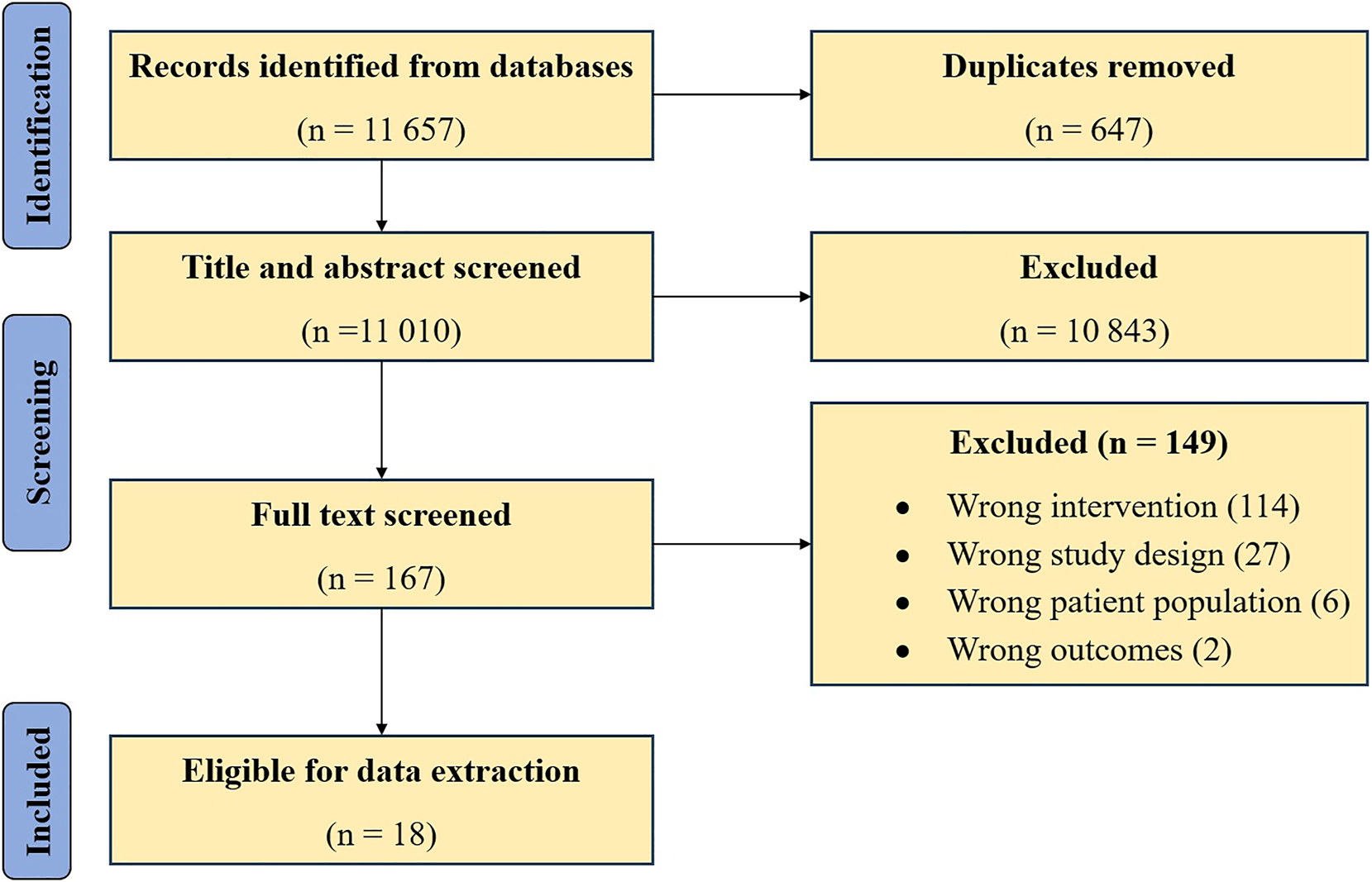
A preferred reporting items for systematic reviews and meta-analyses (PRISMA) flow diagram for the identification of eligible randomized controlled trials (RCTs) for inclusion in the current systematic review.
Data analysis
Data were summarized for demographic information, intervention details, follow-up duration, and outcomes data utilizing frequency and percentage for count data and mean and standard deviation (SD) for continuous data. Pooled analyses were performed for the outcomes of headache severity, headache frequency, disability associated with headache, QOL, ACD rates, and dropout rates due to inefficacy. There was not enough data in the reviewed studies for pooled analyses for the outcomes of RTW and dropouts due to adverse effects. Outcomes were reported descriptively for these data that could not be pooled or for which the heterogeneity was high. When the OMT interventions and comparators in the reviewed studies were homogenous, data were pooled according to the OMT category and comparator type (e.g., sham manipulation, exercise therapy, or medication) utilizing the random effects model with standardized mean difference (SMD) and 95 % confidence interval (CI) for continuous outcomes and odds ratio (OR) and 95 % CI for binary outcomes. If an effect estimate was reported in the reviewed study as other than mean (SD), such as a 95 % CI, median, or interquartile range (IQR), the data were converted to mean (SD) utilizing the formula suggested by the Cochrane Handbook for Systematic Reviews of Interventions [15], 16]. For each summary effect, heterogeneity was assessed through a forest plot and I2 statistic [27], 28], and the precision of the effects was measured with the 95 % CI and whether the CI included the line of no effect. The ROB for the reviewed studies was assessed utilizing the modified Cochrane ROB instrument [29], 30] for the following domains: random sequence generation; allocation concealment; blinding of patients, physicians, data collectors, outcome assessors, and data analysts; and loss to follow-up (incomplete outcome data). The GRADE approach was utilized to rate the quality of evidence for each outcome as high, moderate, low, or very low [31], [32], [33]. The five central domains of GRADE are ROB, heterogeneity, imprecision, indirectness, and publication bias. None of the pooled analyses included 10 or more studies, so we could not assess publication bias. Our review did not include enough studies to perform a subgroup analysis, but a sensitivity analysis was performed for each outcome by pooling different OMT interventions [20], [21], [22]. All analyses were performed with the R package meta [34], and p<0.05 was considered statistically significant.
