Person-centered language and pediatric ADHD research: a cross-sectional examination of stigmatizing language within medical literature
-
Kristyn Robling
, Caitlin Cosby
Abstract
Context
Attention-deficit/hyperactivity disorder (ADHD) is one of the most common neurodevelopmental disorders in children and often goes untreated. A major barrier to treatment is the stigma surrounding the disorder, including from the educational and scientific community. Person-centered language (PCL) is associated with positive health outcomes, and its implementation is recommended by multiple professional groups, but its use has not been quantified for ADHD.
Objectives
The goal of this study is to quantify the adherence to PCL among ADHD-related journal publications utilizing a cross-sectional study design.
Methods
We conducted a cross-sectional examination including a systematic search of PubMed, which encompasses MEDLINE, for ADHD-related articles from January 2014 to March 2021. All journals with at least 20 ADHD-related search returns, human research, and in the English language were included, totaling 5,308 articles from 88 journals. Articles were randomized, and the first 500 were screened for inclusion of prespecified, non-PCL terminology. After exclusion, 311 articles were retained.
Results
Of the 311 retained articles, 131 (42.1%) adhered to PCL guidelines. Among articles with non-PCL, stigmatizing language such as “problem(s) with [the/a] child or problem child” and “suffers from” was found most frequently— occurring in 47.6% (148/311) and 5.8% (18/311) of the articles, respectively. We found no significant association between PCL adherence and study characteristics.
Conclusions
Our findings revealed that over half of the current ADHD literature did not adhere to PCL guidelines. Adherence to PCL by the scientific and medical community will increase the overall efforts to mitigate stigma and increase support for individuals with ADHD.
Attention-deficit/hyperactivity disorder (ADHD), a neurodevelopmental disorder that often persists into adulthood [1], is associated with inattention, hyperactivity, and impulsivity, and affects an estimated 8.4% of children in the United States [2]. ADHD and its symptoms may lead to developmental delays in academic and personal settings [3]. Further, childhood ADHD is often perceived as less serious than adult ADHD and, consequently, is less likely to be viewed as requiring treatment. For parents who are willing to pursue treatment for their child, the common medications prescribed may be ineffective in as many as 20% of patients [4, 5]. Due to symptoms of ADHD and these delays, children with ADHD often face stigma early on and throughout their adolescent years [4], which may lead to poorer mental health, self-esteem, and quality of life [6].
Internalized stigma, especially among children after being diagnosed with ADHD, may become a self-fulfilling prophecy because they see themselves with a disorder of academic performance or anger and aggression rather than a mental health diagnosis that has treatment options [7]. In turn, many kids may fear being labeled or want to hide their diagnosis from their peers in order to avoid feeling less favored as friends by peers and acknowledged as highly disturbing in the class environment [8]. In a previous study of 103 children to compare the approval of peers with various conditions, it was found that those who are around another child diagnosed with ADHD judge them more negatively than healthy children and children with other conditions [9]. This is potentially reinforced by the lack of knowledge that professionals have in diagnosing ADHD [10], and by the societal portrayal of ADHD in the media with children with ADHD often being labeled as “disobedient” or “delinquent”—lacking the ability to be quiet or still for even a short period of time or failing academically—and thereby obscuring the true disease burden of ADHD [11]. These stereotypes, labels, and derogatory language lack medical specificity and create barriers for children within academic settings and society at large, and may also lead parents not seeking help for children who may have ADHD. This implicit bias—which is an unconscious stereotype based on common experience [12] —and the use of negative, stigmatizing language, may exacerbate health care disparities, promote isolation, and influence future healthcare practitioners [12], [13], [14].
To overcome these barriers, a movement arose in the 1970s by a prominent group of psychology researchers that focused on advocating for those with disorders. This movement sought to erase the stigma centered around individuals with disorders by shifting the focus from impairment to celebrating what makes each individual unique [15] and to dissuade the use of stigmatizing language within psychological research. This resulted in a shift toward person-centered language (PCL), which was later adopted by the American Psychological Association (APA) in 1992 [16]. PCL places an emphasis on the person—acknowledging the person and their beliefs—while acknowledging their condition secondarily, and appropriately, thus reducing stigma [17]. Therefore, the use of PCL by clinicians and researchers reveals the recognition of individuals beyond a diagnosis, which may encourage the pursuit of care [18]. The American Medical Association further defined PCL criteria and adopted its use in their Manual of Style (AMAMS) in 2007 [19]. There is little evidence to support specific PCL language for children with ADHD, but we hope that our examination will shed light on some of the language utilized and start a conversation on the proper terms to be utilized in the future. As stigma remains prevalent, especially surrounding children with ADHD [20], we sought to quantify adherence to PCL in accordance with the AMAMS-defined criteria [21] in research journals that most frequently publish pediatric literature focused on ADD and ADHD by examining a variety of articles published across different journals. Given the low rates of PCL adherence in previous studies investigating mental health conditions [22, 23], we hypothesized that we would find a similar prevalence of adherence to PCL guidelines in the pediatric ADHD literature. As a secondary objective, we examined the journal’s guidelines for authors to determine if PCL is a requirement for article submission.
