Abstract
Objectives
This study aimed to compare the effectiveness of the “PICO”, which stands for Patient, Intervention, Comparison, and Outcome, teaching model with traditional didactic teaching in clinical research education.
Methods
90 eight-year clinical medicine students participated in the study, with 45 students randomly assigned to the PICO group and 45 students to the Didactic group. The PICO group received instruction using the “PICO” teaching model, while the Didactic group received instruction using traditional teaching methods. Final grades, course satisfaction, and clinical research competencies were assessed through questionnaires.
Results
The PICO group achieved higher final grades compared to the Didactic group. Within the PICO group, there was a positive correlation between theoretical knowledge scores and group study and mock defense scores. Students in the PICO group reported greater satisfaction with the course design, particularly in meeting their learning needs and improving clinical research thinking and skills. The PICO group also had higher self-assessment scores in knowledge integration, practical application, and research literacy.
Conclusions
The findings highlight the advantages of using the “PICO” teaching model in clinical research education. It leads to improved theoretical knowledge, higher satisfaction levels, and enhanced clinical research competence among medical undergraduates.
Introduction
The primary objective of clinical research is to answer questions that originate in clinical practice [1, 2]. Clinical research methodology is a crucial safeguard for the conduction of high-quality clinical research [3, 4]. Eight-year clinical medicine students represent the future generation of clinicians, who will not only provide patient care but also contribute to scientific endeavors. To equip these students with the necessary skills, the course “Methods, Design and Practice of Clinical Research” has been specifically designed to provide systematic training in the methods and practice of clinical scientific research. This course consists of 48 credit hours and 3 credits. The contents of this course include introduction to clinical research, determination of the direction of clinical research and selection of topics, design of clinical research protocols, implementation and process management of clinical research, clinical research ethics and academic morality, core concepts and basic methods of statistical analysis. The course objectives are presented in Table 1.
Course objectives.
| Knowledge |
|---|
| –Demonstrate essential elements and basic theory of clinical research |
| –Strengthen the foundation of clinical research design framework |
| –Summarize the rationale for clinical research case |
| Ability |
| –Perform sample size calculations and develop statistical analysis |
| strategies based on different research designs |
| –Apply critical thinking and a holistic view to evaluate clinical research |
| –Design a clinical research, write a project application and defend a |
| mock application |
| Emotion and value |
| –Emphasize research integrity, academic standards and teamwork |
| –Focus on the psychology of research subjects and communicate |
| effectively with them |
| –Recognize the ethical issues involved in clinical research and to be |
| patient-centered |
When undertaking this course, students exhibit diverse perceptions and priorities regarding clinical research due to variations in research interests and future career plans. Additionally, students possess varying practical needs for the course and differ in their levels of prior understanding and ability to apply clinical research principles. However, the limited number of hours in the curriculum often poses challenges in meeting the individual needs of all students. Moreover, the course covers a broad range of theoretical content and multiple chapters while encompassing the entire process of clinical research. Elements related to clinical research, laws and regulations, as well as statistical methods, tend to be abstract and complex, making them challenging for students to grasp. Furthermore, traditional classroom lectures often adopt a teacher-driven approach, with students assuming passive roles. This may result in a lack of motivation and engagement, preventing students from fully unleashing their creativity and critical thinking abilities. The absence of interaction and collaboration within the classroom further hampers learning effectiveness and capacity development.
Additionally, clinical research necessitates the involvement of multidisciplinary personnel in the organization and implementation of studies. This calls for the integration and cross-fertilization of knowledge from various fields, such as clinical medicine, epidemiology, statistics, ethics, and even psychology, law, science, and technology. However, the current learning process fails to sufficiently promote students’ ability to integrate and flexibly utilize multidisciplinary knowledge. As designers and implementers of clinical research, students struggle to develop a systematic conceptualization of clinical research that could provide them with practical and fully integrated theoretical guidance. Moreover, the emphasis on theoretical knowledge acquisition without sufficient practical experience leaves students confined to a superficial understanding. Consequently, when faced with real-world clinical research problems, students often find themselves at a loss.
Furthermore, the evaluation of learning outcomes solely focuses on students’ mastery of theoretical knowledge, neglecting the cultivation and assessment of other crucial competencies and literacies, such as practical application, problem-solving, innovation, teamwork, critical thinking, medical humanistic literacy, and medical professional literacy. This one-sided assessment approach tends to perpetuate an exam-oriented education system, where students resort to short-term memorization and mechanical learning strategies to cope with examinations, lacking in-depth comprehension and long-term learning motivation.
One of the fundamental guiding principles in clinical study design is the “PICO” framework, which stands for Patient, Intervention, Comparison, and Outcome [5, 6]. To address the mentioned teaching challenges, our study focuses on the implementation of the “PICO” teaching model within the course “Methods, Design and Practice of Clinical Research” for eight-year clinical medicine students. The “PICO” teaching model emphasizes personalized learning, interactive teaching, clinical practice integration, and outcome-based assessment. In this study, we applied the “PICO” teaching model to assess its effectiveness among eight-year clinical medicine students enrolled in the course “Methods, Design and Practice of Clinical Research”.
