Abstract
Context
Few osteopathic physicians (Doctors of Osteopathic Medicine [DOs]) utilize osteopathic manipulative treatment (OMT) in their clinical practice, although all DOs are trained to do so. The reasons why many do not utilize OMT are not entirely clear. Anecdotally, these authors have observed that if a physician utilizes OMT, it is because they witnessed the efficacy for themselves in real-life clinical diagnoses found on patients or volunteers. This study seeks to explore this phenomenon.
Objectives
This study seeks to explore the relationship between witnessing the efficacy of OMT and the future use of OMT in clinical practice.
Methods
Surveys were sent to DOs who work with Des Moines University’s College of Osteopathic Medicine (COM) clinical students as well as osteopathic medical students enrolled at the Des Moines University’s COM. Survey data were analyzed by separating physicians into cohorts based on their use of OMT and students into cohorts based on their interest in utilizing OMT in future practice.
Results
DOs who practice OMT reported at least one, and often multiple, instances of witnessing the efficacy of OMT on real-life patients or volunteers while in their first 2 years of medical school. Those who do not utilize OMT reported few opportunities to witness the efficacy of OMT on a real-life patient. For physicians, 96.1 % of those who utilize OMT in their practice had the opportunity to see it work positively during the first 2 years of medical school, whereas only 7.4 % who do not utilize OMT had the opportunity. These findings are mirrored in the experience of current osteopathic medical students who are interested and uninterested in utilizing OMT in their future practice.
Conclusions
These findings emphasize the importance of exposing our medical students to some type of ‘real-life’ experience early in their careers; the data show that these experiences can be very beneficial in expanding the interest in utilizing osteopathic manipulative medicine (OMM) in future practice. COMs can consider the implementation of programs that provide this experience to students, including extracurricular activities dedicated to the use of OMT.
Osteopathic manipulative treatment (OMT) is a vital and effective procedure taught to osteopathic physicians (Doctors of Osteopathic Medicine [DOs]) 1], [2], [3], [4. However, it is practiced by very few DOs [5]. Only about 6.1 % of respondents to a 2018 American Osteopathic Association (AOA) survey practice OMT on at least 5 % of their patients. The authors of the paper commented that the use of OMT among physicians continues to decline (Figures 1 and 2).
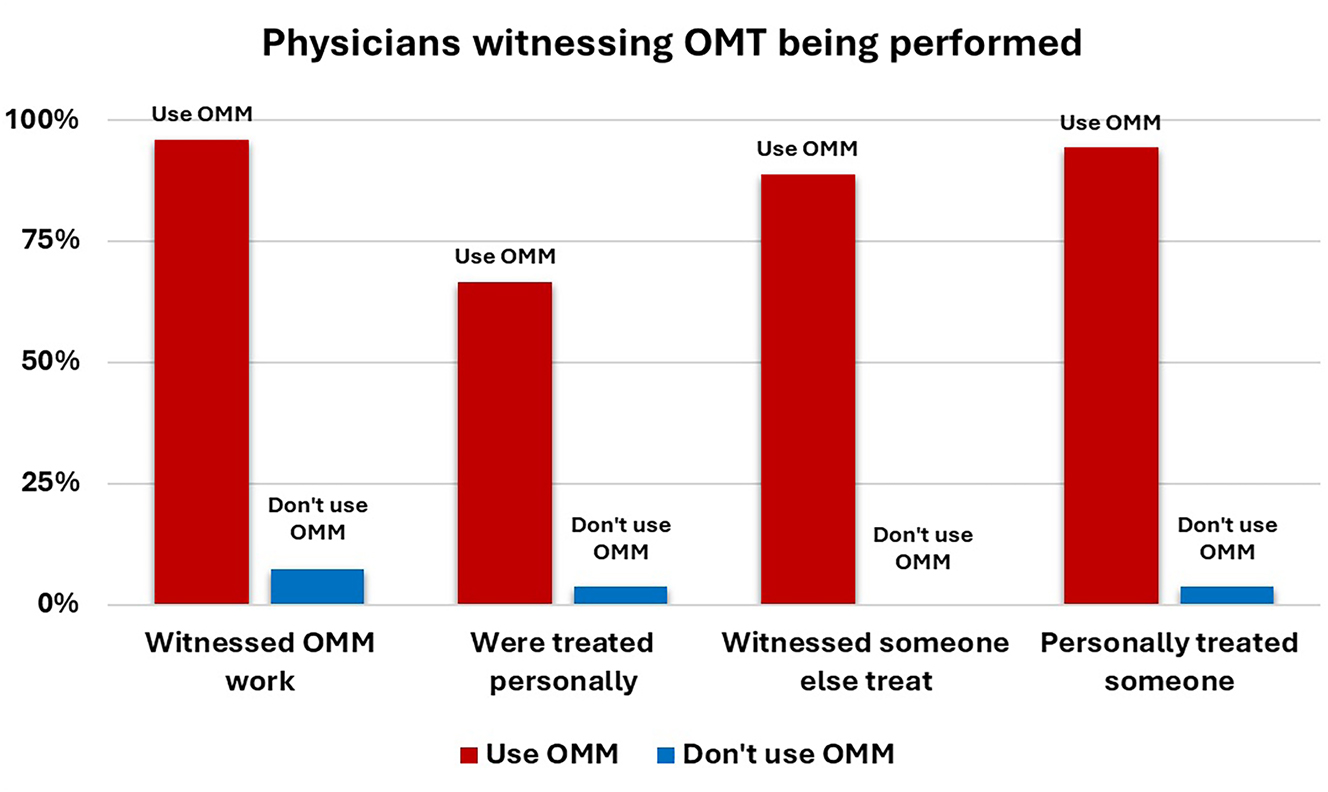
A comparison of physicians witnessing OMT being performed.
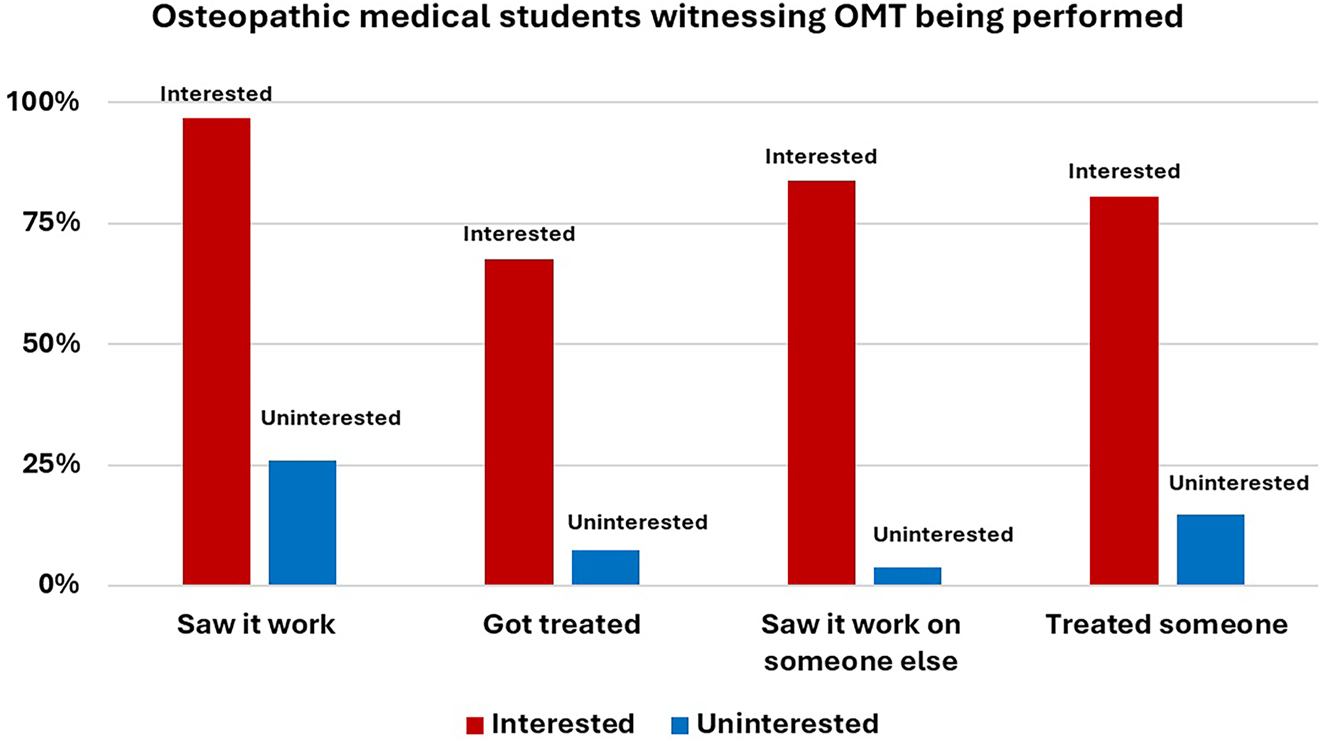
A comparison of medical student respondents regarding witnessing OMT being performed in an extracurricular (TOPPS, OFL, etc.) setting.