Methods
Journal selection and publication randomization and reduction
Two authors (MH and SG) conducted a systematic search utilizing a cross-sectional study design via PubMed (which encompasses MEDLINE) on March 8, 2021, utilizing an adapted, previously published search string [24]: ((“attention deficit disorder with hyperactivity”[MeSH Terms] OR (“attention” [All Fields] AND “deficit” [All Fields] AND “disorder” [All Fields] AND “hyperactivity” [All Fields]) OR “attention deficit disorder with hyperactivity” [All Fields] OR “ADHD” [All Fields]) OR “ADDH” [All Fields]) OR “ADHD” [All Fields]) OR “attention deficit” [All Fields] OR “brain dysfunction” [All Fields]) AND (“humans” [MeSH Terms] AND “English” [Language] AND (“infant” [MeSH Terms] OR “child” [MeSH Terms] OR “adolescent” [MeSH Terms]))) AND (2014:2021[PDAT]). We chose to search PubMed because it is one of the most widely utilized, publicly accessible platforms for biomedical literature [25].
Studies published between January 1, 2014 and March 7, 2021 were filtered, following the publication of the DSM-5 [26] in May 2013—subsequent to the inclusion of PCL guidelines in the AMAMS [19]. Journals were selected for inclusion to retrieve the most frequent sample research focused on ADHD if they have at least 20 search returns from the search strategy. This process has been utilized in multiple studies as a way to glean the journals that most often publish content on the topic of interest that researchers and healthcare professionals in that field are likely to encounter [23, 27, 28].
Google Sheets were utilized for screening and extraction purposes for the randomized search returns. Articles were included in our study if they were original research articles, including research letters, brief reports, case reports, and editorials focused on ADHD pertaining to humans. Studies focused on animal modeling or genetics (which did not address human subjects or populations) and studies not in English were excluded. Only studies published in English were included because PCL guidelines within the AMAMS may not be translatable to other languages. Separate Google Sheets were utilized by two authors (CC and KR) to conduct screening and data procedures in a masked manner until data from 300 articles had been extracted. The investigators were unmasked to meet and verify that there were no discrepancies between the two data sets. They then went through each article that did not match, and they came to an agreement on how each article should be classified. All discrepancies were resolved by revisiting the manuscript text and making changes so that 100% agreement was reached. Data collection was completed on July 1, 2021.
Data extraction
For our primary research question, we assessed adherence to or deviance from guidelines presented in the AMAMS [21]: The AMAMS promotes putting the person first by utilizing person-first language (i.e., avoidance of labels), emotive language (i.e., suffers from, problems with, afflicted by), and euphemistic descriptions of individuals. We systematically searched for the following terms, partial terms, and phrases in conformity with the AMAMS along with the following words identified in the previously published literature that were emotive or had negative connotations [29, 30]: “gifted,” “odd,” “eccentric,” “abnormal,” “retardation,” “sick,” “unstable,” “challenging,” “talkative,” “disturbed,” “difficult*” (“difficult child” or “child is difficult”; not has difficulties with x or y), “crazy,” “disabled,” “mental” (“mental patient”; “mentally ill”; “mental illness”), “spastic,” “suffer*” (“sufferer”; “suffers from”), “problem” (“problems with”; “problem child”) (where “problems with” refers to an individual having “problems with” a child who has ADHD, not a child having “problems with” concentration/attentiveness/etc.), and “afflicted” (with/by). We did not include non-PCL that was included within direct quotes from participants within studies.
The article-level elements extracted were: (1) type of article: original (full) article (including brief report or research letters), case reports, or editorial; (2) type of research: systematic review, clinical trial, cross-sectional, etc; (3) type of intervention (pharmacologic, nonpharmacologic, or no treatment); (4) employment type of first and last author: private, public, or government; and (5) funding statement/source. We defined “government” employment as one associated with a governmental organization, “private” as associated with for-profit organizations with no federal funding, and “public” as employment being within a nonprofit organization or university.
Data analysis
We reported the following: (1) total number of journals and articles from the PubMed searches; (2) number of journals included in our investigation; (3) number of studies that were screened; and (4) number of studies that were included based on the eligibility criteria from each selected journal. Articles including one or more of the labels or terminology listed above were coded as not adherent to the PCL guidelines. Utilizing publications from January 1, 2014 to March 7, 2021, we calculated the proportion of articles without deviance from the AMAMS [21] guidelines relevant to PCL compared to the total number of articles in the included study sample. Further, to evaluate the most common forms of deviance from AMAMS guidelines within these articles, we calculated frequencies, percentages, and 95% confidence intervals. We utilized Fisher’s exact tests to identify potential associations between adherence to PCL and the article and journal characteristics listed above. The Type 1 error rate for analyses were set at 0.05, which were performed utilizing STATA 16.1.
Results
Journal reduction and screening
Our systemic search returned a total of 9,353 articles from 1,371 journals. After journals with less than 20 items in the query were removed, 88 journals were retained from January 1, 2014 to March 7, 2021. From the remaining journals, 5,308 combined articles were randomized, and the first 500 were selected for screening. Of these articles, 311 met the inclusion criteria and 189 did not. Articles met the inclusion criteria if they were peer-reviewed and focused on children with ADHD. Articles were excluded if they did not meet the inclusion criteria. Reasons for exclusion included 78 articles about adult populations, 70 articles unrelated to ADHD, and 41 articles not involving human research. This can be found in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Flow Diagram in Figure 1.
