Assessing nutrition literacy and nutrition counseling proficiency following an interdisciplinary culinary medicine elective
-
Anna N. Kirby
, Joy DeBellis
Abstract
Context
Culinary medicine (CM) is a growing field of education that aims to bridge the gap between the clinical need for nutritional counseling and the lack of education on the topic. Healthcare professionals can aid in nutrition-related noncommunicable disease (NCD) prevention by improving a patient’s dietary behavior. However, the presence of nutrition education in healthcare curricula is lacking. Early evidence indicates that CM could address this gap.
Objectives
The objectives of this study are to determine if the provision of an interdisciplinary CM elective will improve student knowledge and confidence with counseling on nutrition and culinary principles, and to improve personal dietary habits of students.
Methods
This was a one-group pretest-posttest quasi-experimental design. First- and second-year osteopathic medical students (OMS) and nurse practitioner students were recruited to participate in a CM elective via email. Participants were excluded if they were not in good academic standing at their respective institutions. Twelve individuals (n=8 medical; n=4 nursing) were enrolled in the course. Participants completed pre- and postcourse surveys to determine changes in nutrition literacy (Nutrition Literacy Assessment Instrument [NLit42]), nutrition counseling proficiency (Nutrition Survey for Family Practitioners), and dietary quality (Automated Self-Administered 24-h dietary assessment tool; ASA24®). A two-sided, paired t test was conducted to determine changes in outcome variables.
Results
All 12 participants completed the precourse assessments, and 8 participants completed the postcourse assessments. Culinary activity attendance was 94.5 %. Participants exhibited a statistically significant increase in their overall nutrition literacy scores after completing the CM elective (p=0.006). Literacy subcategories indicated that the improvement came from the participant’s ability to understand household measurements (p=0.005) better. Increases in self-reported proficiency were observed for participants’ confidence to counsel on nutrition and prevention/wellness (p=0.02) and macronutrients in health and food safety (p=0.01). No statistically significant changes in the personal dietary pattern or quality were observed.
Conclusions
The interdisciplinary CM elective improved nutrition literacy and some aspects of counseling proficiency. Although small shifts in dietary variables were observed, the elective did not statistically improve participants’ dietary pattern. However, some changes that were observed may lead to clinically relevant outcomes if maintained long-term. These findings are encouraging. Implementing CM as an educational tool could improve healthcare practitioners’ ability to understand and counsel patients on nutrition to prevent the nutrition-related NCDs.
The escalating rates of nutrition-related noncommunicable diseases (NCDs), including cardiovascular disease, type 2 diabetes mellitus, and obesity, have become a critical global health concern. NCDs contribute to 74 % of deaths globally and 88 % of deaths nationally [1], underscoring the urgency of effective preventive measures and patient care strategies. The World Health Organization (WHO) identifies high blood pressure, overweight/obesity, hyperglycemia, and hyperlipidemia as key metabolic factors that contribute to the increased risk for NCDs. The 2013–2030 Agenda for Sustainable Development aims to curb the impact of NCDs, particularly in individuals aged 30–70 years old, making primary care a crucial arena to mitigate behavioral risk factors such as poor dietary behavior [2].
Recognizing the pivotal role of interdisciplinary teams in patient care, the importance of nutrition cannot be overstated. Registered dietitians (RDs) play a central role in this context, providing expertise in translating nutritional science into practical solutions. RDs collaborate with other professionals to implement evidence-based nutrition interventions that contribute to overall patient well-being [3]. However, the challenge lies in the broader healthcare landscape where many professionals lack adequate training in foundational nutrition concepts and behavior modification counseling. Over 70 % of medical school graduates surveyed reported that they were not adequately prepared to provide nutritional counseling in a clinical setting [4]. Nurses have noted these same inadequacies and believe that nurse educators and practitioners should gain a contemporary understanding of the relationship between food and health [5]. Physicians and nurses in primary care are the first point of contact for patients, when interventions to prevent nutrition-related NCDs may have the greatest impact [1]. Additionally, they can facilitate referrals to RDs and adherence to nutrition interventions. Accordingly, their preparedness is crucial. However, there is still a shortage of evidence-based healthcare curricula and contact hours related to clinical nutrition that would help prepare these professionals.
Accordingly, a consequence of this curricular gap, which further drives the development of NCDs, is that nutrition is neglected as part of patient care. For instance, only 46 % of fourth-year medical students, compared to their first-year counterparts at 72 %, believe that nutrition counseling has a valuable role in clinical practice [6]. This can partially be attributed to a lack of confidence in counseling among healthcare professionals due to the insufficient knowledge of appropriate nutritional recommendations. In fact, only 50 % of primary care providers report routinely educating their patients on nutrition [7]. Additionally, 97 % of residents admit to the importance of nutrition in patient care, and only 14 % felt prepared to disseminate nutrition information [8]. Further, the gap in nutritional education not only affects patient outcomes, but it also negatively affects healthcare professionals’ own dietary patterns. Less than 15 % of healthcare students meet the recommended fruit, fiber, and vegetable recommendations, while most exceed their saturated fat requirements [9]. Overwhelming evidence suggests that more time and effort should be reallocated to supporting nutrition education and training to help mitigate NCDs in healthcare professionals and the patient population.