In these authors’ opinions, interest in utilizing OMT must be fostered in medical school, especially in the didactic years before the students go out into clerkships. This opinion is consistent with a review conducted in 2020 done by Snider et al. [6] of medical education practice patterns in osteopathic schools. Third- and fourth-year students are given very little direction in OMT. The AOA Commission on Osteopathic College Accreditation (COCA) requires supervised hands-on OMT training in each year of education [7] but does not specify the method of training and does not require the training to be comprehensive or thorough. This training is, therefore, often superficial, given that most rotations are supervised by physicians who do not understand OMT. Some schools require logs of patient treatments while out on clerkship to meet COCA standards. The value of OMT instruction within this model varies widely based on student confidence going into clerkships, the geographic location of clerkships [6], and whether the preceptor is a DO or an allopathic physician (MD).
Observations during 20 years of being involved in undergraduate and graduate medical education (GME) have yielded the concept of IEAP [8], in which “I” means information, “E” means experience, “A” means acceptance, and “P” means practice. This is the succession of events needed to occur for a physician to learn and practice medicine. They need to sequentially acquire basic information (I), then experience those concepts working positively on patients (E) during rotations, then accept (A) the treatments taught as valid, before they decide on utilizing them in their practice (P). In these authors’ opinion, there is a simple task in fostering interest in OMT. This task is consistent for any treatment modality that students learn in medicine, including pharmaceuticals and surgery. The student needs to see a treatment, in this case OMT, work and produce positive outcomes to consider utilizing that treatment in future practice. Conversely, if a student never sees a medication work, that student is highly unlikely to utilize that treatment regardless of the amount of data in favor of that medication. Anecdotally, these authors have found that every practitioner of OMT has one or more experiences in which they saw OMT contribute partially or completely in the healing of a medical diagnosis, which prompted them to further learn it and utilize it.
When it comes to OMT, there have already been studies to this effect, especially focusing on formal OMT clerkships. One study found that great gains in confidence were achieved by the third week of a 4-week immersive OMT rotation in the clinical years [9]. Anecdotally, these authors have seen that outside these immersive OMT clerkships, students’ opportunities to perform OMT in third- and fourth-year rotations are highly dependent on the individual students’ motivation to do so, and this motivation is not fostered unless the student has seen OMT work positively before the clinical years.
Also, anecdotally, these authors found that most DO preceptors have not practiced OMT since the end of their second year, and yet allow motivated students they precept to practice OMT. This is also true of some MD preceptors. MDs do not receive formal education in OMT during medical school. However, in some cases, the MD preceptors are encouraging their DO students to perform OMT.
Some DO schools have created several extracurricular activities to give students this opportunity to see OMT work on volunteers who are not their fellow student lab partners. The volunteers have clinical problems that they seek to solve with the application of OMT. One such extracurricular activity is Teaching Osteopathic Principles and Practice to Students (TOPPS). TOPPS brings members of the school community, neighboring university students, and Amish volunteers (of all ages) to campus so that students can provide supervised OMT treatments to them for a variety of conditions. These activities allow students (mostly first- and second-year students) to see OMT work in practice addressing real-life clinical medical diagnoses. These authors have witnessed an increase in enthusiasm for OMT among participating students as a result of their engagement in these activities.
