A therapeutic exercise program for adolescents engaged in gender diversity services: study protocol for a non-randomised clinical trial
-
Felicity Austin
, Ashleigh Lin
, Sarah Skeldon
Abstract
Introduction
Despite the well-documented benefits of exercise for adolescents’ physical and mental health, exercise remains an underutilized strategy for improving the health of trans adolescents. This is notable because, compared to their cisgender peers, trans adolescents experience greater health challenges and systemic barriers to being physically active. To date, no research has evaluated an evidence-based exercise service within specialist paediatric gender services in Australia.
Methods
The study is a non-randomised type 2 effectiveness-implementation hybrid trial for adolescents engaged with Child and Adolescent Health Service Gender Diversity Service at Perth Children’s Hospital, Western Australia. The participant group will receive the intervention alongside standard care. The design of the program has incorporated input from the GENder idenTity Longitudinal Experience (GENTLE) Cohort Consumer Advisory group; trans young people, families, and health professionals; guidelines for common medical presentations within paediatric gender services and international physical activity guidelines for adolescents. Program implementation and feasibility (i.e., participant engagement, perceptions and experiences of the intervention), as well as preliminary effectiveness of the targeted exercise program on health outcomes (i.e., quality of life, wellbeing and markers of physical health), will be evaluated as part of a pilot trial.
Discussion
This project addresses a significant gap in research and healthcare and aims to enhance service delivery by integrating exercise into standard care for specialist paediatric gender services in Australia. Anticipated impacts include shaping current and future practices by defining safe, effective exercise for trans adolescents while laying the groundwork for larger scale implementation and research on long-term health benefits.
Introduction
Trans and gender diverse (hereafter trans) adolescents face considerable physical and mental health challenges, including managing disordered exercise and eating behaviours [1], and elevated rates of depression, self-harm and suicide attempts [1]. These challenges are coupled with systemic barriers such as a lack of transgender health knowledge and cultural awareness by providers, variable gender-affirming support, and few flexible exercise programs that are responsive to their unique needs [2]. Available literature indicates that trans young people’s desire for participation is high if meaningful, inclusive, and safe recreational sport and physical activity programs are provided [2], [3], [4].
Research in this area is predominantly retrospective, completed with trans adults, and within a community sport setting rather than with those who are currently engaged in gender-affirming medical care within the paediatric health system [5]. As demand has grown, healthcare systems must adapt to provide timely, inclusive care that affirms identities and fosters mental health, supports healthy lifestyles and promotes well-being, while addressing the unique developmental needs of this population. To date, researchers are yet to examine evidence-based exercise programs within paediatric gender services.
The Child and Adolescent Health Service (CAHS) Gender Diversity Service (GDS) at Perth Children’s Hospital is the state-wide outpatient tertiary specialist service for the assessment of gender dysphoria or incongruence in children and adolescents under 18-years in Western Australia who wish to access gender-affirming medical care (for more information on GDS service model; [6]). Currently, to our knowledge, no targeted exercise services for trans adolescents are integrated into standard care across specialist paediatric gender services in Australia. This conclusion is based on informal consultation with clinical leaders and allied health professionals from multiple tertiary-level services. While individual clinicians may recommend physical activity on a case-by-case basis, structured exercise programs or dedicated exercise professionals (e.g., exercise physiologists) are not formally embedded within existing multidisciplinary models of care. This is of significant concern as trans adolescents are less physically active, more sedentary, and have lower confidence to exercise relative to their peers – a trend that continues into adulthood [2], 4], 7]. One in four trans young people in Australia limit their exercise involvement because of their gender, yet 81 % would like to be more active but felt unable to do so because of the barriers to exercise [1]. This reflects the intersectionality of health, health behaviours, safety concerns, exclusion, stigma, structural challenges, and policy issues [1], [2], [3], [4], [5, 7], 8].
In addition to the physical health challenges that trans adolescents may experience, co-occurring considerations such as disordered eating and/or exercise behaviours [7], 9], neurodivergence (e.g., Autism, Attention Deficit Hyperactivity Disorder; [10], 11]); and social, emotional and/or behavioural challenges impact their wellbeing [1]. Trans adolescents also experience intersecting forms of social marginalisation and are disproportionately affected by health inequalities, often due to societal complexities and stigmatisation such as discrimination, lack of family support, and experiences of homelessness [12], 13]. Given the unique characteristics of this cohort, strategies that can directly impact the lives of marginalised adolescents are essential. Increasing levels of exercise, and adolescents’ motivation and confidence to be active, is a widely advocated approach to optimise physical and mental health [14], 15]. Exercise benefits of specific relevance to the trans adolescent population include managing the symptoms of mental distress, building self-esteem, improving emotional regulation, aiding routine and social connectedness, and supporting optimal well-being [4], 5], 16]. Given the potential significance for trans adolescents’ social, mental, and physical well-being, exercise-based research and service provision represents a novel and under-explored strategy to support the health and development of trans youth.
By developing this trial in partnership with community and alongside the GDS at Perth Children’s Hospital, we aim to directly inform current and future clinical practices on the role of therapeutic exercise for trans adolescents and determine how to embed safe and effective exercise within models of care. This program will be the foundation for future wider-scale research into the implementation and efficacy of exercise-based interventions for supporting the health and wellbeing outcomes of those who engage with specialty paediatric gender services. The aims of the study are:
Design an evidence-based movement program tailored to the specific needs of adolescents 12–17 years of age, engaged with an Australian paediatric gender service.
Evaluate the implementation of the 12-week movement program using established implementation outcomes informed by data from adolescent participants, service providers, and families.
Describe and evaluate the baseline health and fitness characteristics of adolescents aged 12–17 years engaged with an Australian paediatric gender service.
Investigate the preliminary effectiveness of the movement program with respect to key health outcomes and indicators.
The research team anticipates gaining valuable insights into key aspects of implementation, such as the extent to which the intervention is delivered as intended and how well it integrates into existing service structures by examining outcomes such as fidelity, adoption, acceptability, appropriateness, and feasibility. These outcomes will inform the potential for successful integration of the exercise program into existing service structures and its scalability across settings. Furthermore, we hypothesise that the intervention will lead to positive outcomes, such as improved health, increased levels of physical activity, and enhanced overall well-being among participating adolescents. The results from this trial will inform the design, delivery and evaluation of future randomised control trials across specialist paediatric gender services in Australia. The summary of this article is presented in Figure 1.

Graphical representation of this study. Key points: (1) program purpose: A tailored 12-week movement program delivered within a paediatric gender service to support the physical and mental health of transgender adolescents. (2) Implementation & impact: the program is likely to be feasible and acceptable, with positive indicators for physical activity participation, confidence, and wellbeing. (3) Clinical relevance: Findings will inform the integration of inclusive, evidence-based exercise into gender-affirming care models. Figure created with BioRender.
Methods
This manuscript was written in accordance with the SPIRIT (Standard Protocol Items: Recommendations for Interventional Trials) guidelines [17]. The trial was approved by the Child and Adolescent Health Service Health Research Ethics Committee (RGS0000006883) and The University of Western Australia Health Research Ethics Committee (2024/ET000882) and is registered on the ClinicalTrials.gov (ACTRN126250003514125). Trial results will be reported according to guidelines presented in the Consolidated Standards of Reporting Trials (CONSORT) 2010 feasibility studies and clinical trial protocols [18]. Any modifications to the research protocol or trial will be reported to the trial registry as necessary and with the results upon future publication.
Trial design
The methodological objective of this pilot study is to conduct a non-randomised feasibility trial, using considerations for a type 2 effectiveness-implementation hybrid study [19]. This particular study design simultaneously evaluates the clinical effectiveness of an intervention and the feasibility or impact of its implementation within a real-world setting [19]. The primary outcomes will focus on intervention implementation, assessing aspects such as acceptability, appropriateness, fidelity of delivery, dose delivered, reach, and feasibility – encompassing accessibility, participant adherence, engagement, and satisfaction. These outcomes will be evaluated using data collected from program participants, their parents/carers, and the exercise physiologists delivering the intervention. Secondary outcomes are measures of quality of life, well-being, physical activity behaviour, and markers of physical health (e.g., muscle strength, cardiovascular fitness, body composition). Health outcomes will be assessed pre- and post-program with collection of feasibility data throughout program delivery. All participants will also be invited to participate in an interview at the end of the trial to share their experiences (e.g., “what was helpful or what could be improved”). See Figure 2 for the trial flow.
