Sample hemolysis is conventionally defined as the presence of a variable amount of cell-free hemoglobin in serum or plasma. The reference (i.e. “normal”) concentration of free and measurable hemoglobin conventionally ranges between 0.22 and 0.25 g/L in serum and between 0.10 and 0.13 g/L in plasma, respectively [1]. Although no definitive evidence exists about the threshold of “pathological” hemolysis in blood samples, universal consensus has been reached that clinically significant interference for the most hemolysis-vulnerable tests (i.e. potassium, lactate dehydrogenase, aspartate aminotransferase) may start with concentrations of cell-free hemoglobin ≥0.5 g/L [2], [3]. Notably, this cut-off is also conventionally used for monitoring phlebotomy practice [4].
Although the very first studies about the impact of sample hemolysis on the quality of laboratory testing have been published more than 40 years ago [5], the frequency of hemolyzed samples remains high and generates remarkable challenges in clinical laboratory practice [6], [7], [8]. The first important issue is distinguishing between in vitro (i.e. spurious) and in vivo (i.e. hemolytic anemia) hemolysis. The differentiation between these conditions is not meaningless because the former case reflects a kaleidoscope of problems emerging throughout preanalytical sample management, thus including blood drawing, handling, transportation, storage and preparation for testing, whilst the latter mirrors a life-threatening condition, which must be timely communicated to the clinicians for adopting the most appropriate care options. According to this perspective, the second and almost consequential aspect is the need of systematically monitoring sample quality for accurate and rapid identification of hemolysis in serum or plasma, as also currently endorsed by many international accreditation standards such as the International Standards Organization (ISO) 15189:2012 and the International Federation of Clinical Chemistry and Laboratory Medicine (IFCC) [9]. The most obvious consequence is that all laboratories should adopt a reliable strategy for systematic monitoring of sample quality and, moreover, for identifying the presence of, and quantifying, cell-free hemoglobin in either serum or plasma.
In this issue of the journal, we publish an interesting study aimed to assess whether visual inspection of sample hemolysis by comparison with a color chart, rather than automatic assessment of serum or plasma indices, may have an impact on patient safety [10]. Interestingly, the authors concluded that nearly one-third of test results generated with manual handling of hemolyzed specimens were incorrectly managed, mainly for incorrect release of hemolysis-sensitive tests results or for unnecessary suppression of data in specimens with non-clinically significant degrees of hemolysis. In both cases, these circumstances may seriously jeopardize the managed care because release of data biased for the presence of hemolysis may then trigger inappropriate therapeutic options (i.e. administration of potassium-lowering therapy in patients with “spurious” hyperkalemia), whereas unjustified test suppression may delay both diagnosis and treatment of potentially fatal diseases (i.e. delayed or inappropriate management of arrhythmias due to underdiagnosis of in vivo hyperkalemia).
Color vision is conventionally defined as the capability of distinguishing colors according to the wavelengths of light reflected, emitted or transmitted. The individual ability to identify colors and perceiving their intensity depends on multiple factors, such as the local environment and its relative light exposure, but may also relay on some genetic (i.e. Opsin gene polymorphisms), anatomic and pathological aspects, which ultimately make the eyes of one subject more capable than others (color blindness, also known as “daltonism”, is a paradigmatic example) (Figure 1) [11], [12]. All these factors make color recognition rather heterogeneous in different environments and among different individuals, thus supporting the hypothesis that visual assessment of sample quality may be highly inaccurate. Previous and highly reliable evidence has been provided that visual detection of hemolyzed samples is more inaccurate compared with automatic detection [13], [14], thus paving the way to adopting more precise and standardized approaches. The current generation of preanalytical platforms and laboratory instrumentation for either clinical chemistry or coagulation testing is increasingly equipped with the so-called serum (or plasma) indices. Briefly, the extent of hemolysis, turbidity and icterus is roughly estimated by using multichromatic wavelength readings and calculation formulas integrating adjustments for compensating spectral overlap. In most analyzers, the automatic estimation of these indices does not entail the use of specific reagents and is fully automated and rapid, so that objective interference data can be added to, and hence complement, test results. The technical and clinical advantages of this technique are unquestionable because it provides a standardized means of assessing sample quality and can be easily incorporated into automatic decision-making algorithms, thus alleviating routine activity and preventing disputes with clinicians when suppressing data [15].