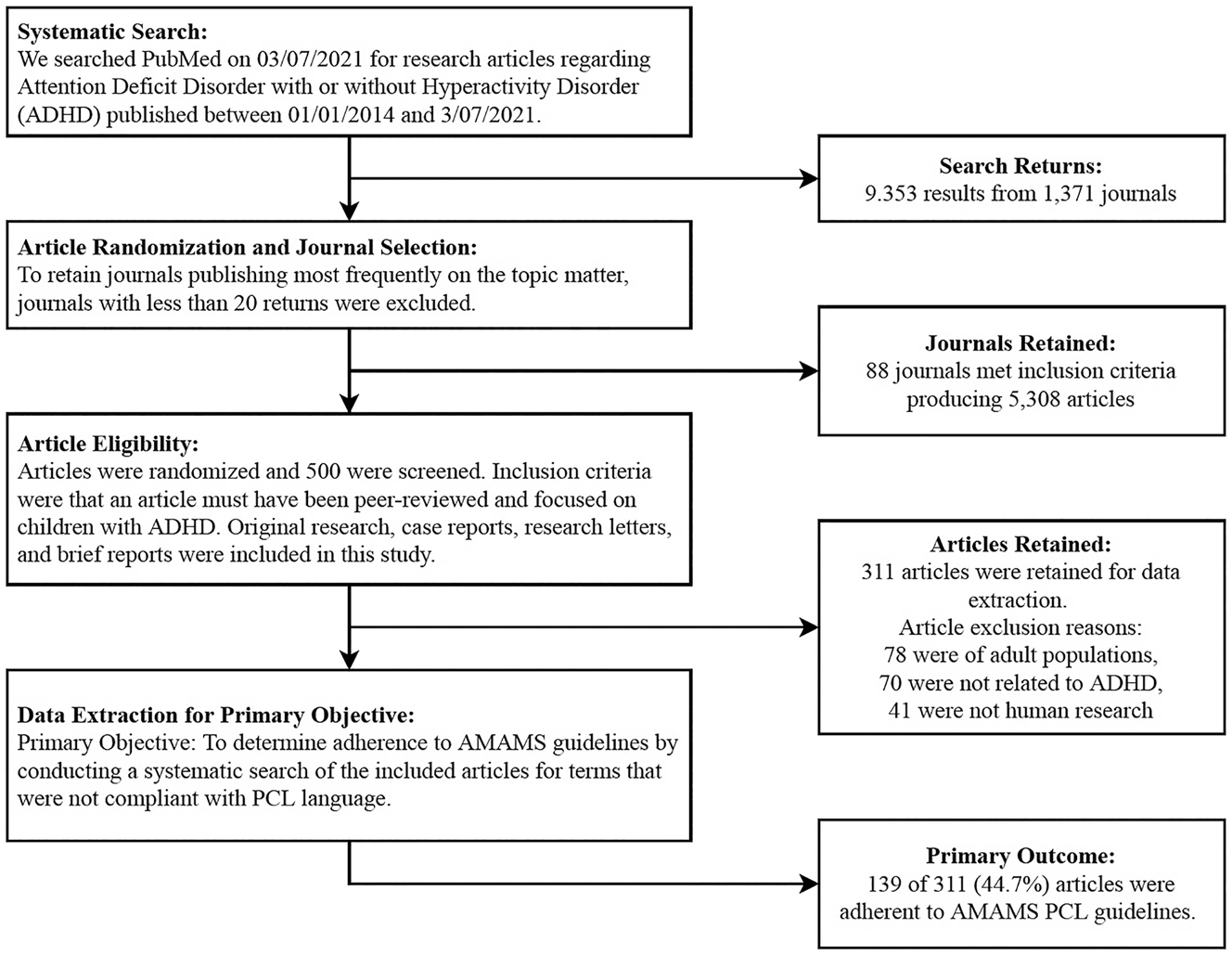
PRISMA flow diagram for systematic search, article selection, and outcomes. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Study characteristics
Of the 311 articles within our sample, 291 were original research (93.6%), and 20 articles were case reports or editorials (6.4%). The majority of the articles by type of research were cross-sectional (237/311; 76.2%) and were funded through grants (168/311; 54.0%). Out of the remaining articles, 12 were clinical trials (3.9%), 19 were literature reviews (6.1%), 12 were not research articles (3.9%), and 31 were systematic reviews (10.0%). In terms of funding, 43 received no funding (13.8%), 5 received government funds (1.6%), 16 receive industry funding (5.1%), 13 received university funding (4.2%), and 66 had no funding statement (21.2%). Of the 311 articles, 56 reported pharmacologic interventions (18.0%), 237 reported no treatment (76.2%), and 18 reported nonpharmacologic interventions (5.8%). First-author employment was most commonly found to be public (304/311; 97.8%) with the remaining being government (5/311; 1.6%) or private (2/311; 0.6%). Last-author employment was most commonly private (304/311; 97.8%) with the remaining being government (4/311; 1.3%). These values can be found in Table 1.