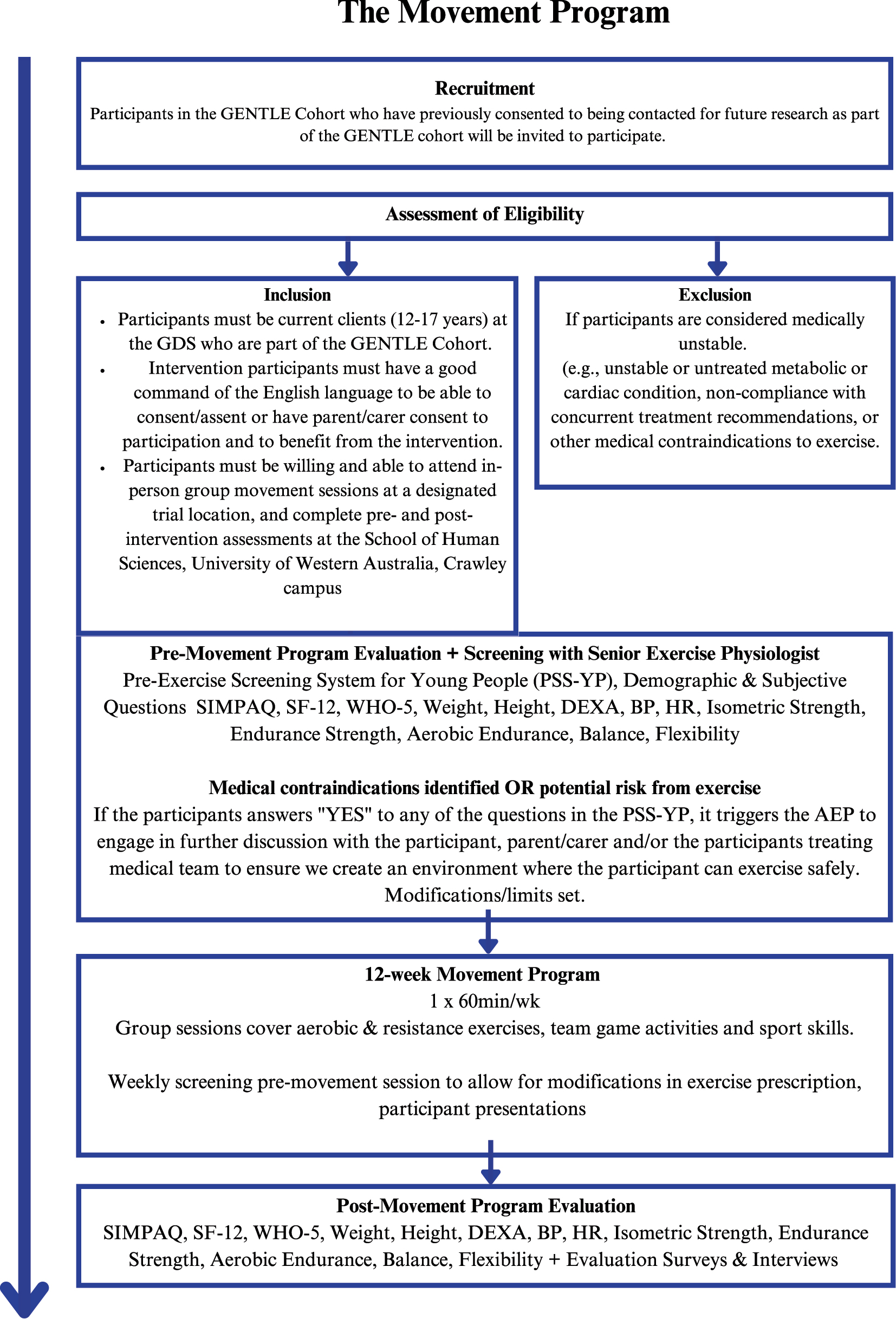
Study flow chart.
Integrated consumer consultation and participation
This study was informed by the GENder idenTity Longitudinal Experience (GENTLE) Cohort Consumer Advisory Group. They represent participants of the GENTLE Cohort, a continuously recruiting longitudinal cohort of young people presenting to the Child and Adolescent Health Service, Perth Children’s Hospital Gender Diversity Service, aimed at tracking the longitudinal health outcomes of children and adolescents engaged with the service. The Consumer Advisory Group provided input twice to ensure the exercise program’s protocol and evaluation structure consider the lived experiences of trans adolescents. Qualitative feedback was also sought from trans young people, their families, and health professionals who are either engaged in specialist paediatric gender services or provide trans healthcare in Australia [20]. Throughout the program, trans young people, families, and exercise instructors will be asked to provide feedback, both informally and through formal measures such as evaluation satisfaction surveys. This feedback will inform ongoing refinements to the trial delivery, ensuring that reasonable adjustments are made to support trial implementation without altering the core research design. By collaborating with trans young people, families, and stakeholders, the research aims to create a consumer-guided safe and inclusive evidence-based exercise service, aligning with the Western Australian Mental Health Commission’s co-production plan and the idea that consumer involvement in healthcare research leads to better outcomes [21].
Study population and eligibility
All trial participants will be current patients (age 12–17 years) who are engaged with the Child and Adolescent Health Service, Perth Children’s Hospital GDS and who have consented to be part of the GENTLE Cohort (Child and Adolescent Health Service Health Research Ethics Committee RGS0000000320). The trial will run for 12 weeks in a series of community locations aiming for 20 participants.
Additional inclusion criteria are as follows:
All trial documentation including Information and Consent Forms have been produced in English only. Trial participants must have a sufficient command of the English language to be able to consent and have parent/carer consent to participation.
Participants must be willing and able to attend in-person group exercise sessions at a designated trial location, and complete pre- and post-intervention assessments at the School of Human Sciences, University of Western Australia, Crawley campus.
Exclusion criteria are as follows:
Participants will be excluded if they are unable to safely participate in exercise based on the Pre-Exercise Screening System for Young People (PSS-YP) [22] tool and initial assessment subjective interview questions with the young person and/or their parent/carer. Exclusion from the trial based on the above medical screening includes medical contraindications to exercise (e.g., unstable or untreated cardiac condition, medical instability due to eating disorder, and/or non-compliance with current treatment recommendations
If potential contraindications to exercise are identified during the initial assessment or screening process (e.g., acute mental health condition), the exercise professional liaises with the participant’s treating medical team (i.e., General Practioner, psychiatrist, paediatrician) to seek clarification or written medical clearance. If a clinical risk is newly identified, the participant is referred for appropriate assessment and support in coordination with their GDS team and primary care provider.
If a young person presents with signs of clinical deterioration, such as recent non-suicidal self-injury wounds, substance use, or non-compliance with treatment, they may need to be temporarily excluded from individual sessions on safety grounds. However, this does not automatically result in exclusion from the entire trial. Ongoing clinical clearance (e.g., regarding recent non-suicidal self-injury) will be sought as needed.
Recruitment
Recruitment methods will include flyers for clinicians to hand out to eligible adolescents during clinic visits and/or via email invitation sent by the GDS Senior Research Officers including Participant Information and Consent Forms, to adolescents identified by their case managers as eligible. Young people known to have a current severe eating disorder will not be invited to participate. Trans adolescents and/or their parents/carers who express an interest by responding via email/telephone call will be placed on a mailing list to receive further details regarding the trial by the lead author. If trans adolescents are ineligible to participate in the trial (e.g., due to age limitations or geographical constraints), the research team will refer the young person to alternative exercise services within Western Australia.