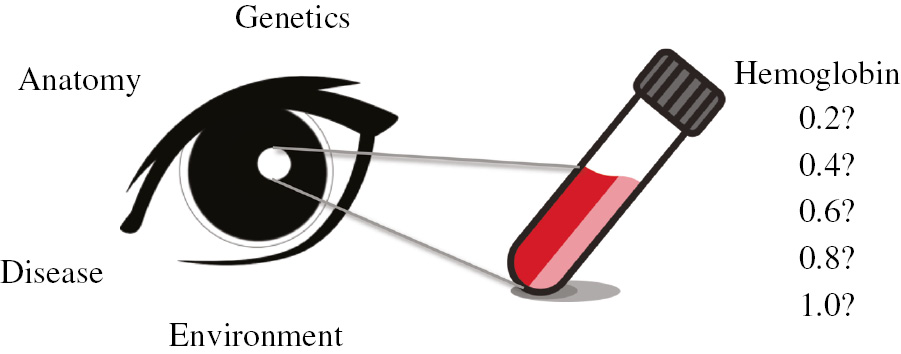
Sources of interindividual variability in visual assessment of sample quality.
Yet, some problems remain even after widespread implementation of serum or plasma indices. Beside the lack of standardized day-to-day quality control material for serum or plasma indices measurement, the use of specific cutoffs for suppressing unreliable test results is a virtually unmanageable issue because each reagent has particular vulnerability to the presence of cell-free hemoglobin or other interfering substances that may be present in the test sample. Hence, parameter-specific cutoffs should be provided by instrument or assay manufacturers based on clinical acceptability criteria [16]. Similarly, the technical approach used for estimating interference from hemoglobin, lipids and bilirubin in serum or plasma are often dissimilar among the various manufacturers, thus making data (either quantitative or semi-quantitative) poorly comparable [17]. Thereby, harmonization of both measurement and interference thresholds seems a rather unreachable target at present. Then, although it has been clearly demonstrated that the turnaround time would not be affected [18], many laboratory professionals are still persuaded that routine assessment of serum or plasma indices may wreck an optimal workflow. Another potential drawback comes from the obvious consequence that routine assessment of sample quality will generate larger suppression of test results, which may then cause adjunctive relational issues with laboratory stakeholders.
Although all these aspects cannot be ignored, the many described advantages, combined with the evidence provided by Luksic et al. [10] that visual inspection may seriously jeopardize patient safety, would finally tip the balance towards replacing manual management with routine use of serum or plasma indices for assessing sample quality. With an adaptation of the foremost Marco Tullio Cicerone’s speech, we can provokingly conclude… “visual assessment of sample quality: quo usque tandem?”
Author contributions: All the authors have accepted responsibility for the entire content of this submitted manuscript and approved submission.
Research funding: None declared.
Employment or leadership: None declared.
Honorarium: None declared.
