Abstract
Context
This national needs assessment study explores the knowledge, attitude, beliefs, and practices (KABP) gaps related to vasomotor symptoms (VMS) associated with menopause among primary care and OB/GYN clinicians. VMS significantly impacts healthcare costs, workplace productivity, and patient psychosocial health, but a notable disconnect exists between healthcare providers and patients, with provider reticence and knowledge gaps playing a contributing role.
Objectives
This study aims to identify and propose optimal educational strategies to address these barriers, with attention to health disparities affecting women of color.
Methods
Methods employed include a multimodal approach of literature review, expert opinion, qualitative interviews, surveys, focus groups, and case studies, ensuring diverse clinician input. Data collection involved in-depth clinician interviews, a nationally disseminated clinician survey, and focus groups.
Results
Results indicate a critical deficiency in healthcare providers’ understanding and management of VMS, especially among OB/GYN residents, with 75 % showing limited knowledge. The study also highlights the disproportionate impact of knowledge gaps on women of color, emphasizing the need for a culturally informed approach in medical training and practice. There’s a notable discrepancy between clinicians’ current and desired abilities in managing VMS, indicating a need for ongoing professional development. Significant variability in approaches to diagnosing and treating VMS, as well as substantial knowledge gaps about treatment options, underscore the need for evidence-based protocols.
Conclusions
Although VMS are a normal aspect of aging, they can significantly disrupt quality of life for many women, necessitating intervention. Beyond the immediate discomfort, VMS can impact quality of life and trigger insomnia and mood disturbances. This study exposes both new and previously recognized gaps in healthcare providers’ knowledge and management skills concerning VMS treatment options, particularly regarding hormonal and nonhormonal therapies. Furthermore, our findings highlight the need for a deeper understanding of how VMS uniquely impacts women of diverse backgrounds. Research, including the Study of Women’s Health Across the Nation (SWAN), suggests that the experience and severity of VMS may be influenced by socioeconomic status, race/ethnicity, body mass index (BMI), and smoking status. However, the complex interplay of these factors and their relative contributions remain unclear. Further investigation is crucial to facilitate equitable access to effective treatment for all women. To bridge these gaps, improved education starting as early as residency is essential. This education should address common misconceptions about VMS and its management. Healthcare providers must enhance their competence in discussing the broad spectrum of VMS impacts and employ effective communication strategies to ensure that patients are well-informed about their symptoms and available treatment options.
Vasomotor symptoms (VMS) represent an important facet of the menopausal journey, significantly impacting healthcare, societal economic costs, and patient psychosocial health [1, 2]. The economic impact of untreated VMS are substantial, increasing healthcare costs by up to 121 % [1]. Concurrently, these symptoms lead to increased absenteeism and diminished productivity in the workplace [2]. From a psychosocial perspective, VMS can profoundly influence a patient’s psyche long after menopausal cessation [3, 4]. The pervasiveness of VMS during the menopausal transition and beyond underscores the significant impact that these symptoms have on women’s lives. Studies have shown that up to 8 out of 10 women experience VMS during menopause [5]. Moreover, these symptoms can persist well beyond the menopausal transition, with nearly half experiencing moderate to severe VMS even 2 years after their last menstrual period [6]. This highlights the substantial and often enduring burden of VMS on women’s health and well-being, emphasizing the need for effective management strategies.
Alarming data suggest a discordance in communication between healthcare providers and patients, predominantly stemming from healthcare providers’ reticence in addressing and managing VMS [7]. This hesitance, compounded by a demonstrable knowledge gap, is evident in surveys indicating 75 % of OB/GYN residents possess limited understanding of pivotal menopausal intricacies, including VMS [8, 9]. Particularly challenging clinical issues for physicians are the nonhormonal therapeutics and complementary and alternative therapies recommended or taken for VMS. While current guidelines recommend shared decision making when weighing the benefits, harms, and uncertainties of these options, physicians do not feel prepared to discuss these options in detail [10]. A new class of nonhormonal therapeutics is also available, with one recently approved by the Food and Drug Administration (FDA) [11]. These novel agents show promise in improving VMS and quality of life in women who experience it [12, 13]. However, without addressing knowledge gaps and potential communication challenges related to nonhormonal agents, the introduction of this new class may contribute to clinical uncertainty and potentially widen existing disparities in VMS management.
The gaps also disproportionately affect women of color, amplifying existing health disparities [5, 14]. The competence and knowledge gaps are perpetuated by the medical education continuum, in which resident physicians are not exposed to patients experiencing menopause symptoms in similar proportions as they will when they enter their own practices [8, 9, 15].