Parents/carers of movement program participants will be invited to participate in the research project evaluation at the same initial contact timepoint as their children. At this timepoint, they will be provided with a detailed Parent/Carer Information Sheet and Consent Form that outlines the purpose of the research, what participation involves, and their rights as participants. Their involvement will primarily consist of completing an evaluation survey via and/or participating in a face-to-face semi-structured interview focused on their perspectives regarding their child’s engagement in the movement program, perceived impacts, and any observed barriers or facilitators to participation (see supplementary material The Movement Program Interview Guide).
Similarly, exercise instructors facilitating the trial will be invited to participate in the research project evaluation. They will be given the Exercise Instructor Information and Consent Form to read, complete and sign. Their involvement will primarily consist of completing an online evaluation survey at the same time points as movement program participants and parents/carers. Instructors will also be invited to participate in a face-to-face semi-structured interview following completion of the intervention, focused on their experiences delivering the program, observations of participant engagement, and perceived barriers or enablers to implementation (see supplementary material The Movement Program Interview Guide). Both parents/carers, and exercise instructors will be notified that their decision to participate in the project, or not participate, will not impact their involvement with the GDS, other health services, or other research partners.
Consent and screening
Prior to the young person’s initial health assessment for the movement program, informed consent must be obtained from both the participant and their parents/carers. Once consent is obtained, participants will undergo medical risk screening using the Pre-Exercise Screening System for Young People [22], and based on responses, additional probing questions related to medical history (e.g., “Have you ever been diagnosed with an eating disorder?”). For participants under 16 years old, parents/carers will complete the exercise and health screening questionnaire with their child present. Adolescents aged 16 and over can complete the questionnaire independently or with parental/carer support.
If the screening process identifies potential risks to exercise participation, medical clearance will be required from the participant’s treating medical team. Any identified medical concerns will be communicated with the relevant healthcare professionals (e.g., Gender Diversity Services Endocrinologist, Gender Diversity Services Case Manager, Eating Disorder Services, or General Practitioner) and the participant’s parents/carers. If participation is deemed by either the treating medical team or parents/carers to be too high risk or inappropriate, the young person is ineligible to participate further in the trial. In such cases, they will be provided tailored support or recommendations alongside their clinical team.
The senior exercise physiologist will conduct pre- and post-session check-ins (e.g., adequate nutritional intake, any new injuries, mood check in) at every session for ongoing monitoring of physical or mental health, and adjust the prescribed exercise activity based on presentation, pre-session check-in and observations, and/or based on feedback from treating team.
Withdrawal of the study participants
Participants may withdraw from the trial at any time, either verbally or in writing. Withdrawal may relate to either the research component (i.e., data collection and evaluation) and/or the intervention component (i.e., participation in the exercise program). Participants who choose to withdraw from the research component may still continue to take part in the movement program if they wish, and this option will be clearly communicated during consent. Conversely, if a participant withdraws entirely – meaning both from the research and the movement program – they will be replaced by individuals on the waitlist where possible. In cases where a participant withdraws and their parent/carer has consented to participate in data collection, the parent/carer will also be notified that their involvement is no longer required, all data will be destroyed and not be used for evaluation purposes. The right to withdraw and its implications are clearly outlined in the participant information sheets and consent forms and will be reiterated during the consent process. All instances of withdrawal, including timing, participant characteristics, and stated reasons, will be systematically recorded and reported as part of the feasibility analysis.
Exercise program design
The movement program has been designed based in collaboration with the GENTLE Community Advisory Group, and a qualitative exploration of trans young people, and their families, and health professionals specialising in gender diversity (i.e., general practitioners, psychiatrists, psychologists, social workers, research officers, exercise physiologists) [20]. The movement program is also informed by research and guidelines for commonly reported health considerations in trans adolescents presentations (e.g., anxiety, depression, eating disorders, body and gender dysphoria, neurodivergence, suicide ideation, non-suicidal self-injury) [1], 2], 9], 22], the World Health Organization (WHO) physical activity guidelines for children and adolescents [23], and the Frequency, Intensity, Time, and Type (FITT) principles which serve as a foundational framework for the prescription and progression of exercise to support health outcomes in youth populations [24]. Current WHO guidelines recommend an average of 60 or more minutes of moderate to vigorous intensity physical activity each day for children aged 5 to 17, as well as activities to strengthen muscle and bone at least 3 days a week [23]. In addition to traditional sport and exercise, the program design explores the broader, more flexible concepts of physical activity, such as active recreation, which has been reported to be an important coping strategy for people experiencing minority stress [25].
All participants will be encouraged to engage in health-promoting physical activity in alignment with WHO and Australian national recommendations [23]. To support this, movement program participants will have the option to engage in a personalised home exercise program prescribed by the lead exercise physiologist at their movement program sessions. This optional home program provides structured guidance for those who wish to incorporate additional home-based exercise to enhance physical activity motivation [15].
The movement program will be held at local community recreational spaces, including indoor (e.g., halls) and outdoor spaces (e.g., ovals). These venues will be carefully set up to prioritise the engagement, and wellbeing of trans young people, ensuring a safe and inclusive environment [2], 5]. Creating a safe and inclusive space may include removing or covering mirrors, displaying LGBTQIA+ affirming signage, providing all-gender bathroom access, and offering orientation and inductions to help participants feel comfortable and supported in the space. Additionally, the chosen locations are geographically spread to support participant accessibility to the program locations.
Participants will attend one supervised group movement session per week for 12 consecutive weeks (frequency). Each session will run for 60 min (time). Each movement session will include a variety of elements, described below, and can be tailored for individual differences, needs and abilities (type). A warm-up and check-in will be undertaken to prepare the participants for physical activity and allow for exercise modifications or limitations. Following the warm-up, cardiorespiratory fitness activities that elevate heart and breathing rates (e.g., running, dancing, or aerobic fitness games), muscular strength exercises targeting strength and endurance of various muscle groups using free weight equipment or bodyweight (e.g., push-ups, squats, planks), and sport skill development or games to assist team building and socialisation (e.g., soccer, pickleball, or floorball) will be delivered. The program’s activities are designed to be adaptable, with exercises that can be progressed and/or regressed to suit varying age groups and abilities, ensuring all participants are both engaged and appropriately challenged. Progression may include increased duration of ctivity, greater resistance, or more complex movements (intensity). To address these differences, participants may be grouped into smaller cohorts based on similar emotional and physical developmental stages, while the movement program remains flexible, occasionally mixing age groups to foster inclusivity, peer learning, and targeted developmental support.
The intended number of participants is 20 young people. A maximum group size of 10, and minimum size of 3 has been determined to ensure the group can be well-facilitated by two exercise physiologists from Thriving in Motion, a community-based, not-for-profit exercise provider with experience working with marginalised youth, including trans young people. A facilitator’s manual for the exercise instructors has been developed by the research team, outlining session plans and the procedures detailed in the protocol to ensure fidelity in the delivery of the intervention. The facilitator’s manual can be accessed by contacting the corresponding author.
Exercise instructors
The trial exercise instructors are Accredited Exercise Physiologists, university-qualified allied health professionals in Australia, holding a master’s-level qualification in clinical exercise physiology. They will receive specialised training to work effectively with trans adolescents and their families. This training includes Youth Mental Health First Aid [26] and tailored inclusive trauma-informed exercise practices. The training has been developed by clinical exercise physiologists and mental health professionals with expertise in gender diversity, adolescent development, and trauma-informed care. It covers affirming communication, safe and inclusive exercise environments, understanding the impact of minority stress and trauma, and strategies to support emotional regulation, autonomy, and psychological safety in movement settings.
Their training will equip them to support the wellbeing and exercise participation of young people who have a range of mental health conditions (e.g., anxiety, depression, suicidal ideation, non-suicidal self-harm), understand adolescent development, and navigate group dynamics and challenges related to social, emotional and behavioural differences. The exercise instructors are also equipped to support neurodivergent individuals, those with co-occurring physical health conditions, and participants experiencing disordered eating and/or exercise behaviours. Alongside their comprehensive training, the exercise instructors will have access to participants’ health screening and physical health assessment reports prior to the movement program commencing in order to tailor the exercise activities to meet the needs of participants.