Culinary medicine (CM) is a rising field that fuses the art of cooking with evidence-based medicine. The primary goal is to empower patients in choosing accessible and high-quality meals to prevent and treat disease and restore well-being through educating future practitioners [10]. Early evidence supports CM’s utility in developing more accomplished healthcare professionals. This is because CM combines theoretical knowledge with practical skill, which promotes long-term, sustainable changes at the personal and professional levels. Additionally, an important component of CM is that it can incorporate interdisciplinary education. WHO has identified interdisciplinary education as critical for collaborative healthcare practices and the delivery of high-quality care to patients [11]. The objective of this research project is to determine whether implementing a CM elective among medical and nurse practitioner students will increase their nutrition literacy and proficiency in counseling patients. A secondary objective is to determine if the CM elective improves the personal dietary habits of those participating. Improving healthcare providers’ nutrition literacy and personal dietary habits is the first step in increasing the quality and amount of nutritional counseling they can provide [12].
Methods
A one-group pretest-posttest quasi-experimental design was utilized. The study protocol was approved by Auburn University and the Edward Via College of Osteopathic Medicine Institutional Review Board with exempt status (IRB# 21–396 EX 2108). From January to February 2022, first- and second-year osteopathic medical students (OMS) and nurse practitioner students were invited via email to participate in a CM elective. Participants were excluded if they were not within good academic standing at their respective institution. This was a pilot project, and 12 individuals were enrolled in the course. In March 2022, participants were invited to complete an assessment of their nutrition knowledge, proficiency with nutrition counseling, and dietary habits. After completing the pretest, students were sent links to access the CM elective content. Following the completion of the course, participants repeated the assessment.
Culinary medicine elective
The primary aim of the CM course was to enhance knowledge of nutrition and culinary techniques that can be applied at the personal level and as a clinical approach within a patient encounter. The course was entirely online and consisted of six educational modules created by an interdisciplinary team consisting of an RD, physician, nurse and pharmacist. Medical students also contributed to the course development. The module content was developed as a Prezi slide deck with an accompanying detailed outline and pertinent recipes. Each module was followed by a virtual hands-on culinary activity with a case-based discussion. The culinary activities were led by an RD with support from one or more interdisciplinary team members. The module content was centered on nutrition-related health issues that commonly present in underserved rural and urban communities (Table 1). The objectives for each module concentrated on enhancing personal health habits, nutrition knowledge, culinary skills, and patient counseling. Recipes were provided that aligned with the cultural, environmental, and economic experiences faced by underserved community members.
Detailed outline of module content for CM elective.
| Subject matter | Overview |
|---|---|
| Nutritional foundations | This module will provide the terminology and basic concepts of nutrition for those who are completely new to nutrition or those who need to refresh their understanding. |
| Weight management and fad diet | Participants will examine the connection between lifestyle habits, energy balance, and body weight. Common nutrition-related misconceptions will be discussed, and guidance on evidence-based recommendations will be provided. In the kitchen, nutrient-dense, palatable recipes will be explored. |
| Hypertension and flavor profiles | This module will highlight the relationship between renal health and sodium intake. It will focus on methods to maintain flavor profiles in foods commonly consumed. The recipes in this module will focus on seasonings to enhance flavor. |
| Hyperlipidemia | This module will explore the diverse physiologic role that dietary fats play in the body, as well as the culinary role that fats play in the kitchen. The culinary focus will be on fat quality, quantity, and utility in a recipe. |
| Carbohydrates and diabetes mellitus | This module will examine the relationship between glucose dysregulation and dietary carbohydrate quantity and quality. The kitchen focus of this module will be on the incorporation of high-fiber carbohydrates into the dietary pattern. |
| Neurocognition | This module will explore the connection between food and optimal brain function. Recipes in this module will focus on foods shown to be neuroprotective. |
-
CM, culinary medicine.
Culinary activity
Following each module, a virtual hands-on culinary activity was conducted. Participants gathered over Zoom to hold a case-based discussion on module content and to cook recipes associated with the medical condition discussed. Zoom is a video conferencing and online meeting platform that allows individuals and groups to hold virtual meetings, webinars, and video conferences. An RD led the activity while an interdisciplinary team of faculty and peers facilitated the case-based discussion and participated in the meal preparation. Prior to the activity, participants signed up for one of three recipes offered and were provided the corresponding ingredients. Following introductions at the beginning of the activity, participants would be organized into a breakout room with the other individuals cooking the same recipe. While in the breakout room, the facilitator would guide them through cooking the recipe and a patient case discussion. Once the recipe was cooked and the discussion was completed, everyone would return to the main room, where a discussion would be held about the experience and case. Each activity was scheduled for 90 min and allowed participants an opportunity to engage in dialogue about nutrition-related disease states and treatments with content experts while learning culinary techniques.
Assessment
Participants were asked to complete assessments prior to beginning the course and directly after completing the course. The assessments included three surveys: the Nutrition Literacy Assessment Instrument (NLit), the Nutrition Survey for Family Practitioners, and the Automated Self-Administered 24 h dietary assessment tool (ASA24®). The NLit is a 42-item validated tool to measure nutrition literacy in an adult population with nutrition-related chronic disease [13]. It assesses three domains: numeracy, comprehension, and application/function within the context of nutrition, diabetes, blood pressure, and atherosclerosis. The Nutrition Survey for Family Practitioners is a 31-item self-report questionnaire to determine nutrition proficiency in counseling [14]. Questions were based on 26 core nutrition areas, complementary and alternative medicine, and food safety. The NLit and Nutrition Survey for Family Practitioners were built into Qualtrics (Qualtrics, Provo, UT), an online survey software tool, and a link was distributed to the participants to complete the surveys. The ASA24® is a web-based tool from the National Cancer Institute (NCI) that enables reliable and valid collection of dietary recalls [15]. The survey allows participants to record their food consumption and eating habits over a period of 24 h. Participants completed the ASA24® on two nonconsecutive days prior to beginning the course and following the course. From the ASA24®, a score for Healthy Eating Index (HEI) was determined. The HEI is an assessment of an individual’s adherence to the dietary pattern of the Dietary Guidelines for Americans (DGAs). The score is based on a 100-point scale (0=no adherence, 100=perfect adherence) calculated from separate food component scores (i.e., total fruit, whole fruits, total vegetables, greens and beans, whole grains, dairy, total protein foods, seafood and plant proteins, fatty acids, refined grains, sodium, added sugars, and saturated fat). This measure gives an indication of diet quality [16].