Materials and methods
Participants and settings
The participants of this study were eight-year clinical medicine students who took the course “Methods, Design and Practice of Clinical Research” during the second semester of their senior year at Shanghai Jiao Tong University School of Medicine from 2020 to 2021. All participants provided informed consent for this study. A total of 90 students were enrolled in the study and randomly assigned to two groups: the “PICO” teaching model group (PICO group) consisting of 45 students, and the Didactic teaching model group (Didactic group) consisting of the other 45 students.
During the course, the “PICO” teaching model was implemented for the PICO group, while the Didactic group received traditional didactic teaching as control. Both groups received an equal number of course hours, were taught the same clinical research knowledge by faculty with equivalent qualifications, and were regularly supervised by a team of teaching supervisors.
Course design and learning assessment for the PICO group
Course design of the “PICO” model
P – personalized learning
Students are provided with customized and personalized learning plans that included required and elective content. The required content covered fundamental principles of clinical research and the essentials of design and practice, while the elective content allowed students to focus on their research interests and career goals. This approach enhanced their research design, practice, and evaluation skills and catered to their personalized needs of clinical research learning. Online elective content was available, consisting of five series: biostatistics, research quality management, medical ethics, research translation and patent, and biobanking.
I – interactive teaching
Basic theoretical knowledge related to clinical research was made available as an online resource for self-study. In the offline course, real clinical research cases were analyzed, and key knowledge points were reviewed. The teaching process emphasized the application of theoretical knowledge and the practical aspects of research. Through online guidance before class, offline guidance during class, and online follow-up after class, students engaged in self-learning before class, discussion-based learning, and practical exercises, extending their learning time and space. Various interactive teaching methods were employed, such as simulations of clinical research situations, role-playing, flipped classroom activities, introduction of classic cases, and group discussions. These approaches aimed to provide students with real experiences, enhance their empathy and doctor-patient communication skills, develop their knowledge framework, foster clinical research thinking, and improve teamwork, problem-solving, and reflective abilities.
C – clinical practice integration
The teaching included lectures and simulated research practice. During lectures, students were engaged in think-pair-share (TPS) activities, group discussions, and in-depth analysis of clinical research cases. The students were required to evaluate clinical research cases using critical thinking and learned about statistical methods and ethical principles relevant to clinical research. Simulated research practice requires students to independently propose a clinical research hypothesis based on their theoretical knowledge. Each group of students had a clinical teacher and a statistics teacher for guidance throughout the process of topic selection, design, statistics, and writing. This approach culminated in a complete clinical research application and a mock defense, preparing students for real clinical research practice in the future. The details of the course design are presented in Table 2.
Course design of Didactic group and PICO group.
| Traditional teaching model | “PICO” teaching model | |
|---|---|---|
| Course content | Lectures | Lectures |
| Required content (offline) | Required content (online and offline) | |
| Basic principles of clinical research | Why do we need clinical research? | |
| Elements of research design | How do we formulate and select clinical research questions? | |
| Selection of research methods | How do we design and implement investigator-initiated clinical studies? | |
| Measurement and evaluation | How do we design case-control studies and cohort studies? | |
| Error control | How do we design randomized controlled clinical studies? | |
| Statistical analysis | How do we understand the relationship between medical ethics and clinical research? | |
| Ethical principles | ||
| Laws and regulations | ||
| Elective content (online) | ||
| Biostatistics | ||
| Research quality management | ||
| Medical ethics | ||
| Research translation and patent | ||
| Biobanking | ||
| Simulated research practice | ||
| Topic selection | ||
| Research design | ||
| Statistical strategy | ||
| Research application writing | ||
| Mock defense | ||
| Teaching process and teaching methods | Offline lectures | Online and offline; lectures and practice |
| Learning assessment | Classroom performance (40 %) | Online classroom quizzes (10 %) |
| Final examination (60 %) | Classroom quizzes and post-course assignments (20 %) | |
| Elective content (10 %) | ||
| Group discussions (20 %) | ||
| Clinical research mock defense (40 %) |
Learning assessment of the “PICO” model
O – outcome-based assessment
Students’ learning effectiveness was evaluated using a multi-dimensional approach, including teacher evaluation, peer evaluation, and self-evaluation. The assessments focused on comprehensive abilities such as integration of clinical research knowledge, professional application, medical research literacy, and humanistic and ethical literacy. The final grades consisted of five components: online classroom quizzes (10 %), classroom quizzes and post-course assignments (20 %), performance in elective content (10 %), performance in group discussions (20 %), and clinical research mock defense (40 %).
Course design and learning assessment for the Didactic group
The Didactic group received traditional didactic teaching. Theoretical lectures were taught according to the course content. Learning effectiveness was assessed based on the teachers’ evaluation of classroom performance (40 %) and the students’ scores in the final examination (60 %).