Outcome measures
Implementation
The implementation outcomes are guided by the design of Type 2 effectiveness-implementation hybrid trials [19] and best practice guidelines feasibility studies [18], incorporating both quantitative and qualitative methods. As per CONSORT guidelines for feasibility and pilot trials, key indicators include participant demographic characteristics (e.g., gender identity, age, medical history), recruitment and retention rates, session attendance and duration, program expectations, and adherence to exercise programming. In addition, implementation outcomes including fidelity of delivery, dose delivered, reach, and satisfaction are included to explore early indicators of successful program delivery and integration into the clinical service setting. These implementation outcomes reflect the dual focus of a Type 2 hybrid design and are described in further detail in Table 1 [19]. Given the novelty of the study, we have developed these measures based on consumer satisfaction surveys from published research in allied health [27], 28].
Implementation outcomes – Type 2 hybrid trial.
| Outcome measure | Description | Method of measurement | Feasibility criteria |
|---|---|---|---|
| Acceptability – participants | Perceived benefit and positive experience of the program | End-of-program survey: participants selecting that their skills (e.g., sports, listening) “improved a little” or “a lot”; participants reporting they would do the program again | ≥75 % reporting program benefit ≥50 % willing to repeat |
| Acceptability – parent/carer | Perceived benefit of the program for their child | End-of-program survey: parents/carers indicating their child’s skills improved and that they would recommend the program | ≥75 % reporting benefit ≥75 % recommending program |
| Adoption | Initial interest or uptake of the program among the eligible population | Number of expressions of interest received, as a proportion of eligible 12–17-year-olds in the GENTLE cohort | ≥25 % interest rate |
| Appropriateness – instructors | Suitability and usability of session plans | End-of-session instructor survey: plan helpfulness, delivery confidence, and perceived difficulty | ≥75 % on each item |
| Appropriateness – Participants | Suitability of program activities for participant skill and comfort levels | End-of-program survey: activity difficulty and confidence to try | ≥75 % on each item |
| Appropriateness – data collection | Suitability of data collection methods | Rate of missing data and reported reasons | <15 % missing data |
| Feasibility (overall) | Practicality and acceptability of the program | Post-program surveys and interviews; likert scales on enjoyment and motivation | ≥80 % report feasibility |
| Fidelity | Extent to which sessions are delivered as planned | Instructor end-of-session surveys and logs | ≥90 % sessions delivered as planned |
| Penetration (reach) | Degree of reach into the target population | Proportion of eligible participants who enrolled | Descriptive |
| Sustainability | Continued delivery beyond the trial period | Follow-up delivery data, qualitative interviews with staff | Exploratory |
| Retention | Participants completing the intervention | Number completing ÷ number enrolled; drop-out reasons recorded | ≥75 % retention |
| Adherence | Participant attendance and compliance | Attendance logs; reasons for absences | ≥90 % adherence |
| Dose delivered | Number and duration of sessions provided | Instructor logs (sessions out of 12 and ∼50 min duration) | ≥90 % of intended dose |
| Dose received | Intensity and participation level | Session intensity via HR data and RPE; session logs | Exploratory |
| Engagement | Participant involvement during sessions | % Of session actively participated | ≥75 % per session |
| Satisfaction – sessions | Satisfaction with individual sessions | End-of-session ratings: enjoyment rated +2 or higher | ≥75 % satisfaction |
| Satisfaction – program (participant) | Overall satisfaction with the program | End-of-program survey: ‘enjoyed it’ or ‘really enjoyed it’ | ≥75 % satisfaction |
| Satisfaction – program (parent/carer) | Overall parent satisfaction | End-of-program survey: ‘somewhat’ or ‘extremely’ satisfied | ≥75 % satisfaction |
| Safety | Participant safety during program | Reported adverse events | No serious adverse events |
All trial participants, their parents/carers and exercise instructors will be invited to opt-in or opt-out for a post-trial evaluation about their trial experience, which includes completing an online questionnaire through a secure website using a unique identifier code and/or selecting the option for a semi-structured interview on the consent form (see supplementary material the Movement Program Interview Guide). Detailed information about the evaluation process, including that the interviews will be audio recorded and transcribed verbatim, will be provided within the information sheet and consent form. All participants’ identities will be de-identified, and audio recordings will be securely stored with access restricted to the named investigators only.
Preliminary effectiveness
Preliminary effectiveness will be evaluated via self-reported health questionnaires and a physical health assessment battery conducted pre- and post-trial, taking approximately 60 min. Physical fitness assessments will take place at the Exercise and Sport Science Department at the University of Western Australia, and participants will be provided a copy and report of all results.
Participant health assessments will include measures of physical activity and sedentary levels, wellbeing, quality of life, and physical fitness. The Simple Physical Activity Questionnaire (SIMPAQ) will be used to assess participants combined physical activity behaviours across various domains of leisure time, domestic, and transport-related activities over a representative 24-h period [29]. Quality of life will be measured using the Short-form-12-health-survye-questionnaire (SF-12) [30], which evaluates physical, mental, and social health across eight domains, while well-being will be assessed using the World Health Organisation-Five Well-Being Index (WHO-5) [31], a short self-report measure of subjective wellbeing over the last two weeks. Physical fitness will be assessed through several validated methods: body composition via DEXA scan [32], 33], cardiovascular health via manual blood pressure readings [34], and muscle strength using grip strength dynamometry [35], 36], plank holds [37], and 60-s squat [37] and push-up tests [37]. Cardiorespiratory fitness will be estimated using the YMCA three-minute step test [38], 39], with heart rate recovery monitored via a Polar optical sensor. Functional balance will be assessed using the Star Excursion Balance Test [40], explosive power via the Standing Broad Jump [41], and flexibility via the Sit and Reach Test [42]. These assessments are widely accepted as reliable and feasible for use in paediatric populations [29], [30], [31], [32], [33], [34], [35], [36], [37], [38], [39], [40], [41], [42] (see Table 2).
Outcome measures for movement program participants.