Thus, there is a responsibility and need to further understand these gaps to refine training paradigms and optimize communication, management, and therapeutic strategies.
Methods
This study was conducted to explore known gaps and uncover additional gaps related to VMS associated with menopause in primary care and OB/GYN clinicians. This national needs assessment aimed to uncover the structures underlying known gaps in knowledge, attitude, beliefs, and practices (KABP) related to VMS and to identify and propose optimal educational strategies to overcome these barriers. The protocol was approved as exempt by the Midwestern University Downers Grove Campus Institutional Review Board (IRB), IRB approval number 21054. The study was conducted between September 7, 2021 and September 6, 2023.
To achieve these objectives, a multimodal methodology encompassing a literature review, expert opinion, qualitative interviews, a survey (Appendix A), a focus group, and case studies were utilized (Figure 1). The qualitative and quantitative research methods provided a comprehensive assessment of gaps in clinical practice related to VMS and permitted the collection of perceived needs of the learners as well as actual needs, examination of problems in clinical practice, and identification of gaps in knowledge, skill, and attitudes that underlie these needs. A competency model informed the interview and survey questions, the interview responses further informed the survey, the survey informed the focus group, and the focus group interpreted the findings through a clinical lens. Participants in the focus groups and the survey each received modest compensation for their involvement. The methodology was designed to facilitate the identification of barriers to learning and change, which is critical for enhancing the effectiveness of educational interventions to realize clinical improvements.

A diagram of the macro components of the methodology is presented.
To ensure the validity and reliability of the data collected, a systematic process was employed to design, develop, and validate the needs assessment tools. This involved a comprehensive review of the current literature, validation by clinical experts, and validation testing with target audiences utilizing a grounded-theory approach. The needs assessment findings reflect the diversity of clinicians who treat and manage patients with VMS associated with menopause.
Data collection occurred in three steps, encompassing in-depth clinician interviews, a nationally disseminated clinician survey, and clinician focus groups. Investigators included a panel of clinical specialists in the treatment and management of patients with VMS associated with menopause, experts in continuing education and needs assessments, and experts in research methodology. This panel reviewed and validated assessment tools, reviewed summary data, interpreted clinical implications, and provided suggestions for further subanalysis.
Clinician interview and survey participants were recruited by the American College of Osteopathic Obstetricians and Gynecologists (ACOOG), the American College of Osteopathic Internists (ACOI), and the American College of Osteopathic Family Physicians (ACOFP). Antidote Education Company assisted with the recruitment of nurse practitioners (NPs) and physician assistants (PAs). Survey participants were also recruited through a contracted national panel provider. All clinicians were vetted and verified to ensure appropriateness for the study utilizing standardized criteria. The interview panel and survey participants were recruited via e-mail and focus group members were recruited from interview participants. Individuals completed an informed consent prior to participation. The interviews and focus groups were conducted via interactive web-based meetings. The survey was web-based utilizing a secure platform. Survey responses were anonymous, with minimal personal information collected, such as profession, specialty, and practice zip code. Interview and focus group responses were only recorded with profession and specialty identifiers to allow data analysis.
A competency model was developed to provide a framework for the needs assessment and related future education. This model consisted of clinical competency statements of behaviors essential to best practices related to VMS associated with menopause. These statements, derived from clinical guidelines and refined with expert and learner input, served as a framework for the development of the interview and survey questions. They were written in performance-oriented language utilizing action verbs, allowing competencies to be linked to gaps in performance, while recognizing that knowledge or attitude gaps may underlie performance gaps. Competencies included in the model are provided in Table 1.
Competencies utilized to develop the model.
| Competencies utilized to develop the model |
|---|
| Initiate a discussion on the severity of vasomotor symptoms with female patients of an appropriate age |
| Identify the impact of the vasomotor symptoms on the patient |
| Identify ethnic, cultural, and social factors affecting the patient |
| Conduct diagnostic tests when warranted (thyroid, glucose, hormones) |
| Refer the patient to a specialist when appropriate |
| Discuss treatment options with the patient, providing the benefits and risks of each option |
| Document the discussion with patients about the severity of vasomotor symptoms and therapeutic options |
| Utilize shared decision making to select the best option for the patient |
| Select the best route of administration and dose for the selected treatment |
| Monitor the patient for compliance, symptom reduction, and side effects |
| Effectively discontinue treatment at the appropriate time |
Qualitative data collected during interviews and focus groups were analyzed utilizing grounded theory and content thematic analysis. Quantitative data collected from surveys were analyzed utilizing appropriate methods for the specific question types. Descriptive statistics were analyzed for profession, specialty, years in practice, identified gender, and location (US state) of practice. Analysis of variance (ANOVA) was utilized to analyze differences in practice, knowledge, skill, and attitudes related to the competence model and the 74 survey items. A paired t-test was utilized to analyze competency categories. Survey responses were scored on a Likert scale, and the mean scores were compared between age groups, genders, profession, and location utilizing an independent sample T-test. Data were complete for all analyzed surveys. ChatGPT, an artificial intelligence–based large language platform, was utilized on a limited basis for some data analysis.
