Abstract
Background
Pain after surgery is not uncommon with 30% of patients reporting moderate to severe postoperative pain. Early identification of patients prone to postoperative pain may be a step forward towards individualized pain medicine providing a basis for improved clinical management through treatment strategies targeting relevant pain mechanisms in each patient. Assessment of pain processing by quantitative sensory testing (QST) prior to surgery has been proposed as a method to identify patients at risk for postoperative pain, although results have been conflicting. Since the last systematic review, several studies investigating the association between postoperative pain and more dynamic measures of pain processing like temporal summation of pain and conditioned pain modulation have been conducted.
Objectives
According to the PRISMA guidelines, the aim of this systematic review was to evaluate whether assessment of experimental pain processing including measures of central pain mechanisms prior to surgery was associated with pain intensity after surgery.
Methods
Systematic database searches in PubMed and EMBASE with the following search components: QST, association, and postoperative pain, for studies that assessed the association between QST and pain after surgery were performed. Two authors independently reviewed all titles and abstracts to assess their relevance for inclusion. Studies were included if (1) QST was performed prior to surgery, (2) pain was assessed after surgery, and (3) the association between QST and pain after surgery was investigated. Forty-four unique studies were identified, with 30 studies on 2738 subjects meeting inclusion criteria. The methodological quality of the include studies was assessed and data extraction included study population, type of surgery, QST variables, clinical pain outcome measure and main result.
Results
Most studies showed moderate to high risk of bias. Type of surgery investigated include 7 studies on total knee replacement, 5 studies on caesarean section, 4 studies on thoracic surgery, 2 studies on herniotomy, 2 studies on hysterectomy/myomectomy, 1 study on tubal ligation, 1 study on gynecologic laparoscopy, 1 study on arthroscopic knee surgery, 1 study on shoulder surgery, 1 study on disc herniation surgery, 1 study on cholecystectomy,1 study on percutaneous nephrolithotomy,1 study on molar surgery, 1 study on abdominal surgery, and 1 study on total knee replacement and total hip replacement. The majority of the preoperative QST variables showed no consistent association with pain intensity after surgery. Thermal heat pain above the pain threshold and temporal summation of pressure pain were the QST variables, which showed the most consistent association with acute or chronic pain after surgery.
Conclusions
QST before surgery does not consistently predict pain after surgery. High quality studies investigating the presence of different QST variables in combination or along with other pain-related psychosocial factors are warranted to confirm the clinical relevance of QST prior to surgery.
Implications
Although preoperative QST does not show consistent results, future studies in this area should include assessment of central pain mechanisms like temporal summation of pressure pain, conditioned pain modulation, and responses to pain above the pain threshold since these variables show promising associations to pain after surgery.
1 Introduction
Pain after surgery is not uncommon and 30% of patients experience moderate to severe postoperative pain [1,2]. High postoperative pain intensity has consistently been associated with an increasing risk of chronic pain [3,4,5], and 10–50% of patients with acute postoperative pain develop chronic pain [6]. Early identification of patients prone to severe postoperative pain may be a step forward towards individualized pain medicine providing a basis for improved clinical management of postoperative pain through improved preemptive analgesia strategies targeting relevant pain mechanisms in each patient or by reducing the number of surgeries causing more pain than relief.
Assessment of pain processing by quantitative sensory testing (QST) prior to surgery has been proposed as a method to identify patients at risk [7,8,9,10]. QST is a psychophysical method using standardized mechanical, electrical, and thermal stimuli to assess sensory and pain perception [11]. Several different aspects of perception can be assessed for each modality including detection threshold, pain threshold, pain intensity, and pain tolerance. Moreover, central pain processing in humans can reliably be assessed by measures of temporal summation of pain (TSP) [12] and conditioned pain modulation (CPM) [13].
The association between postoperative pain and pain processing assessed before surgery has previously been investigated by 3 systematic reviews [14,15,16] with the latest systematic review including 15 studies published in 2011 [14]. Although some QST variables showed some consistency with postoperative pain, the authors concluded that more research including other QST variables was required to establish whether a correlation between preoperative pain processing and postoperative pain truly does exist. Since the last systematic review, a series of studies investigating the association between postoperative pain and pain processing have been published and several studies have demonstrated an association between postoperative pain and measures of more central pain processing [9,17,18]. Preoperative assessment of temporal summation predicted postoperative chronic pain after total knee replacement surgery [9], and less efficient CPM assessed before surgery predicted chronic pain in patients after thoracotomy [7] and abdominal surgery [19].
Thus the primary aim of this systematic review was to investigate the association between postoperative pain and preoperative assessment of experimental pain processing including measures of central pain mechanisms. The findings and the implications for use of QST to identify patients at-risk for postoperative pain as well as the implications for future research in this area will be discussed.
2 Methods
According to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [20], this systematic review investigated the association between preoperative pain processing and pain intensity after surgery.
2.1 Search strategy
In October 2016, we searched PubMed and EMBASE for original articles investigating the association between preoperative pain processing and pain after surgery. A collaborate search strategy with the following search components: QST, association, and postoperative pain were used to increase the search sensitivity (Table 1). Moreover, reference lists from included studies and previous systematic reviews were screened by hand and experts within the field were consulted.
Search strategy.
| Components | Synonyms |
|---|---|
| QST | Quantitative sensory testing, heat pain sensitivity, heat detection threshold, heat pain threshold, heat pain tolerance, cold pain sensitivity, cold detection threshold, cold pain threshold, cold pain tolerance, pressure pain sensitivity, pressure pain threshold, pressure pain tolerance, electrical pain sensitivity, electrical pain threshold, electrical pain tolerance, CPM, conditioned pain modulation, temporal summation of pain, windup |
| Association | Associated, correlation, predictor, predict, predictive |
| Postoperative Pain | Pain after surgery, postsurgical pain, surgery [MeSH], pain after operation |
2.2 Inclusion and selection criteria
Two authors (A.S and C.S) independently reviewed all titles and abstracts to assess their relevance for inclusion. Studies were included if (1) QST was performed prior to surgery, (2) pain was assessed after surgery, and (3) the association between QST and pain after surgery was investigated. The full text articles were retrieved for studies fulfilling all 3 criteria, and duplicates were removed. The 2 authors then assessed all full texts for final inclusion. Disagreement was resolved by consensus or by consulting the third investigator (H.B.V).
2.3 Data extraction, assessment and analysis
From the included studies, bibliographic data such as authors, year of publication and journal were registered and the following data was extracted independently by 2 reviewers (A.S and C.S): study population, QST variables and assessment sites, time of QST, type of surgery, method and time for assessment of pain intensity, statistical methods, main findings, and effect sizes (Table 2). For estimation of effect sizes, the correlation coefficient was converted to the Fisher’s z scale and Cohen’s d was calculated [21]. Effects sizes were evaluated as small (d = 0.20), medium (d = 0.50), and large (d = 0.80). After individual data extraction, discussion and agreement was made. If disagreement still existed between the 2 reviewers, the third investigator (H.B.V) was consulted. The methodological quality of the included studies was assessed independently by 2 reviewers (A.S and C.S) using the criteria by Hayden et al., which assesses bias in studies of prognostic factors [22]. A checklist for each prognostic criteria was made, and the risk of bias were graded as low, moderate or high (Table 3). Given the substantial clinical heterogeneity in the individual studies, we decided that a meta-analysis would be inappropriate and instead focused on the narrative interpretation of the results.