Data collection
Students’ final grades were used as indicators of learning effectiveness. The theoretical knowledge grade was calculated as the average of the scores obtained from multiple choice and short answer questions during the learning process. The PICO group’s grades included online and offline classroom quiz scores and post-class assignment scores, while the Didactic group’s grades included offline classroom quiz scores, post-class assignment scores, and final examination scores. The assignments and quizzes were identical for both groups. At the end of the course, students in both groups completed questionnaires to assess course satisfaction and self-assess competencies.
Data analysis
Statistical analysis was performed using GraphPad Prism 9.0 software. Continuous variables were expressed as mean ± standard deviation, and unpaired t-tests were used to compare differences between the two groups. Categorical variables were described using frequency and/or percentage, and differences between groups were assessed using the Chi-square test or Fisher’s exact test. Pearson correlation analysis was conducted to examine the relationship between variables. A significance level of p<0.05 was used to determine statistical significance.
Results
Baseline comparison of the two teaching groups
The PICO group comprised students with a mean age of (22.00 ± 0.52) years. Among them, 44.44 % (20/45) were male, with a baseline score of (82.57 ± 8.50) points. Two of the students had prior experience participating in clinical studies. The Didactic group consisted of students with a mean age of (22.11 ± 0.71) years, of whom 48.89 % (22/45) were male. Three students had participated in clinical studies. There were no significant differences between the two groups in terms of age, gender, baseline scores, and previous participation in clinical studies (p>0.05, Table 3).
Baseline characteristics of Didactic group and PICO group.
| Variable | PICO group (n=45) | Didactic group (n=45) | Statistics | p-Value |
|---|---|---|---|---|
| Gender (male/female) | 20/25 | 22/23 | X 2=0.179 | 0.673 |
| Age/years | 22.00 ± 0.52 | 22.11 ± 0.71 | T=0.842 | 0.402 |
| Baseline grades before the course (0–100 points; passing mark: ≥60 points) | 82.57 ± 8.50 | 81.42 ± 11.68 | T=0.531 | 0.597 |
| Have participated in clinical researches, n | 2 | 3 | X 2=0.212 | 0.645 |
Course grades of the two teaching groups
Table 4 presents the final grades of the students. The PICO group achieved a mean grade of (93.39 ± 2.61) points, while the Didactic group achieved a mean grade of (90.11 ± 2.24) points (p<0.001). When comparing the theoretical knowledge scores (including final examination scores and/or quiz scores) of the two groups, the PICO group scored significantly higher (88.62 ± 4.44) points than the Didactic group (82.94 ± 3.87, p<0.001). Further analysis of the sub-scores within the PICO group (Figure 1) revealed a positive correlation between theoretical knowledge scores (quiz scores) and group study scores (R=0.756, p<0.001) as well as mock defense scores (R=0.871, p<0.001).
Final grades of Didactic group and PICO group.
| Variable | PICO group (n=45) | Didactic group (n=45) | Statistics | p-Value |
|---|---|---|---|---|
| Average score of examinations and/or quizzes (0–100 points; passing mark: ≥60 points) | 88.62 ± 4.44 | 82.94 ± 3.87 | T=6.472 | <0.001 |
| Final grade (0–100 points; passing mark: ≥60 points) | 93.39 ± 2.61 | 90.11 ± 2.24 | T=6.406 | <0.001 |
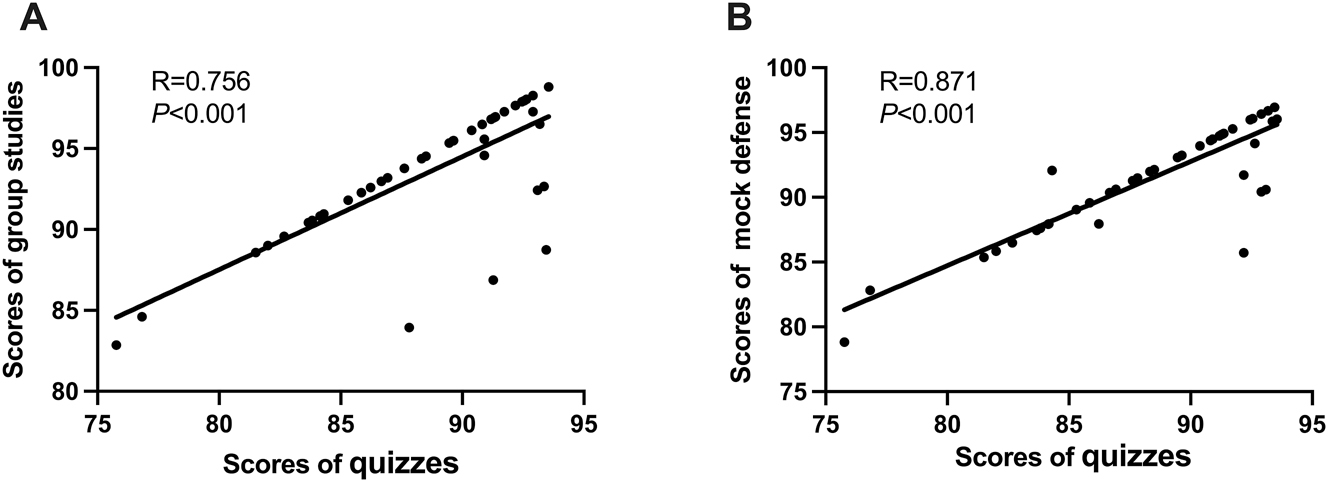
The correlation between different sub-scores in PICO group. (A) The correlation between quiz scores and group study scores; (B) the correlation between quiz scores and research project mock defense scores.