Results
Eighteen RCT studies [35], [36], [37], [38], [39], [40], [41], [42], [43], [44], [45], [46], [47], [48], [49], [50], [51], [52] involving 1,009 participants were included in the current review. The mean age of the participants was 39.7 years (range=18–71 years), and 80 % were female (Table 1). The median follow-up duration was 74 days (range=19–180 days). All reviewed studies reported a comparator intervention or standard of care, except for four studies [38], 39], 42], 45]. None of the reviewed studies met all of the criteria for ROB (Table 2). All studies were at high risk for blinding of physicians. The GRADE evidence for pooled studies is presented in Table 3.
Summary characteristics of randomized controlled trial studies included in the current systematic review (n=18).
| Study | Total no. of patients | Mean age (range) | % female patients | Headache type | Other medications or therapy allowed | Days of follow-up duration | Loss of follow-up accounted for | Adverse effects accounted for | Adverse effects in patients |
|---|---|---|---|---|---|---|---|---|---|
| Cerritelli et al. [35] | 105 | 38.7 | 34.2 | Migraine | Yes | 180 | Yes | Yes | No |
| Deodato et al. [36] | 24 | 47 | 60.0 | TTH | Yes | 90 | Yes | Yes | No |
| Espí-López and Gómez-Conesa [37] | 84 | 39.8 (18–65) | 81.0 | TTH | Yes | 58 | No | Yes | Yes |
| Espí-López et al. [38] | 84 | 39.7 (18–65) | 81.0 | TTH | NR | 58 | No | Yes | Yes |
| Espí-López et al. [40] | 76 | 39.9 (18–65) | 81.6 | TTH | Yes | 28 | Yes | Yes | No |
| Espí-López et al. [41] | 76 | 39.9 (18–65) | 81.6 | TTH | Yes | 28 | Yes | Yes | No |
| Espí-López et al. [43] | 105 | 38.9 (18–65) | 78.1 | TTH | Yes | 84 | No | Yes | No |
| Espí-López et al. [42] | 46 | 33.9 (18–59) | 82.6 | Migraine | NR | 56 | Yes | Yes | No |
| Espi-Lopez et al. [39] | 38 | 32 | 76.3 | TTH | No | 28 | Yes | Yes | No |
| Esterov et al. [44] | 20 | 43.5 (18–71) | 65.0 | MTBI | Yes | Unclear | No | Yes | No |
| Fernández-de-las-Peñas et al. [45] | 84 | 31.2 (21–44) | 54.5 | Whiplash | NR | 19 | Unclear | Yes | No |
| Gandolfi et al. [46] | 22 | 47.8 (18–66) | 86.3 | Migraine | Yes | 28 | Yes | Yes | No |
| Hoyt et al. [47] | 22 | NR | NR | NR | Yes | Unclear | Unclear | No | NA |
| Muñoz-Gómez et al. [49] | 50 | 38.5 (18–50) | 78.0 | Migraine | Yes | 60 | Yes | Yes | No |
| Muñoz-Gómez et al. [50] | 75 | 39.0 | 77.3 | Migraine | Yes | 60 | Yes | Yes | Yes |
| Muñoz-Gómez et al. [48] | 50 | 40.1 | 80.0 | Migraine | Yes | 60 | Yes | Yes | No |
| Rolle et al. [51] | 44 | 34.4 | 85.0 | TTH | Yes | 30 | No | Yes | No |
| Voigt et al. [52] | 42 | 45.1 (24–66) | 100 | Migraine | Yes | 180 | Yes | No | NA |
-
MTBI, mild traumatic brain injury; NA, not applicable; NR, not reported; TTH, tension-type headache.
Risk of bias for the randomized controlled trial studies included in the current systematic review (n=18).
| Study | Random sequence generation | Allocation concealment | Patient blinding | Physician blinding | Data collector blinding | Outcome assessor blinding | Data analyst blinding | Loss of follow-up |
|---|---|---|---|---|---|---|---|---|
| Cerritelli et al. [35] | LR | LR | LR | HR | HR | LR | LR | LR |
| Deodato et al. [36] | LR | LR | HR | HR | HR | HR | HR | LR |
| Espí-López and Gómez-Conesa [37] | LR | LR | LR | HR | LR | HR | HR | LR |
| Espí-López et al. [38] | LR | LR | HR | HR | HR | HR | HR | LR |
| Espí-López et al. [40] | LR | HR | HR | HR | HR | HR | HR | LR |
| Espí-López et al. [41] | LR | LR | HR | HR | HR | HR | LR | LR |
| Espí-López et al. [43] | LR | LR | LR | HR | LR | HR | HR | LR |
| Espí-López et al. [42] | LR | LR | LR | HR | LR | HR | LR | LR |
| Espi-Lopez et al. [39] | LR | LR | HR | HR | LR | LR | LR | LR |
| Esterov et al. [44] | HR | HR | HR | HR | HR | HR | HR | HR |
| Fernández-de-las-Peñas et al. [45] | LR | HR | HR | HR | HR | HR | HR | LR |
| Gandolfi et al. [46] | LR | LR | HR | HR | LR | LR | LR | LR |
| Hoyt et al. [47] | LR | LR | HR | HR | LR | LR | LR | LR |
| Muñoz-Gómez et al. [49] | LR | LR | LR | HR | LR | HR | LR | LR |
| Muñoz-Gómez et al. [50] | LR | LR | LR | HR | LR | LR | LR | LR |
| Muñoz-Gómez et al. [48] | LR | LR | LR | HR | LR | LR | LR | LR |
| Rolle et al. [51] | LR | LR | LR | HR | LR | HR | HR | LR |
| Voigt et al. [52] | HR | HR | HR | HR | HR | HR | HR | HR |
-
HR, high risk of bias; LR, low risk of bias.