Article characteristics and associations of adherence to PCL language.
| Total 311 (100) | Articles with non-PCL 172 (55.31) | Articles adhering to PCL 139 (44.69) | Statistical test, p-Value | |
|---|---|---|---|---|
| Article characteristics | No. (%) | No. (%) | No. (%) | |
|
|
||||
| Type of article | Fisher’s exact | |||
|
|
||||
| Case report | 8 (2.6) | 7 (2.3) | 1 (0.3) | p=0.1 |
| Editorial or comment | 12 (3.9) | 5 (1.6) | 7 (2.3) | |
| Original research | 291 (93.6) | 160 (51.5) | 131 (42.1) | |
|
|
||||
| Type of research | Fisher’s exact | |||
|
|
||||
| Clinical trial | 12 (3.9) | 8 (2.6) | 4 (1.3) | p=0.5 |
| Literature review | 19 (6.1) | 7 (2.3) | 12 (3.9) | |
| None | 12 (3.9) | 7 (2.3) | 5 (1.6) | |
| Cross-sectional | 237 (76.2) | 132 (42.4) | 105 (33.8) | |
| Systematic review | 31 (10.0) | 18 (5.8) | 13 (4.2) | |
|
|
||||
| Type of intervention | Fisher’s exact | |||
|
|
||||
| Pharmacologic | 56 (18.0) | 27 (8.7) | 29 (9.3) | p=0.2 |
| No treatment | 237 (76.2) | 132 (42.4) | 105 (33.8) | |
| Nonpharmacologic | 18 (5.8) | 13 (4.2) | 5 (1.6) | |
|
|
||||
| Article funding | Fisher’s exact | |||
|
|
||||
| No funding | 43 (13.8) | 18 (5.8) | 25 (8.0) | p=0.1 |
| Government | 5 (1.6) | 2 (0.6) | 3 (1.0) | |
| Grant | 168 (54.0) | 90 (28.9) | 78 (25.1) | |
| Industry | 16 (5.1) | 9 (2.9) | 7 (2.3) | |
| University | 13 (4.2) | 11 (3.5) | 2 (0.6) | |
| No funding statement | 66 (21.2) | 42 (13.5) | 24 (7.7) | |
|
|
||||
| First-author employment | Fisher’s exact | |||
|
|
||||
| Government | 5 (1.6) | 1 (0.3) | 4 (1.3) | p=0.1 |
| Private | 2 (0.6) | 0 (0.0) | 2 (0.6) | |
| Public | 304 (97.8) | 171 (55.0) | 133 (42.8) | |
|
|
||||
| Last-author employment | Fisher’s exact | |||
|
|
||||
| Government | 4 (1.3) | 1 (0.3) | 3 (1.0) | p=0.3 |
| Private | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Public | 304 (97.8) | 169 (54.3) | 135 (43.4) | |
-
Studies with only 1 author (n=3) were included in the first-author employment, thus the last-author employment had a sample of 308. PCL, person-centered language.
Adherence to PCL guidelines
Among the sample of articles on children diagnosed with ADHD, we determined that 131 of the 311 (42.1%) articles were adherent to PCL guidelines. Emotive language most frequently appeared among the articles including ‘problems with,’ which was found in 47.6% (148/311) of articles, and ‘suffers from,’ which appeared in 5.8% (18/311). Other labeling and stigmatizing terminology occurred less frequently, with the label ‘mentally ill or mental patient’ being found in 3.9% (12/311) and ‘difficult child’ or ‘child is difficult’ found in 1.6% (5/311) of the articles. ‘Gifted,’ ‘sick,’ and ‘talkative’ were each found in 0.3% (1/311) of articles. ‘Challenging’ and ‘disabled’ were each found in 1.3% (4/311). The term ‘afflicted with/by’ was found in 0.6% (2/311) of articles. These values can be found in Figure 2.
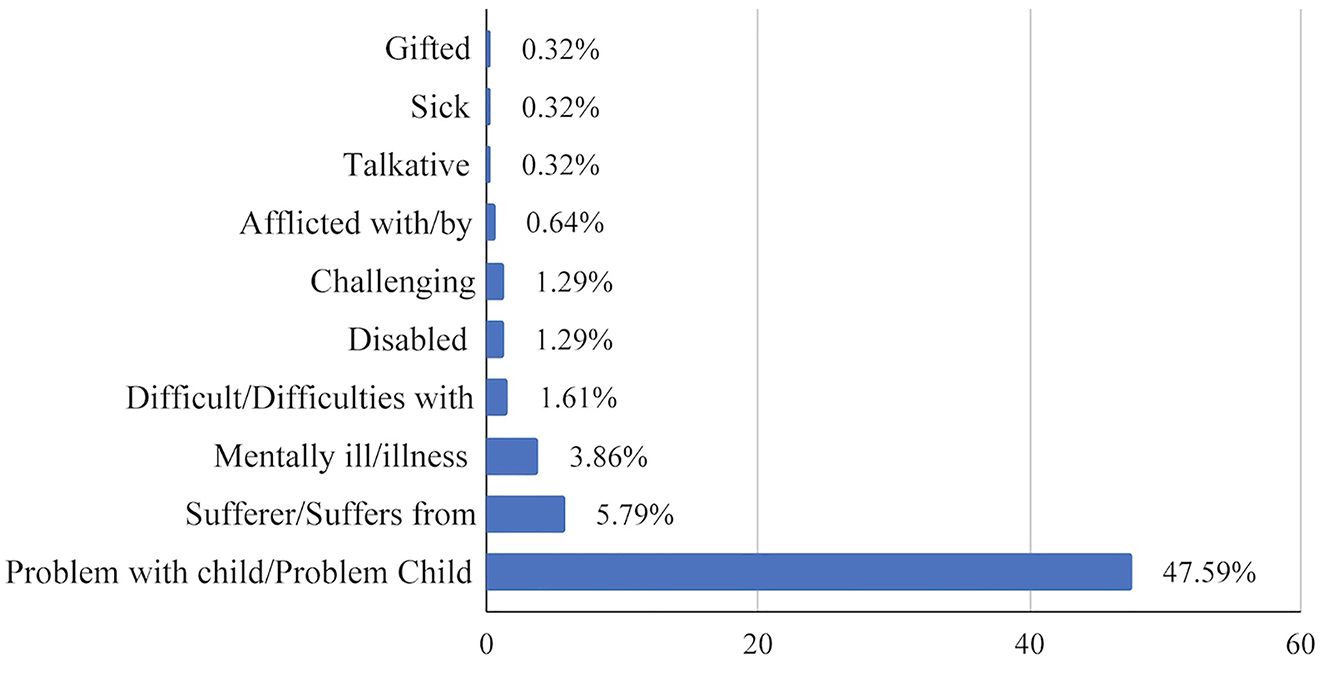
The percent of articles (n=311) with stigmatizing language in published research focused on children with ADHD. The following terms were also included in the systematic search of articles but were not found: Odd, Eccentric, Abnormal, Retarded/Retardation, Unstable, Disturbed, Crazy, and Spastic.