Course satisfaction of the two teaching groups
At the end of the course, a course satisfaction questionnaire was administered to both groups of students to assess their satisfaction towards the courses. The questionnaire covered four aspects: increased learning motivation, meeting learning needs, improved clinical research thinking and skills, and enhanced communication and teamwork skills (Table 5). The results indicated that the students in the PICO group were more satisfied with the course design, with 100 % of them strongly agreeing or agreeing with the statements. Compared to the Didactic group, the PICO group expressed higher satisfaction levels in terms of increased learning motivation, meeting learning needs, improved clinical research thinking and skills, and enhanced communication and teamwork skills (Figure 2). Notably, the PICO group showed a significantly higher level of agreement compared to the Didactic group in meeting learning needs (100.00 % vs. 80.00 %, p=0.017) and improving clinical research thinking and skills (100.00 % vs. 68.89 %, p<0.001) (Figure 2B and C).
Course satisfaction questionnaire.
| Question | Answer | |||
|---|---|---|---|---|
| Learning motivation | ||||
| The course has stimulated my interest in clinical research. | Strongly agree | Agree | Neutral | Disagree |
| The course has made the content accessible and clear. | Strongly agree | Agree | Neutral | Disagree |
| The course has increased my motivation to learn how to design clinical research. | Strongly agree | Agree | Neutral | Disagree |
| The course has improved my ability to in autonomous learning. | Strongly agree | Agree | Neutral | Disagree |
| Learning needs | ||||
| The course is useful for my future career. | Strongly agree | Agree | Neutral | Disagree |
| The course has clarified my purpose of learning. | Strongly agree | Agree | Neutral | Disagree |
| The course has improved my ability to solve case/project problems. | Strongly agree | Agree | Neutral | Disagree |
| The course has helped me to develop innovative thinking. | Strongly agree | Agree | Neutral | Disagree |
| Research thinking and skills | ||||
| The course has facilitated the generalization of my integrating knowledge framework. | Strongly agree | Agree | Neutral | Disagree |
| The course has improved my clinical research thinking and skills. | Strongly agree | Agree | Neutral | Disagree |
| The course has promoted my capacity to transform clinical problems into research inquiries. | Strongly agree | Agree | Neutral | Disagree |
