Abstract
Prevalence estimates of pain differ depending on how it is defined and measured and on the populations studied. It has been estimated that on a given day, as many as 30–44% of the general population experience some kind of pain. Information about the prevalence of pain in Iceland is not available. The aims of this study were to evaluate the prevalence of pain of various origins among the general population of Iceland, to test hypotheses regarding relationships between pain, quality of life (QOL) and demographic variables, to evaluate participants’ beliefs about causes of their pain, and to evaluate how those who experience pain manage it. A random sample of 1286 adults was drawn from a national registry holding information about all citizens of Iceland. Data were collected with a postal-survey. Pain was evaluated with the Brief Pain Inventory (BPI), with instructions modified to evaluate pain in the past week as opposed to the past 24 h. Of 1286 invited, 599 (46.6%) participated, of which, 232 had experienced pain in the past week (40.3%). Participants had a mean (SD) age of 44.94 (17.12) years and 56% were women. Those who had pain perceived their health to be worse than those who had not [B = −0.91, SE = 0.15, Wald = 38.75, p = 0.00], but did not differ on other variables. Of 232 individuals reporting pain, 183 (79.6%) or 30.6% of the total sample had experienced pain for more than three months. On a scale from 0 “no pain” to 10 “pain as bad as I can imagine” the mean (SD) pain severity score (composite of four pain severity scores) for the 232 participants reporting pain was 3.21 (1.73) and pain interference with life activities 2.59 (1.98), also on a 0–10 scale. Pain severity predicted pain interference [B = 0.71; F = 126.14; df = 1,206; p = 0.00], which mediated the effects of pain severity on mood and QOL. Between Pain Interference with Life and Positive Affect [B = −0.06; F = 4.53; df = 1,196; p = 0.04], between Pain Interference and Negative Affect [B = 0.15; F = 23.21; df = 1,196; p = 0.00], and between Pain Interference and Global Quality of Life [B = −0.18; F = 29.11; df = 1,196; p = 0.00]. Most frequent causes for pain were strain injuries (n = 79), resulting from work or sports activity, arthritis (n = 39), mechanical problems (e.g. due to birth defects, curvature, slipped discs, etc.) (n = 37), various diseases (n = 31) and accidents (n = 30). Nineteen participants did not know what caused their pain. Treatments for pain varied, but most had used medications alone (n = 76) or in combination with other treatments (n = 61). The prevalence of pain in the general population of Icelandic adults is similar to what has been reported. Estimates of chronic pain are towards the higher end when compared to data from other European counties, yet comparable to countries such as Norway. This raises questions about possible explanations to be looked for in genetics or cultural point of view. This population based study provides valuable information about the prevalence of pain in Iceland and also supports findings previously reported about pain in the neighboring countries.
1 Introduction
Worldwide, pain is the most prevalent reason for seeking health care [1,2,3]. While pain is common, prevalence estimates differ depending on how pain is defined and measured and on the populations studied. It has been estimated that on a given day, as many as 30-44% of the general population experience some kind of pain [4,5,6]. Prevalence estimates of pain are higher when only hospitalized patients are surveyed with 55-71% of patients reporting pain in the past 24 h [15,16,17]. These numbers are lower when only chronic-or persistent pain is assessed. The International Association for the Study of Pain defines chronic pain as “pain without apparent biological value that has persisted beyond the normal tissue healing time (usually taken to be 3 months)” [7]. The prevalence of chronic pain has been found to range from 17% to 55% [5,8,9,10,11,12]. In the World Health Organization Collaborative Study of Psychological Problems in General Health Care information on persistent pain was collected [13]. Persistent pain was defined as “one or more current pain symptom present on most days over a period of six months or more during the past year” and assessed in a random sample of patients seeking health care at fifteen sites in fourteen countries, located in Asia, Africa, Europe, South-and North-America. Prevalence ranged from 6.2% (Nigeria) to 33% (Chile), with the overall prevalence across all sites of 21.5%. In a recent survey of 46,937 individuals conducted in Europe and Israel, Breivik et al. assessed pain with a severity of five or higher that had lasted for more than six months and found 19% of the sample to experience such pain [14].
Lower socioeconomic status and lower levels of education have been associated with pain [9,11,19,20], pain is more common in women than men [4,5,9,11,18,19,20,21] and increases with increased age [4,5,9,11,20]. Pain is related to interference with life activities [9,13,22], quality of life (QOL) [23,24,25], and psychological problems, including anxiety and depression [9,13,26].
It is widely reported that pain often goes unrecognized and is not adequately managed [16,27,28]. While limited information exists on how people manage their pain, some studies have found that the most common resources are seeking medical help and using medications, either prescription or over the counter. People also use a variety of other approaches to manage their pain, such as physiotherapy and complementary therapies [5,18].
To date, only limited research has been conducted in Iceland concerning pain or pain management. The aims of this population based study that takes advantage of access to an entire nation, were to evaluate the prevalence and severity of pain of various origins among the general population of Iceland, to test hypotheses regarding the relationships between pain, QOL and demographic variables (Fig. 1), to evaluate participants’ beliefs about causes of their pain, and finally, to evaluate how those who experience pain manage it. The study not only provides useful information for the Icelandic community not previously available, it also replicates international findings and explores further self-reported management of pain.