The current study is a survey conducted of current osteopathic medical students and practicing osteopathic physicians. The study gauges student interest in OMT and investigates why they are or are not interested in utilizing OMT in future practice, and if their participation in these extra-curricular activities fostered those reasons. The physician survey gauged whether the physician utilizes OMT in their practice and what fostered their interest in OMT, specifically if treating volunteers in school impacted them.
Methods
Institutional Review Board (IRB) approval was requested for this study from the Des Moines University Office of Research, and the board deemed the methods exempt. A survey was given to practicing osteopathic physicians. A separate survey was sent to current osteopathic medical students. Informed consent was obtained from the participants for these surveys before they were conducted. All Likert scales were nine-point scales in which “1” indicated no interest and “9” indicated high interest [10]. A nine-point Likert scale was chosen to include a midpoint for those respondents with “neutral” or “undecided” opinions and to offer more variance to these respondents and give a higher degree of precision in measuring opinions. This nine-point scale retains its validity when surveying populations of highly educated participants, which we assume in these groups of physicians and medical students. Surveys were sent out and resulted in April/May 2022.
Physicians
Surveys, found in Appendix A, were distributed to 1,443 practicing DOs. These physicians were registered with Des Moines University as preceptors for student clerkships. Board-certified and board-eligible were included. Allopathic physicians were excluded because physicians trained in OMT were targeted. Physicians whose email addresses returned as disabled or undeliverable were excluded. No reminders were sent via email. A total of 76 physicians responded, giving a response rate of 5.27 %. The survey included a yes/no question about the use of OMT in current practice. It included a question about the respondent’s ability to treat volunteers, who were not their lab partners, utilizing OMT in the first 2 years of medical school. A Likert scale was included to assess the influence of these extracurricular activities in their practice of OMT.
Respondents who do not practice OMT were asked their general reasons why they do not practice OMT. Respondents who do practice OMT were asked their general reasons for practicing OMT.
Students
Surveys, found in Appendix B, were distributed to 884 current osteopathic medical students. Students were currently registered in the DO program at Des Moines University. Students in any year of training were included. Students in dual-degree programs were included as long as one of their registered programs was DO. Students whose email addresses returned disabled or undeliverable were excluded. No reminders were sent via email. A total of 57 students responded, which was a response rate of 6.45 %. Respondents were asked a yes/no question about whether they had an opportunity to treat volunteers, who were not their lab partners, utilizing OMT in the first 2 years of school. A Likert scale was utilized to assess their interest in utilizing OMT in their future practice. Scoring 6 or higher was deemed as interested in utilizing OMT. Scoring 5 (neutral) or below was deemed as not interested in utilizing OMT [10].
Student respondents who are generally interested in practicing OMT in the future were asked the reasons why they are interested. If a respondent participated in extracurricular activities offered, they were asked what skills in OMT they believed they gained through the experience. Respondents who are not interested in practicing OMT were asked the reasons why they are not interested.
Survey tool
The digital survey tool “Qualtrics Experience Management” was utilized to generate and administer the survey, found in the Appendices. Physicians were sent one version of the survey, and students were sent another version.
The physician survey began with demographic data gathering including specialty, years in practice, and whether or not they utilize OMT in their medical practice. They were then asked a yes or no question whether they were able to, in their first 2 years of medical school, treat someone that was not their lab partner with OMT. They were asked whether this experience influenced them to utilize OMT on a Likert scale. Next, respondents were asked what exposure to extracurricular OMT they had in the first 2 years of medical school.
Student respondents were likewise asked for demographic information consisting of year in school and whether they were able to attend extracurricular OMT events such as TOPPS and Osteopathic Finish Lines (OFLs). They were then asked whether they were interested in utilizing OMT on a Likert scale. Respondents were then asked about their exposure to witnessing the efficacy of OMT. Students who did attend extracurricular OMT events were asked what skills they believe they gained through their participation.