Associations of PCL and article characteristics
To determine the relationship between the article characteristics and the use of PCL language, we performed Fisher’s exact tests. From these analyses, we found no statistically significant associations between PCL adherence and the first author’s employment, type of article, type of research, type of intervention, article funding, or the employment of the last author (Table 1).
Discussion
From our study, we found that approximately 42.1% of the articles focusing on children diagnosed with ADHD fully adhered to PCL guidelines. Among the non-PCL adherent manuscripts, a large majority included the phrases “problems with” or the label “problem child”—with the former occurring far more often. The phrase, “problems with,” carries negative associations that reiterate the stigma surrounding children with ADHD that behavioral challenges are related to refusal/lack of control, rather than their behaviors being arduous to control or entirely out of their control without some form of treatment. Another common non-PCL phrase identified within the articles was “suffers from,” which conveys emotive phrasing, rather than objectively stating the symptoms that the child is experiencing. The AMA and APA adopted PCL guidelines to provide instructions for authors to utilize clinically accurate terminology in a neutral tone, as the language utilized in medical research may translate, directly or indirectly, through medical education into clinical practice, where the unintentional use of non-PCL may have negative consequences.
The bidirectional exchange of trust and information is an important aspect of the physician–patient relationship. The quality of these relationships has been directly correlated with patient trust and adherence to treatment recommendations [31]. Similarly, Stanford and Kyle, through a survey of 445 parents with children 2–18 years of age, found that the parents of children with obesity who perceived stigma from the child’s healthcare provider would either avoid medical appointments or seek new providers [32]. Although few studies exist regarding PCL within physician–patient interactions specific to ADHD, there is literature that shows that physicians are divided about the diagnosis and treatment of ADHD; some physicians even question the validity of the ADHD diagnosis [33]. These varying attitudes in the medical field can lead to ineffective diagnosis and treatment strategies for the patient, which can lead to non-PCL language and negative outcomes. In a 2010 study on stigma and ADHD with 301 adolescents, the groups with ADHD and depression were rejected the most compared to groups with “normal troubles” and physical illnesses [34]. In 2019, Como et al. determined that providers’ unconscious bias toward autism led to the use of stigmatizing language—damaging physician–patient relationships and augmenting the stigma of this group [35]. With the high level of stigma toward ADHD, children, adolescents, and adults who have symptoms consistent with ADHD may be reluctant to seek help for fear of social rejection or shame [36]. The use of non-PCL language may increase these negative beliefs and delay the appropriate treatment. Alternatively, utilizing PCL may improve health outcomes, wherein another systematic review of attitudes toward mental health problems showed a positive correlation between public attitudes and the decision to seek help in those with mental health problems [37], and may improve communication efforts between providers and patients, specifically when discussing pharmacotherapy [38].
The use of non-PCL may reinforce stigma surrounding children with ADHD and may negatively impact the way that care is provided to the child and may influence their mental health and social lives. This knowledge raises concern for how PCL is being utilized in practice and what impact this has on children who have ADHD. Although many organizations have adopted PCL guidelines, including the AMA, APA, and International Committee of Medical Journal Editors (ICMJE), additional efforts should be made to mitigate non-PCL research. We recommend that researchers investigating ADHD utilize precise, technical language in a neutral tone that adheres to the current AMA guidelines to report research regarding all populations or individuals—especially children. We also recommend more stringent adherence among journals to PCL guidelines, as outlined in AMAMS—requiring authors to change their language prior to publication. Our recommendations to replace non-PCL include utilizing descriptive technical language; for example, hyperactive, restless, and impulsive could replace nondescriptive, stigmatizing language such as “difficult child,” “problem child,” “challenging,” or “disabled.” Additionally, authors could replace “suffers from” or “mental illness” with “have ADHD” or “have been diagnosed with ADHD.” Finding and replacing non-PCL in a manuscript can be done utilizing the ‘Find’ function in the word processor that is being utilized to search for stigmatizing terminology, such as what we have done here. The implementation of these recommendations would likely mitigate the use of non-PCL and promote a transition to PCL in research, ultimately reducing stigma in the scientific community and barriers to healthcare utilization. We also recommend additional training during graduate education, medical school, and residency on patient-centered care for those going into medical research fields. To the best of our knowledge, there is no current journal-level training or checklists that authors can follow other than AMAMS; however, it is our hope that the growing awareness of PCL use will prompt the development of such resources.