| The course has bolstered my ability to critically analyze evidence. | strongly agree | Agree | neutral | disagree |
| Communication and teamwork skills | ||||
| The course has improved collaboration and teamwork skills. | Strongly agree | Agree | Neutral | Disagree |
| The course has sharpened my interpersonal and communication abilities. | Strongly agree | Agree | Neutral | Disagree |
| The course has facilitated the sharing of ideas and information with group members. | Strongly agree | Agree | Neutral | Disagree |
| The course has spurred my active participation in group discussions and collaborative learning. | Strongly agree | Agree | Neutral | Disagree |
| Overall assessment | ||||
| All in all, I am satisfied with this course. | Strongly agree | Agree | Neutral | Disagree |
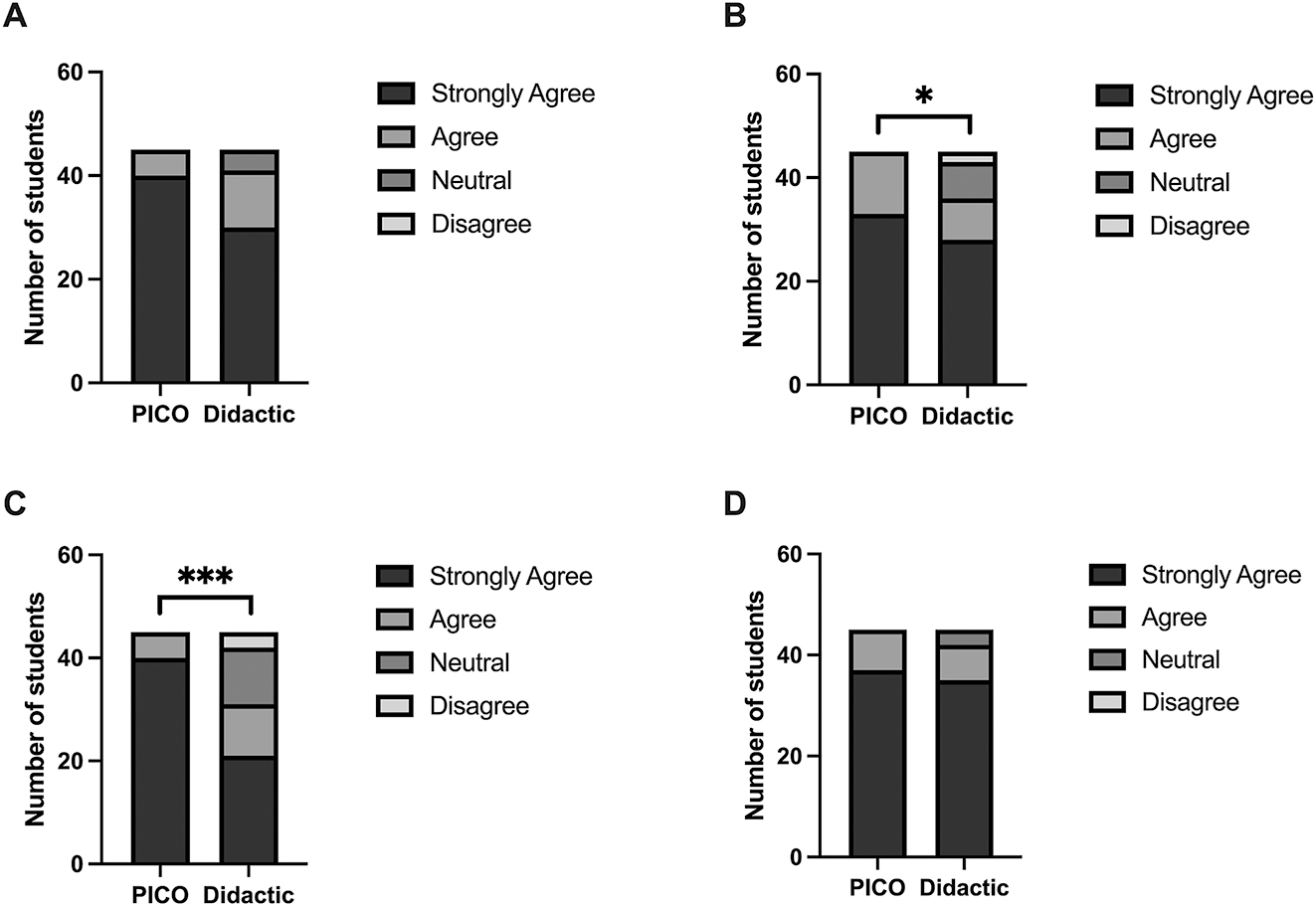
Students’ satisfaction with the course in Didactic group and PICO group. *p<0.05, ***p<0.001. PICO, “PICO” teaching model group; Didactic, Didactic teaching model group. (A) Increased motivation to learn. (B) Met my learning needs. (C) Improved clinical research thinking and skills. (D) Improved communication and teamwork skills.
Clinical research competency of the two teaching groups
Following the course, both groups of students completed a self-assessment scale to evaluate their clinical research competency. The scale comprised four items: knowledge integration, practical application, research literacy, and ethical awareness. Each item was scored on a scale of five. The results demonstrated that the PICO group had higher self-assessment scores across all four competencies compared to the Didactic group (Figure 3). Specifically, the differences between the PICO group and the Didactic group were statistically significant in knowledge integration [(3.99 ± 0.42) vs. (3.60 ± 0.35), p<0.001], practical application [(3.92 ± 0.43) vs. (3.48 ± 0.41), p<0.001], and research literacy [(3.93 ± 0.42) vs. (3.49 ± 0.42), p<0.001] (Figure 3). In the PICO group, 82.22 % (37/45) of the students incorporated the clinical research component into their dissertations, which encompassed controlled studies on new medical technologies, cohort studies on disease prognosis, clinical translational studies using new materials, and investigations of disease causation. In contrast, only 51.11 % (23/45) of the students in the Didactic group included the clinical research component in their dissertations, which was significantly lower than that of the PICO group (p=0.003).