Correlations between QST and pain intensity after surgery. Age of the study population is presented as mean ± standard deviation or median (range). CDT, cold detection threshold; CPT, cold pain threshold; CPTol, cold pain tolerance; CPM, conditioned pain modulation; EDT, electrical detection threshold; EPT, electrical pain threshold; EPTol, electrical pain tolerance; HPT, heat pain threshold; PPT, pressure pain threshold; PPTol, pressure pain tolerance; STCPI, suprathreshold cold pain intensity; STHPI, suprathreshold heat pain intensity; STPPI, suprathreshold pressure pain intensity; TSP, temporal summation of pain; WDT, warm detection threshold; NA, data not presented in study; (U), univariate analysis; (M), multivariate analysis.
| Reference | Study population Number (F/M) Age | Type of surgery | QST parameter | Clinical pain outcome (type and timing) | Statistical methods | Main findings (QST parameter associated with pain after surgery) | Effect size (Cohen’s d) |
|---|---|---|---|---|---|---|---|
| Grosen et al. [17] | 42 (0/42) 19 (17–23) | Thoracic surgery | PPT, CPM | NRS (acute and chronic) | Univariate analysis Multivariate regression model | No significant associations | – |
| Weissman-Fogel et al. [8] | 84 (35/49) 62 ±13 | Thoracic surgery | HPT, STHPI, TSP (heat), PPT, STPPI, TSP (pressure) | NRS (acute) | Univariate analysis Multivariate regression model | HPT (r = −0.24) (U) STHPI (r = 0.23) (U) STPPI (r = 0.25) (M) TSP (pressure) (r =0.23) (M) | 0.50 0.48 0.53 0.48 |
| Lautenbacher et al. [25] | 54 (0/54) 19 ±4 | Thoracic surgery | CPT, HPT, TSP (heat), PPT | NRS (acute) | Multivariate regression model | No significant associations | – |
| Yarnitsky et al. [7] | 62 (24/38) 62 ± 14 | Thoracic surgery | HPT, STHPI, CPM | NRS (acute and chronic) | Univariate analysis Multivariate regression model | CPM and chronic pain (r = −0.37) (U) | 0.84 |
| Buhagiar et al. [26] | 65 (65/0) 30 ± 5 | Caesarean section | EPT, PPT, PPTol | NRS (acute) | Univariate analysis Multivariate regression model | EPT (r = −0.26) (U) PPTol (r = −0.21) (U) | 0.55 0.44 |
| Pan et al. [34] | 34 (34/0) NA | Caesarean section | WDT, HPT, HPI | VAS (acute) | Univariate analysis Multivariate regression model | HPT (r = −0.44) (M) | 1.07 |
| Nielsen et al. [27] | 39 (39/0) 35 (32–37) | Caesarean section | EDT, EPT | VAS (acute) | Univariate analysis | EPT (r = −0.65) (U) | 2.46 |
| Strulov et al. [28] | 47 (47/0) 33 ± 5 | Caesarean section | HPT, STHPI | VAS (acute) | Univariate analysis Multivariate regression model | STHPI (r = 0.41) (M) | 0.97 |
| Granot et al. [10] | 58 (58/0) NA | Caesarean section | HPT, STHPI | VAS (acute) | Univariate analysis | STHPI (r = 0.53) (U) | 1.46 |
| Hsu et al. [23] | 40 (40/0) 41 ± 6 | Hysterectomy/ myomectomy | PPT, PPTol | VAS (acute) | Univariate analysis Multivariate regression model | PPTol (r = −0.52) (M) | 1.41 |
| Ahmad et al. [41] | 120 (120/0) 42 (38–48) | Hysterectomy/ myomectomy | CDT, CPT, WDT, HPT | NRS (acute) | Univariate analysis | No significant associations | – |
| Rudin et al. [42] | 59 (59/0) 38 (35–41) | Tubal ligation | WDT, HPT, STHPI | VAS (acute) | Univariate analysis Multivariate regression model | No significant associations | – |
| Jarrell et al. [43] | 61 (61/0) 33 ± 5 | Gynecologic laparoscopy | PPT, allodynia | NRS (chronic) | Multivariate regression model | Allodynia (r = −0.32) (M) | 0.70 |
| Martinez et al. [29] | 20 (19/1) 69 ± 2 | Total knee replacement | CPT, STCPI, HPT, STHPI, PPT | VAS (acute and chronic) | Univariate analysis | No significant associations | – |
| Petersen et al. [9] | 78 (46/32) (47–86) | Total knee replacement | PPT, TSP (pressure), CPM | VAS (chronic) | Univariate analysis Multivariate regression model | TSP (pressure) (r = 0.24) (U) | 0.50 |
| Lunn et al. [35] | 97 (50/47) 66 (60–73) | Total knee replacement | STHPI | VAS (acute) | Univariate analysis Multivariate regression model | STHPI (r = 0.25) (U) | 0.53 |
| Wylde et al. [40] | TKR: 239 (125/114) 69 ± 8 | Total knee replacement | PPT | VAS (chronic) | Univariate analysis Multivariate regression model | PPT (r = −0.11) (M) | 0.22 |
| THR: 254 (149/105) 67 ± 10 | Total hip replacement | Univariate analysis Multivariate regression model | |||||
| Vaegter et al. [39] | 14 (7/7) 66 ± 6 | Total knee replacement | CPM | NRS (chronic) | Univariate analysis | CPM (r = −0.57) (U) | 1.70 |
| Thomazeau et al. [33] | 109 (78/31) 69 ± 9 | Total knee replacement | EPT | NRS (acute) | Univariate analysis Multivariate regression model | No significant association | – |
| Petersen et al. [45] | 103 (66/27) 69 ± 2 | Total knee replacement | PPT, PPTol, CPM, TSP (pressure) | VAS (chronic) | Univariate analysis Multivariate regression model | PPT (r = −0.22) (M) Patients with a combination of impaired CPM and facilitated TSP had less pain relief | 0.46 |
| Lundblad et al. [30] | 69 (35/34) 68(40–80) | Total knee replacement | EDT, EPT | VAS (chronic) | Multivariate regression model | EDT (r = −0.46) (M) EPT (r = −0.52) (M) | 1.15 1.41 |
| Werner et al. [36] | 20 (6/14) | Knee arthroscopy | HPT, PPT, STPPI | VAS (acute) | Univariate analysis | No significant associations | – |
| Aasvang et al. [38] | 162 (0/162) 59(21–85) | Herniotomy | EDT, EPT | NRS (acute) | Univariate analysis | No significant associations | – |
| Aasvang et al. [37] | 442 (0/442) 55 ±13 | Herniotomy | WDT, HPT, STHPI | NRS (acute) | Univariate analysis | STHPI (r = 0.26) (U) | 0.55 |
| Valencia et al. [18] | 73 (20/53) 45 ± 19 | Shoulder surgery | HPT, STHPI, CPM | NRS (chronic) | Univariate analysis Multivariate regression model | No significant associations | – |
| Wilder-Smith et al. [44] | 41 (10/31) (21–64) | Disc herniation surgery | EDT, EPT, EPTol | NRS (acute) | Univariate analysis | No significant associations | – |
| Bisgaard et al. [31] | 150 (129/21) 41 (20–79) | Cholecystectomy | CPTol | VAS (acute) | Univariate analysis Multivariate regression model | CPTol (r = −0.30) (U) | 0.65 |
| Pedersen et al. [32] | 44 (19/25) 56 (48–66) | Percutaneous nephrolithotomy | EPT, TSP (electrical), PPTol | NRS (acute) | Univariate analysis | No significant associations | – |
| Rudin et al. [24] | 38 (23/15) 30 (25–38) | Molar surgery | WDT, HPT, STHPI | VAS (acute) | Multivariate regression model | STHPI (r = 0.36) (M) | 0.81 |
| Wilder-Smith et al. [19] | 20 (13/7) 53 (47–59) | Abdominal surgery | EPTol, PPTol, CPM | VAS (acute and chronic) | Univariate analysis | CPM (r = −0.68) (U) | 2.97 |
Risk of bias assessment of the 30 studies included in this systematic review. The 6 factors assessed for bias were: Study participation, study attribution, prognostic factor measurement, outcome measurement, study confounding, and statistical analysis [21].