Results
Interviews to develop and refine the competencies and survey were conducted with 31 clinicians (14 OB/GYN physicians, 10 Family Medicine and Internal Medicine physicians, two resident physicians, three women’s health NPs, and two Family Medicine PAs.
The survey was sent to 4,377 clinicians and completed by 349 verified clinicians (133 OB/GYN physicians, 82 Family Medicine physicians, 79 Internal Medicine physicians, nine women’s health NPs and PAs, and 46 primary care NPs and PAs), indicating a 7.9 % response rate. The survey completers were from 45 states. Fifty-six percent of the respondents identified as male, 43 % as female, and 1 % as other. The average years of practice was 19.6 years, the median was 20 years, and the standard deviation was 6.2 years. The survey revealed that a significant portion of the respondents’ patient population falls within the menopausal age range (45–65 years). Specifically, 32.1 % of respondents reported that 41 % or more of their female patients were in this age group, while 50.1 % indicated that 21–40 % of their female patients belonged to this demographic. Only 17.8 % of respondents stated that 1–20 % of their female patients were within the menopausal age range.
Screening and diagnosis
Respondents rated their present ability vs. their desired ability related to care of patients with VMS in the following areas: (1) initiate a discussion on the severity of VMS with female patients of appropriate age (current 3.95, desired 4.45); (2) identify the impact of the VMS on the patient (current 3.99, desired 4.44); and (3) identify ethnic, cultural, and social factors affecting the patient (current 3.47, desired 4.24). Analysis yielded a statistically significant difference between the present and desired proficiencies (t=−5.77, p<0.02).
More than half (57.3 %) of the respondents indicated that they “bring up VMS with all patients of appropriate age or situation,” whereas 19.7 % indicated that they “prefer to allow [my] patient to bring up any VMS.” Almost a quarter (22.9 %) said that hot flashes are included on a checklist the patient completes and reviewed during the visit. When asked for agreement level from 1 (low) to 5 (high) with the statement “My patients feel [that] VMS are a normal part of the aging process and do not always report them as an issue”; the mean response was 3.64, with 71.7 % selecting option 4 or 5 (high agreement). Similar responses were selected when asked for agreement with the statement, “Patients are reluctant to take treatment advice because of fears of hormone therapy (HT),” with a mean response of 3.69 and 72.3 % selecting option 4 or 5 (high agreement).
During the interview phase of the project, clinicians reported being sensitive to individual needs and treating each patient individually but were unaware of ethnic, cultural, and social factors affecting patients. The competency on this topic revealed a moderately low present ability (3.47) and high perceived needs (4.24), with the gap between present and desired ability at 0.77.
Respondents were also asked their agreement level from 1 (low) to 5 (high) with the statements, “There are differences in the way patients are treated for VMS that play a role in disparities of care” (3.66), “I believe women are treated differently for VMS based on socio-economic factors” (3.39), and “I believe women are treated differently for VMS based on cultural factors” (3.44). For these three questions, the mean response was 3.5.
The clinicians indicated a high desire for competence related to the diagnosis and treatment of VMS associated with menopause. The present ability ratings varied, with clinicians reporting strength in the areas of conducting diagnostic tests and shared decision-making. The gaps between present and desired ability were at or above 0.5, reflecting a perceived need for all the competencies except diagnostic testing and patient referrals, revealing an interest by the clinicians to improve practices in these competencies, as represented in Figure 2.

Competency ratings, present vs. desired.
Answers to the question A 47-year-old patient presents complaining of vasomotor symptoms and irregular periods. She has a history of hypothyroidism and a family history of diabetes. Which of the following would aid with the immediate assessment of this patient? (check all that apply), show variability in current practices related to diagnostic testing. The vast majority (90.8 %) prioritized the thyroid stimulating hormone (TSH) level or the HbA1c test (67.9 %) for immediate patient assessment. Fewer clinicians opted for the follicle-stimulating hormone (FSH) level (56.2 %), metabolic panel (47.6 %), and glucose tolerance test (19.5 %), while a mere 3.4 % believed that no labs were necessary. It is important to note that while FSH testing can confirm menopausal status, it should not be the sole determinant in guiding management decisions for VMS. A comprehensive assessment, including a detailed symptom evaluation, patient history, and consideration of other relevant diagnostic tests, should inform the overall management strategy [16].