References
1. Lippi G, Giavarina D, Gelati M, Salvagno GL. Reference range of hemolysis index in serum and lithium-heparin plasma measured with two analytical platforms in a population of unselected outpatients. Clin Chim Acta 2014;429:143–6.10.1016/j.cca.2013.12.010Search in Google Scholar PubMed
2. Cadamuro J, Mrazek C, Haschke-Becher E, Sandberg S. To report or not to report: a proposal on how to deal with altered test results in hemolytic samples. Clin Chem Lab Med 2017;55:1109–11.10.1515/cclm-2016-1064Search in Google Scholar PubMed
3. Lippi G, Cervellin G, Plebani M. Reporting altered test results in hemolyzed samples: is the cure worse than the disease? Clin Chem Lab Med 2017;55:1112–4.10.1515/cclm-2017-0011Search in Google Scholar PubMed
4. Lippi G, Plebani M, Di Somma S, Cervellin G. Hemolyzed specimens: a major challenge for emergency departments and clinical laboratories. Crit Rev Clin Lab Sci 2011;48:143–53.10.3109/10408363.2011.600228Search in Google Scholar PubMed
5. Meites S. Letter: reproducibly simulating hemolysis, for evaluating its interference with chemical methods. Clin Chem 1973;19:1319.10.1093/clinchem/19.11.1319aSearch in Google Scholar
6. Cadamuro J, Fiedler GM, Mrazek C, Felder TK, Oberkofler H, Kipman U, et al. In-vitro hemolysis and its financial impact using different blood collection systems. J Lab Med 2016;40:49–55.10.1515/labmed-2015-0078Search in Google Scholar
7. Cadamuro J, von Meyer A, Wiedemann H, Klaus Felder T, Moser F, Kipman U, et al. Hemolysis rates in blood samples: differences between blood collected by clinicians and nurses and the effect of phlebotomy training. Clin Chem Lab Med 2016;54:1987–92.10.1515/cclm-2016-0175Search in Google Scholar PubMed
8. Li L, Vecellio E, Gay S, Lake R, Mackay M, Burnett L, et al. Making sense of a haemolysis monitoring and reporting system: a nationwide longitudinal multimethod study of 68 Australian laboratory participant organisations. Clin Chem Lab Med 2018;56:565–73.10.1515/cclm-2017-0056Search in Google Scholar PubMed
9. Sciacovelli L, Panteghini M, Lippi G, Sumarac Z, Cadamuro J, Galoro CA, et al. Defining a roadmap for harmonizing quality indicators in Laboratory Medicine: a consensus statement on behalf of the IFCC Working Group “Laboratory Error and Patient Safety” and EFLM Task and Finish Group “Performance specifications for the extra-analytical phases”. Clin Chem Lab Med 2017;55:1478–88.10.1515/cclm-2017-0412Search in Google Scholar PubMed
10. Luksic AH, Gabaj NN, Miler M, Dukic L, Bakliza A, Simundic AM. Visual assessment of hemolysis affects patient safety. Clin Chem Lab Med. 2018;56:574–81.10.1515/cclm-2017-0532Search in Google Scholar PubMed
11. Price TD. Sensory drive, color, and color vision. Am Nat 2017;190:157–70.10.1086/692535Search in Google Scholar PubMed
12. Neitz J, Neitz M. The genetics of normal and defective color vision. Vision Res 2011;51:633–51.10.1016/j.visres.2010.12.002Search in Google Scholar PubMed PubMed Central
13. Simundic AM, Nikolac N, Ivankovic V, Ferenec-Ruzic D, Magdic B, Kvaternik M, et al. Comparison of visual vs. automated detection of lipemic, icteric and hemolyzed specimens: can we rely on a human eye? Clin Chem Lab Med 2009;47:1361–5.10.1515/CCLM.2009.306Search in Google Scholar PubMed
14. McCaughey EJ, Vecellio E, Lake R, Li L, Burnett L, Chesher D, et al. Current methods of haemolysis detection and reporting as a source of risk to patient safety: a narrative review. Clin Biochem Rev 2016;37:143–51.Search in Google Scholar
15. Lippi G. Systematic assessment of the hemolysis index: pros and cons. Adv Clin Chem 2015;71:157–70.10.1016/bs.acc.2015.05.002Search in Google Scholar PubMed
16. Ceriotti F, Fernandez-Calle P, Klee GG, Nordin G, Sandberg S, Streichert T, et al. Criteria for assigning laboratory measurands to models for analytical performance specifications defined in the 1st EFLM Strategic Conference. Clin Chem Lab Med 2017;55:189–94.10.1515/cclm-2017-0772Search in Google Scholar PubMed
17. Nikolac N, Celap I, Filipi P, Hemar M, Kocijancic M, Miler M, et al. Croatian laboratories have a good knowledge of the proper detection and management of hemolyzed, icteric and lipemic samples. Clin Chem Lab Med 2016;54:419–25.10.1515/cclm-2015-0650Search in Google Scholar PubMed
18. Lippi G, Avanzini P, Campioli D, Da Rin G, Dipalo M, Aloe R, et al. Systematical assessment of serum indices does not impair efficiency of clinical chemistry testing: a multicenter study. Clin Biochem 2013;46:1281–4.10.1016/j.clinbiochem.2013.06.007Search in Google Scholar PubMed
©2018 Walter de Gruyter GmbH, Berlin/Boston
Articles in the same Issue
- Frontmatter
- Editorial
- Visual assessment of sample quality: quo usque tandem?