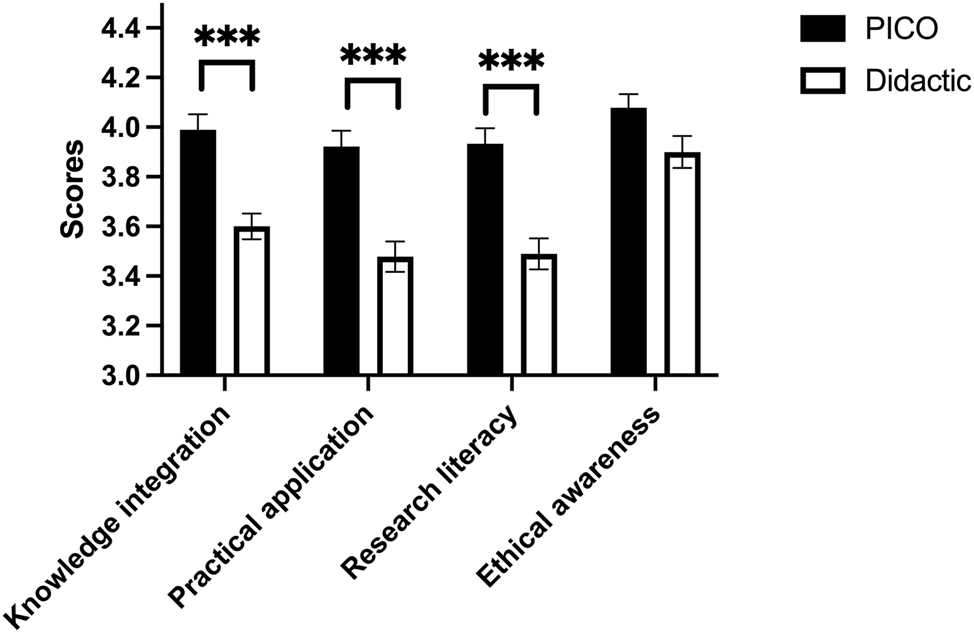
The comparison of students’ self-assessment scores of clinical research competency between the PICO group and Didactic group. ***p<0.001. PICO, PICO teaching model group; Didactic, Didactic teaching model group.
Discussion
This study aimed to compare the effectiveness of two different teaching methods in the context of clinical research education. The results demonstrated significant advantages of the “PICO” teaching model in several aspects, providing valuable insights and a foundation for the educational practice of clinical research methodology.
The students in the PICO group exhibited significant improvement in their theoretical knowledge scores, indicating that the “PICO” teaching model enhanced students’ understanding and mastery of knowledge. Further analysis revealed a positive correlation between theoretical scores and group study or mock defense scores. This suggests that the “PICO” teaching model facilitates the integration and application of students’ knowledge, enabling them to effectively connect theoretical knowledge with practical aspects. The noteworthy progress made in the PICO group not only highlights the effectiveness of the “PICO” teaching model in knowledge transfer but also reflects its positive contribution to students’ cognitive development. This model stimulates students’ interest and initiative in learning, encouraging them to think critically and explore topics more deeply [7, 8]. The positive correlation between theoretical scores and group study or mock defense scores further confirms that the “PICO” teaching model enhances students’ ability to integrate and transfer knowledge, enabling them to flexibly apply what they have learned to solve practical problems [9]. This model directly addresses the challenges outlined in the preamble – particularly the issues of student engagement and motivation. By incorporating personalized learning, interactive teaching, and clinical practice integration, the “PICO” model transforms the passive learning environment typical of traditional lectures into a dynamic, participative one. For instance, the emphasis on real clinical cases and group discussions fosters critical thinking and allows students to connect theoretical concepts to practical applications, thus overcoming the challenge of superficial understanding.
Traditional didactic teaching often results in students adopting a passive role, where they are primarily recipients of information rather than active participants in their learning process. This passivity can lead to disengagement and a lack of motivation, which are detrimental to the acquisition of complex knowledge such as that found in clinical research. In contrast, the “PICO” model requires students to take an active role in their education. By engaging in problem-solving exercises and collaborative discussions, students are more likely to internalize knowledge and develop critical thinking skills. The satisfaction level of the students in the PICO group was significantly higher, indicating their recognition and acceptance of the “PICO” teaching model. This result confirms the effectiveness and appeal of the model. Increased satisfaction among students in the PICO group reflects their positive learning experience and the model’s ability to stimulate their interest and motivation. This high level of satisfaction also directs our attention toward better meeting students’ needs and enhancing their learning experience, ultimately improving the quality of teaching [10]. Moreover, the “PICO” model employs various interactive teaching methods, such as simulations of clinical research situations, role-playing, and flipped classroom activities. These methods facilitate deeper engagement with the material and encourage students to take ownership of their learning. Through these activities, students not only learn the theoretical aspects of clinical research but also practice applying their knowledge in realistic settings, which enhances their overall understanding and retention of the material. In this study, both groups of students accomplished same credit hours, but students in the PICO group did study for relatively longer period of time and space due to their own interest in learning or increased learning needs. Interactive teaching enhances students’ engagement and interest, and interactive teaching encourages communication and cooperation among students, which contributes to knowledge sharing and creativity and improves learning efficiency. The combination of online and offline learning can meet the learning needs of different students and make learning more flexible and personalized, enabling students to learn at a time that best suits them, which also helps to improve learning efficiency. Although the PICO group’s learning hours may have been extended, the improvement in performance is more likely to be due to improved teaching methods and increased learning efficiency. In subsequent studies, we’ll analyze students’ learning behaviors under the “PICO” teaching model, such as the time spent on online learning and the frequency of interactions, and conduct correlation analyses with performance improvement to more precisely measure the relationship between study time and academic performance.
