A rare case of acrocephaly: Saethre-Chotzen syndrome or Crouzon?
-
Rebeca Garrote Molpeceres
Rebeca Garrote MolpeceresHospital Clínico Universitario de Valladolid – Pediatría y sus Áreas Específicas, Avda. Ramón y Cajal, 3 Valladolid Valladolid 47003, Spain, Tel.: +34 699306093/983556053Diesen Autor / diese Autorin suchen:
, Elena Urbaneja Rodriguez
Abstract
Acrocephaly is a common neonatal craniofacial malformation. Saethre-Chotzen syndrome (SCS) is one of the acrocephaly related syndromes less frequently described in the literature. A female newborn term was admitted to our Neonatal Unit to study craniofacial dysmorphia without family history of interest. Pregnancy, childbirth and the neonatal period were uneventful. She had exotropia, short anterior-posterior cranial diameter, flat occiput and wide normotensive anterior fontanelle (beginning at the nose root, continuing through the sagittal suture with the posterior fontanelle) without syndactyly. The scanner imaging confirmed an acrocephaly with fusion of bilateral coronal sutures. We initially suspected a cranyosinostosis due to a Crouzon syndrome or SCS. After differential diagnosis and genetic study the patient was diagnosed as having SCS due to a de novo TWIST1 gene mutation. The craniofacial dysmorphias were corrected early by neurosurgical with good results. This case shows a new example of the phenotypic and genotypic variability of these TWIST1 gene mutations.
Introduction
Acrocephaly or craniosynostosis is a common neonatal malformation, with an incidence of 1/2000–2500 live births. It consists in premature fusion of one or more cranial sutures, causing deformity. Fifteen percent of cases are part of defined syndromes, there are more than 180 different [1].
Saethre-Chotzen syndrome (SCS), also known as acrocephalosyndactyly type III, is one of the less frequent acrocephaly syndromes described in the literature. It shares phenotypic characteristics with Crouzon syndrome, which can hinder its differential diagnosis. Frequently it is caused by TWIST1 gene mutations on chromosomes 7p21.p23, transmitted with autosomal dominant inheritance. It produces premature fusion of coronal, lambdoid, and/or metopic sutures, causing craniosynostosis with craniofacial dysmorphias often associated with syndactyly [1], [2], [3]. Most children affected by SCS have associated mental disability and can have autistic behavior.
We present a female newborn without family acrocephaly history who had SCS caused by a de novo mutation in the TWIST1 gene. She had important craniofacial dysmorphia without syndactyly and mild psychomotor retardation which improved after stimulation in a special center. This case shows a new example of the phenotypic and genotypic variability of these TWIST1 gene mutations [2], [3].
Case report
A female newborn term with 40 weeks of gestation was admitted to our Neonatal Unit in the perinatal period to study craniofacial dysmorphia. There was no family history of interest. Pregnancy, childbirth and the neonatal period were uneventful.
She had the following birth somatometry: weight 3.760 g (Pc90), size 53 cm (Pc>97), cephalic perimeter 34 cm (Pc50). Physical examination showed turricephalic forehead, short anterior-posterior cranial diameter and flat occiput. She had wide anterior fontanelle, beginning at nose root and continuing through the sagittal suture with a posterior fontanelle, low-set hair implantation, bulging forehead, flat face with antimongoloid palpebral fissures, bilateral exotropia, depressed nasal bridge with septal deviation, maxillary hypoplasia, low-set ears with “horizontal cross helix” sign (associated with SCS) and arched palate. She also showed cervical marked hypotonia. No other physical malformations were observed. Cranial X-ray images confirmed the physical findings, due to an early closure of bilateral coronal sutures (Figure 1).