| Outcome | Tool | Description | Timepoint | Test administration |
|---|---|---|---|---|
| Physical activity and sedentary levels | Simple physical activity questionnaire (SIMPAQ) | The simple physical activity questionnaire (SIMPAQ) will be used to assess participants combined physical activity behaviours across various domains of leisure time, domestic, and transport-related activities [29]. The SIMPAQ has been structured to provide a snapshot of a 24-h period that is representative of the previous week and flows from sedentary time to walking, structured exercise/sport to incidental/other activities. An example question is “what activities did you do and how much time did you spend on each activity on each day?” [29]. | Pre & post exercise program | Face-to-face (15 min) |
| Quality of life | Short form – 12 (SF-12) | The 12-item short form survey (SF-12) [30] is a self-reported outcome measure assessing the impact of health on an individual’s everyday life. The SF-12 encompasses eight domains, namely limitations in physical activities because of health problems; limitations in social activities because of physical or emotional problems; limitations in usual role activities because of physical health problems; bodily pain; general mental health (psychological distress and well-being); limitations in usual role activities because of emotional problems; vitality (energy and fatigue); and general health perceptions. An example question is “in general, how would you say your health is?” | ||
| Well-being | The World Health Organisation five well-being index (WHO-5) | The world health Organisation-five well-being index (WHO-5) [31] is a short, self-administered, and positively worded scale designed to measure the level of subjective well-being over the last two weeks [31]. An example question is “how cheerful and in good spirits have you felt over the last two weeks?” | ||
| Body composition | Dual-energy X-ray absorptiometry (DEXA) | Using a dual-Energy X-ray absorptiometry (DEXA), body composition will be evaluated. Prior to the DEXA scan, participants’ height will be measured to the nearest centimeter using a stadiometer, and weight will be recorded to the nearest 100 g using a Seca digital column scale. These measurements are essential for accurate calibration of the DEXA equipment and analysis of results. during the procedure, participants will lie on a specialised table while a scanning arm passes over their body, emitting low-dose X-rays to differentiate between bone, fat, and lean tissues. The scan typically takes about 2 min, with the entire procedure lasting approximately 15 min. DEXA has been recognised as a valid and reliable method for assessing body composition in children and adolescents [32], 33]. | Pre & post exercise program | Face-to-face (45 min) |
| Cardiovascular health | Resting blood pressure | Resting blood pressure will be measured using stethoscope and Welch Allyn handheld sphygmomanometer. This manual method is widely used in clinical settings is considered the gold standard for blood pressure measurement and is essential for accurate assessment of cardiovascular health [34]. | ||
| Isometric strength | Grip strength | Isometric strength will be measured via the grip strength test using a Jamar digital handgrip dynamometer [35], 36]. Handgrip dynamometry is a commonly used indicator for muscle performance and strongly correlates with leg muscle strength and overall muscle function in children and has been deemed feasible and reliable in paediatric populations [36]. | ||
| Endurance strength | Plank hold (0.1 s) | The isometric plank hold will be used to assess trunk muscular endurance [37]. | ||
| Squats in 60 s | The 60 s squat test will be used to examine lower limb strength and endurance [37]. | |||
| Push ups in 60 s | The 60 s push up test is used to examine upper limb strength and endurance [37]. | |||
| Cardiorespiratory Fitness | YMCA 3-min step test | The YMCA three-minute step test is a submaximal exercise test that assesses cardiorespiratory fitness in children by measuring heart rate recovery after a three-minute period of stepping [38]. Participants step up and down on a standardised step at a consistent rate (96 beats per minute) for 3 min. Heart rate will be continuously monitored using a Polar optical heart rate Sensor worn throughout the test. The heart rate recorded 1 min post-exercise will be compared to normative data to estimate the participant’s VO2max. The test is easy to perform, well tolerated and has been deemed valid and reliable for estimating VO2max in children and adolescents [38], 39]. | ||
| Balance | Star excursion balance test (SEBT) | The star excursion balance test (SEBT) will be used to assess the participants’ ability to maintain balance while reaching as far as possible in eight different directions using one leg [40]. | ||
| Power | Standing broad Jump | The Standing broad Jump test will be used to assess explosive power in a horizontal direction and has been demonstrated to be both valid and reliable [41]. Participants will stand behind a marked line with their feet shoulder-width apart and perform a two-footed jump as far forward as possible. The distance from the starting line to the closest heel landing point will be measured. Participants will complete three trials, with the best attempt recorded for analysis. | ||
| Flexibility | Sit and reach test | The sit and reach test is a common measure of flexibility and specifically measures the flexibility of the lower back and hamstring muscles [42]. Participants will sit on the floor with their legs extended and feet placed flat against a Sit n’ reach flexibility Box. They will reach forward as far as possible, keeping their knees extended, and the distance reached will be recorded. Participants will complete two trials, with the best attempt recorded for analysis. |
Retention
To maximise participant retention and reduce loss to follow-up, assessments will be scheduled according to participant preference and availability as much as possible. Appointment reminders will be sent out one week and one day prior to assessment date. Contact will be made immediately following a “no-show” to an assessment or movement program session to record reason and reschedule within the timeframe for the study protocol. To encourage attendance to the post-trial assessments, a comprehensive report will be provided to families upon completion of the final assessment.
Timing
Measures will be assessed at baseline (pre-trial) and within one week following completion of the trial, to reduce the risk of detraining and to more accurately capture the immediate effects of the intervention.
Statistical analysis
All quantitative data will be analysed using Microsoft Excel and IBM Statistical Package for the Social Sciences (SPSS) Statistics software. Data will be screened for completeness and missing values. Participants missing entire datasets (e.g., all physical health assessment data) will be excluded from relevant analyses. For pre–post comparisons, if more than 5 % of data are missing for a given outcome, multiple imputation by chained equations (MICE) will be considered to minimise bias and preserve statistical power. The imputation model will include key demographic variables (e.g., age, sex assigned at birth), and all available outcome variables. Ten imputed datasets will be generated, and results will be pooled to produce final estimates, consistent with standard procedures for small-sample trials. A 50 % intervention adherence rate will serve as the inclusion threshold to help isolate intervention effects, reflecting our preliminary aim to assess the need for a full-scale randomised control trial. An adherence level of ≥50 % is considered sufficient to indicate initial engagement with the intervention, while also accounting for common barriers to full participation within adolescent mental health and gender-affirming care contexts, both characteristic of this cohort. This threshold reflects a pragmatic balance between feasibility and meaningful exposure to the program. We will also conduct sensitivity analyses using higher adherence thresholds (e.g., 75 %) to explore whether intervention effects vary by level of participation. These analyses will help assess the robustness of findings and inform the optimal intervention dose for future trials. Descriptive statistics will be used to summarise pre-to-post-program differences. The magnitude of change in health outcome variables (i.e., physical health, well-being, and quality of life) from baseline to program completion will be assessed by calculating Cohen’s d effect sizes with correlations between the variables. In addition to effect sizes, the clinical significance of changes in health outcomes measured by the SF-12 and WHO-5 will be evaluated using minimum important difference (MID) thresholds or reliable change indices, where available. Given the exploratory nature and small sample size of this trial, formal hypothesis testing will not be conducted. The sample size for this study is in keeping with similar trials [15]. Given the novelty and intent of the intervention, findings will provide valuable insight into the health outcomes, the most effective operation of the movement program, and inform design of future trials and research in this field.
Interviews will be conducted by the research team, who have experience in qualitative research methodology, including interviewing marginalised young people, families, and health professionals. Participants will guide the interview, with probing questions used for clarification and exploration [43]. At the end, participants can ask questions, offer additional information, and provide feedback. Pragmatic considerations (e.g., time and resource constraints) will guide data collection, and we aim to collect sufficient, appropriate information to address our research questions and construct a comprehensive story through our data. We will adopt an inductive reflexive thematic analysis approach [44], 45]. A ‘critical friends’ process will be employed, with co-authors providing feedback on meaning units, themes, and interpretations [46]. Collaborative processes may result in themes being merged, redefined, or recoded based on collective interpretation, ensuring rigor and quality in analysis [47]. Reflexive thematic analysis is a cyclical and iterative process, and various stages of the analysis process will be repeated or returned to.
Data management
All data will be coded, backed-up and securely stored on servers at the University of Western Australia (UWA) which are password and algorithm protected. Any hard copies relating to collection of data will be stored in locked filing cabinets on site at UWA in the School of Human Sciences (Exercise and Sport Science) and as per UWA standard practice, will be retained for 7 years following publication or until the youngest participant turns 25, whichever is longer. Regarding completion of outcome measures, participants will be given a unique identifier code to record on the measures each time instead of using identifying details. Identifying information and research data will be stored separately. Data will be de-identified for entry and analysis in both SPSS and NVivo. Regarding qualitative data, audio recordings will be stored on a secure server and will only be accessible to the named investigators. Transcripts will be de-identified and stored on NVivo software and will only be accessible to the named investigators. All SPSS and NVivo data will be accessible only to the named investigators and will be password protected.
Once the minimum retention period for our dataset has been reached, the University’s Records, Archives & Digitisation Services team will ensure there are no current Freedom of Information or other outstanding actions on the records before initiating the destruction approval process, as per Western Australian University Sector Disposal Authority standard practice.
Possible harms and safety monitoring
While there are minimal risks associated with participation, some discomfort may occur during pre- and post-exercise tests, such as leg fatigue, or increased heart rate or breathing rate. These are typical responses, and participants can stop any test or activity if they feel uncomfortable. Additionally, a small amount of ionizing radiation via DEXA scans is required for this study, and this information is also included in the participant information and consent form. If participants experience distress during assessments, group sessions, or interviews, they can seek immediate support from the trial facilitators. Contact information for external support services (e.g., Qlife, Lifeline, Kids Helpline) will be provided to participants. Participants will also be reminded that they can reach out to their treating team for additional support.
Monitoring adverse events
During the trial, all exercise activities are carefully planned to ensure the physical and psychological safety of participants. Any adverse events, including physical injuries or deterioration in physical or mental health will be monitored closely. Such events will be reported to the participants’ parents/carers and treating team at the GDS for review, with appropriate adjustments, modifications, or if necessary, withdrawal from the study.