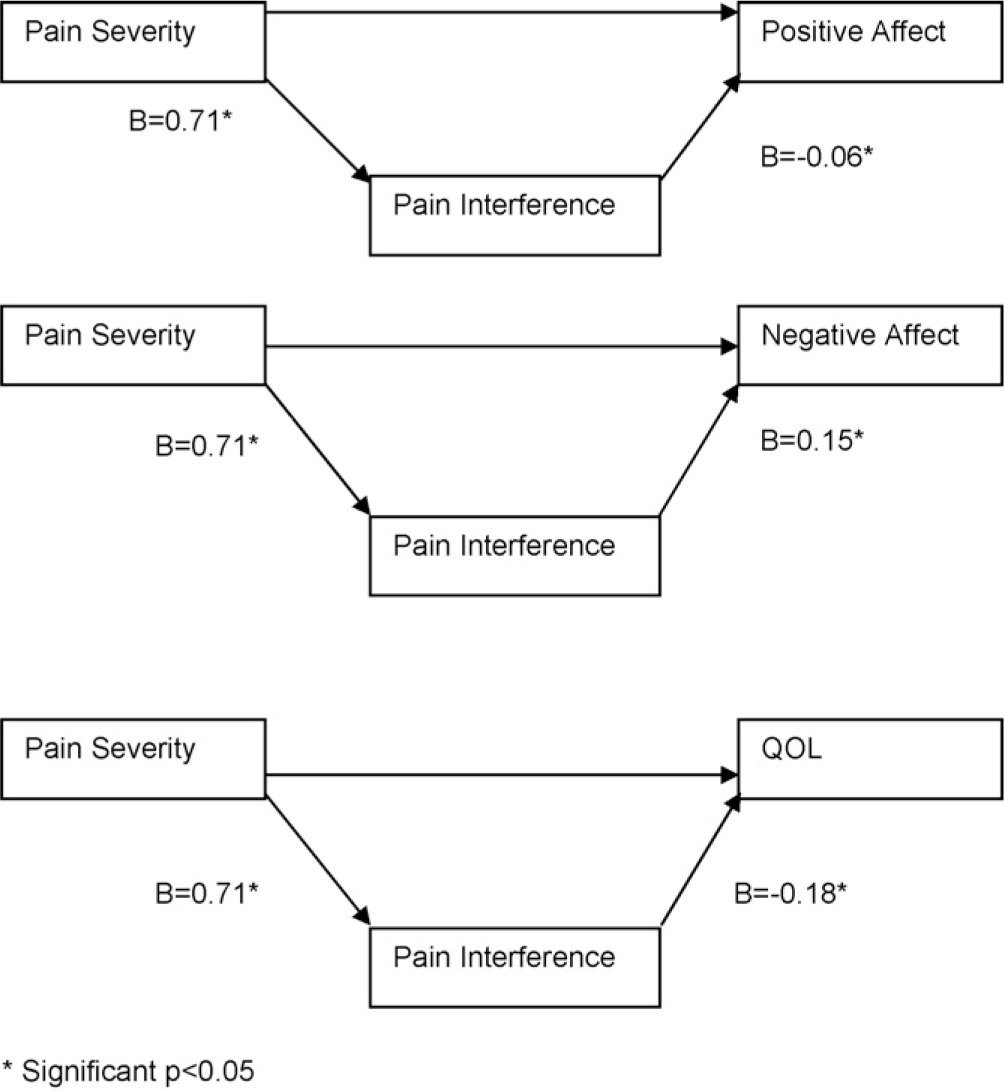
Relationships between pain, pain interference, mood and QOL controlling for age, gender and education. *Significant p < 0.05
2 Methods
2.1 Sample
A random sample of 1286 Icelandic adults, 18 years old and older, was drawn from the Icelandic National Registry, which holds information about names, birth-dates, and addresses of all residents of Iceland. The residents of Iceland numbered 288,201 as of December 1, 2002 [29] a month before data collection started. Of those invited 599 (46.6%) completed the survey.
2.2 Instruments
2.2.1 Demographic characteristics
Information about age, gender, marital status, education, income, region of habitation, and health status was collected.
2.3 Pain severity and pain interference with life activities
The Icelandic version of the Brief Pain Inventory (BPI) [30,31] was used to assess prevalence, severity, and interference of pain. It contains items to evaluate presence and location of pain and four items assess pain severity (worst pain, least pain, average pain, and pain now). Response options range from 0 “no pain” to 10 “pain as bad as I can imagine”, with a single composite severity score (Pain Severity) created by taking the mean of the four severity items for analysis. One open-ended question obtains information about treatments or medications used to treat pain. One item addresses how much pain relief the individual has received, with response options ranging from 0% (no relief) to 100% (complete relief). Finally, seven items evaluate pain interference with life activities. Participants report how any type of pain interfered with various aspects of their lives with options from 0 “Does not interfere” to 10 “Completely interferes”. A single interference score (Pain Interference) was created by taking the mean of the seven interference items. Pain and pain interference are usually assessed with a 24-h timeframe, but in the present study the timeframe was changed from 24-h to “the past week”. Open-ended questions were added to assess how long participants had experienced their pain, and what participants believed caused their pain.
The BPI has been used extensively and found to be both reliable and valid in several languages [e.g. 32,33,34,35,36,37]. Psychometric properties of the Icelandic BPI have been assessed in a convenience sample of 244 individuals and found to be both reliable and valid [38]. In the present study the internal consistency of the severity scale was α = 0.86 and α = 0.78 for the interference scale. Only persons who had experienced pain in the past week were asked to fill out the BPI.
2.4 Mood
Mood was assessed with the Positive and Negative Affect Scale (PANAS) [39] a 20-item measure consisting of two subscales, positive and negative affect. Subjects rate each of the affect words with respect to how they felt during the past week, on a scale of 1 to 5 with anchors of “very slightly”, “a little”, “moderately”, “quite a bit”, and “extremely”. Mean scores for each subscale are used in analyses. The measure has reported reliability (internal consistency) and construct validity [39]. The PANAS was translated into Icelandic by the primary investigator for this study and back-translated into English by another bilingual person. These steps were repeated until agreement was reached. The instrument was pilot tested with 10 Icelandic adults who provided feedback regarding understand-ability of the items. In response to their feedback a new translation was generated for 5 items and this version was then completed by 5 additional Icelandic speaking adults. A new translation was sought for two items in response to their feedback. In this study the internal consistency of the positive scale was α = 0.81 and the negative scale α = 0.88. The correlation between the two scales was r = −0.12. This low correlation supports that the two scales measure two separate constructs.