| Reference | Study participation | Study attrition | Prognostic factor measurement | Outcome measurement | Study confounding | Statistical analysis |
|---|---|---|---|---|---|---|
| Grosen et al. [17] | Low risk | Moderate risk | Low risk | Low risk | Low risk | Low risk |
| Weissman-Fogel et al.[8] | Moderate risk | Low risk | Low risk | Low risk | Moderate risk | Low risk |
| Lautenbacher et al. [25] | Low risk | Low risk | Low risk | Moderate risk | Moderate risk | Low risk |
| Yarnitsky et al. [7] | Low risk | Low risk | Low risk | Moderate risk | Low risk | Moderate risk |
| Buhagiar et al. [26] | Moderate risk | Low risk | Moderate risk | Low risk | Moderate risk | Low risk |
| Pan et al. [34] | Moderate risk | Low risk | Moderate risk | Low risk | Moderate risk | Low risk |
| Nielsen et al. [27] | Low risk | Moderate risk | Low risk | Moderate risk | Moderate risk | Low risk |
| Strulov et al. [28] | Moderate risk | Low risk | Low risk | Low risk | Moderate risk | Low risk |
| Granot et al. [10] | High risk | Low risk | Low risk | Low risk | Moderate risk | Low risk |
| Hsu et al. [23] | Moderate risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Ahmad et al. [41] | Moderate risk | Low risk | Moderate risk | Low risk | Moderate risk | Low risk |
| Rudin et al. [42] | Moderate risk | High risk | Moderate risk | Moderate risk | Moderate risk | Moderate risk |
| Jarrell et al. [43] | High risk | Moderate risk | Moderate risk | Moderate risk | High risk | Low risk |
| Martinez et al. [29] | Moderate risk | Low risk | Low risk | Low risk | Moderate risk | Low risk |
| Petersen et al. [9] | Moderate risk | Low risk | Moderate risk | Moderate risk | Moderate risk | Low risk |
| Lunn et al. [35] | Low risk | Moderate risk | Low risk | Low risk | Low risk | Low risk |
| Wylde et al. [40] | Low risk | Moderate risk | Moderate risk | Moderate risk | Moderate risk | Low risk |
| Vaegter et al. [39] | Low risk | Low risk | Moderate risk | Low risk | Moderate risk | Low risk |
| Thomazeau et al. [33] | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Petersen et al. [45] | Low risk | Moderate risk | Moderate risk | Low risk | Moderate risk | Low risk |
| Lundblad et al. [30] | Moderate risk | Moderate risk | Low risk | Moderate risk | Moderate risk | Low risk |
| Werner et al. [36] | Moderate risk | Low risk | Low risk | Low risk | Moderate risk | Low risk |
| Aasvang et al. [38] | Low risk | Low risk | Low risk | Moderate risk | Moderate risk | Low risk |
| Aasvang et al. [37] | Moderate risk | Low risk | Low risk | Moderate risk | Moderate risk | Low risk |
| Valencia et al. [18] | Low risk | Moderate risk | Low risk | Low risk | Low risk | Low risk |
| Wilder-Smith et al. [44] | Moderate risk | Moderate risk | Low risk | Low risk | Moderate risk | Low risk |
| Bisgaard et al. [31] | Moderate risk | Moderate risk | Low risk | Low risk | Moderate risk | Low risk |
| Pedersen et al. [32] | Low risk | Low risk | Low risk | Low risk | Moderate risk | Low risk |
| Rudin et al. [24] | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Wilder-Smith et al. [19] | Low risk | Low risk | Low risk | Moderate risk | Moderate risk | Low risk |
3 Results
3.1 Studies included
The literature search identified 436 hits of which 30 studies on a total of 2738 subjects (1377 women and 1351 men) were included in this systematic review (Fig. 1 and Table 2). As illustrated in Table 2 the following surgeries were performed: 7 studies on total knee replacement, 5 studies on caesarean section, 4 studies on thoracic surgery, 2 studies on herniotomy, 2 studies on hysterectomy/myomectomy, 1 study on tubal ligation, 1 study on gynecologic laparoscopy, 1 study on arthroscopic knee surgery, 1 study on shoulder surgery, 1 study on disc herniation surgery, 1 study on cholecystectomy, 1 study on percutaneous nephrolithotomy, 1 study on molar surgery, 1 study on abdominal surgery, and 1 study on total knee replacement and total hip replacement. The timing of the preoperative sensory testing varied widely among the studies. Sensory testing was done on the day of surgery [19,23,24], 1–3 days before surgery [7,8,10,17,18,19,25,26,27,28,29,30,31,32,33], and 4 days to 4 weeks before surgery [34,35,36,37,38,39]. Time of preoperative QST was not mentioned in 7 studies [9,40,41,42,43,44,45]. Pain intensity after surgery was assessed with Visual Analogue Scale (VAS) or Numerical Rating Scale (NRS). Acute postoperative pain was assessed in 23 studies with an interval of assessment from immediately after surgery up to 30 days after surgery. Chronic postoperative pain was assessed in 11 studies with an interval of assessment from 3 to 18 months after surgery. Four studies assessed both acute and chronic pain.