Confidentiality and participant autonomy
Participants will be informed that they may skip any questionnaire and/or interview questions (i.e., pre- or post-trial) that make them uncomfortable, and they are free to discontinue their participation at any time without consequence. At the start of the first movement session, a group discussion will be held to establish a collaborative agreement regarding confidentiality and mutual respect.
Monitoring of participant compliance
The procedures for monitoring participant compliance will be the responsibility of the supervising trial investigator (BF) at The University of Western Australia who will ensure the study is conducted in compliance with the protocol, good clinical practice and the application regulatory requirements.
Discussion
Given the high risk of both physical and mental health challenges among trans adolescents [4], exploring novel solutions such as exercise is critical. There are well-established benefits of exercise for children’s physical, mental, and psychosocial health [15], but research on the trans population remains limited [2], 3], 5]. Our findings aim to directly inform current practice with regards to the role of exercise for trans adolescents and enhance multidisciplinary care within specialist paediatric gender services. This research will also pave the way for future research exploring the efficacy of exercise-based programs for improving health outcomes for trans adolescents. Ensuring equitable access to physical activity opportunities, including tailored support for trans adolescents, is critical to fostering a positive relationship with exercise and promoting lifelong health [4].
We anticipate that participation in the trial will result in benefits for the participants including increased health-promoting physical activity participation, enhanced motivation and confidence, and improved understanding of the importance of movement in personal, holistic health and wellbeing from pre-to post-trial. Providing a safe, supportive environment for exercise allows participants to focus on positive health outcomes and build peer support networks, which are key benefits of group-based interventions [15]. We expect that feasibility estimates for recruitment, completion, and retention will be met, and results of outcome measures will enable an effect-size estimation for the planning of a future randomised controlled trial. It is anticipated that participating adolescents, parents/carers and exercise instructors will find the movement program acceptable. The qualitative component will provide a valuable opportunity to gain insight into the experiences and perspectives of all participants. This understanding is crucial for future evaluation and development of the trial for future delivery and scaling up.
Strengths of this trial are the collaborative participatory approach, which involved key stakeholders such as trans youth, parents/caregivers, health professionals, clinical researchers and community advisory groups in the design and development of the program. The collaborative nature of the project is expected to enhance the relevance and acceptability of the program, potentially strengthening future support services and models of care for this population. Additionally, the mixed-methods approach, combining quantitative and qualitative measures, will provide a comprehensive understanding of participant experiences. Positive outcomes from this trial may advocate for the integration of exercise physiology services into paediatric gender services nationwide, contributing to a holistic approach to the health of trans adolescents and improving current best-practice models of care.
Limitations of this trial include potential biases in the dual role of the lead author (FA) who will facilitate the assessments, trial and later analyse the data. To mitigate these risks, several reflexive strategies will be used, including the use of a structured interview guide to promote consistency and reduce interviewer influence, adherence to standardised protocols for physical fitness assessments (see Table 2), calculating scores and interpretations based on established methods and norms (e.g., SF-12 and WHO-5), and engaging in collaborative data analysis with co-authors to facilitate critical dialogue and enhance the trustworthiness of interpretations. Additionally, recruitment was limited to a single, specialised paediatric gender diversity service. While this supports internal validity through a clearly defined clinical cohort, it limits the external validity of findings. Adolescents connected with specialised health services may differ in their experiences when compared to adolescents who have differing access and engagement with health or support service, including greater access to family and multidisciplinary support and gender-affirming care. Future research should expand upon these findings to explore experiences across diverse and less supported contexts, for example rural, underserved, or non-clinical settings.
While positive outcomes from this trial could inform the integration of exercise physiology into paediatric gender services, we acknowledge the possibility of null findings. To minimise bias in the interpretation of such outcomes, the study employs validated and standardised outcome measures, structured assessment protocols, and a pre-specified analysis plan. Reflexive strategies, including collaborative data interpretation and critical dialogue among the research team, will be used to reduce the risk of confirmation bias and enhance transparency. As an effectiveness-implementation study, these methods also support the interpretation of implementation outcomes regardless of efficacy results.
Given the exploratory nature and small sample size of the current trial, formal hypothesis testing was not undertaken, and the absence of a comparator group limits causal inference. However, this intervention design is consistent with best-practice guidelines for early-phase implementation-effectiveness trials, where the focus is on assessing implementation, safety, acceptability, and preliminary effects to inform future trials [19]. The insights gained from this study, including participant responses, health-related outcomes, and practical considerations for intervention delivery, will directly inform the design, methodology, and statistical modelling of future controlled trials aimed at evaluating efficacy. In particular, Bayesian estimation approaches offer a valuable framework for interpreting intervention effects in small or heterogeneous samples and will be considered in future, adequately powered studies to support more robust and nuanced inference. This approach ensures that future trials are methodologically sound, with their design, implementation, and statistical modelling directly informed by empirical data generated from this foundational work.
In conclusion, incorporating safe and inclusive exercise services as an adjunct to gender-affirming care presents an opportunity to positively influence the long-term health and wellbeing of trans adolescents. Young people of all gender identities should have the opportunity, and be supported, to develop healthy physical activity routines and transition into adulthood with a positive relationship with exercise. This research can contribute to a more comprehensive, multidisciplinary approach that addresses both physical and psychosocial needs within paediatric gender services.
Funding source: NHMRC Investigator Grant
Award Identifier / Grant number: 2010063
Funding source: Thriving in Motion
Funding source: Australian Government Research Training Program Scholarship at The University of Western Australia
Funding source: Medical Research Futures Fund (MRFF) Australian Research Consortium for Trans Youth and Children
Award Identifier / Grant number: ARCTYC; MRF2032119
Acknowledgments
The authors would like to acknowledge that the language and terminology of gender identity are diverse and constantly evolving. In consultation with members of the trans and gender diverse community and The Kids Research Institute Australia research team, this article will strive to make use of the most current and inclusive terms and abbreviations available. No exclusion, offense, or distress is intended by the use of language that may not be appropriate to all individuals, in particular those of different cultures.
-
Research ethics: Child and Adolescent Health Service Health Research Ethics Committee (RGS0000006883) 5/7/2024. The University of Western Australia Health Research Ethics Committee (2024/ET000882) 6/8/2024. Trial registration: ACTRN126250003514125.
-
Informed consent: Not applicable.
-
Author contributions: All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Use of Large Language Models, AI and Machine Learning Tools: None declared.
-
Conflict of interest: The lead author (FA) and co-authors (BF, KW) are affiliated with Thriving in Motion, which may present a potential conflict of interest due to their connection with the not-for-profit funder and community provider support the delivery of exercise services for the trial. Authors LS and JM may have a potential conflict of interest regarding their involvement with the GDS and their role in the recruitment of participants for this clinical trial.
-
Research funding: This work was carried out while the corresponding author was in receipt of an Australian Government Research Training Program Scholarship at The University of Western Australia. AL is funded by a NHMRC Investigator Grant (#2010063). Austin, Lin, Furzer, Moore, Saunders, Jackson, Wright, Simpson, Ferguson and Skeldon are researchers affiliated with the MRFF-funded Australian Research Consortium for Trans Youth and Children (ARCTYC; MRF2032119). The authors acknowledge the funding supported by Thriving in Motion for the implementation and facilitation of this clinical trial.
-
Data availability: Not applicable.