Treatment
When asked about treatment-related competencies, most respondents shared a desire for improvement. The mean self-assessed current ability to “Refer the patient when appropriate” was 3.87, with a desired capability of 4.14. Clinicians rated themselves at an average of 3.87 for “Discuss treatment options with the patient, providing benefits and risk of each treatment,” while aspiring for a level of 4.55. The ability to “Document the discussion with patients about the severity of VMS and therapeutic options” had a mean score of 3.91, with the desired level being 4.49. The survey indicated a current mean score of 4 for “Use shared decision making to select the best option for the patient” and a desired level of 4.51. Lastly, for “Select the best route of administration and dose for the selected treatment,” clinicians rated themselves at an average of 3.8, aiming for 4.52. The overall mean desire for improvement was 0.55. All competencies showed statistically significant differences between the current and desired levels, with all p<0.001.
Therapy selection also showed areas of variation in practice. Although these patient descriptions are vague and therapy should be matched to the patient, several of the scenarios had better options to choose. One question stated, “A healthy 50-year-old patient with no comorbidities presents complaining of hot flashes, night sweats, and moodiness. When questioned, she reports vaginal dryness, dyspareunia, and restless sleep related to the night sweats. Along with a suggestion to use lubricants, which of the following options would you consider optimal for this patient?” Responses were:
An over-the-counter (OTC) medication: 6.9 %
Selective serotonin reuptake inhibitor (SSRI)/serotonin-norepinephrine reuptake inhibitor (SNRI) alone: 7.7 %
SSRI/SNRI along with estrogen cream: 27.5 %
Hormone therapy (oral/patch/pellets) 44.7 %
Estrogen vaginal ring: 11.8 %
No treatment: 0.6 %
Other: 0.8 %
There are significant gaps in knowledge about therapies, with two of the three questions being evenly split between true and false.
Estrogen patches are safer than oral formulations for patients who utilize tobacco (50.1 % T/49.9 % F)
A vaginal suppository will relieve VMS as well as decrease vaginal symptoms of menopause (55.9 % T/44.1 % F)
Beta blockers will relieve VMS as well as decrease vaginal symptoms of menopause (20.6 % T/79.4 % F)
When asked about risk factors, there was variation in response to who should be treated with HT. Most clinicians would not treat a patient with hormone-dependent breast cancer, but there was inconsistency with other patient risk factors.
Has hormone-dependent breast cancer (90.3 %)
Has hormone receptor negative breast cancer (44.4 %)
Utilizes tobacco (52.4 %)
Has a family history of stroke (38.1 %)
Has history of myocardial infarction (MI) (58.2 %)
More family physicians (40.7 %) than internists (37.1 %) and OBGYNs (26.8 %) feel that HT risks outweigh its benefits.
Ethnic, cultural, and socioeconomic considerations
During the interview phase of the project, clinicians reported being sensitive to individual needs and treating each patient individually but were unaware of ethnic, cultural, and social factors affecting patients. The competency on this topic presented during the survey revealed a low present ability (mean, 3.47) and high perceived needs (gap between present and desired ability) (mean, 4.24). Additional questions on the survey show only slight agreement with disparities playing a role in how patients are treated:
There are differences in the way patients are treated for VMS that play a role in disparities of care (mean, 3.66/5)
I believe women are treated differently for VMS based on socioeconomic factors (mean, 3.39/5)
I believe women are treated differently for VMS based on cultural factors (mean, 3.44/5)
Confidence and preparation from training
During the interview phase of the project, clinicians reported a lack of experience in treating patients with VMS related to menopause during residency. This was explored in the survey and yielded results to confirm this finding. Clinicians earlier in their careers reported lower confidence in their practices and lower scores for their preparation during residency. The specific questions were, “How confident are you in your ability related to the treatment of vasomotor symptoms associated with menopause?” and “How well did your training prepare you to treat patients with vasomotor symptoms (VMS) related to menopause?” The rating choice was a slider scale from 1 to 100 for both questions. Figure 3 provides more details.