2.5 Quality of life
Global quality of life was measured with a single item stating “I am content with the quality of my life right now”. This item is based on a single item from the Functional Assessment of Cancer Therapy (FACT) scales [40]. The response options in this study, were (1) “Not at all”, (2)“A little bit, (3)“Quite a bit”, and (4)“Very much”. Single item measures for QOL have been used with good results [41] and were chosen for this study instead of lengthy measures to limit response burden.
2.6 Perceived personal health
Personal health was evaluated with a single item generated by the research team. “How is your current health?” Response options were “Very good”, “Good”, “Neither good or poor” “Poor” and “Very poor”.
2.7 Procedure
After obtaining permission from appropriate Institutional Review Boards, specialists at the Icelandic National Registry generated a simple random sample of registered habitants of Iceland, 18 years or older, as of December 31, 2002. Data collection was conducted with a mailed survey from the beginning of January through mid March 2003. The questionnaire, cover letters, and mailing schedule were based on the Tailored Design Method [42].
3 Results
3.1 Sample
The mean (SD) age of the respondents and non-respondents was 44.94 (17.12) and 44.25 (19.44) respectively which is not a significant difference. A majority of respondents were female (56%). Of the 654 women that were invited to participate, 333 returned the questionnaire (51%) while 264 of 618 men (43%) did so (data on gender were not available for two participants). The mean (SD) length of education for respondents was 13.81 (4.27) years. The majority of participants were married, or cohabiting (67.4%) and 68.6% worked either fullor part time outside of the home. 63.8% of participants reported living in Reykjavik and surrounding neighborhoods, 28.1% lived in villages, and 7.1% lived in rural areas. These figures accurately represent the population of Iceland at the time of data collection, with 62% living in Reykjavik and the surrounding neighborhoods, 31.6% living in urban areas throughout the country, and 6% living in rural areas [29]. Unfortunately, data about income were too incomplete to use for any analysis. For further information on demographics see Table 1.
Demographic information.
| All participants, n = 599 | Pain in past week, n = 232(40.3%) | |||
|---|---|---|---|---|
|
|
|
|||
| n | % | n | % | |
| Gender | ||||
| Men | 264 | 44.1 | 95 | 40.9 |
| Women | 333 | 55.6 | 137 | 59.1 |
| Marital status | ||||
| Married/cohabit | 404 | 67.4 | 151 | 65.1 |
| Unmarried | 114 | 19.0 | 44 | 19.0 |
| Divorced | 48 | 8.0 | 22 | 9.5 |
| Widowed | 29 | 4.8 | 14 | 6.0 |
| Missing | 4 | 0.7 | 1 | 0.4 |
| Employment | ||||
| Full time | 339 | 56.6 | 123 | 53.0 |
| Part time | 67 | 11.2 | 29 | 12.5 |
| Homemaker | 19 | 3.2 | 5 | 2.2 |
| Student (±work) | 72 | 12.0 | 23 | 9.9 |
| Retired | 59 | 9.8 | 27 | 11.6 |
| Unemployed | 5 | 0.8 | 4 | 1.7 |
| Disability | 21 | 3.5 | 15 | 6.5 |
| Other | 9 | 1.5 | 6 | 2.6 |
| Residence | ||||
| Reykjavik | 379 | 63.3 | 145 | 62.5 |
| Villages | 168 | 28.0 | 70 | 30.2 |
| Rural areas | 44 | 7.3 | 17 | 7.3 |
3.2 Prevalence of pain
Participants were asked whether they had experienced pain in the past week and 575 participants of 599 answered this question (96%). Of those, 232 (40.3%) had experienced pain in the past week. Of the 232 individuals who reported pain in the past week, 183 (78.9%) indicated that they had experienced this pain for more than three months or 30.6% of the 599 participants. Those who had experienced pain for more than three months did not differ in terms of demographic characteristics, perceived health or QOL from those who had experience pain for less than three months.
Those who had experienced pain in the past week (n = 232) had experienced pain for a length of time ranging from one day to 50 years. The median length of their pain experience was 1095 days (3 years). Their worst pain in the past week had a mean (SD) of 4.85 (2.17). Their least pain in the past week had a mean (SD) of 1.92 (1.86) and their average pain had a mean (SD) of 3.35 (1.93). Participants’ mean (SD) pain now was 2.70 (2.27). Participants’ Pain Severity composite in the past week had a mean (SD) of 3.21 (1.73). Participants’ Pain Interference with life activities had a mean (SD) of 2.59 (1.98).
3.3 Relationships between demographic variables, pain, mood and QOL
Those who had experienced pain in the past week were compared to those who had not in terms of demographic variables. Comparisons were made with a Logistic regression and based on age, gender, education, marital status, habitation, personal health, QOL, and whether participants had been diagnosed with a chronic disease or not. The only significant difference between those who had experienced pain and those who had not was that those who had experienced pain rated their personal health worse [B = −0.91, SE = 0.15, Wald = 38.75, p = 0.00].
The item assessing perceived health was completed by 540 participants. Most participants indicated that their health was “Very good” (42%), or “Good” (39%), while a few indicated that it was “Neither good or poor” (16%) or “Poor” (4%) and none indicated that is was “Very poor”. The mean (SD) score was 1.82 (0.84). For those who had been in pain (n = 232) the findings differed in that, 22.8% said their health was “Very good”, 44% said it was “Good”, for 59% it was “Neither good or poor” and for 18% it was “Poor”. None of the participants who had been in pain said their health was “Very poor”.