- Reviews
- Machine learning in laboratory medicine: waiting for the flood?
- Is irisin the new player in exercise-induced adaptations or not? A 2017 update
- Opinion Paper
- Can a combination of average of normals and “real time” External Quality Assurance replace Internal Quality Control?
- Genetics and Molecular Diagnostics
- The UGT1A1*28 gene variant predicts long-term mortality in patients undergoing coronary angiography
- General Clinical Chemistry and Laboratory Medicine
- Laboratory performance of sweat conductivity for the screening of cystic fibrosis
- Making sense of a haemolysis monitoring and reporting system: a nationwide longitudinal multimethod study of 68 Australian laboratory participant organisations
- Visual assessment of hemolysis affects patient safety
- Strong impact on plasma protein profiles by precentrifugation delay but not by repeated freeze-thaw cycles, as analyzed using multiplex proximity extension assays
- Validation of the Six Sigma Z-score for the quality assessment of clinical laboratory timeliness
- Proficiency testing program for hemoglobin E, A2 and F analysis in Thailand using lyophilized hemoglobin control materials
- Application of κ free light chains in cerebrospinal fluid as a biomarker in multiple sclerosis diagnosis: development of a diagnosis algorithm
- Antiphosphatidylserine/prothrombin antibodies (aPS/PT) as potential diagnostic markers and risk predictors of venous thrombosis and obstetric complications in antiphospholipid syndrome
- An evaluation of the SENTiFIT 270 analyser for quantitation of faecal haemoglobin in the investigation of patients with suspected colorectal cancer
- Evaluation of the Aptima HBV Quant assay vs. the COBAS TaqMan HBV test using the high pure system for the quantitation of HBV DNA in plasma and serum samples
- Reference Values and Biological Variations
- Reference intervals for stone risk factors in 24-h urine among healthy adults of the Han population in China
- Cardiovascular Diseases
- Rule-out of non-ST elevation myocardial infarction by five point of care cardiac troponin assays according to the 0 h/3 h algorithm of the European Society of Cardiology
- Infectious Diseases
- Diagnostic and prognostic value of presepsin vs. established biomarkers in critically ill patients with sepsis or systemic inflammatory response syndrome
- Association of adrenal hormone metabolites and mortality over a 6-year follow-up in COPD patients with acute exacerbation
- Corrigendum
- Corrigendum to: Validation of a pneumatic tube system to transport surgical pathology biopsy samples
- Letters to the Editor
- A transnational collaborative network dedicated to the study and applications of the vascular endothelial growth factor-A in medical practice: the VEGF Consortium
- Detection and a functional characterization of the novel FBN1 intronic mutation underlying Marfan syndrome: case presentation
- Effect of haemolysis on the determination of CCL17/thymus and activation-regulated chemokine (TARC) and CCL22/macrophage-derived chemokine (MDC)
- Evaluation of long-term stability of cannabinoids in standardized preparations of cannabis flowering tops and cannabis oil by ultra-high-performance liquid chromatography tandem mass spectrometry
- Impact of citrated blood collection tubes on red cell morphology: implications for the measurement of plasma glucose
- Validation of a pneumatic tube system to transport surgical pathology biopsy samples
- Antioxidant capacity in patients with type 2 diabetes: a preliminary investigation on gender-specific differences in an Italian population
Articles in the same Issue
- Frontmatter
- Editorial
- Visual assessment of sample quality: quo usque tandem?