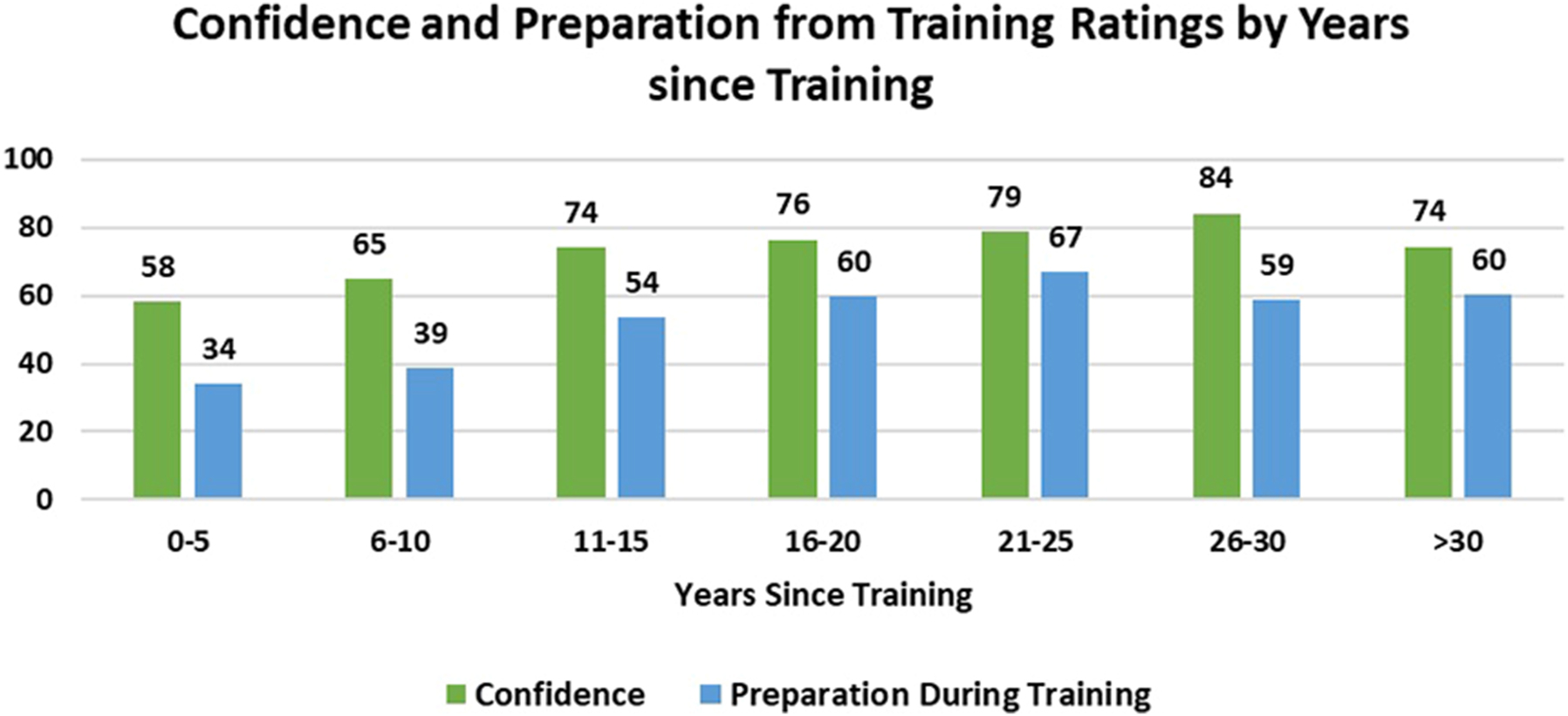
Confidence and preparation from training ratings by years since training.
Discussion
The findings of this comprehensive assessment on VMS associated with menopause offer insights into current clinical practices and pinpoint critical areas for improvement in healthcare delivery and medical education.
Communication gaps and education needs in healthcare providers
Our study highlights a critical deficiency in healthcare providers’ understanding and management of VMS, particularly among OB/GYN residents. This knowledge gap extends beyond hormonal treatments to include nonhormonal therapeutics and alternative therapies. Notably, survey responses indicated that 75 % of OB/GYN residents possess limited knowledge of menopausal intricacies, including VMS management. The introduction of new nonhormonal treatments approved by the FDA adds complexity. Addressing this issue demands an immediate and comprehensive revision of medical education curricula to integrate these evolving treatment paradigms into training programs, ensuring that healthcare providers are adequately equipped to navigate the multifaceted landscape of menopause treatment, including informed decision-making in conjunction with their patients.