Grading of Recommendations Assessment, Development, and Evaluation (GRADE) quality of evidence for pooled analyses of the current systematic review.
| Intervention (no. of participants) | Effect estimatesa | Risk of bias | Heterogeneity | Imprecision | Indirectness | Publication bias | Quality of evidence |
|---|---|---|---|---|---|---|---|
| Headache severity | |||||||
| Soft tissue (128) | −0.34 (−0.74 to 0.06) | − | + | − | + | + | Low |
| ART-HVLA (168) | −0.61 (−1.00 to −0.23) | − | + | + | + | + | Moderate |
| ST-ART-HVLA (168) | −0.48 (−0.83 to −0.13) | − | + | + | + | + | Moderate |
| OMT vs. medications (125) | −1.15 (−1.66 to −0.65) | − | + | + | + | + | Moderate |
| Headache frequency | |||||||
| Soft tissue (128) | −0.22 (−0.58 to 0.15) | − | + | − | + | + | Low |
| ART-HVLA (168) | −0.43 (−0.74 to −0.13) | − | + | + | + | + | Moderate |
| ST-ART-HVLA (220) | −0.62 (−0.89 to −0.35) | − | + | + | + | + | Moderate |
| OMT vs. medications (125) | −2.50 (−6.88 to 1.89) | − | + | − | + | + | Low |
| Disability associated with headaches | |||||||
| Soft tissue (78) | 0.40 (−0.05 to 0.85) | − | + | − | + | + | Low |
| ART-HVLA (128) | −0.28 (−0.77 to 0.20) | − | + | − | + | + | Low |
| ST-ART-HVLA (78) | −0.10 (−0.55 to 0.34) | − | + | − | + | + | Low |
| Quality of life | |||||||
| ART-HVLA (88) | 0.57 (0.14–0.99) | − | + | + | + | + | Moderate |
| All-cause dropouts | |||||||
| ST-ART-HVLA (147) | 0.78 (0.08–7.17) | − | + | − | + | + | Low |
| Per clinicianb (86) | 0.41 (0.05–3.69) | − | + | − | + | + | Low |
| Dropouts due to inefficacy | |||||||
| ST-ART-HVLA (147) | 0.33 (0.03–3.31) | − | + | − | + | + | Low |
-
aEffect estimates are reported as standardized mean difference and 95 % confidence interval (CI) for headache severity, headache frequency, disability associated with headaches, and quality of life. Effect estimates are reported as odds ratio and 95 % CI for all-cause dropouts and dropouts due to inefficacy. bPer-clinician techniques were performed at the treating clinician’s discretion and were based on physical findings. The protocol could include a variety of direct and indirect types of osteopathic manipulative medicine techniques such as MFR, BLT, BMT, and OCMM. ART, articulatory technique (includes springing and low-velocity, moderate-amplitude techniques); BLT, balanced ligamentous tension; BMT, balanced membranous tension (type of OCMM technique); HVLA, high-velocity, low-amplitude (includes all thrust techniques); MFR, myofascial release; OCMM, osteopathic cranial manipulative medicine (includes a wide variety of direct and indirect techniques); OMT, osteopathic manipulative treatment; ST, soft tissue (includes massage and inhibition).
Supplementary Table 1 summarizes the OMT interventions utilized in the reviewed studies and their categorization into specific OMT technique modalities for the meta-analysis. Two studies [42], 50] compared the effectiveness of the OMT protocol with other OMT protocols, and two studies [35], 36] compared the effectiveness of OMT with medications.
Headache severity
When compared with the control, moderate-quality evidence indicated that the combined articulatory and high-velocity, low-amplitude (ART-HVLA) [37], 38], 40], 49] technique (n=168, SMD [95 % CI]=−0.61 [−1.00 to −0.23], I2=32 %, p<0.01) and combined soft tissue, articulatory, and high-velocity, low-amplitude (ST-ART-HVLA) [37], 38], 40], 43] technique (n=220, SMD [95 % CI]=−0.48 [−0.83 to −0.13], I2=38 %, p<0.01) were associated with decreased headache severity (Supplementary Figures 1A and 1B). When compared with medications, moderate-quality evidence indicated that per-clinician myofascial release (MFR), HVLA, visceral, and osteopathic cranial manipulative medicine (MFR, balanced ligamentous tension [BLT], balanced membranous tension [BMT], and osteopathic cranial manipulative medicine [OCMM]) [35], 36] (n=125) was associated with decreased headache severity (SMD [95 % CI]=−1.15 [−1.66 to −0.65], I2=22 %, p<0.01) (Supplementary Figure 1C). Low-quality evidence indicated that the soft tissue (ST) technique alone [37], 38], 40] (n=128) was not associated with decreased headache severity (Supplementary Figure 1D).
For the sensitivity analysis, nine studies [37], 38], 40], 43], [47], [48], [49, 52] (n=536) were pooled to compare any type of OMT technique intervention to the control. Any type of OMT was associated with decreased headache severity (SMD [95 % CI]=−0.58 [−0.84 to −0.32], p<0.01) (Supplementary Figure 1E). However, the heterogeneity among studies was high (I2=50 %).
Headache frequency
When compared with the control, moderate-quality evidence indicated the combined ART-HVLA [37], 38], 40], 49] (n=168; SMD [95 % CI]=−0.43 [−0.74 to −0.13], I2=0 %, p<0.01) and ST-ART-HVLA [37], 38], 40], 43] (n=220, SMD [95 % CI]=−0.62 [−0.89 to −0.35], I2=0 %, p<0.01) techniques were associated with decreased headache frequency (Supplementary Figures 2A and 2B). The ST [37], 38], 40] (n=128) and the per-clinician MFR, BLT, BMT, and OCMM [35], 36] (n=125) were not associated with reduced headache frequency when compared with either the control or medications ((Supplementary Figures 2C and 2D).
For the sensitivity analysis, 7 studies [37], 38], 40], 43], 46], 49], 52] (n=448) were pooled to compare any OMT intervention with the control. Any OMT intervention was associated with improved outcomes (SMD [95 % CI]=−0.42 [−0.62 to −0.22], I2=0 %, p<0.01) (Supplementary Figure 2E).