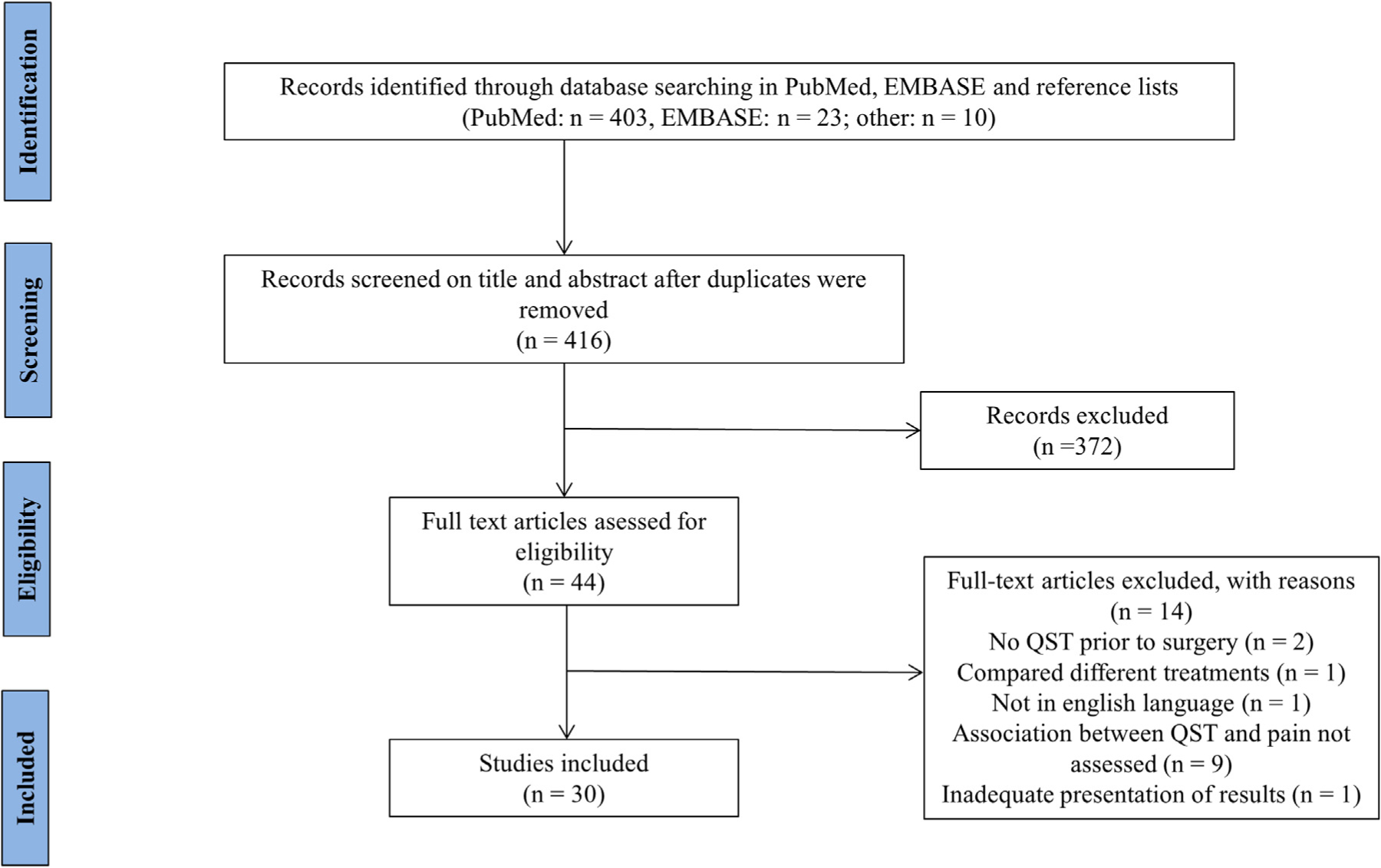
Preferred Reporting Items for Systematic Reviews and Meta Analyses (PRISMA) flow diagram.
3.2 QST variables
3.2.1 Thermal sensory testing
3.2.1.1 Warm detection threshold (WDT)
Warm detection threshold was assessed in 3 studies (Table 2). None of the studies (tubal ligation [42], herniotomy [37], and molar surgery [24]) demonstrated a significant association with acute pain intensity after surgery.
3.2.1.2 Heat pain threshold (HPT)
Heat pain threshold was assessed in 13 studies (Table 2). HPT was negatively associated with acute pain intensity after thoracic surgery [8], and caesarean section [34] suggesting that a lower threshold to heat pain prior to surgery was associated with higher acute pain intensity after surgery. Eleven studies (caesarean section [10,28], hysterectomy/myomectomy [41], tubal ligation [42], total knee replacement [29], knee arthroscopy [36], herniotomy [37], shoulder surgery [18], and molar surgery [24]) demonstrated no significant association between HPT and acute or chronic pain intensity.
3.2.1.3 Suprathreshold heat pain intensity (STHPI)
Suprathreshold heat pain intensity was assessed in 12 studies (Table 2). STHPI was positively associated with acute pain intensity after thoracic surgery [8], caesarean section [10,28], total knee replacement [35], herniotomy [37], and molar surgery [24] indicating that a higher pain intensity to a supra-threshold heat stimuli prior to surgery was associated with higher acute pain intensity after surgery. Five studies (thoracic surgery [7], caesarean section [34], tubal ligation [42], total knee replacement [29], and shoulder surgery [18]) demonstrated no significant associations between STHPI and acute or chronic pain intensity.
3.2.1.4 Cold detection threshold (CDT)
Cold detection threshold was assessed in 1 study prior to hysterectomy/myomectomy [41]. The study did not demonstrate a significant association between CDT and acute pain intensity.
3.2.1.5 Cold pain threshold (CPT)
Cold pain threshold was assessed in 3 studies (Table 2). None of the studies (thoracic surgery [25], hysterectomy/myomectomy [41], and total knee replacement [29]) demonstrated significant associations between CPT and acute or chronic pain intensity.
3.2.1.6 Suprathreshold cold pain intensity (STCPI)
Suprathreshold cold pain intensity was assessed in 1 study prior to total knee replacement surgery [29]. No significant association between STCPI and acute or chronic pain intensity were found.
3.2.1.7 Cold pain tolerance (CPTol)
Cold pain tolerance was assessed in 1 study prior to cholecystectomy [31]. A significant negative association with acute pain intensity was found, indicating that a lower pain tolerance to cold stimuli prior to surgery was associated with higher acute pain intensity after surgery.
3.2.2 Electrical sensory testing
3.2.2.1 Electrical detection threshold (EDT)
Electrical detection threshold was assessed in 4 studies (Table 2). EDT was negatively associated with chronic pain intensity after total knee replacement [30], indicating that a lower electrical detection threshold prior to surgery was associated with higher chronic pain intensity. Studies on caesarean section [27], herniotomy [38] and disc herniation surgery [44] demonstrated no significant associations between EDT and acute pain intensity.
3.2.2.2 Electrical pain threshold (EPT)
Electrical pain threshold was assessed in 7 studies (Table 2). Two studies on caesarean section [26,27], and 1 study on total knee replacement [30] demonstrated significant negative associations with acute pain intensity and chronic pain intensity respectively, indicating that a lower pain threshold to electrical stimuli prior to surgery was associated with higher pain intensity after surgery. Four studies (herniotomy [38], disc herniation surgery [44], total knee replacement [33], and percutaneous nephrolithotomy [32]) demonstrated no significant associations between EPT and acute pain intensity.
3.2.2.3 Electrical pain tolerance (EPTol)
Electrical pain tolerance was assessed in 2 studies (Table 2). No significant associations were found between EPTol and acute or chronic pain intensity after disc herniation surgery [44] or abdominal surgery [19].
3.2.3 Mechanical sensory testing
3.2.3.1 Pressure pain threshold (PPT)
Pressure pain threshold was assessed in 11 studies (Table 2). Significant negative associations between PPT and acute pain intensity after total knee and total hip replacement surgery [40], and between PPT assessed with cuff algometry and pain relief 12 months after total knee replacement surgery [45] were found indicating that a lower pain threshold to pressure prior to surgery was associated with higher acute pain intensity after surgery and less pain relief 12 months after. Nine studies (thoracic surgery [17], caesarean section [26], hysterectomy [23], gynecologic laparoscopy [43], arthroscopic knee surgery [36], and total knee replacement [29]) demonstrated no associations between PPT and acute or chronic pain intensity.