Impact of health disparities
The study distinctly emphasizes the disproportionate impact of knowledge gaps on women of color, with an implication for healthcare inequity in managing menopause-related symptoms. This is demonstrated by the survey finding that clinicians rated their current ability to identify ethnic, cultural, and social factors affecting patients at a moderately low average with a high perceived need for improvement. Additionally, many comments received during the interviews were similar to “I treat all of my patients the same way.” While that may be true, the SWAN study and other research highlight that women of color don’t respond the same way, leading to unmanaged or poorly managed symptoms [5, 14]. Addressing these disparities mandates a holistic, culturally informed approach in medical training and practice, ensuring that clinicians are well versed in the diverse backgrounds of their patients. Differentiated approaches to discussion and treatment are necessary to effectively reduce health disparities.
Need for competency-based training
The findings strongly advocate for competency-based medical education and continuing education. The competencies identified, such as initiating dialogues on VMS severity and considering diverse patient backgrounds, are crucial for patient-centric care. Embedding these competencies into medical education can significantly elevate the standards of patient care and engagement.
Discrepancy between current and desired abilities
The disparity between clinicians’ current and desired capabilities in managing VMS, as revealed by the study, indicates an overarching need for enhanced training and education in this field.
Variations in treatment approaches and knowledge gaps
Our study reveals significant variability in clinicians’ approaches to diagnosing and treating VMS, as well as substantial knowledge gaps about treatment options. For instance, the survey responses on treatment choices for a hypothetical patient scenario showed a wide range of preferences, indicating inconsistencies and potential uncertainties in clinical practice. This variability underscores the need for standardized, evidence-based treatment protocols in this area to ensure consistent and effective patient care.
Importance of addressing misconceptions and patient education
The misconceptions among patients viewing VMS as a routine aspect of aging, coupled with apprehensions regarding HT, highlight the urgent need for enhanced patient education. Clinicians must be equipped not only to dispel these misconceptions but also to provide evidence-based information to assist patients in making informed decisions regarding their treatment.
Recommendations for future research and practice
Considering these findings, there is a clear imperative for additional research to identify the most effective strategies for updating graduate medical training and continuing education in VMS management. Healthcare systems should also consider the implementation of targeted educational initiatives for healthcare providers, aimed at equipping them with the latest insights and best practices in this evolving field.
Limitations and recommendations for future research
The authors acknowledge the following study limitations and make recommendations for future research.
Response rate and sample representation
Limitation: The low response rate of 7.9 % could suggest that the sample was not representative of all clinicians in the United States, potentially introducing bias and limiting the generalizability of the findings.
Recommendation: Future research should aim to enhance participant diversity and number by incorporating clinicians from a broader range of practice settings and geographic locations. Strategies to improve response rates should also be considered to ensure a more representative sample.
Self-reported measures
Limitation: The reliance on self-reported data for assessing proficiency and confidence may lead to biases related to social desirability or inaccurate self-assessment.
Recommendation: Subsequent studies should incorporate methods that mitigate these biases, possibly through the use of validated objective measures or corroboration of self-reported data with performance assessments.
Limited demographic information
Limitation: The collection of minimal personal information restricts the analysis of demographic influences on study outcomes, particularly with respect to geographic, institutional, and socioeconomic factors.
Recommendation: It is advisable for future studies to gather comprehensive demographic data to enrich the dataset and enable a deeper understanding of these variables on clinical practice and attitudes.
Cultural and socioeconomic factors
Limitation: The current study’s exploration of cultural and socioeconomic disparities is hindered by the broad nature of the survey questions and potentially limited cultural competence training among respondents.
Recommendation: Future research should involve more detailed inquiries into how cultural and socioeconomic contexts influence clinical decisions. This might include enhanced training for researchers in cultural competence to better interpret nuanced responses.
Nonresponse bias
Limitation: The absence of data on nonrespondents introduces the potential for nonresponse bias, particularly if the characteristics of nonrespondents differ significantly from those of respondents.
Recommendation: Investigating the reasons for nonresponse and comparing the known characteristics of respondents and nonrespondents can help in understanding and adjusting for any resulting biases.
Use of new therapies
Limitation: Although emerging nonhormonal therapies are discussed, there is a lack of in-depth exploration into clinicians’ readiness to integrate these new treatments into practice.
Recommendation: Future studies should focus on assessing the adoption and impact of novel therapeutic options, investigating barriers to their use, and clinicians’ educational needs to ensure effective implementation.