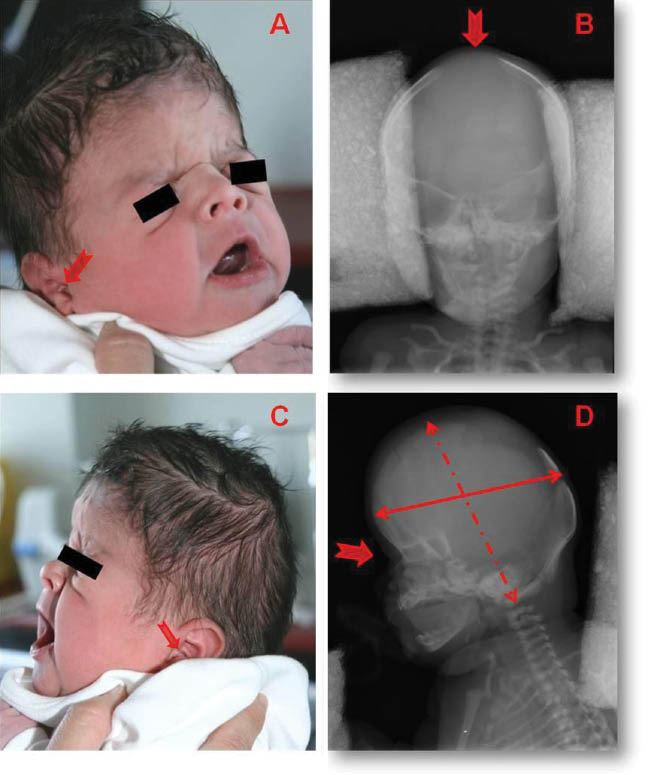
Physical dismorphias (A, C) compared to AP and lateral cranial X-ray images (B, D): turricephalic forehead.
Shortening of the anterior-posterior cranial diameter. Flat occiput. Low hair implantation. Wide normotensive anterior fontanelle (see wide red arrow). Bulging forehead. Flat face with antimongoloid palpebral fissures. Exotropia. Depressed nasal bridge. Maxillary hypoplasia. Low-set ears with “horizontal cross helix” sign (see narrow red arrow).
Vertebral and limbs X-ray, audiometry, echocardiography and abdominal echography were normal. In transfontanelar ultrasound we saw asymmetry because of left lateral ventricle enlargement. The scanner images showed cranial asymmetry with early closure of bilateral coronal and metopic sutures, a large bone defect of the sagittal suture, bilateral exotropia and deviated nasal septum (Figure 2). Radiologists made a 3D cranial scanner reconstruction to aid in defining the type of cranyosinotosis (Figure 3).

Cranial scanner images.
(A) Ventricular asymmetry because of a slight enlargement of the left lateral ventricle. (B) Bilateral exotropia. (C) Deviated nasal septum.
![Figure 3:
3D Cranial scanner images.
(A) Wide anterior fontanelle. (B) Bilateral coronal suture fusion and wide sagittal suture defect and posterior fontanelle [a: anterior, p: posterior]. (C) Turricephaly forehead. (D) Cranial asymmetry.](/document/doi/10.1515/crpm-2015-0057/asset/graphic/j_crpm-2015-0057_fig_007.jpg)
3D Cranial scanner images.
(A) Wide anterior fontanelle. (B) Bilateral coronal suture fusion and wide sagittal suture defect and posterior fontanelle [a: anterior, p: posterior]. (C) Turricephaly forehead. (D) Cranial asymmetry.
We suspect that she suffered from a craniosynostosis due to a Crouzon syndrome or SCS. The genetic study was requested for the most common mutations described associated with them. The patient is a heterozygous carrier of c.422A>G de novo mutation that maps to chromosome band 7p21.1 in the TWIST1 gene, associated with SCS [1], [2], [3].
During the first 3 months of life she required several hospitalizations for clinical respiratory failure associated with infectious processes. The patient was referred to the reference unit of craniofacial surgery, where, after a cranial MRI that ruled tonsillar and hydrocephalus decline, she underwent surgery craniofacial remodeling through bilateral craniectomy placement of the fronto-orbital bar to the age of 8 months. She had good cosmetic outcome (Figure 4) and neurosurgery improved respiratory symptoms, without new admissions to hospital. Initially she had mild psychomotor retardation which improved after stimulation in a special center and at home for a few months.

Before and after neurosurgery acrocephaly correction. (A) 8 months of life. (B) One year old.
Discussion
Acrocephaly syndromes exhibit variable clinical and genetic heterogeneity with a great variety of suture closure combinations which produce craniofacial deformities associated with other organic anomalies and developmental delay. Many of these disorders are caused by mutations in the fibroblast growth factor receptor genes: FGFR2, FGFR3 (encoding fibroblast growth factor receptors), TWIST1 (functions as an upstream regulator of FGFRs) and EFNB1 (gene encoding fibrillin1) [1], [2], [3].
Saethre-Chotzen syndrome (SCS) is an uncommon cause of craniosynostosis produced by the TWIST1 gene mutations on chromosome 7p21.p23 with autosomical dominant inheritance and great phenotypic variability. De novo 7p21.p23 mutations and in FGFR2 have also been reported [1]. It is often characterized by premature coronal sutures fusion, facial dysmorphism, crus auricularis sign, syndactyly, skeletal deformity, high-arched palate and congenital heart malformations [4]. They can have developmental delay, learning difficulties and some cases are associated with autistic behavior [2], [5].