Disability associated with headache
When compared with the control, low-quality evidence indicated that ST [38], 40] (n=78, SMD [95 % CI]=−0.1 [−0.55 to 0.34], I2=0 %, p=0.65) and combined ART-HVLA [38], 40], 49] (n=128, SMD [95 % CI]=−0.28 [−0.77 to 0.20], I2=47 %, p=0.26) and ST-ART-HVLA [38], 40] (n=78, SMD [95 % CI]=−0.1 [−0.55 to 0.34], I2=0 %, p=0.65) were not associated with an improvement in disability associated with headache (Supplementary Figures 3A–3C). For the sensitivity analysis, six studies [38], [39], [40, 46], 49], 52] (n=304) were pooled to compare any OMT intervention with the control. No improvement was found (p=0.38), and heterogeneity among the studies was low (I2=6 %) (Supplementary Figure 3D).
Quality of life
Moderate-quality evidence indicated that combined ART-HVLA [41], 49] (n=88) was associated with improvement in QOL (SMD [95 % CI]=0.57 [0.14 to 0.99], I2=0 %, p<0.01)] (Supplementary Figure 4).
All-cause dropout (ACD) rates
Low-quality evidence indicated that the combined ST-ART-HVLA [37], 38] (n=147, OR [95 % CI]=0.78 [0.08 to 7.17], I2=24 %, p=0.83) and the per-clinician MFR, BLT, BMT, and OCMM [51], 52] (n=86, OR [95 % CI]=0.41 [0.05 to 3.69], I2=35 %, p=0.43) were not associated with ACD rates (Supplementary Figures 5A and 5B). For the sensitivity analysis, five studies [37], 38], 44], 51], 52] (n=301) were pooled, and no association was found between any OMT intervention and ACD rates (OR [95 % CI]=0.68 [0.26 to 1.80], I2=0 %, p=0.44) (Supplementary Figure 5C).
Dropout rates due to inefficacy
Low-quality evidence indicated that the combined ST-ART-HVLA [37], 38] (n=147) technique was not associated with dropout rates due to inefficacy (OR [95 % CI]=0.33 [0.03 to 3.31], I2=0 %, p=0.35) (Supplementary Figure 6A). For the sensitivity analysis, two studies [37], 43] (n=189) were pooled, and no association was found between any OMT intervention dropouts due to inefficacy (OR [95 % CI]=0.19 [0.02 to 1.18], I2=0 %, p=0.66) (Supplementary Figure 6B).
Adverse effects
All but two studies [47], 52] accounted for adverse effects. Among the studies that accounted for adverse effects, three studies [37], 38], 48] reported adverse effects. The reported adverse effects were mild posttreatment cervical pain (n=2) [37], 38] and dizziness (n=5) [48]. Therefore, the total incidence of adverse effects across reporting studies was 7 in 923 participants (0.75 %).
Unpooled outcomes of reviewed studies
Supplementary Table 2 summarizes outcomes data from the reviewed studies that could not be included in the pooled analyses. Only one study [52] (n=70) reported the effect of OMT on RTW; no association was found between OMT and days of disablement.
Discussion
The current review systematically evaluated the existing literature to determine the effectiveness of OMT for treating headaches associated with musculoskeletal dysfunction and assessed the associated harm outcomes. The results indicated that a combined OMT protocol, such as ART-HVLA or ST-ART-HVLA, can be utilized to effectively treat headaches associated with musculoskeletal disorders, especially when compared with an individual OMT technique, such as ST. The primary outcomes of headache severity and frequency were significantly reduced with the ART-HVLA and ST-ART-HVLA techniques. Similarly, the combined ART-HVLA technique was associated with improved QOL. When compared with medications, combined OMT protocols, such as per-clinician MFR, BLT, BMT, and OCMM, were significantly associated with reduced headache severity but not with headache frequency. Additionally, there was low-quality evidence that OMT was not significantly associated with disability and harmful outcomes, such as ACD and dropouts due to inefficacy. Study outcomes of RTW and dropouts due to adverse effects could not be pooled due to insufficient study numbers.
Unlike previous reviews [11], [12], [13], [14], the current study was designed to improve the overall rigor of the research area that investigated osteopathic manual therapies for headaches. For example, the results of previous reviews were limited by an inability to perform pooled meta-analyses because of the heterogeneity in the eligible studies [11], [12], [13], [14]. Those study designs also lacked a systematic and detailed literature search [12], or the search strategy involved limited databases [14], including quasi-randomized trials [11], 13] and case series or observational studies [12]. Previous reviews also excluded trials that compared different types of OMT or combined OMT [11], or their inclusion criteria were limited to specific OMT techniques [13]. Other limitations of previous reviews included the exclusion of patients with psychological or psychiatric conditions [11] or specific headache types, such as migraine headaches or cluster headaches [14]. Finally, many reviews lacked patient-important outcomes, such as RTW, disability, and QOL [11], 13], 14]. These limitations limited the overall generalizability and clinical implications of those reviews [11], [12], [13], [14] of headaches associated with musculoskeletal dysfunction treated with OMT.
To our knowledge, the current review is the first systematic review and meta-analysis to report pooled estimates of OMT’s impact in treating headaches associated with musculoskeletal disorders. We assessed the reported OMT techniques according to similarities between the types of OMT techniques and comparator interventions. As a result of this assessment and pooling of data based on similarities between technique types, heterogeneity in the meta-analysis was low. Additionally, the quality of evidence in the pooled analyses was determined utilizing the GRADE approach. The current review also evaluated the effectiveness of OMT techniques when treating headaches for outcomes that are important to patients, including headache severity, headache frequency, disability associated with headaches, QOL, and RTW. Similarly, we evaluated harm outcomes, including ACD rates and dropouts due to inefficacy or adverse effects, for a more patient-centred assessment of the use of OMT for treating headaches associated with musculoskeletal dysfunction. Most systematic reviews and meta-analyses focus on an intervention’s beneficial results, with little emphasis on the tolerability of the outcomes [53], [54], [55]. Further, less than 10 % of systematic reviews and meta-analyses evaluate harmful outcomes, such as ACD or dropouts from adverse effects and ineffectiveness [53], [54], [55]. This essential data are often missing from these studies because of inconsistent reporting of harm outcomes and a lack of standardized reporting methods [55]. A possible explanation for this omission is that including harmful outcomes leads to fewer eligible studies for review [56].