The Positive and Negative Affect Scale (PANAS) was completed by 549 participants. The mean (SD) on the positive affect scale was 3.27 (0.66), with an observed range of 1-5 (possible range of 1-5 with higher scores indicating more positive mood) for the entire sample, and 3.21 (0.69) for those who had experienced pain in the past week. The mean (SD) score on the negative affect scale was 1.66 (0.67) with an observed range of 1.0-4.7 (possible range 1-5 with higher scores indicating more negative mood) for the entire sample and 1.74 (0.70) for those in pain. Scores on neither the positive nor negative affect scales differed for those who had pain and those who did not.
The global quality of life (QOL) item was completed by 590 participants. The mean (SD) score was 3.2 (0.78) for the total sample, with an observed range of 1-4 (possible range 1-4 with higher scores indicating better quality of life), and 3.06 (0.82) for those in pain. This was not a significant difference.
3.4 Pain variables as predictors of pain interference with life
The following hypothesis were tested; when controlling for gender, age and education (a) pain severity predicts pain related interference with life activities; (b) pain severity predicts positive and negative affect and QOL; and (c) pain related interference with life activities mediates the effects of pain severity on positive and negative affect and quality of life (Fig. 1).
When examining the effects of pain severity on pain interference with life activities we used the pain severity composite score for analysis. Since pain has been reported to differ based on age, gender and education we controlled for these variables in the analysis [e.g. 9,11,19]. Pain Severity significantly predicted Pain Interference with life [B = 0.71; F = 126.14; df = 1,206; p = 0.00] (Fig. 1).
The test of mediation was based on first testing the relationship between the predictor (Pain Severity) and the potential mediator (Pain Interference with Life) as described previously. The second test is of the path between the potential mediator and the dependent variable (mood and QOL) with all variables at an equal level or to the left partialled out. If these two relationships are significant, it will be concluded that Pain Interference with Life is a mediating variable; it is not considered necessary to test the direct path between the independent (Pain Severity) and dependent variables (mood and QOL), and in fact, this path is not considered to be of importance if a significant mediation effect is found [43].
We tested the mediation effect of pain interference between pain severity, mood and QOL. All three mediation effects were significant. Between Pain Interference with Life and Positive Affect [B = −0.06; F = 4.53; df = 1,196; p = 0.04], between Pain Interference and Negative Affect [B = 0.15; F = 23.21; df = 1,196; p = 0.00], and between Pain Interference and Global Quality of Life [B = −0.18; F = 29.11; df = 1,196; p = 0.00] (Fig. 1).
Since the mediation effect of Pain Interference was established it is not necessary to test the direct paths from Pain Severity to the outcome variables as described above. However, these tests are presented here to provide further information. As before all analysis controlled for the effects of age, gender and education. The direct path between Pain Severity and Positive affect was not significant [B = −0.03; F = 1.17; df = 1,197; p = 0.28], but the direct paths from Pain Severity to Negative affect [B = 0.08; F = 7.00; df = 1,197; p = 0.01] and QOL [B = −0.10; F = 8.30; df = 1,197; p = 0.00] were.
3.5 Causes of pain
A content analysis was performed on an open ended question asking participants to specify what they believed to be the cause of their pain. Two researchers conducted the analysis. First, a scoring sheet was generated independently from the data by each researcher, and then a single scoring sheet was generated from the two. The data were then analyzed separately by the two researchers and the analysis compared for consistency. A high degree of agreement was among the two researchers. Of those who had pain, 204 answered the question. Some participants provided multiple answers to those questions. In response to what the participants believed to have caused their pain the most frequently cited causes for pain were strain injuries resulting from work or sports activities (n = 79), arthritis (n = 39), mechanical problems (e.g. due to birth defects, curvature, slipped discs, etc.) (n = 37), disease (n = 31) and accidents (n = 30). A fair number (n = 19) cited that they did not know what caused their pain (Table 2). Many of the participants cited numerous causes for their pain and a few did not specify a cause for their pain but instead wrote in their type of pain (“back ache”, “headache”, etc.).
Causes of pain[a] (n = 204 provided answers).
| Cause | n | % of total number of causes identified[b] |
|---|---|---|
| Strain injuries: related to work and sports activities | 79 | 27.9 |
| Arthritis: e.g. OA, fibromyalgia, RA, and other joint disease | 39 | 13.8 |
| Mechanical problems: e.g. birth defects, curvature, slipped discs, nerve injury, large breasts | 37 | 13.0 |
| Disease: e.g. heart, kidney, GI, cancer | 31 | 11.0 |
| Injuries due to accidents and broken bones | 30 | 10.6 |
| Do not know | 19 | 6.7 |
| Reproductive system-women: pregnancy, birth, pelvic arthropathy, ovulation, menstruation | 13 | 4.6 |
| Other or cannot be categorized | 11 | 3.9 |
| Complications from surgery | 9 | 3.2 |
| Psychological, stress, anxiety | 9 | 3.2 |
| Lifestyle: lack of exercise, food | 6 | 2.1 |
| Total | 283 | 100 |
3.6 Methods used to treat pain
When asked whether participants had sought medical attention for their pain, all 232 individuals who reported having pain in the past week answered this question. Of those, 179 reported having sought medical attention (77.5%). Those who had used medication or other methods to treat their pain in the past week reported an average (SD) pain relief of 43.0% (34.7%).
A content analysis was conducted of responses to the question asking participants what treatments they received for their pain for which 200 participants provided an answer. The same approach was used to the analysis as described above. A majority indicated that they had used medications (n = 137), and most had used analgesic medications (n = 122). A fair number, 47 had been in physical therapy and/or massage, 40 had used exercise, 31 had been in physical therapy, 19 had used heat or cold and 21 had not used anything (Table 3). Many had used a combination of treatments. Most had only used medications alone (n = 76), 61 had used mediations in combination with other treatments, and 42 had used other methods without medications.