Investigations of adherence to PCL guidelines have been conducted in other areas of medicine, which have been found to have similar or lower rates of PCL adherence than what we have found here. A study assessing rates of PCL adherence within publications about amputations demonstrated this deficit with less than 50% adherence to PCL guidelines [27], while nearly 70% of publications on psoriasis were not PCL-adherent [39]. Higher rates of non-PCL were found in studies within addiction research—with nearly 4 out of every 5 publications on alcohol use disorder [23] and opioid use disorder [40] being nonadherent to PCL guidelines. Additionally, Crocker and Smith [17] report a high prevalence of non-PCL use in clinical practice. It is difficult to determine the precise reason for variance in adherence between certain topics; however, a likely factor that is associated with each of the aforementioned medical areas is a correlation with negative stigmas. A stronger association with negative stigmas may correlate to a stronger association with non-PCL use.
Limitations and future directions
A limitation of our study involves the subjectivity of human interpretation of emotive language as defined by the AMA. In an attempt to mitigate these risks, investigators in charge of data extraction were trained in PCL, and the systematic searching of publications utilizing predefined terms was adopted. While our list of predefined terms was based on previous literature, it may not encompass all stigmatizing terminology utilized in ADHD research. For example, the term ‘disruptive’ may be seen as having a negative connotation and was found in 42 papers; however, it is utilized in the DSM-5 and is part of the name of a diagnosis, therefore we excluded it from the analysis. Additionally, the use of solely PubMed articles, as well as the reduction of articles utilized to determine PCL use, may have limited the breadth of the ADHD research we investigated. However, this selection process was utilized to select the articles with the most current and well-researched information on children with ADHD. Strengths of our study include the use of publicly available protocols for reproducibility and the randomization of article selection. Future research should cover the importance of PCL utilization in adherence with AMAMS in journals, clinical practice, and medical education to stress the positive correlation with person-centered care and how it benefits the patient, specifically research on how PCL use in journals, clinical practice, and medical education can impact the mental and physical health of each patient. Future research may also explore how PCL is utilized with a variety of medical conditions and research, particularly with highly stigmatized medical conditions, by investigating word choice and avoidance of negative associations. Additionally, development of PCL guidelines for journals as well as authors would be beneficial for implementing PCL use in medical literature.
Conclusions
Our research found that over half of the scientific literature reviewed did not adhere to PCL guidelines. Given the stigmas associated with children with ADHD and the negative implications that these stigmas have on both mental and physical health, we strongly recommend migrating away from non-PCL use and the implementation of language that adheres to the criteria suggested by AMAMS. This shift in language will serve to reduce the stigma associated with ADHD and contribute to providing the highest-quality person-centered care to each patient.
-
Research funding: None reported.
-
Author contributions: K.R., C.C., S.G., and M.H. provided substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; K.R., C.C., G.P., T.C., and M.B. drafted the article or revised it critically for important intellectual content; M.H. gave final approval of the version of the article to be published; and all authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
-
Competing interests: None reported.
References
1. CDC. What is ADHD?; 2021. Available from: https://www.cdc.gov/ncbddd/adhd/facts.html [Accessed 24 Feb 2021].Search in Google Scholar
2. Danielson, ML, Bitsko, RH, Ghandour, RM, Holbrook, JR, Kogan, MD, Blumberg, SJ. Prevalence of parent-reported ADHD diagnosis and associated treatment among U.S. Children and adolescents, 2016. J Clin Child Adolesc Psychol 2018;47:199–212.10.1080/15374416.2017.1417860Search in Google Scholar PubMed PubMed Central
3. NIMH. Attention-deficit/hyperactivity disorder. Available from: https://www.nimh.nih.gov/health/topics/attention-deficit-hyperactivity-disorder-adhd/index.shtml [Accessed 24 Feb 2021].Search in Google Scholar
4. Lebowitz, MS. Stigmatization of ADHD: a developmental review. J Atten Disord 2016;20:199–205.10.1177/1087054712475211Search in Google Scholar PubMed
5. Ng, QX. A systematic review of the use of bupropion for attention-deficit/hyperactivity disorder in children and adolescents. J Child Adolesc Psychopharmacol 2017;27:112–6.10.1089/cap.2016.0124Search in Google Scholar PubMed
6. Mueller, AK, Fuermaier, ABM, Koerts, J, Tucha, L. Stigma in attention deficit hyperactivity disorder. Atten Defic Hyperact Disord 2012;4:101–14. https://doi.org/10.1007/s12402-012-0085-3.Search in Google Scholar PubMed PubMed Central