Statistical analysis
Each NLit question answered correctly was worth 1 point out of a possible 42. Individuals who scored ≤28 exhibited a likelihood of poor nutrition literacy, 29–38 exhibited a possibility of poor nutrition literacy, and ≥39 exhibited a likelihood of good nutrition literacy. Pre- and post-course NLit scores were utilized to determine changes in knowledge from baseline utilizing a two-tailed, paired t test analysis. The Nutrition Survey for Family Practitioners measured proficiency and comfort with counseling on a 3-point Likert scale (1=“not proficient”; 2=“somewhat proficient”; 3=“totally proficient”). All Likert data were transformed to a numerical scale for analysis. Paired sample t tests were conducted to determine changes in the level of confidence with nutrition counseling from baseline. Participants completed the ASA24® on two nonconsecutive days at baseline and at completion of the course. An average for each variable was generated and the HEI score was calculated at each time point. Wilcoxon signed-rank tests were conducted to determine changes in HEI score, energy, total fat, unsaturated fat, carbohydrate, potassium, sodium, saturated fat, and fiber due to the small number of participants. All statistical analyses were performed in SPSS and SigmaPlot with significance determined at p≤0.05.
Results
Overall, 12 participants enrolled in the course. Eight participants completed all the assessments before and after the course. Of those eight, seven were female (87.5 %), and one was male (12.5 %). Three were in their first year of medical school (37.5 %), four were in their second year of medical school (50 %), and one was a nurse practitioner student (12.5 %). The mean age of participants was 26.6 years old (standard deviation [SD]=3.5). Attendance for the culinary activities was 94.5 %.
Nutrition literacy
Participants exhibited a statistically significant increase in overall literacy score after completing the CM elective (M=34.9, SD=2.2 vs. M=37.0, SD=1.3; p=0.03; Figure 1). When assessing each subcategory, there was a statistically significant improvement in the ability to understand household measurements (M=3.8, SD=1.3 vs. M=5.0, SD=0.9; p=0.02). No other subcategories revealed statistically significant changes in nutrition literacy.
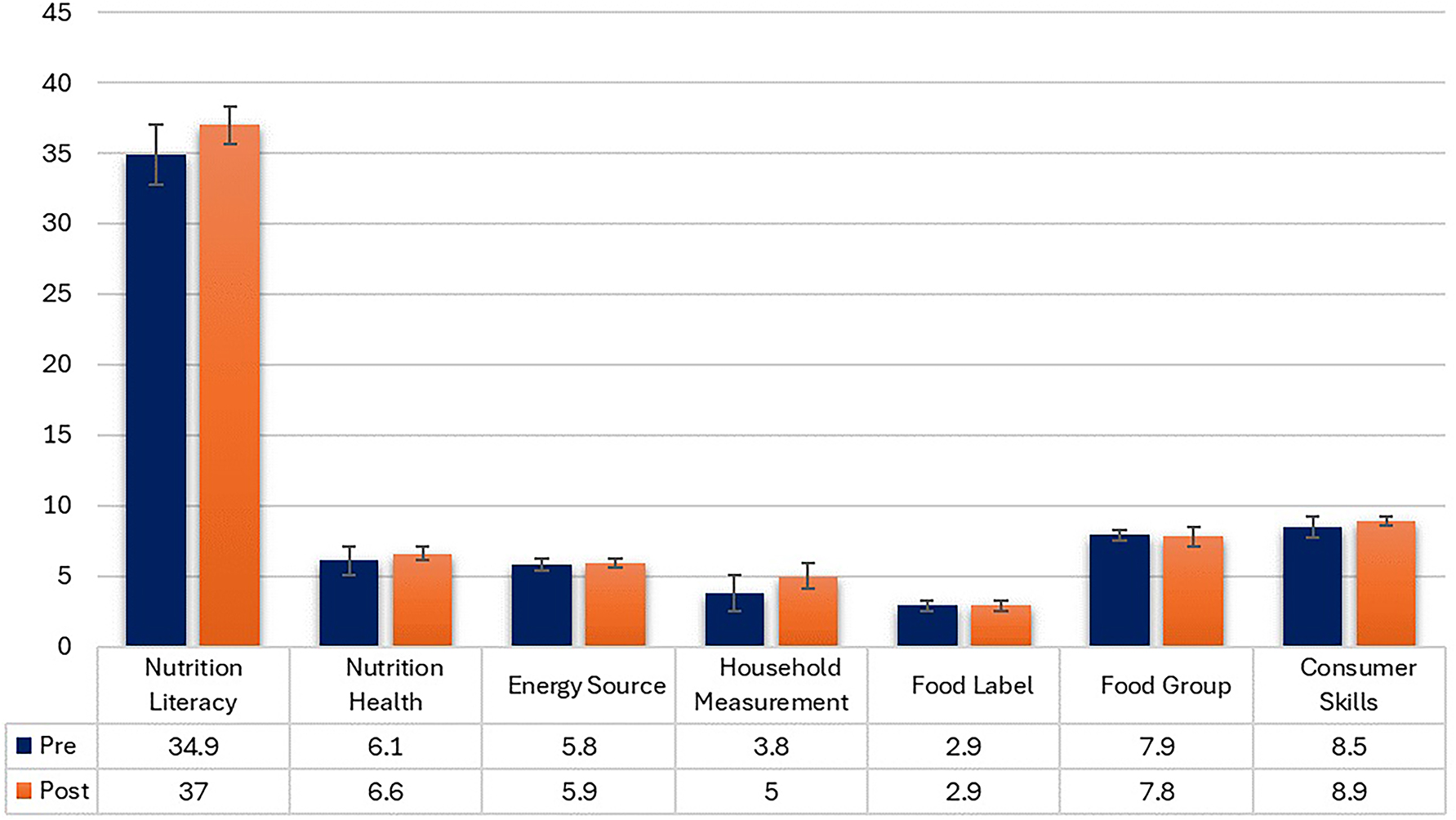
Completing an interdisciplinary CM elective did increase participants overall nutritional literacy as well as their knowledge of household measurements. (*, p≤0.05). The maximum possible total score for the NLit is 42. The maximum possible score for each subcategory is as follows: Nutrition and Health, 7; Energy Source, 6; Household Measurement, 6; Food Label and Numeracy, 6; Food Groups, 8; Consumer Skills, 9.