SCS has poor sonographic prenatal diagnosis, as our patient, whose prenatal echographic screening was normal. Nevertheless Massalska et al. have published a prenatal diagnosis of craniosynostosis caused by a de novo complex chromosomal rearrangement (1; 4; 7) with a microdeletion of 7p21.3–7p15.3, which include the TWIST1 gene [3].
New forms and varieties of craniosynostosis are identified due to the introduction of microarray-based comparative genomic hybridization techniques in their diagnosis [2]. Recently Tahiri et al. have describe a new pattern of sutural fusion “peace sign synostosis” characterized by synostosis of the metopic, bicoronal, and sagittal sutures associated with abnormalities of the TWIST1 gene [6].
Our newborn had all typical SCS craniofacial dysmorphia manifestations but she did not have the commonly syndactyly seen with it, this has been described in other SCS cases [7].
The SCS share phenotypic characteristics with another craniosynostosis, mainly with Crouzon syndrome, which should be included in the differential diagnosis. A detailed physical exploration, imaging examinations (transfontanellar ecography, echocardiography, abdominal ultrasound, cranial scanner, MRI examination) and an exhaustive genetic study are important to identify the type of acrocephaly [1], [2], [3].
SCS caused by microdeletion is generally characterized by mental disability. It has been described that gene(s) deletion in 5′ upstream region of FERD3L (flanking gene of TWIST1, RefSeqNM_152898) contributes to significant developmental delay independent of compressive cranial injuries [2]. Our patient was a heterozygous carrier of the c.422A>G de novo mutation, this fact associated with minimal early neurosurgical correction [8] and neurological stimulation made it possible that she has minimal psychomotor retardation.
The improvement in prenatal ultrasound diagnosis and advances in the development of new genetic diagnostic techniques will make possible an early diagnosis of these syndromes, facilitating typing, individualized programming of a monitoring and therapeutic plan as well as possibility of appropriate genetic counseling to parents.
References
[1] Heuzé Y, Holmes G, Peter I, Richtsmeier JT, Jabs EW. Closing the gap: genetic and genomic continuum from syndromic to nonsyndromic craniosynostoses. Curr Genet Med Rep. 2014;2:135–45.10.1007/s40142-014-0042-xSuche in Google Scholar PubMed PubMed Central
[2] di Rocco F, Benoit A, Vigneron J, Segura PB, Klein O, Collet C, et al. Y-craniosynostosis by premature fusion of the metopic and coronal sutures: a new nosological entity or a variety of Saethre-Chotzen syndrome? Birth Defects Res A Clin Mol Teratol. 2015;103:306–10.10.1002/bdra.23367Suche in Google Scholar PubMed
[3] Massalska D, Bijok J, Kucińska-Chahwan A, Jamsheer A, Bogdanowicz J, Jakiel G, et al. Prenatal diagnosis of craniosynostosis (compound Saethre-Chotzen syndrome phenotype) caused by a de novo complex chromosomal rearrangement (1; 4; 7) with a microdeletion of 7p21.3–7p15.3, including TWIST1 gene – a case report. Ginekol Pol. 2014;85:541–4.10.17772/gp/1768Suche in Google Scholar PubMed
[4] Sharma A, Patel N, Arora S, Ramachandran R. Child with Saethre-Chotzen syndrome: anesthetic management and literature review. Acta Anaesthesiol Belg. 2014;65:179–82.Suche in Google Scholar
[5] Shimada S, Okamoto N, Nomura S, Fukui M, Shimakawa S, Sangu N, et al. Microdeletions of 5.5 Mb (4q13.2–q13.3) and 4.1 Mb (7p15.3–p21.1) associated with a saethre-chotzen-like phenotype, severe intellectual disability, and autism. Am J Med Genet A. 2013;161A:2078–83.10.1002/ajmg.a.36027Suche in Google Scholar PubMed
[6] Tahiri Y, Bastidas N, McDonald-McGinn DM, Birgeld C, Zackai EH, Taylor J, et al. New pattern of sutural synostosis associated With TWIST gene mutation and Saethre-Chotzen syndrome: peace sign synostosis. J Craniofac Surg. 2015;26:1564–7.10.1097/SCS.0000000000001884Suche in Google Scholar PubMed
[7] Cho E, Yang TH, Shin ES, Byeon JH, Kim GH, Eun BL. Saethre–Chotzen syndrome with an atypical phenotype: identification of TWIST microdeletion by array CGH. Childs Nerv Syst. 2013;29:2101–4.10.1007/s00381-013-2235-0Suche in Google Scholar PubMed
[8] Governale LS. Minimally invasive pediatric neurosurgery. Pediatr Neurol. 2015;52:389–97.10.1016/j.pediatrneurol.2014.08.036Suche in Google Scholar PubMed
-
The authors stated that there are no conflicts of interest regarding the publication of this article.