3.2.3.2 Suprathreshold pressure pain intensity (STPPI)
Suprathreshold pressure pain intensity was assessed in 2 studies (Table 2). No significant associations were found between STPPI and acute pain intensity after knee arthroscopy [36] or thoracic surgery [8].
3.2.3.3 Pressure pain tolerance (PPTol)
Pressure pain tolerance was assessed in 5 studies (Table 2). Significant negative associations with acute pain intensity after caesarean section [26] and hysterectomy/myomectomy surgery [41] were demonstrated suggesting that a lower pain tolerance to pressure prior to surgery was associated with higher pain intensity after surgery. Three studies (percutaneous nephrolithotomy [32], total knee replacement [45], and abdominal surgery [19]) demonstrated no significant associations between PPTol and acute or chronic pain intensity.
3.2.4 Temporal summation of pain (TSP)
Temporal summation of pain was assessed in 5 studies (Table 2). Three studies assessed temporal summation of pressure pain (procedure: NRS scores during 10 repeated Von Frey Filaments 225.1-g stimulations, between stimulation intervals unknown) [8], (procedure: NRS scores during 10 repeated Von Frey Filaments 25.6 g, 1 s between stimulation intervals) [9], (procedure: Electronic VAS scores during 10 repeated computer controlled cuff stimulations with an intensity at the average of the cuff pressure pain threshold and tolerance, 1 s stimulations and 1 s between stimulation intervals) [45], 1 study assessed temporal summation to electrical pain (procedure: NRS scores during 5 repeated stimuli (each stimulus was a train of 5 pulses at 200 Hz) at 2 Hz) [32], and 1 study assessed temporal summation to heat pain (procedure: NRS scores during 15 repeated heat stimuli at pain-60 level, 0.7 s stimulations and 2 s between stimulation intervals) [8]. Temporal summation of pressure pain was negatively associated with acute and chronic pain intensity after thoracic surgery [8], and chronic pain after total knee replacement [9] respectively, indicating that higher degree of temporal summation of mechanical pain prior to surgery is associated with higher pain intensity after surgery. Temporal summation to electrical [32] and heat pain [8] respectively, were not associated with acute pain intensity after percutaneous nephrolithotomy and thoracic surgery.
3.2.5 Conditioned pain modulation (CPM)
Conditioned pain modulation was assessed in 7 studies (Table 2). Five studies used the cold pressor test (procedure: PPT at the knee assessed before and after hand immersion in 2 °C water, maximum duration 2min) [9], (procedure: PPT at the thigh assessed before and after hand immersion in 1 °C water, maximum duration 2 min) [17], (procedure: suprathreshold heat pain intensity at the thenar eminence assessed before and 1 min after hand immersion in 8 °C water, maximum duration 1 min) [18], (procedure: electrical pain threshold and tolerance at the leg assessed before and within 1 min after hand immersion in 1 °C water, maximum duration 3 min) [19], (procedure: PPT at the legs, arm and shoulder assessed before and during hand immersion (after 1 min) in 2°C water) [39], 1 study used cuff algometry (procedure: cuff pressure pain threshold at the lower leg assessed before and during tonic painful cuff pressure on the opposite leg, intensity 30–60 kPa) [45], and 1 study used hot water (procedure: suprathreshold heat pain intensity at the forearm assessed before and during (after 30 s) hand immersion in 46.5 °C water) [7] as the conditioning stimulus. Significant negative associations between CPM and acute and chronic pain intensity after abdominal surgery [19], thoracic surgery [7], and total knee replacement [39] were demonstrated, suggesting that less efficient CPM preoperatively is associated with higher pain intensity after surgery. Four studies (total knee replacement [9,45], shoulder surgery [18], and thoracic surgery [17]) demonstrated no significant associations between CPM and acute or chronic pain intensity.
3.2.6 Cutaneous allodynia
Cutaneous allodynia was assessed in 1 study (Table 2). Allodynia (dynamic test with cotton-tipped applicator on the anterior abdominal wall) prior to gynecologic laparoscopy [43] was associated with higher pain intensity after surgery.
3.3 Quality assessment
Quality assessments of the included studies are presented in Table 3. The reviewers (A.S and C.S) initially agreed on 83% of the ratings. Consensus was reached on all items following discussion.
4 Discussion
This systematic review identified 15 new studies since the last systematic review conducted in 2011 [14]. Nineteen studies demonstrated an association between a preoperative QST variable and pain after surgery, however; no consistent association between any preoperative QST and postoperative pain intensity was found. An important finding in this systematic review was that the response to thermal pain above the pain thresholds as well as the QST variables related with central pain mechanisms like temporal summation of pain, and conditioned pain modulation more frequently demonstrated an association with pain intensity after surgery compared to the QST variables more related to the detection and pain thresholds. The association between the QST variables of central pain mechanisms and post-operative pain has not previously been included in systematic reviews across different surgeries. In agreement with previous systematic reviews [14,16,46], this systematic review indicates that detection thresholds for electrical and thermal stimuli as well as thermal pain thresholds are poor predictors of pain intensity after surgery.
4.1 Associations between QST variables and postoperative pain
Univariate analysis demonstrated a significant association between suprathreshold heat pain intensity (STHPI) and acute pain intensity after surgery; however, when multivariate analyses were performed most studies did not demonstrate significant associations [8,24,35] suggesting that when other potentially predictive factors are taken into consideration, no significant association between STHPI and pain intensity after surgery was demonstrated. A previous systematic review noted that the association between STHPI and pain after surgery were observed mainly in the studies on healthy female patients undergoing elective caesarean section or gynecologic procedures [14]. Since then 4 new studies with only males or mixed gender populations have been conducted on total knee replacement [35], herniotomy [37], shoulder surgery [18], and molar surgery [24]. Three of these studies demonstrated significant associations between STHPI and acute postoperative pain intensity, indicating that the association is also present in males. However, none of the recent published studies on mixed populations investigated whether potential associations were influenced by gender.
Pressure pain threshold (PPT) demonstrated significant negative associations between PPT and acute pain intensity in total knee replacement and between chronic pain intensity in total hip replacement when univariate analyses were performed, and for knee replacement when multivariate analyses were performed. Interestingly, a significant association between PPT and pain intensity after musculoskeletal surgery was found [40,45], but no significant associations were demonstrated for visceral surgeries [8,17,23,25,26,43] indicating that PPT may be valuable in predicting postoperative pain after surgery on the deeper musculoskeletal structures but not on the visceral structures.
Temporal summation of pain (TSP) was assessed in 5 studies. Univariate and multivariate analysis demonstrated significant associations between TSP and acute pain intensity [8], and chronic pain intensity [8,9]. All these studies used temporal summation to pressure pain suggesting that temporal summation to pressure pain may be a promising predictor of pain after surgery.
Conditioned pain modulation (CPM) demonstrated significant associations between CPM and acute and chronic pain intensity after thoracic surgery [7] and abdominal surgery [19], as well as between CPM and pain relief 6 months after total knee replacement [39]. However, no significant associations after shoulder surgery [18] or 12 months after total knee replacement [9,45] were found, suggesting that CPM is associated with the pain intensity after surgery on visceral structures, but not consistently after surgery on musculoskeletal structures. However, a recent study demonstrated that patients with knee osteoarthritis who demonstrated reduced CPM and facilitated temporal summation of pain prior to total knee replacement surgery had less pain relief 12 months after surgery [45] suggesting that different QST variables in combination may have relevance when determining which patients are at risk.