The “PICO” teaching model significantly improved the clinical research competency of students in the PICO group. This finding suggests that the model is conducive to cultivating students’ practical application skills and comprehensive abilities, providing a solid foundation for their future development. The incorporation of multidisciplinary knowledge not only equips students with a deeper understanding of clinical research but also prepares them for the collaborative nature of modern healthcare. The ability to integrate knowledge from various fields, such as epidemiology, statistics, and ethics, is essential for conducting high-quality clinical research. In the PICO group, students reported higher self-assessment scores in areas such as knowledge integration, practical application, and research literacy. This improvement can be attributed to the “PICO” model’s emphasis on outcome-based assessment, where students are evaluated on their ability to apply theoretical knowledge to real-world scenarios. By focusing on practical applications, the “PICO” model encourages students to think critically and creatively, preparing them for the challenges they may face in their future careers. Moreover, the “PICO” model promotes the development of essential skills such as statistical analysis, ethical reasoning, and effective communication. These skills are vital for conducting research that adheres to ethical standards and addresses pressing clinical questions. By equipping students with these competencies, the “PICO” model not only enhances their academic performance but also prepares them to contribute meaningfully to the field of medicine. The model develops key abilities such as innovative thinking, practical skills, and teamwork, equipping students with the necessary capabilities to adapt to future challenges. This aligns with the demand for high-quality medical professionals in today’s society. Furthermore, the “PICO” model emphasizes personalized learning, which is crucial for addressing the varying levels of prior knowledge and interest among students. In a cohort of medical students, individuals may have different backgrounds, experiences, and career aspirations. The “PICO” model allows for customization in learning paths, enabling students to choose elective topics that align with their interests and future career goals. This personalization increases motivation and engagement, as students are more likely to invest time and effort into learning when they see its relevance to their personal and professional aspirations.
The high level of satisfaction among students in the PICO group suggests that the model is adaptable and could be applied to other educational contexts beyond clinical research. For example, the principles of personalized learning and interactive teaching could be beneficial in other medical courses, such as pharmacology or pathology, where critical thinking and practical application are essential. In these contexts, the “PICO” model could be employed to help students formulate research questions related to drug efficacy or disease mechanisms, thereby fostering a deeper understanding of these complex subjects. Moreover, the “PICO” model’s focus on collaborative learning is highly relevant in today’s educational landscape, where teamwork and communication skills are increasingly emphasized in professional settings. By incorporating group discussions and collaborative projects, the “PICO” model prepares students not only for academic success but also for their future roles as healthcare professionals, where teamwork is essential for effective patient care. Additionally, the “PICO” model could be adapted for use in other fields outside of medicine. For instance, in disciplines such as education, social sciences, and even business, the emphasis on real-world applicability can enhance student engagement and promote a deeper understanding of the subject matter across various academic disciplines.
Conclusions
In conclusion, the remarkable effects of the “PICO” teaching model in this study offer new perspectives and directions for clinical research courses. However, it is crucial to acknowledge that education is a complex and multifaceted system, and each teaching method has its own applicable contexts and limitations. The insights gained from this study highlight the importance of continuously exploring innovative teaching methods that can enhance student engagement, promote critical thinking, and improve practical skills. Future research should focus on the long-term impact of the “PICO” teaching model on students’ clinical competencies and career trajectories. Additionally, studies could explore the effectiveness of the “PICO” model in various educational settings and disciplines, further validating its applicability as a versatile teaching approach. Ultimately, the application of these research findings should be actively promoted in a wider range of educational practices to foster overall development and progress. By embracing innovative teaching methods like the “PICO” model, educators can better prepare students for the complexities of modern healthcare and contribute to the development of competent, compassionate medical professionals.
Funding source: the Shanghai Jiao Tong University Online and Offline Blended Course Program for 2023-2024 Academic Years
Award Identifier / Grant number: 2023-030-25
Funding source: the Teaching Physician Program of Shanghai Ninth People’s Hospital
Award Identifier / Grant number: JXXYS-2023-5
Funding source: the Medical Education Development and Research Project of Shanghai Ninth People’s Hospital
Award Identifier / Grant number: JYJX03202213
-
Research ethics: Not applicable.
-
Informed consent: Written informed consent was obtained from all participants, in accordance with the Declaration of Helsinki.
-
Author contributions: Shuai Ma – drafting the manuscript, analyzing the data. Shuai Ma, Pei Pan, Gang Xu, Wenyi Yang, Dong Li, Tian Shen, Zhichao Wang, Yong Cai and Min Yao – designing the course. Pei Pan – analyzing the data. Yong Cai – distributing the questionnaire and revision of the manuscript. Min Yao – conceptualizing the study and leading the writing team. The authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Use of Large Language Models, AI and Machine Learning Tools: None declared.
-
Conflict of interest: The authors state no conflict of interest.
-
Research funding: This study was supported by the Teaching Physician Program of Shanghai Ninth People’s Hospital (JXXYS-2023-5), the Medical Education Development and Research Project of Shanghai Ninth People’s Hospital (JYJX03202213) and the Shanghai Jiao Tong University Online and Offline Blended Course Program for 2023–2024 Academic Years (2023-030-25).