Nutrition counseling proficiency
Participants did not report a statistically significant increase in overall proficiency after completing the CM elective (M=2.3, SD=0.2 vs. M=2.4, SD=0.4; p=0.36). However, an assessment of subcategories revealed a statistically significant increase in participants’ proficiency to counsel on nutrition and prevention/wellness (M=2.1, SD=0.3 vs. M=2.6, SD=0.4; p=0.03) and macronutrients in health and food safety (M=2.0, SD=0.2 vs. M=2.6, SD=0.3; p=0.03). Figure 2 illustrates percentages of proficiency (i.e., not proficient, somewhat proficient, and totally proficient) across subcategories before and after the CM elective. Prior to the course, an average of 13 % of participants reported being totally proficient with items in the counseling on nutrition and prevention/wellness category, while an average of 63 % reported being totally proficient following the course. Similarly, an average of 20 % of participants reported being totally proficient at the items in the counseling on macronutrients in health and food safety subcategory prior to the course, while an average of 63 % felt totally proficient after the course. While there were no statistically significant changes in the other subcategories, there was a decrease in the not-proficient answers across all subcategories by an average of 21 %. Additionally, there was an increase in the totally proficient answers across all subcategories by an average of 42 %. Although not all the results were statistically insignificant, there was a consistent trend that participants were gaining proficiency.
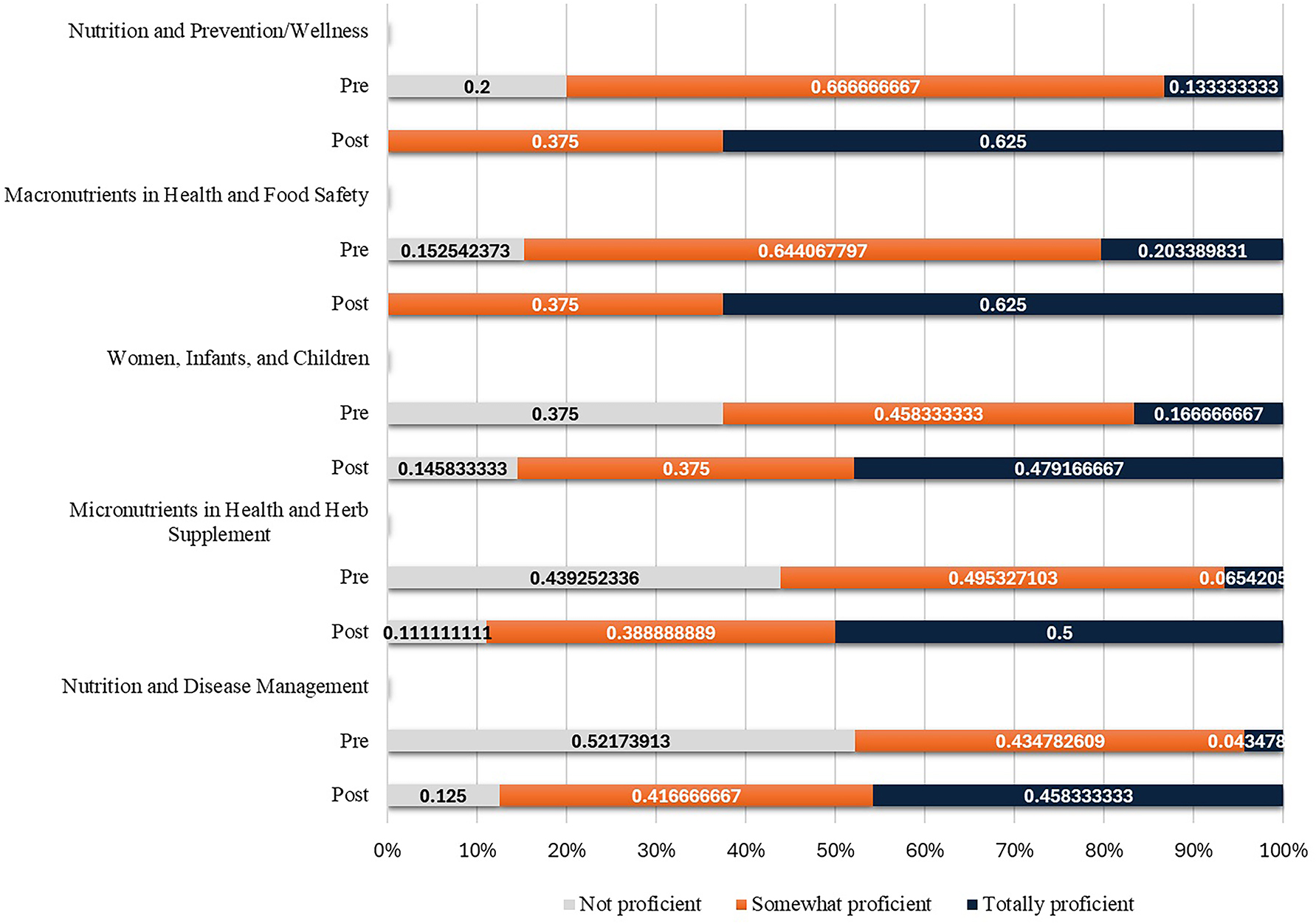
Nutrition counseling proficiency increased following the CM elective for subcategories nutrition and prevention/wellness (p=0.02) and macronutrients in health and food safety (p=0.01).