Treatments for pain[a] (n = 200 provided answers).
| Self-reported treatment | n | % of total number of treatments identified[b] |
|---|---|---|
| Medication (of which analgesics) | 137 (122) | 42.0 (37.4) |
| Physical therapy, physiotherapeutic massage, massage | 47 | 14.4 |
| Exercise-swimming, walking, stretching, yoga | 40 | 12.3 |
| Nothing | 29 | 8.9 |
| Heat or cold | 19 | 5.8 |
| Invasive procedures | 15 | 4.6 |
| Self-care: sleep, rest, posture, cut back on work, take care not to get cold, home massage | 12 | 3.7 |
| Complementary and alternative therapies (chiropractor, acupuncture, homeopathic remedies, relaxation, cranio sacral treatment, marijuana | 11 | 3.4 |
| Other | 7 | 2.2 |
| Orthopedic support (braces and shoes) | 4 | 1.2 |
| Have adjusted | 3 | 0.9 |
| Sought medical help without success | 2 | 0.6 |
| Total | 326 | 100 |
4 Discussion
The prevalence of pain of different origins in the general population of Icelandic adults is similar to what has previously been reported. In this study, the prevalence of pain of various origins in the week prior to data collection was 40.3%, which compares to prevalence estimates of 29.6% (5), 33% (6), and 40% (4) on the day of data collection, and 43.2% in the previous week (5) in studies conducted in other countries.
In this study the prevalence of pain that had lasted for more than three months was 78.9% for those who reported pain on the day of data collection, or 30.6% of the sample Previous prevalence estimates of persistent pain vary greatly. Estimates for pain that has lasted for more than three months range from 17% to 55% [5,8,9,10]. Prevalence estimates, of chronic pain lasting longer than six months, also vary greatly with estimates ranging from 6.2% to 49% [8,13,14]. These differences may both be attributed to different definitions and measurements as well as the populations assessed. Compared to most prevalence estimates it is evident that pain of different origins is common in Iceland, and the strengths of these findings lie in the random sample generated from a general population. When compared to findings from a large European study on the prevalence of pain [14] the prevalence estimates of chronic pain in Iceland are towards the higher end found in that study. The Icelandic findings are, however, very similar to what was found in Norway. This raises questions about possible explanations that could be further pursued through research and cultural aspects and genetics are issues that certainly need to be explored further.
This study provides information regarding the severity of pain and pain related interference with life activities. All of the items suggest that the participants are experiencing mild pain, while the mean score on the pain worst item is close to being considered of moderate severity [44]. This study also examined relationships between pain of different origins and background variables, as well as the relationship between pain and mood and QOL variables. When participants in pain were compared to those without pain, the only significance difference was that those in pain reported poorer health. It was surprising not to find an association between pain and age since such relationships have frequently been reported [e.g. 4,5,10]. This could possibly be explained by the fact that relatively few participants were in the older age groups in this study and, therefore, it is possible that there was not enough power to detect relationships between age and pain variables. This relationship needs to be explored further in future studies.
It is also surprising to find no relationship between pain and gender, and pain and education since such relationships have frequently been identified in previous research [4,6,10,15,45], and this lack of a relationship calls for further investigation. In this study the relationship between pain severity and pain interference with life activities was also examined. Pain severity predicted pain interference with life activities as would be expected [9,13,22]. In addition, the mediation effect of pain interference with life activities between pain and mood and QOL was tested. All three paths are significant, suggesting that pain interference with life activities mediates the effect of pain severity on positive mood, negative mood, and QOL. This is not surprising since disabling effects of pain would be expected to have negative effects on mood and QOL rather than pain in itself.
This study also provides information about what participants perceive to be the cause of their pain. The most commonly identified causes were strain injuries resulting from work or sports activities, arthritis, mechanical problems, disease, and accidents. A fair number of participants stated that they did not know what caused their pain. Limited research is available on what people believe to cause their pain, therefore, this study provides useful insights. Additionally, this study provides information about how participants manage their pain. The vast majority had sought medical attention for their pain and the most common treatment combinations were medication alone, followed by medication in combination with other treatments. A fair number did not use anything to control their pain. This is in line with previous findings where the most common resources have been seeking medical help and using drugs, either prescription medication or over the counter. People have also reported use of a variety of approaches to manage their pain, such as physiotherapy including exercise, electrotherapy, heat and massage and complementary therapies including herbal medicines, massage, heat, and acupuncture [5,18].
One of the major strengths of this study is the access to the entire Icelandic population through the Icelandic National Registry, and the use of a random sample. All Icelandic residents are listed in the registry and it had just been updated before the sample used in the study was generated, thereby, limiting the likelihood of including individuals who had passed away or who had incorrect addresses.
The major limitation of the study is the modest response rate increasing the risk of non-response error. It was possible to compare responders and non-responders in terms of age, and gender. While responders and non-responders did not differ in terms of age, they did differ in terms of gender. The response rate for women was 51%, while response rate for men was 43%. Based on this it is possible that the results more accurately reflect the experiences of women than men. One can also speculate whether those who were invited to participate were more likely to do so if they experienced pain themselves and, therefore, had some investment in the topic. It could on the other had be argued that individuals who were seriously ill or fragile and, therefore, possibly experiencing pain, might not participate in a study regardless of the topic. Based on the phone calls and letters to the PI during the data collection phase it is fair to assume that part of the non-response is in fact due to both of these reasons. It is, therefore, difficult to speculate whether individuals were more likely to participate if they were in pain or if they were not in pain. Despite this limitation, it is fair to conclude that pain of different origins is common in Iceland and that many individuals experience what could be called chronic or persistent pain. The findings are also very much in line with what has previously been reported supporting that the respondents in this study were fairly representative. These findings call for interventions to improve management of pain whether they are at the systems or individual level.