Conclusions
Although VMS are a normal aspect of aging, they can significantly disrupt quality of life for many women, necessitating intervention. Beyond the immediate discomfort, VMS can trigger insomnia and mood disturbances. This study exposes both new and previously recognized gaps in healthcare providers’ knowledge and management skills concerning VMS treatment options, particularly regarding hormonal and nonhormonal therapies.
Furthermore, our findings highlight the need for a deeper understanding of how VMS uniquely impacts women of diverse backgrounds. Research, including the Study of Women’s Health Across the Nation (SWAN), suggests that the experience and severity of VMS may be influenced by socioeconomic status, race/ethnicity, body mass index (BMI), and smoking status [5]. However, the complex interplay of these factors and their relative contributions remain unclear. Further investigation is crucial to facilitate equitable access to effective treatment for all women.
To bridge these gaps, improved education starting as early as residency is essential. This education should address common misconceptions about VMS and its management. Healthcare providers must enhance their competence in discussing the broad spectrum of VMS impacts and employ effective communication strategies to ensure that patients are well informed about their symptoms and available treatment options.
Acknowledgments
Michael Geria, DO, for his leadership of ACOOG which helped make this project possible. Cecilia Banga, DO, for her ACOOG CME Committee leadership, which approved this project.
-
Research ethics: This study was reviewed and approved as exempt by the Midwestern University Downer’s Grove Campus IRB (Application #21054). This was not a clinical trial and entrance into the clinical trial registry was not required. It was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
-
Informed consent: Informed consent was obtained from all individuals included in this study.
-
Author contributions: All authors provided substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; all authors drafted the article or revised it critically for important intellectual content; all authors gave final approval of the version of the article to be published; and all authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
-
Competing interests: No relevant conflicts of interest: Crim, Koh, Larrison, McKeithen, Fleming, Caruso, Prud’homme. Hubka: Speaker’s Bureau for Astellas.
-
Research funding: This study was funded by an independent educational grant from Astellas Pharma US, Inc. Support was used for protected time, data systems, participant compensation, and project management. The supporting company played no role in the design, implementation, or analysis, and was not involved in the decision to publish data.
-
Data availability: The raw data can be obtained on request from the corresponding author.
References
1. Sarrel, PM, Njike, VY, Katz, DL, Lafeuille, MH, Grittner, AM, Fortier, J, et al.. Incremental direct and indirect costs of untreated vasomotor symptoms. Menopause 2015;22:260–6. https://doi.org/10.1097/gme.0000000000000320.Search in Google Scholar
2. Whiteley, J, Nanavati, M, Elraiyah, T, Alvir, J, Shah, S. The impact of menopausal symptoms on quality of life, productivity, and economic outcomes. J Womens Health 2013;22:983–90. https://doi.org/10.1089/jwh.2012.3719.Search in Google Scholar PubMed PubMed Central
3. Potter, B, Hillard, PJ, Santoro, N, Torell, E, Hampton, A. Menopause. Prim Care 2018;45:625–41. https://doi.org/10.1016/j.pop.2018.08.001.Search in Google Scholar PubMed
4. Ratka, A, McCrohon, JA, Valentiner, EJ, Raut, A, Cipher, D, Meczekalski, B, et al.. Menopausal Vasomotor Symptoms (MVS) survey for assessment of hot flashes. J Womens Health 2006;15:77–89. https://doi.org/10.1089/jwh.2006.15.77.Search in Google Scholar PubMed
5. Thurston, RC, Joffe, H. Vasomotor symptoms and menopause: findings from the study of women’s health across the nation. Obstet Gynecol Clin N Am 2011;38:489–501. https://doi.org/10.1016/j.ogc.2011.05.006.Search in Google Scholar PubMed PubMed Central
6. Freeman, EW, Sammel, MD, Sanders, RJ. Risk of long-term hot flashes after natural menopause: evidence from the Penn Ovarian Aging Study cohort. Menopause 2014;21:924–32. https://doi.org/10.1097/gme.0000000000000196.Search in Google Scholar PubMed PubMed Central
7. ACOOG. Data on file. Fort Worth, TX: Am Col Ost OBGYN; 2019.Search in Google Scholar
8. Christianson, MS, King, KA, Youngkin, EQ, Khafagy, AM, Shen, W. Menopause education: needs assessment of American obstetrics and gynecology residents. Menopause 2013;20:1120–5. https://doi.org/10.1097/gme.0b013e31828ced7f.Search in Google Scholar