Personal dietary habits
No statistically significant changes in personal dietary intake or quality were observed (Table 2). Participants’ HEI scores stayed consistent across the course (M=58.3, SD=16.4 vs. M=58.6, SD=14.8; p=0.93). An assessment of total energy intake revealed an average decrease of 307 kcals following the CM elective (M=2,306.5, SD=653.1 vs. M=1999.6, SD=779.5, p=0.33). Decreases in grams of protein (M=93.7, SD=21.9 vs. M=87.3, SD=35.6, p=0.79), total fat (M=111.1, SD=47.3 vs. M=89.0, SD=41.2, p=0.42), and carbohydrate (M=234.2, SD=94.4 vs. M=213.9, SD=98.1 p=0.42) were observed. The mean latencies for grams of fiber before and after the CM course were 24.5 (SD=13.3) and 20.2 (SD=9.5), respectively (p=0.16). The mean latencies in grams of saturated fat before and after the CM course were 37.3 (SD=24.3) and 26.5 (SD=17.4), respectively (p=0.37). A reduction in grams of unsaturated fat intake (M=64.2, SD=28.6 vs. M=55.0, SD=21.6, p=0.48) was observed, along with small reductions in milligrams of potassium (M=2,926.3, SD=1,113.9 vs. M=2,532.3, SD=900.0, p=0.18) and sodium (M=3,707.6, SD=1,143.9 vs. M=3,487.5, SD=920.0, p=0.72).
Changes in HEI score, macronutrients, and micronutrients were observed after the conclusion of the course.
| Variables | Premean | Postmean | p-Value |
|---|---|---|---|
| HEI score | 58.3 | 58.6 | 0.93 |
| Total energy, kcal | 2,306.5 | 1999.6 | 0.33 |
| Protein, g | 93.7 | 87.3 | 0.79 |
| Carbohydrate, g | 234.2 | 213.9 | 0.42 |
| Total fat, g | 111.1 | 89.0 | 0.42 |
| Saturated fat, g | 37.3 | 26.5 | 0.37 |
| Unsaturated fat, g | 64.2 | 55.0 | 0.48 |
| Sodium, mg | 3,707.6 | 3,487.5 | 0.72 |
| Potassium, mg | 2,926.3 | 2,532.3 | 0.18 |
| Fiber, g | 24.5 | 20.2 | 0.16 |
-
HEI, Healthy Eating Index.
The macronutrient distribution for all participants before and after the course is shown in Figure 3. Carbohydrate consumption increased from 53 % of total calories to 55 %. Total fat decreased from 25 % of total calories to 23 %. This decrease can be attributed to decreases in saturated fat from 9 % of total calories to 8 % and in unsaturated fat from 17 to 15 %. Protein stayed constant at 22 % of total calories. However, these changes were not statistically significant.
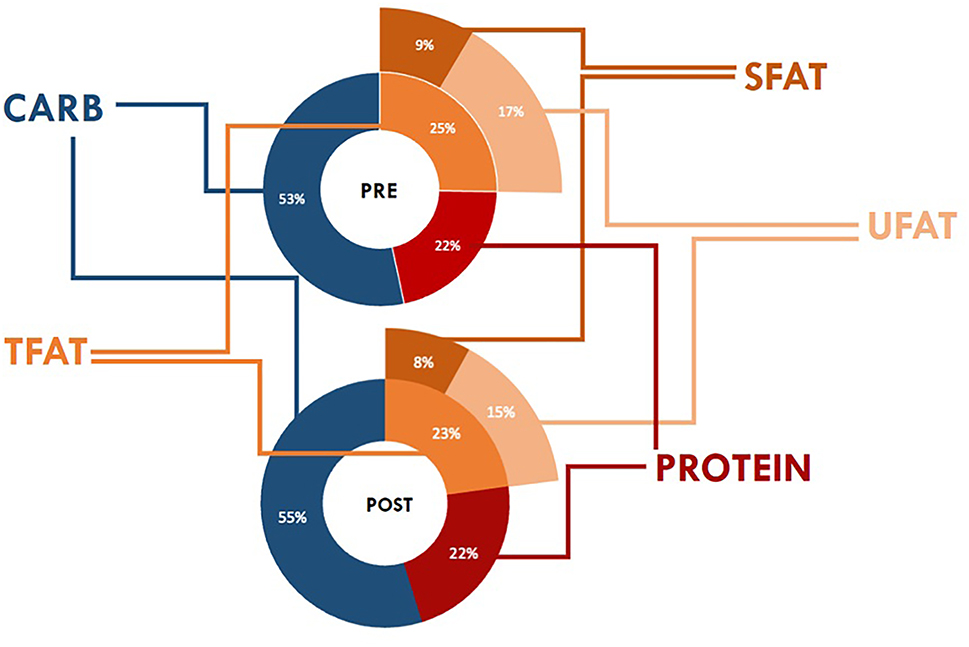
Small shifts in the percentage of total calories for carbohydrates, total fat, saturated fat, and unsaturated fat were observed. The percentage of total calories from protein did not change. SFAT, saturated fat; TFAT, total fat; UFAT, unsaturated fat.