DOI of refers to article: 10.1016/j.sjpain.2010.05.030.
-
Conflicts of interest: The authors do not declare any conflicts of interest.
Acknowledgements
Funding for this study was provided by: (1) Sigma Theta Tau International Small Grant, (2) Oncology Nursing Foundation/Janssen Pharmaceutica LP Cancer Nursing Pain Research Grant, (3) Research Grant from the Icelandic Cancer Society, (4) Scholarship from Landsbanki Íslands (Icelandic National Bank) and, (5) NR03126 awarded to Professor Sandra Ward. The authors wish to thank Elfa Gretarsdottir RN, MS for her assistance with content analysis.
References
[1] Cordell WH, Keene KK, Giles BK, Jones JB, Jones JH, Brizendine EJ. The high prevalence of pain in emergency medical care. Am J Emerg Med 2002;20(3):165-9.Search in Google Scholar
[2] Mantyselka P, Kumpusalo E, Ahonen R, Kumpusalo A, Kauhanen J, Viinamäki H, Halonen P, Takala J. Pain as a reason to visit the doctor: a study in Finnish primary health care. Pain 2001;89:175-80.Search in Google Scholar
[3] Frolund F, Frolund C. Pain in general practice. Pain as a cause of patient-doctor contact. Scand J Prim Health Care 1986;4:97-100.Search in Google Scholar
[4] Buskila D, Abramov G, Biton A, Neumann L. The prevalence of pain complaints in a general population in Israel and its implications for utilization of health services. J Heumatology 2000;27(6):1521-5.Search in Google Scholar
[5] Català E, Reig E, Artés M, Aliaga L, López JS, Segú JL. Prevalence of pain in the Spanish population: telephone survey in 5000 homes. Eur J Pain 2002;6:133-40.Search in Google Scholar
[6] Kind P, Dolan P, Gudex C, Williams A. Variations in population health status: results from a United Kingdom national questionnaire survey. BMJ 1998;316(7133):736-41.Search in Google Scholar
[7] Harstall C, Ospina M. How prevalent is chronic pain. Pain clinical updates. Int Assoc Study Pain 2003;XI(2):1-4.Search in Google Scholar
[8] Andersson HI, EjlertssonG, Leden I, Rosenberg C. Chronic pain in a geographically defined general population: studies of differences in age, gender, social class, and pain localization. Clin J Pain 1993;9(3):174-82.Search in Google Scholar
[9] Blyth FM, March LM, Brnabic AJM, Jorm LR, Williamson M, Cousins MJ. Chronic pain in Australia: a prevalence study. Pain 2001;89(2-3):127-34.Search in Google Scholar
[10] Elliott AM, Smith BH, Penny KI, Smith WC, Chambers WA. The epidemiology of chronic pain in the community. Lancet 1999;354(9186):1248-52.Search in Google Scholar
[11] Rustøen T, Wahl AK, Hanestad BR, Lerdal A, Paul S, Miaskowski C. Prevalence and characteristics of chronic pain in the general Norwegian population. Eur J Pain 2004;8(6):555-65.Search in Google Scholar
[12] Verhaak PF, Kerssens JJ, Dekker J, Sorbi MJ, Bensing JM. Prevalence of chronic benign pain disorder among adults: a review of the literature. Pain 1998;77:231-9.Search in Google Scholar
[13] Gureje O, Von Korff M, Simon GE, Gater R. Persistent pain and well-being. A World Health Organization study in primary care. JAMA 1998;280(2):147-51.Search in Google Scholar
[14] Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain 2006;10(4):287-333.Search in Google Scholar
[15] Costantini M, Viterbori P, Flego G. Prevalence of pain in Italian hospitals: results of a regional cross-section survey. J Pain Symptom Manage 2002;23(3):221-30.Search in Google Scholar
[16] Salomon L, Tcherny-Lessenot S, Collin E, Coutaux A, Levy-Soussan M, Legeron MC, Bourgeois P, Cesselin F, Desfosses G, Rosenheim M. Pain prevalence in a French teaching hospital. J Pain Symptom Manage 2002;24(6):586-92.Search in Google Scholar
[17] Sawyer J, Haslam L, Robinson S, Daines P, Stilos K. Pain prevalence study in a large Canadian teaching hospital. Pain Man Nurs 2008;9(3):104-12.Search in Google Scholar
[18] Bassols A, Bosch F, Baños JE. How does the general population treat their pain? A survey in Catalonia, Spain. J Pain Symptom Manage 2002;23(4):318-28.Search in Google Scholar
[19] Bingefors K, Isacson D. Epidemiology, co-morbidity, and impact on health-related quality of life of self-reported headache and musculoskeletal pain-a gender perspective. Eur J Pain 2004;8(5):435-50.Search in Google Scholar
[20] Smith BH, Elliott AM, Chambers WA, Smith WC, Hannaford PC, Penny K. The impact of chronic pain in the community. Fam Pract 2001;18(3):292-9.Search in Google Scholar
[21] Thomas E, Peat G, Harris L, Wilkie R, Croft PR. The prevalence of pain and pain interference in a general population of older adults: cross-sectional findings from the North Staffordshire Osteoarthritis Project (NorStOP). Pain 2004;110(1-2):361-8.Search in Google Scholar
[22] Neville A, Peleg R, Singer Y, Sherf M, Shvartzman P. Chronic pain: a population-based study. Isr Med Assoc J 2008;10(10):676-80.Search in Google Scholar
[23] Jamison RN, Fanciullo GJ, McHugo GJ, Baird JC. Validation of the short-form interactive computerized quality of life scale (ICQOL-SF). Pain Med 2007;8(3):243-50.Search in Google Scholar
[24] Lame IE, Peters ML, Vlaeyen JW, Kleef M, Patijn J. Quality of life in chronic pain is more associated with beliefs about pain, than with pain intensity. Eur J Pain 2005;9(1):15-24.Search in Google Scholar