References
1. Strauss, P, Cook, A, Winter, S, Watson, V, Wright Toussaint, D, Lin, A. Mental health issues and complex experiences of abuse among trans and gender diverse young people: findings from trans pathways. LGBT Health 2020;7:128–36. https://doi.org/10.1089/lgbt.2019.0232.Suche in Google Scholar PubMed
2. Austin, F, Wright, KE, Jackson, B, Lin, A, Schweizer, K, Furzer, BJ. A scoping review of trans and gender diverse children and adolescents’ experiences of physical activity, sport, and exercise participation. Ment Health Phys Act 2024;26:100576. https://doi.org/10.1016/j.mhpa.2024.100576.Suche in Google Scholar
3. Herrick, SS, Duncan, LR. A systematic scoping review of physical education experiences from the perspective of LGBTQ+ students. Sport Educ Soc 2023;28:1099–117. https://doi.org/10.1080/13573322.2022.2071253.Suche in Google Scholar
4. Teti, M, Bauerband, LA, Rolbiecki, A, Young, C. Physical activity and body image: intertwined health priorities identified by transmasculine young people in a non-metropolitan area. Int J Transgen Health 2020;21:209–19. https://doi.org/10.1080/26895269.2020.1719950.Suche in Google Scholar PubMed PubMed Central
5. Storr, R, Nicholas, L, Robinson, K, Davies, C. ‘Game to play?’: barriers and facilitators to sexuality and gender diverse young people’s participation in sport and physical activity. Sport Educ Soc 2022;27:604–17. https://doi.org/10.1080/13573322.2021.1897561.Suche in Google Scholar
6. Cavve, BS, Bickendorf, X, Ball, J, Saunders, LA, Marion, L, Thomas, CS, et al.. Retrospective examination of peripubertal return for patients of Western Australia’s gender diversity service. LGBT Health 2024;11:606–14. https://doi.org/10.1089/lgbt.2023.0256.Suche in Google Scholar PubMed
7. Schweizer, K, Austin, F, Wright, KE, Lin, A, Bickendorf, X, Jackson, B, et al.. Physical activity behaviours in trans and gender diverse adults: a scoping review. Int J Transgen Health 2025;26:10–24. https://doi.org/10.1080/26895269.2023.2284772.Suche in Google Scholar PubMed PubMed Central
8. Telfer, MM, Tollit, MA, Pace, CC, Pang, KC. Australian standards of care and treatment guidelines for transgender and gender diverse children and adolescents. Med J Aust 2018;209:132–6. https://doi.org/10.5694/mja17.01044.Suche in Google Scholar PubMed
9. McGregor, K, McKenna, JL, Barrera, EP, Williams, CR, Hartman-Munick, SM, Guss, CE. Disordered eating and considerations for the transgender community: a review of the literature and clinical guidance for assessment and treatment. J Eat Dis 2023;11:75. https://doi.org/10.1186/s40337-023-00793-0.Suche in Google Scholar PubMed PubMed Central
10. Mahfouda, S, Panos, C, Whitehouse, AJ, Thomas, CS, Maybery, M, Strauss, P, et al.. Mental health correlates of autism spectrum disorder in gender diverse young people: evidence from a specialised child and adolescent gender clinic in Australia. J Clin Med 2019;8:1503. https://doi.org/10.3390/jcm8101503.Suche in Google Scholar PubMed PubMed Central
11. De Vries, KM. Intersectional identities and conceptions of the self: the experience of transgender people. Symb Interact 2012;35:49–67. https://doi.org/10.1002/symb.2.Suche in Google Scholar
12. Lim, G, Melendez-Torres, GJ, Amos, N, Anderson, J, Norman, T, Power, J, et al.. Demographic predictors of experiences of homelessness among lesbian, gay, bisexual, trans, gender-diverse and queer-identifying (LGBTIQ) young people in Australia. J Youth Stud 2025;28:254–80. https://doi.org/10.1080/13676261.2023.2261864.Suche in Google Scholar
13. Oakley, S, Bletsas, A. The experiences of being a young LGBTIQ and homeless in Australia: re-thinking policy and practice. J Sociol 2018;54:381–95. https://doi.org/10.1177/1440783317726373.Suche in Google Scholar
14. Pascoe, M, Bailey, AP, Craike, M, Carter, T, Patten, R, Stepto, N, et al.. Physical activity and exercise in youth mental health promotion: a scoping review. BMJ Open Sport Exerc Med 2020;6:e000677. https://doi.org/10.1136/bmjsem-2019-000677.Suche in Google Scholar PubMed PubMed Central
15. Wright, KE, Jackson, B, Licari, MK, Dimmock, JA, Furzer, BJ. Thriving families: the feasibility and preliminary efficacy of a multi-component physical literacy program for children with neurodevelopmental, emotional, or behavioural problems. Ment Health Phys Act 2023;25:100558. https://doi.org/10.1016/j.mhpa.2023.100558.Suche in Google Scholar
16. López-Cañada, E, Pereira-García, S, Pérez-Samaniego, V, Valencia-Peris, A, Devís-Devís, J. A mixed-methods study for understanding the motives of trans persons’ participation in leisure-time physical activity and sport. Leis Stud 2024;43:1–6. https://doi.org/10.1080/02614367.2024.2379432.Suche in Google Scholar
17. Qureshi, R, Gough, A, Loudon, K. The SPIRIT checklist – Lessons from the experience of SPIRIT protocol editors. Trials 2022;23:359. https://doi.org/10.1186/s13063-022-06316-7.Suche in Google Scholar PubMed PubMed Central
18. Eldridge, SM, Chan, CL, Campbell, MJ, Bond, CM, Hopewell, S, Thabane, L, et al.. CONSORT 2010 statement: extension to randomised pilot and feasibility trials. BMJ 2016;355:i5239. https://doi.org/10.1136/bmj.i5239.Suche in Google Scholar PubMed PubMed Central
19. Curran, GM, Bauer, M, Mittman, B, Pyne, JM, Stetler, C. Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Med Care 2012;50:217–26. https://doi.org/10.1097/MLR.0b013e3182408812.Suche in Google Scholar PubMed PubMed Central
20. Austin, F, Lin, A, Wright, K, Jackson, B, Simpson, A, Furzer, B. Exercise experiences of adolescents engaged with gender diversity services: a qualitative approach. Psychol Sport Exerc 2025 [In review]. https://doi.org/10.1016/j.psychsport.2025.102826.Suche in Google Scholar PubMed
21. Staley, K. Exploring impact: public involvement in NHS, public health and social care research. Eastleigh: INVOLVE: National Institute for Health Research; 2009.Suche in Google Scholar
22. ESSA. Pre-exercise screening system (PSS): for young people [user guide] [internet]; 2021. Available from: https://www.essa.org.au/Common/Uploaded%20files/Tools%20and%20templates/Young%20People%20Pre%20Screening%20Tool%202021%20-%20Guidelines%20(1).pdf.Suche in Google Scholar
23. WHO. WHO guidelines on physical activity and sedentary behaviour: recommendations [internet]; 2020. Available from: https://www.ncbi.nlm.nih.gov/books/NBK566046/.Suche in Google Scholar
24. Liguori, G, American College of Sports Medicine. ACSM’s guidelines for exercise testing and prescription, 11th ed. Philadelphia: Lippincott Williams & Wilkins; 2020.Suche in Google Scholar
25. Meyer, IH. Resilience in the study of minority stress and health of sexual and gender minorities. Psychol Sex Orient Gender Divers 2015;2:209–13. https://doi.org/10.1037/sgd0000132.Suche in Google Scholar
26. Kelly, CM, Jorm, AF, Kitchener, BA. Development of mental health first aid guidelines on how a member of the public can support a person affected by a traumatic event: a Delphi study. BMC Psychiatry 2010;10:49. https://doi.org/10.1186/1471-244X-10-49.Suche in Google Scholar PubMed PubMed Central
27. Butler, H, Hare, D, Walker, S, Wieck, A, Wittkowski, A. The acceptability and feasibility of the Baby Triple P Positive Parenting Programme on a mother and baby unit: Q-methodology with mothers with severe mental illness. Arch Womens Ment Health 2014;17:455–63. https://doi.org/10.1007/s00737-014-0429-4.Suche in Google Scholar PubMed
28. Mustanski, B, Garofalo, R, Monahan, C, Gratzer, B, Andrews, R. Feasibility, acceptability, and preliminary efficacy of an online HIV prevention program for diverse young men who have sex with men: the keep it up! intervention. AIDS Behav 2013;17:2999–3012. https://doi.org/10.1007/s10461-013-0507-z.Suche in Google Scholar PubMed PubMed Central
29. Rosenbaum, S, Morell, R, Abdel-Baki, A, Ahmadpanah, M, Anilkumar, TV, Baie, L, et al.. Assessing physical activity in people with mental illness: 23-country reliability and validity of the simple physical activity questionnaire (SIMPAQ). BMC Psychiatry 2020;20:1–2. https://doi.org/10.1186/s12888-020-2473-0.Suche in Google Scholar PubMed PubMed Central