7. Moldavsky, M, Sayal, K. Knowledge and attitudes about attention-deficit/hyperactivity disorder (ADHD) and its treatment: the views of children, adolescents, parents, teachers and healthcare professionals. Curr Psychiatr Rep 2013;15:377.10.1007/s11920-013-0377-0Search in Google Scholar PubMed
8. Hoza, B, Mrug, S, Gerdes, AC, Hinshaw, SP, Bukowski, WM, Gold, JA, et al.. What aspects of peer relationships are impaired in children with attention-deficit/hyperactivity disorder? J Consult Clin Psychol 2005;73:411–23.10.1037/0022-006X.73.3.411Search in Google Scholar PubMed
9. Liffick, GG. Reduction of stigma toward children with down syndrome through inclusion. Los Angeles: University of California; 1999. Available from: https://www.proquest.com/dissertations-theses/reduction-stigma-toward-children-with-down/docview/304497071/se-2thesis.Search in Google Scholar
10. Gavin, B, McNicholas, F. ADHD: science, stigma and service implications. Ir J Psychol Med 2018;35:169–72.10.1017/ipm.2018.20Search in Google Scholar PubMed
11. Sonuga-Barke, EJS, Brandeis, D, Cortese, S, Daley, D, Ferrin, M, Holtmann, M, et al.. Nonpharmacological interventions for ADHD: systematic review and meta-analyses of randomized controlled trials of dietary and psychological treatments. Am J Psychiatr 2013;170:275–89.10.1176/appi.ajp.2012.12070991Search in Google Scholar PubMed
12. Chapman, EN, Kaatz, A, Carnes, M. Physicians and implicit bias: how doctors may unwittingly perpetuate health care disparities. J Gen Intern Med 2013;28:1504–10.10.1007/s11606-013-2441-1Search in Google Scholar PubMed PubMed Central
13. Goddu, AP, O’Conor, KJ, Lanzkron, S, Saheed, MO, Saha, S, Peek, ME, et al.. Do words matter? Stigmatizing Language and the transmission of bias in the medical record. J Gen Intern Med 2018;33:685–91.10.1007/s11606-017-4289-2Search in Google Scholar PubMed PubMed Central
14. Ozer, U, Varlik, C, Ceri, V, Ince, B, Delice, MA. Change starts with us: stigmatizing attitudes towards mental illnesses and the use of stigmatizing language among mental health professionals. Dusunen Adam 2017;3:224–32. https://doi.org/10.5350/dajpn2017300306.Search in Google Scholar
15. Wehmeyer, M, Bersani, H, Gagne, R. Riding the third wave: self-determination and self-advocacy in the 21st century. Focus Autism Other Dev Disabl 2000;15:106–15.10.1177/108835760001500206Search in Google Scholar
16. APA. Guidelines for nonhandicapping language in APA journals: American Psychological Association; 1992. Available from: https://apastyle.apa.org/6th-edition-resources/nonhandicapping-language [Accessed 23 Aug 2021].Search in Google Scholar
17. Crocker, AF, Smith, SN. Person-first language: are we practicing what we preach? J Multidiscip Healthc 2019;12:125–9.10.2147/JMDH.S140067Search in Google Scholar PubMed PubMed Central
18. Bickford, JO. Preferences of individuals with visual impairments for the use of person-first language. RE: view; 2004. Available from: https://search.proquest.com/openview/ca603c2093b8212ced8513c9736e334c/1?pq-origsite=gscholar&cbl=48930&casa_token=sBnMU17B9QUAAAAA:wwz9bxqlGvA_-KwIrA0ySpymTegjhyKwa4_M_9x6_LswSmJjk2HYASuuSyapgyKW7ldYFxea1Q0.Search in Google Scholar
19. AMA. AMA manual of style. Chicago, Illinois: American Medical Association; 2007, 10.Search in Google Scholar
20. Danforth, S, Navarro, V. Hyper talk: sampling the social construction of ADHD in everyday language. Anthropol Educ Q 2001;32:167–90.10.1525/aeq.2001.32.2.167Search in Google Scholar
21. AMA. AMA manual of style. Chicago, Illiniois: American Medical Association; 2020, 11.10.1093/jama/9780190246556.001.0001Search in Google Scholar
22. Traxler, B, Nicks, S, Puckett, M, Dunn, K, Croff, JM, Hartwell, M. The use of person-centered language in scientific research articles focusing on opioid use disorder. Drug Alcohol Depend 2021;228:108965.Search in Google Scholar
23. Hartwell, M, Naberhaus, B, Arnhart, C, Ottwell, R, Dunn, K, Rogers, TC, et al.. The use of person-centered language in scientific research articles focusing on alcohol use disorder. Drug Alcohol Depend 2020;216:108209.10.1016/j.drugalcdep.2020.108209Search in Google Scholar PubMed
24. Castells, X, Blanco-Silvente, L, Cunill, R. Amphetamines for attention deficit hyperactivity disorder (ADHD) in adults. Cochrane Database Syst Rev 2018;8:CD007813.10.1002/14651858.CD007813.pub3Search in Google Scholar PubMed PubMed Central
25. Williamson, PO, Minter, CIJ. Exploring PubMed as a reliable resource for scholarly communications services. J Med Libr Assoc 2019;107:16–29.10.5195/jmla.2019.433Search in Google Scholar PubMed PubMed Central
26. American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-5®). Washington, DC: American Psychiatric Pub; 2013.10.1176/appi.books.9780890425596Search in Google Scholar
27. Headley, S, Potter, I, Ottwell, R, Rogers, T, Vassar, M, Hartwell, M. Adherence rates of person-centered language in amputation research: a cross-sectional analysis. Disabil Health J 2021;15:101172.10.1016/j.dhjo.2021.101172Search in Google Scholar PubMed