[25] Laursen BS, Bajaj P, Olesen AS, Delmar C, Arendt-Nielsen L. Health related quality of life and quantitative pain measurement in females with chronic non-malignant pain. Eur J Pain 2005;9(3):267-75.Search in Google Scholar
[26] Munce SE, Stewart DE. Gender differences in depression and chronic pain conditions in a national epidemiologic survey. Psychosomatics 2007;48(5):394-9.Search in Google Scholar
[27] McDonald DD. Gender and ethnic stereotyping and narcotic and analgesic administration. Res Nurs Health 1994;17:45-9.Search in Google Scholar
[28] Whelan CT, Jin L, Meltzer D. Pain and satisfaction with pain control in hospitalized medical patients. Arch Intern Med 2004;164:175-80.Search in Google Scholar
[29] Icelandic statistics; 2003. http://www.statice.is/Statistics/Population. Accessed October 19, 2007.Search in Google Scholar
[30] Daut RL, Cleeland CS, Flanery RC. Development of the Wisconsin brief pain questionnaire to assess pain in cancer and other disease. Pain 1983;17:197-210.Search in Google Scholar
[31] Cleeland SC, Syrjala KL. How to assess cancer pain. In: Turk DC, Melzack R, editors. Handbook of pain assessment. New York: Guilford Press; 1992. p. 362-90.Search in Google Scholar
[32] Radbruch L, Loick G, Kiencke P, Lindena G, Sabatowski R, Grond S, Lehmann KA, Cleeland CS. Validation of the German version of the brief pain inventory. J Pain Symptom Manage 1999;18(3):180-7.Search in Google Scholar
[33] Saxena A, Mendoza T, Cleeland CS. The assessment of cancer pain in north India: the validation of the Hindi brief pain inventory-BPI-H. J Pain Symptom Manage 1999;17(1):27-35.Search in Google Scholar
[34] Ger LP, Ho ST, Sun WZ, Wang MS, Cleeland CS. Validation of the brief pain inventory in a Taiwanese population. J Pain Symptom Manage 1999;18(5):316-22.Search in Google Scholar
[35] Keller S, Bann CM, Dodd SL, Schein J, Mendoza TR, Cleeland CS. Validity of the brief pain inventory for use in documenting the outcomes of patients with noncancer pain. Clin J Pain 2004;20(5):309-18.Search in Google Scholar
[36] Tan G, Jensen MP, Thornby JI, Shanti BF. Validation of the Brief Pain Inventory for chronic nonmalignant pain. J Pain 2004;5(2):133-7.Search in Google Scholar
[37] Yun YH, Mendoza TR, Heo DS, Park HA, Shin HC, Wang XS, Cleeland CS. Development of a cancer pain assessment tool in Korea: a validation study of a Korean version of the brief pain inventory. Oncology 2004;66(6):439-44.Search in Google Scholar
[38] Gunnarsdottir S, Ward S, Serlin RC. Attitudinal barriers to cancer pain management in the Icelandic population. Cancer Nurs 2008;31(2):95-102.Search in Google Scholar
[39] Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol 1988;54(6):1063-70.Search in Google Scholar
[40] Cella DF. Functional Assessment of Cancer Therapy (F.A.C.T.) Manual. Chicago, IL: Rush-Presbyterian-St. Luke’s Medical Center; 1994.Search in Google Scholar
[41] de Boer AG, van Lanschot JJ, Stalmeier PF, van Sandick JW, Hulscher JB, de Haes JC, Sprangers MA. Is a single-item visual analogue scale as valid, reliable and responsive as multi-item scales in measuring quality of life? Qual Life Res 2004;13:311-20.Search in Google Scholar
[42] Dillman D. Mail and Internet surveys. 2nd ed. New York, NY: John Wiley and Sons; 2000.Search in Google Scholar
[43] Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: new procedures and recommendations. Psychol Methods 2002;7(4): 422-45.Search in Google Scholar
[44] Serlin RC, Mendoza TR, Nakamura Y, Edwards KR, Cleeland CS. When is cancer pain mild, moderate or severe? Grading pain severity by its interference with function. Pain 1995;61(2):277-84.Search in Google Scholar
[45] Réthelyi JM, Berghammer R, Kopp MS. Co-morbidity of pain-associated disability and depressive symptoms in connection to sociodemographic variables: results from a cross-sectional epidemiological survey in Hungary. Pain 2001;93:115-21.Search in Google Scholar
© 2010 Scandinavian Association for the Study of Pain
Articles in the same Issue
- Editorial comment
- Functional brain imaging of acute postoperative pain
- Clinical pain research
- Brain activation due to postoperative pain from the right hand measured with regional cerebral blood flow using positron emission tomography
- Editorial comment
- Long-term low-dose transdermal buprenorphine therapy for chronic noncancer pain
- Original experimental
- A 6-months, randomised, placebo-controlled evaluation of efficacy and tolerability of a low-dose 7-day buprenorphine transdermal patch in osteoarthritis patients naïve to potent opioids
- Editorial comment
- Repeated nociceptive stimulation for detecting drug effects
- Original experimental
- The effects of gabapentin in human experimental pain models
- Editorial comment
- Whether the weather influences pain: High prevalence of chronic pain in Iceland and Norway: Common genes? Or lack of sunshine and vitamin D?
- Observational studies
- A population based study of the prevalence of pain in Iceland
- Editorial comment
- Swedish nurses are prone to chronic shoulder and back pain because of miserable working conditions and poor leadership?
- Observational studies
- Predicting of pain, disability, and sick leave regarding a non-clinical sample among Swedish nurses
- Abstracts
- Trigeminal neuralgia or odontogenic pain
- Abstracts
- What’s wrong with animal models of pain?