Analysis
Analysis of the data was performed through Microsoft Excel spreadsheet functions. Physician respondent data was divided by use or nonuse of OMT and analyzed separately. Use vs. nonuse was decided through a yes or no question on respondents’ use. The data were aggregated within these groups and analyzed separately. Total outcomes were then compared between groups. The student respondent data were divided by interest or disinterest in utilizing OMT in future practice utilizing Likert scales as above.
Statistical analysis included percentage comparison, standard deviation, and chi-square test. Additionally, a variation of “Number Needed to Treat” (NNT) was utilized. NNT is a test of population effect and is commonly utilized in reporting the efficacy of new drugs or comparing procedures [11]. The number is reported as a positive number greater than or equal to 1, and the closer to one the number is, the more powerful the population effect. For example, a new intervention with NNT=2 means that for every two people who receive the intervention, one person has a positive effect. A new intervention with NNT=600 means that for every 600 people who receive the intervention, one person has a positive effect. A perfect intervention would have NNT=1, for which every person who receives the intervention is helped. In the case of this study, we utilize a “Number Needed to Expose” (NNE). This means that we are measuring the population effect of exposure to seeing OMT work positively in real life. For every X number of physicians or students who are exposed to seeing OMT work positively, one physician or student will utilize OMT in their future careers.
Results
Physicians
Among the physicians who responded to the survey, 67.1 % utilize OMT in their current practice. Among those physicians who utilize OMT, 96.1 % reported an instance of witnessing OMT work outside of the lab while in the first 2 years of medical school. A brief breakdown of those instances is shown in Table 1.
Left column: responses from physicians who utilize OMT regarding if and how they witnessed OMT work. Right column: responses from physicians who do not utilize OMT regarding if and how they witnessed OMT being utilized.
| Physician respondents | |||
|---|---|---|---|
| Witnessed OMT work | 96.10 % | Opportunity to see it work | 7.41 % |
| Were treated personally | 66.70 % | Were treated personally | 3.70 % |
| Witnessed someone else treating | 88.90 % | Witnessed someone else treating | 0.00 % |
| Personally treated someone | 94.40 % | Personally treated someone | 3.70 % |
|
|
|||
| Number of answers chosen | Reasons to not utilize OMT | ||
|
|
|||
| Average number of answersa | 2.45 | Lack of time to treat | 29.63 % |
| Did not report these choices | 2 | Poor reimbursement | 3.70 % |
| Not appropriate to specialty | 29.60 % | ||
| Respondent not skilled enough | 14.80 % | ||
-
aThe survey had three choices in which they could choose all that apply. The average number of choices from those three was 2.45. OMT, osteopathic manipulative treatment.
Among the physicians who responded to the survey, 32.9 % do not utilize OMT in their current practice. Among those physicians, 7.4 % reported having the opportunity to witness OMT work outside of the lab while in the first 2 years of medical school. A brief breakdown of those opportunities is shown in Table 1.
Each group was also asked if the principles of OMT make sense to them from a medical standpoint. Among physicians who utilize OMT, 85.0 % reported that osteopathic principles make sense to them medically. Among physicians who do not utilize OMT, 22.2 % reported that osteopathic principles do not make sense to them from a medical standpoint, meaning that 77.8 % are either ambivalent or the principles do make medical sense.
Of note, respondents who reported that OMT is not appropriate to their specialty worked as either psychiatrists or orthopedic surgeons. The psychiatrists cited the importance of boundaries with their patients, and orthopedic surgeons cited their ability to fix their patients’ musculoskeletal issues with surgery.
Students
Just over half (53.5 %) of students indicated interest in utilizing OMT in their future practice. Among these students, 96.8 % reported that they had witnessed OMT work in the first 2 years of medical school through extracurricular settings such as TOPPS and OFLs. A breakdown of these instances is shown in Table 2.