The treatment philosophy of any intervention, especially those utilized in osteopathic clinical practice, is based on safety, equitability, effectiveness, and patient-centeredness [57], 58]. Clinical guidelines recommend medications for the treatment of headaches of musculoskeletal origin [59], [60], [61], and different medications can be utilized to stop an acute headache, prevent recurrences, and reduce pain. Nonsteroidal anti-inflammatory drugs (NSAIDs) are the most commonly utilized medications to treat headache pain, but they are associated with adverse effects such as cardiovascular and gastrointestinal complications [59], [60], [61]. Therefore, guidelines also support nonpharmacological measures as part of headache treatment [61]. OMT is considered safe, with the adverse effects being relatively infrequent and minor [62], 63]. Degenhardt et al. [63] found that ART, HVLA, and ST, which were found in the current meta-analysis to be most effective against headaches, were reported as being less likely to produce adverse effects.
The current systematic review had several limitations. Like other systematic reviews, the results of the current review were affected by the inherent limitations of the reviewed RCTs. For example, none of the eligible trials met all of the ROB criteria. Most of the reviewed studies had high ROB and were downgraded for bias, such as lack of blinding. However, this limitation was expected because it is difficult in procedure-based RCTs to blind patients and practitioners completely. Another limitation of our review was that the reviewed studies lacked power, and seven studies [37], 38], [43], [44], [45, 47], 51] did not account for missing data. Further, small sample sizes can increase the risk of error by overestimating or underestimating the effect [64], 65]. Another limitation of our meta-analysis was the relatively small number of studies that specifically assessed osteopathic manipulation within the broader category of manual interventions. Among these, only two studies [44], 47] were performed by osteopathic physicians. Therefore, the reviewed studies focused more on the impact of OMT techniques rather than the holistic approach of osteopathic medicine. Additionally, 10 [37], [38], [39], [40], [41], [42], [43, [48], [49], [50] of the 18 reviewed studies were published by a single investigative team, which introduced a potential source of bias not accounted for by the GRADE criteria. We did not have enough studies to assess the effect of the OMT on RTW. Only one study [52] included in our review evaluated the effect of OMT on RTW and reported no association with days of disablement. As a study outcome, RTW is complex because it depends on many other factors, such as the complexity of the person’s work, psychological well-being, and positive attitude toward RTW [66], 67]. Evidence in pain research has shown that reduced pain severity and improved QOL are significant predictors of RTW [68]. Based on the results of the current review, future trials should consider assessing the effect of OMT on RTW, particularly in relation to headache severity and frequency.
Conclusions
The current systematic review and meta-analysis found moderate-quality evidence that utilizing a combination of OMT technique modalities was most effective for reducing the severity and frequency of headaches and for improving QOL. The current review also found no associations with ACD rates and dropouts due to inefficacy, which suggests that patients tolerated OMT well. Although our pooled meta-analyses showed a clear benefit of utilizing OMT for the treatment of headaches, our results also highlighted a need for more high-quality RCTs with larger sample sizes and a lower ROB to better define the effectiveness of OMT for treating headaches associated with musculoskeletal dysfunction.
Acknowledgments
The authors thank Deborah Goggin, MA, ELS (scientific writer from the Department of Research Support at A.T. Still University), for her editorial support.
-
Research ethics: Not applicable.
-
Informed consent: Not applicable.
-
Author contributions: The authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Use of Large Language Models, AI and Machine Learning Tools: None declared.
-
Conflict of interest: None declared.
-
Research funding: None declared.
-
Data availability: Raw data may be obtained on request from the corresponding author.
References
1. Stovner, LJ, Hagen, K, Linde, M, Steiner, TJ. The global prevalence of headache: an update, with analysis of the influences of methodological factors on prevalence estimates. J Headache Pain 2022;23:34. https://doi.org/10.1186/s10194-022-01402-2.Suche in Google Scholar PubMed PubMed Central
2. Leonardi, M, Raggi, A. A narrative review on the burden of migraine: when the burden is the impact on people’s life. J Headache Pain 2019;20:41. https://doi.org/10.1186/s10194-019-0993-0.Suche in Google Scholar PubMed PubMed Central
3. Yucel, A, Thach, A, Kumar, S, Loden, C, Bensink, M, Goldfarb, N. Estimating the economic burden of migraine on US employers. Am J Manag Care 2020;26:e403–8. https://doi.org/10.37765/ajmc.2020.88547.Suche in Google Scholar PubMed
4. Bonafede, M, Sapra, S, Shah, N, Tepper, S, Cappell, K, Desai, P. Direct and indirect healthcare resource utilization and costs among migraine patients in the United States. Headache 2018;58:700–14. https://doi.org/10.1111/head.13275.Suche in Google Scholar PubMed
5. Raval, AD, Shah, A. National trends in direct health care expenditures among US adults with migraine: 2004 to 2013. J Pain 2017;18:96–107. https://doi.org/10.1016/j.jpain.2016.10.005.Suche in Google Scholar PubMed