-
Data availability: Not applicable.
References
1. Tunis, SR, Stryer, DB, Clancy, CM. Practical clinical trials: increasing the value of clinical research for decision making in clinical and health policy. JAMA 2003;290:1624–32. https://doi.org/10.1001/jama.290.12.1624.Search in Google Scholar PubMed
2. Neely, JG, Hartman, JM, Wallace, MS, Forsen, JWJr. Tutorials in clinical research: part III. Selecting a research approach to best answer a clinical question. Laryngoscope 2001;111:821–31. https://doi.org/10.1097/00005537-200105000-00013.Search in Google Scholar PubMed
3. Kiani, AK, Naureen, Z, Pheby, D, Henehan, G, Brown, R, Sieving, P, et al.. Methodology for clinical research. J Prev Med Hyg 2022;63:E267–78. https://doi.org/10.15167/2421-4248/jpmh2022.63.2S3.2769.Search in Google Scholar PubMed PubMed Central
4. Kao, LS, Tyson, JE, Blakely, ML, Lally, KP. Clinical research methodology I: introduction to randomized trials. J Am Coll Surg 2008;206:361–9. https://doi.org/10.1016/j.jamcollsurg.2007.10.003.Search in Google Scholar PubMed PubMed Central
5. da Costa Santos, CM, de Mattos Pimenta, CA, Nobre, MR. The PICO strategy for the research question construction and evidence search. Rev Lat Am Enfermagem 2007;15:508–11. https://doi.org/10.1590/s0104-11692007000300023.Search in Google Scholar PubMed
6. Schiavenato, M, Chu, F. PICO: what it is and what it is not. Nurse Educ Pract 2021;56:103194. https://doi.org/10.1016/j.nepr.2021.103194.Search in Google Scholar PubMed
7. LoVerde, JA, Kerber, C, Kisch, T, Miller, B, Jenkins, S, Shropshire, M. Comparison of lecture and manipulative teaching methods on learning and application to practice. Nurs Forum 2021;56:520–8. https://doi.org/10.1111/nuf.12575.Search in Google Scholar PubMed
8. Frank, JR, Snell, LS, Cate, OT, Holmboe, ES, Carraccio, C, Swing, SR, et al.. Competency-based medical education: theory to practice. Med Teach 2010;32:638–45. https://doi.org/10.3109/0142159X.2010.501190.Search in Google Scholar PubMed
9. Bandiera, G, Kuper, A, Mylopoulos, M, Whitehead, C, Ruetalo, M, Kulasegaram, K, et al.. Back from basics: integration of science and practice in medical education. Med Educ 2018;52:78–85. https://doi.org/10.1111/medu.13386.Search in Google Scholar PubMed
10. Alamri, HA, Watson, S, Watson, W. Learning technology models that support personalization within blended learning environments in higher education. TechTrends 2021;65:62–78. https://doi.org/10.1007/s11528-020-00530-3.Search in Google Scholar
© 2024 the author(s), published by De Gruyter on behalf of the Shanghai Jiao Tong University and the Shanghai Jiao Tong University School of Medicine
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Frontmatter
- Editorial
- Evolving landscapes in global medical education: navigating challenges and embracing innovation
- Review Articles
- Embarking on the era in new medicine: reshaping the systems of medical education and knowledge
- Aligning the education of medical students to healthcare in the UK
- Characteristics and considerations of French medical education
- Research Articles
- “Global challenge program” projects themed on preventing zoonosis: developing One Health core competences in medical students at SJTU
- Innovative exploration of designing the ‘Host Defense and Immunology’ course based on the concept of seamless learning
- Comparing the effects of blended learning and traditional instruction on “Medical Genetics and Embryonic Development” in undergraduate medical students: a randomized controlled trial
- The application of the “PICO” teaching model in clinical research course for medical students
- Factors bridging medical graduate students’ training and future academic achievements of dermatologists in China
- The teaching design and implementation of “Helicobacter pylori” in medical microbiology
Articles in the same Issue
- Frontmatter
- Editorial
- Evolving landscapes in global medical education: navigating challenges and embracing innovation
- Review Articles
- Embarking on the era in new medicine: reshaping the systems of medical education and knowledge
- Aligning the education of medical students to healthcare in the UK
- Characteristics and considerations of French medical education
- Research Articles
- “Global challenge program” projects themed on preventing zoonosis: developing One Health core competences in medical students at SJTU
- Innovative exploration of designing the ‘Host Defense and Immunology’ course based on the concept of seamless learning
- Comparing the effects of blended learning and traditional instruction on “Medical Genetics and Embryonic Development” in undergraduate medical students: a randomized controlled trial
- The application of the “PICO” teaching model in clinical research course for medical students
- Factors bridging medical graduate students’ training and future academic achievements of dermatologists in China
- The teaching design and implementation of “Helicobacter pylori” in medical microbiology