Left column: responses from students who are interested in utilizing OMT in future practice regarding if and how they witnessed OMT work. Responses from students who attended extracurricular OMT events indicating what skills they gained. Right column: responses from students who are not interested in OMT in future practice regarding how they witnessed OMT being utilized.
| Witnessed OMT work | 96.80 % | Opportunity to see it work | 25.90 % |
|---|---|---|---|
| Were treated personally | 67.70 % | Was treated personally | 7.40 % |
| Witnessed someone else treating | 83.90 % | Witnessed someone else treating | 3.70 % |
| Treated someone personally | 80.60 % | Treated someone personally | 14.80 % |
| Average answersa | 2.32 | ||
| Did not report these choices | 1 | ||
|
|
|||
| Skills gained | Percent | ||
|
|
|||
| Problem-solving of somatic dysfunctions | 74.20 % | ||
| Correlating medical diagnoses to somatic dysfunctions | 38.70 % | ||
| More effective osteopathic treatment | 51.60 % | ||
| Diagnostic accuracy for somatic dysfunctions | 54.80 % | ||
| Other (self-reported confidence in ability to perform OMT) | 6.50 % | ||
| Average answers | |||
-
aThe survey had three choices in which they could choose all that apply. The average number of choices from those three was 2.32. OMT, osteopathic manipulative treatment.
Nearly half (46.5 %) of students indicated little to no interest in utilizing OMT in their future practice. Among these students, 25.9 % reported having an opportunity to see OMT work outside the lab in the first 2 years of medical school. A breakdown of these opportunities is shown in Table 2.
Additionally, students who did attend extracurricular events in which they utilized OMT were asked if they gained specific skills in OMT and what those skills were. These responses are shown in Table 2.
Discussion
Almost all physician respondents who practice OMT (96.1 %) had the opportunity to witness the efficacy of OMT. These physicians reported a high incidence of witnessing successful OMT treatment. The average number of concurrent responses was 2.45 out of three choices, indicating that physicians who utilize OMT witnessed it work in more than one type of event.
Very few physician respondents who do not practice OMT (7.4 %) had the opportunity to witness the efficacy of OMT. The physicians reported low incidence of witnessing OMT being performed. These physicians self-reported their reasons for not practicing OMT. These reasons included a lack of clinical time to perform treatments, poor reimbursement, finding OMT inappropriate to their specialty, and feeling they are not skilled enough in OMT to perform well.
A chi-square test showed that physicians who utilize OMT were more likely to have witnessed the efficacy of OMT on a real-life patient: chi-square (1, n=76)=60.43, p<0.00001. An NNE calculation was performed yielding a result of NNE=1.1. Keeping in mind that a perfect intervention yielding NNE=1.0, witnessing OMT efficacy is a near-perfect intervention for promoting the use of OMT in medical practice.
Almost all student respondents who are interested in utilizing OMT in future practice (96.8 %) had the opportunity to witness the efficacy of OMT. Few student respondents who are not interested in utilizing OMT in future practice (25.9 %) had the opportunity to witness the efficacy of OMT in the first 2 years of medical school. This result shows the importance of early intervention with opportunities to witness the efficacy of OMT.
Those students who are interested in utilizing OMT in the future reported a high incidence of witnessing successful OMT treatment. The average number of concurrent responses was 2.32 out of three choices, indicating that physicians who utilize OMT witnessed it work in more than one type of event. This result shows that the manner of witnessing OMT work in real-life does not need to be fully standardized, as multiple manners are reported by students as being influential in their interest in utilizing OMT in future practice.
Those students who are not interested in utilizing OMT in the future reported low incidence of witnessing OMT being performed.
A chi-square test showed that those who are interested in utilizing OMT in future practice were more likely to have witnessed the efficacy of OMT on a real-life patient in the first 2 years of medical school chi-square(1, n=58)=31.36, p<0.00001. An NNE calculation was performed yielding a result of NNE=1.4. Again, keeping in mind that a perfect intervention yields NNE=1.0, witnessing OMT work appears to be a near-perfect intervention for instilling interest into medical students.
There are limitations to this study and the possibility to expand it. Limitations include this survey being conducted at one university targeting only its students and affiliates. A multisite or national study at other Colleges of Osteopathic Medicine (COMs) would reveal multi-regional trends and capture more widespread views of OMT. The overall response rate of this study was relatively low and could have contributed to nonresponse and selection bias. The response rate could be improved by including students and graduated DOs from other COMs and by providing completion reminders and incentives. Additionally, although allopathic physicians were left out of this study due to variability in OMT exposure and training, a larger study with the resources to vet the training of allopathic physicians who learned OMT after graduating medical school and explore why they electively sought such training could be beneficial to the broader use of OMT.