Discussion
The recent Summit on Medical Education in Nutrition, hosted by the Accreditation Council for Graduate Medical Education (ACGME), in response to the White House Conference on Hunger, Nutrition, and Health, underscored the deficiency in integrated nutrition education within medical training. Recognizing this gap, the ACGME summit emphasized the potential role of CM as a solution [17]. CM electives, deemed innovative, serve as a practical avenue to empower medical providers with the skills needed for evidence-based nutritional counseling, aligning with the imperative to enhance nutritional knowledge across the continuum of medical education. Increasing counseling may lead to a decreased overall prevalence of NCDs, which contribute to many deaths worldwide [1]. CM shows promise as an impactful educational strategy among healthcare students for increasing counseling proficiency, promoting familiarity with evidence-based nutrition interventions, and augmenting understanding of the role of interprofessional engagement in addressing lifestyle-related diseases [12]. While multiple studies on pilot CM electives have shown increased perceived nutritional knowledge [18], [19], [20], very few have utilized assessments to numerically evaluate participants. Therefore, examining literacy scores, along with self-reported nutrition counseling proficiencies and dietary patterns following an experiential educational activity, may be a useful gauge of the effectiveness of CM in healthcare training. Following the 6-module CM elective, overall literacy was increased and there was enhanced self-reported proficiency in counseling on nutrition and prevention/wellness and macronutrients in health. The quantitative results of this study support and strengthen the previous findings of pilot CM courses across the country. Moreover, the findings of this research bear notable relevance to osteopathic medicine, emphasizing the crucial contribution of CM electives in enhancing the proficiency of healthcare practitioners in evidence-based nutritional counseling. This aligns seamlessly with the fundamental principles of osteopathic medicine, highlighting the body’s inherent capacity for healing and the paramount importance of nutrition in promoting overall health maintenance.
Nutritional literacy and counseling proficiency are both important factors in the ability of a healthcare practitioner to improve the diet quality of patients. Therefore, CM’s ability to improve overall nutrition literacy elicits an important clinical role in decreasing NCDs [21]. The significant improvement in understanding of household measurements is encouraging due to the strong correlation between portion sizes, excessive caloric intake, and obesity [22]. The statistically insignificant score changes in the assessment of nutritional foods, energy sources, consumer skills, label reading, and food groups can likely be attributed to the small sample size and the high pre-assessment scores (at or above >90 %). Although self-reported proficiency with counseling increased in certain subcategories like nutrition and wellness/prevention and macronutrients in health, the insignificant scores in other subcategories (i.e., nutrition for women and infants, micronutrients, and nutrition and disease) indicate that expansion of the module content is needed. Further focus on nutrition principles specific to certain populations and augmenting the content covering chronic diseases may be beneficial.
Some professional programs have implemented CM curricula to help improve health literacy and nutrition counseling, but few have reported on the effect on the personal diet quality and dietary habits of participants. The use of the ASA24® and HEI helped address this gap. The HEI score for participants exposed a suboptimal dietary quality. These findings are important because improvements in diet quality have been shown to decrease NCDs [23]. However, healthcare professionals who themselves have deficient dietary habits will not likely invoke strong self-efficacy in their patient population. Further, no significant dietary changes were noted in those who participated in the elective. However, if the small shifts in variables like total energy intake were sustained over time, they would elicit a clinically relevant effect. These results support the understanding that a lack of nutritional education may contribute to the poor dietary habits of healthcare students. The concern is that this may translate to clinical practice.
Limitations of this study included a small sample size and the use of a subjective survey for the nutrition counseling proficiency section. These factors may have contributed to skewed response data. As the CM elective continues to garner participation and the sample size of participants increases, the upward trends in nutritional literacy, proficiency, and personal dietary habits may become statistically significant. In addition, a new objective survey method can be implemented for measuring nutrition counseling proficiency, allowing for stronger data collection and more reliable results. Another distinct challenge included the recruitment for students enrolled in the nurse practitioner program. Many of these nursing students maintain either full- or part-time employment concurrently with their studies, thereby constraining their capacity to participate in extracurricular activities. In the forthcoming iterations of this course, emphasis will be placed on attracting nursing students with more flexible schedules to address this impediment effectively. Additionally, plans are underway to include a broader range of healthcare disciplines in the course, with the second iteration of the course including medical, nursing, pharmacy, and nutrition students to enrich the interdisciplinary scope.