30. Lin, Y, Yu, Y, Zeng, J, Zhao, X, Wan, C. Comparing the reliability and validity of the SF-36 and SF-12 in measuring quality of life among adolescents in China: a large sample cross-sectional study. Health Qual Life Outcome 2020;18:1–4. https://doi.org/10.1186/s12955-020-01605-8.Suche in Google Scholar PubMed PubMed Central
31. Topp, CW, Østergaard, SD, Søndergaard, S, Bech, P. The WHO-5 Well-Being Index: a systematic review of the literature. Psychother Psychosom 2015;84:167–76. https://doi.org/10.1159/000376585.Suche in Google Scholar PubMed
32. Samouda, H, Langlet, J. Body fat assessment in youth with overweight or obesity by an automated bioelectrical impedance analysis device, in comparison with the dual-energy x-ray absorptiometry: a cross sectional study. BMC Endocr Disord 2022;22:195. https://doi.org/10.1186/s12902-022-01111-6.Suche in Google Scholar PubMed PubMed Central
33. Schubert, MM, Seay, RF, Spain, KK, Clarke, HE, Taylor, JK. Reliability and validity of various laboratory methods of body composition assessment in young adults. Clin Physiol Funct Imag 2019;39:150–9. https://doi.org/10.1111/cpf.12550.Suche in Google Scholar PubMed
34. Araujo-Moura, K, Souza, LG, Mello, GL, De Moraes, AC. Blood pressure measurement in paediatric population: comparison between automated oscillometric devices and mercury sphygmomanometers – A systematic review and meta-analysis. Eur J Paediatr 2022;181:1–4. https://doi.org/10.1007/s00431-021-04171-3.Suche in Google Scholar PubMed
35. Wind, AE, Takken, T, Helders, PJM, Engelbert, RHH. Is grip strength a predictor for total muscle strength in healthy children, adolescents, and young adults? Eur J Pediatr 2010;169:281–7. https://doi.org/10.1007/s00431-009-1010-4.Suche in Google Scholar PubMed
36. van den Beld, WA, van den Beld, WA, van der Sanden, GA, Sengers, RC, Verbeek, AL, Gabreëls, FJ. Validity and reproducibility of the Jamar dynamometer in children aged 4–11 years. Disabil Rehabil 2006;28:1303–9. https://doi.org/10.1080/09638280600631047.Suche in Google Scholar PubMed
37. Ojeda, ÁH, Maliqueo, SG, Barahona-Fuentes, G. Validity and reliability of the Muscular Fitness Test to evaluate body strength-resistance. Apunts Sports Med 2020;55:128–36. https://doi.org/10.1016/j.apunsm.2020.08.002.Suche in Google Scholar
38. YMCA of the USA. YMCA fitness testing and assessment manual. Champaign, IL: YMCA; 2000.Suche in Google Scholar
39. Weisstaub, G, González, J, Orizola, I, Borquez, J, Monsalves-Alvarez, M, Lera, L, et al.. Validity and reliability of the step test to estimate maximal oxygen consumption in paediatric population. Sci Rep 2025;15:592. https://doi.org/10.1038/s41598-024-84336-w.Suche in Google Scholar PubMed PubMed Central
40. Picot, B, Terrier, R, Forestier, N, Fourchet, F, McKeon, PO. The star excursion balance test: an update review and practical guidelines. Int J Athl Ther Train 2021;26:285–93. https://doi.org/10.1123/ijatt.2020-0106.Suche in Google Scholar
41. Almarjawi, AC, Wright, KE, Buist, BD, Cairney, J, Ton, TT, Furzer, BJ. Reliability of fitness assessments in children with emotional and behavioural difficulties. Paediatr Exerc Sci 2023;35:206–13. https://doi.org/10.1123/pes.2022-0058.Suche in Google Scholar PubMed
42. Castro-Piñero, J, Chillón, P, Ortega, FB, Montesinos, JL, Sjöström, M, Ruiz, JR. Criterion-related validity of sit-and-reach and modified sit-and-reach test for estimating hamstring flexibility in children and adolescents aged 6–17 years. Int J Sports Med 2009;30:658–62. https://doi.org/10.1055/s-0029-1224175.Suche in Google Scholar PubMed
43. Galletta, A, Cross, WE. Mastering the semi-structured interview and beyond: from research design to analysis and publication. New York: NYU Press; 2013.Suche in Google Scholar
44. Braun, V, Clarke, V, Weate, P. Using thematic analysis in sport and exercise research. In: Routledge handbook of qualitative research in sport and exercise. London: Routledge; 2016:213–27 pp.10.4324/9781315762012-26Suche in Google Scholar
45. Braun, V, Clarke, V. Conceptual and design thinking for thematic analysis. Qual Psych 2022;9:3–26. https://doi.org/10.1037/qup0000196.Suche in Google Scholar
46. Carlson, E, Nygren, F, Wennick, A. Critical friends: health professionals’ experiences of collegial feedback in a clinical setting. J Continuing Educ Health Prof 2018;38:179–83. https://doi.org/10.1097/CEH.0000000000000210.Suche in Google Scholar PubMed
47. Smith, B, McGannon, KR. Developing rigor in qualitative research: problems and opportunities within sport and exercise psychology. Int Rev Sport Exerc Psychol 2018;11:101–21. https://doi.org/10.1080/1750984X.2017.1317357.Suche in Google Scholar
Supplementary Material
This article contains supplementary material (https://doi.org/10.1515/teb-2025-0020).
© 2025 the author(s), published by De Gruyter on behalf of Shangai Jiao Tong University and Guangzhou Sport University
This work is licensed under the Creative Commons Attribution 4.0 International License.
Artikel in diesem Heft
- Frontmatter
- Section: Integrated exercise physiology, biology, and pathophysiology in health and disease
- The impact of exercise on the role of lipid droplets in maintaining health: a narrative review
- Effects of different interventions on microgravity-induced bone loss
- Section: Personalized and advanced exercise prescription for health and chronic diseases
- A therapeutic exercise program for adolescents engaged in gender diversity services: study protocol for a non-randomised clinical trial
- The role of exercise modality on psychological, behavioral, and fitness outcomes among individuals at risk of type 2 diabetes: preliminary evidence from the CHOICE pragmatic randomized trial
- Section: Physical activity/inactivity and health across the lifespan
- Serum metabolic alterations after two weeks of step-reduction and following four weeks of exercise rehabilitation in older adults: a secondary analysis of the ENDURE randomised controlled trial
- Calibration and evaluation of MET models for estimating energy expenditure using thigh and ankle-worn move 4 accelerometer
- Section: Sports medicine and movement science
- Muscular activity of hamstrings under attentional focus instructions: an electromyography based study
- Associations between anthropometric outcomes and fat percentage with physical performance in professional soccer players: a cutoff points approach
Artikel in diesem Heft
- Frontmatter
- Section: Integrated exercise physiology, biology, and pathophysiology in health and disease
- The impact of exercise on the role of lipid droplets in maintaining health: a narrative review
- Effects of different interventions on microgravity-induced bone loss
- Section: Personalized and advanced exercise prescription for health and chronic diseases
- A therapeutic exercise program for adolescents engaged in gender diversity services: study protocol for a non-randomised clinical trial
- The role of exercise modality on psychological, behavioral, and fitness outcomes among individuals at risk of type 2 diabetes: preliminary evidence from the CHOICE pragmatic randomized trial
- Section: Physical activity/inactivity and health across the lifespan
- Serum metabolic alterations after two weeks of step-reduction and following four weeks of exercise rehabilitation in older adults: a secondary analysis of the ENDURE randomised controlled trial
- Calibration and evaluation of MET models for estimating energy expenditure using thigh and ankle-worn move 4 accelerometer
- Section: Sports medicine and movement science
- Muscular activity of hamstrings under attentional focus instructions: an electromyography based study
- Associations between anthropometric outcomes and fat percentage with physical performance in professional soccer players: a cutoff points approach

