A 47-year-old white female presented to an outpatient dermatology practice in January 2019 with a chief complaint of a change within a congenital lesion. Four weeks prior, she noted a change in one of the lesion’s spots. The patient has a history of basal cell carcinoma diagnosed and treated 3 years prior, but she had no personal or family history of melanoma.
A cutaneous examination revealed a hyperpigmented patch, measuring 9.5 cm × 5.3 cm, containing darker papules/macules on her left lateral arm. Within the medial aspect of the lesion was an irregularly pigmented, asymmetric papule measuring 6 mm2 (Figure 1). A scoop-shave biopsy with 2 mm margins was performed.
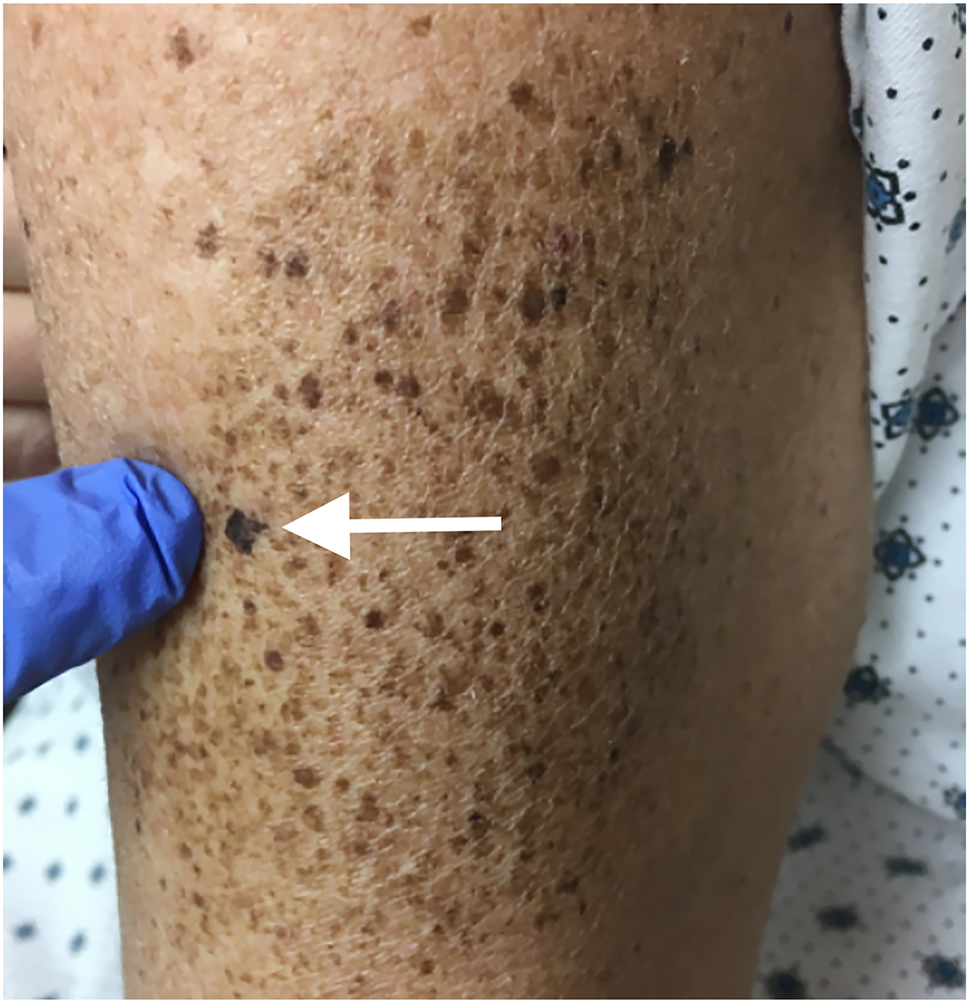
A superficial spreading melanoma within a nevus spilus presented on the left lateral arm. The white arrow points to the suspicious lesion within the nevus spilus, which was proven through biopsy to be a superficial spreading melanoma.
A histopathological examination of the specimen revealed a superficial spreading melanoma, 0.15 mm Breslow thickness, staged at T1a. The patient was referred to a surgical oncologist, who excised the melanoma with 1 cm margins.
Although the patient was characterized as having Fitzpatrick Skin Type III, her skin has a propensity to freckle and produce lentigines, which is a risk factor of melanoma [1]. Additionally, this patient’s risk for developing a melanoma was increased by a modifiable risk factor of excess ultraviolet (UV) exposure indicated by her past skin disease history of a non-melanoma skin cancer (basal cell carcinoma [BCC]). Despite melanoma being overall more common in males, melanoma is more common in females before the age of 50; this patient fell into this category because her diagnosis was made at age 47.
Other factors that increase the risk for developing melanoma that were not applicable to this patient include light eyes (i.e., green or blue), light hair (i.e., red or blond), personal history of melanoma or family history of a first-degree relative with melanoma, male sex, increasing age (>65 years old), precursor lesions (i.e., dysplastic nevi), inherited skin diseases (i.e., dysplastic nevus syndrome, familial atypical mole and melanoma syndrome [FAMMM], xeroderma pigmentosum), and immunosuppression from medications or immune conditions [1].
A nevus spilus, or speckled lentiginous nevus, is a hyperpigmented irregularly shaped lesion with overlying macules and/or papules of smaller size and darker color [2]. They are relatively common, presenting in 0.2–2.3% of the population, and often present on the trunk and upper extremities [3, 4]. Although approximately 80% of nevus spilus present at birth, the most prominent overlying papules and/or macules do not present until later in life [2].