Conclusions
The results of this study indicate that witnessing OMT work successfully outside of curriculum labs is predictive of future use of OMT in clinical practice. These results are also reflected in current osteopathic medical students and their interest in utilizing OMT in the future. The types of events in which a respondent witnessed OMT work vary, indicating that it does not necessarily matter how a participant experienced the efficacy of OMT. The opportunities to witness OMT work do not necessarily need to be standardized in medical school curricula or extracurricular activity.
Given that only 6.1 % of osteopathic physicians utilize OMT in their practice [5] and that this study indicates that up 96.1 % of physicians who utilize OMT witnessed it work, it stands to reason that by providing students with opportunities to witness the efficacy of OMT, we might, as a profession, almost completely reverse the current statistic. Even given the results of physicians who do not utilize OMT (7.4 % had an opportunity to witness the efficacy of OMT), the possibility for the osteopathic profession still reverses the current statistic from 6.1 to 93.6 % use.
The NNE calculation clearly exposes the population effect of this concept. For physicians, NNE=1.1, which is close to 1. This shows that a near 1:1 ratio exists for physicians seeing OMT work positively in real-life and then utilizing it in practice. For students interested in utilizing OMT, NNE=1.4, which is also close to 1. Again, this shows that a near 1:1 ratio exists for students seeing OMT work and utilizing it in their future practice. As DOs continue to define the future of the profession, we propose this as a way to further foster OMT as a distinguishing aspect of osteopathic medicine.
Given the results of this survey study, we propose an increase in exposure to OMT in the first 2 years of osteopathic medical school before the students go out to clinical rotations. Different COMs have different resources available; however, these authors propose that this is not necessarily a limitation to providing opportunities to see OMT work. These opportunities can take the form of student clinics, volunteer treatment sessions, and community outreach projects, among others, with the caveat that they need to see OMT work on real cases, whether on volunteers or on patients. This seems to be the common denominator in steering physicians into utilizing OMT in their practices.
Acknowledgments
Thank you to Dr. Chunfa Ji for his guidance in data analysis for this study.
-
Research ethics: The local Institutional Review Board deemed the study exempt from review.
-
Informed consent: Informed consent was obtained from all individuals included in this study, or their legal guardians or wards.
-
Author contributions: The authors have accepted responsibility for the entire contentof this manuscript and approved its submission.
-
Competing interests: None declared.
-
Research funding: None declared.
-
Data availability: The raw data can be obtained on request from the corresponding author.
References
1. Farra, F, Risio, R, Vismara, L, Bergna, A. Effectiveness of osteopathic interventions in chronic non-specific low back pain: a systematic review and meta-analysis. Complement Ther Med 2021:102616.10.1016/j.ctim.2020.102616Suche in Google Scholar PubMed
2. Hensel, K, Buchanan, S, Brown, S, Rodriguez, M, des, AC. Pregnancy research on osteopathic manipulation optimizing treatment effects: the PROMOTE study. Am J Obstet Gynecol 2015;1:108.e1–9. https://doi.org/10.1016/j.ajog.2014.07.043.Suche in Google Scholar PubMed PubMed Central
3. Lanaro, D, Ruffini, N, Manzotti, A, Lista, G. Osteopathic manipulative treatment showed reduction of length of stay and costs in preterm infants: a systematic review and meta-analysis. Medicine (Baltim) 2017;12:e6408. https://doi.org/10.1097/md.0000000000006408.Suche in Google Scholar
4. Li, R, Jose, A, Poon, J, Zou, C, Istafanos, M, Yao, S. Efficacy of osteopathic manipulative treatment in patients with Parkinson’s disease: a narrative review. J Osteopath Med 2021;121:891–8. https://doi.org/10.1515/jom-2021-0081.Suche in Google Scholar PubMed