9. Kling, JM, Manson, JE, Kaunitz, AM, Crandall, CJ, Skinner, LJ, Stuenkel, CA, et al.. Menopause management knowledge in postgraduate family medicine, internal medicine, and obstetrics and gynecology residents: a cross-sectional survey. Mayo Clin Proc 2019;94:242–53. https://doi.org/10.1016/j.mayocp.2018.08.033.Search in Google Scholar PubMed
10. Yeganeh, L, Adhami, K, Sobhani, S, Vincent, A. Knowledge and attitudes of health professionals regarding menopausal hormone therapies. Climacteric 2017;20:348–55. https://doi.org/10.1080/13697137.2017.1304906.Search in Google Scholar PubMed
11. Lee, A. Fezolinetant: first approval. Drugs 2023;83:1137–41. https://doi.org/10.1007/s40265-023-01917-1.Search in Google Scholar PubMed
12. Fraser, GL, Kingsberg, SA, Langley, SC, Kroll, R, Santoro, N, Lee, M, et al.. A phase 2b, randomized, placebo-controlled, double-blind, dose-ranging study of the neurokinin 3 receptor antagonist fezolinetant for vasomotor symptoms associated with menopause. Menopause 2020;27:382–92. https://doi.org/10.1097/gme.0000000000001510.Search in Google Scholar
13. Lederman, S, Ottery, FD, Cano, A, Santoro, N, Shapiro, M, Stute, P, et al.. Fezolinetant for treatment of moderate-to-severe vasomotor symptoms associated with menopause (SKYLIGHT 1): a phase 3 randomised controlled study. Lancet 2023;401:1091–102. https://doi.org/10.1016/s0140-6736(23)00085-5.Search in Google Scholar
14. Copeland, VC. Health disparities and women of color: closing the gap. Introduction. Soc Work Publ Health 2011;26:1–2. https://doi.org/10.1080/10911350902911359.Search in Google Scholar PubMed
15. Manson, JE, Kaunitz, AM. Menopause management - getting clinical care back on track. N Engl J Med 2016;374:803–6. https://doi.org/10.1056/nejmp1514242.Search in Google Scholar
16. Randolph, JFJ, Sowers, M, Bondarenko, I, Gold, EB, Greendale, GA, Bromberger, JT, et al.. The relationship of longitudinal change in reproductive hormones and vasomotor symptoms during the menopausal transition. J Clin Endocrinol Metab 2005;90:6106–12. https://doi.org/10.1210/jc.2005-1374.Search in Google Scholar PubMed
Supplementary Material
This article contains supplementary material (https://doi.org/10.1515/jom-2024-0011).
© 2024 the author(s), published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Frontmatter
- Cardiopulmonary Medicine
- Review Article
- Comprehensive review of the heart failure management guidelines presented by the American College of Cardiology and the current supporting evidence
- Medical Education
- Original Article
- The predictive validity of MCAT scores and undergraduate GPA for COMLEX-USA licensure exam performance of students enrolled in osteopathic medical schools
- Musculoskeletal Medicine and Pain
- Review Article
- Foot and ankle fellowship-trained osteopathic orthopaedic surgeons: a review, analysis, and understanding of current trends
- Original Article
- Manual therapy plus sexual advice compared with manual therapy or exercise therapy alone for lumbar radiculopathy: a randomized controlled trial
- Neuromusculoskeletal Medicine (OMT)
- Original Article
- Why do physicians practice osteopathic manipulative treatment (OMT)? A survey study
- Obstetrics and Gynecology
- Original Article
- Uncovering gaps in management of vasomotor symptoms: findings from a national need assessment
- Letter to the Editor
- Educating our colleagues and hospital administrators regarding osteopathic medicine
Articles in the same Issue
- Frontmatter
- Cardiopulmonary Medicine
- Review Article
- Comprehensive review of the heart failure management guidelines presented by the American College of Cardiology and the current supporting evidence
- Medical Education
- Original Article
- The predictive validity of MCAT scores and undergraduate GPA for COMLEX-USA licensure exam performance of students enrolled in osteopathic medical schools
- Musculoskeletal Medicine and Pain
- Review Article
- Foot and ankle fellowship-trained osteopathic orthopaedic surgeons: a review, analysis, and understanding of current trends
- Original Article
- Manual therapy plus sexual advice compared with manual therapy or exercise therapy alone for lumbar radiculopathy: a randomized controlled trial
- Neuromusculoskeletal Medicine (OMT)
- Original Article
- Why do physicians practice osteopathic manipulative treatment (OMT)? A survey study
- Obstetrics and Gynecology
- Original Article
- Uncovering gaps in management of vasomotor symptoms: findings from a national need assessment
- Letter to the Editor
- Educating our colleagues and hospital administrators regarding osteopathic medicine