Conclusions
A critical barrier to the inclusion of diet as a tool in medicine is the lack of knowledge and confidence with counseling in both physicians and nurses. From an osteopathic standpoint, emphasizing a holistic approach is crucial. Providing lifestyle counseling is essential, and recognizing the need for a referral to an RD for specialized nutrition guidance supports patients in making impactful lifestyle changes. Furthermore, nurses are frontline healthcare professionals positioned to amplify and reinforce the nutritional approach guiding each patient’s care. It is incumbent across all healthcare disciplines to provide unified messaging to patients. This study demonstrates the positive effect that CM electives have on the nutrition literacy and counseling proficiency of healthcare practitioner students. These findings could translate to enhanced nutritional counseling and a food-forward focus in a patient encounter, thereby ameliorating contemporary clinical practice.
-
Research ethics: The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and the study protocol was approved by Auburn University and the Edward Via College of Osteopathic Medicine Institutional Review Board with exempt status (IRB# 21-396 EX 2108).
-
Informed consent: An information letter was used to notify the participants about the project details and participation in the surveys indicated consent.
-
Author contributions: The authors have accepted responsibility for the entire content of this manuscript and approved its submission. AK, JD, JB, JB, CC, KK, KW, GM, KW, and CW provided substantial contributions to the conception and design as well as the acquisition of data. NN, AK, CC, and CW provided contributions to the analysis and interpretation of data; GM, JD, KW, CW, NN, JB, JB, CC, KW and AK drafted the article or revised it critically for important intellectual content; AK gave final approval of the version of the article to be published; and all authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
-
Competing interests: None declared.
-
Research funding: The current study was funded through the Research Eureka Accelerator Program (REAP) via the Edward Via College of Osteopathic Medicine.
-
Data availability: The raw data can be obtained on request from the corresponding author.
References
1. Budreviciute, A, Damiati, S, Sabir, DK, Onder, K, Schuller-Goetzburg, P, Plakys, G, et al.. Management and prevention strategies for non-communicable diseases (NCDs) and their risk factors. Front Public Health 2020;8:574111. https://doi.org/10.3389/fpubh.2020.574111.Search in Google Scholar PubMed PubMed Central
2. United States of America. Noncommunicable diseases (NCD) risk profiles; 2018. Published online https://www.who.int/nmh/countries/usa_en.pdf [Accessed 27 May 2021].Search in Google Scholar
3. Mitchell, LJ, Ball, LE, Ross, LJ, Barnes, KA, Williams, LT. Effectiveness of dietetic consultations in primary health care: a systematic review of randomized controlled trials. J Acad Nutr Diet 2017;111:1941–62. https://doi.org/10.1016/j.jand.2017.06.364.Search in Google Scholar PubMed
4. Frantz, DJ, McClave, SA, Hurt, RT, Miller, K, Martindale, RG. Cross-sectional study of U.S. Interns’ perceptions of clinical nutrition education. J Parenter Enteral Nutr 2016;40:529–35. https://doi.org/10.1177/0148607115571016.Search in Google Scholar PubMed
5. Simon, K, DeBrew, J. Assessing food insecurity: what nurses should know. Nursing 2021;51:17–9. https://doi.org/10.1097/01.NURSE.0000734036.21689.cd.Search in Google Scholar PubMed
6. Spencer, EH, Frank, E, Elon, LK, Hertzberg, VS, Serdula, MK, Galuska, DA. Predictors of nutrition counseling behaviors and attitudes in US medical students. Am J Clin Nutr 2006;84:655–62. https://doi.org/10.1093/ajcn/84.3.655.Search in Google Scholar PubMed
7. Smith, AW, Borowski, LA, Liu, B, Galuska, DA, Signore, C, Klabunde, C, et al.. U.S. primary care physicians’ diet-physical activity–, and weight-related care of adult patients. Am J Prev Med 2011;41:33–42. https://doi.org/10.1016/j.amepre.2011.03.017.Search in Google Scholar PubMed PubMed Central
8. Vetter, ML, Herring, SJ, Sood, M, Shah, NR, Kalet, AL. What do resident physicians know about nutrition? An evaluation of attitudes, self-perceived proficiency and knowledge. J Am Coll Nutr 2008;27:287–98. https://doi.org/10.1080/07315724.2008.10719702.Search in Google Scholar PubMed PubMed Central
9. Bergeron, N, Al-Saiegh, S, Ip, EJ. An analysis of California pharmacy and medical students’ dietary and lifestyle practices. Am J Pharmaceut Educ 2017;81:5956. https://doi.org/10.5688/ajpe5956.Search in Google Scholar PubMed PubMed Central
10. La Puma, J. What is culinary medicine and what does it do? Popul Health Manag 2015;19:1–3. https://doi.org/10.1089/pop.2015.0003.Search in Google Scholar PubMed PubMed Central
11. World Health Organization. Framework for action on interprofessional education and collaborative practice. Geneva, Switzerland; 2010. Available from: http://who.int/hrh/nursing_midwifery/en/.Search in Google Scholar
12. Magallanes, E, Sen, A, Siler, M, Albin, J. Nutrition from the kitchen: culinary medicine impacts students’ counseling confidence. BMC Med Educ 2021;21:88. https://doi.org/10.1186/s12909-021-02512-2.Search in Google Scholar PubMed PubMed Central