4.2 Quality assessment
Seven of the 30 included studies [17,18,23,24,32,33,35] showed low risk of bias. Among these, only 3 studies demonstrated significant association between QST and pain after surgery in univariate analyses [23,24,35], and only 1 after multivariate analysis [23], which indicate that studies with greater risk of bias tend to demonstrate significant associations, whereas studies with lower risk of bias do not. The 4 main areas for bias in the studies were study participation, study attrition, outcome measurement, and confounding measurement. In study participation inadequate description of the sampling frame, period, and place of recruitment were the main reasons for bias. Bias in study attrition was mainly due to the lack of description of patients lost at follow up. Uncertainty whether researcher was blinded to the results of preoperative testing, was another source of bias. Description of the possible confounding factors was not appropriately accounted for in most studies and multivariate analyses were not performed in the majority of the included studies.
4.3 Implications
The results from this systematic review do not consistently support the use of QST before surgery to identify patients at risk for acute of chronic pain after surgery. Although preoperative QST does not show consistent results, future studies in this area should include assessment of central pain mechanisms like temporal summation of pressure pain, conditioned pain modulation, and responses to pain above the pain threshold since these variables show promising associations to pain after surgery. In addition, 1 QST variable may not be adequate for identifying patients at risk, and a combination of different QST variables, e.g. patients with both facilitated temporal summation of pain and impaired conditioned pain modulation should be further investigated. Furthermore, multivariate analysis including other potential non-QST risk factors for pain after surgery, such as preoperative pain intensity, anxiety, age, and type of surgery should be included [16]. Finally, the body area for QST assessment needs further consideration as some studies assessed QST in painful body areas and others in non-painful body areas. Limitations to this systematic review include search strategies limited to 2 databases, and the lack of quantification of effects through meta-analysis.
5 Conclusion
This systematic review demonstrates that although the association between QST and pain after surgery has been studied extensively no consistent association between variables and pain after surgery exists. The response to thermal pain above the pain thresholds as well as the QST variables related with central pain mechanisms like temporal summation of pain, and conditioned pain modulation more frequently demonstrated an association with pain intensity after surgery compared to the QST variables more related to the detection and pain thresholds.
Highlights
Most studies included in this review showed moderate to high risk of bias.
Most QST variables showed no consistent correlations with pain after surgery.
Responses to pain above the pain threshold showed more consistent correlations.
DOI of refers to article: http://dx.doi.org/10.1016/j.sjpain.2017.01.012.
-
Ethical issues: Ethic Board approval was not required for this systematic review.
-
Conflict of interest: There are no actual or potential conflicts of interest for any of the authors.
References
[1] Botti M, Bucknall T, Manias E. The problem of postoperative pain: issues for future research. Int J Nurs Pract 2004;10:257–63.Search in Google Scholar
[2] Sauaia A, Min SJ, Leber C, Erbacher K, Abrams F, Fink R. Postoperative pain management in elderly patients: correlation between adherence to treatment guidelines and patient satisfaction. J Am Geriatr Soc 2005;53:274–82.Search in Google Scholar
[3] Peters ML, Sommer M, de Rijke JM, Kessels F, Heineman E, Patijn J, Marcus MA, Vlaeyen JW, van Kleef M. Somatic and psychologic predictors of long-term unfavorable outcome after surgical intervention. Ann Surg 2007;245:487–94.Search in Google Scholar
[4] Gagliese L, Katz J. Age differences in postoperative pain are scale dependent: a comparison of measures of pain intensity and quality in younger and older surgical patients. Pain 2003;103:11–20.Search in Google Scholar
[5] Perkins FM, Kehlet H. Chronic pain as an outcome of surgery. A review of predictive factors. Anesthesiology 2000;93:1123–33.Search in Google Scholar
[6] Kehlet H, Jensen TS, Woolf CJ. Persistent postsurgical pain: risk factors and prevention. Lancet 2006;367:1618–25.Search in Google Scholar
[7] Yarnitsky D, Crispel Y, Eisenberg E, Granovsky Y, Ben-Nun A, Sprecher E, Best LA, Granot M. Prediction of chronic post-operative pain: pre-operative DNIC testing identifies patients at risk. Pain 2008;138:22–8.Search in Google Scholar
[8] Weissman-Fogel I, Granovsky Y, Crispel Y, Ben-Nun A, Best LA, Yarnitsky D, Granot M. Enhanced presurgical pain temporal summation response predicts post-thoracotomy pain intensity during the acute postoperative phase. J Pain 2009;10:628–36.Search in Google Scholar
[9] Petersen KK, Arendt-Nielsen L, Simonsen O, Wilder-Smith O, Laursen MB. Presurgical assessment of temporal summation of pain predicts the development of chronic postoperative pain 12 months after total knee replacement. Pain 2015;156:55–61.Search in Google Scholar
[10] Granot M, Lowenstein L, Yarnitsky D, Tamir A, Zimmer EZ. Postcesarean section pain prediction by preoperative experimental pain assessment. Anesthesiology 2003;98:1422–6.Search in Google Scholar
[11] Rolke R, Baron R, Maier C, Tolle TR, Treede RD, Beyer A, Binder A, Birbaumer N, Birklein F, Botefur IC, Braune S, Flor H, Huge V, Klug R, Landwehrmeyer GB, Magerl W, Maihofner C, Rolko C, Schaub C, Scherens A, Sprenger T, Valet M, Wasserka B. Quantitative sensory testing in the German Research Network on Neuropathic Pain (DFNS): standardized protocol and reference values. Pain 2006;123:231–43.Search in Google Scholar
[12] Graven-Nielsen T, Vaegter HB, Finocchietti S, Handberg G, Arendt-Nielsen L. Assessment of musculoskeletal pain sensitivity and temporal summation by cuff pressure algometry: a reliability study. Pain 2015;156:2193–202.Search in Google Scholar
[13] Imai Y, Petersen KK, Morch CD, Arendt Nielsen L. Comparing test–retest reliability and magnitude of conditioned pain modulation using different combinations of test and conditioning stimuli. Somatosens Mot Res 2016:1–9.Search in Google Scholar
[14] Abrishami A, Chan J, Chung F, Wong J. Preoperative pain sensitivity and its correlation with postoperative pain and analgesic consumption: a qualitative systematic review. Anesthesiology 2011;114:445–57.Search in Google Scholar
[15] Werner MU, Mjobo HN, Nielsen PR, Rudin A. Prediction of postoperative pain: a systematic review of predictive experimental pain studies. Anesthesiology 2010;112:1494–502.Search in Google Scholar