5. Healy, C, Brockway, M, Wilde, B. Osteopathic manipulative treatment (OMT) use among osteopathic physicians in the United States. J Osteopath Med 2021;121:57–61. https://doi.org/10.1515/jom-2020-0013.Suche in Google Scholar PubMed
6. Snider, K, Couch, R, Bhatia, S. Osteopathic manipulative medicine practice patterns of third-year and fourth-year osteopathic medical students: an educational research project. J Am Osteopath Assoc 2020;120:293–302. https://doi.org/10.7556/jaoa.2020.048.Suche in Google Scholar PubMed
7. Commission on Osteopathic College Accreditation (COCA). Accreditation of Colleges of osteopathic medicine: COM continuing accreditation standards. American Osteopathic Association; 2022.Suche in Google Scholar
8. Figueroa, JS. The rapid structural screen revisited and the complete axial skeleton evaluation and treatment (CASET). Lecture to 1st Year DO students at Des Moines University; 2020. corrected on 10-6-2022.Suche in Google Scholar
9. Shapiro, L, Defoe, D, Jung, M, Li, S, Yao, S. Effects of clinical exposure to osteopathic manipulative medicine on confidence levels of medical students. J Am Osteopath Assoc 2017;117:e1–5. https://doi.org/10.7556/jaoa.2017.105.Suche in Google Scholar PubMed
10. Chyung, S, Roberts, K, Swanson, I, Hankinson, A. Evidence-based survey design: the use of a midpoint on the Likert scale. Perform Improv 2017;10:15–23. https://doi.org/10.1002/pfi.21727.Suche in Google Scholar
11. Citrome, L, Ketter, T. When does a difference make a difference? Interpretation of number needed to treat, number needed to harm, and likelihood to be helped or harmed. Int J Clin Pract 2013;5:407–11. https://doi.org/10.1111/ijcp.12142.Suche in Google Scholar PubMed
Supplementary Material
This article contains supplementary material (https://doi.org/10.1515/jom-2023-0288).
© 2024 the author(s), published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.
Artikel in diesem Heft
- Frontmatter
- Cardiopulmonary Medicine
- Review Article
- Comprehensive review of the heart failure management guidelines presented by the American College of Cardiology and the current supporting evidence
- Medical Education
- Original Article
- The predictive validity of MCAT scores and undergraduate GPA for COMLEX-USA licensure exam performance of students enrolled in osteopathic medical schools
- Musculoskeletal Medicine and Pain
- Review Article
- Foot and ankle fellowship-trained osteopathic orthopaedic surgeons: a review, analysis, and understanding of current trends
- Original Article
- Manual therapy plus sexual advice compared with manual therapy or exercise therapy alone for lumbar radiculopathy: a randomized controlled trial
- Neuromusculoskeletal Medicine (OMT)
- Original Article
- Why do physicians practice osteopathic manipulative treatment (OMT)? A survey study
- Obstetrics and Gynecology
- Original Article
- Uncovering gaps in management of vasomotor symptoms: findings from a national need assessment
- Letter to the Editor
- Educating our colleagues and hospital administrators regarding osteopathic medicine
Artikel in diesem Heft
- Frontmatter
- Cardiopulmonary Medicine
- Review Article
- Comprehensive review of the heart failure management guidelines presented by the American College of Cardiology and the current supporting evidence
- Medical Education
- Original Article
- The predictive validity of MCAT scores and undergraduate GPA for COMLEX-USA licensure exam performance of students enrolled in osteopathic medical schools
- Musculoskeletal Medicine and Pain
- Review Article
- Foot and ankle fellowship-trained osteopathic orthopaedic surgeons: a review, analysis, and understanding of current trends
- Original Article
- Manual therapy plus sexual advice compared with manual therapy or exercise therapy alone for lumbar radiculopathy: a randomized controlled trial
- Neuromusculoskeletal Medicine (OMT)
- Original Article
- Why do physicians practice osteopathic manipulative treatment (OMT)? A survey study
- Obstetrics and Gynecology
- Original Article
- Uncovering gaps in management of vasomotor symptoms: findings from a national need assessment
- Letter to the Editor
- Educating our colleagues and hospital administrators regarding osteopathic medicine