13. Gibbs, HD, Ellerbeck, EF, Gajewski, B, Zhang, C, Sullivan, DK. The nutrition literacy assessment instrument is a valid and reliable measure of nutrition literacy in adults with chronic disease. J Nutr Educ Behav 2018;50:247–57.e1. https://doi.org/10.1016/j.jneb.2017.10.008.Search in Google Scholar PubMed PubMed Central
14. Mihalynuk, TV, Scott, CS, Coombs, JB. Self-reported nutrition proficiency is positively correlated with the perceived quality of nutrition training of family physicians in Washington State. Am J Clin Nutr 2003;77:1330–6. https://doi.org/10.1093/ajcn/77.5.1330.Search in Google Scholar PubMed
15. Park, Y, Dodd, KW, Kipnis, V, Thompson, FE, Potischman, N, Schoeller, DA, et al.. Comparison of self-reported dietary intakes from the automated self-administered 24-h recall, 4-d food records, and food-frequency questionnaires against recovery biomarkers. Am J Clin Nutr 2018;107:80–93. https://doi.org/10.1093/ajcn/nqx002.Search in Google Scholar PubMed PubMed Central
16. Krebs-Smith, SM, Pannucci, TE, Subar, AF, Kirkpatrick, SI, Lerman, JL, Tooze, JA, et al.. Update of the Healthy eating index: HEI 2015. J Acad Nutr Diet 2018;118:1591–602. https://doi.org/10.1016/j.jand.2018.05.021.Search in Google Scholar PubMed PubMed Central
17. Holton, L, Hitchell, KS, Surdyk, PM, Combes, JR. ACGME summit on medical education in nutrition develops guidance for educators on improving education in nutrition. J Grad Med Educ 2023;15:759–61. https://doi.org/10.4300/JGME-D-23-00801.1.Search in Google Scholar PubMed PubMed Central
18. McClafferty, H, Brown, OW, Vohra, S, Bailey, ML, Becker, DK, Culbert, TP, et al.. Section on integrative medicine; committee on practice and ambulatory medicine; section on integrative medicine. Physician health and wellness. Pediatrics 2014;134:830–5. https://doi.org/10.1542/peds.2014-2278.Search in Google Scholar PubMed
19. Johnston, EA, Arcot, A, Meengs, J, Dreibelbis, TD, Kris-Etherton, PM, Wiedemer, JP. Culinary medicine for family medicine residents. Med Sci Educ 2021;31:1015–8. https://doi.org/10.1007/s40670-021-01283-1.Search in Google Scholar PubMed PubMed Central
20. Asano, S, Jasperse, AE, Schaper, DC, Foster, RW, Griffith, BN. A culinary medicine elective course incorporating lifestyle medicine for medical students. Med Sci Educ 2021;31:1343–9. https://doi.org/10.1007/s40670-021-01310-1.Search in Google Scholar PubMed PubMed Central
21. Rothman, JM, Bilici, N, Mergler, B, Schumacher, R, Mataraza-Desmond, T, Booth, M, et al.. A culinary medicine elective for clinically experienced medical students: a pilot study. J Alternative Compl Med 2020;26:636–44. https://doi.org/10.1089/acm.2020.0063.Search in Google Scholar PubMed
22. Spronk, I, Kullen, C, Burdon, C, O’Connor, H. Relationship between nutrition knowledge and dietary intake. Br J Nutr 2014;111:1713–26. https://doi.org/10.1017/S000711451400008720.Search in Google Scholar
23. Cheng, J, Liang, HW, Klem, ML, Costacou, T, Burke, LE. Healthy eating index diet quality in randomized weight loss trials: a systematic review. J Acad Nutr Diet 2023;123:117–43. https://doi.org/10.1016/j.jand.2022.08.114.Search in Google Scholar PubMed PubMed Central
© 2024 the author(s), published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Frontmatter
- Medical Education
- Original Article
- Assessing nutrition literacy and nutrition counseling proficiency following an interdisciplinary culinary medicine elective
- Neuromusculoskeletal Medicine (OMT)
- Original Article
- Investigating Fryette’s mechanics in computed tomography scans: an analysis of vertebrae spinal physiology using open-sourced datasets and three-dimensional vertebral orientation
- Review Article
- Effect of manual manipulation on mechanical gait parameters
- Obstetrics and Gynecology
- Original Article
- The impact of prepregnancy body mass index on pregnancy and neonatal outcomes
- Public Health and Primary Care
- Original Article
- Associations of clinical personnel characteristics and telemedicine practices
- Clinical Image
- Davener’s dermatosis: a unique presentation of frictional hypermelanosis
- Letters to the Editor
- Fostering a research culture in osteopathic medical education
- Response to “Fostering a research culture in osteopathic medical education”
- Corrigendum
- Corrigendum to: A superficial dissection approach to the sphenopalatine (pterygopalatine) ganglion to emphasize osteopathic clinical relevance
Articles in the same Issue
- Frontmatter
- Medical Education
- Original Article
- Assessing nutrition literacy and nutrition counseling proficiency following an interdisciplinary culinary medicine elective
- Neuromusculoskeletal Medicine (OMT)
- Original Article
- Investigating Fryette’s mechanics in computed tomography scans: an analysis of vertebrae spinal physiology using open-sourced datasets and three-dimensional vertebral orientation
- Review Article
- Effect of manual manipulation on mechanical gait parameters
- Obstetrics and Gynecology
- Original Article
- The impact of prepregnancy body mass index on pregnancy and neonatal outcomes
- Public Health and Primary Care
- Original Article
- Associations of clinical personnel characteristics and telemedicine practices
- Clinical Image
- Davener’s dermatosis: a unique presentation of frictional hypermelanosis
- Letters to the Editor
- Fostering a research culture in osteopathic medical education
- Response to “Fostering a research culture in osteopathic medical education”
- Corrigendum
- Corrigendum to: A superficial dissection approach to the sphenopalatine (pterygopalatine) ganglion to emphasize osteopathic clinical relevance