©2016 Walter de Gruyter GmbH, Berlin/Boston
Artikel in diesem Heft
- Frontmatter
- Case Reports – Obstetrics
- The Bakri balloon implementation during cesarean section without switching to the lithotomy position
- Recurrent large uterine fundal dehiscence during cesarean section after hysteroscopic uterine septum resection with uterine perforation
- Unexpected pregnancy during tamoxifen treatment: a case report and review of the literature
- Postpartum hemorrhage in the setting of a mechanical heart valve
- Spontaneous cord hematoma: report of two cases
- Anencephaly with placental adhesion
- Negative pressure wound treatment for uterine incision necrosis following a cesarean section
- Management of very early preterm premature rupture of membranes (PPROM) in twin pregnancies by selective feticide
- Spontaneous carotid artery dissection in pregnancy
- Spontaneous heterotopic triplet pregnancy with intrauterine monochorionic-monoamnionic twins
- Case Reports – Fetus
- Importance of perinatal care for pregnant women with severe fetal multiple limb abnormalities
- Mitoxantrone exposure in pregnancy: a new case report in a multiple sclerosis patient
- Transient iatrogenic heart block following foetal intracardiac transfusion for severe twin anaemia-polycythaemia sequence
- Vertical transmission of Zika virus (ZIKV) in early pregnancy: two cases, two different courses
- Case Reports – Newborn
- Early neonatal pyloric stenosis after exposure to maternal macrolide therapy
- Case report of neonatal near drowning associated with underwater birth
- Thoracoschisis secondary to a mesenchymal hamartoma associated with diaphragmatic eventration
- Acute myocardial infarction in a premature infant on the first day of life
- A rare case of acrocephaly: Saethre-Chotzen syndrome or Crouzon?
- Chest drain associated neonatal pneumopericardium
- Raynaud’s phenomenon in a newborn: case report and review of the literature
- Late-onset brain abscess due to group B Streptococcus
Artikel in diesem Heft
- Frontmatter
- Case Reports – Obstetrics
- The Bakri balloon implementation during cesarean section without switching to the lithotomy position
- Recurrent large uterine fundal dehiscence during cesarean section after hysteroscopic uterine septum resection with uterine perforation
- Unexpected pregnancy during tamoxifen treatment: a case report and review of the literature
- Postpartum hemorrhage in the setting of a mechanical heart valve
- Spontaneous cord hematoma: report of two cases
- Anencephaly with placental adhesion
- Negative pressure wound treatment for uterine incision necrosis following a cesarean section
- Management of very early preterm premature rupture of membranes (PPROM) in twin pregnancies by selective feticide
- Spontaneous carotid artery dissection in pregnancy
- Spontaneous heterotopic triplet pregnancy with intrauterine monochorionic-monoamnionic twins
- Case Reports – Fetus
- Importance of perinatal care for pregnant women with severe fetal multiple limb abnormalities
- Mitoxantrone exposure in pregnancy: a new case report in a multiple sclerosis patient
- Transient iatrogenic heart block following foetal intracardiac transfusion for severe twin anaemia-polycythaemia sequence
- Vertical transmission of Zika virus (ZIKV) in early pregnancy: two cases, two different courses
- Case Reports – Newborn
- Early neonatal pyloric stenosis after exposure to maternal macrolide therapy
- Case report of neonatal near drowning associated with underwater birth
- Thoracoschisis secondary to a mesenchymal hamartoma associated with diaphragmatic eventration
- Acute myocardial infarction in a premature infant on the first day of life
- A rare case of acrocephaly: Saethre-Chotzen syndrome or Crouzon?
- Chest drain associated neonatal pneumopericardium
- Raynaud’s phenomenon in a newborn: case report and review of the literature
- Late-onset brain abscess due to group B Streptococcus