6. Messali, A, Sanderson, JC, Blumenfeld, AM, Goadsby, PJ, Buse, DC, Varon, SF, et al.. Direct and indirect costs of chronic and episodic migraine in the United States: a web-based survey. Headache 2016;56:306–22. https://doi.org/10.1111/head.12755.Suche in Google Scholar PubMed
7. Von Korff, M, Stewart, WF, Simon, DJ, Lipton, RB. Migraine and reduced work performance: a population-based diary study. Neurology 1998;50:1741–5. https://doi.org/10.1212/wnl.50.6.1741.Suche in Google Scholar PubMed
8. Taşkapilioğlu, Ö, Karli, N. Assessment of quality of life in migraine. Noro Psikiyatr Ars 2013;50:S60–4. https://doi.org/10.4274/Npa.y7310.Suche in Google Scholar PubMed PubMed Central
9. Steiner, TJ. Lifting the burden: the global campaign to reduce the burden of headache worldwide. J Headache Pain 2005;6:373–7. https://doi.org/10.1007/s10194-005-0241-7.Suche in Google Scholar PubMed PubMed Central
10. Steiner, TJ, Birbeck, GL, Jensen, R, Katsarava, Z, Martelletti, P, Stovner, LJ. Lifting the burden: the first 7 years. J Headache Pain 2010;11:451–5. https://doi.org/10.1007/s10194-010-0264-6.Suche in Google Scholar PubMed PubMed Central
11. Cerritelli, F, Lacorte, E, Ruffini, N, Vanacore, N. Osteopathy for primary headache patients: a systematic review. J Pain Res 2017;10:601–11. https://doi.org/10.2147/jpr.S130501.Suche in Google Scholar PubMed PubMed Central
12. Jara Silva, CE, Joseph, AM, Khatib, M, Knafo, J, Karas, M, Krupa, K, et al.. Osteopathic manipulative treatment and the management of headaches: a scoping review. Cureus 2022;14:e27830. https://doi.org/10.7759/cureus.27830.Suche in Google Scholar PubMed PubMed Central
13. Posadzki, P, Ernst, E. Spinal manipulations for cervicogenic headaches: a systematic review of randomized clinical trials. Headache 2011;51:1132–9. https://doi.org/10.1111/j.1526-4610.2011.01932.x.Suche in Google Scholar PubMed
14. Vernon, H, McDermaid, CS, Hagino, C. Systematic review of randomized clinical trials of complementary/alternative therapies in the treatment of tension-type and cervicogenic headache. Compl Ther Med 1999;7:142–55. https://doi.org/10.1016/s0965-2299(99)80122-8.Suche in Google Scholar PubMed
15. Cumpston, M, Li, T, Page, MJ, Chandler, J, Welch, VA, Higgins, JP, et al.. Updated guidance for trusted systematic reviews: a new edition of the Cochrane handbook for systematic reviews of interventions. Cochrane Database Syst Rev 2019;10:ED000142. https://doi.org/10.1002/14651858.Ed000142.Suche in Google Scholar
16. Higgins, JPT, Thomas, J, Chandler, J, Cumpston, M, Li, T, Page, MJ, editors, et al.. Cochrane handbook for systematic reviews of interventions, 2nd ed. Chichester, UK: John Wiley & Sons; 2019.10.1002/9781119536604Suche in Google Scholar
17. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al.. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. https://doi.org/10.1136/bmj.n71.Suche in Google Scholar PubMed PubMed Central
18. Headache Classification Committee of the International Headache Society (IHS). The international classification of headache disorders, 3rd edition. Cephalalgia 2018:1–211. https://doi.org/10.1177/0333102417738202.Suche in Google Scholar PubMed
19. Giusti, R, editor. Glossary of osteopathic terminology, 3rd ed. Chevy Chase, MD: American Association of Colleges of Osteopathic Medicine; 2017.Suche in Google Scholar
20. Franke, H, Franke, JD, Fryer, G. Osteopathic manipulative treatment for chronic nonspecific neck pain: a systematic review and meta-analysis. Int J Osteopath Med 2015;18:255–67. https://doi.org/10.1016/j.ijosm.2015.05.003.Suche in Google Scholar
21. Franke, H, Franke, JD, Fryer, G. Osteopathic manipulative treatment for nonspecific low back pain: a systematic review and meta-analysis. BMC Muscoskelet Disord 2014;15:286. https://doi.org/10.1186/1471-2474-15-286.Suche in Google Scholar PubMed PubMed Central
22. Licciardone, JC. Systematic review and meta-analysis conclusions relating to osteopathic manipulative treatment for low back pain remain valid and well accepted. J Bodyw Mov Ther 2013;17:2–4. https://doi.org/10.1016/j.jbmt.2012.10.003.Suche in Google Scholar PubMed
23. Rehman, Y, Ferguson, H, Bozek, A, Blair, J, Allison, A, Johnston, R. Dropout associated with osteopathic manual treatment for chronic noncancerous pain in randomized controlled trials. J Osteopath Med 2021;121:417–28. https://doi.org/10.1515/jom-2020-0240.Suche in Google Scholar PubMed
24. Rehman, Y, Ferguson, H, Bozek, A, Blair, J, Allison, A, Johnston, R. Osteopathic manual treatment for pain severity, functional improvement, and return to work in patients with chronic pain. J Am Osteopath Assoc 2020;120:888–906. https://doi.org/10.7556/jaoa.2020.128.Suche in Google Scholar PubMed
25. Rehman, Y, Kirsch, J, Snider, KT. Response to “osteopathic manipulative techniques in the treatment of vestibular dizziness not related to the cervical spine”. J Osteopath Med 2023;123:277–8. https://doi.org/10.1515/jom-2023-0010.Suche in Google Scholar PubMed
26. Landis, JR, Koch, GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159–74. https://doi.org/10.2307/2529310.Suche in Google Scholar
27. Higgins, JPT, Thompson, SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002;21:1539–58. https://doi.org/10.1002/sim.1186.Suche in Google Scholar PubMed
28. Higgins, JPT, Thompson, SG, Deeks, JJ, Altman, DG. Measuring inconsistency in meta-analyses. BMJ 2003;327:557–60. https://doi.org/10.1136/bmj.327.7414.557.Suche in Google Scholar PubMed PubMed Central