28. Pham, V, Greiner, B, Ottwell, R, Vassar, M, Hartwell, M. Cross-sectional analysis of patient-centered language use in journals publishing research focused on heart failure. J Patient Cent Res Rev 2021;8:248–54.10.17294/2330-0698.1821Search in Google Scholar PubMed PubMed Central
29. Hartnett, DN, Nelson, JM, Rinn, AN. Gifted or ADHD? The possibilities of misdiagnosis. Roeper Rev 2004;26:73–6.10.1080/02783190409554245Search in Google Scholar
30. Rose, D, Thornicroft, G, Pinfold, V, Kassam, A. 250 labels used to stigmatise people with mental illness. BMC Health Serv Res 2007;7:97.10.1186/1472-6963-7-97Search in Google Scholar PubMed PubMed Central
31. Orom, H, Underwood, W3rd, Cheng, Z, Homish, DL. Scott I ’yanna. Relationships as medicine: quality of the physician-patient relationship determines physician influence on treatment recommendation adherence. Health Serv Res 2018;53:580–96.10.1111/1475-6773.12629Search in Google Scholar PubMed PubMed Central
32. Puhl, RM, Peterson, JL, Luedicke, J. Parental perceptions of weight terminology that providers use with youth. Pediatrics 2011;128:e786–93.10.1542/peds.2010-3841Search in Google Scholar PubMed
33. Tatlow-Golden, M, Prihodova, L, Gavin, B, Cullen, W, McNicholas, F. What do general practitioners know about ADHD? Attitudes and knowledge among first-contact gatekeepers: systematic narrative review. BMC Fam Pract 2016;17:129.10.1186/s12875-016-0516-xSearch in Google Scholar PubMed PubMed Central
34. Kellison, I, Bussing, R, Bell, L, Garvan, C. Assessment of stigma associated with attention-deficit hyperactivity disorder: psychometric evaluation of the ADHD stigma questionnaire. Psychiatry Res 2010;178:363–9.10.1016/j.psychres.2009.04.022Search in Google Scholar PubMed PubMed Central
35. Como, DH, Floríndez, LI, Tran, CF, Cermak, SA, Duker, LIS. Examining unconscious bias embedded in provider language regarding children with autism. Nurs Health Sci 2020;22:197–204.10.1111/nhs.12617Search in Google Scholar PubMed PubMed Central
36. Canu, WH, Newman, ML, Morrow, TL, Pope, DLW. Social appraisal of adult ADHD: stigma and influences of the beholder’s Big Five personality traits. J Atten Disord 2008;11:700–10. https://doi.org/10.1177/1087054707305090.Search in Google Scholar PubMed
37. Angermeyer, MC, Schomerus, G. State of the art of population-based attitude research on mental health: a systematic review. Epidemiol Psychiatr Sci 2017;26:252–64.10.1017/S2045796016000627Search in Google Scholar PubMed PubMed Central
38. Ashford, RD, Brown, AM, Curtis, B. Substance use, recovery, and linguistics: the impact of word choice on explicit and implicit bias. Drug Alcohol Depend 2018;189:131–8.10.1016/j.drugalcdep.2018.05.005Search in Google Scholar PubMed PubMed Central
39. Ottwell, R, Heigle, B, Reddy, AK, Sajjadi, N, Wirtz, A, Cook, C, et al.. The use of person-centered language in medical research journals focusing on psoriasis: cross-sectional analysis. JMIR Dermatology 2021;4:e28415.10.2196/28415Search in Google Scholar
40. Traxler, B, Nicks, S, Puckett, M, Dunn, K, Croff, JM, Hartwell, M. The use of person-centered language in scientific research articles focusing on opioid use disorder. Drug Alcohol Depend 2021;228:108965. https://doi.org/10.1016/j.drugalcdep.2021.108965.Search in Google Scholar PubMed
© 2023 the author(s), published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Frontmatter
- General
- Review Article
- Glucocorticoid use in rheumatoid arthritis patients and the onset of pneumonia: a systematic review and meta-analysis
- Medical Education
- Original Article
- Barriers to research opportunities among osteopathic medical students
- Musculoskeletal Medicine and Pain
- Case Report
- Structural abnormalities and osteopathic considerations in primary immunodeficiencies
- Neuromusculoskeletal Medicine (OMT)
- Original Article
- Does the osteopathic pedal pump reduce lower limb volume in healthy subjects?
- Neuromusculoskeletal Medicine (OMT)
- Clinical Practice
- Enabling health potential: exploring nonlinear and complex results of osteopathic manual medicine through complex systems theory
- Pediatrics
- Review Article
- Person-centered language and pediatric ADHD research: a cross-sectional examination of stigmatizing language within medical literature
- Clinical Image
- Superficial spreading melanoma within a nevus spilus
Articles in the same Issue
- Frontmatter
- General
- Review Article
- Glucocorticoid use in rheumatoid arthritis patients and the onset of pneumonia: a systematic review and meta-analysis
- Medical Education
- Original Article
- Barriers to research opportunities among osteopathic medical students
- Musculoskeletal Medicine and Pain
- Case Report
- Structural abnormalities and osteopathic considerations in primary immunodeficiencies
- Neuromusculoskeletal Medicine (OMT)
- Original Article
- Does the osteopathic pedal pump reduce lower limb volume in healthy subjects?
- Neuromusculoskeletal Medicine (OMT)
- Clinical Practice
- Enabling health potential: exploring nonlinear and complex results of osteopathic manual medicine through complex systems theory
- Pediatrics
- Review Article
- Person-centered language and pediatric ADHD research: a cross-sectional examination of stigmatizing language within medical literature
- Clinical Image
- Superficial spreading melanoma within a nevus spilus