[16] Ip HY, Abrishami A, Peng PW, Wong J, Chung F. Predictors of postoperative pain and analgesic consumption: a qualitative systematic review. Anesthesiology 2009;111:657–77.Search in Google Scholar
[17] Grosen K, Vase L, Pilegaard HK, Pfeiffer-Jensen M, Drewes AM. Conditioned pain modulation and situational pain catastrophizing as preoperative predictors of pain following chest wall surgery: a prospective observational cohort study. PLOS ONE 2014;9:e90185.Search in Google Scholar
[18] Valencia C, Fillingim RB, Bishop M, Wu SS, Wright TW, Moser M, Farmer K, George SZ. Investigation of central pain processing in postoperative shoulder pain and disability. Clin J Pain 2014;30:775–86.Search in Google Scholar
[19] Wilder-Smith OH, Schreyer T, Scheffer GJ, Arendt-Nielsen L. Patients with chronic pain after abdominal surgery show less preoperative endogenous pain inhibition and more postoperative hyperalgesia: a pilot study. J Pain Palliat Care Pharmacother 2010;24:119–28.Search in Google Scholar
[20] Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097.Search in Google Scholar
[21] Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to meta-analysis. West Sussex, United Kingdom: John Wiley & Sons Ltd.; 2009.Search in Google Scholar
[22] Hayden JA, van der Windt DA, Cartwright JL, Cote P, Bombardier C. Assessing bias in studies of prognostic factors. Ann Intern Med 2013;158:280–6.Search in Google Scholar
[23] Hsu YW, Somma J, Hung YC, Tsai PS, Yang CH, Chen CC. Predicting post-operative pain by preoperative pressure pain assessment. Anesthesiology 2005;103:613–8.Search in Google Scholar
[24] Rudin A, Eriksson L, Liedholm R, List T, Werner MU. Prediction of postoperative pain after mandibular third molar surgery. J Orofac Pain 2010;24:189–96.Search in Google Scholar
[25] Lautenbacher S, Huber C, Kunz M, Parthum A, Weber PG, Griessinger N, Sittl R. Hypervigilance as predictor of postoperative acute pain: its predictive potency compared with experimental pain sensitivity, cortisol reactivity, and affective state. Clin J Pain 2009;25:92–100.Search in Google Scholar
[26] Buhagiar L, Cassar OA, Brincat MP, Buttigieg GG, Inglott AS, Adami MZ, Azzopardi LM. Predictors of post-caesarean section pain and analgesic consumption. J Anaesthesiol Clin Pharmacol 2011;27:185–91.Search in Google Scholar
[27] Nielsen PR, Norgaard L, Rasmussen LS, Kehlet H. Prediction of post-operative pain by an electrical pain stimulus. Acta Anaesthesiol Scand 2007;51:582–6.Search in Google Scholar
[28] Strulov L, Zimmer EZ, Granot M, Tamir A, Jakobi P, Lowenstein L. Pain catastrophizing, response to experimental heat stimuli, and post-cesarean section pain. J Pain 2007;8:273–9.Search in Google Scholar
[29] Martinez V, Fletcher D, Bouhassira D, Sessler DI, Chauvin M. The evolution of primary hyperalgesia in orthopedic surgery: quantitative sensory testing and clinical evaluation before and after total knee arthroplasty. Anesth Analg 2007;105:815–21.Search in Google Scholar
[30] Lundblad H, Kreicbergs A, Jansson KA. Prediction of persistent pain after total knee replacement for osteoarthritis. J Bone Joint Surg Br 2008;90:166–71.Search in Google Scholar
[31] Bisgaard T, Klarskov B, Rosenberg J, Kehlet H. Characteristics and prediction of early pain after laparoscopic cholecystectomy. Pain 2001;90:261–9.Search in Google Scholar
[32] Pedersen KV, Olesen AE, Osther PJ, Arendt-Nielsen L, Drewes AM. Prediction of postoperative pain after percutaneous nephrolithotomy: can preoperative experimental pain assessment identify patients at risk. Urolithiasis 2013;41:169–77.Search in Google Scholar
[33] Thomazeau J, Rouquette A, Martinez V, Rabuel C, Prince N, Laplanche JL, Nizard R, Bergmann JF, Perrot S, Lloret-Linares C. Acute pain factors predictive of post-operative pain and opioid requirement in multimodal analgesia following knee replacement. Eur J Pain 2016;20:822–32.Search in Google Scholar
[34] Pan PH, Coghill R, Houle TT, Seid MH, Lindel WM, Parker RL, Washburn SA, Harris L, Eisenach JC. Multifactorial preoperative predictors for postcesarean section pain and analgesic requirement. Anesthesiology 2006;104: 417–25.Search in Google Scholar
[35] Lunn TH, Gaarn-Larsen L, Kehlet H. Prediction of postoperative pain by pre-operative pain response to heat stimulation in total knee arthroplasty. Pain 2013;154:1878–85.Search in Google Scholar
[36] Werner MU, Duun P, Kehlet H. Prediction of postoperative pain by preoperative nociceptive responses to heat stimulation. Anesthesiology 2004;100: 115–9.Search in Google Scholar
[37] Aasvang EK, Gmaehle E, Hansen JB, Gmaehle B, Forman JL, Schwarz J, Bittner R, Kehlet H. Predictive risk factors for persistent postherniotomy pain. Anesthesiology 2010;112:957–69.Search in Google Scholar
[38] Aasvang EK, Hansen JB, Kehlet H. Can preoperative electrical nociceptive stimulation predict acute pain after groin herniotomy? J Pain 2008;9:940–4.Search in Google Scholar
[39] Vaegter HB, Handberg G, Emmeluth C, Graven-Nielsen T. Preoperative hypoalgesia after cold pressor test and aerobic exercise is associated with pain relief six months after total knee replacement. Clin J Pain 2016 [in Press], https://www.ncbi.nlm.nih.gov/pubmed/27526332.Search in Google Scholar
[40] Wylde V, Sayers A, Lenguerrand E, Gooberman-Hill R, Pyke M, Beswick AD, Dieppe P, Blom AW. Preoperative widespread pain sensitization and chronic pain after hip and knee replacement: a cohort analysis. Pain 2015;156:47–54.Search in Google Scholar
[41] Ahmad S, De Oliveira Jr GS, Bialek JM, McCarthy RJ. Thermal quantitative sensory testing to predict postoperative pain outcomes following gynecologic surgery. Pain Med 2014;15:857–64.Search in Google Scholar
[42] Rudin A, Wolner-Hanssen P, Hellbom M, Werner MU. Prediction of postoperative pain after a laparoscopic tubal ligation procedure. Acta Anaesthesiol Scand 2008;52:938–45.Search in Google Scholar
[43] Jarrell J, Ross S, Robert M, Wood S, Tang S, Stephanson K, Giamberardino MA. Prediction of postoperative pain after gynecologic laparoscopy for nonacute pelvic pain. Am J Obstet Gynecol 2014;211, 360 e1–e8.Search in Google Scholar
[44] Wilder-Smith OH, Tassonyi E, Crul BJ, Arendt-Nielsen L. Quantitative sensory testing and human surgery: effects of analgesic management on postoperative neuroplasticity. Anesthesiology 2003;98:1214–22.Search in Google Scholar
[45] Petersen KK, Graven-Nielsen T, Simonsen O, Laursen MB, Arendt-Nielsen L. Preoperative pain mechanisms assessed by cuff algometry are associated with chronic postoperative pain relief after total knee replacement. Pain 2016;157:1400–6.Search in Google Scholar
[46] Grosen K, Fischer IW, Olesen AE, Drewes AM. Can quantitative sensory testing predict responses to analgesic treatment? Eur J Pain 2013;17:1267–80.Search in Google Scholar
© 2016 Scandinavian Association for the Study of Pain
Articles in the same Issue
- Scandinavian Journal of Pain
- Editorial comment
- Cardiovascular risk reduction as a population strategy for preventing pain?