29. Akl, EA, Sun, X, Busse, JW, Johnston, BC, Briel, M, Mulla, S, et al.. Specific instructions for estimating unclearly reported blinding status in randomized trials were reliable and valid. J Clin Epidemiol 2012;65:262–7. https://doi.org/10.1016/j.jclinepi.2011.04.015.Suche in Google Scholar PubMed
30. Higgins, JPT, Altman, DG, Gøtzsche, PC, Juni, P, Moher, D, Oxman, AD, et al.. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. https://doi.org/10.1136/bmj.d5928.Suche in Google Scholar PubMed PubMed Central
31. Guyatt, GH, Oxman, AD, Kunz, R, Falck-Ytter, Y, Vist, GE, Liberati, A, et al.. Going from evidence to recommendations. BMJ 2008;336:1049–51. https://doi.org/10.1136/bmj.39493.646875.AE.Suche in Google Scholar PubMed PubMed Central
32. Guyatt, GH, Oxman, AD, Kunz, R, Vist, GE, Falck-Ytter, Y, Schünemann, HJ. What is “quality of evidence” and why is it important to clinicians? BMJ 2008;336:995–8. https://doi.org/10.1136/bmj.39490.551019.BE.Suche in Google Scholar PubMed PubMed Central
33. Guyatt, GH, Oxman, AD, Vist, GE, Kunz, R, Falck-Ytter, Y, Alonso-Coello, P, et al.. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336:924–6. https://doi.org/10.1136/bmj.39489.470347. AD.Suche in Google Scholar
34. Balduzzi, S, Rücker, G, Schwarzer, G. How to perform a meta-analysis with R: a practical tutorial. Evid Base Ment Health 2019;22:153–60. https://doi.org/10.1136/ebmental-2019-300117.Suche in Google Scholar PubMed PubMed Central
35. Cerritelli, F, Ginevri, L, Messi, G, Caprari, E, Di Vincenzo, M, Renzetti, C, et al.. Clinical effectiveness of osteopathic treatment in chronic migraine: 3-armed randomized controlled trial. Compl Ther Med 2015;23:149–56. https://doi.org/10.1016/j.ctim.2015.01.011.Suche in Google Scholar PubMed
36. Deodato, M, Guolo, F, Monticco, A, Fornari, M, Manganotti, P, Granato, A. Osteopathic manipulative therapy in patients with chronic tension-type headache: a pilot study. J Am Osteopath Assoc 2019;119:682–7. https://doi.org/10.7556/jaoa.2019.093.Suche in Google Scholar PubMed
37. Espí-López, GV, Gómez-Conesa, A. Efficacy of manual and manipulative therapy in the perception of pain and cervical motion in patients with tension-type headache: a randomized, controlled clinical trial. J Chiropr Med 2014;13:4–13. https://doi.org/10.1016/j.jcm.2014.01.004.Suche in Google Scholar PubMed PubMed Central
38. Espí-López, GV, Gómez-Conesa, A, Gómez, AA, Martínez, JB, Pascual-Vaca, AO, Blanco, CR. Treatment of tension-type headache with articulatory and suboccipital soft tissue therapy: a double-blind, randomized, placebo-controlled clinical trial. J Bodyw Mov Ther 2014;18:576–85. https://doi.org/10.1016/j.jbmt.2014.01.001.Suche in Google Scholar PubMed
39. Espi-Lopez, GV, Ingles, M, Carrasco-Fernandez, JJ, Serra-Añó, P, Copete-Fajardo, L, Gonzalez-Gerez, JJ, et al.. Effects of foam rolling vs. manual therapy in patients with tension-type headache: a randomized pilot study. J Clin Med 2022;11:1778. https://doi.org/10.3390/jcm11071778.Suche in Google Scholar PubMed PubMed Central
40. Espí-López, GV, Rodríguez-Blanco, C, Oliva-Pascual-Vaca, A, Benítez-Martínez, JC, Lluch, E, Falla, D. Effect of manual therapy techniques on headache disability in patients with tension-type headache. Randomized controlled trial. Eur J Phys Rehabil Med 2014;50:641–7.Suche in Google Scholar
41. Espí-López, GV, Rodríguez-Blanco, C, Oliva-Pascual-Vaca, A, Molina-Martínez, F, Falla, D. Do manual therapy techniques have a positive effect on quality of life in people with tension-type headache? A randomized controlled trial. Eur J Phys Rehabil Med 2016;52:447–56.Suche in Google Scholar
42. Espí-López, GV, Ruescas-Nicolau, MA, Nova-Redondo, C, Benítez-Martínez, JC, Dugailly, PM, Falla, D. Effect of soft tissue techniques on headache impact, disability, and quality of life in migraine sufferers: a pilot study. J Alternative Compl Med 2018;24:1099–107. https://doi.org/10.1089/acm.2018.0048.Suche in Google Scholar PubMed
43. Espí-López, GV, Zurriaga-Llorens, R, Monzani, L, Falla, D. The effect of manipulation plus massage therapy versus massage therapy alone in people with tension-type headache. A randomized controlled clinical trial. Eur J Phys Rehabil Med 2016;52:606–17.Suche in Google Scholar
44. Esterov, D, Thomas, A, Weiss, K. Osteopathic manipulative medicine in the management of headaches associated with postconcussion syndrome. J Osteopath Med 2021;121:651–6. https://doi.org/10.1515/jom-2020-0035.Suche in Google Scholar PubMed
45. Fernández-de-las-Peñas, C, Fernández-Carnero, J, Fernández, AP, Lomas-Vega, R, Miangolarra-Page, JC. Dorsal manipulation in whiplash injury treatment: a randomized controlled trial. J Whiplash Relat Disord 2004;3:55–72. https://doi.org/10.1300/J180v03n02_05.Suche in Google Scholar
46. Gandolfi, M, Geroin, C, Valè, N, Marchioretto, F, Turrina, A, Dimitrova, E, et al.. Does myofascial and trigger point treatment reduce pain and analgesic intake in patients undergoing onabotulinumtoxinA injection due to chronic intractable migraine? Eur J Phys Rehabil Med 2018;54:1–12. https://doi.org/10.23736/S1973-9087.17.04568-3.Suche in Google Scholar PubMed
47. Hoyt, WH, Shaffer, F, Bard, DA, Benesler, JS, Blankenhorn, GD, Gray, JH, et al.. Osteopathic manipulation in the treatment of muscle-contraction headache. J Am Osteopath Assoc 1979;78:322–5.Suche in Google Scholar
48. Muñoz-Gómez, E, Inglés, M, Aguilar-Rodríguez, M, Mollà-Casanova, S, Sempere-Rubio, N, Serra-Añó, P, et al.. Effect of a craniosacral therapy protocol in people with migraine: a randomized controlled trial. J Clin Med 2022;11:759. https://doi.org/10.3390/jcm11030759.Suche in Google Scholar PubMed PubMed Central