- Abstracts
- Immunotherapy for neuroblastoma elicits a complement dependent whole body allodynia
- Abstracts
- Pain mechanisms in animal models of rheumatoid arthritis
- Abstracts
- Translating basic research to pharmacological treatment of neuropathic pain
- Abstracts
- Free Poster Presentations: Forearm heat pain does not inhibit electrically induced tibialis anterior muscle pain
- Abstracts
- Offset analgesia evoked by non-contact thermal stimulator
- Abstracts
- Inhibition of FAAH reverses spinal LTP
- Abstracts
- Hyperexcitable C-nociceptors in human paroxysmal pain
- Abstracts
- Pain sensitivity and experimentally induced sensitization in red haired women
- Abstracts
- How are opioids used in Norway? Persistent use, utilization of depot formulation and age profile in non-palliation patients
- Abstracts
- To which extent does incident and persistent use of weak opioids predict problematic opioid use?
- Abstracts
- Is transdermal buprenorphine for chronic non-malignant pain used long term without co-medication with other potentially addictive drugs?
- Abstracts
- Prostaglandin E2 production in synovial tissue and acute postoperative pain after knee arthroscopy
- Abstracts
- Girl presenting with oesophageal spasm pain after fundoplication
- Abstracts
- Epidemiology of persistent postoperative pain: Association of persistent pain and sensory abnormalities
- Abstracts
- Cost–benefit of a 13-week multidiciplinary rehabilitation course for chronic non-malignant pain patients
- Abstracts
- A novel and effective treatment modality for medically unexplained pain
- Abstracts
- Somatocognitive therapy in the management of chronic gynaecological pain. A review of current approach and historical background
- Abstract
- The Manual Intervention Trial (MINT)—The effect of various combinations of naprapathic manual therapy. The study protocol of a randomized controlled trial
- Abstracts
- The experience of chronic pain, loss and grief
- Abstracts
- Effect of buprenorphine and fentanyl in experimental induced superficial, deep and hyperalgesic pain
- Abstract
- Pretreatment with opioids enhances afferent induced long-term potentiation in the rat dorsal horn
- Abstracts
- Pigs in pain—Porcine behavioural responses towards mechanical nociceptive stimulation directed at the hind legs
- Abstracts
- A human experimental bone pain model
Articles in the same Issue
- Editorial comment
- Functional brain imaging of acute postoperative pain
- Clinical pain research
- Brain activation due to postoperative pain from the right hand measured with regional cerebral blood flow using positron emission tomography
- Editorial comment
- Long-term low-dose transdermal buprenorphine therapy for chronic noncancer pain
- Original experimental
- A 6-months, randomised, placebo-controlled evaluation of efficacy and tolerability of a low-dose 7-day buprenorphine transdermal patch in osteoarthritis patients naïve to potent opioids
- Editorial comment
- Repeated nociceptive stimulation for detecting drug effects
- Original experimental
- The effects of gabapentin in human experimental pain models
- Editorial comment
- Whether the weather influences pain: High prevalence of chronic pain in Iceland and Norway: Common genes? Or lack of sunshine and vitamin D?
- Observational studies
- A population based study of the prevalence of pain in Iceland
- Editorial comment
- Swedish nurses are prone to chronic shoulder and back pain because of miserable working conditions and poor leadership?
- Observational studies
- Predicting of pain, disability, and sick leave regarding a non-clinical sample among Swedish nurses
- Abstracts
- Trigeminal neuralgia or odontogenic pain
- Abstracts
- What’s wrong with animal models of pain?
- Abstracts
- Immunotherapy for neuroblastoma elicits a complement dependent whole body allodynia
- Abstracts
- Pain mechanisms in animal models of rheumatoid arthritis
- Abstracts
- Translating basic research to pharmacological treatment of neuropathic pain
- Abstracts
- Free Poster Presentations: Forearm heat pain does not inhibit electrically induced tibialis anterior muscle pain
- Abstracts
- Offset analgesia evoked by non-contact thermal stimulator
- Abstracts
- Inhibition of FAAH reverses spinal LTP
- Abstracts
- Hyperexcitable C-nociceptors in human paroxysmal pain
- Abstracts
- Pain sensitivity and experimentally induced sensitization in red haired women
- Abstracts
- How are opioids used in Norway? Persistent use, utilization of depot formulation and age profile in non-palliation patients
- Abstracts
- To which extent does incident and persistent use of weak opioids predict problematic opioid use?
- Abstracts
- Is transdermal buprenorphine for chronic non-malignant pain used long term without co-medication with other potentially addictive drugs?
- Abstracts
- Prostaglandin E2 production in synovial tissue and acute postoperative pain after knee arthroscopy
- Abstracts
- Girl presenting with oesophageal spasm pain after fundoplication
- Abstracts
- Epidemiology of persistent postoperative pain: Association of persistent pain and sensory abnormalities
- Abstracts
- Cost–benefit of a 13-week multidiciplinary rehabilitation course for chronic non-malignant pain patients
- Abstracts
- A novel and effective treatment modality for medically unexplained pain
- Abstracts
- Somatocognitive therapy in the management of chronic gynaecological pain. A review of current approach and historical background
- Abstract
- The Manual Intervention Trial (MINT)—The effect of various combinations of naprapathic manual therapy. The study protocol of a randomized controlled trial
- Abstracts
- The experience of chronic pain, loss and grief
- Abstracts
- Effect of buprenorphine and fentanyl in experimental induced superficial, deep and hyperalgesic pain
- Abstract
- Pretreatment with opioids enhances afferent induced long-term potentiation in the rat dorsal horn
- Abstracts
- Pigs in pain—Porcine behavioural responses towards mechanical nociceptive stimulation directed at the hind legs
- Abstracts
- A human experimental bone pain model