- Observational study
- Diabetes mellitus and hyperlipidaemia as risk factors for frequent pain in the back, neck and/or shoulders/arms among adults in Stockholm 2006 to 2010 – Results from the Stockholm Public Health Cohort
- Editorial comment
- Exercising non-painful muscles can induce hypoalgesia in individuals with chronic pain
- Clinical pain research
- Exercise induced hypoalgesia is elicited by isometric, but not aerobic exercise in individuals with chronic whiplash associated disorders
- Editorial comment
- Education of nurses and medical doctors is a sine qua non for improving pain management of hospitalized patients, but not enough
- Observational study
- Acute pain in the emergency department: Effect of an educational intervention
- Editorial comment
- Home training in sensorimotor discrimination reduces pain in complex regional pain syndrome (CRPS)
- Original experimental
- Pain reduction due to novel sensory-motor training in Complex Regional Pain Syndrome I – A pilot study
- Editorial comment
- How can pain management be improved in hospitalized patients?
- Original experimental
- Pain and pain management in hospitalized patients before and after an intervention
- Editorial comment
- Is musculoskeletal pain associated with work engagement?
- Clinical pain research
- Relationship of musculoskeletal pain and well-being at work – Does pain matter?
- Editorial comment
- Preoperative quantitative sensory testing (QST) predicting postoperative pain: Image or mirage?
- Systematic review
- Are preoperative experimental pain assessments correlated with clinical pain outcomes after surgery? A systematic review
- Editorial comment
- A possible biomarker of low back pain: 18F-FDeoxyGlucose uptake in PETscan and CT of the spinal cord
- Observational study
- Detection of nociceptive-related metabolic activity in the spinal cord of low back pain patients using 18F-FDG PET/CT
- Editorial comment
- Patients’ subjective acute pain rating scales (VAS, NRS) are fine; more elaborate evaluations needed for chronic pain, especially in the elderly and demented patients
- Clinical pain research
- How do medical students use and understand pain rating scales?
- Editorial comment
- Opioids and the gut; not only constipation and laxatives
- Observational study
- Healthcare resource use and costs of opioid-induced constipation among non-cancer and cancer patients on opioid therapy: A nationwide register-based cohort study in Denmark
- Editorial comment
- Relief of phantom limb pain using mirror therapy: A bit more optimism from retrospective analysis of two studies
- Clinical pain research
- Trajectory of phantom limb pain relief using mirror therapy: Retrospective analysis of two studies
- Editorial comment
- Qualitative pain research emphasizes that patients need true information and physicians and nurses need more knowledge of complex regional pain syndrome (CRPS)
- Clinical pain research
- Adolescents’ experience of complex persistent pain
- Editorial comment
- New knowledge reduces risk of damage to spinal cord from spinal haematoma after epidural- or spinal-analgesia and from spinal cord stimulator leads
- Review
- Neuraxial blocks and spinal haematoma: Review of 166 case reports published 1994–2015. Part 1: Demographics and risk-factors
- Review
- Neuraxial blocks and spinal haematoma: Review of 166 cases published 1994 – 2015. Part 2: diagnosis, treatment, and outcome
- Editorial comment
- CNS–mechanisms contribute to chronification of pain
- Topical review
- A neurobiologist’s attempt to understand persistent pain
- Editorial Comment
- The triumvirate of co-morbid chronic pain, depression, and cognitive impairment: Attacking this “chicken-and-egg” in novel ways
- Observational study
- Pain and major depressive disorder: Associations with cognitive impairment as measured by the THINC-integrated tool (THINC-it)
Articles in the same Issue
- Scandinavian Journal of Pain
- Editorial comment
- Cardiovascular risk reduction as a population strategy for preventing pain?
- Observational study
- Diabetes mellitus and hyperlipidaemia as risk factors for frequent pain in the back, neck and/or shoulders/arms among adults in Stockholm 2006 to 2010 – Results from the Stockholm Public Health Cohort
- Editorial comment
- Exercising non-painful muscles can induce hypoalgesia in individuals with chronic pain
- Clinical pain research
- Exercise induced hypoalgesia is elicited by isometric, but not aerobic exercise in individuals with chronic whiplash associated disorders
- Editorial comment
- Education of nurses and medical doctors is a sine qua non for improving pain management of hospitalized patients, but not enough
- Observational study
- Acute pain in the emergency department: Effect of an educational intervention
- Editorial comment
- Home training in sensorimotor discrimination reduces pain in complex regional pain syndrome (CRPS)
- Original experimental
- Pain reduction due to novel sensory-motor training in Complex Regional Pain Syndrome I – A pilot study
- Editorial comment
- How can pain management be improved in hospitalized patients?
- Original experimental
- Pain and pain management in hospitalized patients before and after an intervention
- Editorial comment
- Is musculoskeletal pain associated with work engagement?
- Clinical pain research
- Relationship of musculoskeletal pain and well-being at work – Does pain matter?
- Editorial comment
- Preoperative quantitative sensory testing (QST) predicting postoperative pain: Image or mirage?
- Systematic review
- Are preoperative experimental pain assessments correlated with clinical pain outcomes after surgery? A systematic review
- Editorial comment
- A possible biomarker of low back pain: 18F-FDeoxyGlucose uptake in PETscan and CT of the spinal cord
- Observational study
- Detection of nociceptive-related metabolic activity in the spinal cord of low back pain patients using 18F-FDG PET/CT
- Editorial comment
- Patients’ subjective acute pain rating scales (VAS, NRS) are fine; more elaborate evaluations needed for chronic pain, especially in the elderly and demented patients
- Clinical pain research
- How do medical students use and understand pain rating scales?
- Editorial comment
- Opioids and the gut; not only constipation and laxatives
- Observational study
- Healthcare resource use and costs of opioid-induced constipation among non-cancer and cancer patients on opioid therapy: A nationwide register-based cohort study in Denmark
- Editorial comment
- Relief of phantom limb pain using mirror therapy: A bit more optimism from retrospective analysis of two studies
- Clinical pain research
- Trajectory of phantom limb pain relief using mirror therapy: Retrospective analysis of two studies
- Editorial comment
- Qualitative pain research emphasizes that patients need true information and physicians and nurses need more knowledge of complex regional pain syndrome (CRPS)
- Clinical pain research
- Adolescents’ experience of complex persistent pain
- Editorial comment
- New knowledge reduces risk of damage to spinal cord from spinal haematoma after epidural- or spinal-analgesia and from spinal cord stimulator leads
- Review
- Neuraxial blocks and spinal haematoma: Review of 166 case reports published 1994–2015. Part 1: Demographics and risk-factors
- Review
- Neuraxial blocks and spinal haematoma: Review of 166 cases published 1994 – 2015. Part 2: diagnosis, treatment, and outcome
- Editorial comment
- CNS–mechanisms contribute to chronification of pain
- Topical review
- A neurobiologist’s attempt to understand persistent pain
- Editorial Comment
- The triumvirate of co-morbid chronic pain, depression, and cognitive impairment: Attacking this “chicken-and-egg” in novel ways
- Observational study
- Pain and major depressive disorder: Associations with cognitive impairment as measured by the THINC-integrated tool (THINC-it)