49. Muñoz-Gómez, E, Inglés, M, Serra-Añó, P, Espí-López, GV. Effectiveness of a manual therapy protocol based on articulatory techniques in migraine patients. A randomized controlled trial. Musculoskelet Sci Pract 2021;54:102386. https://doi.org/10.1016/j.msksp.2021.102386.Suche in Google Scholar PubMed
50. Muñoz-Gómez, E, Serra-Añó, P, Mollà-Casanova, S, Sempere-Rubio, N, Aguilar-Rodríguez, M, Espí-López, GV, et al.. Potential add-on effects of manual therapy techniques in migraine patients: a randomised controlled trial. J Clin Med 2022;11:4686. https://doi.org/10.3390/jcm11164686.Suche in Google Scholar PubMed PubMed Central
51. Rolle, G, Tremolizzo, L, Somalvico, F, Ferrarese, C, Bressan, LC. Pilot trial of osteopathic manipulative therapy for patients with frequent episodic tension-type headache. J Am Osteopath Assoc 2014;114:678–85. https://doi.org/10.7556/jaoa.2014.136.Suche in Google Scholar PubMed
52. Voigt, K, Liebnitzky, J, Burmeister, U, Sihvonen-Riemenschneider, H, Beck, M, Voigt, R, et al.. Efficacy of osteopathic manipulative treatment of female patients with migraine: results of a randomized controlled trial. J Alternative Compl Med 2011;17:225–30. https://doi.org/10.1089/acm.2009.0673.Suche in Google Scholar PubMed
53. McIntosh, HM, Woolacott, NF, Bagnall, AM. Assessing harmful effects in systematic reviews. BMC Med Res Methodol 2004;4:19. https://doi.org/10.1186/1471-2288-4-19.Suche in Google Scholar PubMed PubMed Central
54. Ernst, E, Pittler, MH. Assessment of therapeutic safety in systematic reviews: literature review. BMJ 2001;323:546. https://doi.org/10.1136/bmj.323.7312.546.Suche in Google Scholar PubMed PubMed Central
55. Zorzela, L, Golder, S, Liu, Y, Pilkington, K, Hartling, L, Joffe, A, et al.. Quality of reporting in systematic reviews of adverse events: systematic review. BMJ 2014;348:f7668. https://doi.org/10.1136/bmj.f7668.Suche in Google Scholar PubMed PubMed Central
56. Saldanha, IJ, Lindsley, KB, Money, S, Kimmel, HJ, Smith, BT, Dickersin, K. Outcome choice and definition in systematic reviews leads to few eligible studies included in meta-analyses: a case study. BMC Med Res Methodol 2020;20:30. https://doi.org/10.1186/s12874-020-0898-2.Suche in Google Scholar PubMed PubMed Central
57. Steel, A, Blaich, R, Sundberg, T, Adams, J. The role of osteopathy in clinical care: broadening the evidence-base. Int J Osteopath Med 2017;24:32–6. https://doi.org/10.1016/j.ijosm.2017.02.002.Suche in Google Scholar
58. Carnes, D. What can osteopaths learn from concerns and complaints raised against them? A review of insurance and regulator reports. Int J Osteopath Med 2016;22:3–10. https://doi.org/10.1016/j.ijosm.2016.07.002.Suche in Google Scholar
59. Sico, JJ, Antonovich, NM, Ballard-Hernandez, J, Buelt, AC, Grinberg, AS, Macedo, FJ, et al., 2023 US Department of Veterans Affairs and US Department of Defense clinical practice guideline for the management of headache. Ann Intern Med. 2024/12/17 2024;177:1675-94. https://doi.org/10.7326/ANNALS-24-00551.Suche in Google Scholar PubMed
60. Ailani, J, Burch, RC, Robbins, MS, Board of Directors of the American Headache Society. The American Headache Society Consensus Statement: update on integrating new migraine treatments into clinical practice. Headache 2021;61:1021–39. https://doi.org/10.1111/head.14153.Suche in Google Scholar PubMed
61. Stevens, C. Brenner and Stevens’ pharmacology, 6th ed. Elsevier; 2022:339–46 pp. (chap. 29).Suche in Google Scholar
62. Bagagiolo, D, Rosa, D, Borrelli, F. Efficacy and safety of osteopathic manipulative treatment: an overview of systematic reviews. BMJ Open 2022;12:e053468. https://doi.org/10.1136/bmjopen-2021-053468.Suche in Google Scholar PubMed PubMed Central
63. Degenhardt, BF, Johnson, JC, Brooks, WJ, Norman, L. Characterizing adverse events reported immediately after osteopathic manipulative treatment. J Am Osteopath Assoc. 2018;118:141-9. https://doi.org/10.7556/jaoa.2018.033.Suche in Google Scholar PubMed
64. Faber, J, Fonseca, LM. How sample size influences research outcomes. Dental Press J Orthod 2014;19:27–9. https://doi.org/10.1590/2176-9451.19.4.027-029.ebo.Suche in Google Scholar PubMed PubMed Central
65. McNeish, DM, Stapleton, LM. The effect of small sample size on two-level model estimates: a review and illustration. Educ Psychol Rev 2016/06/01 2016;28:295–314. https://doi.org/10.1007/s10648-014-9287-x.Suche in Google Scholar
66. Hedlund, Å, Kristofferzon, ML, Boman, E, Nilsson, A. Are return to work beliefs, psychological well-being and perceived health related to return-to-work intentions among women on long-term sick leave for common mental disorders? A cross-sectional study based on the theory of planned behaviour. BMC Public Health 2021;21:535. https://doi.org/10.1186/s12889-021-10562-w.Suche in Google Scholar PubMed PubMed Central
67. Hedlund, Å, Nilsson, A, Boman, E, Kristofferzon, ML. Predictors of return to work and psychological well-being among women during/after long-term sick leave due to common mental disorders: a prospective cohort study based on the theory of planned behaviour. Health Soc Care Community 2022;30:e5245–58. https://doi.org/10.1111/hsc.13943.Suche in Google Scholar PubMed PubMed Central
68. Figueredo, JM, García-Ael, C, Gragnano, A, Topa, G. Well-being at work after return to work (RTW): a systematic review. Int J Environ Res Publ Health 2020;17:7490. https://doi.org/10.3390/ijerph17207490.Suche in Google Scholar PubMed PubMed Central
Supplementary Material
This article contains supplementary material (https://doi.org/10.1515/jom-2025-0075).
© 2025 the author(s), published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.