The malignant potential of a nevus spilus is rare with a 0.13–0.2% occurrence [4]. Although not considered a malignant precursor, recommended surveillance of a nevus spilus involves a baseline assessment with clinical follow-up and digital dermatoscopy [5, 6]. All patients with a nevus spilus should be educated about the appearance of a melanoma and instructions for skin self-examination.
The early detection of melanoma is critical to decrease its mortality. The “ABCDEs” of melanoma help a physician or a patient identify the clinical features of melanoma [7]. “A” stands for Asymmetry because melanoma is often not symmetrical. “B” stands for Border because the border of a melanoma is often irregular or ill-defined. “C” stands for Color because melanoma often has more than one color. “D” is for Diameter b a melanoma often presents greater than 6 mm (i.e., the size of a pencil eraser). Lastly, “E” stands for Evolution, which is the most important factor of all the “ABCDEs” and signifies a change in the size, shape, or color of a preexisting lesion. It is important to note that not all melanomas will fall into all of these parameters, but they can help guide physicians and patients when a concerning lesion is present.
-
Research funding: None reported.
-
Author contributions: All authors provided substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; all authors drafted the article or revised it critically for important intellectual content; all authors gave final approval of the version of the article to be published; and all authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
-
Competing interests: None reported.
-
Informed consent: The patient described in this report provided written informed consent.
References
1. The American Cancer Society Medical and Editorial Content Team. Risk factors for melanoma skin cancer. American Cancer Society; 2019. Available from: https://www.cancer.org/cancer/melanoma-skin-cancer/causes-risks-prevention/risk-factors.html [Accessed 11 Oct 2022].Suche in Google Scholar
2. Lazavo, R. Speckled lentiginous nevus. Practice essentials, pathophysiology, epidemiology; 2022. Available from: https://emedicine.medscape.com/article/1061990-overview [Accessed 1 Jul 2022].Suche in Google Scholar
3. Corradin, MT, Giulioni, E, Fiorentino, R, Santeufemia, DA, Re, GL, Vettorello, A. In situ malignant melanoma on nevus spilus in an elderly patient. Acta Dermatovenerol 2014;23:17–9. https://doi.org/10.2478/v10162-012-0048-6.Suche in Google Scholar
4. Brito, MH, Dionísio, CS, Fernandes, CM, Ferreira, JC, Rosa, MJ, Garcia, MM. Synchronous melanomas arising within nevus spilus. An Bras Dermatol 2017;92:107–9. https://doi.org/10.1590/abd1806-4841.20175230.Suche in Google Scholar PubMed PubMed Central
5. Stewart, CL, Tetzlaff, MT, Ming, ME. Nevus spilus (speckled lentiginous nevus, naevus sur naevus). Dermatology Advisor; 2019. Available from: https://www.dermatologyadvisor.com/home/decision-support-in-medicine/dermatology/nevus-spilus-speckled-lentiginous-nevus-naevus-sur-naevus/[Accessed 1 Jul 2022].Suche in Google Scholar
6. Haenssle, HA, Kaune, K, Buhl, T, Thoms, K, Padeken, M, Emmert, S, et al.. Melanoma arising in segmental nevus spilus: detection by sequential digital dermatoscopy. J Am Acad Dermatol 2009;61:337–41. https://doi.org/10.1016/j.jaad.2008.12.035.Suche in Google Scholar PubMed
7. The American Cancer Society Medical and Editorial Content Team. Signs and Symptoms of Melanoma Skin Cancer. American Cancer Society; 2019. Available from: https://www.cancer.org/cancer/melanoma-skin-cancer/detection-diagnosis-staging/signs-and-symptoms.html [Accessed 11 Oct 2022].Suche in Google Scholar
© 2023 the author(s), published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.
Artikel in diesem Heft
- Frontmatter
- General
- Review Article
- Glucocorticoid use in rheumatoid arthritis patients and the onset of pneumonia: a systematic review and meta-analysis
- Medical Education
- Original Article
- Barriers to research opportunities among osteopathic medical students
- Musculoskeletal Medicine and Pain
- Case Report
- Structural abnormalities and osteopathic considerations in primary immunodeficiencies
- Neuromusculoskeletal Medicine (OMT)
- Original Article
- Does the osteopathic pedal pump reduce lower limb volume in healthy subjects?
- Neuromusculoskeletal Medicine (OMT)
- Clinical Practice
- Enabling health potential: exploring nonlinear and complex results of osteopathic manual medicine through complex systems theory
- Pediatrics
- Review Article
- Person-centered language and pediatric ADHD research: a cross-sectional examination of stigmatizing language within medical literature
- Clinical Image
- Superficial spreading melanoma within a nevus spilus
Artikel in diesem Heft
- Frontmatter
- General
- Review Article
- Glucocorticoid use in rheumatoid arthritis patients and the onset of pneumonia: a systematic review and meta-analysis
- Medical Education
- Original Article
- Barriers to research opportunities among osteopathic medical students
- Musculoskeletal Medicine and Pain
- Case Report
- Structural abnormalities and osteopathic considerations in primary immunodeficiencies
- Neuromusculoskeletal Medicine (OMT)
- Original Article
- Does the osteopathic pedal pump reduce lower limb volume in healthy subjects?
- Neuromusculoskeletal Medicine (OMT)
- Clinical Practice
- Enabling health potential: exploring nonlinear and complex results of osteopathic manual medicine through complex systems theory
- Pediatrics
- Review Article
- Person-centered language and pediatric ADHD research: a cross-sectional examination of stigmatizing language within medical literature
- Clinical Image
- Superficial spreading melanoma within a nevus spilus