- Reviews
- Machine learning in laboratory medicine: waiting for the flood?
- Is irisin the new player in exercise-induced adaptations or not? A 2017 update
- Opinion Paper
- Can a combination of average of normals and “real time” External Quality Assurance replace Internal Quality Control?
- Genetics and Molecular Diagnostics
- The UGT1A1*28 gene variant predicts long-term mortality in patients undergoing coronary angiography
- General Clinical Chemistry and Laboratory Medicine
- Laboratory performance of sweat conductivity for the screening of cystic fibrosis
- Making sense of a haemolysis monitoring and reporting system: a nationwide longitudinal multimethod study of 68 Australian laboratory participant organisations
- Visual assessment of hemolysis affects patient safety
- Strong impact on plasma protein profiles by precentrifugation delay but not by repeated freeze-thaw cycles, as analyzed using multiplex proximity extension assays
- Validation of the Six Sigma Z-score for the quality assessment of clinical laboratory timeliness
- Proficiency testing program for hemoglobin E, A2 and F analysis in Thailand using lyophilized hemoglobin control materials
- Application of κ free light chains in cerebrospinal fluid as a biomarker in multiple sclerosis diagnosis: development of a diagnosis algorithm
- Antiphosphatidylserine/prothrombin antibodies (aPS/PT) as potential diagnostic markers and risk predictors of venous thrombosis and obstetric complications in antiphospholipid syndrome
- An evaluation of the SENTiFIT 270 analyser for quantitation of faecal haemoglobin in the investigation of patients with suspected colorectal cancer
- Evaluation of the Aptima HBV Quant assay vs. the COBAS TaqMan HBV test using the high pure system for the quantitation of HBV DNA in plasma and serum samples
- Reference Values and Biological Variations
- Reference intervals for stone risk factors in 24-h urine among healthy adults of the Han population in China
- Cardiovascular Diseases
- Rule-out of non-ST elevation myocardial infarction by five point of care cardiac troponin assays according to the 0 h/3 h algorithm of the European Society of Cardiology
- Infectious Diseases
- Diagnostic and prognostic value of presepsin vs. established biomarkers in critically ill patients with sepsis or systemic inflammatory response syndrome
- Association of adrenal hormone metabolites and mortality over a 6-year follow-up in COPD patients with acute exacerbation
- Corrigendum
- Corrigendum to: Validation of a pneumatic tube system to transport surgical pathology biopsy samples
- Letters to the Editor
- A transnational collaborative network dedicated to the study and applications of the vascular endothelial growth factor-A in medical practice: the VEGF Consortium
- Detection and a functional characterization of the novel FBN1 intronic mutation underlying Marfan syndrome: case presentation
- Effect of haemolysis on the determination of CCL17/thymus and activation-regulated chemokine (TARC) and CCL22/macrophage-derived chemokine (MDC)
- Evaluation of long-term stability of cannabinoids in standardized preparations of cannabis flowering tops and cannabis oil by ultra-high-performance liquid chromatography tandem mass spectrometry
- Impact of citrated blood collection tubes on red cell morphology: implications for the measurement of plasma glucose
- Validation of a pneumatic tube system to transport surgical pathology biopsy samples
- Antioxidant capacity in patients with type 2 diabetes: a preliminary investigation on gender-specific differences in an Italian population

